Abstract
Purpose
Low back pain (LBP) is the leading cause of disability worldwide. Clinical research advocates using the biopsychosocial model (BPS) to manage LBP, however there is still no clear consensus regarding the meaning of this model in physiotherapy and how best to apply it. The aim of this study was to investigate how physiotherapy LBP literature enacts the BPS model.
Material and methods
We conducted a critical review using discourse analysis of 66 articles retrieved from the PubMed and Web of Science databases.
Results
Analysis suggest that many texts conflated the BPS with the biomedical model [Discourse 1: Conflating the BPS with the biomedical model]. Psychological aspects were almost exclusively conceptualised as cognitive and behavioural [Discourse 2: Cognition, behaviour, yellow flags and rapport]. Social context was rarely mentioned [Discourse 3: Brief and occasional social underpinnings]; and other broader aspects of care such as culture and power dynamics received little attention within the texts [Discourse 4: Expanded aspects of care].
Conclusion
Results imply that multiple important factors such as interpersonal or institutional power relations, cultural considerations, ethical, and social aspects of health may not be incorporated into physiotherapy research and practice when working with people with LBP.
When using the biopsychosocial model with patients with low back pain, researchers narrowly focus on biological and cognitive behavioural aspects of the model.
Social and broader aspects such as cultural, interpersonal and institutional power dynamics, appear to be neglected by researchers when taking a biopsychosocial approach to the care of patients with low back pain.
The biopsychosocial model may be inadequate to address complexities of people with low back pain, and a reworking of the model may be necessary.
There is a lack of research conceptualising how physiotherapy applies the biopsychosocial model in research and practice.
IMPLICATIONS FOR REHABILITATION
Introduction
Low back pain (LBP) is the leading cause of disability worldwide, with 1 in 6 Australians having experienced back problems in 2017–2018 [Citation1,Citation2]. Guidelines recommend the adoption of a biopsychosocial framework in the assessment and treatment of people with LBP in both acute and chronic stages [Citation3–7]. Conservative non-pharmacological care is considered to be a primary treatment option and, as such, people with LBP commonly seek care from physiotherapists and other rehabilitation health professionals for both short and long-term LBP. Recommendations reflect assessment and management of physical, psychological and social factors considered to be contributors to the pain and disability experienced by people with LBP. This trifecta of factors is known as the “biopsychosocial (BPS) model” and is now almost ubiquitously advocated as the approach of choice for musculoskeletal pain management [Citation4–7]. Despite these strong recommendations for the approach, it is not yet clear whether the conceptual understanding of the BPS model in physiotherapy is sufficient to apply it in practice.
The BPS model was developed to counter the narrow focus of the biomedical model, which has been the dominant Western healthcare approach (including pain management). The biomedical model is primarily based on a structural conceptualisation of pain. It seeks to find a source of pain (often from evidence of changes on imaging) and then aims to address this by targeting tissues presumed to be at fault [Citation8]. However, considerable research has shown that this approach has limited success; pain is often not associated with these types of patho-anatomical changes [Citation9]. There is strong evidence from modern pain science that pain is a more complex phenomenon and other factors are also likely to be important to patients’ pain experiences. Because of the reductionist assumptions underpinning the biomedical model, it has received considerable critique, arguing that the biomedical model cannot explain the complex array of pain experiences [Citation8,Citation10]. Thus, there was a need for new approach [Citation11,Citation12].
The BPS model was proposed by Engel in 1977 [Citation12] to broaden the biomedical approach by promoting a more humanistic perspective of healthcare, acknowledging not only biological but also psychological, and social influences [Citation11,Citation12]. In relation to LBP, Waddell’s work in 1987 [Citation13] was key early literature that advocated for a shift from a biomedical to the BPS model of care, to recognise the role of psychological and social – in addition to biological – aspects in the clinical assessment and treatment of this condition. Subsequently, many researchers in physiotherapy and related fields have argued for this approach, including demonstrating that psychological (behaviours, beliefs, distress, depression, anxiety and fear) and social factors (financial, family and work-related issues) can be associated with patient’s outcomes [Citation14], and have relationships to the persistence of pain and disability [Citation3,Citation15]. Furthermore, psychosocial factors such as being unemployed and catastrophizing were strong prognostic indicators of long-term disability in both acute/subacute and chronic LBP in primary care [Citation16], demonstrating that a multidimensional assessment and management may be warranted.
From the outset, Waddell [Citation17,Citation18] argued that there can be no clear division between the three BPS elements; they interact and overlap. Consistent with this proposal, longitudinal studies have shown that it is the interaction between psychological and biological features that predicts outcome, rather than the factors alone [Citation19]. In contrast to this more complex view, most research tends to take a segmented approach to the BPS model, and some aspects are considered more frequently than others [Citation20–22]. These applications remain reminiscent of the biomedical model’s reductionist and dualist separation of body and mind. Adding to this debate, Stilwell and Harman’s [Citation22] 2019 in-depth discussion of the BPS model in the context of musculoskeletal pain (not limited to physiotherapy or LBP) argues strongly that the BPS model itself is poorly conceptualised. These authors suggest that, despite its earlier conceptualisation, the model too easily results in a reductionist application which fragments patients’ pain into biological, psychological and social. They conclude that these simplistic applications of the BPS model are likely to be inadequate in considering the complexities of pain conditions, and that a more holistic approach is needed [Citation22]. This simplification may, for example, lead to a systematic and unacknowledged preference for certain features over others [Citation23,Citation24], which could perpetuate insufficient management of LBP.
At present, clinical guidelines, systematic reviews and position statements, including from the World Health Organisation, strongly recommend using the BPS model to inform assessment and management of LBP [Citation25–27]. Despite these recommendations for the approach, it is unclear whether there is sufficient understanding of what the BPS model means in physiotherapy research and practice, and there are questions regarding whether psychological and social aspects are given sufficient attention [Citation28–30]. For example, several studies suggest that physiotherapists’ clinical reasoning when managing LBP patients largely continues to focus on biomedical aspects and provides inadequate attention to other elements of the BPS model [Citation28,Citation31,Citation32]. Similarly, a study by Cowell et al. [Citation29], indicated that although physiotherapists recognized the importance of the BPS model, they had difficulty managing patients with LBP who have psychosocial features that contribute to their pain. These studies concluded that physiotherapists could benefit from further training in this area. This research raises concerns that physiotherapists may have narrow conceptualisations of the BPS model, which are at odds with its key tenants, which may explain the discrepancy between best practice guidelines and actual practice.
To our knowledge, there has been little investigation and critical analysis of how physiotherapy conceptualises and enacts the BPS model, including whether some conceptualisations are given more legitimacy than others. The aim of this study was to investigate the concepts and assumptions underpinning the use of the term “biopsychosocial” in physiotherapy literature with respect to the assessment and management of people with LBP.
Materials and methods
We conducted a literature search using key electronic databases. To gain an overview of the literature we undertook a systematic search of the literature using two key databases. The resulting pool of literature was critically reviewed and the data interpreted using a Foucauldian discourse analysis.
Search methods
The examination of the biopsychosocial model presented in this paper is based on analysis of 66 articles found in a search of existing literature on physiotherapy LBP assessment and management. The search was conducted in June 2019, and updated in October 2020, using the electronic databases PubMed and Web of Science. We included articles if they: (a) were published or updated preceding October 2020; (b) explicitly discussed implementation of the “biopsychosocial model”; (c) pertained to LBP assessment and/or management, (d) discussed assessment and/or management by physiotherapists, and (e) were published in English. These inclusion criteria ensured each article had sufficient discussion of, or reference to, the BPS model in the context of physiotherapy and LBP for analysis. The search included combinations of keywords in the title and abstract such as “biopsychosocial”, “physical therap*”, “physiotherap*”, “physical therap*” and low* back pain’, resulting in 529 articles. After excluding 466 papers that did not fit the inclusion criteria, and duplicates, 63 articles were included. The excluded studies focussed on the following: other musculoskeletal conditions, assessment and treatment of LBP in a multidisciplinary team, and mention of the BPS model in the abstract without explicitly discussing or implementing it in the body of the article. We then searched the reference list of these 63 articles, identifying three additional articles fitting the inclusion criteria, making a total of 66 articles for this review.
Theoretical approach
The nature of a critical review is focussed on meaning and concepts rather than an evaluation of quality or outcomes. A “critical review” is an established approach that aims to analyse and critically appraise the available literature. As Grant and Booth [Citation33, p.97] explain, the: “emphasis is on the conceptual contribution of each item of included literature, not on formal quality assessment.” A critical review challenges existing models or schools of thought and provides a platform for innovative conceptual development and subsequent investigation and implementation. This critical review used the qualitative method “Foucauldian discourse analysis” [Citation34] to analyse how the concept “biopsychosocial” is used within the selected articles.
