Abstract
Purpose
Current research suggests that feeling a lack of control is common among people living with Motor Neurone Disease (plwMND). This systematic review explores and synthesises evidence about: (1) What factors contribute towards perceptions of control in plwMND (2) How do plwMND attempt to maintain control in their daily lives?
Methods
A systematic search from inception to January 2022 for peer-reviewed journal articles in English reporting qualitative and mixed-method primary studies or reviews of plwMND’s perceptions or experiences of control was conducted on CINAHL, MEDLINE, PsycINFO, ASSIA, Embase and AMED. Eligible articles underwent quality appraisal, data extraction and a thematic synthesis was carried out.
Results
Twenty publications, 19 primary studies and one review, from nine countries, reporting the views of 578 participants aged from 20 to 90 years were included. Two key analytical themes were identified (1) diagnosis can lead to a disruption of previously held control beliefs (2) plwMND use a range of control strategies to attempt to retain control in their lives.
Conclusion
This is the first systematic review and qualitative evidence synthesis to reveal the strategies plwMND use to regain control and that control beliefs about health, fate, identity and bodily control are significantly altered by the diagnosis.
Outcome measures for plwMND should consider personal values and preferences as well as objective clinical measurements.
plwMND use a range of control strategies which may alter and change over time therefore healthcare professionals may also need to review and adapt treatment decisions over time.
The differing viewpoints of healthcare professionals and plwMND should be considered in clinical situations to reduce the potential for conflict.
Implications for rehabilitation
Introduction
Motor Neurone Disease (MND) is a neurodegenerative disorder of unknown aetiology where the motor neurones no longer function effectively leading to muscle wasting and the associated decline in physical function [Citation1]. The disease pattern can vary individually but the progressive nature of the disease means that, although the timing is unpredictable [Citation2], the decline in the ability to complete activities of daily living and maintain a social life is inevitable. The most common physical problem is muscle weakness, which leads to problems with mobility, swallowing, speech and breathing eventually leading to respiratory failure, which is usually the cause of death [Citation1,Citation3]. Although rare, MND has a large socioeconomic cost [Citation4] and the effects on daily life are profound for both people living with MND (plwMND) and their families and carers [Citation5,Citation6].
There is as yet no cure for MND, and thus medical care involves symptom treatment or the provision of life-sustaining treatments such as Non-invasive Ventilation (NIV) to aid breathing and placement of a feeding tube when nutritional intake is impaired. Although thought to have the potential to improve quality of life or prolong survival [Citation7], neither of these life-sustaining treatments offer any respite in the progression of the disease [Citation8] and 50% of patients die within 3 years of symptom onset [Citation9].
There is no definitive diagnostic indicator for MND and due to the diversity of initial symptoms plwMND may have gone through a period of many months of referrals to various specialists before being “stunned” by the terminal diagnosis [Citation10,p.82]. After this initial shock plwMND must learn how to live with the unpredictable progression of this disease. Research shows a great diversity in this experience [Citation5,Citation11] but one factor which seems to be consistent is a perception of a loss of control within their lives. Within health research many concepts and theoretical models of control have been researched: for a comprehensive discussion of control in relation to neurodegenerative diseases see Eccles and Simpson [Citation12]. This review will focus on the concept of perceived control which has been defined as the belief that a particular situation is under control or can be controlled [Citation12]. Research on other neurodegenerative illnesses has shown that perceived control is an important factor in the quality of life [Citation13,Citation14]. Increasing a person’s perception of control in a given situation is thought to lead to an increased sense of well-being [Citation15].
The onset of a life-limiting disease is known to be a source of stress that can lead to feelings of loss of control, helplessness and anxiety [Citation16]; more specifically feelings of a lack of control have been highlighted as a major cause of anxiety and stress for plwMND and their carers [Citation17]. The importance of attempting to maintain a sense of control in the lives of plwMND has been found in a previous qualitative thematic synthesis [Citation18] which investigated in general terms people’s experiences of living with MND. A previous quantitative review [Citation12] highlighted a lack of research measuring perceived control in MND and also the lack of consistency in methods of assessing perceived control but there is an increasing body of qualitative research exploring people’s experiences of MND [Citation18]. However, there have been no qualitative evidence syntheses focusing specifically on how plwMND perceive and experience control; such a synthesis could lead to a richer interpretation and deeper understanding of the phenomena.
The aim of this systematic review and synthesis of qualitative studies is to explore plwMND’s perception and experiences of control within their daily lives, the potential reasons for a perceived lack of control and how plwMND adapt to this. This is important because research suggests that a person’s quality of life and ability to cope with MND may be related to their perception of how much control they have within their life [Citation19,Citation20]. An in-depth exploration of perceptions and experiences of control or lack of control during life with MND may suggest ways to improve quality of life and inform health and support services for plwMND.
This review explores the following questions:
What factors contribute towards perceptions of control within plwMND?
How do people living with MND attempt to maintain control in their daily lives?
Methods
This qualitative systematic review follows the methods for thematic synthesis [Citation21]. The inductive approach of thematic synthesis was chosen to enable the data to be explored without a priori analytical frameworks, generating initial themes from the data and developing these into new interpretations or analytical themes. In reporting this research the ENTREQ Enhancing transparency in reporting the synthesis of qualitative research: reporting guidance [Citation22] have been used and can be seen in Supplementary File 2.
Inclusion and exclusion criteria
The inclusion and exclusion criteria were formulated by NG with support from FH (a senior qualitative researcher) and are documented in . Peer-reviewed journal articles, both primary studies and qualitative evidence syntheses, containing qualitative data which focused upon the daily lives of plwMND of any type were included. As there may be a discrepancy between plwMND’s views of their life and the views of their carers or health professionals [Citation23,Citation24], only articles where the data came directly from plwMND were included. The phenomenon of interest was plwMND’s perceptions or experiences of control. The term control can be subjective therefore other terminologies such as autonomy, agency, adaptation and any domains potentially related to control were included, articles that made no mention of control, or any aspects related to control in the full text were excluded. Quantitative research was excluded but articles reporting mixed methods studies were included if the qualitative data could be separated and extracted. Articles pre-1999 were excluded as were those not in English.
Table 1. Inclusion and exclusion criteria.
Systematic search and screening process
The SPIDER tool [Citation25] for qualitative evidence synthesis offers a systematic strategy for searching for qualitative (and mixed-methods) research studies and was used to help identify the key search concepts: (1) Sample – Adults with MND of any type (2) Phenomenon of interest – plwMND’s perceptions or experiences of control or any domains related to control in their day to day lives (3) Design – qualitative research. The search terms were mapped for each key search concept and the strategy tailored for each database; an example search can be found in the Supplementary Files. Six relevant databases CINAHL, Medline, PsycINFO, ASSIA, Embase, andAMED were searched up to January 2022. Full search histories are available on request from the corresponding author.
