Abstract
Purpose
Perceived control is an important construct for the psychological well-being of people affected by chronic conditions, and higher perceived control is associated with better outcomes. Psychosocial interventions have been trialled in these populations to improve both global and specific perceptions of control. However, most interventions involving people with Parkinson’s have focused on single-domain forms of control, while those addressing global perceived control are yet to be reviewed. This study aimed to identify and map the types of psychosocial interventions in individuals with Parkinson’s which have included forms of global perceived control as an outcome.
Materials and Methods
Scoping review based on a search across MEDLINE, PsycINFO, CINAHL, Academic Search Ultimate.
Results
From an initial return of 4388 citations, 12 citations were eventually included. These consisted of 8 quantitative and 4 qualitative studies, and covered 4 overarching categories of psychosocial interventions. Mixed results were found for cognitive, educational, and physical interventions, while a randomised controlled trial on mindfulness-based lifestyle programme showed more preliminary positive evidence.
Conclusions
Further rigorous research is required on the topic to build on these preliminary findings. In the meantime, clinicians may need to consider programmes which proved effective with populations similar to people with Parkinson’s.
Perceived control is a psychological construct important for people with chronic illnesses, which can be targeted by psychosocial interventions.
This article reviewed psychosocial interventions targeting global forms of perceived control in Parkinson’s.
Mixed results were reported for the cognitive, educational, and physical interventions identified, while a randomised controlled trial on a mindfulness-based lifestyle programme showed more promising evidence.
In the meantime, clinicians may need to consider programmes found to be effective with people with similar conditions to Parkinson’s.
IMPLICATIONS FOR REHABILITATION
Introduction
Perceived control is a psychological construct which has been defined as “the belief that one can determine one’s own internal states and behavior, influence one’s environment, and/or bring about desired outcomes” [Citation1] (p. 5). While there is a lack of theoretical consensus concerning this definition [Citation2,Citation3], it can be conceptualised as a broad construct encompassing a range of distinct yet complementary sub-constructs, each with their own literature [Citation3,Citation4]. These include general perceptions of control covering multiple domains of an individual’s life, such as feeling in control of health and social aspects in life (‘mastery’ [Citation5]), having personal control over outcomes as opposed to attributing them to external forces (‘locus of control’ [Citation6]), feeling able to execute the actions required by an outcome (‘self-efficacy’ [Citation7]), and feeling capable of controlling one’s adaptation to events in life, as opposed to controlling the events themselves (‘adaptive control’ [Citation4]). Based on these global perceptions, a number of single-domain forms of control have also been theorised, often covering very specific aspects such as control over an illness’ symptoms [Citation8], creativity [Citation9], and one’s own body and balance [Citation10,Citation11].
Irrespective of its exact conceptualisation, perceived control is considered of paramount importance for the psychological well-being of people with chronic health conditions [Citation12], with decades of literature showing a consistent link between higher levels of perceived control and better clinical outcomes, more successful adjustment to illness, fewer psychological difficulties, improved medication adherence, and higher quality of life [Citation1,Citation13–15]. In particular, perhaps due to the loss of physical control caused by motor impairments, perceived control has shown to play a pivotal role in the well-being of people with motor neurodegenerative diseases [Citation3,Citation16–20], including Parkinson’s disease [Citation21,Citation22].
Parkinson’s disease is a progressive motor neurodegenerative condition causing a number of issues which include slowed movements, muscular rigidity, rest tremor, postural and gait impairments, as well as cognitive difficulties which can eventually lead to dementia [Citation23,Citation24]. Parkinson’s is the second most common neurodegenerative disease in older people [Citation25], and is usually diagnosed after the age of 50 [Citation26]. Since no cure is currently available, symptomatic treatments represent the mainstay of its clinical management [Citation23] and frequently involve high levels of polypharmacy [Citation27]. In addition to motor and cognitive issues, people with Parkinson’s (PwPFootnote1) can experience a wide range of psychological difficulties, including depression, anxiety, apathy, impulse control disorders, and more rarely psychosis [Citation28–30]. These may also be coupled with a number of socio-relational issues, which can include stigma, loss of independence, loneliness, dehumanisation, as well as difficulties of social cognition such as impaired communication, emotion expression, and identification of emotional cues [Citation31–33]. Moreover, the combination of these biopsychosocial issues often lead PwP to have lower perceived control compared to the general population [Citation3,Citation34,Citation35].
Interventions have been trialled to improve perceived control in people living with chronic illness, focusing on its sub-constructs – due to their conceptually distinct nature – and addressing both global and single-domain perceptions. Traditionally, these interventions have taken the form of a wide range of psychosocial approaches, such as psychological therapy focused on cognitive restructuring of control beliefs [Citation36], cognitive rehabilitation based on touchscreen technologies [Citation37], educational workshops [Citation38], and self-management programmes [Citation39]. However, with regards to Parkinson’s in particular, most interventions appear to have focused on single-domain forms of control revolving around the body – and especially falls efficacy and fear of falling (for a review see [Citation40]) – while little is currently known about psychosocial interventions addressing global perceptions of control in PwP. This gap represents a considerable limitation in the literature, since global perceptions of control have been extensively identified as independent constructs compared to more specific forms of control [Citation22,Citation41–44]. Their development or improvement has also been suggested to play a more dominant role in an individual’s adjustment to new life demands (i.e., after the diagnosis of a chronic illness), particularly by exerting a top-down effect which extends into more specific domains of perceived control [Citation41,Citation45].
