Abstract
Purpose
Goal setting is key to stroke rehabilitation, but access for people with aphasia is challenging. Based on the Goal setting and Action Planning (G-AP) framework, we developed an accessible goal setting resource (Access G-AP).
Methods
Access G-AP was designed using a three-phase, user-centred design process. Phase 1: Access G-AP Draft A was designed using evidence-based recommendations. Phase 2: Draft A was reviewed by stroke survivors with aphasia (focus groups 1&2) and rehabilitation staff (questionnaire). Phase 3: Suggested recommendations informed Access G-AP Draft B, which was further reviewed by stroke survivors with aphasia (focus group 3). The final version of Access G-AP was approved by stroke survivors with aphasia at a debrief meeting. Data were analysed using content analysis.
Results
Recommended design improvements included reducing text, adding bullet points, and diversifying images. Both participant groups highlighted that Access G-AP should be used collaboratively to support stroke survivor involvement. Staff recommended Access G-AP training and additional resources to support stroke survivors with severe aphasia.
Conclusions
Access G-AP was co-developed to support people with aphasia to access and engage in stroke rehabilitation goal setting. Further research is required to establish the feasibility of Access G-AP in clinical practice.
Evidence-based accessible formatting strategies and an iterative design process can inform the design of accessible goal setting resources.
Accessible goal setting materials should be relevant to stroke survivors with aphasia and responsive to their needs.
Rehabilitation staff require training and support to use accessible goal setting resources (like Access G-AP) with stroke survivors with aphasia, especially those with severe aphasia.
Evaluation of the feasibility of Access G-AP in clinical practice is now required.
IMPLICATIONS FOR REHABILITATION
Introduction
Collaborative and patient-centred goal setting is recommended as best practice in international stroke rehabilitation guidelines [Citation1–5]. It involves the development and pursuit of goals that are important to the stroke survivor via shared decision making between the patient, their family, and healthcare professionals [Citation1–5]. It is key to rehabilitation, which all stroke survivors have a right to access [Citation6,Citation7]. Stroke survivors with aphasia want information about the rehabilitation process and support to help them make decisions about their rehabilitation [Citation8]. A recent review of person-centred goal setting by Kang et al. [Citation9] also highlighted the importance of preparation to support patient engagement, for example through patient education. It is therefore important that stroke survivors, including those with aphasia, are supported to understand and participate in the goal setting process in order for it to be truly collaborative [Citation10,Citation11]. However, verbal or written information about the goal setting process, including a record of goals, is not routinely provided to stroke survivors [Citation12–15] or those with aphasia. In addition, the importance of goal setting and the steps involved are not always adequately communicated to stroke survivors [Citation14,Citation15]. This can leave stroke survivors feeling unclear about their role in goal setting and result in a clinician-led rather than patient-centred goal setting process [Citation16–18]. Stroke survivors’ goals and the rehabilitation they receive may therefore not reflect their priorities, hopes, and needs for recovery.
Accessibility is defined as “the provision of flexibility to accommodate each user’s needs and preferences” [Citation19]. There is a need for greater availability of accessible goal setting resources specifically for use by stroke survivors with aphasia and multidisciplinary rehabilitation teams in order to ensure that goal setting is collaborative and patient centred [Citation20]. Stroke survivors with aphasia prefer accessible information and resources [Citation21,Citation22]. Strategies to enhance the accessibility of visual and written information include, for example, large text, simple language, images, and colour [Citation21–23]. These can be used to develop resources supporting the goal setting process. However, Shrubsole et al. [Citation24] reported a lack of goal setting tools designed specifically for stroke survivors with aphasia in rehabilitation. Elston et al. [Citation25] recently developed an aphasia supplement to an Australian goal setting programme, and field testing suggested that it was useful in practice at two inpatient rehabilitation units. Given the range of rehabilitation contexts, services, and stroke survivor needs, accessible goal setting resources need to be flexible and responsive.
The Goal setting and Action Planning (G-AP) framework is a theory- and evidence-based method to support stroke survivors to consider, plan, and work towards their goals collaboratively with rehabilitation staff [Citation10,Citation11,Citation26,Citation27]. The G-AP framework consists of four stages repeated in a cyclical process:
Goal negotiation and goal setting.
Action planning and coping planning.
Action.
Appraisal, feedback, and decision making.
G-AP includes a stroke survivor held record (from here on referred to as the original G-AP record) to support goal negotiation, planning, and monitoring. In two process evaluations involving four community rehabilitation teams, 26 stroke survivors, and more than 40 multidisciplinary staff members, the original G-AP record was found to be useful as a way to record goals and plans and review progress [Citation11,Citation26,Citation27]. However, the record was not fully accessible for stroke survivors with aphasia, which staff noted as a barrier to implementing G-AP in practice [Citation11,Citation27].
To help address the need for greater availability of accessible goal setting resources, we sought to (i) develop the original G-AP stroke survivor held record into an accessible resource (Access G-AP) and (ii) identify and address barriers and facilitators to the resource’s accessibility, usability, and usefulness from the perspectives of stroke survivors with aphasia and rehabilitation staff.
Methods
Study design
We developed and reviewed Access G-AP in a qualitative and iterative three-phase user-centred design process with stroke survivors with aphasia and rehabilitation staff (). User-centred design directly involves target users in the design process to help establish the acceptability and usability of a resource [Citation28–31]. The process consists of three stages: (i) developing an understanding of the users; (ii) product design; and (iii) evaluation [Citation32]. This study focused on stages (ii) and (iii), as sufficient preliminary understanding of the users had already been developed via the literature [Citation20]. User-centred design supports iterative, stakeholder-informed development and was thus considered a suitable approach for this study.
Figure 1. Access G-AP design process.