Discourse analysis is concerned with the underpinning assumptions of text (i.e., language) or visual representations (e.g., images) and how they inform the way people think and act [Citation34,Citation35]. According to Foucault [Citation36], discourse is more than mere meaning. Discourse is the way knowledge or “truth” is constituted via any type of communication that informs and shapes practices, identities, and power relations. Foucault argues that some discourses shape and create knowledge systems, while others are marginalised and subjugated [Citation36]. Researchers using a Foucauldian discourse analysis thus investigate and describe rules, divisions and systems underpinning a particular body of knowledge and its power structures [Citation37]. The analysis makes explicit the various ways of thinking and meaning-making processes that contribute to constructing apparent “truths” and “realities” [Citation38]. In relation to this critical review, the 66 included articles were analysed to consider the different discourses underpinning the BPS model used by researchers in physiotherapy assessment and management of LBP care.
Data analysis
We adapted Foucauldian discourse analysis procedures outlined by Willig [Citation34]. Analysis involved an iterative organization of the data into key discourses. Data was compiled into an Excel document and we added the quotes that underpinned each of the discourses in separate columns. Two trained research assistants (health science students) conducted the initial literature search under close guidance by the first (KM) and senior (JS) authors. KM (a physiotherapist with seven years of clinical experience and research experience in both quantitative and qualitative methodologies) read through each of the 66 articles for references to the BPS model and any of its elements. Segments of the articles containing relevant references to the BPS were identified. We call these segments “texts” in this article to describe and refer to fragments or sections of articles (or, at times, the discussions pertain to whole articles). For example, if mainly biological elements were considered (e.g., biological outcome measures and/or assessment tools) then a text was deemed to be underpinned by a biological discourse. If the article mentioned using the BPS model but primarily behavioural approaches were used, this text was considered to reflect a psychological discourse. Most articles were underpinned by more than one discourse and the discourses were named to describe common and less common assumptions underpinning the use of the term biopsychosocial in the texts. To enhance rigor and trustworthiness of the results, JS (a physiotherapist with social science training and experience in discourse analysis and qualitative methodology) and RO (a medical sociologist with extensive qualitative and discourse experience) independently read through the dataset, and discourses were discussed until agreement was reached across the investigators. The other investigator (PH, a physiotherapist and neuroscientist with extensive quantitative training) provided an external perspective and confirmed the final analysis.
Results
We analysed 66 articles for this study (Appendix A). They varied considerably in terms of focus and methodology. Approximately one third of the articles focussed on treatment of people with LBP, one third were about physiotherapy assessment, and one third evaluated physiotherapists’ beliefs about the BPS model in LBP management. Methodologies ranged from quantitative (e.g., systematic reviews, randomized controlled trials, case reports, cross-sectional studies and quasi-experimental studies) to qualitative (e.g., interviews, cross-sectional surveys) and also included non-empirical papers (e.g., perspective study, masterclass, professional issue discussion, trial protocols).
As discussed above, our aim was not to evaluate the different methodologies, or the success of assessment/management approaches, but rather to focus on how the BPS model was conceptually constructed among the texts. That is, we examined the assumptions/truths underpinning the texts' discussions of the BPS. Discussions about the BPS were apparent in various aspects of the articles, such as the introduction, or the use of particular treatments/outcome measures. A small number of articles only mentioned the term BPS in the title and conclusion, with no further mention in the body of the paper, however, we were able to examine these texts because assumptions were apparent in the content.
We organised our analysis outcomes into four key discourses: namely, “Conflating the BPS with the biomedical model”, “Cognition, behaviour, yellow flags and rapport”, “Brief and occasional social underpinnings” and “Expanded aspects of care” (see ). Most articles had more than one discourse evident, but the emphasis on certain factors over others was apparent in how articles constructed the understanding of the BPS model. We discuss each discourse separately below, using quotes from the texts to demonstrate how the discourses underpinned understandings of the BPS model. The most common elements discussed by texts when having a BPS approach are represented in .
Figure 1. Visual representation of the biological, psychological, social, and extended aspects of low back pain care presented by the selected articles in this critical review.
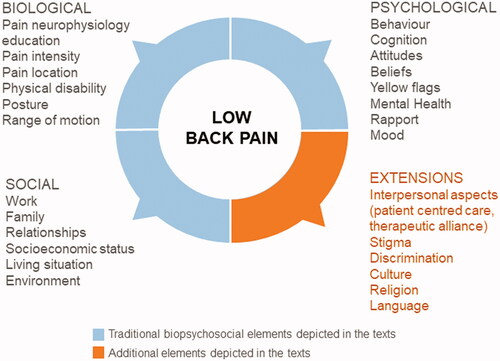
Table 1. Overview of the four discourses underpinning the use of the term “biopsychosocial” in physiotherapy literature in the management of people with low back pain (LBP).
Discourse 1: conflating the BPS with the biomedical model
Our analysis identified that many of the texts conflated the BPS with the biomedical model, particularly when focusing on biological outcomes or pain neurophysiology. The discourse “Conflating the BPS with the biomedical model” was frequently apparent in texts that suggested that the BPS model was used but, in fact, predominantly focussed on biological aspects of LBP care. That is, although the term “biopsychosocial” was used, and authors acknowledged the psychological and social aspects of the model, the focus continued to be on biological aspects in the enactment of the research. Of note, this discourse was evident despite explicit and extensive criticism of the biomedical model within the majority of these texts, including discussion of its insufficiency in explaining patients’ LBP (as discussed in our introduction above).
This discourse was underpinned by two key related and overlapping assumptions that were often apparent in the texts: a singular focus on biological outcomes and assessment tools, and conflation of the BPS model with pain neurophysiology. These two factors are discussed separately below.
Focus on biological measurements
One way in which the BPS was conflated with the biological was in the choice of evaluation measures in articles that investigated intervention/assessment effectiveness. In these texts the effectiveness of LBP management and assessment of patients was predominantly tested using biological measurements that focused on pain and (physical) disability. Although the majority of articles also used psychological outcomes in combination with biological, the psychological outcomes received less attention. For example, disability, pain intensity and pain location were the most frequent primary outcomes used to assess and evaluate patients [Citation39–44], and active range of motion, posture and spinal movement were also frequently used [Citation43,Citation45–50]. In their perspective paper about a movement control schema, Alrwaily et al. [Citation45] suggest that this type of approach exists within a BPS perspective. However, throughout the article, the focus continued to be on biological aspects. Pain, physical disability and clinical assessment such as neurodynamic tests, joint motion, and motor control were the main focus of this schema. Overall, psychosocial aspects, where present, had little attention or detail in texts. There were considerably fewer of these measures used, and they were rarely used as primary outcomes.
Pain neurophysiology
One of the recurring ways the texts conflated the BPS with biologically-focussed elements was the use of treatment approaches that focused on educating patients about pain neurophysiology. Although the proposed underlying mechanism of treatment approaches such as “pain neurophysiology education” and “explain pain” is argued to address psychological elements (discussed in the second discourse below), these modern pain neuroscience education approaches involve explaining pain neurobiology and neurophysiology to the patient in order to help them decrease their pain and disability. These approaches were argued to be essential to a “BPS approach” in some texts. For example, Puentedura and Louw [Citation51, p.123] wrote “True BPS model includes a greater understanding of how the nervous system processes injury, disease, pain threat and emotions”. Another example was Mansell et al.’s [Citation40] secondary analysis of a randomized controlled trial that indirectly examined this approach. They stated:
A recent approach developed in Australia, Explain Pain, involves teaching patients about the biological processes underpinning why they are (still) experiencing pain. It is defined as an educational intervention underpinned by a biopsychosocial approach to pain, where physical therapists or clinicians aim to build a strong rapport with patients and encourage them to ask questions to improve their understanding. [our emphasis] [Citation40, p.1139]
Although other elements, such as patient rapport and emotions were mentioned or alluded to in these and other examples, it is the biological aspects of emotions (the nervous system processes) that are foregrounded. Thus, many of the texts that engaged with pain neurophysiology education [Citation40,Citation48,Citation52–56], although stating this approach to be part of the BPS model, often largely reduced it from its trifecta to the “bio.”
