Abstract
Purpose
Employment of young adults with chronic physical conditions entering the labor market after finishing post-secondary education remains behind compared to typically developing peers. The aim of this study is to evaluate changes in their paid employment levels after following a vocational rehabilitation intervention (‘At Work’).
Materials and methods
Participants aged between 16 and 27 years (n = 90) were recruited via rehabilitation physicians and a jobcoach agency and participated in a vocational rehabilitation program. Cochran’s Q and McNemar tests served to test the development of intervention participants’ paid employment over time. Chi-square tests were used to compare intervention participants’ paid employment level with national reference data selected on age and having a self-reported chronic physical condition.
Results
Paid employment level of the intervention cohort significantly increased from 10.0% at baseline to 42.4% at 2-years follow-up (p < 0.001). At 2-years follow-up, their employment rates approached the employment rates of national reference data (42.4% versus 52.9%, p = 0.17).
Conclusion
Starting from a disadvantaged position, the paid employment rate of the intervention cohort substantially increased over time, approaching the employment rate of reference data. ‘At Work’ seems to be appropriate for supporting this specific group who face obstacles to enter the labor market, to find competitive employment.
‘At Work’ is a vocational rehabilitation intervention for young adults with chronic physical conditions who experience problems with finding and maintaining competitive employment after finishing post-secondary education.
The ‘At Work’ intervention entails a combination of group sessions and individual coaching sessions based on the supported employment methodology.
Paid employment rates of the intervention cohort substantially increased on the short- and long term, and approached employment rates of reference data of persons with chronic physical conditions.
The ‘At Work’ intervention seems appropriate to support young adults with chronic physical conditions who experience barriers for work participation, to enter the labor market and find competitive and sustainable employment.
IMPLICATIONS FOR REHABILITATION
Introduction
Advancements in medical care enable the vast majority of children with chronic physical conditions to live into adulthood [Citation1,Citation2]. Emerging adulthood represents a critical developmental stage for all young people as they experience multiple transitions including leaving high school, finishing post-secondary education, getting a job, forming new personal relationships and moving out of parents’ homes to live on their own [Citation3,Citation4]. Previous studies consistently report that young people with chronic physical conditions more often experience restricted autonomy and societal participation [Citation3,Citation5,Citation6], and need support in developing adult roles [Citation3,Citation7–9]. Roebroeck and colleagues underlined the need for incorporating a lifespan perspective throughout pediatric and adult healthcare [Citation8]. From this perspective, Young Adult Teams of health care professionals have been set up, which proved to be useful in supporting young adults’ social participation, for instance by providing group-based interventions focusing on specific life areas [Citation8,Citation10].
In the process of transition into adulthood, one of the challenges is to find work [Citation11–14]. Young adults with chronic physical conditions experience substantial difficulties, such as problems with disability disclosure, traveling to work, limited accessibility of buildings, limited adaptation of workplaces or working conditions, discrimination, lack of support of manager or colleagues, low self-esteem and lack of life skills [Citation9,Citation12,Citation15–19]. In persons with chronic physical conditions, low employment rates are common in both Europe and the USA [Citation20,Citation21]. Adequate support in finding and keeping work may result in optimal work participation, and may prevent lifelong financial dependency, unemployment, and poor quality of life [Citation22,Citation23].
Several interventions are developed to support young people with chronic physical conditions in finding and maintaining employment. Most of these interventions mainly address the development of more general life skills or provide support in finding temporary jobs as a student [Citation24–29]. To our knowledge, none of these programs are primarily focused on support for entering the labor market after finishing post-secondary education, and to this aim the ‘At Work’ program was developed [Citation24,Citation25]. ‘At Work’ is a vocational rehabilitation program provided by the Young Adult Teams of three out-patient rehabilitation clinics in The Netherlands. The intervention includes a combination of group education, peer-mentorship, individual jobcoaching based on the supported employment methodology, and experimental learning. These intervention elements are evaluated as useful and appropriate to improve psychosocial development and vocational participation among young people with chronic conditions [Citation24,Citation25,Citation28–31]. Studies on existing programs that address the development of life skills in general or provide support in finding temporary jobs during education, showed some positive preliminary results [Citation25–29]. However, there are relatively few rigorously designed, published studies that have evaluated the effectiveness of life skills and vocational rehabilitation programs for young adults with physical disabilities, and there is a need for large-sample studies in this field [Citation25,Citation28]. So far, also the ‘At Work’ program was only evaluated in a feasibility study (n = 12), indicating increased paid employment rates from 8% at baseline to 33% and 42% at 1-year and 2-years follow-up [Citation32].