As a consequence, the overarching aim of the present review was to scope the current literature on psychosocial interventions for PwP which have included global perceptions of control as an outcome. This was seen as having not only the potential to help shed light on the gap in the current literature, but also to inform the development of more targeted and effective psychosocial interventions to improve perceived control in individuals with Parkinson’s.
Methods
Scoping reviews [Citation46] are defined as exploratory studies that “systematically map the literature available on a topic, identifying key concepts, theories, sources of evidence and gaps in the research” [Citation47] (p. 34). They permit the exploration of both conceptually and methodologically heterogenous topics (e.g., psychological/physical interventions, quantitative/qualitative methods) within the context of a developing and/or diverse body of literature, while retaining a fully systematic and replicable search strategy [Citation47,Citation48]. The methodology is outlined below, organised in accordance with the latest guidance for the conduct of scoping reviews available from The Joanna Briggs Institute [Citation49].
Identifying the research question
Based on the issues discussed above, the present review aimed to address the following research question: what types of psychosocial interventions studies have measured global perceptions of control as an outcome in people with Parkinson’s and with what findings?
Identifying relevant studies
The inclusion criteria required studies to: a) be related to individuals with a clinically confirmed diagnosis of Parkinson’s; b) involve people aged 18 or above; and c) describe the delivery of any psychosocial intervention addressing global perceptions of control as primary or secondary outcomes in PwP, d) be published fully in the English language. Reports of original empirical data were included. Qualitative studies that evaluated interventions were also included. ‘Psychosocial interventions’ were defined as non-pharmacological and non-surgical interventions “designed to affect the actions that individuals take with regard to their health” [Citation50] (p. 643). ‘Global perceptions of control’ were conceptualised as either the assessment of a general form of control (e.g., general perceived control, generalised self-efficacy; [Citation34,Citation51,Citation52] or a multi-domain assessment of control (e.g., multidimensional health locus of control [Citation53]). Reviews, commentaries, editorials, conference proceedings, unpublished theses, and letters were excluded.
Study selection
Following a preliminary search of the extant literature, free text and subject terms were identified to build a logic grid for the full search strategy (available as Supplementary Material). Based on this, a comprehensive search string was developed () to search four bibliographic databases – MEDLINE, Academic Search Ultimate, CINAHL, PsycINFO – from inception until December 2021 via the EBSCO platform. Hand searches were also carried out across the reference lists of key reviews and shortlisted citations to identify additional relevant studies. While the present review focused on global perceptions of control, search terms covering most domains of perceived control were included to ensure citations were not overlooked due to terminological issues.
Table 1. Overview of adopted search terms and identified items per database.
Based on the Joanna Briggs Institute guidance for scoping reviews [Citation49], and given the difficulty in selecting a quality assessment relevant to the different study designs included, a formal quality appraisal of the evidence was not performed in the present review. However, efforts were made to highlight any theoretical, methodological, and clinical limitations in the included studies whenever feasible and appropriate.
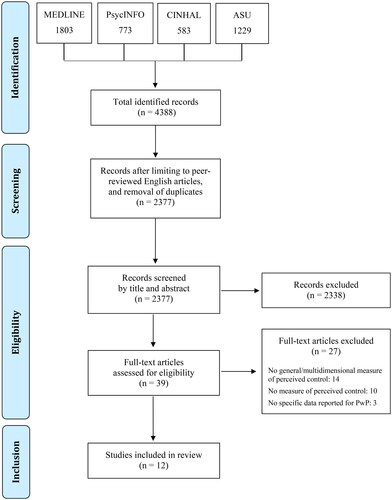
The initial search results were checked for duplicates and languages other than English, and then study titles and abstracts were screened against the inclusion and exclusion criteria. All remaining full-text articles were screened for eligibility by one reviewer (NZ) and double checked and confirmed by three more (KHOD, CF, JS), with any doubts or disagreements between reviewers solved through collective discussions. illustrates the PRISMA flow diagram for the study selection and data charting processes. An extension of the PRISMA Checklist for scoping reviews (‘PRISMA-ScR’) is also available as a Supplementary Material.
Figure 1. PRISMA diagram for selection of studies.
Charting the data
Data extraction in scoping reviews is often referred to as ‘data charting’ and is intended as a process which “provides the reader with a logical and descriptive summary of the results that aligns with the objective/s and question/s of the scoping review” ([Citation46]; p. 420). As a consequence of this descriptive nature, the adoption of coding methods for intervention components such as the Behaviour Change Technique (BCT; [Citation54]) or Practical Reviews in Self-Management Support (PRISMS; [Citation55]) was considered beyond the scope of the present study.
The charting process was carried out by one reviewer (NZ) and double-checked for accuracy by further three (KHOD, CF, JS). The following data were extracted from each study: category of intervention, country, design, sample, intervention’s specifics, relevant outcome, type of outcome, relevant measures, type of measures, and key results.
