Abstract
Purpose
The aim of this study was to explore factors that influence stroke survivors’ ability to persevere with home-based upper limb practice.
Methods
A qualitative descriptive study embedded within a theoretical framework was conducted. Data were collected through semi-structured focus group, dyadic, and individual interviews. The Theoretical Domains Framework and Capability, Opportunity, Motivation – Behaviour (COM-B) model guided data collection and directed content analysis.
Findings
Participants were 31 adult stroke survivors with upper limb impairment, with 13 significant other/s, who were living at home in Queensland, Australia. Three central tenants aligned with the COM-B and six themes were identified. Stroke survivors’ capability to persevere was influenced by being physically able to practice and being able to understand, monitor and modify practice, their opportunity to persevere was influenced by accessing therapy and equipment required for practice and fitting practice into everyday life, and their motivation to persevere was influenced by having goals and experiencing meaningful outcomes and having support and being accountable.
Conclusion
Persevering with practice is multifaceted for stroke survivors. All facets need to be addressed in the design of strategies to enhance stroke survivors’ ability to persevere and in turn, enhance their potential for continued upper limb recovery.
Many stroke survivors do not persevere with long-term home-based upper limb practice despite the belief that high dose practice will promote continued recovery.
Therapists need to support stroke survivors to setup individualised goal-based home programs that they can complete independently, or with support, within their everyday life.
Stroke survivors need coaching to monitor and modify their practice and map their progress, so that they can recognise and experience meaningful recovery.
To optimise upper limb recovery after stroke, strategies to enhance stroke survivors’ capability, opportunity, and motivation to persevere across the continuum of recovery, need to be co-designed by stroke survivors, therapists and researchers.
IMPLICATIONS FOR REHABILITATION
Keywords:
Introduction
Upper limb recovery after stroke is often a challenging and lifelong journey [Citation1]. Approximately 40% of stroke survivors experience upper limb weakness early after stroke [Citation2]. Compelling evidence indicates that high dose, task-specific practice reduces motor impairment and improves activity and participation in all phases of recovery [Citation3,Citation4]. Furthermore, advances in stroke treatment and models of care (e.g., specialised stroke units) have resulted in an overall decrease in post-stroke morbidity [Citation5]. Despite this, stroke survivors still have a high prevalence of long-term physical unmet needs [Citation6], and perceive difficulty accessing follow-up services [Citation7]. Consequently, stroke survivors are increasingly expected to manage practice independently in their home environment [Citation8] and find “getting going and keeping going” with practice challenging [Citation1]. As upper limb recovery can extend for years post-stroke [Citation9], enabling perseverance with home-based upper limb practice is paramount.
Stroke survivors believe that high dose practice will enhance recovery [Citation1]. Yet, their adherence to home-based practice is often low [Citation10,Citation11] and continued practice long-term is uncommon [Citation1]. For instance, only 28% of stroke survivors report continuing with home-based practice at seven months post-stroke [Citation12]. The ability to persevere is critical for commitment to long-term practice [Citation13] and stroke survivors recognise that persevering is key to achieving meaningful recovery [Citation14].
Adhering to home-based practice from the stroke survivors’ perspective has been considered in a small number of studies [Citation1,Citation11,Citation15,Citation16], yet few directly address upper limb practice. Therefore, the aim of this study was to identify factors that influence perseverance with home-based upper limb practice from the perspective of stroke survivors and their significant others.
Methods
Study design
A qualitative descriptive approach embedded within a theoretical framework and a pragmatic worldview underpinned this study. A qualitative descriptive approach is defined as a low inference methodological approach that aims to produce an account of a phenomenon or experience in everyday terms [Citation17,Citation18]. This approach was chosen because it enabled exploration of stroke survivors’ experiences of persevering with home-based upper limb practice in a naturalistic setting [Citation17,Citation18]. Recognising perseverance as a behaviour, the Theoretical Domains Framework (TDF) [Citation19] and the Capability, Opportunity, Motivation – Behaviour (COM-B) model [Citation19] were used to guide data collection and analysis. The TDF and COM-B are routinely used in combination as a framework for understanding behaviour and mediators of behaviour change, and to investigate and address issues with implementation [Citation19]. The COM-B has three central tenants (capability, opportunity and motivation) [Citation19] and the TDF has 14 theoretical domains (e.g., knowledge, skills, professional role and identity, beliefs about capabilities, optimism, etc.) [Citation19]. Situating the research within a pragmatic worldview allowed for exploration of real-world practice-based knowledge to solve problems concerned with what works for whom, and why [Citation20].
Reflexivity statement
The research team consisted of five experienced physiotherapists with expertise in neurological rehabilitation (BN, MS, SJ, RB, KH) and a rehabilitation consultant physician (PC). Two of the physiotherapists (RB, KH) had extensive research and clinical experience in the field of upper limb recovery post-stroke. Five members of the research team had qualitative research experience (BN, MS, SJ, RB, KH), two of whom had extensive experience (RB, KH). Five participants were known to the principal investigator (BN) and rehabilitation consultant (PC), as they completed their rehabilitation in the unit where both worked clinically.
