Abstract
Purpose: With the growing attention in pediatric rehabilitation services for supporting self-management, the need increases for more shared understanding of the concept. The aim of this study was to explore parent activation, associated factors of- and underlying perceptions on parental self-management of parents of children with chronic conditions.
Materials and methods: Using a mixed-methods strategy, first variations in self-management behaviors, motivation and perceived autonomy support were assessed with a cross-sectional survey among parents of children with chronic conditions (N = 239). Statistical analysis involved descriptive statistics and univariate analysis of variance. The survey was followed by 18 in-depth interviews with parents. Thematic analysis was used to recognize relevant topics in the qualitative data.
Results: In the survey most parents reported being active self-managers. Nevertheless, only one third persisted in self-management when under stress. Autonomous motivation was strongly associated with parental self-management. In the interviews, parents mentioned attuning with professionals and finding balance as important aspects of self-management. To facilitate self-management, professionals were expected to have expert knowledge, be engaged and empathic.
Conclusion: From the perspective of parents, self-management should be viewed as a collaborative effort in which they are supported by professionals, rather than having to manage it “by themselves”.
To facilitate self-management, parents expect professionals to have expert knowledge and additionally show interpersonal competences as openness, engagement and empathy.
Motivating parents may facilitate their level of self-management regarding the care for their child with a chronic disorder.
Good communication and collaboration with professionals appear to be key aspects of parental self-management.
Parents expect pediatric rehabilitation teams to tune their services to the needs, desires and expectations of parents to support them in “self-managing” the care for their child.
Implications for rehabilitation
Introduction
Self-management has emerged as an important theme in the ongoing development of pediatric rehabilitation. These services provide interdisciplinary treatment to children and adolescents experiencing problems in their activities and participation due to an illness or health condition with consequential impairments, mostly also in motor functions [Citation1]. Chronic conditions self-management appears in governmental policy plans as a strategic target to foster autonomy of persons with chronic conditions, both for organizing as well as defraying various forms of support and care [Citation2,Citation3]. Policies aiming to promote autonomy and individualize treatment stem largely from humanitarian and/or emancipatory ideals. Equality, individual freedom, and self-determination are acknowledged as fundamental human rights [Citation4,Citation5] that may be compromised for citizens facing chronic conditions due to the way care is delivered. Additionally, chronic conditions have grown in numbers worldwide due to changes in life-style and increased survival despite health risks. Chronic health issues nowadays affect approximately 25% of the group of children and youth, represented in for instance asthma, obesity, attention-(hyper)activity disorder, and concomitants of prematurity or congenital syndromes due to improved treatment and pre-/neonatal care like cerebral palsy and Down syndrome [Citation6]. As such, chronic conditions have become one of the major threats to public health and a growing economic burden on society. Curbing these threats is considered a collective responsibility, where primary care systems need to adopt and support self-management of these health issues [Citation3,Citation7].
In healthcare for pediatric populations, parents play a central and crucial role. Studies on family-centred care, in which children and their parents are a central intervention focus, suggest that services need to be tuned to both parents’ and children's needs and expectations [Citation8–10]. Essential for effective support is therefore to understand their conception of self-management [Citation11].
Conceptions of self-management
Health policies already feature a diversity of conceptions of self-management [Citation12]. People with chronic conditions need continuous access to healthcare providers and deal with a broad range of professionals over prolonged periods of time. Self-management places persons with a chronic condition and their families at the center of their own health care, optimizing their ability for participation in their health process. Effective self-management empowers people through knowledge acquisition about their conditions. It actively engages them in shared goal setting with professionals, in discussion of treatment preferences and planning of daily care, in alignment with their abilities, social needs, values, and other priorities in life [Citation13]. The General Self-Management Model developed in the Netherlands by the Dutch Institute for Health Care Improvement (CBO) [Citation14] emphasizes communication, partnership, trust, and respect between professionals and people with illnesses or disorders.
Parental Self-management, applied to parents of children with chronic conditions, would be reflected in the competences of parents in terms of their knowledge, skills and confidence to actively participate in the healthcare processes concerning their child’s development, health and well-being. Rehabilitation professionals should empower parents and their children for such engagement, taking differences in individual needs, desires and possibilities into account [Citation15].
Motivation and self-management
In the light of the shifting views and expectations regarding disability and healthcare [Citation16], researchers such as Shogren and Turnbull [Citation17] have focused on processes in which self-determination of children with disabilities and their families are emphasized. Self-Determination Theory (SDT) as described by Ryan and Deci [Citation18] in general offers an explanation how external factors, such as an illness or chronic condition, are likely to diminish well-being. According to SDT, when people perceive that adapting to such condition contributes to the satisfaction of their basic psychological needs for autonomy, relatedness, and competence, this can lead to a long-term increase of their well-being. [Citation19,Citation20]. Research on self-determination-oriented healthcare interventions fostering positive health behaviors, such as physical activity or smoking cessation, showed more success if people were autonomous motivated and if professionals were perceived as autonomy supportive [Citation21–24]. Although the research evidence is still limited, theoretical and empirical arguments suggest that also for parents, perceived autonomy supportive pediatric rehabilitation and concomitant autonomous motivation are associated with stronger self-management. Besides SDT, also another theoretical framework, the Theory of Planned Behavior [TPB], argues that the adherence to a certain behavior is influenced by one’s motivation [Citation25–27]. Studies on TPB-based self-management practices emphasize the impact of attitudes to self-management behavior [Citation28] and of social context, including family, friends and community [Citation29] on a person’s motivation for self-management.
There is growing attention for chronic condition self-management within the field of pediatric rehabilitation. However, the concept of parental self-management remains relatively underexplored, especially the views of parents, and how they perceive their participation and relations in the rehabilitation processes regarding their child [Citation30,Citation31]. Positive associations between parent involvement and self-management were reported in recent studies on parental support and self-management in adolescents with diabetes [Citation32,Citation33]. Barlow et al. [Citation34] underlined the positive effects of a focus on self-management for parents of children with a chronic condition in coping with consequences of those conditions on their lives, such as stress, social isolation, insufficient time or lack of comprehension and compassion by others.