Therefore, the current study aims to evaluate changes in employment rates, in a large cohort of participants of the ‘At Work’ program. Employment rates at baseline (T0), post-intervention (T1) and 2-years follow-up (T2) were assessed for intervention participants and compared to external national reference data of young adults with chronic physical conditions. Due to the disadvantaged starting position of intervention participants – since they entered the intervention because of difficulties in finding and maintaining competitive employment – we assumed that, at the start of the intervention the paid employments rates within the intervention cohort were lower compared to those of the national reference data. We hypothesized that a) within the intervention cohort, the rates of paid employment will significantly increase in 2 years’ time; and b) the paid employment rates of the intervention cohort at 2-years follow-up after baseline will equal the rates of the reference data of young adults with chronic physical conditions, thus overcoming their disadvantaged employment participation.
Materials and methods
Design
Cohort study with 2-years follow-up after baseline, and comparison with external national reference data selected on age (16–30 yrs) and having a self-reported chronic physical condition.
Vocational rehabilitation intervention: ‘at work’
‘At Work’ is a multidisciplinary vocational rehabilitation intervention for young people (16–27 years) with chronic physical conditions. Participants have finished their post-secondary education and experienced difficulties in finding and/or maintaining competitive employment, i.e., not seasonal or temporary. The intervention aims to improve young adults’ life skills and to provide support for their vocational participation [Citation32,Citation33]. A detailed overview of the content of the intervention is presented elsewhere [Citation30].
The 1-year program integrates vocational services provided by a job coach of a reintegration company into rehabilitation services provided by a Young Adult Team of an outpatient rehabilitation clinic. The intervention consists of six two-hour group sessions, facilitated by an occupational therapist and a job coach. A psychologist is involved in some group sessions addressing psychological issues. Group sessions aim to empower young adults and, thus, increase participants’ self-efficacy, knowledge, work-skills and awareness of their own values and needs [Citation34,Citation35]. Participants learn to apply for a job, to negotiate for workplace modifications or adjustment of working conditions, to disclose their condition and to feel self-efficacious in dealing with work-related problems. Group sessions entail peer-support, modelling, experimental learning and education. These intervention elements are evaluated as useful and appropriate to improve young adults’ life skills and to provide support for their vocational participation [Citation24,Citation25,Citation28–30]. Topics that are discussed during the group meetings consider work and health, interests and capacities, social benefits and insurances, searching for vacancies and performing a job-interview. The intervention continues with weekly individual coaching sessions based on the supported employment methodology [Citation31]. These sessions are provided by a job coach for about one year. This coaching entails help in finding and applying for a suitable job, and support for dealing with the social and physical work environment, i.e., informing the employer and colleagues about the chronic physical condition, and arrangement of workplace modifications or adjusted working conditions. If necessary, an occupational therapist could be consulted during the individual coaching trajectory.
Recruitment intervention cohort
The vocational rehabilitation intervention was developed in 2007, and from that point until now provided at outpatient rehabilitation clinics with Young Adult Teams. In the current study we included all young adults that participated in the intervention in the period 2007–2016. Three rehabilitation centers participated: Rijndam Rehabilitation/Erasmus MC (Rotterdam), Reade Rehabilitation Centre (Amsterdam) and Basalt (Leiden). These centers collaborated with the job coach agency ‘VolZin’. Young adults with chronic physical conditions were referred to the intervention by a rehabilitation physician, if they met each of the following inclusion criteria: a) aged between 16 and 27 years, b) unemployed or not suitably employed, defined as a job that is not consistent with the individual’s education, physical abilities and preferences, c) had finished education, or will finish education within 6 months; d) an adequate understanding of the Dutch language and d) no severe intellectual impairments. All participants received verbal and written information about the study. If they were willing to participate in the study they signed an informed consent form. The medical ethics committee of Erasmus MC Rotterdam approved this study (MEC-2012-381) and all participating centers granted local approval.
Measurements intervention cohort
Procedure
Data of intervention participants in the period 2007–2009 were collected as part of a prospective feasibility study [Citation32,Citation33] using self-report questionnaires. Data of participants in the period 2009–2012 were collected by clinical monitoring of background characteristics and employment status of the intervention participants. Data of intervention participants in the period 2012–2016 were gathered in a prospective using self-report questionnaires. All measurements were performed at baseline (T0), post-intervention (T1, 1-year after baseline) and 2-years follow-up after baseline (T2). All over the years, the same operationalization of variables and measurement instruments were s used.