The Townsville Hospital and Health Service Human Research Ethics Committee granted state-wide ethical approval for this research (HREC/2018/QTHS/47495). Ethical approval was acknowledged by James Cook University (H76780). All participants (stroke survivors and significant others) provided verbal and written informed consent.
Setting
This study was conducted in Queensland, Australia. Queensland is home to approximately 88,000 stroke survivors, with 5,371 hospital admissions for stroke in 2020 [Citation21]. The majority of Queensland-based stroke survivors are male (55%) [Citation21], 70 years of age or older (58%) [Citation21] and live in a non-metropolitan area (53%) [Citation22] with limited rehabilitation services.
Participants
Stroke survivors were eligible to participate if they: (1) were ≥18 years of age; (2) had been living at home in Queensland for at least one month post-stroke; (3) had self-reported upper limb disability resulting from stroke; (4) were able to communicate (verbally, written, or with augmented communication devices), or had a significant other who was able to facilitate communication; and (5) were able to provide informed consent. Those who had a pre-stroke neurological disability that affected their upper limb function (e.g., polio or Parkinson’s disease) were excluded. At the stroke participant’s discretion, significant others were eligible to participate if they were: (1) ≥18 years of age; (2) able to communicate; and (3) able to provide informed consent. A ‘significant other’ refers to any person that was invited by a stroke participant to accompany them during the interview. This covered a partner, family member or friend and was not defined a priori. Significant others were included as they may offer critical insights about stroke survivors’ experiences with perseverance, thereby providing a broader perspective than that of the stroke survivor alone. While stroke survivors were the focus of interviews, significant others could provide support, clarification and extension of viewpoints, or a different perspective on the stroke survivor’s experience. Stroke survivors’ and significant others’ viewpoints were both considered to be rich in value; therefore, both were considered without differentiation.
Recruitment flyers were distributed through agencies relevant to stroke survivors (e.g., the Stroke Foundation, stroke support groups, and outpatient rehabilitation facilities), on community notice boards, and via social media (e.g., Facebook and Twitter). Recruitment also occurred through word-of-mouth and snowballing. Those interested in participating contacted the principal investigator (BN) for further information.
Data collection
The principal investigator (BN) with co-researchers (RB, KH, PC) developed a topic guide consisting of open-ended questions and prompts. Open-ended questions were intentionally broad to explore participants’ experiences of persevering with home-based upper limb practice (). Prompts were structured according to the COM-B and TDF for in-depth exploration of factors that mediate perseverance. Stroke survivors were asked questions according to the topic guide. Significant others provided clarification and supporting information.
Table 1. Individual, dyadic and focus group interview guide.
Data were collected via semi-structured individual, dyadic, and focus group interviews; conducted in a community setting, participant’s homes, or via videoconference. Focus group and dyadic interviews were chosen to engage multiple participants in a conversational setting, providing researchers with the opportunity to explore and clarify experiences. Individual interviews were chosen so participants could provide an individual and in-depth account of their experience, not influenced by group context. Furthermore, individual interviews offered an avenue for researchers to explore and challenge minimally discussed points. Each participant’s interview type and setting were guided by their personal preference. Stroke participants and their significant others were interviewed together. The principal investigator (BN) initially collected demographic information (e.g., age, home location, self-reported severity of upper limb disability, time since stroke etc.) and engaged in rapport building conversations with participants, then facilitated all interviews. Toward the end of each interview, BN summarised the main points and gave participants an opportunity to clarify or expand on these points. A co-researcher (MS or SJ) observed focus group interviews and recorded field notes. Interviews were voice recorded and transcribed verbatim by a professional transcription service.
Following each interview, the facilitator (BN) ± observer (MS or SJ) reflected on the dominant ideas and viewpoints expressed by participants and recorded notes regarding preliminary themes. Using an iterative approach, monthly discussions between the research team (BN, RB, KH, MS, PC) were used to revisit, review, refine and explore the relationship between preliminary themes. Researchers aimed for pragmatic saturation to ensure the relevance of the study findings to a broader social and geographical context [Citation23]. Interview transcriptions and researcher reflections were included as data.