Protocol registration
No protocol was registered for the present review.
Results
From an initial return of 4388 citations, a total of 2377 was left following the preliminary filtering for duplicates and languages other than English. Screening titles and abstracts identified 39 full-text articles to inspect. Twelve studies met criteria for inclusion in the review, eight of which were quantitative investigations (including four RCTs [Citation56–59]), while the remaining four reported qualitative findings. Two of these reported quantitative and qualitative findings from the same sample [Citation58,Citation60]. Five investigations were carried out in the USA, three in Australia, two in the UK, one in Canada, and one in Norway.
Four overarching types of psychosocial interventions were identified: cognitive, educational, mindfulness-based, or physical. Consensus around these categories was reached by all reviewers following collective discussions and based on the predominant features of each intervention reported in the included studies (e.g., educational over cognitive or physical over educational). To aid this process, as well as for the sake of clarity, operational definitions for each type of intervention based on relevant literature were also developed (see ).
Table 2. Operational definitions of intervention types.
The findings of the studies which met the inclusion criteria are outlined and discussed below, categorised by types of interventions. When available, randomised controlled trials (RCTs) are highlighted in each category. illustrates the key results and characteristics of the included studies, while a full list of the remaining full-texts along with the reason for their exclusion is available as a Supplementary Material.
Table 3. Key characteristics of included studies.
Cognitive interventions
Only one study investigated a cognitive intervention which measured global perceptions of control in PwP. Hindle and colleagues [Citation56] carried out a single-blinded pilot RCT to compare a goal‐oriented cognitive rehabilitation programme in 10 people with Parkinson-related dementia with relaxation training and treatment as usual (TAU). The intervention consisted of eight weekly 1‐hour sessions exploring the use of compensatory or restorative strategies to cope with deficits involving planning, orientation, and memory skills. A measure of generalised self-efficacy (General Self-Efficacy Scale, GSE [Citation51]) was included as a secondary outcome. The results showed a statistically significant improvement in self-efficacy in the intervention group compared to relaxation training post-intervention. However, this was not maintained at 6-month follow-up, and no significant differences were observed between the intervention group and TAU at any time points.
Educational interventions
Educational interventions were investigated by three studies. Connor et al. [Citation57] enrolled 162 veterans with Parkinson’s in an RCT examining the effectiveness of the Care Coordination for Health Promotion and Activities in Parkinson’s Disease (CHAPS) programme for improving quality of care compared to TAU. The intervention consisted of guided care management sessions and resources administered by registered nurses. At post-intervention, the results showed no significant changes between the intervention group and TAU in levels of generalised self-efficacy (measured by the GSE as a secondary outcome).
Similar findings were reported by a non-randomised trial [Citation61] which administered the Stanford Chronic Disease Self-Management Program (CDSMP) to 27 PwP and found no significant changes in self-efficacy measured as a secondary outcome post-intervention using the Chronic Disease Self-Efficacy Scale (CDSES; [Citation62]). However, a sense of increased self-efficacy with regards to resource access and disease management appear to emerge as relevant themes from qualitative semi-structured interviews with the participants following the intervention.
Soundy and colleagues [Citation63] also carried out qualitative semi-structured interviews to explore the experiences of PwP participating in ‘First Steps’, a peer-led educational intervention developed by Parkinson’s UK for newly diagnosed individuals. The results, based on a hermeneutic phenomenological analysis, highlighted perceptions of control as playing a pivotal role in allowing participants to take action, ‘fight back’, and promote optimal adjustment following their diagnosis.
Mindfulness-based interventions
Two articles reported findings from a mixed-methods RCT exploring the effectiveness of a mindfulness-based lifestyle programme for improving Parkinson-related functioning and well-being against a wait list control [Citation58,Citation60]. The intervention consisted of six weekly 2-h group sessions including mindfulness techniques such as the body scan, attention to breath, and letting go of negative thoughts. Perceived control was assessed as a secondary outcome through a multi-domain measure, the Multidimensional Health Locus of Control (MHLC) Form B [Citation64]. At post-intervention, the results showed a significant group effect only for the internal dimension of locus of control [Citation58], suggesting that the participants of the intervention group reported significantly higher perceptions of internal causal attributions. However, the effect size was small (Cohen’s d = .28), and no group differences were observed at the 6-month follow-up. Moreover, the study suffered from considerable attrition, with over one third of participants in the intervention group lost from baseline to post-intervention (from 35 to 23) and in the control group from post-intervention to follow-up (from 37 to 25).
Semi-structured interviews carried out with RCT participants at post-intervention and follow-up [Citation60] identified general perceptions of control as a fundamental and pervasive theme for PwP, who appeared to feel a more achievable view of control at the end of the programme. At 6-month follow-up, some participants also felt that mindfulness training had allowed them to achieve a renewed view of control as part of taking responsibility and ownership over thoughts.