With regard to the clinical monitoring, data on background characteristics, and status of paid and unpaid employment were prospectively registered at the reintegration company and outpatient rehabilitation clinics. For the present study these data were extracted from the clients’ charts and entered in a digital data-extraction form by two researchers.
Outcome measures
In the intervention cohort, paid employment (primary outcome), and unpaid employment and unemployment (secondary outcomes) were assessed independently (0 = no; 1 = yes). Paid employment is defined as performing a paid job for at least 12 h per week, in accordance with the definition of Statistics Netherlands at the time of this study [Citation36,Citation37].
Background characteristics
Background characteristics were assessed at T0. In the intervention cohort, age, gender, onset of chronic physical condition (0 = acquired; 1 = congenital), special education (0 = no; 1 = yes), recipient of disability benefits (0 = no; 1 = yes), paid work experience (0 = no; 1 = yes), unpaid work experience (0 = no; 1 = yes), and job search period (0 = not yet; 1 = 0–1year; 2= > 1 year) were recorded. Educational level was operationalized based upon the International Standard Classification of Education (ISCED): (0) low = pre-vocational practical education or lower (ISCED levels 1 or 2); (1) medium = pre-vocational theoretical education or upper secondary vocational education (ISCED levels 3 (vocational), 4 or 5); (2) high = general secondary education, higher professional education, or university (ISCED levels 3 (general), 6 or higher) [Citation38,Citation39]. Severity of physical limitations was assessed using the 7-item indicator developed by Organization for Economic Cooperation and Development (OESO), assessing physical limitations (3 items) and limitations in hearing and seeing (4 items) on a 4-point Likert scale (1 = no physical limitations; 2 = slight physical limitations; 3 = moderate physical limitations; 4 = severe physical limitation). The severity of physical limitations was classified as severe if at least one item scored 4, as moderate if at least one item scored 3, as slight if at least one item scored 2, and as no limitations if all items scored 1. This measure has a good reliability (Cronbach’s alpha = 0.79) [Citation40]. At baseline, problems related to competitive employment were identified using the Canadian Occupational Performance Measure (COPM) [Citation41]. The COPM is designed to help patients identify important problems they experience in occupational performance in the domains of selfcare, productivity and leisure [Citation42]. In a semi-structured interview a person selects a maximum of five prioritized activities that he or she wants, needs, or is expected to perform. Since we focused on problems related to competitive employment, we only report problems in the domains productivity and self-care (precondition for work). The COPM has good validity and interrater reliability, and is useful for young adults with physical disabilities [Citation43].
External national reference data of young adults with chronic physical conditions
Data were collected by Statistics Netherlands, as part of a national health survey. In order to match the national reference data to the intervention cohort we used data of young adults a) with a self-report chronic physical condition, b) aged between 16 and 30 years; c) who indicated the severity of their physical limitations on the OESO-indicator [Citation40]; and d) were recruited in the period 2007–2016. Each year Statistics Netherlands recruited a new population [Citation37], and, in total, reference data of 2024 responders were used in the current study: 68.5% of them reported no physical limitations; 23.1% slight physical limitations; 4.6% moderate physical limitations; and 3.8% severe physical limitations. Responders of the reference data indicated whether they had a paid job for at least 12 h per week, comparable with participants in the intervention cohort. Since the yearly employments rates in the period 2007 till 2016 and the number of respondents in a specific year were slightly differed between years, we calculated an averaged employment rate for the period 2007–2016, weighted for the number of respondents in a specific year. The averaged employment rate was also specified for four subgroups according to the severity of physical limitations.
Analysis
Descriptive statistics were used to describe the characteristics of the intervention cohort. Chi-square tests for dichotomous variables and independent t-tests for continuous variables were used in order to check for selective drop-out of responders at T1 and T2. Cochran’s Q test served to test the overall development of intervention participants’ employment rate (paid employment, unpaid employment and unemployment) over time. Post-hoc McNemar tests were used to compare paired proportions at two different assessment moments (0 to 1 yr; 0 to 2 yr; 1 to 2 yr). Similar analyses were conducted for subgroups regarding severity of physical limitations.
Chi-square statistics were applied to compare the paid employment rates of the intervention cohort at baseline and at 2-years follow-up to the national reference data and the effects were estimated by means of the relative risk ratios (RRs). For all analyses IBM SPSS Statistics version 21.0 (Chicago, USA) was used and the predefined level for statistical significance was 5%.