Data analysis
Demographic data were analysed descriptively using Microsoft Excel. Qualitative data were analysed via directed content analysis [Citation24,Citation25] using NVivo software (QSR International’s NVivo 12). To identify factors that influenced perseverance, BN deductively coded ten interview transcripts to the TDF domains and mapped the domains to the three central tenants of the COM-B [Citation19]. Then to describe factors that influenced perseverance within each of the central tenants, ideas and viewpoints that dominated were gathered into six themes and refined through discussion with the research team (BN, KH, RB). These six themes were then used to code all interview transcripts, 10% of which were independently verified by a co-researcher (MS) with follow-up discussion to resolve any conflicting viewpoints. Member checking was conducted with five participants to reflect, revise, and confirm themes. Participants for member checking were chosen to reflect the variation within the sample (e.g., did/did not persevere, mild/severe impairment, metropolitan/rural and remote etc.). Of the five member checks conducted, two stroke participants and a significant other were previously known to the team.
Findings
Forty-four participants (31 stroke survivors and 13 significant others) were recruited (). Each participant’s stroke journey was highly personal, therefore many chose to tell their story in an individual or dyadic interview rather than a focus group. The average interview duration was 54 min (range 22–125 min).
Figure 1. Flow of participants: Participant recruitment, eligibility, and interview type selection.
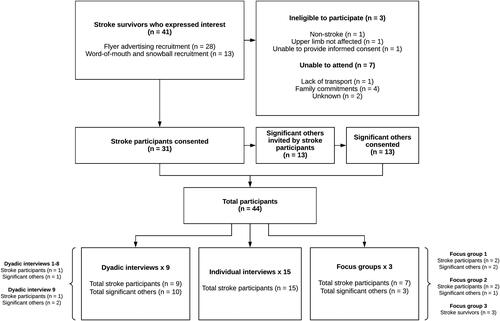
Stroke participants () were both male and female (17:14) aged from 22–78 years. The majority were non-indigenous Australians, living in rural or remote Queensland with a severely affected upper limb in the chronic phase of recovery, and considered themselves to have persevered with practice. Significant others () were both male and female, typically the participant’s spouse and on one occasion, their parents.
Table 2. Characteristics of stroke survivors.
Table 3. Characteristics of significant others.
Deductive analysis demonstrated that the three central tenants of the COM-B (capability, opportunity and motivation) were evident within the data. Inductive analysis identified six themes () which are described below with supporting quotes. Capability, opportunity and motivation were essential for all participants to persevere. The importance of each theme, and the degree to which the themes overlapped to enable perseverance, was different between individuals, and for each individual over time.
Figure 2. Perseverance with home-based upper limb practice (adapted from Mitchie et al. 2014 [Citation19]).
![Figure 2. Perseverance with home-based upper limb practice (adapted from Mitchie et al. 2014 [Citation19]).](/cms/asset/7976b2af-ea70-4432-b68f-a2e02e866da2/idre_a_2191011_f0002_b.jpg)
Capability to persevere
Participants felt their capability to persevere was influenced by being physically able to practice and being able to understand, monitor and modify practice.
Being physically able to practice
Participants felt their physical ability to practice was dependent on how severely their arm was affected (e.g., weakness, sensation loss, ataxia). Persevering with practice was more difficult for those with severe impairment as attempts at moving their affected arm were often physically exhausting and painful.
Well, the arm is just painful. It wears one down after a while. I don’t know, just moving it. To be quite honest it’s as though I’ve got a ton of concrete in my arm…when every day’s the same you think, bugger. (Stroke Survivor: 70, severe, chronic)
Despite this, some participants with severe impairment found ways to persevere. Some practiced independently through self-stretching or using equipment that provided physical assistance. One participant went to the pool as he found that the water buoyancy allowed him to move his arm more easily, while another set up a pulley system in his home. Some relied on their significant other to provide physical assistance for practice (e.g., moving their arm during an exercise or stretching regime). Participants expressed sadness and frustration when they did not have enough movement to be able to practice by using their arm in everyday tasks.
I persevere until it drives me off my head trying to do the little bits and pieces and I give it away…I just find frustration sets in when I’m trying to do [tasks] with two hands. (Stroke Survivor: 78, severe, chronic)
In contrast, participants with mild to moderate impairment reported persevering independently by involving their arm in everyday tasks. To avoid frustration related to failed practice attempts, they used a range of strategies, such as, rest periods, swapping tasks, or using assistive devices to aid in task performance (e.g., splints to control movement, joystick to control a game rather than a keyboard).
Like if my hand is starting to cramp and get slow, and I’m getting frustrated, changing [the task] or giving [my arm] a bit of a break for a bit and then coming back and then persevering again. That increases my success rate of doing things, rather than just throwing the towel in. (Stroke Survivor: 34, mild, chronic)
Participants were aware that they had to practice a lot, and repetitively to improve. Practicing a lot could be not only physically challenging but also mentally draining.
You can’t just go, yeah, I’ve done enough today, should be right. It’s got to be really consistent. You’ve got to push hard and it’s just tiring. It’s a really long hard slog of tiny, miniscule wins that sometimes are imperceptible. (Stroke Survivor: 49, severe, chronic)
Being able to understand, monitor and modify practice
Participants emphasised the need to understand what they needed to practice, and to acquire skills to modify practice and monitor its effects. In this regard, upper limb therapy was perceived to be neglected in the hospital and home setting.
