Abstract
Background
Older patients with lower limb amputation, categorised as having “limited community mobility”, are under-researched. Understanding their experience with a new prosthetic ankle-foot is important when designing clinical trials. The aim of this qualitative study was to explore the adjustments they made after amputation and the acceptability of a self-aligning ankle-foot (SA-AF) to older adults.
Methods
Fourteen participants, who took part in the STEPFORWARD randomised controlled feasibility trial (ISRCTN15043643), were purposively recruited; nine were intervention participants and five were standard care participants. They were asked to reflect on their life prior to and consider the adjustments they made following their amputation. Participants in the intervention group were also asked about their views of the new SA-AF compared to their standard non-SA-AF. A thematic analysis was undertaken.
Results
Three broad themes were identified: The impact of the amputation; Role of clinical support; and Experiences of the SA-AF. The findings tell a narrative of the long-term impact that amputation has on these individuals’ lives. Participants randomised to receive the SA-AF were very positive about it, reporting less pain, greater mobility and being able to do more.
Conclusion
Participants who used the SA-AF found it an acceptable intervention. These findings suggest that a full-scale RCT is warranted.
IMPLICATIONS FOR REHABILITATION
There is a high degree of acceptability among an older patient group with a transtibial amputation to use a self-aligning ankle foot.
Patients reported experiencing better mobility and more prosthetic comfort with the self-aligning ankle-foot.
Key outcomes important to participants include engagement in social and daily activities and balance confidence.
Introduction
There are approximately 6000 new referrals to prosthetics services annually in the UK. The majority of amputations in the UK occur in adults over 50 years, at the transtibial (below-knee) level, and are caused by diabetes and/or peripheral vascular disease [Citation1–3]. Therefore, patients who are referred to prosthetics services are likely to be older and have a number of comorbidities which need to be managed alongside their amputation. For many people, their amputation is preceded by managing recurrent pain associated with their limb [Citation4]. Following amputation, postoperative complications and mortality are often reported [Citation5,Citation6]. The adjustment to becoming a prosthesis user should not be underestimated; the challenges can be multifaceted, including physical, psychological and social aspects [Citation3,Citation7]. The impact of an amputation affects a patient not only in terms of physical adjustment but also psychologically. Previous studies have identified themes that are important to this patient population, including changes to their self-identity [Citation8], new coping strategies [Citation9], changes to their physical image and the importance of social support [Citation10].
Many older people with a transtibial amputation are prescribed a standard prosthesis, such as the solid-ankle-cushioned-heel (SACH), uniaxial or multiaxial prosthetic ankle-foot. These types of prostheses are not able to self-adjust to different walking surfaces, such as stairs and slopes, which can make negotiating everyday environments difficult. This can also influence how much daily activity a person engages in while wearing their prosthesis and consequently affects their overall mobility. An alternative, commercially-available prosthetic ankle-foot is one which can self-align by adjusting to slopes due to its hydraulic-ankle articulation mechanism. Some self-aligning prosthetic ankle feet have been designed for users categorised as having ‘limited community mobility’ (K2 users), in order to overcome some of the limitations of the standard prosthesis. A self-aligning prosthetic ankle-foot has been found to help people walk more quickly [Citation11] and improve minimum ground clearance to avoid a fall [Citation12]. A number of self-aligning prosthetic ankle feet are available for prescription on the UK NHS (National Health Service), but they are not routinely prescribed for older adults with a transtibial amputation who have been categorised as having ‘limited mobility’.
There is a paucity of clinical trials with robust study designs to demonstrate the effectiveness of specific prosthetic components. A recent systematic review of randomised controlled trials (RCTs) assessing the effectiveness of prosthetic and orthotic interventions found only four studies investigated prosthetics, and these only focused on different socket systems, not on prosthetic ankle feet or knees [Citation13]. The British Society of Rehabilitation Medicine (BSRM) also noted that “there is an urgent need for controlled, prospective trials of the use and effectiveness of various prosthetic components and hardware in prescription” [Citation14]. In particular, trials are needed that involve patients who represent the majority of referrals to prosthetics services such as older patients with health multi-morbidities.
STEPFORWARD [Citation15,Citation16] was a feasibility trial designed to assess the acceptability of a self-aligning prosthetic ankle-foot to older adults with comorbidities and the feasibility of undertaking a full-scale RCT evaluating the self-aligning prosthesis. Participants were established standard prosthesis users, who were randomly allocated into an intervention (self-aligning) or standard treatment (existing, non-self-aligning) prosthetic ankle-foot group. The STEPFORWARD trial provided a unique opportunity to explore participants’ experiences of moving from a standard rigid prosthetic ankle-foot onto a self-aligning ankle-foot. To the best of our knowledge, no previous studies have reported on the experiences of people who received an alternative prosthesis. As such, this qualitative research aimed to explore trial participants’ reflections on adjusting to life after amputation and explored the acceptability of the self-aligning prosthetic ankle-foot, with a specific focus on daily life and functional activities.
Methods
Design
This was a qualitative study using audio-recorded semi-structured interviews. Interviews were undertaken with a total of 14 participants (nine self-aligning prosthesis users in the intervention group and five standard prosthesis users in the standard treatment group) who were purposively selected towards the end of their participation in the STEPFORWARD trial based on their age and gender to match the participants in the trial (Grant number: PB-PG-0816-20029; ISRCTN15043643). They were recruited from all five of the participating NHS sites across England (Hull, Nottingham, Preston, Portsmouth and Norwich). Details about the patient identification and recruitment process for the trial have already been published [Citation15,Citation16]. Adults with a non-traumatic unilateral, transtibial amputation, who were aged 50 years or older, and had been using a standard prosthetic ankle-foot for at least one year prior to study enrolment, were eligible to participate in the trial. Potential participants were initially identified by sites via two main methods: during a routine clinic visit or via screening of the clinic database. Those identified in the clinic were provided with an invitation pack during their visit, while those identified using the database were posted to the invitation pack. The packs provided information about the trial and patients, who were interested in taking part, were asked to complete and return a Consent to Contact form. There was a procedure in place to contact patients approximately two weeks after the expected receipt of the invitation pack to ensure each patient had the opportunity to participate in the trial if they wished. Once in receipt of the Consent to Contact form, a member of the patient’s routine multi-disciplinary team would contact the patient to complete the first section of the Screening Form over the telephone. Potentially eligible participants were then invited for a face-to-face screening visit, to complete the full screening process ensuring they met all the eligibility criteria. Eligible patients then consented, completed the baseline assessments, and were randomised.
