Abstract
Purpose
Health care providers have highlighted the need for tools and resources that support promotion of exercise behavior within comprehensive multiple sclerosis (MS) care. This study involved a final quality improvement evaluation of exercise promotion models and materials for inclusion within this setting.
Methods and materials
Our research team distributed a paper-based survey containing Likert scales, open answer questions, and copies of the models for editing. We distributed this survey among health care providers across the United States. We conducted a novel mixed-methods analysis evaluating quantitative, qualitative, and creative data.
Results
We received completed surveys from 13 health care providers who strongly rated the clarity and applicability of the models and materials, and reported that no major improvements were necessary. The minor improvements were specific per comprehensive MS care center. The feedback indicated that the “Exercise in Medicine” models and materials are guides such that the processes should be integrated into real world practice by amending roles and responsibilities with the team members and structure per comprehensive MS care center.
Conclusion
This paper presents finalized models and materials for exercise promotion within comprehensive MS care that are ready to be tested for feasibility and efficacy in a clinical trial.
Health care providers require support to promote exercise within the context of comprehensive MS care.
The practice models in this article provide guides regarding how to promote exercise in this context.
Implementing these exercise promotion guides can reduce the burden of neurologists, and ensure patients receive exercise support from appropriate providers.
These guides should be implemented within the context of each individual care center, and not as an explicit step by step guide as each care center is unique.
IMPLICATIONS FOR REHABILITATION
Introduction
Exercise is one of the best strategies for safely managing multiple sclerosis (MS) symptoms, relapses, and disability progression [Citation1,Citation2]. Nevertheless, fewer than 20% of persons with MS engage in sufficient amounts of exercise for experiencing health benefits [Citation3]. This may be remediated by addressing the gap between evidence-based benefits and translation of these benefits into behavior change [Citation1] through the patient-provider interaction in comprehensive MS care. Qualitative data from both MS patients and health care providers indicate that meaningful exercise behavior change can occur in this relationship [Citation4,Citation5]. The recognized potential of the patient-provider interaction has become the focus of a pivotal line of research creating a systematic process for exercise behavior change in comprehensive MS care. Further, there is a need to extend exercise support beyond care centers and into the community. Indeed, a key issue identified regarding the long-term adoption of exercise behavior is the gap between direct health care services and community-based exercise support and programs [Citation6,Citation7]. Cooperation between health care providers and exercise specialists can be one of the most important stages for a patient’s successful transition from rehabilitation to community practice, but is often neglected [Citation8]. In this paper, we present a systematic process for exercise behavior change in MS that includes an interdisciplinary intervention within comprehensive care including neurologists, nurse practitioners, physical therapists (PTs), and occupational therapists (OTs), and community support through exercise specialists. This process is called “Exercise in Medicine.”
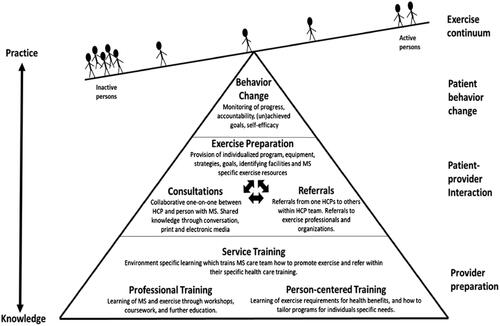
The foundation for creating the “Exercise in Medicine” process was based on the respective needs and wants of persons with MS and health care providers for exercise promotion. Persons with MS desired (a) information and knowledge of the benefits of exercise and exercise promotion, (b) materials for home and community exercise, and (c) tools from health care providers for initiating and maintaining exercise behavior [Citation4]. Health care providers desired (a) opportunities for exercise promotion, (b) education on effective exercise for persons with MS, and (c) tools and strategies that would facilitate exercise behavior change [Citation5]. These qualitative data were the building blocks for the creation of a conceptual model that encompassed the needs and wants of both entities [Citation9]. This model was then put through a rigorous vetting process that involved evaluation by persons with MS [Citation10] and health care providers [Citation11] resulting in a final conceptual model, the “Exercise Promotion for Multiple Sclerosis Conceptual Model” (). The conceptual model involves three hierarchically organized, interactive layers that represent (a) the necessary training of health care providers in exercise promotion; (b) the interactive, dynamic consultation between the patient and the provider regarding exercise promotion; and (c) ongoing support of patients by health care providers for initiation and maintenance of exercise behavior change. These three layers support the ultimate goal of increasing exercise engagement among persons with MS.
The conceptual model was deemed a useful and meaningful tool for exercise promotion, yet health care providers suggested the importance of developing tools that translate this model into practice [Citation11]. Such practical tools were developed through a quality improvement (QI) approach using a Plan-Do-Study-Act (PDSA) design. QI approaches are an essential first step for developing, refining, and implementing materials for clinical practice in health care settings [Citation12]. The PDSA design facilitates rapid generation of knowledge and support by testing materials prior to implementation [Citation13], and can occur through a ramp involving multiple cycles of QI assessment [Citation14]. PDSAs rely on a small number of specific persons relative to the context of the implementation setting to collect just enough data to select one of three outcomes; adopt, adapt, or abandon the change idea [Citation15].
