Abstract
Purpose
Post-stroke survivors report that feedback helps to increase training motivation. A wearable system (M-MARK), comprising movement and muscle sensors and providing feedback when performing everyday tasks was developed. The objective reported here was to create an evidence-based set of upper-limb tasks for use with the system.
Materials and methods
Data from two focus groups with rehabilitation professionals, ten interviews with stroke survivors and a review of assessment tests were synthesized. In a two-stage process, suggested tasks were screened to exclude non-tasks and complex activities. Remaining tasks were screened for suitability and entered into a categorization matrix.
Results
Of 83 suggestions, eight non-tasks, and 42 complex activities were rejected. Of the remaining 33 tasks, 15 were rejected: five required fine motor control; eight were too complex to standardize; one because the role of hemiplegic hand was not defined and one involved water. The review of clinical assessment tests found no additional tasks. Eleven were ultimately selected for testing with M-Mark.
Conclusions
Using a task categorization matrix, a set of training tasks was systematically identified. There was strong agreement between data from the professionals, survivors and literature. The matrix populated by tasks has potential for wider use in upper-limb stroke rehabilitation.
Rehabilitation technologies that provide feedback on quantity and quality of movements can support independent home-based upper limb rehabilitation.
Rehabilitation technology systems require a library of upper limb tasks at different levels for people with stroke and therapists to choose from.
A user-defined and evidence-based set of upper limb tasks for use within a wearable sensor device system have been developed.
IMPLICATIONS FOR REHABILITATION
Introduction
Approximately two-thirds of patients who survive a stroke have upper limb limitations, with only 5 to 20% demonstrating full recovery at 6 months post stroke [Citation1] contributing to reduced quality of life for survivors and caregivers [Citation2]. Principles of neuroplasticity from animal studies [Citation3] and motor learning from human studies suggest that repetition, challenge and feedback are some of the main facilitators for recovery of function [Citation4]. Studies comparing large differences in amount of therapy have shown greater functional improvement than those with smaller differences, for example [Citation5]. Furthermore, best practice guidelines recommend a prolonged period of rehabilitation [Citation7] but economic pressures have led to reduction in therapy time [Citation8] and intensity of practise in the clinic rarely reaches a number of repetitions that appears optimal based on animal studies [Citation6]. Stroke survivors therefore need to train at home to sustain and augment their rehabilitation. According to stroke survivors, themselves, training at home is not motivating unless accompanied by therapist input and a source of feedback [Citation9]. Assisting and optimizing self-management of rehabilitation is, consequently, a goal for both clinicians and researchers.
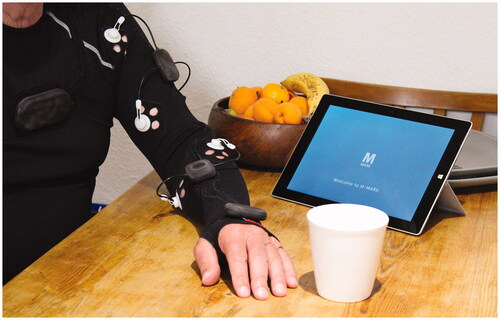
To address this problem we designed, built, and tested a novel device to support home-based rehabilitation that provided feedback on performance to both patients and therapists. M-MARK, an acronym for Mechanical Muscle Activity with Real time Kinematics [Citation10], comprises a garment with embedded inertial measurement unit (IMU) sensors to detect movement of trunk, shoulder, elbow, wrist (but not finger) coupled with mechanomyography (MMG) to detect synchronous mechanical muscle activity in biceps brachii, triceps brachii, wrist/finger extensors and flexors [Citation11]. Data are transmitted via Bluetooth from the device to a computer tablet with a user interface for system set up and to display feedback ().
Figure 1. M-MARK system including garment, sensors and user interface.