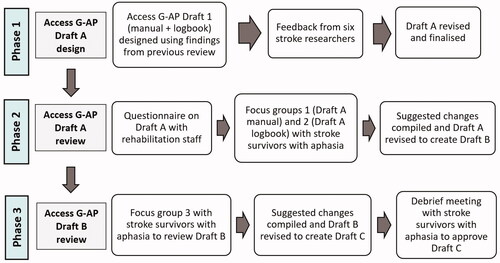
The three phases of this study () included: designing Access G-AP Draft A (Phase 1); reviewing Access G-AP Draft A with stroke survivors with aphasia and rehabilitation staff and re-designing Access G-AP based on this feedback (Phase 2); and reviewing, re-designing, and approving Access G-AP Draft B with stroke survivors with aphasia (Phase 3). Phases 2 and 3 included stages (ii) and (iii) of user-centred design, with each phase involving both (re)design and evaluation. The methods utilised in this study included three focus groups with stroke survivors with aphasia, using participatory techniques to support communication [Citation33], and a semi-structured questionnaire with rehabilitation staff, completed electronically (Supplementary file 1).
Focus groups structured around a small number of questions and prompts were considered most suitable for stroke survivor feedback, as they supported discussion and agreement on resource changes and allowed the stroke survivors to hold the decision-making power. Focus groups also facilitated peer support and the use of aphasia-friendly participatory techniques to support stroke survivors with aphasia to express their opinions. A semi-structured email questionnaire was used for rehabilitation staff feedback to support healthcare professionals to contribute their views on Access G-AP with flexibility and minimal time commitment. The questionnaire was also designed to provide feedback in a format that would be straightforward to share with the stroke survivor focus group and allow them to have the final say on the resource design.
Patient and public involvement
To enhance study quality, we utilised Patient and Public Involvement (PPI). PPI enhances the quality of research and implementation of services, helps to address population concerns, and promotes shared decision making [Citation34]. It has also been used successfully with people with aphasia to enhance equality and collaboration in health research [Citation35]. Stroke survivors with aphasia external to the study reviewed and approved the accessible information sheets and consent forms. The rehabilitation staff questionnaire was piloted by four rehabilitation staff and focus group methods piloted with two stroke survivors with aphasia all external to the study. A summary of the PPI utilised in the study, using the Guidance for Reporting Involvement of Patient and the Public Short Form [Citation36], is available (Supplementary file 2).
Participants and recruitment
Participants included: (i) adult stroke survivors diagnosed with aphasia and able to consent and participate in focus groups without carer or guardian assent; (ii) healthcare professionals in any clinical therapy role working directly with patients (e.g., allied health professionals, nurses), with at least two years of experience working with stroke survivors with aphasia in a community rehabilitation setting, and active in that role in the previous 12 months.
Stroke survivors with aphasia were recruited via a peer-led community aphasia support group in England. The group runs weekly drop-in sessions and regular classes and events, and members include people with aphasia and their carers. Members were invited to participate at a short information presentation at a weekly drop-in session and were provided with accessible information and consent forms. Demographic information including age, sex, and time since stroke was recorded by the researcher [EB] at the time of recruitment. Aphasia severity was assessed via participant self-report of communication difficulties and researcher observation of their communication. Focus groups with stroke survivors with aphasia took place at the support group’s venue, in a room adjacent to their usual drop-in session space. Focus groups were held alongside the drop-in sessions to minimise time and travel commitments for participants. This meant that participants did not need to change their normal routine, and there was no additional demand on caregivers to provide extra transport to participants.
Rehabilitation staff were recruited via the Scottish Stroke Allied Health Professionals Forum (SSAHPF), a Chest Heart & Stroke Scotland network. Forum members include allied health professionals and allied health professional support workers in Scotland with an interest in stroke, including speech and language therapists (SLTs), physiotherapists, occupational therapists, and rehabilitation assistants. Members were invited to take part via the forum’s mailing list. Rehabilitation staff returned the questionnaire via email. Ethical approval for the study was obtained from Glasgow Caledonian University Health and Life Sciences Ethics Committee in March 2019 [HLS/NCH/18/019; HLS/NCH/18/026].
Procedure
Feedback topics
We sought feedback from stroke survivors with aphasia and rehabilitation staff on the accessibility, usability, and usefulness of Access G-AP resource. Accessibility was a central concern, as people with aphasia may experience challenges in accessing written information [Citation20,Citation37]. Accessibility consisted of four design categories: text, colour, layout, and images [Citation20]. We also sought feedback on usability and usefulness, as they are emphasised as important for intervention uptake in the Medical Research Council (MRC) complex intervention development guidance [Citation38]. Usability related to how easily the resource could be used by staff in practice, and usefulness captured staff opinions on the resource’s value and whether they would be willing to use it.
Phase 1: Access G-AP draft a design
In Phase 1, an initial Access G-AP Draft A was designed by EB based on findings from a previous review of communication and goal setting accessibility [Citation20] and input from six stroke rehabilitation researchers [LS, LW, MB and others external to the project]. We based Access G-AP Draft A on the original G-AP stroke survivor held record due to favourable review in previous evaluations [Citation11,Citation26,Citation27]. The original G-AP record included a brief explanation of the G-AP process and pages to generate and record ideas, goals, action plans, and progress. To create Access G-AP Draft A, the original G-AP record document was divided into two documents: (i) a stroke survivor manual to explain the goal setting process and (ii) a logbook to collaboratively generate goals and record goals and action plans. An appointments page was also added to the logbook to support stroke survivors with aphasia to manage appointments with multiple staff members. The separate manual provided more detailed explanations of the process without creating a large single document that could be overwhelming. The Access G-AP manual fulfilled the role of preparation, an important part of goal setting [Citation9], as it could be issued and explained to stroke survivors before starting goal planning sessions, thus giving them time to think about, or discuss with family and friends, what they want to work towards [Citation39].
People with aphasia have reported preferring more realistic graphic-style images or photos to line drawings or cartoons [Citation21,Citation40,Citation41]. We therefore used a library of graphic images hosted by the Speakeasy aphasia group. The images relate to research concepts, stroke recovery, and rehabilitation, were co-designed with people with aphasia, and include people with a range of ages, ethnicities, and disabilities [Citation42].
Phase 2: Review of access G-AP draft A
In Phase 2, Access G-AP Draft A was reviewed via two focus groups with five stroke survivors with aphasia and written feedback (questionnaire) from seven rehabilitation staff. The first author [EB], a researcher with speech and language therapy training, facilitated all focus groups. The third author [RMcM], a researcher and speech and language therapist trained and experienced in participatory techniques and group facilitation, co-facilitated the first session with EB. EB completed written reflections after each focus group detailing what was successful and what needed modifying at the next session. All focus groups were video and audio recorded and transcribed and lasted approximately two hours.