The first PDSA study [Citation6] involved 20 health care providers (5 neurologists, 5 nurse practitioners, 5 PTs, and 5 OTs) who completed an online survey containing Likert and short answer questions regarding 3 different practice models for implementing the “Exercise in Medicine” process – the 3 practice models were dependent on each patient’s safety and readiness for exercise and the degree of health care provider intervention required before the patient could safely engage in independent exercise. Results from this first PDSA study indicated that health care providers valued the screening tool and models as necessary and useful resources for promoting exercise within comprehensive MS care. There were recommendations for improvements including (a) direct referral to PT/OT rather than a nurse for exercise promotion as appropriate; (b) contextualizing the models within the “Exercise Promotion Conceptual Model in Multiple Sclerosis”; (c) providing information on training and resources for neurologists, nurse practitioners, PTs, and OTs; and (d) providing information on community support. We incorporated these improvements and created refined screening tools and models that were then “ramped up” for the second PDSA cycle.
This second PDSA cycle [Citation16] involved an online survey involving Likert and short answer questions distributed among comprehensive MS care centers throughout the United States (US) via e-mail from the National Multiple Sclerosis Society (NMSS). We received 13 completed surveys from health care providers. This was a lower response than anticipated, but the data informed further refinement and improvement of the exercise promotion materials. The changes included (a) the addition of checklists per practice model, (b) changing the role of referral from the neurologist to the nurse, and (c) including questions regarding current exercise behavior into a quick screening tool. Such changes resulted in refined practice models that were evaluated in this study (Supplemental materials).
Accordingly, the current study involved a 3rd PDSA examination of practice models and materials for exercise promotion through the patient-provider interaction in comprehensive MS care. We expected minimal substantive feedback regarding problems with the models and materials, and therefore expected a decision of “adopt” the change idea [Citation15].
Materials and methods
We adopted a PDSA quality improvement design for evaluating and improving models and materials for exercise promotion in comprehensive MS care. The PDSA method followed valid guidelines [Citation13] and we received approval for this study from the University of Alabama at Birmingham.
Design and sampling – “plan”
This was the 3rd PDSA cycle conducted focusing on improving models and materials. After the 2nd round PDSA, we redesigned the materials incorporating improvements recommended by participants, amended the survey by including checklists, and transposed the survey from online to paper-based. The survey incorporated a novel, mixed-methods design whereby participants were asked to complete quantitative, qualitative, and creative methods in that participants could literally write on the models being evaluated and edit, amend, and delete content as necessary (the survey is included in Supplementary materials). We then conducted a search through the NMSS website and navigators portal and created a list of all comprehensive care centers in the US that had at minimum a neurologist and nurse, but preferably with a PT and/or OT. All comprehensive MS care Centers of Excellence across the US that had a neurologist and nurse practitioner on staff were included in this sampling frame (n = 150).
Data collection – “do”
We sent the surveys through the US postal service including a prepaid, addressed envelope with which surveys could be returned. We sent surveys in batches of approximately 50 to comprehensive care centers to better manage the data. Surveys were sent at the beginning of January, February, and March with a closing date of 10 April 2020. Two weeks after surveys were sent, we sent a reminder letter. We offered the chance to be placed in a drawing for 1 of 4 $250 visa gift cards for the MS team as an incentive and thank you for participating. Consent was self-selection as prospective participants had the choice of completing and returning the survey or not participating. We included only fully completed surveys in data analysis. Upon receipt of completed surveys, we input quantitative data into SPSS, qualitative data into a word document, and models that had been edited first-hand into a separate folder. All identifying information were separated and stored in a double locked space.
Data analysis – “study”
The response rate was low with only 11 care centers represented (a 7.3% response rate) and 13 complete surveys. The majority of respondents in the 3rd cycle of PDSA were different from the 1st and 2nd cycles. This lends greater input and support regarding the continued revision and improvement of the “Exercise in Medicine” models and materials, and that health care providers may perceive this process being effective within the context of their unique comprehensive care center. Data were analyzed using analytical eclecticism, which complemented the novel, mixed methods design of the survey. Analytical eclecticism is an approach that allows researchers to address different elements of scholarship from different research traditions [Citation17]. To apply analytical eclecticism to this mixed methods data set, we analyzed quantitative data with SPSS descriptive statistics, and qualitative and creative data through qualitative content analysis. Following Hsieh and Shannon’s [Citation18] guide to content analysis, we adopted a summative content approach. In this approach researchers note the number of occurrences a word or phrase is used, and then explore this within a wider, more meaningful context. In this case of this research, after counting occurrences of, for example, “referral to community support” as a strength, we then contextualized this within the wider “Exercise in Medicine” process and in the context of exercise promotion in comprehensive MS care. The “Act” part of PDSA will be presented in the Results section wherein we apply improvements recommended based upon the data.
Results
Of 13 completed surveys, one participant was a neurologist, 3 were nurse practitioners, 5 were PTs, and 4 were OTs. Health care providers were representative of 12 states from across the US. Ten participants were female and 3 were male. Age ranged between 33 and 65 years with a mean age of 53 years. Years of experience ranged between 2 and 42 years with a mean years of experience of 19 years. All participants answered mixed-methods questions regarding strengths, weaknesses, and improvements of the quick screen model, “Exercise in Medicine” models, and “Exercise in Medicine” checklists. SPSS descriptive data highlighted overall perceptions, and the qualitative content supported and expanded reasons for quantitative scores, thereby providing a more in-depth and contextualized evaluation. Of note, there were no significant differences between care centers or disciplines regarding suggestions or reports of strengths and weaknesses.