Algorithms were written to extract meaningful metrics from the sensor data to quantify amount and quality of movement and muscle activity and software was written to generate visual feedback in the form of an Avatar representing the patient’s movement and textual feedback guidance. The device was designed to be prescribed and set-up by a therapist and used independently by patients with face-to-face or remote support via video or telephone call from a health professional. To ensure clinical usability of the M-MARK device in terms of garment fit and ease of donning and doffing, as well as clarity of the user-interface and value of feedback, it was developed using “Person-Centered” design methodology with therapists, stroke patients with a range of abilities and their carers, and a final version was later tested with six patients and three therapists. Patients received qualitative feedback of their performance (from the sensors in the form of an avatar) immediately after, not during, a trial; a faded feedback schedule was employed. Quantitative summary feedback was received after a set number of trials consisting of number of repetitions and average time per task. Both types of feedback were also available for therapists with additional quantitative variables: joint range of motion (% compared to unaffected limb), smoothness, and trunk compensation (% movement compared to the unaffected limb). Summary feedback over time (weekly/monthly) was available to track intensity of training and change in performance.
An early aim of the project, and the topic of this research article, was to create a library of standard tasks for training and assessment. Tasks needed to be evidence-based, represent a range of functional movements at different ability levels, allow for progression and be considered important and relevant by therapists and patients.
Formation of task categorization framework
A Task categorization matrix () was constructed, based on motor control and rehabilitation literature, encompassing a range of upper limb motor control and rehabilitation requirements. The matrix comprised seven rows (1–7) representing task types. Task types were divided into two general categories, bilateral (two arms) and unilateral (one arm). Bilateral tasks were sub-divided into asymmetrical and symmetrical [Citation12]. We selected the most common type for each form: (Row 1) asymmetrical stabilization tasks in which the paretic hand is used to stabilize while the non-paretic hand has a complementary (more dexterous role) in the service of a common goal (e.g., stabilizing a piece of paper while writing). (Row 2) symmetrical in-phase tasks, in which both arms perform the same movement at the same time in the service of a common goal (e.g., lifting a tray). Unilateral arm movements were sub-divided into three types; continuous/repetitive, discrete and demanding serial motor control requirements [Citation13]. (Row 3) continuous/repetitive tasks (e.g., cleaning a window/brushing hair). We included (Row 4) unilateral supination/pronation (e.g., turn a card), cognoscente that inability to supinate the forearm, due to flexor synergy, is common among people with stroke [Citation14]. Serial tasks comprise multiple discrete movements “strung” together to complete a task with a clear beginning and ending. For example, picking up an object is composed of the three discrete tasks of reaching, grasping and lifting. Serial tasks were sub-divided into three types with different biomechanical requirements; (Row 5) reach away from the body ± grasp, lift and place; (Row 6) retrieve towards the body ± grasp and lift; (Row 7) reaching down ± grasp and use.
Table 1. Categorization of arm and hand tasks with progressions based on the literature.
Matrix columns representing four levels of difficulty were defined based on consensus between three physical therapist researchers (RT, CM, JB) between them with 20 years’ clinical experience in stroke rehabilitation including upper limb and more than 30 years’ experience in stroke upper limb research, and one kinesiology-rehabilitation researcher (JW) with 25 years’ experience, then confirmed by previous work by Woytowicz et al. [Citation15]. The levels of difficulty (basic to progressively more complex movements specific to each task) related to four levels of limb impairment (severe, severe/moderate, mild/moderate, mild), and the motor patterns that characterize each. Increasing difficulty was achieved through task specific progressions involving one or more of the following: number of elements in a serial task, which demanded more complex planning and motor control; number of planes of motion, for example an antigravity movement requires more ranges of motion and strength; changing the grip of an object from a power to a radial-digital grip, requiring finer motor control; and performing the task from a different starting position e.g., in standing. Within each task category, range of motion, speed and number of repetitions could be increased for training purposes and to provide challenges appropriate to each ability level. See which presents the categorization matrix.
Objective
The objective of this study was to populate the task categorization matrix described above with upper limb training tasks, identified through a systematic process.
Materials and methods
Data were sourced primarily from a two-part user-needs assessment study comprising one-to-one interviews with patients and carers, and focus groups with health professionals working in stroke rehabilitation. Secondarily, to add validity to the selection of tasks and ensure we included tasks considered by the wider rehabilitation community to be important in recovery, we reviewed valid and commonly used clinical assessment tools to identify additional tasks or task categories that we had not previously considered. Data from the three sources were synthesized to populate the task matrix described above.