Once participants were randomised to either the intervention (self-aligning prosthetic ankle-foot) or standard treatment (existing, non-self-aligning ankle-foot) group, they were followed up twice post-randomisation: interim (9 weeks) and final (16 weeks). Participants who had expressed interest in being interviewed were contacted by a member of the research team after their final follow-up. For those still interested, an interview invitation pack was sent out which included: an invitation letter, a participant information sheet about the interviews, and a consent form. A follow-up telephone call was made one week later and, if willing, they were asked to return a signed copy of the consent form and a date was arranged for the interview to take place. All interviews were carried out over the telephone and were audio recorded. Prior to commencing interviews, consent was verbally re-confirmed and participants were informed that they could stop the interview at any time. The trial received favourable ethical approval from the NHS Yorkshire and the Humber—Leeds West Research Ethics Committee (ref: 18/YH/0089) and Health Research Authority in May 2018.
Participants
The STEPFORWARD trial recruited 55 participants; of this 14 participants consented to be interviewed, which is 25% of the total sample recruited. Eleven participants, assigned to the intervention group, were invited to take part in an interview; ten of whom consented (all male). One declined due to other health problems. Nine participants assigned to the standard group were invited to take part; four (three male; one female) consented to be interviewed. Five declined - three due to ongoing health problems and two were not contactable after receipt of their consent form. The mean (SD) age was 69.1 (11.9) years (range 53–86 years) for the intervention participants and 65.7 (9.7) years (range 56–76 years) for the standard treatment participants. Nine of the participants were retired at the time of the interviews (n = 6 intervention; n = 3 standard treatment) and five participants were either self-employed or in paid employment (n = 3 intervention; n = 2 standard treatment). All participants were established prosthesis users.
Interviews
A topic guide was developed to cover background topics including the cause of amputation, general health and social situation. Participants were also asked about their experience of using their standard prosthetic ankle-foot prior to participating in the trial (“Can you describe how wearing a prosthesis has impacted on your daily life?”). The interviews also explored intervention participants’ views of their new self-aligning prosthetic ankle-foot, including the fitting, any learning and adjustments required to use it, and the impact of the prosthetic ankle-foot on their daily living (“Thinking about your previous prosthesis and the new self-aligning one, what do you like, or not like, about your prosthetic device?” Points to follow-up with a participant: how regularly they wore it, confidence in doing activities, activities they avoided). The topic guide was used flexibly in order to keep the natural flow of conversation during the interviews, enabling participants to openly discuss their experiences. The different topics covered in the topic guide were developed following consultation and discussion with the trial public involvement group and also from within the trial team in order to explore trial processes which would be needed to feed into a full trial. All interviews were carried out by NM. Interviews typically lasted between 45–60 min.
Analysis
The audio recordings were transcribed verbatim and imported into the program NVIVO (version 12). Thematic analysis was undertaken to search for common themes running through the conversations [Citation17]. Transcripts from the intervention and control groups were analysed together as the focus of this analysis was not a between-group comparison. Initial coding was undertaken deductively around the topic areas explored with the participants. Thirty per cent of transcripts were double-coded by NM and HL. These transcripts were compared and coding was refined until a consensus was reached. The rest of the transcripts were coded by NM. Following familiarisation and initial coding, code refinement was collaborative between NM and HL; the quotes in each code were re-read and the codes’ overall meaning was discussed. As coding and refinement progressed, the initial themes were refined, drawing on the experiences and narratives expressed in the interviews. Codes were removed, modified and added until they formed themes which told a coherent narrative of the data; this did not involve the exclusion of any interviews as there were instances where more than one code could be used for a particular section of the transcript.
Results
Three themes were identified (see ): The impact of the amputation; Role of clinical support; and Experiences of the self-aligning prosthesis.
Figure 1. Key themes identified in our analysis.
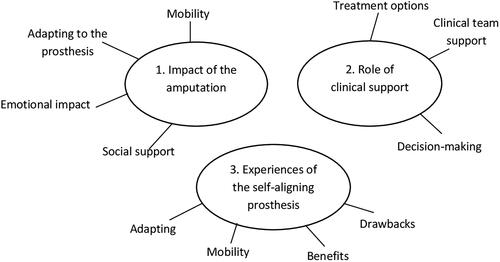
In this way, the findings tell a narrative of the long-term impact that amputation has had on these individuals’ lives. Specifically, we focus on how they adapted to their circumstances, their experience of using the self-aligning prosthesis, how they felt this benefitted them and any issues they encountered. The first two themes include intervention and standard participants, while the third theme only includes intervention participants.
Theme 1: the impact of the amputation (participants from the intervention and standard treatment groups)
Adapting to the prosthesis
A number of participants found it difficult to come to terms with the loss of their leg. However, they discussed how they were able to make adjustments to help them adapt to life following amputation. This was either by managing their own expectations of what they could achieve or by making practical changes to their daily routines. Physically, these included holding on to handrails for support, using a walking stick or resting their knee against something when standing up. Participants felt more reassured if they knew there was something to ‘catch’ onto if they felt they were about to fall.