The neglect of the treatment of the arm is what’s outstanding, the neglect of it…there’s just no advice. None. (Significant Other: 71, spouse [Stroke Survivor: 72, severe, chronic])
Many felt that they did not acquire the skills to independently drive practice and needed further direction.
I was wanting to get in and start doing some … start improving tomorrow, today, this afternoon, before I go to bed. Yeah. And I had no direction, I didn’t know what I was supposed to be doing. (Stroke Survivor: 70, mild, late subacute)
Others tried to work it out for themselves, seeking to improve their knowledge by discussing practice strategies with their support networks. They also utilised Stroke Foundation resources and researched stroke recovery to improve their knowledge. Some participants felt that understanding neuroplasticity and what practice would promote neuroplasticity, helped them to persevere. Others feared that their arm would take too long to recover, or that recovery may be incomplete or not happen at all, which led to difficulty persevering.
Participants felt while progress was a powerful driver for persevering, recovery was often “slow” and “minute”, making it challenging to track progress over time.
It’s just the fact that you don’t know if you’re improving or not. I mean, if I could open my hand right now, I’d know, well, I’m improving. But when, you know, you’re moving it just fractionally, sometimes you don’t know if your mind’s playing games with you or what. (Stroke Survivor: 59, severe, chronic)
In this situation, participants thought that having a skilled therapist to monitor, provide feedback, and upgrade their exercise program could have helped them persevere.
Opportunity to persevere
Participants felt the opportunity to persevere was influenced by accessing therapy and equipment for practice and fitting practice into everyday life.
Accessing therapy and equipment required for practice
To enhance practice opportunities, participants felt they needed access to therapy and equipment. Stroke specific therapy was highly valued because it offered access to skilled therapists and appropriate equipment for practice. Access to no-cost or government-funded therapy was generally infrequent (once/week) and time limited. A few participants engaged in regular self-funded therapy (once-twice/week), while the majority found it too costly. Many participants in rural and remote locations found it extremely challenging or impossible to participate in any therapy because of access issues (e.g., distance, travel time, therapist turnover). Having access to skilled therapists who provided effective, challenging but achievable programs, was perceived to help them persevere.
Many participants felt that the transition from therapist-led to self-directed rehabilitation happened prematurely, and they did not always feel included in the decision. Transition appeared to happen because therapists believed participants either were not progressing enough, or were functioning well enough to manage without further therapy.
I only had about … I think I had two [therapy] sessions… And they basically said, well there’s nothing that we can do with you, you’re fine now, you can go. But I said, ‘But I’m not fine, I’m not fine!’ (Stroke Survivor: 70, mild, late subacute)
Some participants were prescribed home-based practice, while others received no direction at all. When prescribed, practice routines were frequently labelled as “boring” and “repetitive” or inappropriate, especially when exercises were too difficult to complete independently, were lacking variability, or were not helpful in the context of participants’ everyday life. Participants also reported lacking direction about how to progress their practice, or how long to keep practicing for, and felt that they would have benefited from further follow-up. Those who were provided with personalised practice and access to appropriate therapist follow-up found it easier to persevere.
I basically had myself a three-hour program that I did every single day. And then when the [therapists] visited that was on top of [the exercise program] so I’d combine all the exercises I’d learned from them plus trying to get a bit of cardio in. (Stroke Survivor: 38, mild, chronic)
Many participants who were several years post-stroke no longer accessed therapy, despite still wanting to recover more. Some preferred to be self-directed in their practice, or were unsure if further therapy would be beneficial, while others had difficulty understanding their therapy entitlements. Some were frustrated by their lack of recovery and sought out alternatives to traditional rehabilitation. Some tried massage, Botox, personal training, or Pilates where others tried Bowen Therapy, Reiki, Chiropractic intervention, and Naturopathy.
Participants reported using a variety of equipment to help them practice, generally off the shelf, low-cost items in line with what they had used in hospital (e.g., functional electrical stimulation, mobile phone applications). While some were aware of more advanced rehabilitation equipment (e.g., robotics, immersive reality), none used it due to high cost or an inability to purchase the equipment in Australia. Most found persevering easier if they were using equipment relevant to their everyday life.
Fitting practice into everyday life
Participants emphasised that to persevere, practice had to fit into their everyday life. Most who did structured practice preferred to have a routine, scheduling and dedicating time to practice to reinforce the habit. Others dual-tasked (e.g., practicing while watching the news) to fit practice into their day. A few participants enjoyed the flexibility of setting a time to practice based on other events happening that day.
Really scheduling my exercise, really scheduled in and allowing nothing to get in the way. Put it on par with, you know, face washing, having breakfast, getting dressed, cleaning teeth. (Stroke Survivor: 68, mild, chronic)
Many participants were not doing structured home-based practice. Instead, they described making a conscious effort to seek out practice opportunities within their everyday life, involving their arm in daily tasks and hobbies.