Parents of children with chronic conditions express a wide range of desires, needs and expectations [Citation35–37], so the meaning, experiences and values linked to self-management can vary as well. Conceptions of self-management may affect therapy goals and approaches [Citation38]. What is an optimal approach for one individual, may well be insufficient or overdone for the other [Citation39]. Thorough consideration of parents’ role and how exactly they facilitate their child’s autonomy is, therefore, suggested [Citation30]. Increased insight in parental perspective can help to tune-in to their individual needs and preferences, improving engagement between families with complex needs and healthcare services [Citation11]. This study adds to the existing literature by focusing on the meaning and value of self-management to parents, their motivations and their expectations of healthcare professionals.
The purpose of the current study was to quantitatively and qualitatively describe the various perceptions on parental self-management of parents of children with chronic conditions using pediatric rehabilitation services. Associations were explored between different self-management experiences, perceived autonomy support and motivation, and demographic factors as age, gender, education, family structure and family income suggested in literature [Citation40–43].
The following research questions were addressed:
To what extent do parents of children with chronic conditions report active forms of self-management?
Are perceived autonomy support, autonomous motivation for self-management and self-reported activity regarding self-management interrelated?
Are demographic factors (parental age, gender, education, family income, relationship status and illness severity associated with parents’ self-reported activity regarding self-management?
What are the views, expectations, perceived barriers and facilitators of parents concerning self-management?
Materials and methods
Design
In this study a mixed-methods design was used. According to a sequential explanatory strategy [Citation44] parents’ activation regarding self-management and possible associated factors were quantitatively explored in Phase A with a cross-sectional survey. In Phase B semi-structured interviews were conducted with parents scoring over the full range of the spectrum, using qualitative analysis to obtain deeper understanding of the underlying views, expectations, perceived barriers and facilitators that might relate to their activation regarding self-management. Data integration has been performed as described by Fetters and colleagues [Citation45]. On the methods level, quantitative data were linked to the qualitative data in the sampling frame through connecting in which interview participants were selected based on their scores in the survey. On the report level, a contiguous approach was followed describing the quantitative and qualitative results in two separate sections. The qualitative results were reported as a narrative. In the Discussion section, the findings from quantitative and qualitative analyses were synthesized.
The context of the investigation regarded two Dutch centers for rehabilitation where parents and their children with a chronic condition received rehabilitation services over longer periods of time, provided by professionals from nine pediatric rehabilitation teams.
Sample and procedures
Phase a
In total 608 parents of children receiving treatment from participating pediatric rehabilitation institutes, were invited by post to participate in an online survey on parental self-management. Parents were also offered the possibility to fill out the questionnaire paper-based, or by face-to-face interview. Included were parents with a child aged 0–12, with a chronic condition according to the description of Mokkink et al. [Citation46]. Excluded were parents with children not receiving any actual interdisciplinary treatment at the time of the investigation. A cut off at age 12 was chosen because until this age, according to Dutch legislation regarding “Medical Treatment Agreement” [Citation47], parents have full right of decision about the intervention.
Phase B
All parents participating in the survey were asked for permission to approach them again during the second phase of the study for a 45–60-min semi-structured interview on their perceptions of self-management. Ultimate selection of the interviewees was based on maximum variation purposeful sampling [Citation48]. Depending on their scores on the Parent-PAM, parents over the full available spectrum of levels of activity regarding self-management were included. To broaden the diversity of opinions, individual information of participants on motivation, perceived autonomy support, and demographic variables like gender, age, income, education and relationship status, retrieved from the survey were also considered during the inclusion process.
Invitation for the interviews was performed stepwise by telephone in an iterative process of data collection and data analysis, until saturation was achieved from qualitative coding of the content. Most parents were interviewed at home. Some chose to be interviewed at the rehabilitation center where their child received treatment. Each interview initially focused on several basic questions but could explore different aspects of self-management depending on the responses of the interviewee. All dialogs were audio recorded and transcribed verbatim immediately afterwards.
Ethical considerations
Reflexivity This study has been conducted from a critical emancipatory paradigm for health care research [Citation49]. The investigators aimed to contribute to the empowerment of parents for self-management in accordance with their preferences and abilities, and to strengthen their position as partners of the rehabilitation professionals involved with their child. They belief that for partnership comprehension of parents’ perspectives by professionals is essential. This contributed to their choice for a mixed methods approach and to actually give parents voice through the narrative presentation of the qualitative data extracts.
According to the researchers’ view people can be their own agent of change. For this reason, the study has been conceptualized within the theoretical framework of SDT. As SDT emphasizes on support of basic needs to become motivated for self-management, the interviews also focused on experiences and expectations of parents regarding the support of professionals. The main researcher is a pediatric rehabilitation professional who in his clinical work experiences how both professionals and parents can struggle with their roles regarding self-management (support). To promote trustworthiness, a second researcher without a clinical role was involved in the iterative process of data collection and extraction. Integration and presentation of the quantitative and qualitative findings were characterized by ongoing reflective discussion within the research group.
All parents were asked for informed consent, for the survey as well as for the interviews. Confidentiality of all information retrieved from the study and anonymity in relation to any future reports were guaranteed. The study was accepted by the Scientific Quality Committee of Amsterdam Public Health research institute and the Scientific and Ethical Review Committee of Vrije Universiteit Amsterdam, and by the boards of the involved rehabilitation centers.
Instruments
Phase A
Parent activation regarding self-management
The self-reported activation of parents regarding self-management, expressed in their knowledge skills and confidence, was measured with use of the Parent-Patient Activation Measure [Parent-PAM] (©Insignia Health 2013). The Parent-PAM is an adapted version of the Patient Activation Measure [PAM-13] developed by Hibbard et al. [Citation50], which is a 13-item, Gutman like, 0–100 incremental scale, measuring self-management of one’s health or chronic condition. A Dutch validation study of the PAM-13 supported convergent validity of the PAM-13NL with the SBSQ-D, an instrument for measuring health literacy [Citation51].
