Abstract
Purpose
To investigate how a quality improvement program (BRIDGE), designed to promote coordination and continuity in rehabilitation services, was delivered and perceived by providers in routine practice for patients with rheumatic and musculoskeletal diseases.
Methods
A convergent mixed methods approach was nested within a stepped-wedge, randomized controlled trial. The intervention program was developed to bridge gaps between secondary and primary healthcare, comprising the following elements: motivational interviewing; patient-specific goal setting; written rehabilitation-plans; personalized feedback on progress; and tailored follow-up. Data from health professionals who delivered the program were collected and analyzed separately, using two questionnaires and three focus groups. Results were integrated during the overall interpretation and discussion.
Results
The program delivery depended on the providers’ skills and competence, as well as on contextual factors in their teams and institutions. Suggested possibilities for improvements included follow-up with sufficient support from next of kin and external services, and the practicing of action and coping plans, standardized outcome measures, and feedback on progress.
Conclusions
Leaders and clinicians should discuss efforts to ensure confident and qualified rehabilitation delivery at the levels of individual providers, teams, and institutions, and pay equal attention to each component in the process from admission to follow-up.
Implications for Rehabilitation
Quality in rehabilitation should be characterized by a continuous and coordinated process from goal setting to follow-up.
To improve the quality, sufficient involvement of next of kin and external services is needed.
Clinicians may need training to build confidence in motivational interviewing, action- and coping planning, feedback on progress, and follow-up.
Leaders should organize education sessions, optimize schedules, insert standardized outcome measures, and facilitate collaboration across levels of care and services.
Background
Patients with long-term rheumatic and musculoskeletal diseases (RMDs) constitute a large proportion of the population needing rehabilitation services [Citation1]. Rehabilitation has the potential to yield profound benefits for individuals and society by optimizing everyday functioning for people who experience functional limitations in the course of their disease [Citation2–3]. Despite the impression that an increasing number of patients benefit from rehabilitation, such services are not sufficiently prioritized in or integrated into current health systems [Citation1,Citation3].
Recommendations from the World Health Organization (WHO) for scaling up rehabilitation address not only improving availability but also efforts to improve the quality of delivered care [Citation3]. Public evaluations from WHO and different countries, including Norway, document that rehabilitation quality varies among healthcare providers and sites. In addition, these evaluations show that coordination is limited across services involved in rehabilitation, such as between levels of healthcare, between health services and a patient’s place of employment or education, and between health services and the labor and welfare administration [Citation3–6]. In addition, global and national health authorities have called for more patient involvement and co-determination regarding rehabilitation plans and needed follow-up and for better systems of standardization and documentation of quality [Citation3–6].
The use of quality indicators (QIs) may help to define and monitor the recommended quality of care because such indicators comprise defined and measurable elements of practice performance that are relevant for drawing inferences about the quality of provided care [Citation7–9]. A QI set has been developed for the RMD context to identify measurable elements of a team-based rehabilitation process that facilitate recommended continuity in a patient-centered rehabilitation process and efficient coordination across involved professions and services [Citation10]. In this set, the indicators explicitly reflect the providers’ responsibility to facilitate a high degree of patient participation in all phases of a rehabilitation process, such as individual goal setting, development of written rehabilitation plans, tailored follow-up, and use of standardized instruments for baseline assessments and outcome monitoring [Citation10]. Hence, several interacting elements are needed to ensure a high-quality rehabilitation process, and a number of behaviors are required by those delivering the rehabilitation. Efforts to fulfill the QIs for rehabilitation thus may be considered complex interventions in which the providers are expected to strike a balance between fidelity to key elements of a high-quality rehabilitation process and tailoring that process to the local setting and individual patient [Citation10].
With a growing interest in quality improvement in health services for RMDs [Citation11–17], more knowledge is needed about using complex interventions to improve quality in rehabilitation processes and how providers deliver and perceive such quality improvement programs [Citation18]. The BRIDGE program is a quality improvement program, comprising five interacting elements needed to provide a high degree of patient involvement in a continuous and coordinated rehabilitation process from goal setting to follow-up. Included elements in the BRIDGE program are motivational interviewing (MI), patient-specific goal setting, written plans for rehabilitation, personalized feedback on progress, and tailored follow-up. Knowledge is needed about what efforts are necessary to deliver such programs. In the current study, we used a mixed methods approach to evaluate the delivery of the BRIDGE program from the perspective of health professionals who delivered it as part of a multicenter study. The overall aim was to investigate how the providers delivered and perceived the BRIDGE program.