Quick screen model
The quick screen model represents a decision tree that assists healthcare providers to assess the readiness, safety, and required intervention of patients with MS before prescribing exercise. The vertical column represents questions that will inform healthcare providers regarding assignment of patients into “Exercise in Medicine” Model 1 (minimal interventions), “Exercise in Medicine” Model 2 (moderate intervention), or “Exercise in Medicine” Model 3 (significant intervention).
Participants were asked to rate the clarity, relatability and appropriateness of each scenario, as well as their confidence initiating each, on a scale of 1= not at all, to 5 = very. Participants highly rated the clarity of the quick screen process with a mean score of 4.1 (range 1–5; SD = 1.2), and further highly scored the relatability of the quick screen process with a mean score 4.0 (range 1–5; SD = 0.8). Appropriateness scores were in the middle range with a mean score of 3.2 (range 1–5; SD = 1.6), and confidence of nurses carrying out the screen was the lowest score of 2.9 (range 1–5; SD = 1.4).
Reasons for these scores were reflected in the qualitative data regarding strengths, weaknesses, and improvements of the quick screen model. Regarding strengths, 5 participants stated the quick screen model was easy to follow: “(1) Easy to follow (2) short timing for evaluation (3) not confusing” (OT, 11 years experience); 4 highlighted the clarity of the process, “Clear, easy to follow, effectively captures almost all patients” (PT, 5 years experience); 4 stated the idea of screening patients for exercise was a key strength, “The overall concept of screening patients for exercise intervention” (PT, 18 years experience); 2 discussed the consideration of insurance as a positive aspect, “Agree path is largely dependent on insurance coverage options for PT and ability to exercise on their own” (nurse, 22 years experience); and 2 identified the acknowledgement of different requirements of therapy:
This offers an easy to integrate screen to identify people who might be appropriate to refer to therapy! 2) catching this as early as possible and asking everyone with MS who has a medical appointment will help cast a wider net. (OT, 19 years experience)
Other strengths that were mentioned only once by healthcare providers were: screening helped the physician, “Getting MS nurse involved will help physician and appointment” (neurologist, 42 years experience); patient safety was considered, “Patient safety was considered as part of decision” (nurse, 22 years experience); and it was brief, “Can be done quickly and efficiently before appointment” (nurse, 10 years experience).
On the other hand, participants highlighted a main weakness of the quick screen model being centered around the nurse. Five stated the nurse determining the length of therapy was not appropriate:
I think this is a great idea; however nurse don’t understand the clinical reasoning that goes into establishing the length of a plan of care (etiology of impairments, barriers and facilitators to compliance, translation to phone/community, prognosis for recovery etc.) This would be difficult for a non-therapist to determine which track a person should go down. This is something even nurse would have a challenge doing. (OT, 19 years experience)
Three highlighted the nurse doing the screen in general was a weakness, “Here our nurses have little face to face contact with patients 2) “RN time is largely on phone” (nurse, 22 years experience); 3 stated no perceived weaknesses, 2 participants expressed a belief that readiness to exercise questions were missed, “Misses readiness questions” (PT, 2 years experience); 2 questioned the lack of focus on barriers to therapy, “Didn’t factor in transportation or other barriers to therapy” (nurse, 10 years experience); 2 stated there was a missed opportunity to describe benefits of exercise:
As indicated on the diagram, I think there is still an opportunity to mention exercise and it’s benefits. Many people won’t see their neuro for 6–12 months, so check-in at the next visit seems like a missed opportunity to at least mention exercise benefits. (nurse, 10 years experience)
And 2 stated the arbitrary 18 PT/OT visits was a main issue
How does nursing determine if need >18 visits? Why did you pick 18 visits? If 18 is cut off you are missing majority of patients needing(s) and getting great benefits from PT visits. (PT, 13 years experience)
Weaknesses that were mentioned once were we did not include speech therapy in the core team:
LEAVES OUT SPEECH!!! I know this is focusing on activity, but cognitive challenges can be the biggest limiting factor to success and are a VERY important part of rehab to following through with consistent exercise. (OT, 19 years experience)
Further, the screen would take too long to complete, “Hard to in our MDC clinic (multi D) or provider visit (although those visits are already not long enough! Adding another screen may be hard in regular FU” (nurse, 22 years experience); why insurance would influence access to therapy:
Why should health insurance have anything to do with whether a patient has access to exercise/rehab (out patient therapy)? The patient and therapist can decide what is appropriate/necessary care for their condition, work around patient resources, locate funding etc. (OT, 3 years experience)
And there were no specifics for wheelchair users, “Not specific on including patients mobility such as wheelchair bound, how would they do exercise?” (PT, 18 years experience). Such qualitative data supports why relatability and appropriateness scores were scored lower than others.