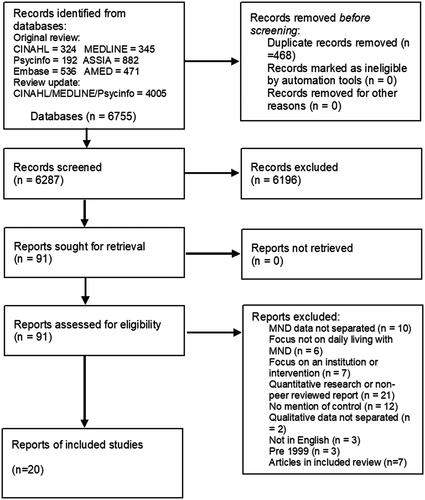
In total, the searches yielded 6755 citations. The results and screening process are detailed fully in the PRISMA flow chart [Citation26] in . Retrieved references were screened by title and abstract then by full text by the lead author, 20% of titles and abstracts were independently screened by the third author and another PhD student. Any disagreements in screening were discussed between screeners and an agreement was sought.
Figure 1. PRISMA 2020 flow diagram.
One of the articles found was a qualitative thematic synthesis of experiences of living with MND [Citation18]. As the review article was a thematic synthesis with data extraction and analysis processes very similar to those intended for this paper and the review article met the inclusion criteria it was decided to include the review article rather than all the individual primary studies included in this review. In a qualitative analysis reanalysing these same primary studies may not yield any more significant results than those already found in the existing review.
Quality appraisal
All primary articles included in the final selection of this review were subject to quality assessment using the Joanna Briggs Institute Critical Appraisal Checklist for Qualitative Research [Citation27]. Of these articles five were unclear if there was congruity between the stated philosophical perspective and the research methodology, ten had no statement locating the researcher culturally or theoretically and ten did not address the influence of the researcher on the research and vice-versa. No primary articles were excluded during the quality appraisal process as all 19 articles adequately portrayed participants’ voices.
Characteristics of included studies
Characteristics of included studies are shown in . The 20 included articles were 19 primary qualitative research articles [Citation28–46] and one qualitative evidence synthesis [Citation18]. Primary studies were located in the United Kingdom (n = 11), Italy (n = 1), Ireland (n = 2), New Zealand (n = 1), Australia (n = 1), Sweden (n = 1) China (n = 1) and jointly the United Kingdom and Australia (n = 1). The included review article [Citation18] synthesised 20 studies located in the United Kingdom (n = 10), USA (n = 3), Sweden (n = 3), New Zealand (n = 10), Ireland (n = 1), Australia (n = 1) and Canada (n = 1). Of the 19 primary study articles, only nine [Citation28–30,Citation32,Citation34,Citation37,Citation44–46] specified the type of MND with which participants had been diagnosed. The duration of illness ranged from one month to 19 years but was not specified in four of the articles [Citation29,Citation36,Citation43,Citation45] and the ages of the 578 participants ranged from 20 to 90 years. None of the articles state investigating perceptions of control is the main aim of the study.
Table 2. Characteristics of included studies.
Data extraction and synthesis
Following the process of familiarisation with the texts (common to qualitative analysis), copies of each article were imported into the qualitative data analysis software NVivo 12 (QSR International), which was used for the synthesis. Data were considered to be the results or findings sections of each article, including any example participant quotes and tables of relevance [Citation21].
Following data extraction, Thomas and Harden’s [Citation21] three stages of thematic analysis were followed. Firstly, each line of text in the extracted data was read and coded according to its meaning and content. No, a priori framework was used, codes were constructed inductively from the data and were altered and merged during the coding process, for example, an initial code about participants questioning medical opinion developed into a code encompassing all interactions with healthcare staff. This initial process led to 48 separate free codes being constructed.
The second stage was to explore the coded data and annotations linked to the codes to highlight any similarities or differences in meaning and identify any links between the coding categories to create a tree hierarchy of the initial codes which helped to visualise the relationships between the codes and aided the translation of concepts between the individual articles. This process led to the formation of descriptive themes generated from the initial data. The third and final phase was further analysis and discussion of this coding with the senior qualitative researcher (FH), developing more overarching analytical themes which relate back to the original research questions.
Results of synthesis
The translation of concepts between studies led to the development of two key analytical themes and seven subthemes; an overview of themes and supporting articles are shown in .
Table 3. Overview of themes and study support at subtheme unit.
Theme 1 – a diagnosis of MND can lead to a significant disruption of previously held control beliefs
Control beliefs are people’s individual beliefs about how much control they have within their world [Citation47]. The significant disruption of control beliefs theme highlights how the physical symptoms and the investigative pathway towards the subsequent diagnosis of MND can dramatically affect these individual control beliefs. The four subthemes illustrate four different control beliefs which appeared to be affected by a diagnosis of MND: health, fate, body and identity.
Sub theme - Control beliefs about health
The studies suggested that prior to diagnosis most participants believed they were in control of their lives and their health. Several studies demonstrated that participants were working or caring for family, had active hobbies and took a fully active role in their communities [Citation29,Citation32,Citation34,Citation38,Citation41].
The first symptom mentioned by participants was often a small loss of physical control over the body [Citation36,Citation39]. Harris [Citation38,p.2065] reports “Charles was out walking his dog when he first noticed his foot drop.” Being unable to explain these symptoms led to the first doubts about the belief that they were in control of their health, Hocking [Citation39,p.25] described this as a “wobble” in participants’ lives.
Participants sought the help of the medical profession [Citation39,Citation41] in the belief that they would be able to make a quick diagnosis and suggest treatment and thus they would regain control over their health. One participant (Bert) said:
So I’m thinking to myself, it could be this, that or the other, it’ll be something…I even thought it might be a tumour, something in my head that needs a quick zap, go in with a drill and pull it and the job’s done [Citation41,p.944].