The Parent-PAM was previously used in a study on parental activation in hematopoietic stem cell transplant demonstrating sufficient internal consistency reliability (α = 0.85), in line with the Dutch PAM-13 (α = 0.88). That investigation also reported sufficient agreement between PAM-13 and Parent-PAM regarding the distributions of the four levels: belief in an active role; confidence and knowledge to take action; taking action; and staying the course under stress [Citation11].
Motivation
The Treatment Self-Regulation Questionnaire [TSRQ] assessed types of motivation for parents to engage in self-management. This instrument was developed by Williams et al. [Citation52] and used in a population of adults with obesity to measure their motivation to follow a weight-loss and maintenance program at a community hospital in the USA. Their study identified two subscales: controlled, externally regulated reasons and intrinsic, autonomous reasons. The TSRQ has been modified for use in various studies about the motivation for health behaviors. A more recent validation study across three health behaviors, namely smoking, diet and physical exercise, among 2731 adult participants at four universities in de United States, showed acceptable internal consistency reliabilities (α = 0.73 to 0.93) [Citation53]. The TSRQ has different versions varying from 9 up to 19 questions. Some versions also include a subscale amotivation. In this study, a 12-item version of the TSRQ was used with subscales controlled motivation and autonomous motivation.
Perceived autonomy support
Perceived support for self-management from pediatric rehabilitation professionals like the physician, physiotherapist, occupational therapist, speech and language therapist, social worker or psychologist working with their child, was measured with the Healthcare Climate Questionnaire [HCCQ]. The instrument has 15 items and uses a 7-point Likert scale. The HCCQ was developed and tested in the same study as the TSRQ, and high internal consistency was found (α = 0.96) [Citation52]. Research testing Self-Determination Theory in oral-self care, also reported good internal consistency and validity of the HCCQ [Citation23].
Not all questionnaires used in the survey were available in Dutch language and none of the questionnaires were used before in the same population as this investigation. Therefore, translation of the instruments and slight rephrasing of some items took place to improve suitability. The translation and/or adaptation process followed international guidelines delineated by Beaton et al. [Citation54] and the World Health Organization (WHO) [Citation55]. The steps included, translation of the instrument from English to Dutch, synthesis within the project group, back translation to English by a native speaker with expert knowledge of the Dutch Language, testing in an expert panel together with cognitive interviewing, and final adaptations to the questionnaires.
For each of the instruments used in this study, internal consistencies of scale and subscales were computed, expressed in Cronbach’s α. Reliability of the translated and adapted HCCQ, TSRQ and Parent-PAM in this study was adequate ().
Table 1. Internal consistency reliabilities of the adapted instruments.
To investigate the factor structure, a Confirmatory Factor Analysis (CFA) was conducted using Mplus. The model fit was evaluated by four fit indices. Chi-square, RSMEA, CFI and TLI [Citation56]. Values suggested a reasonable fit for HCCQ (one domain) and TSRQ (two factors). Additional Rasch analysis of the Parent-PAM confirmed a one factor structure, justifying its use in the Dutch setting. Given the adequate internal consistency reliability scores, the original scale structures of the instruments were retained.
Phase B
To explore the perceptions of parents regarding self-management, a semi-structured interview was developed with seven main questions (). The questions were formulated by the researcher and discussed with members of the research group. Subsequently these were adapted, piloted with three parents, and using parents’ feedback finalized for use in the interviews.
Table 2. Basic interview questions.
Data analysis
Phase A
Descriptive group statistics were computed in SPSS 24. Distributions, skewness and kurtosis, missing values and outliers were investigated. Pearson correlations were computed between the three relevant constructs autonomy support, motivation and self-management. (significant at p < 0.05). Associations between demographic factors and self-management were tested by General Linear Model Univariate Analysis of Variance.
Phase B
Qualitative analysis of the semi-structured interviews was performed following a cyclic scheme, involving repeated coding and recoding of earlier and next interviews. Data were analyzed by means of coding, categorization and theme identification, with use of NVIVO 11 (© QSR International Pty Ltd). This method resembled the open coding and axial coding process often described in grounded theory [Citation57]. To enhance the credibility of the qualitative analysis, each transcript was summarized and sent to corresponding participants for member checking. All analyzed transcripts were reviewed by a second researcher who commented on the findings and proposed new topics and codes, or a rephrasing of existing codes. Based on the discussions between both researchers, adjustments and/or additions were made. A third investigator was asked for peer feedback on a regular basis, for suggestions and to evaluate whether data were appropriately interpreted, and procedures were respected.
Results
Phase A
In total 239 of 608 parents took part in the survey (response rate 39%). The two most frequent reasons for nonparticipation were, I am too busy, and I already participate in other research. Characteristics of the samples of the survey and the interviews can be found in .
Table 3. Characteristics of the samples.
Parent activation, motivation and perceived autonomy support for self-management
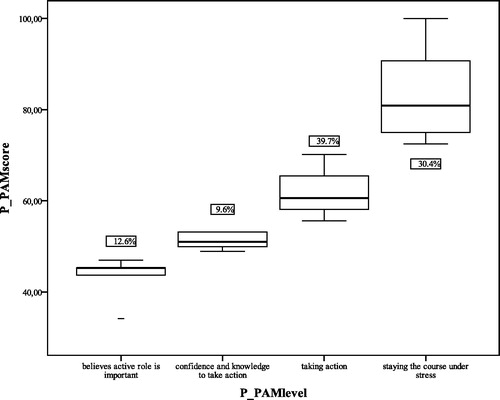
Regarding the first research question how parents report concerning their active self-management, 12.6% of the parents believed an active role is important (Parent-PAM level 1) and 9.6% thought they also had confidence and knowledge to become active (Parent-PAM level 2). According to the Parent-PAM both level one and two were not really active self-managers though; 39.7% of the parents actually took action (level 3), but only 30.5% of all parents took action and could also maintain this under stress (level 4), .
The scores of parents on the Parent-PAM had a mean of approximately 65 on a 0–100 scale, indicating that on average parents perceived themselves as active, but had difficulties to continue this during stressful periods. For descriptive statistics of the Parent-PAM, the TSRQ and the HCCQ ().