User needs assessment
Data were generated via one-to-one interviews with sub-acute stroke survivors and carers, and focus groups with healthcare professionals. Data from both interviews and focus groups were audio recorded, transcribed verbatim and analyzed by applying pre-determined task and activity inclusion and exclusion criteria and fitting data that passed the criteria into the categorization matrix. All personal details were removed and data were anonymized.
Participants
Two groups of participants were recruited. Sub-acute stroke patients (and if appropriate their carer, i.e., someone who lived with them and provided support), were recruited from two rehabilitation sites in the UK (Portsmouth Hospitals University NHS Trust and North Bristol NHS Trust). Patients had been discharged from the acute stroke unit and were receiving community-based upper limb rehabilitation as part of an early supported discharge service. Patients were included if they had some upper limb movement and were currently undergoing upper limb rehabilitation, and scored 19 or higher on the Montreal cognitive assessment [Citation16] (scores between 19 and 25 correspond to mild cognitive impairment, and 25–30 represent normal cognition). They were excluded if their upper limb deficit was so minimal that treatment was not warranted and/or they were unable to provide useful feedback (either patient alone or with support of carer) due to communication difficulties. Purposive sampling was used to ensure a range of demographics: age, gender, social support, familiarity with technology and stroke-related upper limb severity. Upper limb severity was determined from the clinical assessment of the treating therapist and was based on what movement/activities patients could or couldn’t do. The categories they defined were: severe (minimal single-joint shoulder/elbow/hand movement in synergy to perform basic assisted functional activity e.g., sliding movements on a table or grasp object in lap); moderate (some single and multi-joint movement to perform part of a functional activity e.g., reach arm away from body, grasp and release object on a table) and mild most movement recovered but loss of fine control.
Rehabilitation professionals were recruited from the same two rehabilitation centers. Purposive sampling ensured a range of professions were recruited. Participants were senior staff with a minimum of three years’ experience in stroke rehabilitation. All potential participants were given a participant information sheet and gave written informed consent prior to recruitment. The guidelines of the Declaration of Helsinki were followed and the rights, dignity, safety and well-being of participants were respected throughout the study. Ethical approval was obtained from the NHS South West – Frenchay Research Ethics Committee (Ethics No. 188571).
Interviews with stroke patients
Interviews were conducted at the patient’s home between 1 and 16 weeks after discharge from an acute stroke unit to allow time for reflection on their rehabilitation without compromising recall. All interviews lasted between 60 and 90 min and were attended by a rehabilitation research fellow, a medical device industrial designer and a community physiotherapist. Interviews were semi-structured using a broad topic guide including which tasks, or functional activities as this is a more commonly used term, were important to them during their rehabilitation in hospital and at home. This allowed respondents a high level of control over the topics discussed.
The following questions, relative to task selection, were used in the interview schedule:
Which tasks or activities using your arms would you most like to be able to improve?
Which arm tasks and activities that you have practised in your rehabilitation have been most useful?
The following prompts encouraged respondents to expand on topics they felt were important and to suggest additional topics:
Are the tasks and activities you have suggested unilateral, bilateral or both?
What position are you in when doing these tasks and activities, e.g., sitting or standing?
Focus groups with health professional participants
Two focus groups were conducted, one at each rehabilitation center. The schedule was similar to that used with stroke patients and explored tasks or functional activities they would like included, at what level of patients’ ability they were appropriate for and how they could be progressed. Preferences on the design and use of the system were also explored, but are not reported here. The primary question put to participants was: what upper limb tasks or activities do you use with patients? The following prompts encouraged members of the group to expand on the topics they raised:
For what level of ability is the task or activity suitable?
How might the task or activity be adapted for patients with different levels of ability?
Are they unilateral and or bilateral tasks or both?
What position are patients in when they practise these tasks or activities, e.g., sitting or standing?
Data analysis
Data from 1:1 interviews and focus groups were recorded and transcribed verbatim. While upper limb tasks suggested by stroke patients were extracted from the transcriptions verbatim, health professionals’ suggestions were combined into one aggregate record for each focus Group to manage multiple citations during the group discussion. Raw data were anonymized and entered into an excel spreadsheet. Suggested tasks were labelled by data source. A frequency analysis of the stroke participant data determined how many times each suggested task was cited.