However, the lack of diagnostic markers in MND makes a quick diagnosis unlikely and most participants had a long and unsatisfactory process of diagnosis [Citation32,Citation34,Citation36,Citation37,Citation39]. The diagnostic process itself contributed to the erosion of the belief that the medical profession would be able to help regain control over health [Citation38,Citation39,Citation41,Citation45,Citation46]. In some cases, this led to mistrust as one participant put it: “The whole thing was disjointed and the worst of it, I was being kept in the dark…I’d lost confidence in the whole [swears] thing” [Citation34,p.322]. When the diagnosis was finally disclosed, and it was explained that there is no real treatment or cure, participants’ previous beliefs that they or medical professionals were able to control their health appeared to be profoundly altered [Citation36,Citation37]. Phrases such as “bombshell” [Citation41,p.943] and “a blow” [Citation32,p.5036] were used to highlight the devastating shock of a terminal diagnosis. Yuan et al. [Citation46] suggest that some people believed their doctor had misdiagnosed them and were in denial about their diagnosis.
Sub theme: Control beliefs about fate
Articles highlighted participant beliefs that through being a “good” person or leading a healthy lifestyle they were able to have some control over their fate, in the context of living a long and healthy life [Citation41,Citation42]. Hogden et al. [Citation40,p.832] offered a participant quote: “Because I’m such a healthy person, and to get something like this, you think ‘Ok what did I do?’ It’s not right.”
Studies [Citation41,Citation42,Citation46] demonstrated how diagnosis presented a significant challenge to beliefs in the control of fate. Participants in these studies spoke of feeling that they were being punished and of losing their belief in God post-diagnosis. This quote from one participant illustrates his struggle with the belief that if he led a good life, he would have a long and healthy life:
I have never done anybody any harm…never been in trouble with the police…lead a good life…why me and I thought ‘it’s not fair’ yet people are robbers, the muggers, all the rapists; they live till forever and I got this and I’m not going to live my full term [Citation41,p.942].
“Looking for a reason - why me?” emerged as an inductive code during the synthesis process and this search for causal understanding was a theme throughout the articles [Citation32,Citation36,Citation38,Citation39,Citation41]. This seemed to be something plwMND struggled with soon after diagnosis [Citation39,Citation41]. However, current medical understanding of MND cannot offer any explanations for the cause of the disease nor clear potential risk factors. This lack of causal explanation presented a challenge to participants’ beliefs that they (or others) had some control over their fate, and this appeared to be dealt with in differing ways.
Some people seemed to go through a process of coming to terms with this challenge to their control beliefs concluding that MND was not their fault and the cause was something they had not had any control over [Citation36,Citation41]. The participant quoted above, who initially thought his diagnosis unfair as he had led a good life, over time changed his view to believe that life events were random and that his diagnosis was not connected with whether he had led a good life or not. The authors of this study suggested this to be “successfully navigating these central concerns of maintaining control and reaching causal understanding.” [Citation41,p.945].
Other participants seemed to struggle with the challenge to their control beliefs and were unable to accept that no action or person or divine being had control over the cause [Citation32,Citation40–42]. This could lead to feelings of bitterness, resentment, anger, frustration and despair as demonstrated by this participant’s quote “…neurology controls are useless if you do not know the cause and there isn’t a cure, it’s just a waste of time” [Citation32,p.5039]. Those who were able to accept that their previous control beliefs about their fate needed adaptation post-diagnosis appeared better able to cope with their new life with MND [Citation30,Citation41]:
I have reflected on my granddaughter. Each time I see her – she can do more. And each time she sees me – maybe I can do less. And that’s an interesting balance. I’m not bitter. I could be but I chose not to be [Citation30,p.6]
Sub theme: Control beliefs about the body
The accumulating physical losses caused by MND led to some study participants doubting the belief that they were in control of their bodies [Citation18,Citation28,Citation33,Citation35,Citation39,Citation41,Citation44–46]. It was found that plwMND expressed that their bodies felt and moved differently and no longer reacted to commands [Citation39]. The sense that their body was now in control of them is demonstrated in this quote:
personally I think it’s [that] my own body is withdrawing from my old life…I’m not doing it deliberately. My body is saying you know pull back from that and that’s what’s happening [Citation33,p.115].
This reduced sense of command over the body was a feature expressed in several studies [Citation28,Citation29,Citation32,Citation41,Citation46] but it was not just the inability to give the body individual commands that were lost. The growing realisation that nothing could control the rate of physical decline [Citation29,Citation40] some plwMND expressed as feeling like their body had been taken over by something else “this alien that has taken over my body and I have not too much defence against it” [Citation33,p.116].
This lack of belief that they were able to control their bodies along with the knowledge that MND can affect almost all areas of the body led to fears of losing all physical control [Citation18,Citation33,Citation42,Citation46]. Some plwMND feared they would become “trapped” [Citation43,p.450] or “prisoners in their own bodies” [Citation42,p.2144], able to understand the world around them but powerless to move or communicate their needs or wishes:
It’s going in the direction of taking all my faculties, my independence, me speech, my mobility, concentration, eating. Everything I was doing is now gone [Citation33,p.115].
Unlike the significant disruption of control beliefs over fate or health, the loss of the belief that they were in control of their bodies appeared to be linked to existential issues [Citation29,Citation30,Citation32–34]. Ozanne et al. [Citation42,p.2144] reported that “interviewees appeared to feel their physical loss put their whole existence on hold.” Participants in other studies also questioned whether life without control of the body is a life or just an existence [Citation29,Citation34,Citation42], one person expressed that he may be alive but not living [Citation41].
This question of whether life with MND is living or just existing was spoken about openly by plwMND in several articles [Citation29,Citation30,Citation32–34]. In their studies Ando et al. [Citation29] and Foley et al. [Citation34] found existential questions to be involved in plwMND’s treatment decision-making, suggesting that for some plwMND life-sustaining treatments such as non-invasive ventilation or tube feeding may be perceived to be contributing towards existing rather than living. Some participants saw these treatments as having the potential to prolong a life that to them was not worth living without being able to control the body, as this quote highlights:
And it can potentially prolong your life when even though all the MND symptoms carry on getting worse, you might have departed by then [/…] I don’t want things keeping me alive when frankly I’d be better off dead [Citation35,p.1005].
Potentially influenced by traditional culture, participants in China spoke about making the most of their remaining days but seldom discussed death [Citation46]
Sub theme: Control beliefs about identity
Identity appeared to be closely bonded to the roles people played within their lives, whether this was mainly through work, family or community activities, all roles required physical ability to carry them out. The physical losses caused by MND often meant these activities were no longer possible therefore, for plwMND, their role within their lives changed and thus their identity was now no longer within their control [Citation18,Citation29–31,Citation33,Citation39,Citation43,Citation44]. Increasing dependence often led to substantial role changes within family dynamics, with the carer of the family sometimes becoming the cared for [Citation32,Citation46]. Many participants found this change devastating [Citation18,Citation30,Citation32,Citation33,Citation39,Citation41,Citation46]. Cultural identity may also play a role here, Yuan et al. [Citation46] in their study in China found younger plwMND felt guilt that their elderly parents had to care for them because the cultural expectation is that they should care for their parents.