Results
Background characteristics of the intervention cohort
Background characteristics of the intervention cohort (n = 90) are presented in . Participants had a mean age of 24.5 years (SD = 3.0) at baseline, 14.4% had no physical limitations, 45.6% slight physical limitations, 20.0% moderate physical limitations and 20.0% severe physical limitations. Most of the participants had an acquired chronic condition (67.7%), a medium educational level (62.9%), were disability benefit recipient (75.6%), had prior paid work experience (77.6%) and/or unpaid work experience (64.9%). At baseline, most intervention participants reported problems with employment (77.8%), such as problems with finding a suitable job, writing an application letter, or doing a job interview. They also reported problems in preconditions for employment, such as housekeeping (50.0%), e.g., too tired after work to cook healthy food; functional mobility (38.9%), e.g., problem with transport to work or acquiring a driving license; personal care (31.5%), e.g., problems with dressing up in time; and education (9.3%), e.g., problems with finding a job that is consistent with their educational background or their education did not fit with their physical abilities.
Table 1. Background characteristics intervention cohort at baseline, post-intervention, and 2-years follow-up.
Among the intervention cohort, nine participants could not be traced or did not respond for the assessment at post-intervention (T1), and twenty-six participants were lost at 2-years follow-up after baseline (T2). At T1, non-responders were more often male (88.9%; p = 0.03). Both at T1 and T2, non-responders were younger (mean age = 21.3 and 23.0 years respectively; p < 0.001 and p = 0.01 respectively). In addition, at T2 non-responders more often received disability benefits at baseline (64.0%; p = 0.03), had more prior paid work experience (63.7%; p = 0.04) and were less often searching for a job for more than one year (9.1%; p = 0.01). None of these characteristics correlated with the outcome measure paid and unpaid employment, and unemployment post-intervention and at two years follow-up.
Development of employment rates over time within the intervention cohort; and a comparison with external national reference data
Of the intervention cohort, nine participants (10.0%) had paid employment at baseline. Their jobs at that time, did not fit with their interests (n = 1); educational level (n = 5) e.g., student jobs or sheltered employment; physical capacities (n = 2); or reason for work switch was unknown (n = 1). All participants having paid employment post-intervention and at 2-years follow-up, found competitive employment, i.e., not sheltered. They were active in several sectors, for example ICT, healthcare, finance, retail, and education.
Overall, at baseline the paid employments rates of the intervention cohort were significantly lower compared to the national reference data of young adults with physical conditions (10.0% versus 52.9%, p < 0.001, RR = 0.19). Within the intervention cohort, paid employment significantly increased over time. The rates of paid employment were significantly higher at both post-intervention and 2-years follow-up (30.9%, 95%CI = 20.8–41.0; and 42.2%, 95%CI = 32.1–56.3 respectively) compared to baseline (10.0%, both p’s < 0.001). At 2-years follow-up the paid employment rate among the intervention participants (42.2%) approached the rate among the national reference data (52.9%, p = 0.17, RR = 0.80) (; ).
Figure 1. Development of paid employment rates within the intervention cohort, and a comparison with national reference data. ^Significant development over time within the intervention cohort. a,bSignificantly differs from baseline within the intervention cohort. *Significantly differs from national reference data.
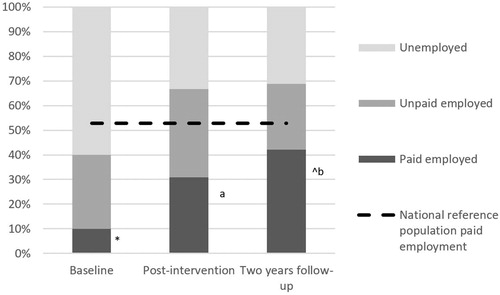
Table 2. Employment rates within the intervention cohort, and a comparison with national reference data.
Unpaid employment rates increased from 30.0% at baseline to 35.8% post-intervention and thereafter decreased to 26.6% at 2-years follow-up (). However, this development over time was not significant (p = 0.55).
Subgroups analyses according to the severity of physical limitations
For all four severity subgroups within the intervention cohort (i.e., no, slight, moderate and severe physical limitations), the paid employment rates at baseline were significantly lower compared to the paid employment rates of the corresponding subgroups of the national reference data (respectively 23.1% versus 56.0%, p = 0.02, RR = 0.79; 9.8% versus 50.6%, p ≤ 0.001, RR = 0.19; 5.6% versus 40.9%, p = 0.003, RR = 0.14; and 5.6% versus 29.2%, p = 0.03, RR = 0.19).