“They’re [standard prosthesis] not good on uneven ground or grass. Obviously up and downstairs I definitely have to use a bannister. I still can’t go up or downstairs without using a bannister because how do I explain it? Weight transfer. Sometimes going downstairs if I’ve not got hold of the bannister I find it quite difficult to slow myself down, if you get what I mean and I don’t trust myself. I feel I would go over the top with the ankle.” P2111 (Male, 53 years, intervention group)
All participants had to make some level of adjustment following their amputation. For some this related to their outlook on their circumstances and, for the participants we interviewed, they managed this quite positively by embracing the change and identifying new ways of living. For example, one participant modified their electric scooter to enable them to move compost delivered for their garden and changed their garden into raised beds in order to continue with their love of gardening. However, participants also discussed that, if a situation could not be managed or adapted to adequately, they would avoid it together, acknowledging their own limitations rather than pushing themselves to the point of harm.
[Referring to walking up or down hills or steps] “I don’t if I can help it. If I can’t drive there I don’t go there mostly nowadays.” P1114 (Male, 59 years, control group)
Emotional impact
Many participants reported developing a fear of falling while using their standard prosthesis. For some, this fear lasted for quite a considerable length of time (or was still ongoing). This fear significantly impacted their confidence in carrying out everyday activities and therefore their overall mobility. This often led to them avoiding certain surfaces, routes or activities which would elicit this fear.
“It was good to get about; there’s always that fear of falling. I think almost a year after I got it I was more worried about falling over than walking on it.” P1104 (Male, 54 years, intervention group)
Participants also expressed a feeling of vulnerability; those who felt more vulnerable found it harder to adapt to using the prosthesis. This in turn impacted their ability to engage in their usual daily activities and adversely affected their mental well-being. One participant also talked about their expectation of benefits from having the amputation and how this was very different from the reality.
“Well I expected an artificial leg would be better than the leg I had but it was a bloody nightmare. I’ve been through 17 years of on and off problems, okay I’ve had some good times but I’ve had a lot of the same sort of thing as I got when I lost the artery, spasmodic pains for 24/30 hours until I got onto the Gabapentin and that’s three pills a day which destroys your nervous system, I think. Well having the leg chopped off destroys your sexual life. It’s quite a nightmare. It’s the worst nightmare to have, having it cut off.” P2113 (Male, 84 years, intervention group)
“Well you’re kind of vulnerable basically. You’ve got to remember that this happened to me when I was 60 losing the leg and, you know, you just feel vulnerable so all the time you’re watchful… Maybe I’m over emphasising it but that’s how it is for me anyway and so that’s how I feel. It certainly…it’s obviously limited my life, particularly as I’m on my own…” P2109 (Male, 75 years, intervention group)
Participants talked about the need to be independent and to do things for themselves. This is often related to self-care or being able to pick “themselves up off the ground” if they fell over. They all felt that they had two options: either be miserable or face the situation head-on with a positive attitude. Many opted for the latter option, stating that they just needed to get on with it.
“You know if I fell over, right, I’ve got to get myself up because nobody is going to lift you. They’re going to have to get the ambulance to come and lift you and all the rest of it, so you’ve got to be able to do all these things you see and I want to be independent, that’s the big thing.” P2109 (Male, 75 years, intervention group)
“I think I tried to avoid realising what had happened, that me leg had gone. It took me quite a while to realise that it had gone and it won’t be coming back…My answer to that was I either stay at home and be miserable or I get out and do what I can.” P1206 (Female, 72 years, control group)
“I’ve had a try at everything. There’s no use sitting down and being a couch potato all day.” P2105 (Male, 59 years, intervention group)
Social support
Social support could have both positive and negative aspects. Participants described how they turned to their social support network (family and friends) to discuss the prospect of having their foot amputated. Through this process, they recognised that the current and future management of their condition impacted not only their own health and well-being but also that of their social support network. Participants experienced support from their network in both emotional and practical ways.
“So, you know, I had a discussion with the family and said it’s not getting any better, so I made the decision to have it taken off. The family have been a big help. My dad and my brothers and my daughter.” P2111 (Male, 53 years, intervention group)
“It took a couple of months to learn how to do it but it’s like some of these shops they have gentle slopes going up into the shop or in our train station, I have to get me daughter behind me to push me up if I couldn’t push me-self up the slope and she helped me get up.” P2102 (Male, 66 years, intervention group)
Social activities and personal interactions with others were reported to be more limited after the amputation. This was mostly due to their inability to engage in their previous pastimes because of mobility or confidence issues; participants spoke of relationships breaking down as a result of their amputation.
“Well because you can’t really walk in the countryside and do the things that normal people do, your wife hates you and goes to find somebody who’s fully capable of doing everything they can do. It’s fairly normal. If you lose a limb you can lose your partner and when the difference in age was so great I had to agree with her.” P2113 (Male, 84 years, intervention group)
Mobility
Participants characterised their mobility according to the limitations of their prosthesis, in terms of what they were and were not able to do following their amputation and with the fitting of their standard prosthesis. Most participants did not report mobility improvements after having a prosthesis fitted following their amputation (for all participants this had been a standard prosthesis). Rather, they described how they sometimes felt unsteady on their feet or had problems with their balance; they felt this limited their movement and resulted in frequent trips and falls - some of which were serious, resulting in hospitalisation. Participants reported difficulties with using the standard prosthesis, specifically, they felt there was a difference in how they moved their non-amputated (sound) leg compared to the prosthesis and where they needed to apply pressure in order to mobilise their non-amputated (sound) leg. Another common issue for participants was that the prosthesis did not provide them with any feedback about their foot position, so they would not necessarily know if they were about to fall. Many had to rely on their eyesight to guide their walking which affected their mobility in terms of how confidently, easily and quickly they could move.