Focus group 1 (manual)
Stroke survivors with aphasia discussed the Access G-AP Draft A manual, including its accessibility and any changes to improve it. Commentary charts, which provided a visual approach for participants to express and organise their thoughts [Citation33,Citation43,Citation44], were used to support co-generation (). They have successfully been used with people with aphasia in Participatory Learning and Action (PLA) research. A separate chart was used for each manual page and consisted of a flip-chart page divided into three columns: positive, neutral, and negative.
Figure 2. Example commentary chart used in Phase 2.
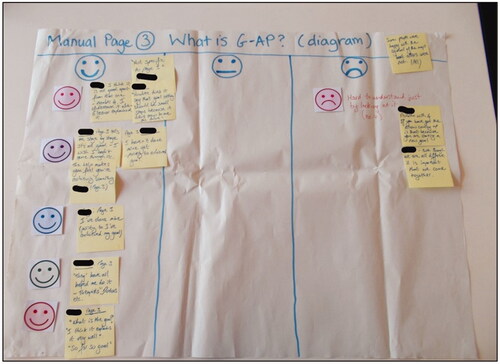
Participants with aphasia were shown and read each manual page in turn by the researcher [EB] and were asked, “What do you think of this page?.” Each participant selected coloured cards depicting happy, neutral, and sad faces to represent their opinion. Cards were placed in the relevant commentary chart column. Participants were invited to discuss their opinions of the text, pictures, colour, and layout of a page and what they thought should be improved. Categories were not restrictive, and participants with aphasia could discuss any aspects of the design or the resource more generally. A formal question guide was not used; rather, the question, “What do you think of this page?” served as an invitation to comment on each page, with further prompts to consider each design element if required (e.g., “What do you think about the pictures?”). This format was developed by the research team [EB, LS, LW, MB] and tested in the pilot session [EB] in order to maintain an open and minimally restrictive discussion. Comments were scribed by the facilitator and co-facilitator and attached to the chart. Once completed, participants discussed whether the chart made sense and represented their views and whether anything further should be added.
Focus group 2 (logbook)
Participants with aphasia reviewed the Access G-AP Draft A logbook, following the same procedure described above for focus group 1. Participants also discussed the usability and usefulness of the manual and logbook, recorded on separate commentary charts.
Rehabilitation staff questionnaire
Our semi-structured questionnaire aimed to collect feedback from rehabilitation staff on Access G-AP Draft A (Supplementary file 1). Staff who agreed to take part received the Access G-AP Draft A manual and logbook and questionnaire via email. Following review of Access G-AP Draft A, rehabilitation staff completed the questionnaire, which included unrestricted space for comments. Questionnaires were returned anonymously. Staff were asked to comment on the accessibility, usability, and usefulness of the draft resource in clinical practice. Staff were invited to suggest changes or additions that could improve the resource for both stroke survivors with aphasia and rehabilitation staff. These changes were compiled with those suggested by stroke survivors with aphasia in focus groups 1 and 2 and applied to created Access G-AP Draft B.
Phase 3: Review of access G-AP draft B
In Phase 3, the stroke survivors with aphasia who participated in Phase 2 reviewed Access G-AP Draft B in a third focus group. Based on feedback from the stroke survivors with aphasia following focus group 2, commentary charts were not used in this focus group. Stroke survivors with aphasia were again asked, “What do you think of this page?.” Their comments were then scribed onto sticky notes and placed onto the resource pages. After the focus group, EB transferred the comments onto a commentary chart to assist analysis. Changes suggested at this focus group were applied to create the final Access G-AP (Draft C). Stroke survivors with aphasia participated in a final debrief meeting to review and approve Draft C and reflect on their study participation experiences.
Decision making process
Every attempt was made to implement changes suggested by stroke survivors with aphasia and rehabilitation staff. We used the focus group format to allow differences of opinion to be resolved and to optimise stroke survivor ownership of the decision-making process. If a compromise or resolution was not possible during the focus groups, this was noted as a difference of opinion, and no change was made. If a suggested change from stroke survivors with aphasia was not possible (e.g., changing essential components of the G-AP process), no change was made, and it was discussed at the next focus group. All changes suggested by rehabilitation staff and changes made based on previous stroke survivor suggestions were discussed with stroke survivors with aphasia in the Phase 3 focus group. However, if a rehabilitation staff suggested change conflicted with a stroke survivor preference, the preference of the stroke survivor was chosen. This process allowed the stroke survivors with aphasia to agree or disagree with all applied changes and suggest further adjustments, giving them final say on the resource design.
Data analysis
EB performed qualitative content analysis on all collated data from stroke survivors with aphasia and rehabilitation staff. Codes, sub-categories, categories, and themes were determined by EB via the procedures described by Graneheim and Lundman [Citation45], which provide a systematic approach to categorising qualitative data. The data source was the pooled focus group discussion data and staff questionnaire comments, including commentary charts and transcripts. A meaning unit was a participant comment relating to a single topic. To maintain context, utterances and responses were treated as whole comments where possible. If an utterance or written response concerned multiple unrelated topics, it was split into multiple comments according to the topics.
Analysis was conducted in three stages:
Data were divided by EB into design data or other data (not design-related) content areas, which later formed themes.
EB deductively analysed design data, collected via pre-determined categories (accessible and inaccessible, or positive and negative) and sub-categories (text, layout, colour, pictures) used to facilitate data generation. Themes were generated to reflect categories and sub-categories.
EB inductively analysed all other data. Following repeated reading of the data, data were condensed and abstracted. Similar meaning units were highlighted and coded to create sub-categories. These were then revised, combined, and categories identified. The two areas of “design” and “other” were formed into themes based on the categories.