Those for whom identity was strongly related to their role in paid employment seemed to find the challenge to their control beliefs particularly difficult [Citation29]. Self-image appeared to be strongly related to work identity and for participants having to rely on carers for washing and dressing meant a loss of control over identity which could lead to frustration and resentment, as the following quotes demonstrate:
In business it’s important, you know, dress the part- not like this, I hate this now that I’m wearing” Simon [Citation29,p.349].
And as well she didn’t shave me so I have no shave now and I hate that …I think that might be the worst thing about these motor neurones. Matthew [Citation29,p.347].
Mistry and Simpson [Citation41] suggested that whilst the level of impairment and thus dependence are important, it is perhaps other changes, such as loss of self-image or identity, which affect psychosocial wellbeing. This seems to be reflected in Ando et al. [Citation29] as the above quotes indicate it was not the loss of independence that was an issue but the impact on self-image, so important to these people’s sense of identity, was not being maintained by their carer.
There was also evidence in the studies of some participants attempting to retain the belief that they controlled their identity by finding new roles or activities post-diagnosis [Citation30,Citation32,Citation39,Citation42,Citation44,Citation46]. These included helping the family with manageable tasks, inspiring others with MND and working out practical ways to continue normal activities despite MND. The use of technology to maintain control of identity was highlighted in Pavey et al. where one participant in the study stated “I come across as ‘me’ in email.” [Citation43,p.449].
Theme 2 – plwMND use a range of control strategies to attempt to retain control in their lives
Sakellariou et al. [Citation18] suggested that plwMND do not have control over the disease and therefore try to have control over their lives. This theme explores how plwMND attempted to retain control over their lives; evidence of a range of different control strategies used by plwMND was found and will be elaborated upon here.
The significant disruption of long-held control beliefs and the changes to daily life brought about by MND meant that in order to “move beyond the confines of the MND body” [Citation43,p.447] and maintain a life worth living, participants used differing control strategies to attempt to retain some form of control within this new life. Control strategies are what people do to retain control in situations where this has been challenged [Citation47]. The control strategies documented below were all derived from this synthesis of studies.
Although described separately for ease of explanation, these control strategies were not necessarily used separately by plwMND but intertwined with each other and could be adopted or abandoned along the illness trajectory according to their usefulness at the time [Citation28,Citation29,Citation34,Citation35,Citation38,Citation40]. When changes in control strategy were forced due to the speed of MND progression this led to frustration [Citation44]. Due to the unpredictable length of time, people can live with MND there is the opportunity for a change in plwMND’s views over time as the disease progresses [Citation28,Citation38]. What was at one time perceived as an unacceptable loss of control may over time be reconsidered [Citation30,Citation34,Citation35,Citation40]. There is an example of this in Pavey et al. [Citation43,p.447] where participant ‘Andrew’ explained how incidental use of a wheelchair led to a change in his control strategy. After years of struggling with a walking stick, he realised that using a wheelchair could enhance the level of perceived control in his life rather than reducing it, as this quote demonstrates:
Over the years my attitude has changed considerably. Originally, I resisted the need to use a wheelchair and stuck (stubbornly) to using a stick……Looking back using a walking stick was a ludicrous situation but had anyone talked to me about it, I would have ignored them.
Three control strategies were identified in this synthesis: developing their own illness beliefs, focusing on the present, and maintaining personal values. Each are explained in more detail below.
Sub theme: Retaining control through developing their own illness beliefs
The lack of certainty in the available information on illness progression along with conflicting information from healthcare professionals and seeking information from the internet [Citation35,Citation39,Citation40,Citation44] led some participants in studies in the United Kingdom, New Zealand and Australia to feel frustrated with their situation. There was evidence of supportive health professionals [Citation44] but there was also evidence of poor provision of healthcare services in studies set in both the United Kingdom and Ireland [Citation33–35,Citation44]. For example, in Ando et al [Citation29] six of the nine participants expressed problems with their interactions with hospitals, two of these participants felt so negatively that they would not consider a trial of NIV treatment.
This uncertainty of information and in some cases negative experiences with healthcare services could lead to plwMND lacking trust in healthcare services and contribute to an erosion of the belief that healthcare professionals would be able to help them maintain control [Citation18,Citation29,Citation31,Citation33–35,Citation38–40,Citation44].
These issues and uncertainties may have led to some participants feeling that they could not rely upon medical or healthcare professionals and thus they developed their own illness beliefs to attempt to retain a level of control over their illness [Citation18,Citation28,Citation43,Citation44] as explained by “Fay”: “Well I thought the more I walk, the more I’ll be able to walk” [Citation43,p.448]. These personal beliefs in illness progression could be stronger than beliefs in treatments recommended by health professionals as Stephen illustrates:
If I’m not breathing for myself and letting a machine do it I’ll get worse quicker than if I just keep breathing on my own [Citation28,p.52].
This could lead to plwMND questioning the need for the treatments recommended by health professionals or seeking alternative therapies [Citation31,Citation44]. Other studies suggested that due to the progressive nature of MND personal beliefs in illness progression may only be a short-term method of retaining control. “Fay,” quoted above, initially believed she could control her ability to keep walking but as time progressed, she realised her personal illness belief was not working:
and now I know I must’ve looked like a drunken old bag walking down the road. But to me, you know, I thought the more I did the stronger I would become but it wasn’t to be…. [Citation43,p.448].
Sub theme: Retaining control through focusing upon the present
Living day by day and only dealing with issues when necessary, appeared in several studies [Citation18,Citation30,Citation32,Citation35–37,Citation40,Citation42,Citation44]. This strategy appeared to be a way of maintaining some control over an overwhelming situation, as this quote demonstrates:
to a large extent I keep my head pretty well buried in the sand as far as the reality of it all is concerned. Because as soon as you lift your head up and start to think about these things - you have to every now and then - it all gets a bit overwhelming [Citation40,p.833].