The key improvements participants identified involved: additional questions included to the screen (5 participants):
(1) What do you feel are the benefits of exercise (2) When was your last PT? (3) Was it helpful (4) What did it help, what not? (5) Would you be willing to do? (6) What would be your goals? (7) What are your barriers, insurance, $, transportations, family support, time of work etc. (PT, 7 years experience)
Three participants suggested changing the responsibility of screen to the PT, “Include a PT as the HCP. Each MS center should have a PT on staff dedicated to this” (PT 14 years experience). Four participants stated no improvements were required, “No changes” (OT, 11 years experience) and 1 participant suggested identifying mobility level:
Patients should be identified by mobility level prior to the tree (1) wheelchair/transfer mobility level (no walking) (2) household distance ambulator (50 feet or less) (3) community distance ambulator (prolonged distances). (PT, 18 years experience)
“Exercise in medicine” model 1
Model 1 depicts a course of exercise promotion for patients with MS who require minimal healthcare provider intervention. With this scenario, the nurse takes the lead by conducting the quick screen process, placing the recommendation for the Model 1 process into notes for the neurologist, then providing patients with the exercise toolkit (to be provided by the Exercise Neuroscience Research Lab (ENRL)). The exercise toolkit includes tangible materials such as exercise equipment, DVDs, instructions and accountability documents such as diaries. Part of this toolkit also involves a one to one coaching and support intervention with individualized programs delivered by exercise specialists to provide community support. The objective is to support persons with MS in long term exercise behaviour change by meeting the exercise guidelines for MS and reap the physical, social and psychological benefits this entails [Citation19]. Referral to community support via the ENRL is made through the nurse. The ENRL then take on responsibility for providing community exercise support and delivering the behavior change intervention. Participants highly rated the clarity of “Exercise in Medicine” Model 1 with a score of 4.1 (range 2–5; SD = 0.8). Relatability and appropriateness were scored in the middle range with scores of 3.6 (range 1–5; SD = 1.1) and 3.7 (range 1–5; SD = 1.4), respectively. Confidence of respective roles was highly scored with a mean score of 4.1 (range 2 − 5; SD = 1.0).
Qualitatively, participants highlighted 6 strengths of “Exercise in Medicine” Model 1: (1) the provision of tele-support and resources as follow-up after the patient’s clinical appointment (5 participants), “Offers follow-up, telesupport and resources! Love it!” (OT, 19 years experience); (2) the idea to implement exercise behavior change (3 participants), “This is a great idea, specifically exercise behavior change” (PT, 18 years experience); (3) the model is easy to follow (2 participants), and easy to apply (2 participants), 1) Easy to follow 2) Easy to apply” (OT, 11 years experience); (4) the model is consistent with center practice (1 participant), “Exercise plan is consistent with what we try to do for promotion” (PT, 14 years experience); and (5) the model is a great way to get people who may not require PT/OT involved in exercise (1 participant), “Great way to get people who may not need PT/OT at the moment but might help them engage in exercise” (OT, 19 years experience).
There were, however, weaknesses. These weaknesses were very specific within comprehensive care centers. Four participants stated no weaknesses in the model and only one participant each mentioned (1) what is the ENRL?, (2) what is in the toolkit? (3) why just the ENRL as follow-up, (4) no education for PT/OT, (5) no time to implement, and 6) the bottom half of the model with the pyramids distracts:
What is the ENRL - need to have definition for those that are not familiar, maybe put in () next to the full or add to the bottom with. (OT, 21 years experience)
Don’t know what it’s in the toolkit. (nurse – 9 years experience)
The model does not allow for other potential resources, besides ENRL (unless that is specifically contained in the toolkit). There may be local resources which would be helpful for exercise promotion. Also, other web resources may be helpful in getting someone to indicate an exercise program. (nurse, 10 years experience)
There is no education about PT/OT in the clinic. (PT, 18 years experience)
Not enough time in visits already and would be hard to incorporate more screening. (nurse, 22 years experience)
Bottom 1/2 pyramid don’t add to this model; they distract the reader. The print is tiny. (PT, 13 years experience)
To improve the model, again participants stated specific requirements for respective comprehensive care centers. Four participants stated no improvements were necessary; but 1 participant each stated the necessity of including a phone support system for patients with cognitive deficits, a timeline for when community support interventions would start, removal of the conceptual model from the bottom of the model, and changing the role of the nurse and the PT:
Very concerned that patients cannot access website or remember how due to cognitive decline. Provide a telephone support system to assist with community support. (OT, 11 years experience)
Include timeline between when patient is told they get ENRL support to when contact is made. (nurse, 22 years experience)
Take out pyramids. (PT, 13 years experience)
No concerns about the model itself neurologists and RNs GENERALLY SPEAKING, are not the best resources for advice on exercise. PTs should be the main driver. The toolkit and ENRL support must be of high quality. (PT, 5 years experience)
“Exercise in medicine” model 2
Model 2 depicts a course of exercise promotion for patients that require moderate health care provider intervention before engaging in community-based exercise. With Model 2, a patient expresses an interest in exercise and has insurance for health care provider intervention, but has mild physical/cognitive/sensory deficits that require short-term health care provider intervention. Once again the nurse initiates the quick screen, determines if the patient requires intervention through Model 2, and inserts this process into neurologist notes. Neurologists encourage exercise as a therapeutic intervention and refer to PT/OT. The nurse manages this referral. The role of PT/OT is to assess physical deficits and work with the patient toward safe engagement in exercise. PTs/OTs provide the exercise promotion toolkit when the patient is ready to be discharged. Referral to community support via the ENRL is made through the PT once the patient is cleared to exercise safely. The ENRL then take on responsibility for providing exercise support and delivering the behavior change intervention.