To summarise, texts underpinned by the discourse “Conflating the BPS with the biomedical model” often referred to the importance of psychosocial aspects in the assessment and treatment of people with LBP and suggested that they were using a BPS model to underpin their work. However, the way they wrote about and enacted LBP care in their research focused on biological aspects, largely conflating the BPS with biology.
Discourse 2: cognition, behaviour, yellow flags and rapport
Approximately a third of texts examined were underpinned by the “Cognition, behaviour, yellow flags and rapport” discourse, in which the BPS approach was predominantly seen to be about attending to certain psychological aspects of LBP care. These texts also alluded to biological and social aspects, however, their key focus was largely restricted to the psychological. This played out in three key ways. First, there was a focus on thought patterns influencing patient behaviours and presumably, as a result, LBP. This included concepts such as cognition, behaviour, attitudes, and beliefs, which were frequently linked, confounded, and/or overlapping amongst the texts. Second, the (narrow) psychological focus was also evident in references to, and use of abbreviated psychological assessment tools such as, “yellow flags”: a checklist approach to evaluating psychological (and some social) “warning signs”. Finally, discussions of physiotherapists’ attitudes towards the BPS model also contributed to the BPS as psychological discourse – bringing in an element of interpersonal/relational psychological elements. There were occasionally other psychological elements present.
Changing patient thoughts that influence behaviours
The “Cognition, behaviour, yellow flags and rapport” discourse was apparent in the authors’ frequent use of cognitive and behavioural approaches to assess and manage patients with LBP. The emphasis on cognition and behaviour was apparent in the focus on: (1) cognitive behavioural therapies, (2) “lifestyle change” and (3) some pain neurophysiology approaches.
The stated aim of using these approaches was almost always to change patients’ “unhelpful” beliefs about their pain. This approach was believed to result in changes in patient behaviour (such as movement patterns or levels of activity), and consequently a reduction in their pain. For example, nine studies [Citation46–50,Citation57–60] referred to an intervention known as cognitive functional therapy, which was discussed in the texts as being BPS-oriented. For example, in their overview of this treatment, Cowell et al. [Citation57, p.80] state that “Cognitive functional therapy is a biopsychosocially oriented behavioural intervention for low back pain”. The association between cognitive functional therapy and behavioural change can also be seen in how O’Sullivan et al. [Citation50, p.1479] conceptualise the treatment.
Cognitive functional therapy is a novel, person-centered behavioural intervention that addresses multiple dimensions in NSCLBP [non specific chronic low back pain]. This intervention combines a functional behavioural approach of normalizing provocative postures and movements while discouraging pain behaviours, with cognitive reconceptualization of the NSCLBP problem. [our emphasis]
Although cognitive functional therapy does address other aspects of LBP care, the emphasis evident in these studies was in changing patients’ behaviour. The assumption that behavioural changes are a fundamental aspect of the BPS model was evident in a number of other articles which advocated for related cognitive behavioural change approaches, such as graded activity and graded exposure in vivo [Citation27,Citation61,Citation62]. Ostelo and colleagues explicitly discussed what they saw as “probable shifts” that come with adopting the BPS model: “The BPS model is advocated, thereby probably shifting the treatment orientation towards a more behavioural perspective” [our emphasis] [Citation61, p.219]. The BPS, in these conceptualisations, involves a focus on behaviour change.
Another behavioural focus was that of “lifestyle change”. Some texts identified and emphasised that a change in patient’s “lifestyle behaviours” was central to LBP management when adopting a BPS approach. Although physical inactivity was the most common behaviour discussed as beneficial to change in the texts, alcohol consumption, smoking, and “lifestyle stress” were also mentioned [Citation29,Citation63]. In these texts, self-care and self-management were prioritised as important for physiotherapists to address with patients [Citation29,Citation64,Citation65]. For example, Berger mentioned that teams working with pain management should have skills in “[m]aintenance [which] focuses on self-management (e.g., exercise, cognitive behavioural) and ongoing symptomatic intervention” [Citation64, p.17]. Self-management (individual behaviour change) was generally assumed to be the best approach [Citation43,Citation46,Citation48,Citation49].
As mentioned in our discussion above of the “Conflating the BPS with the biomedical model” discourse, pain neurophysiology education was frequently mentioned in the studies. Unlike the previous discourse, where the emphasis was placed in pain neurobiology and neurophysiology, we considered these mentions to fit within “Cognition, behaviour, yellow flags and rapport” discourse when pain neurophysiology was depicted as a predominantly psychological intervention. Nijs et al. in their perspective study discussed the integration of pain neuroscience education with motivational interviewing, an approach used mainly by psychologists, and how “Combining MI [motivational interviewing] and PNE [pain neuroscience education] may motivate patients to invest time and energy into changing their thoughts/beliefs by reading PNE materials at home” [Citation66, p.851]. Again, these interventions were usually directed towards addressing patients’ “inadequate” cognition, beliefs, behaviours and/or thoughts [Citation46,Citation48,Citation50,Citation51,Citation54–56,Citation66]. This approach is also clear in a clinical perspective paper by Goudman et al. [Citation54] advocating pain neuroscience education as a perioperative intervention. In their introduction, they described this treatment in the following way:
Pain neuroscience education is a cognitive-based intervention to inform patients about what to expect from the evolution of their pain, deemphasize the patho-anatomical content, and focus on the factors that contribute to the development of pain, all within a biopsychosocial framework, meaning that pain neuroscience education is changing the beliefs of patients. [our emphasis] [Citation54, p.935]
Assessing or changing patient’s beliefs were positioned as fundamental targets.
Psychological assessment tools
Another narrow approach to the psychological aspect of the BPS was evident in the mention or use of “yellow flags” and other standardised psychological assessment tools. Yellow flags are designed to be a rapid way to screen for “psychosocial” warning signs evident in the presentation of a patient with LBP. They encompass factors that are considered to negatively influence a patient’s recovery such as fear-avoidance behaviours, beliefs regarding pain, low mood, and mental health diagnoses. For example, according to Stewart et al. [Citation67, p.197] “The identification of an individual’s beliefs in relation to their back is central to the yellow flags assessment procedure”. Some studies mentioned the recognition of these psychological risk factors as fundamental when using a BPS model of care [Citation68,Citation69]. This assumption of a strong interplay between yellow flags and BPS model was often very explicitly stated, for example:
LBP and disability can only be addressed by the early recognition and management of biopsychosocial risk factors. Consideration of these factors, or ‘yellow flags’, has been added to the recently updated clinical guidelines for the management of acute LBP in the UK [Citation68, p.215].
In addition to psychological aspects, yellow flags also consider some social aspects of LBP care (discussed in the next discourse).
Other standardised measures with a psychological focus were behavioural outcome measures and assessment tools. Harking back to the cognition/behaviour focus in the previous section, often, these were based on cognitive principles. At times, they were used in addition to the previously mentioned biological measurements. Patients’ pain beliefs were depicted as important aspects in the assessment and/or management of LBP care within a BPS framework in these texts. For example, the Fear Avoidance Beliefs Questionnaire and Back Beliefs Questionnaire (which both assess cognitive aspects of LBP) were used often, indicating that the authors considered this an important domain of the BPS model in LBP [Citation41,Citation43,Citation47,Citation48,Citation56,Citation64,Citation70]. The Pain Catastrophizing Scale (which screens for “excessively negative” pain beliefs) and Tampa Scale for Kinesiophobia (excessive fear of movement) were also used as outcome measures, but less frequently [Citation40,Citation62,Citation70,Citation71].
Physiotherapists’ attitudes and beliefs
Diverging from the patient-focussed discussions above, texts were underpinned by an acknowledgment of the relevance of clinician-held beliefs (and, presumably, related behaviours). These texts implicitly included some acknowledgement that interpersonal and relational aspects of LBP mattered within the clinic. Here the focus was almost exclusively on physiotherapists’ beliefs about, and attitudes towards, biomedical and biopsychosocial elements of LBP, including ten studies which used the Physiotherapist Attitudes and Beliefs scale [Citation29,Citation39,Citation44,Citation57,Citation72–77]. The importance that Beneciuk and George [Citation44] place on physiotherapists’ thinking, for example, is depicted in their discussion of their findings about the feasibility of BPS oriented care:
(…) these findings suggest that physical therapists’ attitudes and beliefs can be changed and maintained toward a biopsychosocially oriented treatment approach and that those changes may positively influence patient clinical outcomes when combined with a stratified care approach [Citation44, p.1128].
The change in physiotherapists’ attitudes and beliefs is positioned as important for LBP patient’s outcome.