Rates of paid employment in the intervention cohort increased over time in all severity subgroups, but this development was only significant in the subgroups slight and severe physical limitations (p = 0.002 and p = 0.01 respectively). The paid employment rate of participants with slight physical limitations significantly increased from 9.8% at baseline to 36.8% (95%CI = 21.5–52.1) post-intervention (p = 0.03), whereas, the employment the rates of participants with severe physical limitations significantly increased from 5.6% at baseline to 40.0% (95%CI = 15.2–64.8) at 2-years follow-up (p = 0.03) (; .
Figure 2. (a) Development of paid employment rates of subgroup no physical limitations within the intervention cohort, and a comparison with national reference data. *Significantly differs from national reference data. (b) Development of paid employment rates of subgroup slight physical limitations within the intervention cohort, and a comparison with national reference data. ^Significant development over time within the intervention cohort. a,bSignificantly differs from baseline within the intervention cohort. *Significantly differs from national reference data. (c) Development of paid employment rates of subgroup moderate physical limitations within the intervention cohort, and a comparison with national reference data. *Significantly differs from national reference data. (d) Development of paid employment rates of subgroup severe physical limitations within the intervention cohort, and a comparison with national reference data. ^Significant development over time within the intervention cohort. bSignificantly differs from baseline within the intervention cohort. *significantly differs from national reference data.
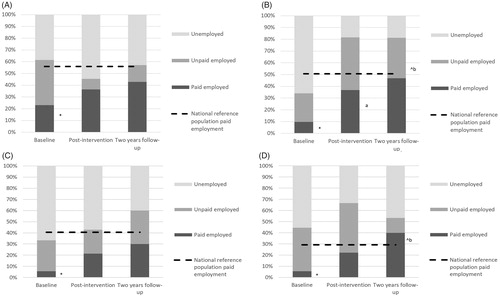
At 2-years follow-up, paid employment level of all subgroups of the intervention cohort approached the rates of the corresponding subgroups of national reference data (no physical limitation, p = 0.37, RR = 0.79; slight physical limitation, p = .42, RR = 0.93; moderate physical limitation, p = 39, RR = 0.74; severe physical limitation, p = .28, RR = 1.40) (; ).
Discussion
In the present study we evaluated changes in young adults’ employment rates after participating in a vocational rehabilitation intervention. Starting from a disadvantaged position, the paid employment rate of the intervention cohort substantially increased on the short- and long term, and approached the employment rate of reference data of young adults with chronic physical conditions. In addition, intervention participants that achieved paid employment found a job in a competitive work environment. We evaluate these results as positive, considering the disadvantaged starting position of the intervention participants as compared to respondents of the national reference data. The reason is that the intervention cohort only included persons reporting problems in finding competitive employment, whereas the reference data also included persons who did not experience any employment problems, notwithstanding their chronic physical condition.
Most vocational programs for youth with disabilities as described in the literature are provided during adolescence, and facilitate the transition to temporary or seasonal employment [Citation27–29]. Being engaged in education or doing temporal or seasonal work during adolescence is considered important, because it improves the psychosocial development, by providing a context for developing life skills and exploring personal interests and abilities [Citation11,Citation44]. However, previous studies showed that some young adults still lag behind in life skill development when finishing post-secondary education and they need more time to get ready for work [Citation45,Citation46]. Some other authors of studies advised to provide this specific subgroup with tailored support [Citation46], and the present results showed that ‘At Work’ may be an effective vocational rehabilitation intervention to fill this gap.
The ‘At Work’ intervention is, to our knowledge, among the first that is specifically developed for those young adults facing barriers to enter the competitive labor market. The program entails group sessions combining different components, such as peer-support, role-playing, and skills training, that are aimed to support life skills development, as well as job coach sessions aimed to support job placement and sustainable work participation. Results of previous studies showed that these components of the ‘At Work’ program, are perceived appropriate and effective to support life skill development of young adults [Citation24–26,Citation28]. In addition, on-the-job training and job placement assistance were found to be effective for improving work participation of adults with chronic physical conditions [Citation47,Citation48].