Physical interventions
Six studies investigated measured global perceptions of control in PwP following physical interventions. Sajatovic et al. [Citation59] carried out an RCT to explore the impact of a tailored group exercise self-management programme (‘Enhanced EXerCisE thErapy for PD, ‘EXCEED’) on depression, compared to individual self-guided exercise and self-management. The group intervention consisted of 1-h exercise sessions, three times a week, including low-resistance cycling and strength training. Generalised self-efficacy was measured as a secondary outcome with the GSE. At post-intervention, no significant difference was observed in self-efficacy between groups, and there were no significant within-group changes for participants undergoing EXCEED.
Ritter and Bonsaksen [Citation65] recruited 83 PwP to an uncontrolled pre-post study of a physical rehabilitation intervention based on the principles of the Parkinson Wellness Recovery® programme. This consisted of three weeks of exercises to slow the progression of the disease and improve symptoms, functioning, and quality of life. Generalised self-efficacy, assessed with the GSE, was a primary outcome. Following the interventions, the authors found a significant improvement in self-efficacy, albeit with a small effect size (Cohen’s d = 0.28).
A further uncontrolled pre-post study investigated a Parkinson’s therapeutic dance programme (‘Let’s Dance!’) twice a week for eight weeks with six PwP [Citation66]. The post-intervention assessment found no significant changes in generalised self-efficacy as a primary outcome measured with the GSE. Positive results were instead reported by a qualitative content analysis [Citation67] concerning the subjective experiences of 10 PwP who underwent a similar programme (‘Dancing with Parkinson’s’). These highlighted general increases in perceptions of control over life and Parkinson’s, and a shift towards more internal locus of control. Similarly, a thematic analysis of the experiences of 13 PwP undergoing an online dance therapy feasibility programme (‘ParkinDANCE Online’) identified an increased sense of mastery post-intervention [Citation68].
Finally, Cucca and colleagues [Citation69] investigated a 10-week art therapy programme for 18 PwP with an uncontrolled pre-post design. The intervention consisted of 20 sessions of 90-min administered twice a week involving a wide range of Parkinson-adapted physical artistic tasks, such as clay manipulation, drawing and painting, collage, and murals. At post-intervention, the results showed no significant changes in self-efficacy measured as a secondary outcome with a multidomain scale (PROMIS Self-Efficacy for Managing Chronic Conditions; [Citation70]).
Discussion
Summary of main findings
This scoping review mapped the types of psychosocial interventions for individuals with Parkinson’s which have measured global perceptions of control as an outcome, and associated findings. To our knowledge, this is the first review of these interventions in PwP. From 4388 initially identified citations, 12 were eventually found eligible for inclusion.
Our results indicate that general or multi-domain perceived control has been an outcome assessed in studies of four main types of psychosocial intervention for PwP: cognitive, educational, mindfulness-based, and physical interventions. These studies have evaluated four different global perceptions of control: general perceived control, locus of control, mastery, and self-efficacy. Of these, the most commonly investigated is generalised self-efficacy, evaluated in five studies using the GSE and in two studies with the CDSES or PROMIS Self-Efficacy for Managing Chronic Conditions respectively. A further study used the MHLC Form B as a multidimensional measure of locus of control. While these measures have been validated in populations including PwP [Citation71–73], only the GSE has undergone a formal validation with this population specifically, showing excellent psychometric properties (Cronbach’s α = .95; [Citation74]).
To date, only one study investigated a cognitive intervention (i.e., goal-oriented cognitive rehabilitation) with PwP using generalised self-efficacy as a secondary outcome [Citation56] (RCT). This showed significantly higher scores compared to relaxation training at post-intervention in the short term, but no significant difference in the longer term (i.e., after six months) or in comparison to TAU at any timepoint. Similarly mixed results were found by the three studies which tested educational interventions, with no significant impact observed for generalised self-efficacy compared to TAU when measured quantitatively with the GSE [Citation57] (RCT) or the CDSES [Citation61]. However, positive findings were reported for self-efficacy and general perceived control from qualitative interviews with PwP following participation in educational interventions [Citation61,Citation63].
Despite the long-recognised association between the constructs of perceived control and mindfulness [Citation75], only one investigation testing the impact of mindfulness-based interventions on global perceptions of control was identified in this review. This appeared to show some positive results, with significant improvements in internal locus of control compared to TAU in the quantitative analysis [Citation58] (RCT) and increased feelings of general perceived control emerging post-intervention qualitative interviews [Citation60].
Finally, the six studies testing physical interventions reported very mixed results. In particular, therapeutic dance programmes reported positive findings for general perceived control and mastery when using qualitative methods [Citation67,Citation68], while no changes were found for self-efficacy at post-intervention when an uncontrolled quantitative design was adopted [Citation66]. Similar negative results were reported for self-efficacy following the administration of art therapy [Citation69] and enhanced exercise therapy for Parkinson’s [Citation59] (RCT), while a significant improvement was observed after a tailored rehabilitation programme [Citation65].