In discussing physiotherapist attitudes and beliefs, a number of texts pointed again to the idea that the psychological is about behaviour and cognition (as discussed above). For example, Magalhães et al. [Citation72] argued that physiotherapists have two different belief systems when managing people with LBP. The first is biomedically focused, and according to the authors, the second:
(…)is one that follows a biopsychosocial model in which pain is explained not only by tissue damage but also by social and psychological factors. In this case, physical therapy treatment is based on principles of cognitive behavioural therapy that addresses these factors. [our emphasis] [Citation72, p.249]
Here, both psychological and social are reduced to cognition/behaviour via cognitive behavioural therapy.
Other psychological domains
In contrast to the almost ubiquitous thinking based on cognitive and behaviour theories discussed so far in this discourse (patient beliefs/behaviour, assessment tools and physiotherapists beliefs/attitudes), there were a few texts that mentioned other psychological domains. The most commonly cited was mental health such as emotional distress, anxiety and depression [Citation47,Citation63,Citation64,Citation78,Citation79]. For example, the BPS approach was invoked by Park et al. [Citation80] in their quasi-experimental study that compared the effects of an exercise program using the Nintendo-Wii game with stability exercise. Park et al. [Citation80, p.985] argued that the “Nintendo Wii exercise program could be a biopsychosocial intervention for work-related LBP in factory workers” because this type of exercise program significantly improved not only physical, but also mental health. Similarly, in their qualitative study of the feelings, beliefs, and attitudes of newly trained physiotherapists about using the BPS model with LBP patients, Franca et al. [Citation78, p.87] also linked the BPS to mental health when they identified that the “most commonly reported factors were depression, stress, anxiety, and low income”. However, on the few occasions mental health was mentioned, it was given little attention or focus beyond such brief acknowledgements (e.g., it was rarely measured). However, multiple other psychological aspects that may be important were not attended to, such as feelings of shame, guilt, co-dependency behaviours, and some interpersonal and intrapersonal interactions [Citation81–85].
To summarise this discourse, this third of all texts were underpinned by the discourse that the BPS model is (narrowly) psychological. Although there were a number of factors that could be considered “psychological” they largely fell into the cognitive/behavioural and attitudinal aspects with only infrequent attention to other aspects such as mental health, emotions, and many elements of clinician/client interpersonal connections, suggesting physiotherapists are likely to have a fairly constrained conceptualisation and enactment of the “psycho” part of the BPS in this context. Some texts were not exclusively underpinned by this discourse, such as yellow flags being underpinned by psychological and social domains. Although the term “psychosocial” was extensively used, the focus tended to be on the psychological aspect, and articles rarely made a clear distinction between the two (intersecting) aspects of this term.
Discourse 3: brief and occasional social underpinnings
Whereas the texts underpinned by the first two discourses focused on the biological and psychological aspects of the BPS approach, some texts attended to (often briefly) the social aspects of working with patients with LBP. This discourse was apparent in the texts when the BPS was considered to be “social” – that is, LBP was not considered to be an individual issue located in the patient’s body (biological) or a person’s beliefs, behaviours, thinking patterns or mood (psychological), but rather it was contextualised within the broader social environment in which someone is situated. The “Brief and occasional social underpinnings” discourse was considerably less common in the texts than the previous two discourses. This marginalisation of the social was explicitly illustrated in a discussion of the relative importance of factors: “Cognitive factors may be more important than sociodemographic factors in the development of disability related to LBP” [Citation73, p.437]. The main social concepts introduced in the texts in relation to the BPS were work, family relationships, social assessment tools, and socioeconomic factors. Other social domains that are known to impact individuals’ health such as class, gender, macro socio-economic and political context, and access to healthcare [Citation86] were not discussed at all.
Work
Although no single social element commonly underpinned understandings of the BPS in the texts, work was the most common. For example, work-related stress, job satisfaction and physical demands were mentioned by a number of the texts [Citation32,Citation51,Citation64,Citation87,Citation88,Citation89,Citation90,Citation91] as important factors to assess and address when taking a BPS approach in LBP management. This assumption of the importance of work context was clear. For instance, Foster and Delitto [Citation90, p.798] discussed some aspects of work to be key elements affecting LBP recovery: “Occupational factors that have evidence from more than one systematic review include heavy physical demands, ability to modify work, social support, short job tenure, job satisfaction, and fears of reinjury”. Miller [Citation92] also argued that social pressures in returning to work environment should also be considered, but the author did not provide any further explanation of how this would be managed in practice. Although explored in different ways, work was clearly the most investigated social element, and the only factor that was examined in some detail, not simply mentioned.
Relationships
Occasionally authors mentioned patients’ relationships or “social network” (e.g., partners, family and significant others) as being part of the BPS approach [Citation27,Citation32,Citation62,Citation79,Citation87]. Caneiro et al. [Citation48] and Foster and Delitto [Citation90] identified social isolation as a factor involved in the development and persistence of LBP, as well as a key obstacle to LBP recovery. For example, Caneiro et al. [Citation48, p.544] identified that “a lack of awareness of [a participant’s] body schema and the mechanisms associated with his LBP, and social isolation from sport and friends” [our emphasis] were part of the psychosocial and cognitive domains of the multidimensional classification system of a male rower with LBP. However, this was not explored in detail in the text. In another study that investigated the beliefs and knowledge of physiotherapists about the BPS model [Citation32], all participants recognised social factors, including social relations, as key aspects contributing to a person with LBP’s pain and disability, but no further exploration of how to address those aspects in the clinical encounter were mentioned. This absence or lack of detail about human relationships and their relevance to the BPS model of LBP care was ubiquitous.
Socioeconomic status
Socioeconomic status was another social concept present within the texts, but to a much lesser extent than work and relationships. Although several studies mentioned socioeconomic status [Citation39,Citation47,Citation61,Citation63,Citation64,Citation71,Citation93,Citation94] it was generally given little attention. An exception was the study by Valencia et al. which aimed to investigate the mechanisms by which patients’ education and income levels influence pain, disability and physical impairment in LBP. They argued for the importance of these factors: “(…) researchers studying biopsychosocial models should consider the mechanisms by which SES [Socioeconomic status] influences psychosocial pathways and health outcomes” [Citation93, p.328]. In their interview study of physiotherapists, Franca et al. [Citation78] reported that participants also recognised financial income as a social element of the BPS approach, but this was not explored further. Of the papers we reviewed, only Wijma [Citation87] explicitly considered housing or living situation as important to LBP care. This infrequent focus on socioeconomic status in the papers related to physiotherapy practice included in this review contrasts other literature which highlights its key role in health outcomes (discussed in more detail in the discussion).
“Social” assessment tools
As discussed in previous discourses, the use of assessment tools was frequent in the adoption of the BPS model in LBP care. Occasionally these assessment tools had elements of the “BPS as social” discourse underpinning them. For example, the SF36 (a health survey intended to measure quality of life) was the main outcome presumed to measure the social component of the BPS model [Citation39,Citation42,Citation95,Citation96]. The use of the SF36 again demonstrates the systematic marginalisation of the social aspects of the BPS as the tool primarily assesses physical and psychological elements and only has a small social component.
Similar to “BPS as psychological” the social discourse also underpinned the use of yellow flags to screen for social aspects in a few texts [Citation67,Citation68,Citation69]. The psychological and social domain were closely related and/or conflated in this context: “Yellow flags are maladaptive attitudes and beliefs concerning back pain, frequent display of pain behaviours, reinforcement of pain behaviours by family members, heightened emotional reactivity, lack of social support, job dissatisfaction, and compensation issues” [Citation68, p.215]. The use of such tools tends to simplify and confound the social component of the BPS, as they do not take into consideration complex social constructs and interactions.
The social context was sometimes referred to in the texts as “environmental factors”. For example, when talking about employment and social networks, two texts [Citation32,Citation97] referred to those aspects as part of patients’ environmental contexts and also considered this as being part of the BPS model of care. Similarly, Nagarajan [Citation94] used the International Classification of Functioning, Disability and Health framework to depict some “environmental factors” that could influence patient’s outcome such as positive family environment, good economic background, and marital status. Although Matthews et al. [Citation65] recognised social environment as important for physiotherapists to address, they were linked with autonomous motivation, returning to a “BPS as psychological” discourse.
In summary, the “Brief and occasional social underpinnings” discourse was much less evident in texts than the previous discourses. Texts often reduced the social aspects of the BPS approach in LBP care to work (e.g., job satisfaction, stress, and workload) and relationships, but neglected broader aspects such as the social determinants of health and social gradient of disease (e.g., gender, race, class and ethnicity). The lack of importance placed on social aspects demonstrates how texts in physiotherapy favour biological and psychological over social domains when assessing and treating LBP patients.