Table 4. Descriptive statistics of the Parent-PAM, TSRQ and HCCQ.
The mean scores of parents on their motivation for self-management and of their perceived autonomy support, were measured on a 1–7 Likert scale. Based on the means of the TSRQ, parents reported to be highly autonomous (intrinsic) motivated and less influenced by extrinsic factors. Also, the relatively high HCCQ mean score suggested that parents perceived professionals as fairly autonomy supportive.
Associated factors of parental self-management
With respect to the second and third research question, perceived autonomy support was weakly positively associated with autonomous motivation (r = 0.14, p = 0.037) Autonomous motivation was strongly associated with self-reported parental activation (r = 0.51, p = 0.000). Neither perceived autonomy support nor controlled motivation was associated with parental activation (p = 0.052 and p = 0.715, respectively). However, perceived autonomy support appeared to be weakly negatively associated with illness severity of the child (r= −0.15, p = 0.022).
Univariate variance analyses showed that demographic factors (parental gender, education level, income, relationship status) and illness severity jointly explained 6% of the variance in parental activation (F(8, 197)=1.59; p = 0.129) and no individual factor was significantly related to self-reported parental activation, except for parental age which was associated with higher levels of activation (ß = 0.01; F(1, 206)=6.17, p = 0.014).
Phase B
The fourth research question addressed the underlying perceptions of parents regarding self-management. In total 18 parents were interviewed. The age of the parents varied between 26 and 55 years with an average age of 37.7. During the qualitative analytic process, the interviews could be structured around four general topics. Several themes were identified ().
Table 5. General topics and identified themes.
The variety of parent opinions is reflected in the narrative overview of themes and topics, with accompanying quotes. After each quote some demographic information on the respondent is added, Sex (M/F); Age parent (years); Living with or without partner (Partner/No-Partner - P/NP); Age child (years).
The perspectives of parents underlying their motivations for self-management were expressed in their attitudes towards self-management, the expectations they had of professionals, and the external factors that influenced their self-management processes.
Attitudes towards self-management
The attitudes of parents could be categorized in terms of their views, values and competences regarding self-management. Parents gave a broad variety of ‘views’ on the general concept of self-management in relation to the care for their child. Some parents articulated that self-management involves “making one’s own decisions”: That you are the one deciding in what way your child will develop. That you decide what happens with your child, which therapies it gets (F;27;NP;3). For other parents, self-management meant having more possibilities to “become engaged” in the treatment process of their child: That the professional would take me seriously as “manager” of the care for my child (F;39; P;10). Although all parents agreed that a focus on promoting self-management and autonomy of citizens in “governmental policy” in principle is a good development, there also were major concerns: It is good to look what people can do themselves, but then they for instance say about my child, can’t a neighbor just help out? But that is not possible, not with his background. To work with him you really need specific training (F;44;NP;6). While some parents saw self-management as a process in which they are in the lead, for others the professional should be the one to give direction. Nevertheless, all parents emphasized that for self-management, though not experienced by everybody as a free choice, “partnership” and “collaboration” with professionals are essential, as one parent concluded: That name self-management. It is a bit misleading: “Self”, it actually should be called: together-management (F;30;P;2).
Parents specifically endorsed the “value” of self-management, with as main reason that they are ones ultimately responsible for the care for their child and therefore, need to be in the lead: Do you have another choice? I would almost say. For me it goes without saying. If doctors take over and I as a parent lose authority, it will not work. This is about ownership (M;31;P;1).
With regard to their “competence” for self-management, most of the interviewed parents stated that it is important to obtain “adequate knowledge” about the condition of their child. Parents described parental self-management as a continuous “learning process”. They often felt insecure especially during the first years, but by learning becoming more confident and skilled over the course of time, developing “self-efficacy”: To be thrown into the deep, some will manage, but others probably will not at all. I myself had to learn this through the years. I totally wasn’t a person who would persevere in something. I really had to learn that (F;33;P;8).
Expectations regarding self-management support
The assumptions of parents concerning the support for self-management by professionals could be divided into three groups. In the “relationship with professionals” it was essential for parents to “feel acknowledged” and be able to “trust” the professional. If those lacked, working together would be difficult. Parents furthermore pointed out that their relationship with the professional was influenced by his or her “personal traits” such as age, experience, and character: It is more about the person himself. My current physiotherapist and I, we really get along well together. So, you make contact much more easily (F;39;P;10). Concerning the “expertise of professionals”, parents first and foremost expected professionals to have “state-of-the-art knowledge” about the problems of their child. Nevertheless, parents also expected more general “interpersonal skills” of professionals. The ability to tune-in was considered essential. With other professionals, but also tuning-in to the differences between parents: She does that very well with those differences between me and my partner. She maneuvers exactly in between, taking both of us seriously (F;51;P;8).
Most expectations of parents were actually related to the “attitude of professionals”. “Openness”, “empathy”, and “engagement” were were important themes to parents. Engagement went beyond a more academic involvement, as formulated by one of the parents: Well, besides my child getting what she needs, the only thing I really expect of professionals, is “love”. If you work with children with disabilities you really need to have your heart in what you do (F;27;NP;3). “Clarity and guidance” were also considered critical aspects of professional attitude, positive, or negative when lacking: They are all trying to help, but in the end, you are the one who must decide… It is such a difficult process in which I would have liked a bit more guidance (F;48;P;10). Some parents specifically mentioned the professional’s “attitude towards their child”, for instance whether there was a click or not: With his current therapist, he doesn’t have that connection, which means he does other things, misbehaves (F;32;P;5).
In summary, though parents had a wide diversity of expectations of self-management support, they most of all expected support that fitted their own individual situation the best, as one parent stated: I really believe their commitment is sincere, but it is the difference between a professional who knows how to push the right buttons and the one who does not (F;42;P;5).