Data were then analyzed in a two-stage process by the same team of researchers mentioned earlier (RT, JW, CM, JB). In the first stage, raw data were filtered into three categories.
single purposeful tasks that could potentially be used in the system
non-tasks (e.g., joint specific exercises such as mass flexion/extension of hand, shoulder flexion, elbow flexion/extension; wrist circumduction and shoulder shrugging) where there is no specific functional task and no obvious outcome by which to measure successful performance.
highly complex Activities of Daily Living (ADL; e.g., dressing, making breakfast) that involved multiple component tasks performed in a variety of ways that were too complex to standardize, or to measure in a reliable way using the M-MARK system.
In stage two of the analysis all single purposeful tasks (a) were screened to assess their suitability. Each activity or task was categorized using the matrix shown in . If tasks were rejected the reason was cited using the following coding:
performance of the task primarily required fine-motor skills that could not be accurately measured or quantifiable by the system.
performance of the task was too complex to be accurately measured and standardized by either IMU or MMG or both – for example a task that could be performed with a wide range of normal, but different movement patterns and therefore not replicable.
role of the hemiplegic hand was not defined
performance of the task was not practical, for example, it required the use of items not typically available or could damage the system e.g., washing up.
Suitable tasks generated from stage two were entered into the matrix by classification into task type and level of stroke severity for which it was appropriate. Where there was more than one task per cell in the matrix, we used the frequency analysis (supplemental appendices 1 and 2) and professional judgement to select a single example.
Review of valid, commonly used clinical assessment tests
Using the website on Rehabilitation Measures http://www.rehabmeasures.org on 26 March 2016, we found 346 rehabilitation tests. Tests were initially screened using the following inclusion criteria:
Involved arm function for whole or part of the test.
Designed for Stroke (may include other populations)
Consisted of observer or performance measures (i.e., not self-reported)
Aimed at the Body Structure Function or Activity level of the International Classification Framework for Rehabilitation (World Health Organization; 2002).
Included tests and items within the tests were then screened to exclude: Non-tasks e.g., Joint specific exercises; Complex activities of daily living that could not be standardized; tasks that were impractical with M-MARK and tasks that required use of fine-motor skills. The final set of tasks identified from the tests were compared with those identified by patients and health professionals.
Results
User needs analysis
Ten stroke patients were recruited. Mean age: 71.3 (SD 10.1) years, time since stroke: 12.7 (SD 6.8) weeks and time since discharge: 5.4 (SD 4.9) weeks. Four were female, six had a left hemiparesis and in three the stroke affected their dominant upper limb. Patients’ stroke-related upper limb severity was categorized by their treating therapist as: severe (n = 5); moderate (n = 3) and mild (n = 2). Type of stroke: partial anterior (n = 3); thalamic infarction (n = 2); total anterior (n = 2); lacunar infarct (n = 1); frontal parietal hemorrhage (n = 1) and basal ganglia hemorrhage (n = 1). All patients took part in the single one-to-one interview. Seven of the 10 patients were accompanied by their carer during the interview, two had no carer at home. Twenty-three rehabilitation professionals were recruited and took part in one of two focus groups. The groups comprised: physiotherapists (n = 9), occupational therapists (n = 8), therapy assistants (n = 2), speech and language therapists (n = 2), a rehabilitation nurse (n = 1), and a psychologist (n = 1).
In phase one of the analysis across both patients and healthcare professionals, 75 unique tasks were suggested, a further eight suggestions were not included because they were not a task (i.e., they were exercises). Forty-two of the 75 were rejected because they were complex activities of daily living and therefore too variable to standardize. The remaining 33 single, purposeful tasks were then considered in the second stage of analysis to assess their suitability for the M-MARK system. Five were rejected at this stage because they could not be accurately measured as they involved fine motor control, eight because they could not be accurately measured being too complex to standardize, one because the role of hemiplegic hand could not be defined and one because the task was not practical, i.e., it involved using water. Eighteen tasks were therefore considered suitable ().