Discourse 4: expanded aspects of care
The “Expanded aspects of care” discourse draws attention to aspects that do not easily fit within the above three discourses when considering the assumptions underpinning physiotherapy BPS approaches to LBP care. Patient-centred care and therapeutic alliance were the main elements mentioned. Other aspects such as time, stigma and discrimination, and multidisciplinary team were present, but rarely. Cultural and related factors such as religion and language were infrequently referred to in texts. Other factors that may be relevant to a comprehensive approach to LBP management such as micro-macro politics, ethics, and morals were not present at all.
Texts that were underpinned by this discourse often focussed on interpersonal elements of the physiotherapy-patient interaction as a pathway to attend to the broader social context of the patient. In these texts, the BPS model was often used interchangeably with “patient-centred care” and constructed fairly narrowly as a “therapeutic alliance” between patients and physiotherapists. For example, Sanders et al. [Citation97] investigated physiotherapists’ attitudes towards adopting a BPS approach in practice and mentioned in their introduction that “(…) any discussion about therapeutic decisions will begin with the patient’s perspective” [Citation97, p.1]. This extract shows an underlying consideration of power dynamics between patients and physiotherapists in the decision-making process, but there was no further detail in how to address this issue. Similarly, Stewart et al. [Citation67] suggests an emphasis on the client’s unique experience and meaning of pain, and a careful use and implementation of questionnaires in clinical practice due to their limitation in regards to a person’s context. According to Bunzli et al. [Citation46] a strong therapeutic alliance was thought to be required to change patients’ pain beliefs to a more BPS perspective. In addition, a number of texts mentioned that the therapeutic bond facilitates patient engagement and effective communication with health-professionals, however again little more was stated here [Citation29,Citation46,Citation56,Citation57,Citation92,Citation97]. The focus on “beliefs” and “effective communication strategies” seems largely to reduce the social to a “Cognition, behaviour, yellow flags and rapport” discourse instead of introducing new elements of these aspects of care.
Other factors such as time, stigma and multidisciplinary work were rarely mentioned but may provide some insights into why there is little evidence that physiotherapists have explored the complexities of the non-biological aspects of LBP management. For example, in a study of physiotherapists’ perceptions when using a BPS approach in a primary care setting, Cowell et al. [Citation29] concluded that time was a barrier to exploring BPS aspects – perhaps suggesting a deprioritisation of these factors by physiotherapists. Further evidence of such deprioritisation was in other studies which showed that physiotherapists believe that the BPS model was more commonly and effectively delivered by a multidisciplinary team, rather than by physiotherapists in isolation [Citation27,Citation52,Citation61,Citation62]. In a systematic review of qualitative studies that considered the perceptions of physiotherapist’s when assessing and managing psychosocial factors with patients with LBP, Synnott et al. [Citation98] highlighted that some physiotherapists stigmatised LBP patients when these elements were involved in treatment. All these factors were mentioned both infrequently and with little exploration.
Despite their importance, cultural, racial, language and/or religious factors were rarely mentioned in the texts. If they were, there was no further explanation of how acknowledgement of the importance of such factors would change or influence assessment and/or management of LBP care. Five articles mentioned these factors in a superficial manner [Citation41,Citation47,Citation51,Citation93,Citation97]. These texts only included culture in a list, without further exploring the relation between culture in more depth with LBP. For example, O’Keefe et al. [Citation47, p.2] acknowledged “culture” as a factor that was associated with LBP, “There is strong evidence that non specific chronic low back pain is associated with a complex interaction of factors. These include physical factors (…), cognitive factors (…) psychological factors (…), neurophysiological factors (…), and social factors (e.g., socioeconomic status, family, work and culture)” [our emphasis]. Only Alamam et al. [Citation41, p.E889] directly considered culture as a potentially key influence on LBP-related disability: “culturally determined beliefs about the meaning of pain, the context in which it occurs, and the associated emotions can influence the pain experience”. One article also discussed physiotherapy as having a particular “culture”: Foster and Delitto [Citation90] used the term to describe the current dominant practices of physiotherapy as being focused on biomedical, rather than psychosocial, aspects of care. This text suggests that the culture of physiotherapy matters to LBP care. However, overall, cultural factors were minimally explored.
This final discourse “Expanded aspects of care” encompassed features not usually classified as biological, psychological or social. Although some important aspects came into play, such as patient-centred care, stigma and time, they were less commonly mentioned than other aspects.
Discussion
The results of our analysis indicate that there are clear patterns in the way the physiotherapy literature conceptualises the BPS model when applying it with people with LBP. This critical review was not an exhaustive search of the literature, but did involve extensive searches of two key databases for relevant articles and included others found in their reference lists. It is possible that a small number of articles was missed that could have been incorporated in our results, however, as patterns were clear and repeated in our sample, it is unlikely they would have considerably changed our results. Throughout the literature reviewed, it was clear that there were four main discourses: conflation between the BPS and the biomedical model; narrow focus on some psychological dimensions (particularly behaviour and cognition) of LBP; little consideration of the social dimensions; and minimal consideration of other important dimensions of LBP care such as culture and power.
Despite the biomedical model being considerably contested in physiotherapy and LBP management in the last few decades, contemporary literature is underpinned by a biomedical discourse. This finding is consistent with that of Suls and Rothman [Citation99] who conducted a search of the Medline database to determine the frequency of the terms “biomedical” and “biopsychosocial” in titles and abstracts of medical articles and found that, although the use of the term biopsychosocial has been rapidly growing in recent years, the biomedical remains dominant. Our work adds to this literature by highlighting that even when the term biopsychosocial is used, it can be underpinned by biomedical concepts. Our analysis highlighted conflation of the biomedical model with the BPS model, which was particularly evident in the choice of primary outcome measures and LBP treatments based on pain neurophysiology education. The use of primary outcomes in LBP research such as pain and disability has received criticism in the literature since some of the most commonly used tools may not measure what they propose, and insufficiently capture what is important for patients [Citation100–102]. Stilwell and Harman [Citation22] similarly emphasise how the BPS model usually has a neuro- or brain-centric approach to pain, which sustains the focus on biology. By emphasising the brain, and reducing the individual pain experience to a response of the nervous system, there is a return to (or persistence of) reductionist and dualistic thinking reminiscent of the mind-body dichotomy. Here, “key dimensions of our humanness – language, culture, history, society – are ignored”. (Tallis, 2011, cited in Rose and Abi-Rached [Citation103, p.16]). Although replacing biological outcomes for psychosocial outcomes may seem an appropriate approach to reducing conflation of the BPS model with the biomedical model, it would arguably be an overly simplistic solution. The use of methodologies that support the use of outcome measures may have suited the biomedical model, however these methodologies are underpinned by positivism (the idea that there is a single, stable reality that can be measured) and may be an inadequate way to approach the complex interaction between the person and their social context [Citation67]. Instead, it may be more appropriate to consider utilising different methodologies and methods (e.g., drawing from social science approaches such as ethnography or critical qualitative approaches [Citation104,Citation105]) to better approach understanding of the complexities of living with LBP. These approaches have rarely been used to understand LBP management in physiotherapy.
The physiotherapy literature also frequently and narrowly prioritised targeting people’s cognition and behaviour when taking a BPS approach to LBP. Other potentially important psychological dimensions such as mood or mental health were rarely considered. The literature analysed emphasised that a change in attitudes and beliefs (and associated behaviour change) was important for patients and physiotherapists. Thus, when attending to the “psycho” in the model, the literature often reduced this to activities underpinned by cognitive behavioural models. These models have been critiqued for placing the responsibility for health on the individual, by adopting “better ways of living” including healthy lifestyle behaviours [Citation106,Citation107]. Thus, although there may be a shift from the paternalistic biomedical approach, physiotherapy may be shifting to an individualistic approach to LBP care, where patients (and physiotherapists) are positioned as responsible for their condition to the exclusion of social structure considerations (e.g., the socio-economic and political circumstances in which people live, and the way social systems are organized). Potential issues with this approach are well documented elsewhere: on an individual level they can result in guilt, stigma, and disengagement with health services; on a broader level they can result in inequitable access to care or services that are poorly designed for some communities [Citation108].