“It’s the balance as well that’s tricky. I kind of get no feedback from my feet in how I’m walking. Yeah I just have to rely on sight really to see whether I’m overbalancing or not.” (P1104) (Male, 54 years, intervention group)
“Err I can’t walk as far as I want to go. I can’t, you know, it’s very uncomfortable at times. It doesn’t hurt, it’s just uncomfortable. I’m not steady on me feet as such in the garden…you know, you don’t know you’re tripping over because you can’t feel nothing.” P1110 (Male, 76 years, control group)
Participants also described how the “type of ground” affected their stability, leading them to avoid certain routes and even certain activities altogether. In order to support their mobility they relied heavily on bannisters, walking aids and mobility scooters. Most had made adjustments by managing their expectations of what they could achieve including how they engaged with the world around them; or by making practical changes to their routines, such as ensuring they rested their leg. For some, they planned to go out as if they were on an expedition. They did this to manage both the practical aspects of being away from home and any anxiety they had about being somewhere unfamiliar.
“But you have to plan everything out is what I’m trying to say and everything from, you know, if you were going anywhere you would have to plan where the lavatory was and all this sort of thing, you know.” P2109 (Male, 75 years, intervention group)
“Well if I’d been out during the morning to do some shopping and that with my daughter, when I got home to relax it I used to take the leg off to relax me knee and my hip.” P2102 (Male, 66 years, intervention group)
The amputation and prosthesis frequently limited participants’ activities of daily living as well as their engagement in social and physical activities. It is important to note that although the prosthesis limited their ability to undertake activities, this was more likely a continuation of previous limitations rather than the onset of a new set of limitations, as many reported how their mobility had already been impacted by the deterioration of their leg prior to amputation. For some of the participants, their daily living and social activities were very restricted. This included the ability to go up slopes and stairs, which often contributed to them doing fewer jobs in the house and garden. Others reported that they were not able to get outside of their house. The cessation of previous physical activities such as hiking, walking, fishing, playing golf, playing football and running also took away the opportunity for social interaction and engagement.
“But the truth is social things I don’t really go to. I’m treasurer of a club. I do a bit of work and that but I don’t go to the meetings because it involves going up some stairs in an Indian restaurant which frankly I don’t feel very safe on…So, you know, it’s just sort of confined me in a way. I haven’t flown anywhere or anything like that, you know. So I’m sort of a bit confined to barracks. It’s probably me where I feel more comfortable.” P2109 (Male, 75 years, intervention group)
“I used to do a lot of long distance walking. Used to go for 2 or 3 weeks walking across the Moors, all over the place and now I can’t do that. That was me hobby gone.” P2102 (Male, 66 years, intervention group)
Positively, some individuals were able to return to previous physical pastimes, although this usually required re-learning movements, and managing the consequences of wearing a prosthesis such as pain, blisters on the residual limb and general stiffness and soreness.
“No, a couple of years [referring to time before being able to go back to playing] because with golf it is all pivot and movement…Yeah it was a good couple of years before I actually managed to hit a few balls. It’s the soreness. When it gets really sore. I mean I’ve played with blisters on the front which is when it happens you have to take the [prosthetic] leg off.” P2111 (Male, 53 years, intervention group)
A few participants identified some encouraging aspects of their amputation. In particular, one participant pushed themselves to walk further distances and felt proud of their achievement. Others described how they looked at other people with amputation with a sense of admiration and envy at what they were able to accomplish with their prosthesis.
“I mean I’ve talked to people I’ve met at the limb centre and some of them walk miles and, you know, they don’t find their leg, the artificial leg a problem.” P2113 (Male, 84 years, intervention group)
However, the amputation impacted some participants’ ability to engage in paid work, with two participants reporting that they had to stop working after they had their amputation.
“So moving about on, you know, crutches and the lifestyle I used to have was so restricting. I’ve only ever worked with me hands all me life [locksmith], so you know there’s such a lot that I just can’t do. But that’s, you’ve to meet things head on and work ways round it.” P2107 (Male, 62 years, intervention group)
“Obviously I don’t do outside playtime duties anymore [school caretaker]. I find it difficult during fire drills as well because we’ve got to walk out kind of 50 yards out and 50 yards back and that’s finished me for the day.” P1104 (Male, 54 years, intervention group)
Theme 2: Role of clinical support (participants from the intervention and standard treatment groups)
Decision-making
This sub-theme focuses on the time leading up to the participants’ amputation. The opinions among the participants varied with regard to how they were involved in decision-making about their amputation and treatment. Some participants felt very informed and involved in the process, whereas others believed they had no or only a little involvement or input into decisions as illustrated by P2103.
“They didn’t ask me. He said we’ve done all we can, he said we recommend what to do. He said if the poison [gangrene] gets any further you might have to have a double knee amputation. So I said if you do it now I can have a below the knee one? They said yes. So I gave them permission to take me leg off below the knee.” P2103 (Male, 86 years, intervention group)
Sometimes this lack of involvement was an active choice because they felt the clinicians had provided all the information and so they followed the course of action suggested. But for others, they acknowledged that at the time the clinician was speaking to them about treatment options, including amputation, they were either in too much pain or under the influence of medication to really listen and take any information on board meaningfully.
[Discussing the speed they were informed about an amputation] “Well best way I suppose if you think about it. It saves lingering on. I was doped up anyway. It didn’t make a lot of difference”. P1110 (Male, 76 years, control group)
None of the STEPFORWARD participants had their amputation under traumatic circumstances, e.g., following a road traffic accident, and they had all struggled with issues relating to their foot for a number of years prior. However, participants often described the circumstances leading to their amputation as one where there was limited time and the idea of amputation was suggested very late in the day. One participant (P1110) recounted how they only had three days between being admitted to the hospital for treatment on their leg and being informed that they needed to have an amputation. This meant some participants were not able to mentally prepare for the psychological and practical impact of the amputation.