It appeared that for some, it was not just the disease and its consequences that caused them to feel overwhelmed but also the variety and number of healthcare services involved in their care [Citation29,Citation34,Citation38]. For other participants, contemplating their future life with MND was not thought to be helpful [Citation31–33,Citation35,Citation36]. In fact, some participants felt they had “no future” [Citation33,p.115]. The certainty of knowing that they were going to die but the uncertainty of not knowing when that would be was at the forefront of participants’ minds [Citation28,Citation30,Citation34,Citation42,Citation44] as James explained: “It’s a funny situation….It’s like being on death row without knowing when the executioner is going to pop in” [Citation37,p.1585]. Therefore, as a way of attempting to retain some form of control within their lives, they focused only on the present circumstances [Citation31,Citation35,Citation36,Citation40], for example, not wishing to think about a gastrostomy until unable to take food orally or only planning a few weeks ahead [Citation44]. The effort involved in just surviving day to day is shown in this quote:
Until you get to that stage you don’t actually focus on it because you’re actually focusing on the stage where you’re on. And that kind of consumes all your energy and all your time. So, until you actually reach that point you don’t deal with it [Citation35,p.1009].
Sub theme: Retaining control by focusing on maintaining their own personal values
Some plwMND when faced with the terminality of their diagnosis went through a process of evaluation of their lives and personal values [Citation18,Citation30,Citation40–42]. Supportive relationships became more important and people spoke of strengthening relationships with those who meant most to them [Citation30,Citation36,Citation42,Citation46]. As demonstrated by this quote: “What do I think is important? Having someone who cares about you, that we stand up for each other. These are things I took for granted before” [Citation42,p.2145].
Activities that met the most important values were maintained and those which reduced in importance now life had been limited were discarded [Citation30,Citation42]. Some chose to give up work and focus on family life:
After I was told that diagnosis and that I would be in a chair within 12 months, I decided to leave work….I wanted to spend more time with my family. My work wasn’t that important to me. [Citation40,p.833].
This focus only on what was important to the individual enabled a feeling of control within their lives and personal measures of disease progression were based upon the ability to continue doing the things which they valued most. Thus, plwMND developed their own personal outcome measures based on their values [Citation18,Citation29,Citation30,Citation44].
If the disease progressed to a stage where tools, equipment or services were required to enable the continuation of the activities which met these personal values, then they were accepted, and daily life adapted accordingly [Citation29–31,Citation43]. For example, Oliver accepted NIV as it enabled him to still go on family holidays, “It’s been good for me using that ventilator. I mean if, for instance going up to his caravan…I don’t think I would have been able to go” [Citation28,p.53].
Frustration was evident if participants could no longer take part in or no longer felt enjoyment from activities that met their personal values [Citation30,Citation44]. If tools, equipment or services did not enable the continuation of an activity that was valued or if they were perceived as taking too much time or effort to master [Citation31], then plwMND did not perceive the need for them [Citation29,Citation33]. Ando et al [Citation29] gave the example of “Catherine” whose breathing had been medically determined as poor but as she was still able to be in control of the things she valued, she did not perceive that NIV would be of benefit to her. As she said “Actually my own breathing is quite good…I’m usually just sat here during the day or I’m in bed and it doesn’t cause me any problems” [Citation29,p.353]. This shows she was still able to do the activities she valued and hence although her breathing tests may have indicated NIV would be of benefit she did not perceive there to be a need for this.
Discussion
The synthesis identified two analytical themes and seven subthemes which offer insights into which factors contribute toward perceptions of control and suggest a range of control strategies that people use to maintain control in their daily lives. Here we summarise how this synthesis answered these questions and how the findings bear relation to other literature in the field.
Factors which contribute towards feelings of lack of control
The suggestion in this synthesis that MND can begin to affect personal control beliefs prior to diagnosis appears to be new. However, it relates to research that suggests that the diagnostic process and delivery of the diagnosis is a key stage in the journey of plwMND and can significantly impact both plwMND and their carers [Citation10,Citation48,Citation49]. This synthesis suggests that the dissolving of previously held control beliefs may be involved in plwMND’s ability to come to terms with their diagnosis. Some participant's beliefs around control of fate quoted in the results have some resonance with the moral model of disability [Citation50], which attributes disability to a moral failing or punishment of past deeds. Research considering MND from the lens of disability theories is lacking but this may be a relevant future area of research. The alterations in control beliefs found in this synthesis significantly affect two key areas involved in adaptation to life with MND - the sense of self [Citation51] and dealing with existential issues [Citation52].
The sense of self and the belief in having control over identity for some participants in this synthesis appeared to be crucial to their ability to live more positively with MND and was also identified by Sakellariou [Citation18] as a way of taking control of one's life. This however did not appear to be an issue always considered by the authors of the studies included in this synthesis. For example, in Ando et al. [Citation28,p.53], one of the participants “Stephen” expresses “I go to work and some days it’s killing me to go. But I have to keep going and not give in,” the authors interpret this as a resistance to MND itself but perhaps what “Stephen” was expressing was an inability to come to terms with the belief that he is no longer in full control of his identity. He was continuing to battle into work to maintain his identity thus his refusal of NIV may be because he could not see how it would help him retain control over his identity. Whereas the authors, focusing on the physical effects of breathing suggested NIV would have “the potential for the amelioration of his current state” [Citation28,p.54]. In this case, it appears the psychosocial effects of MND are more important to the plwMND than the physical effects focused on by the authors and would suggest that clinical outcomes as assessed at medical consultations may not be the outcomes that matter to plwMND. This would have implications for evidence-based healthcare as the outcomes that matter to plwMND may not be the quantitative outcomes commonly used in quantitative studies and systematic reviews [Citation7]. This suggests that further understanding of the effects of MND on the sense of self from the point of diagnosis is needed. Acknowledgement by medical professionals that for some plwMND psychosocial issues may be of more importance to them than their physical symptoms may aid communication and understanding between plwMND and medical professionals.
The belief that participants were no longer in control of their bodies appeared to lead to consideration of existential issues and the question of when a life is worth living. Due to the wide range of illness duration within the included studies, it is impossible to determine where in the disease trajectory this question became a concern for plwMND but if it is related to belief in control over the body that would suggest that these issues are perhaps considered by patients long before they reach the end of their lives. Terminal diseases are usually considered to be of short duration however for those diagnosed with MND, although they know the disease is terminal upon diagnosis, the time period of disease progression can vary considerably. Lerum et al. [Citation53] suggest that MND inhabits an unusual place somewhere between chronic and terminal illness and thus is perhaps difficult to deal with in healthcare systems organised to treat an illness as chronic until it becomes terminal. This point was noted in this synthesis where these existential issues highlighted did not appear to be dealt with by current healthcare systems, in a range of high-income countries including the United Kingdom, Italy, Ireland and Sweden. Palliative care was not mentioned in the studies as being considered until near the end of life. Palliative care offers a holistic approach that would encompass these existential concerns, this review has highlighted the importance of these issues to plwMND and the provision of person-centred palliative care from the point of diagnosis may enable increased perceptions of control and improve quality of life. The findings of this synthesis would point towards an agreement with research that suggests that palliative care in terminal illness should begin from the point of diagnosis [Citation54,Citation55] and not be left towards the end of life as the participants in the included studies found.