In our study we further specified intervention outcomes for subgroups with different levels of experienced physical limitations. We choose to estimate this by the OESO-indicator, since this was also available in the reference data. However, although the intervention cohort consisted of young people with chronic physical conditions who report problems with finding competitive employment, some of them reported no physical limitations according to the OESO-indicator. People in this subgroup are those without impairments in seeing, hearing or walking, but they still may have other physical impairments, for example chronic pain, that were not included in the indicator. Also, some of them might have other impairments in neuropsychological functioning which may influence their work participation, such as in attention, response inhibition, or memory, for example patients with an acquired brain injury [Citation12]. Therefore, participants indicating no physical limitations on the OESO-indicator may still face problems when they enter the labor market or experience a negative impact of their chronic physical condition on their work participation. The question arises whether a classification based on severity of these specific physical limitations according to the OESO indicator is the most appropriate to get insight in intervention effects for specific subgroups with different levels of experienced impact of their chronic physical condition. It seems relevant to take other aspects, such as the participant’s work readiness into account, when differentiating effects of vocational rehabilitation interventions between subgroups. However, these additional data were not available in the national reference data, and we had to use the same definition of experienced impact of the chronic physical condition in both populations in order to allow comparison of the intervention cohort to national reference data.
Strengths and limitations
This is the first study, to our knowledge, that evaluates the effects of a vocational rehabilitation intervention on work participation in a large sample of young people with chronic physical conditions who experienced problems in finding competitive employment after finishing post-secondary education. Insights into effects of these types of interventions are important, since the work participation of young people with chronic physical conditions is known to lag behind compared to healthy age-mates [Citation20,Citation21,Citation49].
The subgroup analyses entailed less power in each subgroup which may have led to trends that were not statistically significant, especially in the subgroups of no and moderately physical limitations. However, the subgroup analyses provided some additional information about intervention outcomes for persons with different severity levels regarding physical limitations in the present intervention cohort, that included a wide range of chronic physical conditions.
Since the ‘At Work’ program focused on a heterogeneous sample of young adults with a wide range of chronic physical conditions, it is not possible to relate findings to specific conditions. The heterogeneity of the population, however, is considered as a strong point of the intervention, since young adults with different chronic physical conditions may face similar challenges entering the labour market [Citation50]. In fact, intervention participants recognized and learned from each other’s experiences during the group sessions [Citation30].
There is some discrepancy between the intervention cohort and the external national reference data regarding the type of chronic conditions. The intervention cohort consists of young adults with physical disabilities in rehabilitation care, whereas the reference data includes young adults with a broader range of chronic physical conditions, also addressing chronic conditions such as asthma or diabetes. Possibly, this difference might have influenced the estimated employment rates. Therefore it is worthwhile to directly compare the intervention cohort to a control group of young adults with similar chronic physical conditions, who are known in rehabilitation care but did not participate in the intervention.
Conclusion
Starting from a disadvantaged position, the level of paid work participation of the intervention cohort substantially increased on the short- and long term, and approached the level of work participation of national reference data of young adults with chronic physical conditions. The combination of group sessions and job coaching seems to be appropriate to support this specific group of young adults with chronic physical conditions who experience barriers in finding competitive and sustainable employment after finishing their post-secondary education.
Acknowledgements
The authors are grateful to all the young people that filled in the questionnaires. Rijndam Rehabilition (Monique Floothuis OT MSc, Lineke Verhoef OT, Gera Hakkesteegt OT, and Wilma van der Slot MD, PhD), Basalt Leiden (Winnifred Molenaar and Carin Fröberg OT), Reade, and Bureau VolZin (Natascha van Schaardenburgh OT, Theo Blom OT, and Jolie Derkx OT) are thanked for their efforts on recruiting participants and for providing the ‘At Work’ intervention. Hogeschool Rotterdam (Joan Verhoef PhD) is thanked for their valuable contribution to the study design. This work was supported by SIA-RAAK, the Foundation Innovation Alliance with funding from the Dutch ministry of Education, Culture and Science (OCW) (PRO-02-025).
Disclosure statement
The authors have no competing interests to declare
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- WHO. World report on disability. Geneva: World Health Organization; 2010.
- White PH. Access to health care: health insurance considerations for young adults with special health care needs/disabilities. Pediatrics. 2002;110(6 Pt 2):1328–1335.
- Chamberlain MA, Kent RM. The needs of young people with disabilities in transition from paediatric to adult services. Eura Medicophys. 2005;41(2):111–123.
- Gorter JW, Stewart D, Woodbury-Smith M. Youth in transition: care, health and development. Child Care Health Dev. 2011;37:757–763.