Overall, descriptive scores for “Exercise in Medicine” Model 2 were high. The clarity of “Exercise in Medicine” Model 2 was scored as 4.1 (range 2–5; SD = 0.9). Relatability was scored as a mean of 3.9 (range 1–5; SD = 1.1), and appropriateness of roles scored as 3.8 (range 1–5; SD = 1.2). Confidence in implementing the model through respective roles was also scored highly with a mean of 4.3 (range 3–5; SD = 0.9).
Highlighted strengths of this particular model were similar to model 1. Three participants stated the tele-support and resources were a key positive of the model:
Outlines an appropriate way to follow up after discharge! Love it! 2) I like that they get the toolkit before therapy starts. This will get this started sooner rather than later (sometimes there is a wait to get into OT/PT). (OT, 19 years experience)
Two participants highlighted the model was easy to follow, 1 participant stated that the difference between Model 1 and Model 2 was appropriate, “Difference between/transition from model 1 and model 2 and appropriate and intuitive” (PT, 5 years experience); 1 participant stated Model 2 sets the stage for successful PT, “Helps set stage for successful PT treatment plan” (PT, 7 years experience); and 1 participant stated Model 2 would be easy to apply, “Easy to apply in practice” (nurse, 9 years experience).
Four participants stated no weaknesses were identified, 3 stated the nurse’s role was not appropriate, “Nurse would not be the one to do this” (nurse, 10 years experience); and, similar to Model 1, 1 participant stated again not knowing the content of the toolkit or the involvement of the ENRL.
To address these weakness, 4 participants stated no improvements were required, 3 stated the PT should be the driving health care provider for the “Exercise in Medicine” process, “The physical therapists should be the ones to determine length of plan of care” (OT, 19 years experience) and 1 person each stated removing the conceptual model pyramid and providing telephone support would improve Model 2; “Take out pyramids” (PT, 13 years experience), “Phone system for another layer of communication” (OT, 11 years experience).
“Exercise in medicine” model 3
Model 3 depicts the course of exercise promotion for patients who require significant health care intervention before engaging in exercise independently. With Model 3, a patient expresses an interest in exercise and has insurance for health care provider intervention, but has moderate physical/cognitive/sensory deficits that requires longer, intensive health care provider intervention. Health care roles and responsibilities in Model 3 are the same as Model 2, but health care providers expect that patient deficits will be more severe and require a longer intervention plan. Again, referral to community support via ENRL is made through the PT once the patient is cleared to exercise safely. The ENRL then take on responsibility for providing exercise support and delivering the behavior change intervention.
Scores for “Exercise in Medicine” Model 3 were similar to “Exercise in Medicine” Model 2 with all 4 elements scored highly. Clarity was scored as 4.2 (range 2–5; SD = 0. 9), relatability scored as 3.8 (range 1–5; SD = 1.4), appropriateness scored as 3.9 (range 1–5; SD = 1.3), and confidence implementing model scored as 4.2 (range 2–5; SD = 1.1).
Strengths, weakness, and improvements of “Exercise in Model 3” were very similar to Model 2. Strengths included the tele-support and resources provided to patients (5 participants), “In fear of sounding repetitive, the community telesupport and exercise toolkits are strongest contributions of models” (OT, 19 years experience); the model was easy to follow (3 participants), the model was easy to apply (2 participants), and the model may help facilitate behavior change (1 participant); “This approach may help facilitate long term behavior change” (PT, 5 years experience).
Weaknesses stated were similar to previous results with the majority of participants stating they perceived no weaknesses (4 participants), and other weaknesses highlighted by 1 participant. For model 3, these weaknesses were: (1) Don’t know what ENRL is; (2) Don’t know what’s in toolkit; (3) Don’t know clear difference between 2 and 3; “No clear difference between model 2 and 3; Is there a time frame/sessions difference?” (PT, 18 years experience); (4) Who checks inappropriate/unsafe exercise is not given? “Depending on how a patient gets triaged into this model, care should be taken that an inappropriate or unsafe exercise is given” (OT, 19 years); and (5) Not appropriate for nurse to do role, “Nurse should not decide length of therapy” (PT, 13 years).
Reflecting these weaknesses, improvements revolved around not changing the model (4 participants), and improvements that would work in each participant’s care center including: (1) More freedom for PT to recommend plan, “You never know what patient will need till you assess them. Give PT more freedom to determine length and structure of therapy and create therapy plan” (PT, 13 years); (2) Add education resources for PT/OT, (3) Add timeline to contact ENRL, “Add timeline when will be contacted by ENRL to model” (PT, 18 years experience); (4) Have information to give to patients after visit, “Potentially having different information to give patients depending on level of function, safety etc., at the end of the visit.” (PT, 18 years experience); and (5) Take out pyramids.
“Exercise in medicine” checklists
The “Exercise in Medicine” Checklists outline the key “to-dos” that are required by each health care provider to ensure the success of each model process. The checklists are included in each model’s “clinic” and “referral” sections and contain “checkboxes.” Participants highly scored the clarity of the “Exercise in Medicine” Model 1 checklist with a score of 4.5 (range 3–5; SD = 0.7). Relatability of the checklist in practice was scored as 3.8 (range 1–5; SD = 1.2) and appropriateness scored as 3.6 (range 1–5; SD = 1.4). Confidence implementing the model through respective roles was scored as 3.9 (range 1–5; SD = 1.4).