In contrast to earlier thoughts regarding the need to shift physiotherapy towards more psychologically-informed interventions for people with persistent pain [Citation109–111], we argue that this approach needs to be considered critically. This shift may lead to a “psychologisation” of chronic pain and, similar to a critique in the area of education, this type of intervention may be considered “individualistic, a-historical and a-political” [Citation112, p.93]. For example, interpersonal dynamics in patient-clinician interactions were rarely addressed in texts, but known to have a strong effect on LBP outcome [Citation113]. As Lehman et al. [Citation85] argues, this could in part be an issue inherent to the BPS approach: interpersonal aspects are complex constructs and Engel’s BPS model does not address them in a dynamic way. Elements such as micro-politics, cultural considerations, and institutional power inequities are likely to be implicated and require further exploration. Although the literature we examined did mention certain aspects of patient-clinician communication in LBP management [Citation29,Citation56,Citation65,Citation114], this was not given much attention and the complexities of interpersonal relationships were not further explored. This narrow application of the BPS model accords with earlier observations of the model, which suggest it is a naïve approach to illness and disease, with limited reflexivity, that often leads to an under appreciation of the social and political aspects implicated in healthcare and health research [Citation115].
Our findings also suggest that the physiotherapy literature rarely attends to social and other broader aspects of care. As mentioned, the included texts often reduced social aspects of the BPS approach to mainly work, and intimate/family relationships. These results are in line with those of Verhagen [Citation116], which discuss that the social level of the BPS model tends to be narrowed and individualistic and fails to consider the effects of broader social, cultural, religious/spiritual and political dimensions. Similarly, the literature review in the discipline of psychology of Suls and Rothman’s [Citation99] found that variables measuring social and macro domains (cultural, socioeconomic status, ethnicity) received considerably less coverage in comparison to psychological and biological variables. Reducing approaches to LBP care to biomedical and behavioural factors also goes against the larger body of knowledge that recognises LBP disability as inseparable from socioeconomic contexts as they are entangled with a person’s cultural and personal beliefs about their back pain [Citation3]. This suggests there should be a concerted effort to avoid fragmentation of the biological, psychological and social aspects of the BPS model. The division between these dimensions can lead to a reinforcement of individual-society dualism, a tendency to think that individuals are autonomous with no connection to the social world around them [Citation34].
Over-compartmentalisation of the three aspects of the BPS model prevents clinicians from recognising complexity and contextuality of patients, and frequently reduces them to a biological or behavioural (and individualistic) component. Further, the de-prioritisation of some very key aspects of LBP is important as it is likely to lead to a neglect of micro- and macro- aspects of living with LBP that physiotherapists should consider. From a Foucauldian perspective [Citation117,Citation118] this prioritisation of certain factors over others is a matter of power – biomedicine continues to be foregrounded, as do certain types of psychological approaches which do not journey far from biomedicine. Put differently, the “truth” that is constructed about LBP is that it remains the domain of biomedicine and (behavioural) psychology. By marginalising aspects of care, such as interpersonal and systemic power dynamics in healthcare contexts (e.g., patient-clinician, healthcare organisation-patient), consideration of socioeconomic circumstances, moral dimensions of care/living with LBP, broader political aspects (e.g., who pays for care, patient rights, insurance costs), religious (e.g., beliefs about the meaning of illness and approaches to care), and cultural (e.g., differing cultural beliefs about living with pain) the BPS model may be an insufficient framework for LBP care. There is a need to rethink the application of, and perhaps the entire concept of, the BPS model.
Some work has begun on the expansion and (re)conceptualisation of healthcare beyond the BPS model. For Stilwell and Harman [Citation22], an enactive approach to pain can be a promising framework. Through an embodied, embedded, enacted, extended, and emotive approach to pain (referred to as the “5Es”), the relational and dependent process between “brain-body-world” are interconnected, which contrasts to the usual fragmented presentation of the BPS model. Similarly, Nicholls and colleagues [Citation119] advocate for a better exploration of people’s connection with each other and the world around them, using the philosophical concept of “connectivity” to challenge individualised physiotherapy practice. According to the authors, by recognising the connections and assemblages between ourselves and the world (e.g., not only with people, but places, ideas, technologies), connectivity moves towards a more contextualised way to enact healthcare. Further, Setchell et al. [Citation30] argue that using Mol’s conceptualisation of multiplicity as a methodology to understand the clinical encounter “allows greater access to the complexities, subtleties, contradictions and ambiguities of physiotherapy (and other healthcare) practice: a step towards resisting complacency and closure.” [Citation30, p.166] Different ways of thinking and doing health are needed and, as shown by these authors, possible.
In conclusion, the results of this study call for a rethinking of the BPS model in physiotherapy LBP research and practice. The narrow focus on biological factors and cognitive behavioural change is inadequate to address the complexities of LBP and the methodologies used are, overall, ill-suited to in-depth understandings of psychosocial and other factors of care. This study suggests that broader and new perspectives towards a more comprehensive and flexible approach to researching and enacting LBP care are warranted. Our review analysed studies with a wide range of methodologies, and showed that despite different approaches to investigating LBP, they were underpinned by similar discourses. This provided fairly broad, non-penetrating insight into the literature which may have missed some articles due to the search terms chosen. It would be interesting to look in more detail at particular environments to see how this conceptualisation varies (for example looking at hospital-based literature, or that from private practice). It is also important to note that our investigation focussed on physiotherapy research, but did not investigate what happens in clinical practice. Although these two areas of physiotherapy are likely to be related, an investigation of what happens in clinical practice when applying the BPS approach would be salient to consider if similar biological and psychological discourses (and practices) occur. Our findings are also likely to relate to other conditions beyond LBP, and other healthcare professions applying the BPS approach. Future investigations could further examine this possibility.
Acknowledgements
We thank Tami-Lorrie Dawson and Dzung Nguyen for their contribution to the literature search and abstract review.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858.
- Australian Institute of Health and Welfare. Back problems. Canberra: AIHW; 2019.
- Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383.
- Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530.
- Bernstein IA, Malik Q, Carville S, et al. Low back pain and sciatica: summary of NICE guidance. BMJ. 2017;356:i6748.
- Koes B, Tulder M, Lin C-W, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094.
- NSW Agency for Clinical Innovation. Management of people with acute low back pain: model of care. Chatswood: NSW Health; 2016. p. 39.
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971–979.
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–816.
- Bonica JJ. The management of pain. South Med J. 1954;47(8):802.
- Engel GL. The biopsychosocial model and the education of health professionals. Ann N Y Acad Sci. 1978;310:169–187.
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136.
- Waddell G. 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976). 1987;12(7):632–644.
- Pincus T, Burton AK, Vogel S, et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27(5):E109–E120.
- Gatchel RJ. The continuing and growing epidemic of chronic low back pain. Healthcare (Basel). 2015;3(3):838–845.
- Grotle M, Foster NE, Dunn KM, et al. Are prognostic indicators for poor outcome different for acute and chronic low back pain consulters in primary care? Pain. 2010;151(3):790–797.
- Waddell G. The back pain revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2004.
- Waddell G. Biopsychosocial analysis of low back pain. Baillieres Clin Rheumatol. 1992;6(3):523–557.
- Klyne DM, Moseley GL, Sterling M, et al. Are signs of central sensitization in acute low back pain a precursor to poor outcome? J Pain. 2019;20(8):994–1009.
- Davidson L, Strauss JS. Beyond the biopsychosocial model: integrating disorder, health, and recovery. Psychiatry. 1995;58(1):44–55.
- Duncan G. Mind-body dualism and the biopsychosocial model of pain: what did Descartes really say? J Med Philos. 2000;25(4):485–513.
- Stilwell P, Harman K. An enactive approach to pain: beyond the biopsychosocial model. Phenom Cogn Sci. 2019;18(4):637–665.
- Chalmers KJ, Madden VJ. Shifting beliefs across society would lay the foundation for truly biopsychosocial care. J Physiother. 2019;65(3):121–122.
- Daluiso-King G, Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiother Theory Pract. 2020. DOI:10.1080/09593985.2020.1765440
- World Health Organisation. World report on disability. Geneva: World Health Organisation; 2011.
- National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management (NICE guideline NG59). London: National Institute for Health and Care Excellence (UK); 2016.
- van Erp RMA, Huijnen IPJ, Jakobs MLG, et al. Effectiveness of primary care interventions using a biopsychosocial approach in chronic low back pain: a systematic review. Pain Pract. 2019;19(2):224–241.
- Bishop EA, Foster EN. Do physical therapists in the United Kingdom recognize psychosocial factors in patients with acute low back pain? Spine (Phila Pa 1976). 2005;30(11):1316–1322.
- Cowell I, O’Sullivan P, O’Sullivan K, et al. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: a qualitative study. Musculoskelet Sci Pract. 2018;38:113–119.