Ways that people living with MND attempt to maintain control in their daily lives
The synthesis suggests that plwMND develop strategies to help them maintain control and that these strategies alter and change as the disease progresses. The impact these strategies may have on healthcare is discussed here.
Retaining control through focusing on the present
The use of strategies by plwMND to deal with losses of control was common throughout the synthesis. Many plwMND spoke of dealing with life day by day and not wanting to think about the future. However, this control strategy appears to conflict with the current professional opinion and guidelines. Recent care guidelines in the UK [Citation56,Citation57] encourage advance or anticipatory care planning perhaps even from the point of diagnosis. However, our findings reveal that plwMND are perhaps not ready to plan for the future and some plwMND feel they have no future or find the future overwhelming.
These differences of opinion appear to cause conflict between clinicians and plwMND, and this point is evident in Hogden et al. [Citation40,p.829] who suggest “clinicians perceive that the patients’ ability to engage in timely decision making is extremely challenging.” This may explain the current interest in research into how plwMND make decisions about their care [Citation58–60].
However, from the plwMNDs’ perspective, reducing their focus to the present time is probably quite effective in helping to control the overwhelming and disempowering effects of a future with MND. Greenaway et al. interpret this as a state of “active denial or non-acceptance” [Citation35,p.1006] but the findings from our synthesis would suggest that perhaps these people are not denying they have MND but are distancing themselves from it and the future as a method of controlling the situation. Denial can be an effective coping strategy. Indeed, research into Parkinson’s disease, a similarly chronic and progressive illness, has suggested that acceptance and denial may be intertwined, with denial not necessarily being maladaptive [Citation13]. Therefore, it appears that further research is needed to bridge this gap between the clinician’s wishes to plan for future care and plwMND who perhaps use focusing upon the present as a control strategy that works for them.
Retaining control through focusing on personal values
Another strong theme through the synthesis was of plwMND focusing upon the activities that mattered to them most thus “deteriorating performance of familiar activities became the benchmark for progression of the disease” [Citation39,p.25]. This focus on personal values appeared to be the basis of plwMND setting their own outcome measures which differed from clinicians.
This difference in outcome measures has also been found in previous research by Brown [Citation61] where she considered that professionals and lay people approach MND from differing value standpoints. Clinical care for MND often focuses on symptom management and enhancing quality of life. However, those outcome measures used by clinicians may not be of value to plwMND [Citation62]. These studies appear to support the finding in this synthesis that outcome measures for plwMND are not objective measurements that can be measured with a standardised tool but are very subjective and specific to personal values. For clinicians, this can make treatment difficult as assessment processes tend to use standardised tools which are not patient-specific but for plwMND, these outcome measures used by clinicians may not be meeting their individual needs. This could lead to misunderstanding if the parties involved are working towards different outcome measures.
There has been researching that suggests that patient-perceived outcomes are important in MND and may give a better measure of the quality of life than some standardised tools [Citation63]. However, it is encouraging to note that the recent General Standards for Neurological Care and Support for Scotland [Citation56] have person-centred care as Standard 7 encouraging the management of risk to support personal outcomes thus improving quality of life. These standards were only published in 2020, therefore it will be interesting to observe their impact on care for plwMND.
Strengths and limitations
The strengths of this review include the conduct of comprehensive literature searching of six databases using a robust search strategy. The literature screening process involved independent screening of 20% of retrieved references by two reviewers, with strong agreement. The involvement of two senior experienced qualitative researchers to support the junior researcher strengthened all aspects of the review. The included articles represent the views of 578 plwMND aged 20 to 90, from across nine countries. The similarity of perspectives on a control found in the synthesis across these nine high-income countries suggests an element of cultural commonalities.
The review was undertaken as an unfunded Masters's dissertation. Some steps of the rapid review methodology [Citation64–66] were adopted, for example, no grey literature was included and no citation searching was undertaken. Therefore it is possible that relevant studies may have been omitted, however, the omission of a few relevant studies in a qualitative review is not problematic because the purpose is to develop conceptual understanding rather than to draw firm conclusions about the effectiveness of an intervention [Citation67,Citation68].
The studies in this synthesis covered a range of high-income European, Scandinavian and Australasian countries and China, reflecting differing cultural contexts and healthcare systems. Other cultures may have different perceptions of control that were not apparent in this synthesis; and the issues discussed here may not be applicable to other healthcare systems such as those in lower-income countries. Another potential limitation is that only nine of the 19 included primary studies specified the type of MND that participants had and illness duration ranged from one month to 19 years, therefore no conclusions could be drawn about the impact of different types of MND which have different severity levels and duration. This may be important, particularly in research into perceptions of control which may be related to MND severity and duration.
One important issue not acknowledged in this review or in the primary studies included in the review is that of the potential effects of cognitive impairment among plwMND. None of the included studies mentioned any form of cognitive appraisal of participants; it is increasingly being recognised that cognitive impairment may be present therefore cognitive appraisal should be considered in future MND research.
Conclusion
This thematic synthesis has explored in-depth the perceptions and experiences of control for plwMND. It has expanded upon the findings of the included systematic review [Citation18] by adding an extra 19 studies to the body of evidence and contributing further depth and detail to their finding that plwMND attempt to regain some control within their lives, revealing the strategies that people actually use.
It is also proposed that control beliefs about health, fate, identity and bodily control are significantly altered by a diagnosis of MND. Due to the rarity of the disease and the diversity of the symptoms, diagnosis can often be a long process and this synthesis found that some alteration of control beliefs may occur prior to diagnosis. This suggests that upon diagnosis, MND may have already had a significant psychosocial impact and this impact should be assessed and considered in care planning. For plwMND, the psychological impacts of a terminal diagnosis are immediate. If the focus of MND care is on treating physical symptoms and not dealing with the extensive psychosocial impact caused by a terminal diagnosis this may not be meeting plwMND’s needs. The factors found which contribute towards a perceived lack of control, such as a lack of palliative care input from diagnosis and the differing viewpoints on the significance of outcome measures would suggest further research is needed into ways that the organisation of healthcare may be contributing towards a perceived lack of control. The finding that some plwMND are perhaps not ready to plan for the future would suggest further research is required to understand plwMND’s immediate needs as well as anticipated needs due to illness progression.