Factors influencing self-management
Parents experienced several external factors that supported or impeded their self-management processes. In the category “obstructing factors”, “planning problems” often appeared a recurrent nuisance for many parents: …only the planning, really! They for instance plan a therapy session on Friday half past two in the afternoon. Then my child behaves badly every week and messes things up, which could be expected since it is end of the week (F;32;P;5). Also, the accessibility of the planning office was indicated by many parents as frustrating: They are only reachable in the mornings. I work at those hours and when I have a moment, I get the answering machine: you must call between eight and twelve, and I think: But I’m calling between eight and twelve (F;30;P;6)?!
Another impediment was “bureaucracy”, especially in relation to procedures concerning helping aids: So, we needed a new wheelchair. I notice this and bring it up to the rehabilitation team. They conclude the same. But then local government also must come, and another independent professional must have a look. Meanwhile several months have passed and I still have no wheelchair for my child (F;38;P;6). Last, “lack of coordination” was regularly mentioned as an obstructing factor, for instance related to appointments for team-meetings with professionals. Coordination could also be related to the therapy frequencies of children: It is quite a lot that my child receives, physiotherapy, occupational therapy, speech and language therapy, which is too much for him (F;48;P;10).
“Communication” was indicated most often as “supporting factor” of self- management. Parents emphasized the importance of short lines of communication. Among professionals themselves, but also referring to parent-professional contact: That you can say what is on your mind, even without having an appointment (F;35;P;10). If physical communication was not possible, indirect contact for instance through email or a communication notebook was valued too. “Continuity” of professionals was described by several parents as a supporting factor as well: I appreciate that my child works with some therapists who are there over such a long period of time, that they get to know him very well (F;48;P;10). “Flexibility” was another theme that arose: Then it becomes a tailor-made approach. That you look which parent is up to it and which parent is not. Parents who are not able to self-manage, please keep investing in them (F;39;P;10).
Finally, “parent-to-parent contact” was reported repeatedly in the interviews: I think parent meetings could help. Parents who exchange their experiences, I really think it could help (F;42;P;5).
Degree of self-management
When asked to elaborate on the extent to which they considered themselves active self-managers, some parents stated that to become a self-manager, “acceptance” of the situation was necessary, which obviously was not that easy, as expressed by a mother who said: You take up everything you think is possible. Though in the end nothing really fitted. I just wanted too much at the same time, which cost me a lot of energy (F;48;P;10). Several parents emphasized the necessity of “taking initiative”. Furthermore, “finding balance” for instance between self-managing and asking for support was a dilemma for many parents: I find it very difficult. On one hand, you want to take the lead, but on the other hand personally I would be happy if somebody would take over, or partially (F;30;P;2). Balancing self-management with the needs of the partner or the rest of the family also was a recurring issue: It is sometimes quite difficult because you are in a family with two other children as well. They also ask a lot of energy (F;44;P;3). …. When a balance was found though, this created space for positive development: In a way, we now have the feeling that everything makes sense. We are all happy and we can combine the situations well. We have gotten a totally new way of life (F;40;P;2).
Discussion
Perspectives on and experiences with self-management varied widely among parents of children with chronic conditions using pediatric rehabilitation services. Nevertheless, synthesis of the quantitative and qualitative data revealed several noteworthy relations between the level of activity regarding self-management reported by parents in the survey and the underlying views and experiences mentioned during the interviews.
The impact of stress on parental self-management
Although in the survey according to their scores on the Parent-PAM about two-thirds of the parents reported to be active self-managers in the care for their child, more than half of those parents could not sustain this in stress situations. Approximately one-fifth of all parents reported not to be active at all. Thus, while pediatric rehabilitation has embraced parental involvement as a guiding principle [Citation58–60] to enhance outcomes for children [Citation61,Citation62], active parental self-management cannot be presumed for all parents, all the time. During the succeeding interviews, almost all parents reported that balancing between self-management and support, within the family, with a partner, and/or with work remained a continuous challenge. Given the fact that parents of children with chronic conditions are prone to high levels of anxiety and stress [Citation61,Citation63,Citation64], the strength of active self-management is a relevant concern for professionals supporting parents. Disbalance in the functioning of parents or family situation may be associated with both mental as physical health of children with chronic conditions [Citation65] and should, therefore, continuously be considered.
The role of motivation and perceived support
The survey showed that parents considered themselves autonomously motivated for parental self-management and not very much influenced by extrinsic factors. Additionally, autonomous motivation went along with active parental self-management. Consistent with Self-Determination Theory and in line with other findings in the health field [Citation66–68], parents’ perceived autonomy support from professionals was positively associated with their autonomous motivation. Even though no causal conclusions can be drawn, this suggests a potential pathway for professional conduct that contributes to parental autonomous motivation and in turn to parental self-management [Citation61,Citation69]. Furthermore, illness severity of the child was negatively associated with the autonomy support perceived by parents, which might indirectly influence their motivation for self-management. Professionals should, therefore, be attentive to the increasing risk of alienation in their relationship with parents, depending on the severity of the condition of the child [Citation12].
Adequate communication was mentioned in the interviews as one of the most important supporting factors of parental self-management, corroborated in studies on parent engagement [Citation70,Citation71]. The flip side was that if the communication process was flawed, this also immediately had a negative impact on parents’ perceptions. Such statements of parents endorse the possible association between supportive professional behavior and parents’ motivations for active engagement in self-management.
Age and the learning process
The association of age with parental activation in the survey parallels remarks made by parents in the interviews when they described self-management as a learning process in which they gradually, as their child became older and their own experience grew, felt more confident and competent “self-managers”. Parental self-management as a learning process that becomes easier with age and experience, is reaffirmed by Alsem et al. [Citation72] and Kratz et al. [Citation61] in studies about parents’ perspectives and chronic illness management. This dynamical character of self-management implies that professionals should be continuously attentive to the changing context of individual parents and children from the start throughout the full course of treatment [Citation32,Citation73,Citation74].