“I felt that there wasn’t enough information given to me before I had the leg cut off. I don’t see that it stops the action but I would have liked to have been more aware of what I was up against, what I was heading into”. P2113 (Male, 84 years, intervention group)
One participant recounted how, although they had not felt prepared for their life as an amputee and the impact the operation would have on them, they had used their professional experience within the healthcare sector to aid their own decision-making. The clinician wanted to carry out a double (bilateral) amputation but they believed unilateral amputees coped better.
“But having the bit of advantage with nursing people that had had amputations…I knew that people with below knee amputations coped much better than a higher one and he [surgeon] wanted to do the full leg amputation and I just wouldn’t agree to it”. P1206 (Female, 72 years, control group)
Clinical team support
This sub-theme focuses on the time leading up to the participants’ amputation or the time after their amputation. Most patients felt supported by their multi-disciplinary team after their amputation.
“They’ve all been excellent. I mean I’ve had great support from the hospital and yeah the physios, you know, have put themselves backwards to fit me in and do lots of running up and down.” P1104 (Male, 54 years, intervention group)
“Yeah I got a lot of support off the artificial limb unit. As soon as the new one [standard prosthetic ankle-foot] arrived, they rang me up, made me an appointment to go and have the foot fitted.” P1101 (Male, 56 years, control group)
The relationship a patient has with their care team can play a key role in the decisions they make. Having a positive and supportive relationship with the physiotherapist enabled a participant (P2109) to understand and consider the impact of having an amputation.
“She [physiotherapist] showed me a leg. She explained quite a bit about it. She was absolutely great, you know, so I was prepared for what was going to happen and that’s why I had the operation…I was more aware.” P2109 (Male, 75 years, intervention group)
However, some participants felt unsupported and were unhappy with how long they had to wait to receive care or a prosthesis after their amputation. One participant felt that they had been badly let down because the expected post-amputation support did not happen. Others felt more heard by the clinical team if they had a family member to advocate on their behalf.
“You’re having a laugh aren’t you! I never had any back-up from anybody. I was just, well say kicked out, once I left hospital that was it, I was by myself.” P1114 (Male, 59 years, control group)
“When I went down there I had my son with me and the wife and he told them what I wanted. He wants to play his golf, he wants to do this and he wants to do that, you know, whatever else have you. I think they listened to him more than me.” P1110 (Male, 76 years, control group)
“Well I’ll tell you this, they said I would [get] so much help. I would have me house probably altered so that I could have a wheelchair in here and everything…Never heard anymore from them. So all I got out of it really was a wheelchair.” P2112 (Male, 74 years, intervention group)
Treatment options
Some of the participants said they had had a discussion about treatment options available to them but the overall impression was that these were not necessarily ‘true’ options. This was large because, nearly all participants, had been managing problems with their foot/leg for a number of years already and had tried less invasive procedures previously. At the point they did have a discussion about their condition, there were very few if any, other options available. Usually, discussions centred on the unfolding nature of their condition and the potential consequences of not having the amputation.
[Talking about foot management prior to amputation] “Then the pain came back and I had another operation and that one worked for a while and in 2017, I think it was, they said it was failing because I had pain and a cold leg and they said possibly gangrene was there and they advised me to try a spine puncture…and then they did another operation on the arteries which failed and then they said, well the only alternative is amputation, you know, and I agreed to that.” P2108 (Male, 78 years intervention group)
Following the amputation, participants reported that they had not had any choice or discussion about the prosthesis they would receive. All participants were fitted with a standard, non-self-aligning prosthetic ankle-foot after the swelling had decreased and the wound on their residual limb had healed. Some participants described how they had enquired about an alternative prosthetic ankle-foot, but were not successful in getting it prescribed. One participant mentioned how they had really needed to push for what they wanted; this participant was emboldened to pursue their request for a swimming leg after seeing another amputee with one.
“When I got that [referring to his swimming leg] I really had to argue over it…and the only reason I got it was the fellow, an American fellow was in…he had two legs like and I said, how come you’ve got two legs? He said that’s me swimming leg. You’ve got to demand it. They won’t give it to you, you must demand…They say yeah they’ve got lifting equipment and all this. I don’t want to be running around to somebody else. I want to do it me self, give me a swimming leg, you know.” P1110 (Male, 76 years, control group)
Participants in the intervention group were asked specifically about their experience of the self-aligning prosthetic ankle-foot, its availability to patients and when prosthetic prescription should be discussed with patients. This group of participants were very positive about their experience of the self-aligning ankle-foot. Many felt that the self-aligning ankle-foot should be offered as an option and much earlier in the rehabilitation journey so that they can adapt their walking more effectively following amputation.
“Well it may not be offered in the first place but within the first three years it should be offered to the patient.” P2113 (Male, 84 years, intervention group)
“I mean I don’t know what the difference is in pricing, like having a moveable ankle or not, but people should be fitted with this moveable ankle, to be honest. I mean I don’t know what the price difference is but this is so much better and if you were learning to walk on one, this would be so much better to learn to walk on one.” P2112 (Male, 74 years, intervention group)
Although all intervention participants had the opportunity to receive additional physiotherapy to support their transition from the standard ankle-foot to the self-aligning version, none of them had taken up this offer.
“Well it took me a couple of weeks or so to get used to it but everything is…I’m used to it now. So nobody has given me any physio with it.” P2105 (Male, 59 years, intervention group)
Theme 3: Experience of the self-aligning prosthesis (participants from the intervention group only)
Adapting
Participants reported having to adapt and get used to the new self-aligning ankle-foot as it felt, and worked, quite different to the standard, non-self-aligning one they had been used to. The self-aligning ankle-foot was described as being “looser” and “rolling back” which initially posed some problems. Participants stated that “Well it [the flexibility] took a bit to getting used to because I’ve been used to having a fixed foot for all them years you see but now actually, well it’s only the last couple of months that I’m getting used to it” [P2103]. As the participants had all lived with their old prosthesis for many years, being given a new, more moveable prosthesis was likened to “learning to walk again” [P2103]. For most participants, it took them a couple of weeks to adapt. Others felt that adaptation took them much longer and some participants felt that they were still not used to the new self-aligning ankle-foot. Those who struggled to adapt to the new ankle-foot talked of almost having to make themselves prefer it because they felt they should, rather than because they actually did; in other words, they wanted to prefer the new one.