Implications for future research
A noticeable contrast between the findings of quantitative and qualitative studies could be observed, with the latter consistently reporting more positive outcomes, even when they were part of the same mixed-methods intervention. A number of reasons may account for this. On one hand, the theoretical fragmentation which has traditionally characterised the construct of perceived control might make it harder to carry out accurate standardised measurements of subconstructs [Citation14]. This may be especially challenging when studies do not include perceived control tools specifically built or validated for Parkinson’s – as was largely the case in the present review, where only one of the measures used (GSE) was validated with PwP. Moreover, only two out of eight of the identified quantitative studies included perceived control as a primary outcome, showing no major differences in intervention design or delivery. This also means that most interventions (including all the RCTs) were not designed to have an effect on this construct specifically. Thus, future investigations should aim to include global perceptions of control as one of the primary outcomes of interventions while also adopting measures which are at least specifically validated (if not purposely built, like the Parkinson’s UK Scale of Perceived Control [Citation34]) for the Parkinson’s population.
On the other hand, the subjective and interpretative nature of the qualitative analyses, based on participants’ personal accounts filtered through the personal lens of researchers, means that specific subconstructs and psychological models of perceived control are less likely to be investigated or described when positive findings are reported. Future studies should be particularly mindful of these theoretical and methodological limitations. More specifically, quantitative investigations should aim to contain threats to validity and reliability by adopting robust validated tools to measure perceived control as a primary outcome (ideally based on the COMET initiative’s principles [Citation76]), while meeting essential criteria for rigour and trustworthiness (e.g., transparency, credibility; [Citation77]) should be prioritised when using qualitative methods.
In addition, despite the construct of perceived control being psychological in nature [Citation1,Citation14], no psychotherapeutic interventions for global perceived control in PwP were identified. Therefore, future studies investigating the impact of psychotherapy on global perceptions of control in individuals with Parkinson’s are strongly warranted. These may draw inspiration from psychological models already adopted successfully with PwP [Citation29], as well as other neurodegenerative conditions [Citation78–80].
Implications for clinical practice
While the current literature investigating the impact of psychosocial interventions on global perceptions of control in PwP is limited, our review indicates a number of potential implications for clinicians. First, although preliminary, the positive results around mindfulness-based lifestyle programmes add to the evidence in favour of adopting third wave approaches (e.g., mindfulness-based stress reduction or mindfulness-based cognitive therapy; [Citation81,Citation82]) to target perceived control [Citation75], particularly in light of their feasibility in this population [Citation29]. Therefore, this may represent an avenue worth considering for clinicians until more evidence on other psychotherapeutic models becomes available.
Similarly, until further research is carried out specifically with PwP, clinicians may want to consider psychosocial and/or psychological programmes which have shown to be effective at addressing perceived control with older people and other populations with chronic disability. In particular, these may include cognitive restructuring around control beliefs [Citation36], cognitive training to improve internal locus of control, touchscreen techniques to address feelings of mastery [Citation37], educational workshops on shifting health-related locus of control [Citation38], and self-management programmes to enhance self-efficacy [Citation39].
Limitations
When considering the present findings, we must bear in mind the intrinsic limitations of scoping reviews. These enable us to map emerging evidence, at a stage when there are relatively few studies, using heterogenous methods, with mixed results, precluding clinical recommendations, as is the case here. Scoping reviews such as this one identify the type of studies required to advance clinical treatments, and thus precede later systematic reviews at more advanced stages of research, which may also adopt specific taxonomies to code intervention components.
In addition, a number of limitations specific to the nature of the current literature should be considered. For instance, all included studies except one ([Citation65], set in Norway) were carried out in English-speaking countries, and no study was available outside Western countries. This is likely to exert some influence on the outcomes of interventions, particularly since evidence has shown that perceptions of control can vary significantly across different socio-cultural contexts (e.g., [Citation83,Citation84]). Similarly, the current lack of normative data on perceived control measures with specific conditions like Parkinson’s as well multiple cultures may limit the reliability of outcome changes reported post-intervention.
Conclusions
The current evidence on psychosocial interventions to improve global perceptions of control in individuals with Parkinson’s is considerably limited. Further rigorous research, carried out across different socio-cultural contexts, is warranted to build on these preliminary findings and investigate new approaches, such as targeted psychological interventions. In the meantime, clinicians may need to consider programmes which proved effective with populations similar to people with Parkinson’s.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Supplemental Material
Download MS Word (66.2 KB)Disclosure statement
Katherine Deane, UEA, is supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration East of England (NIHR ARC EoE) at Cambridge and Peterborough NHS Foundation Trust. The views expressed are those of the author[s] and not necessarily those of the NIHR or the Department of Health and Social Care.
Additional information
Funding
Notes
1 The terms ‘Parkinson’s’ and ‘people with Parkinson’s’ (or ‘PwP’) have been adopted in this article in lieu of the more common ‘Parkinson’s disease’ and ‘people with Parkinson’s disease’ (or ‘pwPD’) as the former currently represent Parkinson’s UK’s preferred way to describe this population in order to reduce the stigma associated with the term ‘disease’.
References
- Wallston KA, Wallston BS, Smith S, et al. Perceived control and health. Curr Psychol. 1987;6(1):5–25.
- Skinner EA. A guide to constructs of control. J Pers Soc Psychol. 1996;71(3):549–570.
- Eccles FJR, Simpson J. A review of the demographic, clinical and psychosocial correlates of perceived control in three chronic motor illnesses. Disabil Rehabil. 2011;33(13-14):1065–1088.