Table 2. Categorization of potential tasks suggested by stroke participants and carers during 1-to-1 interviews and by healthcare professionals in the focus groups.
These 18 suitable tasks were entered into the categorization matrix according to task category (rows) and level of ability (columns). In some instances, a task was either simplified or made more challenging so that it could be included in more than one ability level; e.g., dragging an object towards the body was a simplified version of bringing a cup to the mouth to drink. Using this process resulted in 28 tasks shown in . Eleven tasks, two, three or four in each category of severity ( in bold), were subsequently chosen to be tested further as part of the M-MARK system.
Table 3. Final selection of tasks and their progressions used to populate the categorization matrix.
Clinical assessment test analysis
The review of valid, commonly used tests identified 19 that satisfied the initial screening criteria. The following five tests were excluded because they only included tasks that failed the criteria, listed earlier, for being suitable for use with M-MARK:
Barthel Index of Activities of Daily Living
Hand-Held Dynamometer
National Institutes of Health Stroke Scale
Nine-hole Peg Test
Orpington Prognostic Scale.
Individual tasks from the remaining fourteen tests were selected using the same exclusion criteria as for the tasks suggested by patients and health professionals. In examples of each task category can be seen along with the test that included at least one task (but often many more) of that category. All seven task categories in the matrix were represented by tasks identified in the review, although none of the assessment tests included all seven categories. Cross comparison with show that the analysis of these standardized tests revealed no new task category. However, some of the tests provided different tasks to representing that category.
Table 4. The assessment tests and example tasks are classified by task category.
Discussion
In this study we have created a novel, evidence-based set of tasks to promote upper limb task training and monitor functional recovery following stroke. Tasks were selected to be appropriate for use with a sensor-based, wearable system (M-MARK) incorporating guidance, instructions and feedback on a computer tablet. A task categorization matrix was created, based on a review of motor control and rehabilitation principles that comprised seven task categories and four ability levels (). The matrix was then populated with tasks using a person-centered design process that integrated what patients (and carers) wanted to practice, what therapists thought they needed to practice and what is known from the motor control and rehabilitation literature to be critical for recovery. There was considerable overlap between tasks suggested by patients (and carers), and those suggested by health professionals (see frequency analyses in supplemental appendices 1 and 2). There was also agreement between tasks generated by users and those found in a review of validated and commonly used outcome measures. From the final matrix a subset of 11 tasks were chosen to form the training and assessment focus for the system (shown in bold in ).
The tasks selected meet the therapy-related criteria identified by Hochstenbach-Waelen and Seelen as being important for successful implementation of technology assisting upper limb training post-stroke which can be summarized as: patient-tailored and goal-tailored; task-oriented and resembling the real-life context of patients as closely as possible; include progression of difficulty; and offer variability in exercise [Citation17].
One of the criteria for inclusion of tasks was that they could be measured using IMU and MMG sensors. While this meant excluding both complex and fine motor tasks it provided rich data to inform patients and therapists about number of repetitions, time to perform task, range and smoothness of movement, amount of compensatory movement and relative muscle activity, as well as generating accurate visual feedback in the form of an Avatar representing patient’s arm movement. Other assessment tests may generate assessor-measured time or the ability to complete a task data as a quantitative outcome, or a rating system providing a quasi-objective method of assessing movement quality. The M-MARK system generates simultaneous quantitative and qualitative outcome data useful both for the therapist as a measure of progress and the patient as immediate motivational feedback. This richness of data underpins the system’s novel function to integrate training and assessment. M-MARK has been designed to augment standard rehabilitation and be used by patients independently at home (with carer help where needed). Independent use involves the oversight of a therapist to set-up their individualized upper limb exercise programme, determine number and difficulty of tasks and repetitions, and monitor progress. The tasks are the basis of this personalized task-orientated training program, allowing therapists to determine different dosages of exercise according to individual sensorimotor impairments and acknowledging that people may accomplish and make progress in the tasks in different ways. Metrics generated from the tasks can be used to provide motivational feedback to patients, for periodic assessment for therapists to review progress, and a decision-making tool to progress training. What matters is the individual progress in the different task categories and not what scores one individual may have relative to others. Tasks, therefore, are intended to be used as a measure of an individual’s progress during rehabilitation not as an outcome measure in clinical trials.