“I don’t want to prefer the other [standard] one. I want to prefer this [self-aligning] one because that’s how it works because I’ve got to make myself mentally make it work and I will do, you know, I can get around with the sticks it’s just that there are problems with balance as well with me and the fact that the ankle is looser. So that’s something that I’ve got to explore. If you like that’s something that I would have thought I’ve got to have another few months sort of testing.” P2109 (Male, 75 years, intervention group)
Mobility
For most, the self-aligning ankle-foot afforded them improved mobility compared to their usual standard foot, which was often achieved after a period of adaptation. Participants found activities such as walking up and down slopes easier with the self-aligning ankle-foot. However, this varied with some participants reporting no or limited change; whereas others experienced great improvements. Additionally, the mobility benefits were not the same for all participants. For example, some found that the self-aligning prosthesis greatly aided them in walking downhill, but not uphill; whereas others reported the opposite.
“Walking is better. Going downhill with the new ankle is much, much better because you step into it and it rolls downhill. Going uphill it’s the same as the rigid ankle because you’re stepping up.” P2111 (Male, 53 years, intervention group)
“No it’s about the same [mobility]. As I say I don’t walk far now, it’s about the same. But the only difference is since I’ve had this new foot is going up slopes, I’m better at walking up slopes.” P2103 (Male, 86 years, intervention group)
Some participants said that they were not in a position, physically or psychologically, to increase their mobility levels meaningfully, even if the self-aligning prosthetic ankle-foot allowed for it. This may reflect the fact that they had already lived with their amputation for many years so had grown accustomed to a sedentary lifestyle.
“Well it’s certainly not made me into wonder man all of a sudden. There’s nothing spectacular I can tell you about because I don’t go out and I don’t climb stairs and I tried to avoid slopes because of, yeah you get used to doing things like that, you know, avoiding difficult situations.” P2108 (Male, 78 years intervention group)
“Yeah the trouble is now I can’t walk far now because my knees are going…I’ve got quite a few aids to help me. I go out on one of those buggies every morning and I can walk from the buggy into a shop and that’s me limit.” P2103 (Male, 86 years, intervention group)
Benefits
Despite some participants identifying limited improvements with the self-aligning ankle-foot, in general, participants were overwhelmingly positive towards the self-aligning prosthesis. The benefits they reported mainly related to experiencing less pain, having greater movement and an associated feeling of increased confidence in moving around. Most participants reported that the self-aligning ankle-foot made the prosthesis more comfortable to wear, with less or no pressure or pain in the hip and knee in comparison to the standard foot. The absence of pain when using the self-aligning ankle-foot, had a profound impact on some participants who believed that it had improved their life greatly and their ability to move around independently. In addition, some reported feeling more confident and competent about walking than they previously did; this became a freeing experience.
Participants felt as though they had more precise movement with the self-aligning ankle-foot, stating that they could feel the ground more and had a better response from the terrain they were walking on, particularly when navigating slopes, stairs and uneven ground.
“You could tell…you felt the difference as soon as they put the [self-aligning prosthetic ankle-] foot on and I stood up and walked. There was just no pressure in the knee, none in the hip and no pain at all.” P2102 (Male, 66 years, intervention group)
“I got this one and that’s been a whole different ballgame because walking up and down slopes is far better, steps is better. So the difference that’s made is, you know, a hundred percent on the last one. I’ve found this leg that I’ve got now really good.” P2107 (Male, 62 years, intervention group)
While some participants reported a marked difference in terms of comfort, often keeping the self-aligning prosthesis on all day rather than taking it off when they were at home (as they did with their standard prosthesis).
“Yeah as soon as I get up in the morning, I have it stood at the side of me bed and as soon as I get up I put that leg on and it’s on until I go to bed.” P2103 (Male, 86 years, intervention group)
Participants felt as though they walked normally with the self-aligning prosthesis, which enhanced their confidence in being mobile and around others. One participant claimed that “it feels like a proper walk instead of a clumpy walk” [P2107] and another described his experience as “I walk down a short maximum steepness hill and before I used to walk down like a crab…And now I walk down like a gentleman and that is the difference” [P2103]. As a consequence, participants found that the self-aligning ankle-foot had enabled them to ‘do more’ and get back more to how they used to be; some stated that it had completely changed their walking ability and their enjoyment of walking. For others, it had also changed their quality of life and well-being in that it made them feel “A lot happier” [P2103] and “normal” [P2105].
“Having this now doesn’t make me feel as out of place as I was on the first [standard, non-self-aligning] limb because it was so obvious on that first limb and even standing…. it was more awkward. It was more awkward. I can almost stand like a normal person now from sitting, you know.” P2107 (Male, 62 years, intervention group)
Drawbacks
Drawbacks mostly focused on the extent to which the prosthesis impacted their mobility and quality of life. For some participants, the self-aligning ankle-foot had less impact on their mobility than they had anticipated and their quality of life had not improved. Other participants were put off using the self-aligning prosthesis when it was first fitted because it was different to what they had been used to and some learning was required in order to become familiar with, and confident using the device. This led some participants to report negative experiences and feelings around this. Furthermore, a number of participants reported feeling wobbly on the self-aligning ankle-foot and one participant reported a recent onset of lower back pain. They were not sure whether it was related to using this particular ankle foot.