Throughout the process, we referred to the content analysis trustworthiness checklist provided by Elo et al. [Citation46]. This supported fulfilment of the four elements of trustworthiness as described by Lincoln and Guba [Citation47]: credibility, transferability, dependability, and confirmability. To support transferability, we have endeavoured to provide a detailed description of the context of data collection. To improve credibility, decisions about themes, categories, and sub-categories were peer checked by a second researcher [LW] and discussed, and participant data and analysis were checked again to ensure appropriate interpretations [EB, LW]. To support dependability and confirmability, an audit trail was maintained, ensuring an accurate record of data collection, collation, and analysis, and the first author [EB] completed written reflections after each focus group [Citation48].
Results
Participants
Stroke survivors with aphasia
Five stroke survivors with aphasia, referred to from hereon in by pseudonyms as Sarah (SS1), John (SS2), Naomi (SS3), Ian (SS4), and Paula (SS5) were recruited. Four were retired, and the other aimed to return to work. Participants ranged in age from 27 to 88, and time since stroke ranged from five months to 16 years. Most had “mild” aphasia and experienced communication challenges across word finding, comprehension, writing, reading, and fluency. One stroke survivor’s aphasia was more moderate and required more support to take part in the focus group, such as paraphrasing, repeating, and simplifying questions and discussion points and using gestures (e.g., thumbs up).
Rehabilitation staff
Participants included seven rehabilitation staff (one physiotherapist and six SLTs) based in Scotland. Most reported >12 years’ experience working with stroke survivors with aphasia in rehabilitation, while one SLT had 1–5 years’ experience.
Summary of changes
Access G-AP draft A
Participants with aphasia considered the manual text to be generally clear, with some improvements such as clarifying and foregrounding the process of taking small steps to achieve goals. Rehabilitation staff feedback was also largely positive, and the short, simple sentences were reported to facilitate accessibility. Both stroke survivors with aphasia and rehabilitation staff suggested that the text should be reduced and presented as bullet points. The amount of bold text was also reduced on the recommendation of rehabilitation staff, as they suggested that it was used excessively and obscured the key messages. Other stroke survivor adjustments included, for example, changing a picture of the rehabilitation team to include the patient. Based on rehabilitation staff feedback, pictures were also updated to reflect a wider range of ethnicities. One rehabilitation staff participant did not like the style of the pictures (coloured graphics), so examples of alternative picture styles (line drawings and cartoons) were discussed with stroke survivors with aphasia at the next focus group (see Access G-AP Draft B below).
A diagram was used to illustrate the G-AP process, but participants with aphasia found it difficult to follow without a verbal explanation, and rehabilitation staff similarly found it too complex. We simplified the diagram and noted that staff users should provide an explanation to accompany the diagram. An option was added to display each of the G-AP stages as cards to reduce cognitive load by placing and discussing one at a time. On the recommendation of a staff participant, a worked example of the G-AP process was also added in Draft B and included possible goals and action plans. Few changes were made to the logbook. Although the stroke survivors with aphasia found the logbook layout straightforward, rehabilitation staff thought that having multiple goals and action plans on each page could be confusing. To address this, we made alternative goal and action plan pages with only one goal or action plan per page, to allow stroke survivors with aphasia to choose their ideal format. Rehabilitation staff also suggested including a visual scale to rate confidence in completing action plans, which was included in Draft B.
Access G-AP draft B
Stroke survivors with aphasia agreed with most changes made based on their own and rehabilitation staff suggestions. Further minor changes were suggested to clarify parts of the text and improve the comprehensibility of images. The rehabilitation staff suggestion of diversifying pictures was received well by the stroke survivors, who suggested additional improvements such as including more young people. Stroke survivors liked the presentation of individual goals and action plans on separate pages, but suggested keeping the original format (multiple goals presented on a page) to allow people to choose. Stroke survivors with aphasia were shown alternative picture styles based on rehabilitation staff feedback but preferred the more realistic graphics used in Access G-AP Drafts 1 and 2.
Access G-AP draft C
Stroke survivors with aphasia approved Draft C as the final version (Supplementary file 3). Draft C included:
A manual explaining the G-AP process, including a worked example of G-AP and cards displaying each stage of the process;
A logbook including (a) sections to generate and record goals, action plans, and progress, (b) a visual confidence rating scale, and (c) an appointments page.
Content analysis
This section presents the qualitative content analysis results gleaned from the focus group discussions and questionnaires. Two overall themes were developed from the “design” and “other” data: design impacts on accessibility and getting the resource in place and making it work ().
Table 1. Summary of themes, categories, and sub-categories.
Design impacts on accessibility
Design impacts on accessibility concerned the accessibility of the content and format of the Access G-AP drafts, including “accessible design features” and “inaccessible design features.” Accessible text features included, for example, simple text, short sentences, and bolding. In contrast, inaccessible text features included excessive or complicated text and excessive use of bold, as this could reduce the clarity of key messages. Bullet points were also more accessible than continuous text, which increased cognitive load:
For me, um like bullet points, that’s fine … my brain switches off … theory work is a no-go, like no, like sleep um… my brain is go to sleep. (Naomi, stroke survivor)
Pictures were more accessible when they were realistic and had a clear meaning, and inaccessible pictures were unfamiliar symbols or images with a vague or abstract meaning. However, pictures did not need to be completely literal to be accessible, as long as the meaning was appropriate to the context with supporting text. One rehabilitation staff participant suggested that the goal-related images were too abstract and should be more literal, such as a goal post to represent goals. However, the map and compass images used in Access G-AP to depict the goal setting process were received well by stroke survivors with aphasia, who related to the analogy of a journey:
I think it tells a complete story … it tells people sitting around talking about it, compass and a map. It will tell you how to get there, wherever you want to be. (Ian, stroke survivor)
Accessible layout features included the use of boxes to separate text and appropriately ordered information. For example, stroke survivors with aphasia wanted more explanation at the start of the manual about goals including “small steps” to create a foundation for understanding the goal setting process. Inaccessible layout features included the need to cross-reference information (e.g., with goals and action plans recorded in different sections of the logbook) and complicated diagrams. For example, a diagram was used to illustrate the G-AP process, but stroke survivors with aphasia found it difficult to follow without a verbal explanation, and rehabilitation staff similarly felt it would be too complicated. It was therefore simplified and noted that staff would need to provide an explanation to accompany the diagram. The use of colour coding the differentiate sections also facilitated accessibility.