Unlike most technologies that promote recovery of upper limb function such as rehabilitation robots (e.g., Mit-Manus), hand-held devices (e.g., GripAble) and camera-based systems (e.g., Wii), all of which use virtual reality, M-MARK enables patients to practise every day functional tasks that are personalized and tailored to their own recovery and encompass a range of upper limb movements. Using “real objects” and specific functional tasks also provides normal sensory input and allows real-life progression in terms of range and direction of movement, motor control and force required, as well as number of repetitions and speed of performance. In addition to this, because the sensor component of the system is wearable, it can be used in a range of different environments and in different postures e.g., standing and sitting, enabling progressions of tasks. Although a computer tablet is required to receive feedback, users do not look at it while performing the tasks, enabling them to focus solely on the task in hand and, therefore, the sensorimotor mapping between intention and movement execution. As far as we know there are no other comparable systems.
Limitations
The limitations of this study relate to both the study design and the limitations of the system. Our classification framework included only two types of bilateral tasks, asymmetrical (stabilization) and symmetrical (in-phase). It did not include an asymmetrical task with independent goals (e.g., lifting a glass with one hand while moving a plate) or two other types of symmetrical tasks, alternating or anti-phase (e.g. pulling a rope) and complex phasing (e.g. playing a drum) (see Woytowicz et al., for a description of the five types of bilateral tasks [Citation12]). The rationale for not including these three types was that they are both less common and also more difficult to measure using the system. Furthermore, they were not found in the clinical assessment tests.
By design, our user needs assessment relied on the opinions of a limited number of patients and therapists, though the rigor of this process was increased by involving patients and carers who were currently undergoing their rehabilitation, and health professionals experienced in stroke rehabilitation. Furthermore, decisions of what to include in the matrix relied upon quasi-objective criteria applied through knowledge and experience. We did not evaluate the final set of tasks through, for example, a Delphi study or validation with a larger number of patients and therapists. The system has, however, been tested in a small feasibility study with six patients and three therapists, providing qualitative feedback on all aspects of the system including the tasks [Citation18].
The M-MARK system is of limited use for higher functioning stroke survivors because it cannot provide feedback on fine finger movement. A glove, embedded with sensors can measure fine gradations of movement and some can provide assistance [Citation19] but gloves have two disadvantages: help is often needed for donning and doffing and sensory input is reduced or altered by the glove. Indeed, our current system of 11 tasks is weighted towards lower functioning patients thus increasing its usability with these patients and those in the early recovery stages.
As with any technology used independently for training purposes, emphasis on tasks and accomplishment of tasks risks encouraging compensatory strategies (e.g., shoulder abduction instead of flexion; excessive pronation) or partial/total substitution by the non-paretic arm [Citation20,Citation21]. Patients may need to initially practice exercises rather than tasks to re-train (restore) joint movements that are impaired (e.g., wrist extension, elbow extension, shoulder flexion and lateral rotation, forearm supination). It may still be preferable, however, where possible, to re-train these movements in the context of a task and the system allows for this e.g., requiring forearm supination to pick up an object and using the task of “turning a card” to practice this movement. This limitation is mitigated by the visual feedback provided by the Avatar which highlights abnormal movement synergies and textual “quality” of movement feedback on common compensatory movements such as “try to keep your trunk still when reaching forwards.”
Future directions
The driver for this research was the development of a set of tasks for use with a specific wearable technology. The tasks identified through our systematic approach may, however, have wider application in conventional rehabilitation, the design of future technologies and as a self-assessment tool that patients could use remotely in their own home. The dramatic change in delivery of rehabilitation cause by the Covid-19 pandemic has created need for such assessment procedures.
Currently we are only able to process data from 11 tasks; future work will enable more tasks and progressions to be included in the system, so that tasks are even more likely to align with patients’ goals and interests, thereby increasing motivation. In addition, the system needs to be used in a larger clinical feasibility trial to provide more data on usability and acceptability.