“The only thing is since I’ve had the [self-aligning] ankle I don’t know whether it is the hydraulic ankle but I’ve had lower back pain which is absolutely, I go to a chiropractic once a week and I’ve just been to the doctors and I’ve got to go for some physio.” P2111 (Male, 53 years, intervention group)
“I can’t stand for a long time. I get where I start wobbling a bit. Where with the old one I could stand still but with this new one you see, I suppose it’s like getting used to it with joints moving, I seem to be wobbling a bit. When I’m in the house because I’ve got carpets, thick carpets and thick underlay, that makes me wobble as well.” P2105 (Male, 59 years, intervention group)
“When I first got it, I was negative, there’s no doubt about it because I thought…it was fitted and I walked up and down this room and I thought…I’m not certain about this, nearly fell over on a chair and this sort of thing.” P2109 (Male, 75 years, intervention group)
Discussion
The qualitative research described in this paper was carried out as part of a feasibility trial which examined the acceptability of a self-aligning prosthetic ankle foot. All participants have established prosthesis users who had been previously fitted with a standard, non-self-aligning prosthetic ankle-foot. The interviews provided a forum for exploring their experience further. Three broad themes were identified: The impact of the amputation; Role of clinical Support; and Experiences of the self-aligning prosthesis.
All participants had managed their affected foot for a number of years prior to amputation and experienced neuromusculoskeletal pain and difficulty walking during this time, which corroborates findings from other previous studies [Citation4,Citation18]. As such, some expected that the pain would have stopped after amputation. Norlyk et al. (2013) similarly found that patients ‘learned’ to accept a level of pain associated with their amputation which became part of the process of learning to use their altered body. Many participants in this study reported struggling to regain their full mobility after the amputation and some developed new issues, such as a fear of falling, when using a prosthesis. Participants described having to learn to walk again, but even once fitted with a prosthesis, they were not always able to walk very far. The provision of a self-aligning ankle-foot did not necessarily overcome the issues identified by participants following their amputation. Some participants placed a lot of expectations on how the self-aligning ankle-foot could make a difference to their mobility and everyday life. They described how they needed to familiarise themselves with the new ankle foot, which for many led to improved mobility and capability, including being able to tackle different surfaces more confidently than on their standard ankle foot. Sanders et al. (2020) suggested that those who experienced the greatest difficulty and adjustment following their amputation were those with high expectations related to their outcomes. This may help shed light on how participants in our interviews perceived the self-aligning ankle-foot, as they may have seen their participation in the trial as an opportunity to try something new and therefore placed a significant emphasis on it. There are several studies which explore how patients, following amputation, need to adapt their sense of self and self-identity [Citation3,Citation19–Citation21] in order to be able to achieve improvements in their mobility. It may also be the case that, when these participants were presented with the opportunity to use a self-aligning ankle-foot, it was akin to being fitted with their initial prosthesis. Therefore they may need to reassess their relationship with the new prosthetic ankle-foot over a longer period of time than the study duration in order to progress with it more positively.
Overall, and despite presenting some contrasting views, participants were overwhelmingly positive about the self-aligning ankle-foot compared to the standard prosthesis. They reported less pain, greater mobility and being able to do more than previously, although this was relative to their own perceived ‘starting point’. Drawbacks were identified such as feeling some instability, which affected their sense of balance. Therefore they needed to adjust to walking with the self-aligning ankle-foot. For some, the drawback was around their expectations of what would be possible compared to what was actually achievable in view of their own physical health.
Implications of findings on a future trial
The participant interviews have identified a number of factors that have implications for the design of a full-scale RCT.
Participants who had used the self-aligning ankle foot found it an acceptable intervention. Together with the findings from the feasibility RCT, which showed that the trial was able to recruit and retain participants for follow-up data collection, this supports the feasibility of a full-scale RCT [Citation16].
There was variation in how participants experienced the transition from a non-self-aligning to a self-aligning ankle-foot. A number of participants said they needed to learn to use the self-aligning prosthetic ankle-foot. Participants in the trial only had a short period of time to use the self-aligning ankle-foot (approximately 12 weeks after randomisation, excluding 3 weeks reserved for ordering and fitting the ankle-foot) before the interview and follow-up. A longer adaptation period should be considered in a future trial. A minimum of 12 months, following the fitting of the self-aligning ankle-foot, should ensure that participants have passed through the adaptation phase, therefore allowing a fair comparison against the standard prosthetic ankle-foot in a future trial.
As part of the feasibility RCT, all participants allocated to the intervention group were offered additional physiotherapy following the fitting of the self-aligning ankle-foot based on their clinical need [Citation15]. Several studies [Citation20–22] have emphasised the importance of gait rehabilitation following amputation, which may be equally relevant for patients who move on to a higher-functioning or alternative prosthesis. Additional physiotherapy may be required to enable them to unlearn old movements and compensatory adaptations they had developed. We are unaware of any studies related to changing to an alternative prosthesis involving this population. A future trial should explore ways to encourage patients to attend physiotherapy according to clinical need in order to support each person’s use of their prosthesis and enhance their mobility.
Interviews with participants highlighted key outcomes which were of significance to them and should be considered for inclusion in a future trial and indeed any research assessing the effectiveness of prosthetic components in this population. These include avoiding falls and developing balance confidence, being able to engage in daily activities, maintaining social activities and networks and personal well-being.
For pragmatic reasons, the feasibility RCT limited the inclusion criteria to people who have established prosthesis users (i.e., patients with an amputation > 1 year) and who were using a standard, non-self-aligning ankle-foot. Participants expressed that they thought it would be useful if the self-aligning prosthesis was offered sooner to amputees so that they could adapt to the self-aligning ankle-foot earlier. A full-scale trial is likely to have more inclusive eligibility criteria, including less established prosthesis users (i.e., including patients with an amputation <1 year).
A future full-scale RCT should consider embedding a qualitative study on recruitment optimisation to maximise the diversity of the included participants, e.g., women, younger users, amputation due to trauma or cancer, as these groups were absent in the current RCT.