Getting the resource in place and making it work
Getting the resource in place and making it work concerned considerations for using the Access G-AP resource in practice and included “support for and from staff,” “person-centredness,” and “empowerment.”
“Support for and from staff” concerned possible barriers and facilitators to using Access G-AP. Rehabilitation staff reported that training and additional support would be needed for staff using Access G-AP, including both goal setting and communication training, particularly for non-SLT members of the multidisciplinary team. Staff suggested including additional support materials to support stroke survivors with severe aphasia to engage with the G-AP process, such as picture cards and examples of goals and action plans. Stroke survivors with aphasia also emphasised the need for staff to support them to understand and use Access G-AP, as not all could read and write, and some aspects such as the G-AP process diagram needed explanation. Sarah, a stroke survivor with aphasia, described a negative experience in her own rehabilitation of being given a goal worksheet without support to understand it:
… my nurse gave me a sheet of paper, and it’s like balloons, and to fill in the balloons, I my brain was just muddled up, and I didn’t know what to do with it, so when she came back, and I said I haven’t filled it up, because I couldn’t get the understanding of it. (Sarah, stroke survivor)
Naomi also emphasised the importance of rehabilitation staff taking the time to properly explain resources and information:
Explain, pictures and reasons before they leave, yeah, rather than um “Here is like an exam- example like here is a logbook and uh I’m not gonna explain it, and um I’ll see you next week” [laughs] … yeah, explain it, you know and I what do I do with it, do I look at it? Or… come on… reason! (Naomi, stroke survivor)
Staff highlighted the positives and negatives of the logbook in terms of record keeping. Both staff and stroke survivors with aphasia agreed that being able to record and plan goals in a concrete, visual way would be useful. However, one staff participant highlighted that a paper resource could be problematic and reduce usability for staff, as it would require duplication of notes onto the health service’s electronic records system.
“Person-centredness” addressed the relevance and adaptability of Access G-AP. Stroke survivors with aphasia and staff felt that “relevant content” was important. Rehabilitation staff suggested, and stroke survivors with aphasia agreed, that pictures should reflect diverse populations (e.g., different ages and ethnicities):
Include people with different ages … a young person might think “where’s me?” (Naomi, stroke survivor)
Stroke survivors with aphasia also appreciated that the manual included content that resonated with their own experiences, such as taking small steps to reach goals and making a plan with the rehabilitation team. Tailoring to individual needs meant ensuring that Access G-AP would be sufficiently flexible to adapt to different physical and communication needs. This may include a manual version with accessible text but no pictures and ensuring the logbook could be used by stroke survivors with a hemiparesis (e.g., storing it in a ring binder with a lever instead of plastic pockets).
“Empowerment” concerned the importance of making the goal setting process and resource content encouraging and shared by stroke survivors with aphasia and rehabilitation staff. Stroke survivors with aphasia discussed the value of positivity. They felt it was important to maintain a positive attitude to their recovery and for the goal setting process and resource to support optimism.
I’m positive … because … you start from where you are when you’re ill, and then you gradually make your way to your goal of trying to get to your goal, and you talk about it which is good, what we’re doing or your therapist does or nurse or counsellor who are there to help you. (Sarah, stroke survivor)
Stroke survivors with aphasia particularly liked pictures depicting rehabilitation staff with stroke survivors, which they interpreted as staff encouraging the stroke survivor to maintain hope and keep striving for their goals:
The therapist is talking to the stroke survivor and letting them know there’s a way out. (Naomi, stroke survivor)
Stroke survivors with aphasia having ownership of the Access G-AP documents was also valued by staff, who thought that this aspect of the resource would facilitate shared decision making and support stroke survivors to “own” their goals.
Discussion
We developed an accessible goal setting and action planning resource (Access G-AP) using a multi-phase, user-centred design process. Barriers and facilitators to its accessibility, usability, and usefulness were identified and addressed with stroke survivors with aphasia and rehabilitation staff. Findings indicated that accessible goal setting resources should have a positive tone, be flexible to adapt to individual needs, and support stroke survivors with aphasia to have ownership of the goal setting process. Key issues for Access G-AP implementation included the need for staff training and support to use Access G-AP with stroke survivors with aphasia, a person-centred approach, and supporting stroke survivors with aphasia to be empowered in the goal setting process.
Building flexibility into accessible goal setting resources
The accessible design features were central to the perceived usability of Access G-AP, and stroke survivors with aphasia and rehabilitation staff preferred simple and clear information. This is supported by previous studies advocating accessible text [Citation21,Citation22,Citation41]. In questionnaire [Citation21] and interview [Citation22] studies with people with aphasia, Rose et al. explored their preferences for printed education materials, which included accessible features such as large text, 1.5 line spacing, and graphics [Citation21,Citation22]. Our participants also found bolding useful, but rehabilitation staff emphasised that it should be judicious and used only for essential key words.
Stroke survivors with aphasia in our study generally preferred coloured graphics to line drawings or cartoons. This is supported by findings from Rose et al. in their questionnaire study [Citation21] and a further study in which people with aphasia completed a reading comprehension task and a graphic preference survey [Citation40]. However, both studies also found that individual preferences varied, and some participants preferred photographs [Citation21,Citation40]. In our study, one stroke survivor with aphasia did not want any pictures in Access G-AP. This suggests that accessibility is not “one size fits all” and that flexibility is essential to support person-centred accessible goal setting practice. Based on our findings, flexibility in the context of goal setting can include adapting pictures or formats to suit individual stroke survivors and rehabilitation teams, using only pen and paper to plan goals when required, and using communication support tools for people with severe aphasia.