Qualitative data provided by participants stated: the “Exercise in Medicine” Checklist 1 had clear roles (3 participants), “Clear roles defined” (PT, 13 years experience); was easy to follow (2 participants) and easy to apply (1 participant), “Easy to follow. Easy to apply” (OT, 11 years experience); and provides more time for neurologists during the patient’s appointment (1 participant), “Allocation of neurologist time spent with patient more efficient due to RN assisting with pre and post appointment” (PT, 18 years experience). Regarding weaknesses, 5 participants stated there were no weaknesses, 2 stated nurses were not in every clinic, 2 indicated that nurses did not have time to do this:
I think the challenge (which wasn’t mentioned earlier, but appropriate to the different models) are some of the pre-appointment nursing responsibilities. In some settings, it may not be an area where nursing has time to implement along with other duties. (nurse, 10 years experience)
One noted that the scenarios were not clear, “What are scenarios? This is not clear enough” (PT, 18 years experience), and 1 argued that the wording was “too loose,” “words like encourage are to loose, vague – a tangible replacement is necessary” (PT, 5 years experience).
Five participants stated no improvements were necessary, 1 observed that the addition of PT/OT education was necessary, 1 reported that there was a need to integrate a flexible way of screening; “Consider different ways to implement screening, maybe part of paperwork while in the waiting room” (nurse, 10 years experience); and 1 stated that the PT should do the screen, “PT to do screen” (PT, 13 years experience).
The “Exercise in Medicine” Model 2 Checklist was very highly scored overall. Clarity of the model was scored at 4.6 (range 3–5; SD = 0.7), relatability scored as 3.9 (range 1–5; SD = 1.1), appropriateness scored as 4.3 (range 3–5; SD = 0.9), and confidence scored as 4.6 (range 3–5; SD = 0.7). “Exercise in Medicine” Model 3 Checklist was scored highly. Clarity of the model was scored as 4.4 (range 3–5; SD = 0.8), relatability scored as 3.8 (range 1–5; SD = 1.2), appropriateness scored as 4.4 (range 3–5; SD = 0.9), and confidence scored as 4.5 (range 3–5; SD = 0.8).
Strengths, weaknesses, and improvements of Model 2 and 3 checklists were identical. To surmise, strengths noted were that the checklists were (1) easy to follow (2 participants), (2) easy to apply (2 participants), (3) provided clear roles (2 participants), (4) provided clear instructions (2 participants), (5) aligned to the traditional approach in the participant’s center (1 participant), (6) closed communication gap between clinic and community (1 participant), and (7) triaged people to appropriate therapy (1 participant). Five participants stated no weaknesses in the checklists, while 2 participants stated they did not have a nurse at their centers, and 1 person each stated that there may be delays in referrals, nurses didn’t have time, scenarios were not clear, there was a lack of designation to follow up with neurologist, and there was no time frame to get the ENRL involved:
Lack of timelines/timeframes indicated specifically how long is support from ENRL - what qualifies a patient for support from ENRL - what is indicator they don’t need it anymore? can they be cut off on services. (PT, 18 years experience)
Reflecting these weaknesses, 5 participants stated no improvements were required, 3 stated PTs needed to be more involved, 1 person suggested that tele-support is needed, 1 proposed that a continuation loop is needed to feedback to the neurologists, “Add continuum of care loop to indicate post-therapy to follow up with neurologist” (PT, 18 years experience) and 1 stated speech therapy should be included.
“Act”
PDSA is a methodology that involves a ramp of multiple cycles of QI assessment [Citation14] using small numbers of specific persons relative to a context in order to collect just enough data to select whether adopt, adapt, or abandon the change idea [Citation15]. Across the PDSA ramp, health care providers have reported increasingly higher scores regarding clarity, relatability, appropriateness, and confidence in assigned roles within each model scenario. Within this particular iteration, scores regarding clarity were particularly high across all materials. This is further supported by qualitative testimony where comments regarding material clarity and ease of following the process were the most numerous strengths mentioned. Confidence implementing the models was highly scored, and highlighted that healthcare providers were perhaps comfortable taking on assigned roles and responsibilities within the “Exercise in Medicine” process. When merging the high scores and the supplementary qualitative data, we can conclude that the models and materials are easy to follow and in-line with the responsibilities of health care providers regarding exercise promotion. One further strength noted was the support provided in the community after the clinic appointment. This may be based on the gap between clinic-based exercise such as in-patient rehabilitation, or a referral for PT, and the continuation of exercise behavior based on this recommendation.
The majority of participants did not identify substantial weaknesses in the models and checklists, and suggested that no improvements were necessary. We decided, therefore, that we could adopt the models and materials as presented. We did acknowledge, however, that there were some weaknesses identified, but in evaluating within a larger context these were specific within the care team or structure of each unique care center. Therefore, the uniqueness of comprehensive care centers was an important consideration. The common improvement suggested by participants was transitioning the role of screening away from the nurse as it was not appropriate for the nurse to determine the length of therapy, but this proposition contradicted the improvement explicitly stated in the 2nd cycle of PDSA whereby participants stated the nurse should undertake this task. This added further support of emphasizing the “Exercise in Medicine” as a guide of process rather than an explicit instruction that must be performed by the assigned disciplines.
Collectively, we have adopted these checklists and models for implementation, but we will produce an instruction manual that makes clear the “Exercise in Medicine” process is a guide and that roles and responsibilities can be amended as required per context. We will further state the screening process involves a minimum of questions, and comprehensive care centers can craft additional questions as necessary. This supports the adaptability of the “Exercise in Medicine” process when applied within comprehensive MS care centers.