Conclusion
Using a pre-determined task categorization matrix based on motor control and rehabilitation principles, and a person-centered design using interviews with patients, carers, and focus groups of health care professionals, a set of tasks was systematically created for use with M-MARK as a training and assessment system. A review of established assessment tests found no additional tasks or categories that should be included within the system.
Supplementary_data_tables_1_and_2.docx
Download MS Word (44.2 KB)Acknowledgements
We thank all the patients, their carers and the health professionals who participated in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011;377(9778):1693–1702.
- Morris JH, van Wijck F, Joice S, et al. Predicting health related quality of life 6 months after stroke: the role of anxiety and upper limb dysfunction. Disabil Rehabil. 2013;35(4):291–299.
- Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–S39.
- Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44(1):75–84.
- Schneider EJ, Lannin NA, Ada L, et al. Increasing the amount of usual rehabilitation improves activity after stroke: a systematic review. J Physiother. 2016;62(4):182–187.
- Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–e169.
- Dworzynski K, Ritchie G, Playford ED. Stroke rehabilitation: long-term rehabilitation after stroke. Clin Med. 2015;15(5):461–464.
- Lang CE, MacDonald JR, Gnip C. Counting repetitions: an observational study of outpatient therapy for people with hemiparesis post-stroke. J Neurol Phys Ther. 2007;31(1):3–10.
- Touillet A, Guesdon H, Bosser G, et al. Assessment of compliance with prescribed activity by hemiplegic stroke patients after an exercise programme and physical activity education. Ann Phys Rehabil Med. 2010;53(4):250–257-65.
- Burridge JH, Lee A, Turk R, et al. Telehealth, wearable sensors, and the internet: will they improve stroke outcomes through increased intensity of therapy, motivation, and adherence to rehabilitation programs? J Neurol Phys Ther. 2017;41:S32–S38.
- Meagher C, Franco E, Turk R, et al. New advances in mechanomyography sensor technology and signal processing: validity and intrarater reliability of recordings from muscle. J Rehabil Assist Technol Eng. 2020;7:2055668320916116.
- Woytowicz E, Whitall J, Westlake KP. Age-related changes in bilateral upper extremity coordination. Curr Geriatr Rep. 2016;5(3):191–199.
- Schmidt RA, Lee TD, Winstein CJ, et al. Motor control and learning: a behavioral emphasis. 6th ed. Champaign (IL): Human Kinetics; 2019.
- Kung PC, Lin CC, Ju MS. Neuro-rehabilitation robot-assisted assessments of synergy patterns of forearm, elbow and shoulder joints in chronic stroke patients. Clin Biomech. 2010;25(7):647–654.
- Woytowicz EJ, Rietschel JC, Goodman RN, et al. Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl-Meyer assessment of the upper extremity in chronic stroke. Arch Phys Med Rehabil. 2017;98(3):456–462.
- Aggarwal A, Kean E. Comparison of the folstein mini mental state examination (MMSE) to the montreal cognitive assessment (MoCA) as a cognitive screening tool in an inpatient rehabilitation setting. NM. 2010;01(02):39–42.
- Hochstenbach-Waelen A, Seelen HA. Embracing change: practical and theoretical considerations for successful implementation of technology assisting upper limb training in stroke. J Neuroeng Rehab. 2012;9(52):52.
- Turk R, Boyson A, Meagher C, et al. Clinical feasibility of a wearable sensor device to support upper limb rehabilitation post-stroke: mechanical muscle activity with real time kinematics (M-MARK). presented at: Second Congress on NeuroRehabilitation and Neural Repair, Maastricht, 2019.
- Radder B, Prange-Lasonder G, Kottink AIR, et al. Feasibility of a wearable soft-robotic glove to support impaired hand function in stroke patients. J Rehabil Med. 2018;50(7):598–606.
- Krakauer JW, Carmichael ST, Corbett D, et al. Getting neurorehabilitation right: what can be learned from animal models? Neurorehabil Neural Repair. 2012;26(8):923–931.
- Levin MF, Kleim JA, Wolf SL. What do motor "recovery" and "compensation" mean in patients following stroke? Neurorehabil Neural Repair. 2009;23(4):313–319.