- Chipperfield JG, Perry RP, Stewart TL. Perceived control. In: Encyclopedia of human behavior. 2nd ed. Burlington, USA: Elsevier; 2012. p. 42–48. http://dx.doi.org/10.1016/B978-0-12-375000-6.00109-9
- Pearlin LI, Schooler C. The Structure of coping. J Health Soc Behav. 1978;19(1):2–21.
- Rotter J. Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr Gen Appl. 1966;80(1):1–28. http://psycnet.apa.org/journals/mon/80/1/1/
- Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122–147.
- Sirois FM. The control beliefs inventory. Unpublished manual. Ottawa, Ontario, Canada: Carleton University; 2003.
- Shaw A, Kapnek M, Morelli NA. Measuring Creative Self-Efficacy: an item response theory analysis of the creative Self-Efficacy scale. Front Psychol. 2021;12:678033.
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:239–243.
- Fuchs T, Koch SC. Embodied affectivity: on moving and being moved. Front Psychol. 2014;5:1–12.
- Dempster M, Howell D, McCorry NK. Illness perceptions and coping in physical health conditions: a meta-analysis. J Psychosom Res. 2015;79(6):506–513.
- Thompson SC, Kyle DJ. The role of perceived control in coping with the losses associated with chronic illness. In: Harvey J, Miller E, editors. Loss and trauma: general and close relationship perspectives. New York: Routledge; 2000. p. 131–145. http://psycnet.apa.org/record/2000-05604-009
- Reich JW, Infurna FJ. Perceived Control: theory, research, and practice in the first 50 years. New York: Oxford University Press; 2016.
- Walker J. Control and the psychology of health: theory, measurement, and applications. Philadelphia: Open University; 2001. https://books.google.co.uk/books?id=IOfaAAAAMAAJ
- Zarotti N, Simpson J, Fletcher I. ‘I have a feeling I can’t speak to anybody’: a thematic analysis of communication perspectives in people with huntington’s disease. Chronic Illn. 2019;15(1):61–73.
- Zarotti N, Coates E, McGeachan A, HighCALS Study Group, et al. Health care professionals’ views on psychological factors affecting nutritional behaviour in people with motor neuron disease: a thematic analysis. Br J Health Psychol. 2019;24(4):953–969.
- Bishop M, Frain MP, Tschopp MK. Self-management, perceived control, and subjective quality of life in multiple sclerosis: an exploratory study. Rehabil Couns Bull. 2008;52:46–56.
- Zarotti N, Eccles F, Broyd A, et al. Third wave cognitive behavioural therapies for people with multiple sclerosis: a scoping review. Disabil Rehabil. 2022;6:1–16.
- Eccles FJR, Craufurd D, Smith A, et al. Experiences of Mindfulness-Based cognitive therapy for premanifest huntington’s disease. J Huntingtons Dis. 2021;10(2):277–291.
- Verity D, Eccles FJRR, Boland A, et al. Does perceived control mediate the relationship between stigma and well-being for individuals with Parkinson’s disease? J Neurol Sci. 2020;14:116841.
- Walihagen MI, Brod M, Reimer M, et al. Perceived Control and Well-Being in Parkinson’s disease. West J Nurs Res. 1997;19(1):11–31.
- Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015;24:92–98.
- Weintraub D, Burn DJ. Parkinson’s disease: the quintessential neuropsychiatric disorder. Mov Disord. 2011;26(6):1022–1031.
- Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68(5):384–386.
- Willis AW, Schootman M, Kung N, et al. Epidemiology and neuropsychiatric manifestations of young onset Parkinson’s disease in the United States. Park Relat Disord. 2013;19(2):202–206.
- Daley DJ, Deane KHOO, Gray RJ, et al. Adherence therapy improves medication adherence and quality of life in people with Parkinson’s disease: a randomised controlled trial. Int J Clin Pract. 2014;68(8):963–971.
- Simpson J, McMillan H, Reeve D. Reformulating psychological difficulties in people with Parkinson’s disease: the potential of a social relational approach to disablism. Parkinsons Dis. 2013;2013:608562.
- Zarotti N, Eccles FJR, Foley JA, et al. Psychological interventions for people with Parkinson’s disease in the early 2020s: where do we stand? Psychol psychother theory. Res Pract. 2021;94:760–797.
- Ghazi-Noori S, Chung TH, Deane K, et al. Therapies for depression in Parkinson’s disease. Cochrane Database Syst Rev. 2003;2010
- Maffoni M, Giardini A, Pierobon A, et al. Stigma Experienced by Parkinson’s disease patients: a descriptive review of qualitative studies. Parkinsons Dis. 2017;2017:7203259.
- Macleod AD, Grieve JWK, Counsell CE. A systematic review of loss of independence in Parkinson’s disease. J Neurol. 2016;263(1):1–10.
- Prenger MTM, Madray R, Van Hedger K, et al. Social Symptoms of Parkinson’s disease stocchi F, editor. Parkinsons Dis. 2020;2020:1–10.