Rehabilitation staff and stroke survivors with aphasia need support to use accessible goal setting resources
Rehabilitation staff highlighted that training in communication support strategies and use of the G-AP framework would be required to support successful use of Access G-AP in practice. Even without the presence of aphasia, goal setting with stroke survivors has been reported by healthcare professionals as challenging [Citation17]. Aphasia presents additional challenges that necessitate additional staff training and support, including knowing how to develop and use accessible information resources and how to use a range of conversations strategies with different patients [Citation49–53]. The goal setting and action planning process is also likely to involve discussions about complex or sensitive topics, such as hopes for the future and managing setbacks and disappointment [Citation26]. Rehabilitation staff therefore need additional skillsets to support communication needs during these complex goal-related discussions, such as foundational counselling strategies for holding difficult conversations about goal non-attainment and prognosis. The New Zealand Stroke Rehabilitation Strategy [Citation5], for example, recommends that staff receive training in providing emotional and psychological support. SLTs have also reported valuing specialist training to support the psychosocial needs of people with aphasia, for example, by exploring difficult emotions and helping patients and families to understand the impact of aphasia [Citation54].
Stroke survivors with aphasia also emphasised the need for support from rehabilitation staff to understand and use Access G-AP. Some had been frustrated by being given rehabilitation materials without support or explanation. A recent narrative review of communication accessibility in the context of goal setting found that stroke survivors with aphasia benefit from a combination of verbal and written or visual communication support [Citation20], for example, accessible printed information accompanied by a simple verbal explanation. Therefore, even accessible goal setting resources, like Access G-AP, cannot stand alone and can only be fully accessible when delivered with support from rehabilitation staff.
The importance of positivity in goal setting resources
Stroke survivors with aphasia discussed the importance of the goal setting information itself reflecting hope and interpreted pictures as having a positive or negative message. In their development and evaluation of an aphasia goal setting package using goal menus, Elston et al. [Citation25] also found that some stroke survivors with aphasia who informed resource development wanted the pictures to be positive. Bright et al. [Citation55] interviewed four people with aphasia and found that hope for desired outcomes or goals helped provide direction and purpose, motivating them to engage in their rehabilitation. These findings have important implications for the way goal setting information is presented and how rehabilitation staff discuss progress, as a lack of encouraging messages in goal setting resources and conversations could potentially have a negative impact on willingness to engage in rehabilitation and emotional wellbeing.
Strengths and limitations
Our iterative design process supported meaningful contributions from stroke survivors with aphasia and rehabilitation staff and allowed stroke survivors with aphasia to approve or disagree with the implementation of their suggestions. The process created a stroke rehabilitation goal setting resource that was acceptable to the participating stroke survivors with aphasia and rehabilitation staff, who considered that it would be useful in practice.
Although we invited multidisciplinary rehabilitation staff involved in goal setting to participate in this study, most were highly experienced SLTs. Given that Access G-AP is designed for use by multidisciplinary teams, broader multidisciplinary representation may have provided different insights. Rehabilitation staff contributed written feedback on one version of Access G-AP. Thus, we could not clarify their comments, request elaboration, or discuss and resolve differences of opinion amongst staff. All our participants with aphasia were drawn from a region in England with high socio-economic levels. Most members were white, spoke English as their first language, were professional prior to their stroke or retirement, and had access to support and resources after their stroke. Thus, our findings may not reflect the experiences of people with aphasia with poor healthcare access, from low socio-economic and minority backgrounds, or those lacking access to support groups. While we aimed to recruit stroke survivors of different ages and with a range of communication needs, this was not possible as many members could not commit to the data collection schedule. We also lacked the views of people with severe aphasia, whose accessibility needs may have been greater or different to those experienced by our participant group. Finally, only one participant was still directly engaged with NHS rehabilitation services, reducing their ability to relate to Access G-AP as a “real” and practical resource.
Implications
The accessibility of goal setting resources depends on support from rehabilitation staff using tailored communication support. Resources like Access G-AP can be useful anchors to support goal setting, but the way rehabilitation staff support stroke survivors with aphasia should be informed by individual stroke survivors’ communication needs and personal context and an understanding of how to apply communication strategies.
Goal setting resources should be adaptable to meet the needs of different stroke survivors and contexts. The need for tailoring to the person and their communication abilities has implications for the practicality of Access G-AP in clinical practice. Rehabilitation staff may see stroke survivors with aphasia in the community, an inpatient or residential facility, or an outpatient facility, which could have their own (or no) goal setting practices and different time and resource limitations. Teams will likely need extra time to tailor the resource and strategies and provide additional support to stroke survivors with severe aphasia. Teams may also need to rely on an SLT being available to provide support or initial training. This reflects broader implementation issues reflecting integration with service infrastructure and various rehabilitation team contexts.
The families of stroke survivors with aphasia can also play a key role in the goal setting process [Citation56], and “family-centred” care is advocated in stroke and aphasia rehabilitation, provided that it is the preference of the stroke survivor and in their interest [Citation1,Citation57–60]. Thus, goal setting resources such as Access G-AP must be flexible enough to support family involvement throughout the process. The Access G-AP manual describes the goal setting process as a collaborative effort between the stroke survivor, their family, and the rehabilitation team. Provision of the manual before goal setting formally begins is intended to allow time for stroke survivors with aphasia and their families to talk about what is important to them and what they want to work towards. The G-AP process in itself is also flexible, allowing for the development of goals that relate to the whole family unit alongside goals for the individual stroke survivor. However, the degree of flexibility of Access G-AP in practice will depend on the rehabilitation staff. As rehabilitation staff have reported that involving families in goal setting with stroke survivors with aphasia can be challenging [Citation15], it is important that family involvement is incorporated into future Access G-AP training.
Rehabilitation staff in this study reported that they would need training (in supported communication and goal setting) to effectively deliver Access G-AP. Both training and ongoing support are important facilitators of practice change [Citation20]. Although evidence-based communication partner training programmes such as Supported Conversation for Adults with Aphasia are available and could inform accessible goal setting training, such programmes can involve a high cost and may not be feasible for rehabilitation teams. There is therefore a need for specific, freely available training that can be used to support goal setting with stroke survivors with aphasia. Work to develop this online training to support use of Access G-AP in practice is currently underway.
Our findings confirm the value of involving service users in healthcare resource design, including stroke survivors with communication challenges and healthcare professionals. Future research should focus on the feasibility, piloting, and evaluation of the clinical and costs effectiveness of Access G-AP and accompanying training in community rehabilitation settings. Training would benefit from involving stroke survivors with aphasia familiar with Access G-AP as trainers alongside rehabilitation staff trainers to harness their lived experience and expertise. It would be useful to involve a stakeholder advisory group, as this could further optimise the acceptability and relevance of interventions. Targeted, purposeful recruitment may also help to ensure representation of the full multidisciplinary team in future studies.