Self-management support - a personalized process
There were considerable differences in the reported levels of parental self-management during the survey, as well as in the desired amount and form of involvement in the management process of their children expressed in the interviews. Still, all consulted parents underscored that self-management is a way to take responsibility for one’s own child. However, parents also acknowledged that self-management may not always be feasible for every parent. Therefore, subsidiary, tailor-made self-management support for all parents delivered by professionals remains important [Citation58,Citation75]. Such focused support may address the most important impediments to effective self-management according to the parents, which were related to therapy planning, availability of the planning office, and bureaucratic procedures. Similar organizational issues were previously delineated by Kratz et al. [Citation61] in a study on childhood chronic illness management.
Need for additional skills of professionals
Parents' expectations in relation to self-management support went beyond “state of the art” knowledge of professionals about the chronic condition. Both, parents scoring high and low on active parental self-management in the survey, indicated that they also expected interpersonal skills and attitudes of professionals, like openness, empathy and engagement. Van Houtum et al. [Citation76] argued, based on a nationwide study on chronic disease self-management in the Netherlands, that perceived needs related to self-management tasks and support are more often general rather than specific to the occurring chronic condition at hand. Studies on parent and child engagement in mental healthcare confirm that professionals should possess discipline transcending competences to be able to tune-in to each specific child and parents, to be sensitive and responsive to their context, and to induce trust and engagement by listening, empathy, emotional attendance and use of relational skills [Citation77].
Limitations
Although parents with a minority cultural background and low education were represented in both the survey as well as the interview study, but their number was lower than found in the general population [Citation78,Citation79]. Furthermore, the current study does not include children’s and adolescents’ own perspectives on self-management, which are relevant as well [Citation62]. The cross-sectional, single-informant, self-report design of the study makes the findings inconclusive regarding causal direction, although the relevance of presented associations is underscored by the qualitative results. The 39% response to the survey should be taken into account before the findings are generalized beyond the investigated samples.
Implications for practice and further research
Parents who are adapting to self-management may recognize their individual struggles and dilemmas within the diversity of perceptions and reflections reported in this study. This diversity accentuates the need for professionals to address strength of active self-management in individual parents as well as variation within parents across time. Since autonomous motivation was identified as a significant factor associated with parental activation for self-management and perceived autonomy support correlated positively with motivation, interpersonal skills in scaffolding parents’ personal growth in this area of life is an important competence domain for professionals. The organizational barriers to self-management identified by the parents in this study should trigger rehabilitation institutes to make their services more parent-friendly, lower the level of stress, and thereby improve the support of self-management. In implementing these changes, attention may be necessary towards the perceptions, attitudes and types of motivation of pediatric rehabilitation professionals themselves towards self-management support.
Conclusion
The findings in this study confirm existing literature [Citation61,Citation80–82] explaining chronic conditions self-management as a process in which collaboration and partnership with professionals are essential. If there is one lesson that could be drawn from this study, it would be that from the perspective of parents the concept of self-management in the care for their child with a chronic condition, is considered more a matter of together-management rather than managing it “by themselves”.
Acknowledgements
This study was conducted at Merem Medical Rehabilitation and De Hoogstraat Rehabilitation in the Netherlands and was generously supported by its staff and management. Special thanks of the authors go to the site ambassadors and to all parents who participated in the study.
Disclosure statement
There are no declarations of interest reported by the authors.
Additional information
Funding
References
- Pangalila R, Becher J, Maathuis K, Kinderrevalidatie in Nederland [Paediatric rehabilitation in the Netherlands]. In: Hadders-Algra M, Maathuis K, Pangalila R, et al. eds. Kinderrevalidatie. (fifth revised ed.). Assen: Koninklijke Van Gorcum BV. 2015. p. 5–27.
- Zwar N, Harris M, Griffiths R, et al. A systematic review of chronic disease management. Research Centre for Primary Health Care and Equity, School of Public Health and Community Medicine, UNSW 2006; [cited 2018 Feb 23]. Available from: http://rsph.anu.edu.au/research/projects/systematic-review-chronic-disease-management
- Nolte E, McKee M, Knai C. Managing chronic conditions: an introduction to the experiences in eight countries. In: Nolte E, Knai C, McKee M, editors. Managing chronic conditions: experiences in eight countries. Copenhagen: European Observatory on Health Systems and Policies, WHO; 2008 [2018 cited Feb 23]. p. 1–15. Available from: http://apps.who.int/iris/bitstream/10665/107920/1/E92058.pdf?ua=1
- United Nations. Universal declaration of human rights. [cited 2018 Mar 1]. Available from: http://www.un.org/en/universal-declaration-human-rights/
- United Nations. International covenant on civil and political rights. 1976 [cited 2019 Mar 1]. Available from: http://www.ohchr.org/Documents/ProfessionalInterest/ccpr.pdf
- Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303:623–630.
- WHO (World Health Organization). Innovative care for chronic conditions: building Blocks for Action. 2002 [cited 2018 Mar 1]. Available from: http://www.who.int/chp/knowledge/publications/icccreport/en/
- Palisano RJ, Almarsi N, Chiarello LA, et al. Family needs of parents of children and youth with cerebral palsy. Child Care Health Dev. 2010;36:85–92.
- Jeglinsky I, Autti-Rämö I, Brogren Carlberg E. Two sides of the mirror: parents’ and service providers’ view on the family-centeredness of care for children with cerebral palsy. Child Care Health Dev. 2012;38:79–86.
- McDowell BC, Duffy C, Parkes J. Service use and family-centred care in young people with severe cerebral palsy: a population based, cross-sectional clinical survey. Disabil Rehabil. 2015;37:2324–2329.
- Pennarola BW, Rodday AM, Mayer DK, et al. Factors associated with parental activation in pediatric hematopoietic stem cell transplant. Med Care Res Rev. 2012;69:194–214.
- Lawn S, McMillan J, Pulvirenti M. Chronic condition self-management: expectations of responsibility. Patient Educ Couns. 2011;84:e5–e8.