The ability to adapt to alterations in control beliefs appears to affect how plwMND come to terms with their diagnosis and therefore their quality of life. It seems that plwMND are not only dealing with the physical symptoms of MND from an early point in the disease journey but also the psychological, existential and social impacts which in turn can affect the quality of life. This suggests that the holistic approach of palliative care is required for some plwMND from the point of diagnosis but also that the individual nature of people’s experiences highlights a need for future research to listen to these experiences. The first author is currently undertaking further research using narrative methods to identify issues that may be unaddressed by current healthcare systems.
This synthesis found some control strategies used by plwMND that conflict with current care guidelines and outcome measures. Focusing on the present, setting personal goals or outcome measures and developing their own illness beliefs all conflicted with health professional’s standardised systems of care, leading to frustration on both sides. None of the included articles had perceived control as the main focus of their research but the synthesis of these articles indicates perceived control to be a major factor in plwMND’s decision-making and wellbeing. Further research into control beliefs and how plwMND select control strategies would explore the conflicts highlighted in this synthesis and hopefully lead to a more satisfactory healthcare system and a relationship which meets the needs of both the plwMND and the healthcare professionals.
Supplementary File 2.docx
Download MS Word (17.6 KB)Supplementary_File_1.docx
Download MS Word (15.8 KB)Acknowledgments
The authors are grateful to Clare Jouanny, Ph.D. researcher, who helped with the screening process.
Disclosure statement
The authors report no conflict of interest.
References
- Talbot K. Motor neurone disease. Postgrad Med J. 2002;78(923):513–519.
- Gordon PH, Cheng B, Salachas F, et al. Progression in ALS is not linear but is curvilinear. J Neurol. 2010;257(10):1713–1717.
- Holkham L, Soundy A. The experience of informal caregivers of patients with motor neurone disease: a thematic synthesis. Palliat Support Care. 2018;16(4):487–496.
- Schepelmann K, Winter Y, Spottke AE, et al. Socioeconomic burden of amyotrophic lateral sclerosis, myasthenia gravis and facioscapulohumeral muscular dystrophy. J Neurol. 2010;257(1):15–23.
- Soundy A, Condon N. Patients experiences of maintaining mental well-being and hope within motor neuron disease: a thematic synthesis. Front Psychol. 2015;6:606.
- Aoun SM, Bentley B, Funk L, et al. A 10-year literature review of family caregiving for motor neurone disease: moving from caregiver burden studies to palliative care interventions. Palliat Med. 2013;27(5):437–446.
- Radunovic A, Annane D, Rafiq MK, et al. Mechanical ventilation for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev. 2017;10(10):CD004427.
- Miller RG, Jackson CE, Kasarskis EJ, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2009;73(15):1218–1226.
- Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942–955.
- Aoun SM, O'Brien MR, Breen LJ, et al. The shock of diagnosis’: qualitative accounts from people with motor neurone disease reflecting the need for more person-centred care. J Neurol Sci. 2018;387:80–84.
- McCabe MP, O'Connor EJ. Why are some people with neurological illness more resilient than others? Psychol Health Med. 2012;17(1):17–34.
- Eccles FJR, Simpson J. A review of the demographic, clinical and psychosocial correlates of perceived control in three chronic motor illnesses. Disabil Rehabil. 2011;33(13–14):1065–1088.
- Eccles FJR, Murray C, Simpson J. Perceptions of cause and control in people with Parkinson's disease. Disabil Rehabil. 2011;33(15–16):1409–1420.
- Bishop M, Frain MP, Tschopp MK. Self-management, perceived control, and subjective quality of life in multiple sclerosis:an exploratory study. Rehabil Couns Bull. 2008;52(1):45–56.
- Pagnini F, Bercovitz K, Langer E. Perceived control and mindfulness: implications for clinical practice. J Psychother Integr. 2016;26(2):91–102.
- Neipp López MC, López-Roig S, Pastor MÁ. Control beliefs in cancer: a literature review. Anuario de Psicología. 2007;38(3):333–355.
- Ferrie JWP, Watson N. Living with MND: an evaluation of care pathways available to adults with and the families or carers of adults with motor neurone disease in Scotland. Glasgow: University of Glasgow; 2013.
- Sakellariou D, Boniface G, Brown P. Experiences of living with motor neurone disease: a review of qualitative research. Disabil Rehabil. 2013;35(21):1765–1773.
- Hogg KE, Goldstein LH, Leigh PN. The psychological impact of motor neurone disease. Psychol Med. 1994;24(3):625–632.
- Soofi AY, Bello-Haas V, Kho ME, et al. The impact of rehabilitative interventions on quality of life: a qualitative evidence synthesis of personal experiences of individuals with amyotrophic lateral sclerosis. Qual Life Res. 2018;27(4):845–856.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45.
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
- Bolmsjo I, Hermeren G. Interviews with patients, family, and caregivers in amyotrophic lateral sclerosis: comparing needs. J Palliat Care. 2001;17(4):236–240.
- Lule D, Ehlich B, Lang D, et al. Quality of life in fatal disease: the flawed judgement of the social environment. J Neurol. 2013;260(11):2836–2843.
- Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–1443.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Joanna Briggs I. The Joanna briggs institute critical appraisal tools for use in JBI systematic reviews checklist for qualitative research. Adelade: Joanna Briggs Institute; 2017.
- Ando H, Chakrabarti B, Angus RM, et al. Experience of long-term use of non-invasive ventilation in motor neuron disease: an interpretative phenomenological analysis. BMJ Support Palliat Care. 2014;4(1):50–56.
- Ando H, Williams C, Angus RM, et al. Why don't they accept non-invasive ventilation?: Insight into the interpersonal perspectives of patients with motor neurone disease. Br J Health Psychol. 2015;20(2):341–359.
- Ando H, Cousins R, Young CA. Flexibility to manage and enhance quality of life among people with motor neurone disease. Disabil Rehabil. 2022;44(12):2752.
- Cave R, Bloch S. Voice banking for people living with motor neurone disease: views and expectations. Int J Lang Commun Disord. 2021;56(1):116–129.
- Cipolletta S, Gammino GR, Palmieri A. Illness trajectories in patients with amyotrophic lateral sclerosis: how illness progression is related to life narratives and interpersonal relationships. J Clin Nurs. 2017;26(23-24):5033–5043.
- Foley G, Timonen V, Hardiman O. Exerting control and adapting to loss in amyotrophic lateral sclerosis. Soc Sci Med. 2014;101:113–119.