Conclusions
We developed and produced an Access G-AP resource that provides a foundation for supporting accessible goal setting and was acceptable to participating stroke survivors with aphasia and rehabilitation staff. Support from rehabilitation staff is crucial for stroke survivors with aphasia to fully participate in goal setting, which is a dynamic and relationship-based process involving collaboration between staff and stroke survivors with aphasia. Person-centredness and empowerment are also key considerations for the implementation of accessible goal setting interventions like Access G-AP. Resources should be relevant and adaptable, and rehabilitation staff need support to understand the role of positivity and hope and to facilitate stroke survivor ownership of goal setting.
Supplementary_file_3_Access_G-AP_Draft_C.docx
Download MS Word (2.8 MB)Supplementary_file_2_GRIPP2-SF.docx
Download MS Word (15.8 KB)Supplementary_file_1_Questionnaire_completed_by_rehabilitation_staff.docx
Download MS Word (16.7 KB)Acknowledgements
We would like to thank the stroke survivors with aphasia and rehabilitation staff who generously gave their time to participate in the study and share their perspectives.
Disclosure statement
EB was supported by a Glasgow Caledonian University PhD studentship and Foundation for Women Graduates Foundation grants. LS is supported by a Stroke Association Clinical Lectureship award (TSA LECT 2016/02). The Nursing, Midwifery, and Allied Health Professions Research Unit and MCB are supported by the Chief Scientist Office, Scottish Government Health, and Social Care Directorate, UK. The views expressed here are those of the authors and not necessarily those of the funders.
References
- Irish Heart Foundation: Council for Stroke. National Clinical Guidelines and Recommendations for the Care of People with Stroke and Transient Ischemic Attack (revised version) [Internet]. 2010. Available from: http://irishheart.ie/wp-content/uploads/2017/04/guidelines.pdf.
- Stroke Foundation. Clinical Guidelines for Stroke Management [Internet]. 2017. Available from: https://files.magicapp.org/guideline/a0e5b148-3f2b-46c5-a68e-ab8e678e6f1b/published_guideline_3973-5_4.pdf.
- Royal College of Physicians. National clinical guideline for stroke. 2016.
- Heart and Stroke Foundation. Canadian stroke best practice recommendations, 6th ed. 2018.
- Green G, Maddula M. New Zealand Stroke Rehabilitation: A strategy [Internet] 2018. Available from: https://strokenetwork.org.nz/new-zealand-stroke-rehabilitation–a-strategy.
- World Health Organisation. World report on disability. Lancet. 2011;377(9782):1977.
- Right to R. Community rehabilitation: Live well for longer; 2019.
- Worrall L, Sherratt S, Rogers P, et al. What people with aphasia want: Their goals according to the ICF. Aphasiology. 2011;25(3):309–322.
- Kang E, Kim MY, Lipsey KL, et al. Person-centered goal setting: a systematic review of intervention components and level of active engagement in rehabilitation goal-setting interventions. Arch Phys Med Rehabil. 2021;130(1):121–130.e3.
- Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: Development of a theoretically informed practice framework. Clin Rehabil. 2011;25(5):468–482.
- Scobbie L, McLean D, Dixon D, et al. Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Serv Res. 2013;13:190.
- Rosewilliam S, Roskell C, Pandyan A. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil. 2011;25(6):501–514.
- Plant S, Tyson SF. A multicentre study of how goal-setting is practised during inpatient stroke rehabilitation. Clin Rehabil. 2018;32(2):263–272.
- Scobbie L, Duncan EA, Brady MC, et al. Goal setting practice in services delivering community-based stroke rehabilitation: a United Kingdom (UK) wide survey. Disabil Rehabil. 2015;37(14):1291–1298.
- Brown SE, Scobbie L, Worrall L, et al. A multinational online survey of the goal setting practice of rehabilitation staff with stroke survivors with aphasia. Aphasiology. 2022;2022:1–25.
- Leach E, Cornwell P, Fleming J, et al. Patient centered goal-setting in a subacute rehabilitation setting. Disabil Rehabil. 2010;32(2):159–172.
- Plant S, Tyson S, Kirk S, et al. What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clin Rehabil. 2016;30(9):921–930.
- Sugavanam T, Mead G, Bulley C, et al. The effects and experiences of goal setting in stroke rehabilitation – a systematic review. Disabil Rehabil. 2013;35(3):177–190.
- United Nations. Accessibility and development: Mainstreaming disability in the post-2015 development agendaitle [Internet]. 2015. Available from: http://www.un.org/disabilities/documents/accessibility_and_development.pdf.
- Brown SE, Brady MC, Worrall L, et al. A narrative review of communication accessibility for people with aphasia and implications for multi-disciplinary goal setting after stroke. Aphasiology. 2021;35(1):1–32.
- Rose T, Worrall LE, Hickson LM, et al. Guiding principles for printed education materials: design preferences of people with aphasia. Int J Speech Lang Pathol. 2012;14(1):11–23.
- Rose T, Worrall LE, Hickson LM, et al. Aphasia friendly written health information: content and design characteristics. Int J Speech Lang Pathol. 2011;13(4):335–347.
- Howe TJ, Worrall LE, Hickson LMH. Interviews with people with aphasia: environmental factors that influence their community participation. Aphasiology. 2008;22(10):1092–1029.
- Shrubsole K, Worrall L, Power E, et al. Recommendations for post-stroke aphasia rehabilitation: an updated systematic review and evaluation of clinical practice guidelines. Aphasiology. 2017;31(1):1–24.
- Elston A, Barnden R, Hersh D, et al. Developing person-centred goal setting resources with and for people with aphasia: a multi-phase qualitative study. Aphasiology. 2021;2021:1–20.
- Scobbie L, Brady MC, Duncan EA, et al. Goal attainment, adjustment and disengagement in the first year after stroke: a qualitative study. Neuropsychol Rehabil. 2020;2020:1–19.