Discussion
Healthcare providers, particularly neurologists, require tools and support for promotion of exercise among patients with MS [Citation4]. Over the past 5 years, we have created an exercise promotion system that can be integrated within MS care. This system was developed through empirical data [Citation4,Citation5] resulting in development and refinement of a conceptual model [Citation10,Citation11] and the translation of concept into practical models and materials through quality improvement methodology [Citation16,Citation20]. We believe the 3rd cycle of PDSA methodology has yielded final materials and models required for applying the “Exercise is Medicine” process within practice. As such, we have chosen to adopt the materials, but amend the description for improving implementation within comprehensive MS care. We have edited the description underlying the purpose of the “Exercise in Medicine” process highlighting that the roles and responsibilities can be amended between health care professions in such a way that best fit each unique comprehensive care center structure.
The conclusion of the materials development process to implement “Exercise in Medicine” is a significant step forward regarding the aim of integrating exercise promotion into comprehensive MS care by serving persons with MS and reducing the burden on neurologists. The final iteration of the “Exercise in Medicine” models and checklists meets the needs of both persons with MS and health care providers, as outlined in previous research [Citation11]. We anticipate that the final manual and process highlighting that each care center can amend roles and responsibilities will result in more efficient and timely exercise interventions for persons with MS. This may increase the number of persons with MS who meet the exercise guidelines for MS and improvement of health related quality of life, particularly as the “Exercise in Medicine” process incorporates health care provider and exercise specialists, and a long term community based exercise plan. Literature has highlighted a key pitfall in long term exercise behaviour among persons with neurologic conditions is a gap between outpatient rehabilitation release and community-based exercise support [Citation7]. The “Exercise in Medicine” process addresses this gap with direct referral to MS exercise and wellness specialists at the ENRL. This group provides community exercise support through provision of an exercise toolkit containing equipment, instructions and accountability documents, one to one coaching and support, and individualized programs to ensure persons with MS meet the exercise guidelines for MS [Citation19]. This process is a transformative approach linking medicine, rehabilitation, therapy and community based exercise [Citation8] that is a necessary addition to MS care.
We designed the “Exercise in Medicine” process within the context of comprehensive MS care, but we acknowledge that such an approach may be adapted for use in other chronic health conditions. We note that we have independently developed the “Exercise in Medicine” process through initial qualitative empirical data, building this into a conceptual model then transferring the conceptual idea into a more applicable format, but that this process is akin to the conceptual model developed for heart disease [Citation21]. Both the MS and heart disease exercise promotion models involve health care providers, barriers within clinical practice, acknowledge insurance limitations, and provide toolkits and materials for engaging and measuring exercise. The similarity across these chronic conditions supports the necessity for conceptual models, resources, and materials that promote and support exercise behavior, and that such models may be transferred and applied among other chronic health conditions with some small amendments that contextualize each specific condition. Thus, the models and materials we have developed may have significant implications not only within the literature and practice within MS, but beyond into other health conditions that can be managed through exercise interventions. Indeed, we advocate that the “Exercise in Medicine" process may be transferable to other chronic health conditions. Transferability in this sense, as defined by Tracy [Citation22] and Smith [Citation23], is that groups or persons in one setting might choose to adopt a practice from a difference settings. For example, health care providers in other conditions such as stroke, heart disease, Parkinson’s etc., might perceive overlap within the context of their practice and adopt the “Exercise in Medicine” process as something that may be beneficial for promoting and supporting exercise with their patients. As such, we advocate that the “Exercise in Medicine” models and materials need not be attributed only to cases of MS, but may be adopted and refined for practice within comprehensive care of any chronic illness or condition.
Related to transferability, and adding further support for “Exercise in Medicine” as a transferable and applicable process, the development of these models and materials also lends itself to analytical generalizability – a further qualitatively specific concept of rigor. Analytic generalizability can refer to a new concept or new theory that makes sense and has significance in other research, even though contexts or populations may be different [Citation23]. Thus, we posit that the “Exercise in Medicine” process is analytically generalizable as this model may be applied in the context of other chronical health conditions, but it is also similar to other models exploring exercise behaviour from rehabilitation to community exercise. For example, though each were developed separately through their own line of stringent research, there are apparent commonalities between the “Exercise in Medicine” process, the Transformative Exercise Framework [Citation8], and a physical activity promotion framework developed by the American Heart Association [Citation21]. Development of 3 similar frameworks in different contexts and different methodologies adds strength to the argument that the “Exercise in Medicine” process achieves analytic generalizability and can make a meaningful contribution to long-term management and wellness of persons with MS.
As we have chosen to adopt the “Exercise in Medicine” models and materials, we are now ready to test the feasibility and efficacy of this process in real world practice. We will create a final manual that outlines the “Exercise in Medicine” process and emphasize the importance of contextualizing the process within the structure and team that is in each unique comprehensive care center. Once this is complete, we will prepare for a clinical trial of this systems-based process from feasibility through efficacy and effectiveness in a comprehensive MS care center. This clinical trial will allow us to further vet and test the materials and the entire “Exercise in Medicine” process in preparation for larger scale implementation for improving exercise promotion in comprehensive MS care.