- Setchell J, Nicholls DA, Gibson BE. Objecting: multiplicity and the practice of physiotherapy. Health (London). 2018;22(2):165–184.
- Driver C, Lovell GP, Oprescu F. Physiotherapists’ views, perceived knowledge, and reported use of psychosocial strategies in practice. Physiother Theory Pract. 2019. DOI:10.1080/09593985.2019.1587798
- Zangoni G, Thomson OP. ‘I need to do another course’ - Italian physiotherapists’ knowledge and beliefs when assessing psychosocial factors in patients presenting with chronic low back pain. Musculoskelet Sci Pract. 2017;27:71–77.
- Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108.
- Willig C, Stainton Rogers W. The SAGE handbook of qualitative research in psychology. Los Angeles (CA); London: SAGE; 2008. (Handbook of qualitative research in psychology).
- Setchell J, Costa N, Ferreira M, et al. Individuals’ explanations for their persistent or recurrent low back pain: a cross-sectional survey. BMC Musculoskelet Disord. 2017;18(1):466.
- Foucault M, Gordon C. Power/knowledge: selected interviews and other writings, 1972–1977. New York: Pantheon Books; 1980.
- McNaughton N. Discourse(s) of emotion within medical education: the ever-present absence. Med Educ. 2013;47(1):71–79.
- Pluut B. Differences that matter: developing critical insights into discourses of patient-centeredness. Med Health Care Philos. 2016;19(4):501–515.
- Casserley-Feeney SN, Daly L, Hurley DA. The access randomized clinical trial of public versus private physiotherapy for low back pain. Spine (Phila Pa 1976). 2012;37(2):85–96.
- Mansell G, Storheim K, Lochting I, et al. Identification of Indirect Effects in a Cognitive Patient Education (COPE) intervention for low back pain. Phys Ther. 2017;97(12):1138–1146.
- Alamam DM, Moloney N, Leaver A, et al. Pain intensity and fear avoidance explain disability related to chronic low back pain in a Saudi Arabian Population. Spine (Phila Pa 1976). 2019;44(15):E889–E898.
- Bath B, Lovo Grona S. Biopsychosocial predictors of short-term success among people with low back pain referred to a physiotherapy spinal triage service. J Pain Res. 2015;8:189–202.
- Belache FTC, Souza CP, Fernandez J, et al. Trial protocol: cognitive functional therapy compared with combined manual therapy and motor control exercise for people with non-specific chronic low back pain: protocol for a randomised, controlled trial. J Physiother. 2018;64(3):192.
- Beneciuk JM, George SZ. Pragmatic implementation of a stratified primary care model for low back pain management in outpatient physical therapy settings: two-phase, sequential preliminary study. Phys Ther. 2015;95(8):1120–1134.
- Alrwaily M, Timko M, Schneider M, et al. Treatment-based classification system for patients with low back pain: the movement control approach. Phys Ther. 2017;97(12):1147–1157.
- Bunzli S, McEvoy S, Dankaerts W, et al. Patient perspectives on participation in cognitive functional therapy for chronic low back pain. Phys Ther. 2016;96(9):1397–1407.
- O’Keeffe M, Purtill H, Kennedy N, et al. Individualised cognitive functional therapy compared with a combined exercise and pain education class for patients with non-specific chronic low back pain: study protocol for a multicentre randomised controlled trial. BMJ Open. 2015;5(6):e007156.
- Caneiro JP, Ng L, Burnett A, et al. Cognitive functional therapy for the management of low back pain in an adolescent male rower: a case report. J Orthop Sports Phys Ther. 2013;43(8):542–554.
- Meziat Filho N. Changing beliefs for changing movement and pain: Classification-based cognitive functional therapy (CB-CFT) for chronic non-specific low back pain. Man Ther. 2016;21:303–306.
- O’Sullivan K, Dankaerts W, O’Sullivan L, et al. Cognitive functional therapy for disabling nonspecific chronic low back pain: multiple case-cohort study. Phys Ther. 2015;95(11):1478–1488.
- Puentedura EJ, Louw A. A neuroscience approach to managing athletes with low back pain. Phys Ther Sport. 2012;13(3):123–133.
- Cuenca-Martinez F, Cortes-Amador S, Espi-Lopez GV. Effectiveness of classic physical therapy proposals for chronic non-specific low back pain: a literature review. Phys Therapy Res. 2018;21(1):16–22.
- George SI. What is the effectiveness of a biopsychosocial approach to individual physiotherapy care for chronic low back pain? Internet J Allied Health Sci Pract. 2008;6(1):1–10.
- Goudman L, Huysmans E, Ickmans K, et al. A Modern pain neuroscience approach in patients undergoing surgery for lumbar radiculopathy: a clinical perspective. Phys Ther. 2019;99(7):933–945.
- King R, Robinson V, Elliott-Button HL, et al. Pain reconceptualisation after pain neurophysiology education in adults with chronic low back pain: a qualitative study. Pain Res Manag. 2018;2018:3745651.
- Lindback Y, Enthoven P, Oberg B. Patients’ experiences of how symptoms are explained and influences on back-related health after pre-surgery physiotherapy: a qualitative study. Musculoskelet Sci Pract. 2019;40:34–39.
- Cowell I, O’Sullivan P, O’Sullivan K, et al. The perspectives of physiotherapists on managing nonspecific low back pain following a training programme in cognitive functional therapy: a qualitative study. Musculoskeletal Care. 2019;17(1):79–90.
- O’Sullivan K, O’Keeffe M, Forster BB, et al. Managing low back pain in active adolescents. Best Pract Res Clin Rheumatol. 2019;33(1):102–121.
- O’Neill A, O’Sullivan K, O’Sullivan P, et al. Examining what factors mediate treatment effect in chronic low back pain: a mediation analysis of a Cognitive Functional Therapy clinical trial. Eur J Pain. 2020;24:1765–1774.
- Holopainen R, Piirainen A, Karppinen J, et al. An adventurous learning journey. Physiotherapists’ conceptions of learning and integrating cognitive functional therapy into clinical practice. Physiother Theory Pract. 2020. DOI:10.1080/09593985.2020.1753271
- Ostelo RW, Stomp-van den Berg SG, Vlaeyen JW, et al. Health care provider’s attitudes and beliefs towards chronic low back pain: the development of a questionnaire. Man Ther. 2003;8(4):214–222.
- van Erp RMA, Huijnen IPJ, Koke AJA, et al. Development and content of the biopsychosocial primary care intervention ‘Back on Track’ for a subgroup of people with chronic low back pain. Physiotherapy. 2017;103(2):160–166.
- Mitchell T, O’Sullivan PB, Smith A, et al. Biopsychosocial factors are associated with low back pain in female nursing students: a cross-sectional study. Int J Nurs Stud. 2009;46(5):678–688.
- Berger P. Perspectives on physiotherapy guidelines for chronic low back pain. S Afr J Physiother. 2007;63(3):15–21.
- Matthews J, Hall AM, Hernon M, et al. A brief report on the development of a theoretically-grounded intervention to promote patient autonomy and self-management of physiotherapy patients: face validity and feasibility of implementation. BMC Health Serv Res. 2015;15:260.
- Nijs J, Wijma AJ, Willaert W, et al. Integrating motivational interviewing in pain neuroscience education for people with chronic pain: a practical guide for clinicians. Phys Ther. 2020;100(5):846–859.
- Stewart J, Kempenaar L, Lauchlan D. Rethinking yellow flags. Man Ther. 2011;16(2):196–198.
- Hurley DA, Dusoir TE, McDonough SM, et al. Biopsychosocial screening questionnaire for patients with low back pain: preliminary report of utility in physiotherapy practice in Northern Ireland. Clin J Pain. 2000;16(3):214–228.
- Ferguson FC, Brownlee M, Webster V. A Delphi study investigating consensus among expert physiotherapists in relation to the management of low back pain. Musculoskeletal Care. 2008;6(4):197–210.
- Beales D, Lutz A, Thompson J, et al. Disturbed body perception, reduced sleep, and kinesiophobia in subjects with pregnancy-related persistent lumbopelvic pain and moderate levels of disability: an exploratory study. Man Ther. 2016;21:69–75.
- Simon CB, Lentz TA, Bishop MD, et al. Comparative associations of working memory and pain catastrophizing with chronic low back pain intensity. Phys Ther. 2016;96(7):1049–1056.
- Magalhães MO, Costa LO, Cabral CM, et al. Attitudes and beliefs of Brazilian physical therapists about chronic low back pain: a cross-sectional study. Rev Bras Fisioter. 2012;16(3):248–253.