I don’t specifically sit down and do a rehab program at home, where I’ll go and do meaningless menial tasks, like putting pegs on a piece of wood, and then taking them back. I don’t do that sort of rehab anymore. I do real-life rehab. So like pegging out clothes, making sandwiches, sweeping the floor, brushing my teeth. Just real like normal things, helping tidy things up, wiping benches, doing washing. Normal tasks. (Stroke Survivor: 34, mild, chronic)
Others reported frequent self-stretching throughout the day. Interestingly, participants did not always view integrating their arm use in everyday life as practice.
I thought right from the onset I can either go ten years of flogging myself working hard exercising to gain full use of my limbs. Or I could take twenty years and just do it slowly in amongst my daily routine and enjoy myself doing what I do. (Stroke Survivor: 67, severe, chronic)
A couple of participants found that persevering was easier when it was conducted away from the home (e.g., gym, Pilates studio), because they had to book and pay for a session in advance. This meant time for these sessions was dedicated and protected.
Motivation to persevere
Participants’ motivation to persevere was influenced by having goals and experiencing outcomes, and having support and being accountable.
Having goals and experiencing outcomes
Participants reported that having goals that were intricately linked to who they were (e.g., their beliefs, values, or culture) and the things that mattered to them (e.g., their relationships, hobbies, and occupation), drove perseverance. While many had a vision of being able to use their arm and hand again like they used to, most broke down their goals into smaller steps that were realistic and achievable. Interestingly, few participants reported setting formal goals either with a health professional or independently. Still, having goals and a vision for recovery were not enough alone to persevere long-term; they needed to see meaningful progress.
The biggest thing was the changes I could see. I’d do something I couldn’t do last week, or I couldn’t do yesterday. And that just gave me the strength to keep going because I could see that change. (Stroke Survivor: 38, mild, chronic)
Participants spoke about even small flickers of muscle activity spurring them on early post-stroke, however as time went on, their ability to complete everyday tasks and hobbies became more important. When they could not complete everyday tasks, they tended not to recognise their progress, nor find it meaningful enough to drive perseverance.
I get a bit over doing upper limb exercises just because of the lack of improvement in function…it makes me less likely to practice. If I got it right or if I saw improvement than that would probably motivate me to keep going. (Stroke Survivor: 47, mild-moderate, chronic)
When progress was lacking, practice was considered not worth the time and effort, leaving them feeling disheartened. Not being able to monitor their own progress effectively, meant that some participants completely abandoned practice.
I think some of the reasons why I’ve stopped is that recovery is very slow… those exercises are just so tedious and so long and then you don’t get any recovery out of it. (Stroke Survivor: 36, severe, chronic)
While participants who had little to no arm recovery often stopped ‘practicing’, many continued with self-stretching to keep their arm and hand loose and minimise functional loss. Others were devastated by therapists telling them that their arm and hand would never recover, destroying their motivation to persevere.
The first physio that we visited said to me…no, no, no, we’re not going to look at your arm because it’s never coming back. When this woman said to me, your arm’s never coming back, it sank in somewhere. And I resent her having said that to me because it’s something that stuck with me all these years, that my arm’s never coming back. (Stroke Survivor: 49, severe, chronic)
For some participants, fear of getting worse was a stronger motivator for persevering than progressing. Participants reported being noticeably worse after a period of not practicing, which negatively affected their mood, relationships and occupations.
If I don’t keep up with a rehab style approach to living my life, I notice that things sort of fall apart in that space… everything goes backwards. It ends up being this vicious cycle where you end up spiralling out of control. It affects the things that I need to do [work/home duties], and my relationships with people. (Stroke Survivor: 34, mild, chronic)
For some participants, arm and hand dysfunction was a new normal. While many stopped practicing, they still hoped for recovery. Others persevered because they strongly rejected the stigma and pity associated with being disabled.
I’m doing it, I persevere, and I practice so hard out of, purely out of self-interest. It’s because I want to be able to do things, and I don’t want people to treat me as a cripple, as a disabled person, yeah…. I want to be regarded as a normally functioning person. Treated as normal. (Stroke Survivor: 70, mild, late subacute)
Participants who had more function found it easier to set goals and gauge their progress when completing everyday tasks and hobbies, which ultimately helped them to persevere.
Having support and being accountable
Support from family, friends and therapists helped participants maintain the motivation to persevere. This support could mean physically assisting them or providing them with equipment for practice, or encouraging them by recognising their progress.
I’ve got great support as you see. My friends bought me the things to do the braiding. And [my husband] has made me equipment and stuff. I’ve got a good little community here. (Stroke Survivor: 49, moderate, chronic)
Being accountable drove participants to persevere, particularly to therapists for the amount and accuracy of their practice, and the progress achieved.