Limitations
This study is not without limitations. Participants were representative of less than 10% of over 150 comprehensive MS care centers. Further, the “Exercise in Medicine” models and materials were developed with a core care team of neurologists, nurses, PTs, and OTs in mind. Other disciplines such as physical medicine and rehabilitation, speech therapists, social workers, physician assistants, physiatrists, exercise practitioners and other multi-disciplinary roles were not acknowledged. Also, although we chose to adopt these models and materials for the next step of clinical trials, we are not yet ready to expand a scalable implementation process within comprehensive MS care. Related to our methodology, there are also limitations to note. First, the descriptive quantitative measures were developed for this study to tell the research story a different way, as such they do not have the strongest psychometric properties. Further, although we conducted a content analysis rigorously, qualitative analysis is only as strong as the data that is captured. While we hoped for in-depth, rich qualitative data, this was at times not the case. While PDSA methodology calls for a small number of expert participants to feedback on quality improvement measures, we do also note that changes made on few comments is a limitation. To address this, our future research plan involves broad and larger numbers of samples that will assist translation into action.
Conclusions
This paper presents the 3rd ramp of a PDSA cycle for evaluating and improving materials for exercise promotion in comprehensive MS care. This last iteration has resulted in finalized materials that can support health care providers when promoting exercise among patients with MS. Though we have not changed the models and materials, we will ensure the importance of applying the “Exercise in Medicine” process within the unique context of the structure and team of comprehensive care centers in order to “best fit” into practice. We conclude that we have created a robust and approved guide outlining how to effectively promote exercise integrated within comprehensive MS care, thereby translating from the conceptual model to applicable tools and are ready for clinical trials to further assess the “Exercise in Medicine” system.
Supplemental Material
Download Zip (3.6 MB)Acknowledgements
The authors would like to thank the contribution of participants that made this research possible.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Motl RW, Sandroff BM, Kwakkel G, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017;16(10):848–856.
- Motl RW, Pilutti LA. The benefits of exercise training in multiple sclerosis. Nat Rev Neurol. 2012;8(9):487–497.
- Klaren RE, Motl RW, Dlugonski D, et al. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehab. 2013;94(12):2342–2348.
- Learmonth YC, Adamson BC, Balto JM, et al. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: a qualitative study. Health Expect. 2017;20(4):574–583.
- Learmonth YC, Adamson BC, Balto JM, et al. Investigating the needs and wants of healthcare providers for promoting exercise in persons with multiple sclerosis: a qualitative study. Disabil Rehabil. 2018;40(18):2172–2180.
- Rimmer JH. Getting beyond the Plateau: bridging the gap between rehabilitation and community-based exercise. PM&R. 2012;4(11):857–861.
- Rimmer JH, Henley KY. Building the crossroad between inpatient/outpatient rehabilitation and lifelong community-based fitness for people with neurologic disability. J Neurol Phys Ther. 2013;37(2):72–77.
- Rimmer J, Lai B. Framing new pathways in transformative exercise for individuals with existing and newly acquired disability. Disabil Rehabil. 2017;39(2):173–180.
- Motl RW, Barstow EA, Blaylock S, et al. Promotion of exercise in multiple sclerosis through health care providers. Exerc Sport Sci Rev. 2018;46(2):105–111.
- Richardson EV, Blaylock S, Barstow E, et al. Evaluation of a conceptual model to guide health care providers in promoting exercise among persons with multiple sclerosis. APAQ. 2019;36(1):109–131.
- Richardson EV, Barstow E, Fifolt M, et al. Evaluation of a conceptual model regarding exercise promotion through the patient–provider interaction in multiple sclerosis: health care provider perspectives. Qual Health Res. 2020;30(8):1262–1274.
- Duffy G, McCoy K, Moran J, et al. The continuum of quality improvement in public health. Qual Manage Forum. 2010;35(4):1.
- Agency for Healthcare Research and Quality (AHRQ). Plan-Do-Study-Act (PDSA) cycle. 2008; [cited 2020 Mar 14]. Available from: https://www.ahrq.gov/health-literacy/quality-resources/tools/literacytoolkit/healthlittoolkit2-tool2b.html.
- Taylor MJ, McNicholas C, Nicolay C, et al. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23(4):290–298.
- Leis JA, Shojania KG. A primer on PDSA: executing plan–do–study–act cycles in practice, not just in name. BMJ Qual Saf. 2017;26(7):572–577.
- Fifolt M, Richardson EV, Barstow E, et al. Using quality improvement for refining program materials for exercise promotion in comprehensive multiple sclerosis care. J Health Qual. 43(4):249–258.
- Thomas G. A typology for the case study in social science following a review of definition, discourse, and structure. Qual Inq. 2011;17(6):511–521.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Motl RW, Backus D, Neal WN, et al. Rationale and design of the STEP for MS trial: comparative effectiveness of supervised versus telerehabilitation exercise programs for multiple sclerosis. Contemp Clin Trials. 2019;81:110–122.
- Richardson EV, Fifolt M, Barstow EA, et al. Exercise promotion in multiple sclerosis through the patient–provider interaction: development of practice models. Translat J ACSM. 2020;5(7):59–68.
- Lobelo F, Rohm Young D, Sallis R, et al. Routine assessment and promotion of physical activity in healthcare settings: a scientific statement from the American Heart Association. Circulation. 2018;137(18):495–522.
- Tracy SJ. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq. 2010;16(10):837–851.
- Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qual Res Sport Exer Health. 2018;10(1):137–149.