- Simpson J, Chatzidamianos G, Fletcher I, et al. A new scale measuring adaptive perceived control for people with Parkinson’s: initial construction and further validation. J Neurol Sci. 2018;391:77–83.
- Simpson J, Zarotti N, Varey S, et al. ‘It’s a double whammy’: a qualitative study of illness uncertainty in individuals with Parkinson’s disease in the context of COVID-19. Chronic Illn. 2021;18(4):174239532110431.
- Robinson SA, Lachman ME. Perceived Control and behavior change. In: Reich JW, Infurna FJ, editor. Perceived control. New York (NY): Oxford University Press; 2016. p. 201–228.
- Tyack C, Camic PM. Touchscreen interventions and the well-being of people with dementia and caregivers: a systematic review. Int Psychogeriatr. 2017;29(8):1261–1280.
- Barlow MA, Liu SY, Wrosch C. Chronic illness and loneliness in older adulthood: the role of self-protective control strategies. Heal Psychol. 2015;34(8):870–879.
- Marks R, Allegrante JP, Lorig K. A Review and synthesis of research evidence for Self-Efficacy-Enhancing interventions for reducing chronic disability: implications for health education practice (part II). Health Promot Pract. 2005;6(1):37–43.
- Abou L, Alluri A, Fliflet A, et al. Effectiveness of physical therapy interventions in reducing fear of falling among individuals with neurologic diseases: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102(1):132–154.
- Grether T, Sowislo JF, Wiese BS. Top-down or bottom-up? Prospective relations between general and domain-specific self-efficacy beliefs during a work-family transition. Pers Individ Dif. 2018;121:131–139. Available from
- Shelton SH. Developing the construct of general self-efficacy. Psychol Rep. 1990;66(3):987–994.
- Hortop EG, Wrosch C, Gagné M. The why and how of goal pursuits: effects of global autonomous motivation and perceived control on emotional well-being. Motiv Emot. 2013;37(4):675–687.
- Chipperfield JG, Greenslade L. Perceived control as a buffer in the use of health care services. Journals Gerontol - Ser B Psychol Sci Soc Sci. 1999;54:146–154.
- Emirza S, Öztürk EB, Şengönül AS. The quality of international mobility experiences, general self-efficacy and job search self-efficacy: a time-lagged investigation. Curr Psychol. 2021;40(4):1580–1591.
- Peters M, Godfrey C, McInerney P, et al. Chapter 11: scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI Manual for evidence synthesis. JBI; 2020. p. 406–451. https://synthesismanual.jbi.global
- Grimshaw J. A knowledge synthesis chapter. 2010. http://www.cihr-irsc.gc.ca/e/41382.html
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10.
- Cutler DM. Behavioral Health interventions: what works and why? In: Anderson NB, Bulatao RA, Cohen B, editor. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington (DC): National Academies Press (US); 2004. p. 643–676.
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinman J, editor. Measures in health psychology: a user’s portfolio. Causal and control beliefs. Windsor: NFER-NELSON; 1995. p. 35–37.
- Thompson SC, Spacapan S. Perceptions of control in vulnerable populations. J Soc Issues. 1991;47(4):1–21.
- Wallston KA, Stein MJ, Smith CA. Form C of the MHLC scales: a Condition-Specific measure of locus of control. J Pers Assess. 1994;63(3):534–553.
- Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
- Pearce G, Parke HL, Pinnock H, et al. The PRISMS taxonomy of self-management support: derivation of a novel taxonomy and initial testing of its utility. J Health Serv Res Policy. 2016;21(2):73–82.
- Hindle JV, Watermeyer TJ, Roberts J, et al. Goal-orientated cognitive rehabilitation for dementias associated with Parkinson’s disease-A pilot randomised controlled trial. Int J Geriatr Psychiatry. 2018;33(5):718–728.
- Connor KI, Cheng EM, Barry F, et al. Randomized trial of care management to improve Parkinson disease care quality. Neurology. 2019;92(16):E1831–E1842.
- Advocat J, Enticott J, Vandenberg B, et al. The effects of a mindfulness-based lifestyle program for adults with Parkinson’s disease: a mixed methods, wait list controlled randomised control study. BMC Neurol. 2016;16(1):166.
- Sajatovic M, Ridgel AL, Walter EM, et al. A randomized trial of individual versus group-format exercise and self-management in individuals with Parkinson’s disease and comorbid depression. Patient Prefer Adherence. 2017;11:965–973.
- Vandenberg BE, Advocat J, Hassed C, et al. Mindfulness-based lifestyle programs for the self-management of Parkinson’s disease in Australia. Health Promot Int. 2019;34(4):668–676.
- Pappa K, Doty T, Taff SD, et al. Self-Management program participation and social support in Parkinson’s disease: mixed methods evaluation. Phys Occup Ther Geriatr. 2017;35(2):81–98.
- Lorig K, Stewart A, Ritter P, et al. Outcome measures for health education and other health care interventions. Thousand Oaks (CA): sage Publications, Inc; 1996.
- Soundy A, Collett J, Lawrie S, et al. A qualitative study on the impact of first steps-a peer-led educational intervention for people newly diagnosed with Parkinson’s disease. Behav Sci (Basel). 2019;9(10):107.