- Australian Health Ministers’ Advisory Council. National strategic framework for chronic conditions. Canberra: Australian Government; 2017. [cited 2018 Apr 20]. Available from: http://www.health.gov.au/internet/main/publishing.nsf/content/nsfcc
- CBO (Dutch Institute for Health Care Improvement). Kort & Krachtig: Generiek model zelfmanagement [General Model Self-management]. Zelfzorgondersteund- instrumentenkiezer. 2011 [cited 2018 Mar 1]. Dutch. Available from: http://zelfzorgondersteund-instrumentenkiezer.nl/wp-content/uploads/2016/03/KortKrachtig-GeneriekModel2011.pdf
- Pulvirenti M, McMillan J, Lawn S. Empowerment, patient centred care and self-management. Health Expect. 2014;17:303–310.
- Huber MH. How should we define it? BMJ. 2011;343:235–237.
- Shogren KA, Turnbull AP. Promoting self-determination in young children with disabilities; the critical role of families. Infants Young Child. 2006;19:338–352.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;5:68–78.
- Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psychol. 2008;49:82–185.
- Ryan RM, Patrick H, Deci EL, et al. Facilitating health behaviour change and its maintenance: interventions based on self-determination theory. Eur Health Psychol. 2008;10:2–5.
- Williams GC, Deci EL. Activating patients for smoking cessation through physician autonomy support. Med Care. 2001;39:813–823.
- Ryan RM, Williams GC, Patrick H, et al. Self-determination theory and physical activity: the dynamics of motivation in development and wellness. Hell J Psychol. 2009;6:107–124.
- Münster Halvari AE, Halvari H, Bjornebekk G, et al. Motivation and anxiety for dental treatment: testing a self-determination theory model of oral self-care behaviour and dental clinic attendance. Motiv Emot. 2010;34:15–33.
- Farholm A, Halvari H, Niemiec CP, et al. Changes in return to work among patients in vocational rehabilitation: a self-determination theory perspective. Disabil Rehabil. 2017;39:2039–2046.
- Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process. 1991;50:179–211.
- Ajzen I. Perceived behavioural control, self-efficacy, locus of control, and the theory of planned behaviour. J Applied Soc Psych. 2002;32:665–683.
- Javadi M, Kadkhodaee M, Yaghoubi M, et al. Applying theory of planned behavior in predicting of patient safety behaviors of nurses. Mater Sociomed. 2013;25:52–55.
- Hagger SM, Hardcastle SJ, Hingley C, et al. Predicting self-management behaviors in familial hypercholesterolemia using an integrated theoretical model: the impact of beliefs about illness and beliefs about behaviors. Int J Behav Med. 2016;23:282–294.
- Lee LT, Bowen PG, Mosley MK, et al. Theory of planned behavior: social support and diabetes self-management. JNP. 2017;13:265–270.
- Lindsay S, Kingsnorth S, McDougall C, et al. A systematic review of self-management interventions for children and youth with physical disabilities. Disabil Rehabil. 2014;36:276–288.
- Almasri N, An M, Palisano RJ. Parents' perception of receiving family-centered care for their children with physical disabilities: a meta-analysis. Phys Occup Ther Pediatr. 2018;38:427–443.
- Dashiff C, Suzuki-Crumley J, Kracke B, et al. Cystic fibrosis related diabetes in older adolescents: parental support and self-management. J Spec Pediatr Nurs. 2013;18:42–53.
- Goethals ER, Oris L, Soenen B, et al. Parenting and treatment adherence in type 1 diabetes throughout adolescence and emerging adulthood. J Pedatr Psychol. 2017;42:922–932.
- Barlow J, Swaby l, Turner A. Perspectives of parents and tutors to a self-management program for parents/guardians of children with long-term and lifelimiting conditions: a life raft we can sail along with. J Community Psychol. 2008;36:871–884.
- Siebes RC, Ketelaar M, Gorter JW, et al. Needs of families with children who have a physical disability: a literature review. Crit Rev Phys Rehabil Med. 2012;24:85–108.
- Alsem MW, Siebes RC, Gorter JW, et al. Assessment of family needs in children with physical disabilities: development of a family needs inventory. Child Care Health Dev. 2014;40:498–506.
- Terwiel M, Alsem MW, Siebes RC, et al. Family-centred services: differences in what parents of children with cerebral palsy rate important. Child Care Health Dev. 2017;43:663–669.
- Wiart L, Ray L, Darrah J, et al. Parents’ perspectives on occupational therapy and physical therapy goals for children with cerebral palsy. Disabil Rehabil. 2010;32:248–258.
- Trappenburg J, Jaarsma T, van Os-Medendorp H, et al. Self-management: one size does not fit all. Patient Educ Couns. 2013;92:134–137.
- Neylon OM, O'Connell MA, Skinner TC, et al. Demographic and personal factors associated with metabolic control and self-care in youth with type 1 diabetes: a systematic review. Diabetes Metab Res Rev. 2013;29:257–272.
- Hernandez R, Ruggiero L, Riley BB, et al. Correlates of self-care in low-income African American and Latino patients with diabetes. Health Psychol. 2014;33:597–607.
- Wilski M, Tasiemski T, Kocur P. Demographic, socioeconomic and clinical correlates of self-management in multiple sclerosis. Disabil Rehabil. 2015;37:1970–1975.
- Protheroe J, Whittle R, Bartlam B, et al. Health literacy, associated lifestyle and demographic factors in adult population of an English city: a cross-sectional survey. Health Expect. 2017;20:112–119.
- Creswell JW. Chapter 10, Mixed methods procedures. Research design: qualitative, quantitative and mixed methods approaches. (third edition) London: Sage Publications. 2009.; p. 203–223.
- Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs - principles and practices. Health Serv Res. 2013;48:2134–2156.
- Mokkink LB, van der Lee JH, Grootenhuis MA, et al. Defining chronic diseases and health conditions in childhood (0-18 years of age): National Consensus in the Netherlands. Eur J Pediatr. 2008;167:1441–1447.
- Dutch Ministry of Health, Welfare and Sport. Wet inzake Geneeskundige Behandelovereenkomst (WGBO) [Law on Medical Treatment Agreement]. Burgerlijk Wetboek 7, afd.5, art. 446-468. Overheid. [cited 2018 Mar 10]. Dutch. Available from: http://wetten.overheid.nl/BWBR0005290/2017-1010#Boek7_Titeldeel7_Afdeling5
- Palinkas LA, Horwitz SM, Green CA, et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42:533–544.