- Petit A, Begue C, Richard I, et al. Factors influencing physiotherapists’ attitudes and beliefs toward chronic low back pain: impact of a care network belonging. Physiother Theory Pract. 2019;35(5):437–443.
- Alshehri MA, Alzahrani H, Alotaibi M, et al. Physiotherapists’ pain attitudes and beliefs towards chronic low back pain and their association with treatment selection: a cross-sectional study. Bmj Open. 2020;10(6):e037159.
- Gomes AS, de Sá Ferreira A, Reis FJJ, et al. Association between low back pain and biomedical beliefs in academics of physiotherapy. Spine (Phila Pa 1976). 2020;45(19):1354–1359.
- Leysen M, Nijs J, Van Wilgen P, et al. Attitudes and beliefs on low back pain in physical therapy education: a cross-sectional study. Braz J Phys Ther. 2020. DOI:10.1016/j.bjpt.2020.08.002
- Schröder K, Öberg B, Enthoven P, et al. Confidence, attitudes, beliefs and determinants of implementation behaviours among physiotherapists towards clinical management of low back pain before and after implementation of the BetterBack model of care. BMC Health Serv Res. 2020;20(1):443.
- Franca AA, Santos VD, Filho RL, et al. ‘It’s very complicated’: perspectives and beliefs of newly graduated physiotherapists about the biopsychosocial model for treating people experiencing non-specific low back pain in Brazil . Musculoskelet Sci Pract. 2019;42:84–89.
- Igwesi-Chidobe CN, Coker B, Onwasigwe CN, et al. Biopsychosocial factors associated with chronic low back pain disability in rural Nigeria: a population-based cross-sectional study. BMJ Glob Health. 2017;2(3):e000284.
- Park JH, Lee SH, Ko DS. The effects of the Nintendo Wii Exercise program on chronic work-related low back pain in industrial workers. J Phys Ther Sci. 2013;25(8):985–988.
- Setchell J. What has stigma got to do with physiotherapy? Physiother Can. 2017;69(1):1–5.
- De Souza L, Oliver Frank A. Patients’ experiences of the impact of chronic back pain on family life and work. Disabil Rehabil. 2011;33(4):310–318.
- Cano A, Gestoso M, Kovacs F, et al. The perceptions of people with low back pain treated in the Spanish National Health, and their experience while undergoing a new evidence-based treatment. A focus group study. Disabil Rehabil. 2014;36(20):1713–1722.
- Bunzli S, Watkins R, Smith A, et al. Lives on hold: a qualitative synthesis exploring the experience of chronic low-back pain. Clin J Pain. 2013;29(10):907–916.
- Lehman BJ, David DM, Gruber JA. Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Soc Personal Psychol Compass. 2017;11(8):e12328.
- Rebecca Olson AM, Fitzgerald L, Hichey S. The social and cultural determinants of health. In: Dune KM, R. Williams, editor. Cultural diversity and health in Australia: towards culturally safe health care. Crows Nest (Australia): Allen &Unwin; 2020.
- Wijma AJ, van Wilgen CP, Meeus M, et al. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: the first step in pain neuroscience education. Physiother Theory Pract. 2016;32(5):368–384.
- Roussel NA, Neels H, Kuppens K, et al. History taking by physiotherapists with low back pain patients: are illness perceptions addressed properly? Disabil Rehabil. 2016;38(13):1268–1279.
- Nordstoga AL, Vasseljen O, Meisingset I, et al. Improvement in work ability, psychological distress and pain sites in relation to low back pain prognosis: a longitudinal observational study in primary care. Spine (Phila Pa 1976). 2019;44(7):E423–e429.
- Foster NE, Delitto A. Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice-challenges and opportunities. Phys Ther. 2011;91(5):790–803.
- Pensri P, Janwantanakul P, Worakul P, et al. Biopsychosocial factors and perceived disability in saleswomen with concurrent low back pain. Safety and Health at Work. 2010;1(2):149–157.
- Miller JS, Pinnington MA, Stanley IM. The early stages of low back pain: a pilot study of patient diaries as a source of data. Fam Pract. 1999;16(4):395–401.
- Valencia C, Robinson ME, George SZ. Socioeconomic status influences the relationship between fear-avoidance beliefs work and disability. Pain Med. 2011;12(2):328–336.
- Nagarajan M, Nair MR. Importance of fear-avoidance behavior in chronic non-specific low back pain. J Back Musculoskelet Rehabil. 2010;23(2):87–95.
- Wand BM, Bird C, McAuley JH, et al. Early intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine (Phila Pa 1976). 2004;29(21):2350–2356.
- Cabak A, Rudnicka A, Kulej L, et al. Biopsychosocial rehabilitation programme for patients with chronic back pain. pilot study. Ortop Traumatol Rehabil. 2017;19(2):165–174.
- Sanders T, Foster NE, Bishop A, et al. Biopsychosocial care and the physiotherapy encounter: physiotherapists’ accounts of back pain consultations. BMC Musculoskelet Disord. 2013;14(1):65.
- Synnott A, O’Keeffe M, Bunzli S, et al. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother. 2015;61(2):68–76.
- Suls J, Rothman A. Evolution of the biopsychosocial model: prospects and challenges for health psychology. Health Psychol. 2004;23(2):119–125.
- Froud R, Patterson S, Eldridge S, et al. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet Disord. 2014;15:50.
- Froud R, Ellard D, Patel S, et al. Primary outcome measure use in back pain trials may need radical reassessment. BMC Musculoskelet Disord. 2015;16(1):88.
- Hush JM, Refshauge KM, Sullivan G, et al. Do Numerical Rating Scales and the Roland-Morris Disability Questionnaire capture changes that are meaningful to patients with persistent back pain? Clin Rehabil. 2010;24(7):648–657.
- Rose N, Abi-Rached J. Governing through the brain: neuropolitics, neuroscience and subjectivity. Camb J Anthropol. 2014;32(1):3–23.
- Jette AM, Delany C, Lundberg M. The value of qualitative research in physical therapy. Phys Ther. 2019;99(7):819–820.
- Setchell J, Nicholls DA, Wilson N, et al. infusing rehabilitation with critical research and scholarship: a call to action. Physiother Can. 2018;70(4):301–305.
- Baum F, Fisher M. Why behavioural health promotion endures despite its failure to reduce health inequities. Sociol Health Illn. 2014;36(2):213–225.
- Van Den Broucke S. Needs, norms and nudges: the place of behaviour change in health promotion. Health Promot Int. 2014;29(4):597–600.
- Australian Institute of Health and Welfare. Australia’s health 2016. Canberra: AIHW; 2016.
- Main CJ, George SZ. Psychologically informed practice for management of low back pain: future directions in practice and research. Phys Ther. 2011;91(5):820–824.
- Wilson S, Chaloner N, Osborn M, et al. Psychologically informed physiotherapy for chronic pain: patient experiences of treatment and therapeutic process. Physiotherapy. 2017;103(1):98–105.
- Keefe FJ, Main CJ, George SZ. Advancing psychologically informed practice for patients with persistent musculoskeletal pain: promise, pitfalls, and solutions. Phys Ther. 2018;98(5):398–407.
- Ecclestone K. Emotionally‐vulnerable subjects and new inequalities: the educational implications of an ‘epistemology of the emotions. Int Stud Sociol Educ. 2011;21(2):91–113.
- Ferreira PH, Ferreira ML, Maher CG, et al. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Phys Ther. 2013;93(4):470–478.
- Beneciuk JM, George SZ, Greco CM, et al. Targeted interventions to prevent transitioning from acute to chronic low back pain in high-risk patients: development and delivery of a pragmatic training course of psychologically informed physical therapy for the TARGET trial. Trials. 2019;20(1):256.
- Pilgrim D. The biopsychosocial model in health research: its strengths and limitations for critical realists. J Crit Real. 2015;14(2):164–180.
- Verhagen PJ. Psychiatry and religion: consensus reached! Mental Health Relig Cult. 2017;20(6):516–527.
- Foucault M. The birth of the clinic: an archaeology of medical perception. London: Tavistock; 1973.
- Foucault M. The archaeology of knowledge. New York: Harper & Row, 1976.
- Nicholls DA, Atkinson K, Bjorbaekmo WS, et al. Connectivity: an emerging concept for physiotherapy practice. Physiother Theory Pract. 2016;32(3):159–170.
Appendix A
Table A1. Characteristics of studies included in this critical review that discussed the biopsychosocial model in low back pain in physiotherapy.