Strengths and limitations
The current study has some limitations and therefore the findings should not be taken out of the context in which they were collected. The population which made up the sample was not able to fully capture the perspectives of the full range of users including, age, women, different ethnic groups and limb loss due to trauma. Linked to this is the small number of participants who were interviewed; a total of 14 participants were interviewed, and of these nine were randomised to the intervention group of the RCT. Only one woman participated in the interviews, however, this is reflective of the number of women who participated in the trial and more broadly have had a lower limb amputation in the general population. Therefore the results do not necessarily reflect a broad range of views and analysis on the basis of gender was not possible. Another point of consideration is the length of time the participants in the intervention group were using the self-aligning ankle prosthesis before the final follow-up. This was a short period of time and the impact of changing from one prosthesis to another may have longer-term impacts which could not be explored. However, this study is the first study we are aware of that has reported on the experiences of patients who were given an alternative prosthesis alongside those patients who retained their prosthesis. The findings from the interviews have helped to highlight elements which warrant further exploration in a full-scale trial, including how patients adapt to their prosthesis, and the potential practical and psychological support they may require to adjust to the capability of a different prosthesis.
Conclusion
This is the first study to establish the acceptability of using a self-aligning ankle-foot in an older population with transtibial amputation and other health comorbidities within the context of a mixed-methods RCT. The interviews carried out as part of the STEPFORWARD feasibility trial have identified the importance patients attributed to being mobile, independent, undertaking usual daily activities and engaging in social activities has for patients. Participants described how a standard, non-self-aligning ankle foot limited their mobility on slopes and stairs, negatively affecting their ability to participate in daily activities. Participants found the self-aligning ankle-foot highly acceptable, though there was variability in the impact it had on their mobility, which may have been improved with longer use before follow-up. As such, the findings support a robust clinical evaluation of the effectiveness and cost-effectiveness of a self-aligning ankle-foot in people with a transtibial amputation.
Acknowledgements
The authors wish to thank all the participants in this study who generously gave their time and shared their experiences with the team.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J. 2002;95(8):875–883.
- University of Salford. LIMBLESS statistics: repository for quantitative information on the UK limbless population referred for prosthetics treatment, annual report 2011-2012. Salford (UK): University of Salford; 2013.
- Norlyk A, Martinsen B, Kjaer-Petersen K. Living with clipped wings—patients’ experience of losing a leg. Int J Qual Stud Health Well-Being. 2013;8(1):21891.
- Watson-Miller S. Living with a diabetic foot ulcer: a phenomenological study. J Clin Nurs. 2006;15(10):1336–1337.
- Belmont PJ, Jr., Davey S, Orr JD, et al. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(3):370–378.
- Kristensen MT, Holm G, Kirketerp-Møller K, et al. Very low survival rates after non-traumatic lower limb amputation in a consecutive series: what to do? Interact Cardiovasc Thorac Surg. 2012;14(5):543–547.
- Murray CD, Forshaw MJ. The experience of amputation and prosthesis use for adults: a metasynthesis. Disabil Rehabil. 2013;35(14):1133–1142.
- Senra H, Oliveira RA, Leal I, et al. Beyond the body image: a qualitative study on how adults experience lower limb amputation. Clin Rehabil. 2012;26(2):180–191.
- Couture M, Desrosiers J, Caron CD. Coping with a lower limb amputation due to vascular disease in the hospital, rehabilitation, and home setting. ISRN Rehabilitation. 2012;2012:1–9.
- Grech C, Debono RF. The lived experience of persons with an amputation. Malta J Health Sci. 2014;1(2):54–59.
- Barnett CT, Brown OH, Bisele M, et al. Individuals with unilateral transtibial amputation and lower activity levels walk more quickly when using a hydraulically articulating versus rigidly attached prosthetic ankle-foot device. J Prosthet Orthot. 2018;30(3):158–164.
- Johnson L, De Asha AR, Munjal R, et al. Toe clearance when walking in people with unilateral transtibial amputation: effects of passive hydraulic ankle. J Rehabil Res Dev. 2014;51(3):429–437.
- Healy A, Farmer S, Pandyan A, et al. A systematic review of randomised controlled trials assessing effectiveness of prosthetic and orthotic interventions. PLoS One. 2018;13(3): e0192094.
- British Society of Rehabilitation Medicine. Amputee and prosthetic rehabilitation – standards and guidelines. 3rd ed. Report of the working party (Co-Chairs: Hanspal RS, Sedki I). London (UK): British Society of Rehabilitation Medicine; 2018.
- Mitchell N, Coleman E, Watson J, et al. Self-aligning prosthetic device for older patients with vascular-related amputations: protocol for a randomised feasibility study (the STEPFORWARD study). BMJ Open. 2019;9(9):e032924.
- Vanicek N, Coleman E, Watson J, et al. STEPFORWARD study: a randomised controlled feasibility trial of a self-aligning prosthetic ankle-foot for older patients with vascular-related amputations. BMJ Open. 2021;11(3):e045195.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Vase L, Nikolajsen L, Christensen B, et al. Cognitive-emotional sensitization contributes to wind-up-like pain in phantom limb pain patients. Pain. 2011;152(1):157–162.
- Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil. 2004; 26(14-15):837–850.
- Miller MJ, Jones J, Anderson CB, et al. Factors influencing participation in physical activity after dysvascular amputation: a qualitative meta-synthesis. Disabil Rehabil. 2019;41(26):3141–3150.
- Ostler C, Ellis-Hill C, Donovan-Hall M. Expectations of rehabilitation following lower limb amputation: a qualitative study. Disabil Rehabil. 2014;36(14):1169–1175.
- van Twillert S, Postema K, Geertzen JH, et al. Improving rehabilitation treatment in a local setting: a case study of prosthetic rehabilitation. Clin Rehabil. 2009;23(10):938–947.