- Wallston BS, Wallston KA, Kaplan GD, et al. Maides S a. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol. 1976;44(4):580–585.
- Ritter VC, Bonsaksen T. Improvement in quality of life following a multidisciplinary rehabilitation program for patients with Parkinson’s disease. J Multidiscip Healthc. 2019;12:219–227.
- Prewitt CM, Charpentier JC, Brosky JA, et al. Effects of dance classes on cognition, depression, and Self-Efficacy in Parkinson’s disease. Am J Dance Ther. 2017;39(1):126–141.
- Bognar S, DeFaria A, O’Dwyer C, et al. C. More than just dance: experiences of people with Parkinson’s disease in a dance program…Canadian physiotherapy association national congress 2016 may 26-28 Victoria BC. Physiother Canada. 2016;68:37.
- Morris ME, Slade SC, Wittwer JE, et al. Online Dance therapy for people with Parkinson’s disease: feasibility and impact on consumer engagement. Neurorehabil Neural Repair. 2021;35(12):1076–1087.
- Cucca A, Rocco D, Acosta A, et al. Art therapy for Parkinson’s disease. Park Relat Disord. 2021;84:148–154.
- Gruber-Baldini AL, Velozo C, Romero S, et al. Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res. 2017;26(7):1915–1924.
- Wallston KA. The validity of the multidimensional health locus of control scales. J Health Psychol. 2005;10(5):623–631.
- Estrada-Bellmann I, Meléndez-Flores JD, Cámara-Lemarroy CR, et al. Determinants of self-efficacy in patients with Parkinson’s disease. Arq Neuropsiquiatr. 2021;79(8):686–691.
- Shulman LM, Velozo C, Romero S, et al. Comparative study of PROMIS self-efficacy for managing chronic conditions across chronic neurologic disorders. Qual Life Res. 2019;28(7):1893–1901.
- Nilsson MH, Hagell P, Iwarsson S. Psychometric properties of the general Self-Efficacy scale in Parkinson’s disease. Acta Neurol Scand. 2015;132(2):89–96.
- Pagnini F, Bercovitz K, Langer E. Perceived control and mindfulness: implications for clinical practice. J Psychother Integr. 2016;26(2):91–102.
- Prinsen CAC, Vohra S, Rose MR, et al. Core Outcome measures in effectiveness trials (COMET) initiative: protocol for an international delphi study to achieve consensus on how to select outcome measurement instruments for outcomes included in a “core outcome set. Trials. 2014;15(1):1–7.
- Nowell LS, Norris JM, White DE, et al. Thematic Analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16:1–13.
- Zarotti N, Dale M, Eccles F, et al. Psychological Interventions for people with huntington’s disease: a call to arms. JHD. 2020;9(3):231–243.
- Zarotti N, Mayberry E, Ovaska-Stafford N, et al. Psychological interventions for people with motor neuron disease: a scoping review. Amyotroph Lateral Scler Front Degener. 2021;22(1-2):1–11.
- Simpson J, Eccles FJ, Zarotti N. Extended evidence-based guidance on psychological interventions for psychological difficulties in individuals with Huntington’s disease, Parkinson’s disease, motor neurone disease, and multiple sclerosis 2021. https://zenodo.org/record/4593883#.YdNTgy-l2DU
- Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–156.
- Teasdale JD, Segal ZV, Williams JMG, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–623.
- Cheng C, Cheung SF, Chio JHM, et al. Cultural meaning of perceived control: a meta-analysis of locus of control and psychological symptoms across 18 cultural regions. Psychol Bull. 2013;139(1):152–188.
- Grob A, Little TD, Wanner B, Euronet, et al. Adolescents’ well-being and perceived control across 14 sociocultural contexts. J Pers Soc Psychol. 1996;71(4):785–795.
- Beck AT. Cognitive therapy: Nature and relation to behavior therapy. Behav Ther. 1970;1(2):184–200.
- Hofmann SG, Asnaani A, Vonk IJJ, et al. Efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427–440.
- Wilson BA, Winegardner J, van Heugten CM, et al. Neuropsychological rehabilitation: the international handbook. New York (NY): Psychology Press; 2017.
- Walsh J. Psychoeducation in mental health. Oxford: Oxford Unversity Press; 2010.
- Larsen MH, Mengshoel AM, Andersen MH, et al. “A bit of everything”: health literacy interventions in chronic conditions – a systematic review. Patient Educ Couns. 2022;105(10):2999–3016.
- Macht M, Gerlich C, Ellgring H, et al. Patient education in Parkinson’s disease: formative evaluation of a standardized programme in seven european countries. Patient Educ Couns. 2007;65(2):245–252.
- Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11(3):230–241.
- Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York (NY): Delta; 1990.
- Biddle S, Mutrie N. Psychology of physical activity: determinants, Well-Being and interventions. New York (NY): Routledge; 2007. https://www.taylorfrancis.com/books/9781134211937
- Bognar S, DeFaria AM, O’Dwyer C, et al. More than just dancing: experiences of people with Parkinson’s disease in a therapeutic dance program. Disabil Rehabil. 2017;39(11):1073–1078.