They [therapists] were important to keep me going because you’re answerable to somebody and you’re wasting their time if you’re not doing anything. (Stroke Survivor: 67, severe, chronic)
Family and friends rarely held participants to account for practice completed. They believed it was the therapist’s role and feared it could negatively impact their relationship with the participant.
I purposely did not hold them accountable. They were doing Physio and Occupational Therapy and everything else. I didn’t want them to feel that the exercises had to be done before I got home. The last thing they needed was another sergeant major. (Significant Other: 53, spouse [Stroke Survivor: 49, moderate, chronic])
Still, participants felt a responsibility to show up, work hard, and be a role model; persevering so that they could be involved in activities that were important to family and friends.
Many participants felt accountable to themselves and responsible for their own practice. Persevering was part of their identity (e.g., pre-stroke occupation, habits, values and beliefs) – they held the belief that you get out what you put in, and you need to commit to long-term hard work to see results.
I would say recovery is just, it’s a grind. And I don’t like practicing every day. But you just have to keep on keeping on, and sort of make the best of a bad situation. And I’ve resigned to the fact that it will be something that I have to work on every day for the rest of my life. (Stroke Survivor: 34, mild, chronic)
Discussion
The purpose of this study was to learn from stroke survivors about factors that influence their ability to persevere with home-based upper limb practice. Findings revealed that stroke survivors’ capability to persevere was influenced by the extent to which they have the physical ability to practice and are able to understand, monitor and modify practice. Their opportunity to persevere was influenced by their access to therapy and equipment required for practice and being able to fit practice into their everyday life. Their motivation to persevere was influenced by being accountable to, and supported by, therapists, family, and friends; and the extent to which their practice activities aligned with their goals and allowed them to experience meaningful outcomes. These factors are important for therapists and researchers to consider when designing strategies to enhance stroke survivors’ ability to persevere with practice long-term.
This is a novel investigation of persevering with home-based upper limb practice outside of a trial context. Interestingly, findings were similar to those identified to promote adherence to short-term upper limb practice interventions [Citation28,Citation29] and long-term maintenance of physical activity [Citation16,Citation30,Citation31] within stroke trials. For instance, being physically able to practice was integral; if practice became too challenging participants would either cease practice, or rely on family members to assist [Citation16,Citation28]. Access to therapists and equipment for practice was imperative for long-term adherence [Citation16,Citation28–31], with participants relying on therapists to monitor and modify their practice and feeling accountable to them for the amount practice completed and their progress [Citation16,Citation28–31]. Working on personalised goals that allowed participants to see meaningful progress and implementing a routine to fit practice into everyday life were key to enhancing both motivation and practice opportunities [Citation16,Citation28–31]. Given that perseverance with practice may improve recovery after stroke, findings from this study combined with previous studies, indicate that stroke rehabilitation services have a role in ensuring that stroke survivors have the capability, opportunity, and motivation to persevere with practice once they return home.
Participants in this current study reported losing motivation to persevere when they could not see meaningful progress. They felt they needed access to therapists to prescribe and monitor their practice and provide them with feedback on their progress, yet this was rarely available. In contrast, in a previous stroke trial, despite not seeing meaningful progress, participants remained motivated to practice because of their hope for recovery and not wanting to “give up” part-way through the trial [Citation28]. This could reflect the opportunity that a stroke trial provides for stroke survivors to engage with therapists who prescribe and monitor their progress, in keeping with the requirements for persevering with practice. Furthermore, participation in research can be viewed by stroke survivors as an opportunity to try new rehabilitation programs [Citation32], which may increase their motivation to practice. It is reasonable to speculate that to persevere with practice outside of a trial context, many stroke survivors will need access to therapists who can coach them to identify goals that matter to them, co-design practice options with them, and support them to monitor and progress their practice.
The reality for stroke survivors is that upper limb recovery can be minimal and slow but can continue to improve spontaneously to at least two years after stroke [Citation9]. Recognising this long window of opportunity, optimising recovery means practicing throughout their recovery journey. Yet, many participants in this study felt that their arm and hand were neglected across the recovery continuum, and reported receiving little training or ongoing support to help them persevere with practice in their home without a therapist present. Certainly, this picture of neglect fits with other studies that have reported low volumes and intensity of upper limb therapy post-stroke [Citation33,Citation34]. As with previous studies, participants reported that even when prescribed, exercises were often generic, boring, and repetitive [Citation16,Citation35]. Furthermore, they were rarely taught how to monitor and progress their own practice, despite research demonstrating that adherence to practice is better when stroke survivors have the required skills, knowledge, and support for practice [Citation1,Citation8,Citation16,Citation33,Citation36]. This study highlights the importance stroke survivors place on receiving appropriately timed education, support and training that is relevant to their daily occupations. Therefore, knowing that persevering with practice is important for optimising long-term recovery, it is vital that strategies to enhance perseverance with practice are embedded within stroke rehabilitation guidelines and practice early after stroke.