- Tijmstra J, Boeije H. Benaderingen van onderzoek. [Research approaches]. In: Boeije H, ’t Hart H, Hox J, editors. Onderzoeksmethoden 8ste geheel herziene druk. [Research methods. eighth fully revised version]. Den Haag: Boom Lemma; 2009. p.64–101. Dutch.
- Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the Patient Activation Measure. Health Serv Res. 2005;40:1918–1930.
- Rademakers J, Nijman J, Van der Hoek L, et al. Measuring patient activation in the Netherlands: translation and validation of the American short form Patient Activation Measure (PAM13). BMC Public Health. 2012;12:1–7.
- Williams GC, Grow VM, Freedman ZR, et al. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–126.
- Levesque CS, Williams GC, Elliot D, et al. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviours. Health Educ Res. 2006;22:691–702.
- Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. SPINE. 2000;25:3186–3191.
- WHO (World Health Organization). Process of translation and adaptation of instruments. [cited 2018 Mart 1]. Available from: http://www.who.int/substance_abuse/research_tools/translation/en/
- Schreiber JB, Nora A, Stage FK, et al. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res. 2006;99:323–338.
- Boeije H. Analyseren in kwalitatief onderzoek [Analysing in qualitative research]. Den Haag: Boom Lemma. 2012. Chapter 4, Methoden en technieken van kwalitatieve analyse. [Methods and techniques of qualitative analysis]. p. 84-121. Dutch.
- Rosenbaum P, Gorter JW. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012;38:457–463.
- Cross A, Rosenbaum P, Grahovac D, et al. Knowledge mobilization to spread awareness of the “F-words” in childhood disability: lessons from a family researcher partnership. Child Care Health Dev. 2015;41:947–953.
- Ketelaar M, Bogossian A, Saini M, et al. Assessment of the family environment in pediatric neurodisability: a state-of-the-art review. Dev Med Child Neurol. 2017;59:259–269.
- Kratz L, Uding N, Trahms N, et al. Managing childhood chronic illness: parent perspectives and implications for parent-provider relationships. Fam Syst Health. 2009;27:303–313.
- Schwartz DD. Axelrad ME. Chapter 7, The role of parents. Healthcare partnerships for pediatric adherence: promoting collaborative management for pediatric chronic illness care. Houston: SpringerBriefs in Public health. 2015; p. 91–101.
- Lach LM, Kohen DE, Garner RE, et al. The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disabil Rehabil. 2009;31:607–618.
- Parkes J, Caravale B, Marcelli M, et al. Parenting stress and children with cerebral palsy: a European cross-sectional survey. Dev Med Child Neurol. 2011;53:815–821.
- Leeman J, Crandell JL, Lee A, et al. Family functioning and the well-being of children with chronic conditions: a meta-analysis. Res Nurs Health. 2016;39:229–243.
- Patrick H, Williams GC. Self-determination theory: its application to health behavior and complementarity with motivational interviewing. Int J Behav Nutr Phys Act. 2012;9:18–12.
- Shigaki C, Kruse RL, Mehr D, et al. Motivation and diabetes self-management. Chronic Illn. 2010;6:202–214.
- Koponen AM, Simonsen N, Suomen S. Quality of primary health care and autonomous motivation for effective diabetes self-management among patients with type 2 diabetes. Health Psychol Open. 2017;4:1–9.
- Haskard Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834.
- King G, Desmarais C, Lindsay S, et al. The roles of effective communication and client engagement in delivering cultural sensitive care to immigrant parents of children with disabilities. Disabil Rehabil. 2015;37:1372–1381.
- Alsem M, Ausems F, Verhoef M, et al. Information seeking by parents of children with physical disabilities: an exploratory qualitative study. Res Dev Disabil. 2017;60:125–134.
- Alsem MW, Verhoef M, Gorter JW, et al. Parents’ perceptions of the services provided to children with cerebral palsy in the transition from preschool rehabilitation to school-base services. Child Care Health Dev. 2016;42:455–463.
- Orrell-Valente JK, Cabana MD. 'The apple doesn't fall far from the tree': the role of parents in chronic disease self-management. Curr Opin Pediatr. 2008; 20:703–704.
- Van Houtum L, Rijken M, Groenewegen P. Do everyday problems of people with chronic illness interfere with their disease management? BMC Pub Health. 2015;15:1–9.
- Fordham L, Gibson F, Bowes J. Information and professional support: key factors in the provision of family-centred early childhood intervention services. Child Care Health Dev. 2012;38:647–653.
- van Houtum L, Rijken M, Heijmans M, et al. Patient-perceived self-management tasks and support needs of people with chronic illness: generic or disease specific? Ann Behav Med. 2015;49:221–229.
- King G, Currie M, Petersen P. Child and parent engagement in the mental health intervention process: a motivational framework. Child Adolesc Ment Health. 2014;19:2–8.
- CBS. Bevolkingsontwikkeling; migratieachtergrond en generatie [Population growth; migration background and generation]. StatLine. [cited 2018 Apr 16]. Dutch. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/70751ned/table?ts=1523914608251
- CBS. Sociale monitor, welvaart en welzijn in de Nederlandse samenleving [Social monitor, welfare and well-being in the Dutch Society. ]. StatLine. [cited 2018 Apr 16]. Dutch. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/81573NED/table?ts=1523915290217
- Battersby M, von Korf M, Schaefer J, et al. Twelve evidence-based principles for implementing self-management support in primary care. Jt Comm J Qual Patient Saf. 2010;36:561–570.
- Palisano RJ, Chiarello LA, King GA, et al. Participation-based therapy for children with physical disabilities. Disabil Rehabil. 2012;34:1041–1052.
- Bartlett D, Chiarello LA, Hjorngaard T, et al. Moving from parent “consultant” to parent “collaborator”: one pediatric research team’s experience. Disabil Rehabil. 2017;39:2228–2235.