- Foley G, Timonen V, Hardiman O. Understanding psycho-social processes underpinning engagement with services in motor neurone disease: a qualitative study. Palliat Med. 2014;28(4):318–325.
- Greenaway LP, Martin NH, Lawrence V, et al. Accepting or declining non-invasive ventilation or gastrostomy in amyotrophic lateral sclerosis: patients' perspectives. J Neurol. 2015;262(4):1002–1013.
- Gysels MH, Higginson IJ. The lived experience of breathlessness and its implications for care: a qualitative comparison in cancer, COPD, heart failure and MND. BMC Palliat Care. 2011;10(pagination):15.
- Harris DA. Lived-through past, experienced present, anticipated future: understanding "existential loss" in the context of life-limiting illness. Palliat Support Care. 2015;13(6):1579–1594.
- Harris DA, Jack K, Wibberley C. The meaning of living with uncertainty for people with motor neurone disease. J Clin Nurs. 2018;27(9–10):2062–2071.
- Hocking C, Brott T, Paddy A. Caring for people with motor neurone disease. J Aust Rehabil Nurses' Assoc. 2006;9(3):24–28.
- Hogden AV, Greenfield D, Nugus P, et al. What influences patient decision-making in amyotrophic lateral sclerosis multidisciplinary care? A study of patient perspectives. Patient Prefer Adherence. 2012;6:829–838.
- Mistry K, Simpson J. Exploring the transitional process from receiving a diagnosis to living with motor neurone disease. Psychol Health. 2013;28(8):939–953.
- Ozanne AO, Graneheim UH, Strang S. Finding meaning despite anxiety over life and death in amyotrophic lateral sclerosis patients. J Clin Nurs. 2013;22(15–16):2141–2149.
- Pavey A, Warren N, Allen-Collinson J. It gives me my freedom': technology and responding to bodily limitations in motor neuron disease. Med Anthropol. 2015;34(5):442–455.
- Pinto C, Geraghty AWA, Yardley L, et al. Emotional distress and well-being among people with motor neurone disease (MND) and their family caregivers: a qualitative interview study. BMJ Open. 2021;11(8):e044724.
- Weeks KR, Gould RL, McDermott C, et al. Needs and preferences for psychological interventions of people with motor neuron disease. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20(7–8):521–531.
- Yuan MM, Peng X, Zeng TY, et al. The illness experience for people with amyotrophic lateral sclerosis: a qualitative study. J Clin Nurs. 2021;30(9–10):1455–1463.
- Skaff M. Sense of control and health. In Aldwin CM, Park CL, Spiro A, editors. Handbook of health psychology and aging. New York: Guilford Publications; 2007.
- O'Brien MR, Whitehead B, Jack BA, et al. From symptom onset to a diagnosis of amyotrophic lateral sclerosis/motor neuron disease (ALS/MND): experiences of people with ALS/MND and family carers – a qualitative study. Amyotroph Lateral Scler. 2011;12(2):97–104.
- Pavey A, Allen-Collinson J, Pavey T. The lived experience of diagnosis delivery in motor neurone disease: a sociological-phenomenological study. Sociol Res Online. 2013;18(2):36.
- Andrews EE, et al. Disability models. In: Budd MA, Hough S, Wegener STeditors. Practical psychology in medical rehabilitation. Cham: Springer International Publishing; 2017. p. 77–83.
- Young C, Ando H, Cousins R, editors. What is unique about quality of life in motor neurone disease?: A qualitative query. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. Conference: 25th International Symposium on ALS/MND; 2014; Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. Conference: 25th International Symposium on ALS/MND. Brussels Belgium. Conference Publication: (var.pagings). 15 (SUPPL. 1) (pp 117); Informa Healthcare; 2014.
- Bolmsjo I. Existential issues in palliative care: interviews of patients with amyotrophic lateral sclerosis. J Palliat Med. 2001;4(4):499–505.
- Lerum SV, Solbraekke KN, Holmoy T, et al. Unstable terminality: negotiating the meaning of chronicity and terminality in motor neurone disease. Sociol Health Illn. 2015;37(1):81–96.
- Murray SA, Kendall M, Mitchell G, et al. Palliative care from diagnosis to death. BMJ. 2017;356:j878.
- Oliver DJ. Palliative care in motor neurone disease: where are we now? Palliative Care. 2019;12(1):1–14.
- Scotland HI. General standards for neurological care and support. Scotland: NHS Scotland; 2019.
- National Institute for Health and Care Excellence. Motor neurone disease: assessment and management (NICE guideline 42). United Kingdom: National Institute for Health and Care Excellence; 2016.
- Clarke G, Fistein E, Holland A, et al. Planning for an uncertain future in progressive neurological disease: a qualitative study of patient and family decision-making with a focus on eating and drinking. BMC Neurol. 2018;18(1):115.
- Foley G, Hynes G. Decision-making among patients and their family in ALS care: a review. Amyotroph Lateral Scler Frontotemporal Degener. 2018;19(3–4):173–193.
- King SJ, Duke MM, O'Connor BA. Living with amyotrophic lateral sclerosis/motor neurone disease (ALS/MND): decision-making about ‘ongoing change and adaptation. J Clin Nurs. 2009;18(5):745–754.
- Brown JB. User, carer and professional experiences of care in motor neurone disease. Primary Health Care Research & Development. 2003;4(3):207–217.
- Simmons Z, Bremer BA, Robbins RA, et al. Quality of life in ALS depends on factors other than strength and physical function. Neurology. 2000;55(3):388–392.
- Simmons Z. Patient-Perceived outcomes and quality of life in ALS. Neurotherapeutics. 2015;12(2):394–402.
- Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: methods and implications of rapid reviews. Implementation Sci. 2010;5(1):1–10.
- Whitlock EP, Lin JS, Chou R, et al. Using existing systematic reviews in complex systematic reviews. Ann Intern Med. 2008;148(10):776–782.
- Khangura S, Konnyu K, Cushman R, et al. Evidence summaries: the evolution of a rapid review approach. Syst. 2012;1(1):1–9.
- Ames H, Glenton C, Lewin S. Purposive sampling in a qualitative evidence synthesis: a worked example from a synthesis on parental perceptions of vaccination communication. BMC Med Res Methodol. 2019;19(1):1–9.
- Benoot C, Hannes K, Bilsen J. The use of purposeful sampling in a qualitative evidence synthesis: a worked example on sexual adjustment to a cancer trajectory. BMC Med Res Methodol. 2016;16(1):1–12.