Clinical and research implications
Strategies that equip stroke survivors with the capability, opportunity and motivation to persevere need to be integrated into survivors’ routines from the commencement of rehabilitation. In particular, practice needs to align with survivors’ individual goals and produce outcomes that are meaningful within the context of their everyday lives. Future research could build on these findings by exploring the impact of personal (e.g., age, gender, degree of upper limb impairment etc.) and environmental (e.g., rurality, access to services etc.) factors on perseverance. Furthermore, access to long term support to monitor and progress practice needs to be integrated into service models. Further research is required to develop, implement, and evaluate coaching strategies, co-designed with stroke survivors and therapists, to enable stroke survivors to persevere. Ultimately, this will allow stroke survivors to optimise their upper limb recovery.
Strengths and limitations
A qualitative descriptive approach allowed for in-depth information to be collected from a large (n = 44) and diverse sample, providing important insights about stroke survivors’ experiences from different perspectives and in turn, potential transferability to many contexts and settings. The inclusion of significant others may have lessened recall bias where participants were a long-time post-stroke, or had difficulty remembering or articulating their experiences, allowing for a more complete picture. Generally, those interviewed individually shared an intensely personal and in-depth account of their experience. Participants interviewed with their significant other/s or in focus groups may have been reluctant to share such personal aspects of their experiences. Conversely, participants in focus group or dyadic interviews may have been more comfortable to share other aspects of their experience due to the conversational manner and comradery of shared experience. Ultimately, use of multiple interview methods and settings (e.g., home, community, videoconference) allowed for triangulation of data, compensating for limitations of each method, and exploiting respective benefits [Citation37]. Given that over half the study participants reported having severe upper limb impairment, the findings may be more reflective of the experience for those with severe, than for those with mild to moderate impairment. Despite researchers choosing a varied sample for member checking, it was conducted with a small proportion of total participants who can only comment on their individual experiences. Finally, participants known to researchers may have moderated their responses, or conversely, been more open in discussing their experiences as they felt it was a shared journey [Citation38].
Conclusion
Perseverance with practice after stroke is multifaceted. Participants reported needing the physical ability to practice, the ability to understand, monitor and modify practice and access to therapy and equipment. Furthermore, being able to participate in goal-directed, personalised practice that was integrated into their everyday life and produced meaningful outcomes was essential. All facets need to be addressed in the design and implementation of strategies to enhance stroke survivors’ ability to persevere with practice and in turn, optimise their upper limb recovery.
Acknowledgements
The research teams thank participants for providing valuable insights through sharing their respective experiences. The research team acknowledges the support provided by the James Cook University Murtupuni Centre for Rural and Remote Health, particularly Sarah Jackson (SJ) for her assistance as a focus group observer, and Leann Shaw for her cultural support and mentoring. The research teams acknowledge the assistance provided by individuals and organisations in advertising for recruitment to this study.
This study was supported by a Study, Education and Research Trust Fund Grant administered by Townsville University Hospital to PC, BN, RB, and KH. The views expressed in this publication do not necessarily represent those of the Townsville University Hospital, its Administrator, and/or Queensland Health. BN is supported by an Australian Government Research Training Program Scholarship administered by James Cook University. KH is supported by a National Health and Medical Research Council of Australia Fellowship [APP1088449].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
- Barker R, Brauer S. Upper limb recovery after stroke: the stroke survivors’ perspective. Disabil Rehabil. 2005;27(20):1213–1223.
- Simpson LA, Hayward KS, McPeake M, et al. Challenges of estimating accurate prevalence of arm weakness early after stroke. Neurorehabil Neural Repair. 2021;35(10):871–879.
- Grefkes C, Fink GR. Recovery from stroke: current concepts and future perspectives. Neurol Res Pract. 2020;2(1):1–10.
- Veerbeek JM, van Wegen E, van Peppen R, et al. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS One. 2014;9(2):e87987.
- Zhai S, Gardiner F, Neeman T, et al. The cost-effectiveness of a stroke unit in providing enhanced patient outcomes in an Australian teaching hospital. J Stroke Cerebrovasc Dis. 2017;26(10):2362–2368.
- Lin BL, Mei YX, Wang WN, et al. Unmet care needs of community-dwelling stroke survivors: a systematic review of quantitative studies. BMJ Open. 2021;11(4):e045560.
- Guo Y, Zhang Z, Lin B, et al. The unmet needs of community-dwelling stroke survivors: a systematic review of qualitative studies. Int J Environ Res Public Health. 2021;18(4):2140.
- Donoso Brown EV, Fichter R. Home programs for upper extremity recovery post-stroke: a survey of occupational therapy practitioners. Top Stroke Rehabil. 2017;24(8):573–578.