- Scobbie L, Duncan EAS, Brady MC, et al. Facilitators and “deal breakers”: a mixed methods study investigating implementation of the goal setting and action planning (G-AP) framework in community rehabilitation teams. BMC Health Serv Res. 2020;20(1):791.
- Rekha Devi K, Sen AM, Hemachandran K. A working framework for the user-centred design approach and a survey of the available methods. Int J Sci Res Publ. 2012;2:4.
- Jayes M, Palmer R, Enderby P. Development of a mental capacity assessment support tool: a user-centred design process. Int J Stroke. 2015;10:65.
- Nagykaldi ZJ, Jordan M, Quitoriano J, et al. User-centered design and usability testing of an innovative health-related quality of life module. Appl Clin Inform. 2014;5(4):958–970.
- Plaisance A, Witteman H, Leblanc A, et al. Development of a decision aid for cardiopulmonary resuscitation and invasive mechanical ventilation in the intensive care unit employing user-centered design and a wiki platform for rapid prototyping. PLoS One. 2018;13(2):e0191844.
- Kravetz AF. The role of user centered design process in understanding your users [Internet]. 2005; [cited 2018 Nov 10]. Available from: https://www.nul.nagoya-u.ac.jp/event/iadlc/archives/IADLC2005/kravetz.pdf.
- Mc Menamin R, Tierney E, Mac Farlane A. Who decides what criteria are important to consider in exploring the outcomes of conversation approaches? A participatory health research study. Aphasiology. 2015;29(8):914–938.
- Boivin A, Currie K, Fervers B, et al. Patient and public involvement in clinical guidelines: international experiences and future perspectives. Qual Saf Health Care. 2010;19(5):e22.
- Mc Menamin R, Griffin M, Grzybowska B, et al. Working together: experiences of people with aphasia as co-researchers in participatory health research studies. Aphasiology. 2021;2021:1–22.
- Staniszewska S, Brett J, Simera I, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ. 2017;358:j3453.
- Worrall L, Rose T, Howe TJ, et al. Access to written information for people with aphasia. Aphasiology. 2005;19(10–11):923–929.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ. 2008;337:a1655.
- Clinical Centre for Research Excellence in Aphasia Rehabilitation. Aphasia rehabilitation best practice statements: Comprehensive supplement to the Australian aphasia rehabilitation pathway. 2014. Available from: http://www.aphasiapathway.com.au/flux-content/aarp/pdf/2014-COMPREHENSIVE-FINAL-01-10-2014-1.pdf.
- Rose T, Worrall LE, Hickson LM, et al. Exploring the use of graphics in written health information for people with aphasia. Aphasiology. 2011;25(12):1579–1599.
- Rose T, Worrall L, McKenna K. The effectiveness of aphasia‐friendly principles for printed health education materials for people with aphasia following stroke. Aphasiology [Internet]. 2003;17(10):947–963.
- Pearl G, Cruice M. Facilitating the involvement of people with aphasia in stroke research by developing communicatively accessible research resources. Top Lang Disord. 2017;37(1):67–84.
- de Brún T, O’Reilly – de Brún M, Van Weel-Baumgarten E, et al. Using participatory learning & action (PLA) research techniques for inter-stakeholder dialogue in primary healthcare: an analysis of stakeholders’ experiences. Res Involv Engagem. 2017;3(1):28.
- Mc Menamin R, Tierney E, Mac Farlane A. Addressing the long-term impacts of aphasia: How far does the conversation partner programme go? Aphasiology. 2015;29(8):889–913.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112.
- Elo S, Kääriäinen M, Kanste O, et al. Qualitative content analysis: a focus on trustworthiness. SAGE Open. 2014;4(1):215824401452263.
- Lincoln YS, Guba EG. Naturalistic inquiry. Thousand Oaks: Sage Publications; 1985.
- Koch T. Establishing rigour in qualitative research: the decision trail 1993. J Adv Nurs. 2006;53(1):91–100.
- Hersh D, Godecke E, Armstrong E, et al. Ward talk”: nurses’ interaction with people with and without aphasia in the very early period poststroke. Aphasiology. 2016;30(5):609–628.
- Horton S, Lane K, Shiggins C. Supporting communication for people with aphasia in stroke rehabilitation: transfer of training in a multidisciplinary stroke team. Aphasiology. 2016;30(5):629–656.
- Jensen LR, Løvholt AP, Sørensen IR, et al. Implementation of supported conversation for communication between nursing staff and in-hospital patients with aphasia. Aphasiology. 2015;29(1):57–80.
- O’Halloran R, Grohn B, Worrall L. Environmental factors that influence communication for patients with a communication disability in acute hospital stroke units: a qualitative metasynthesis. Int J Lang Commun Disord. 2011;46(1):30–47.
- Simmons-Mackie NN, Kagan A, O’Neill Christie C, et al. Communicative access and decision making for people with aphasia: Implementing sustainable healthcare systems change. Aphasiology. 2007;21(1):39–66.
- Northcott S, Simpson A, Moss B, et al. Supporting people with aphasia to 'settle into a new way to be': speech and language therapists’ views on providing psychosocial support. Int J Lang Commun Disord. 2018;53(1):16–29.
- Bright FAS, McCann CM, Kayes NM. Recalibrating hope: a longitudinal study of the experiences of people with aphasia after stroke. Scand J Caring Sci. 2020;34(2):428–435.
- Howe TJ, Davidson B, Worrall L, et al. You needed to rehab … families as well: family members’ own goals for aphasia rehabilitation. Int J Lang Commun Disord. 2012;47(5):511–521.
- Hebert D, Lindsay MP, McIntyre A, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11(4):459–484.
- Hallé M-C, Le Dorze G. Understanding significant others’ experience of aphasia and rehabilitation following stroke. Disabil Rehabil. 2014;36(21):1774–1782.
- Dehghan Nayeri N, Mohammadi S, Pedram Razi S, et al. Investigating the effects of a family-centered care program on stroke patients’ adherence to their therapeutic regimens. Contemp Nurse. 2014;47(1–2):88–96.
- Visser-Meily A, Post M, Gorter JW, et al. Rehabilitation of stroke patients needs a family-centred approach. Disabil Rehabil. 2006;28(24):1557–1561.