- Donkervoort M, Roebroeck M, Wiegerink D. Determinants of functioning of adolescents and young adults with cerebral palsy. Disabil Rehabil. 2007;29(6):453–463.
- King GA, Baldwin PJ, Currie M, et al. Planning successful transitions from school to adult roles for youth with disabilities. Child Health Care. 2005;34(3):195–216.
- Nieuwenhuijsen C, van der Laar Y, Donkervoort M, et al. Unmet needs and health care utilization in young adults with cerebral palsy. Disabil Rehabil. 2008;30(17):1254–1262.
- Roebroeck ME, Jahnsen R, Carona C, et al. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51(8):670–678.
- Lindsay S, McPherson AC, Maxwell J. Perspectives of school-work transitions among youth with spina bifida, their parents and health care providers. Disabil Rehabil. 2017;39(7):641–652.
- Bent N, Tennant A, Swift T, et al. Team approach versus ad hoc health services for young people with physical disabilities: a retrospective cohort study. Lancet. 2002;360(9342):1280–1286.
- Lindsay S. Employment status and work characteristics among adolescents with disabilities. Disabil Rehabil. 2011;33(10):843–854.
- Achterberg TJ, Wind H, de Boer AG, et al. Factors that promote or hinder young disabled people in work participation: a systematic review. J Occup Rehabil.. 2009;19(2):129–141.
- van Mechelen MC, Verhoef M, van Asbeck FW, et al. Work participation among young adults with spina bifida in the Netherlands. Dev Med Child Neurol. 2008;50(10):772–777.
- Verhoef JA, Bramsen I, Miedema HS, et al. Development of work participation in young adults with cerebral palsy: a longitudinal study. J Rehabil Med. 2014;46(7):648–655.
- Shier M, Graham J, Jones ME. Barriers to employment as experienced by disabled people: a qualitative analysis in Calgary and Regina, Canada. Disabil Soc. 2009;24(1):63–75.
- Roessler R, Neath J, McMahon B, et al. Workplace discrimination outcomes and their predictive factors for adults with multiple sclerosis. Rehabil Couns Bul. 2007;50(3):139–152.
- Lindsay S. Discrimination and other barriers to employment for teens and young adults with disabilities. Disabil Rehabil. 2011;33(15–16):1340–1350.
- Lindsay S, McDougall C, Menna-Dack D, et al. An ecological approach to understanding barriers to employment for youth with disabilities compared to their typically developing peers: views of youth, employers, and job counselors. Disabil Rehabil. 2015;37(8):701–711.
- Lindsay S, Cagliostro E, Carafa G, et al. Disability disclosure and workplace accommodations among youth with disabilities. Disabil Rehabil. 2018;40(25):2971.
- Eurostat. European social statistics. Luxembourg: European Commission; 2013.
- experts TANoED. The labour market situation of disabled people in European countries and implementation of employment policies: a summary of evidence from country reports and research studies. Leeds: Academic Network of European Disability Experts (ANED); 2009.
- Pawłowska-Cyprysiak K, Konarska M, Żołnierczyk-Zreda D. Self-perceived quality of life of people with physical disabilities and labour force participation. Int J Occup Saf Ergon. 2013;19(2):185–193.
- Hall J, Kurth NK, Hunt SL. Employment as a health determinant for working-age, dually-eligible people with disabilities. Disabil Health J. 2013;6(2):100–106.
- King G, McPherson A, Kingsnorth S, et al. Residential immersive life skills programs for youth with disabilities: service providers' perceptions of experiential benefits and key program features. Disabil Rehabil. 2015;37(11):971–980.
- Kingsnorth S, Healy H, Macarthur C. Preparing for adulthood: a systematic review of life skill programs for youth with physical disabilities. J Adolesc Health. 2007;41(4):323–332.
- Kingsnorth S, King G, McPherson A, et al. A retrospective study of past graduates of a residential life skills program for youth with physical disabilities. Child Care Health Dev. 2015;41(3):374–383.
- Lindsay S, Adams T, McDougall C, et al. Skill development in an employment-training program for adolescents with disabilities. Disabil Rehabil. 2012;34(3):228–237.
- Lindsay S, Hartman L, Fellin M. A systematic review of mentorship programs to facilitate transition to post-secondary education and employment for youth and young adults with disabilities. Disabil Rehabil. 2016;38(14):1329–1349.