- Borschmann KN, Hayward KS. Recovery of upper limb function is greatest early after stroke but does continue to improve during the chronic phase: a two-year, observational study. Physiother. 2020;107:216–223.
- Emmerson KB, Harding KE, Taylor NF. Home exercise programmes supported by video and automated reminders compared with standard paper-based home exercise programmes in patients with stroke: a randomized controlled trial. Clin Rehabil. 2017;31(8):1068–1077.
- Miller KK, Porter RE, DeBaun-Sprague E, et al. Exercise after stroke: patient adherence and beliefs after discharge from rehabilitation. Top Stroke Rehabil. 2017;24(2):142–148.
- Mahmood A, Solomon JM, English C, et al. Measurement of adherence to home-based exercises among community-dwelling stroke survivors in India. Physiother Res Int. 2020;25(2):e1827.
- Dishman RK, Ickes W. Self-motivation and adherence to therapeutic exercise. J Behav Med. 1981;4(4):421–438.
- Jones F, Mandy A, Partridge C. Reasons for recovery after stroke: a perspective based on personal experience. Disabil Rehabil. 2008;30(7):507–516.
- Kåringen I, Dysvik E, Furnes B. The elderly stroke patient’s long-term adherence to physiotherapy home exercises. Adv Physiother. 2011;13(4):145–152.
- Mahmood A, Nayak P, Kok G, et al. Factors influencing adherence to home-based exercises among community-dwelling stroke survivors in India: a qualitative study. Eur J Physiother. 2021;23(1):48–54.
- Sullivan-Bolyai S, Bova C, Harper D. Developing and refining interventions in persons with health disparities: the use of qualitative description. Nurs Outlook. 2005;53(3):127–133.
- Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. HERD. 2016;9(4):16–25.
- Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. Great Britan: Silverback Publishing; 2014.
- Creswell JW, Poth CN. Qualitative inquiry and research design: choosing among five approaches. United States of America: Sage Publications; 2016.
- No postcode untouched Australia: Stroke Foundation. 2022. https://strokefoundation.org.au/What-we-do/Research/No-Postcode-Untouched
- Dwyer M, Francis K, Peterson GM, AuSCR Consortium, et al. Regional differences in the care and outcomes of acute stroke patients in Australia: an observational study using evidence from the Australian stroke clinical registry (AuSCR). BMJ Open. 2021;11(4):e040418.
- Low J. A pragmatic definition of the concept of theoretical saturation. Sociol Focus. 2019;52(2):131–139.
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115.
- Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Modified Monash Model Australia: Australian Government. 2019. https://www.health.gov.au/resources/apps-and-tools/health-workforce-locator/health-workforce-locator
- Bernhardt J, Hayward KS, Kwakkel G, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: the stroke recovery and rehabilitation roundtable taskforce. Int J Stroke. 2017;12(5):444–450.
- Levy T, Christie LJ, Killington M, et al. “Just that four letter word, hope”: stroke survivors’ perspectives of participation in an intensive upper limb exercise program; a qualitative exploration. Physiother Theory Pract. 2021;38(11):1624–1638.
- Kelly K, Brander F, Strawson A, et al. Pushing the limits of recovery in chronic stroke survivors: a descriptive qualitative study of users perceptions of the queen square upper limb neurorehabilitation programme. BMJ Open. 2020;10(10):e036481.
- Patterson S, Ross-Edwards B. Long-term stroke survivors’ needs and perceptions of an exercise maintenance model of care. Int J Ther Rehabil. 2009;16(12):659–669.
- Poltawski L, Boddy K, Forster A, et al. Motivators for uptake and maintenance of exercise: perceptions of long-term stroke survivors and implications for design of exercise programmes. Disabil Rehabil. 2015;37(9):795–801.
- Carlstedt E, Månsson Lexell E, Ståhl A, et al. Stroke survivors’ preferences regarding study participation in rehabilitation research. BMC Med Res Methodol. 2022;22(1):1–9.
- Hayward KS, Brauer SG. Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clin Rehabil. 2015;29(12):1234–1243.
- Lang CE, MacDonald JR, Reisman DS, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil. 2009;90(10):1692–1698.
- Neibling BA, Jackson SM, Hayward KS, et al. Perseverance with technology-facilitated home-based upper limb practice after stroke: a systematic mixed studies review. J Neuroeng Rehab. 2021;18(1):1–26.
- Olofsson A, Andersson S-O, Carlberg B. ‘If only I manage to get home I’ll get better’-Interviews with stroke patients after emergency stay in hospital on their experiences and needs. Clin Rehabil. 2005;19(4):433–440.
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. EFI. 2004;22(2):63–75.
- Mills J, Bonner A, Francis K. Adopting a constructivist approach to grounded theory: implications for research design. Int J Nurs Pract. 2006;12(1):8–13.