- Lindsay S, Lamptey DL, Cagliostro E, et al. A systematic review of post-secondary transition interventions for youth with disabilities. Disabil Rehabil. 2018;4:1–14.
- Bal MI, Sattoe JN, van Schaardenburgh NR, et al. A vocational rehabilitation intervention for young adults with physical disabilities: participants' perception of beneficial attributes. Child Care Health Dev. 2017;43(1):114–125.
- Bond GR, Drake RE, Campbell K. Effectiveness of individual placement and support supported employment for young adults. Early Interv Psychiatry. 2016;10(4):300–307.
- Verhoef JA, Miedema HS, Van Meeteren J, et al. A new intervention to improve work participation of young adults with physical disabilities: a feasibility study. Dev Med Child Neurol. 2013;55(8):722–728.
- Verhoef JA, Roebroeck ME, van Schaardenburgh N, et al. Improved occupational performance of young adults with a physical disability after a vocational rehabilitation intervention. J Occup Rehabil. 2014;24(1):42–51.
- Bartholomew LK, Parcel GS, Kok G, et al. Planning health promotion programs: an intervention mapping approach. 3rd ed. San-Francisco: Jossey-Bass; 2011.
- Varekamp I, Verbeek JH, van Dijk FJ. How can we help employees with chronic diseases to stay at work? A review of interventions aimed at job retention and based on an empowerment perspective. Int Arch Occup Environ Health. 2006;80(2):87.
- Statistics Netherlands-StatLine [internet]. Den Haag:Statistics Netherands; 2019. [cited 2019 Feb 11]. Available from: http://statlinecbsnl/statweb/
- Statistics Netherlands [internet]. Den Haag: Statistics Nether;ands; 2019. [cited 2019 Feb 11]. Avaibale from: www.cbs.nl/en-GB/menu/themas/arbeid-sociale-zekerheid.
- Donkervoort M, Wiegerink DJ, van Meeteren J, et al. Transition to adulthood: validation of the Rotterdam Transition Profile for young adults with cerebral palsy and normal intelligence. Dev Med Child Neurol. 2009;51(1):53–62.
- Unesco. International standard classification of education. Montreal: Unesco Institute for Statistics; 2011.
- Botterweck A, Frenken F, Janssen S, et al. Plausibiliteit nieuwe metingen algemene gezondheid en leefstijlen 2001. Heerlen: CBS; 2001.
- Law M, Baptiste S, Carswell A, et al. Canadian occupational performance measure. Ottawa: CAOT Publications ACE; 1998.
- Eyssen IC, Steultjens MP, Oud TA, et al. Responsiveness of the Canadian occupational performance measure. JRRD. 2011;48(5):517–528.
- Nieuwenhuijsen C, Donkervoort M, Nieuwstraten W, et al. Experienced problems of young adults with cerebral palsy: targets for rehabilitation care. Arch Phys Med Rehabil. 2009;90(11):1891–1897.
- Lindsay S. A scoping review of the experiences, benefits, and challenges involved in volunteer work among youth and young adults with a disability. Disabil Rehabil. 2016;38(16):1533–1546.
- Haverman L, Verhoof EJ, Maurice-Stam H, et al. Health-related quality of life and psychosocial developmental trajectory in young female beneficiaries with JIA. Rheumatology. 2012;51(2):368–374.
- Bal MI, Sattoe JNT, Miedema HS, et al. Social participation and psychosocial outcomes of young adults with chronic physical conditions: comparing recipients and non-recipients of disability benefits. Ann Phys Rehabil Med. 2018;61(2):85–91.
- Huang IC, Holzbauer JJ, Lee EJ, et al. Vocational rehabilitation services and employment outcomes for adults with cerebral palsy in the United States. Dev Med Child Neurol.. 2013;55(11):1000–1008.
- Vooijs M, Leensen MC, Hoving JL, et al. Interventions to enhance work participation of workers with a chronic disease: a systematic review of reviews. Occup Environ Med. 2015;72(11):820–826.
- National Institute for Public Health and the Environment. Chronische ziekten en multimorbiditeit. [Chronic illness and multimorbidity]. Den Haag: National Institute for Public Health and the Environment; 2019. [cited 2019 Feb 11]. Available from: http://www.nationaalkompas.nl/gezondheid-en-ziekte/ziekten-en-aandoeningen/chronische-ziekten-en-multimorbiditeit.
- Sawyer SM, Macnee S. Transition to adult health care for adolescents with spina bifida: research issues. Dev Disabil. 2010;16(1):60–65.