Methods
Design
We used a mixed methods approach for two reasons. First, quality of healthcare was understood as a multidimensional concept, requiring many different measures [Citation7]. Our intention was to relate and combine measurable and not directly measurable aspects of how the BRIDGE program was delivered.
Second, the BRIDGE program was expected to have the potential to improve both structural and process dimensions of the quality of the provided rehabilitation processes, and a convergent mixed approach [Citation19] enabled us to generate a comprehensive account on how the program influenced both dimensions. The structural dimension was related to the setting within which the rehabilitation was delivered. In our study, this dimension was defined as written materials and written procedures available for daily use at rehabilitation centers, describing the rehabilitation process they intended to deliver [Citation7, Citation10]. The process dimension was related to enacting the continuous and coordinated rehabilitation process itself in terms of the actual activities and collaboration between BRIDGE program providers and patients, from admission and throughout the follow-up period [Citation7, Citation10].
Our guiding study objectives were as follows: (1) to evaluate whether written procedures regarding intended rehabilitation practice were supplemented or changed because of the BRIDGE program (quantitative data); (2) to evaluate the health professionals’ assessments of whether the elements of the BRIDGE program were delivered (quantitative data); (3) to explore the health professionals’ perspective on changes in their practice or behaviors when delivering the BRIDGE program (qualitative data); and (4) to compare and combine the results from objectives 1–3 (a mixed approach).
The clinical setting
Providers at eight Norwegian rehabilitation centers delivered the BRIDGE program as part of the intervention phase in a stepped-wedge cluster-randomized controlled trial (RCT), the BRIDGE trial [Citation20], presented in Box 1. The main results of the trial are published elsewhere [Citation21].
In the control phase (T1), providers delivered their traditional programs, which could include asking patients about their goals, but involved variability or even insufficient descriptions of intended phases in a rehabilitation process. When switching to the intervention phase (T2), providers started to deliver the more structured and defined rehabilitation process described by the BRIDGE program (Box 1), which was intended to be similar across all participating centers and facilitate a high degree of patient involvement in a continuous and coordinated rehabilitation process for each patient.
The BRIDGE research team selected the interacting elements comprising the program based on four preceding research projects in Norway, Norwegian public reports documenting a lack of coordination and continuity across levels of rehabilitation care, and theories on goal setting and behavioral change in rehabilitation, as described elsewhere [Citation20–21]. In brief, the theories addressed a rehabilitation process based on the patient’s autonomy, strengths and capabilities, valued and prioritized rehabilitation goals, and confidence in agreed-upon plans and actions. The theoretical grounding also addressed feedback on progress in order to affirm patient motivation, adjust goals or actions if necessary, facilitate problem-solving and adherence to self-management strategies over time, and establish and coordinate tailored support from others until the patient develops new habits, needed changes, and meaningful goal attainment in their daily life [Citation20–21].
Box 1. The overarching BRIDGE trial and the BRIDGE program.
Table
Data collection
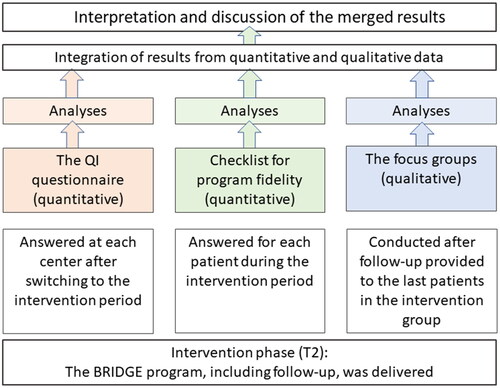
During T2, quantitative and qualitative data were collected on how the BRIDGE program was delivered and how it influenced rehabilitation quality, as reported from the provider perspective. Data sources consisted of health professionals’ responses to two questionnaires and results from focus groups (FGs) consisting of members from the multidisciplinary teams delivering the program at each center. The types of data collection were concurrent but separate and did not depend on each other [Citation19]. We kept the data from questionnaires and FGs separate during the analyses, before mixing the results during the overall interpretation and discussion [Citation19] ().
Figure 1. Procedural diagram for the convergent approach: the quantitative and qualitative data were collected separately in the intervention-phase of the trial, before they were analysed separately, and then integrated and discussed for the purpose of a mixed, complementary investigation of the delivery of the BRIDGE program. QI: quality indicators.
Data source 1: quality indicators (quantitative data, a questionnaire)
A QI set developed for use in multidisciplinary RMD rehabilitation [Citation10] reflected recommendations for three dimensions of quality (structure, process, and outcome). Used in primary and secondary care, the QI set has shown adequate feasibility, face and content validity, and responsiveness [Citation10, Citation22]. The set consisted of two separate questionnaires and allowed for measuring quality from the perspectives of both providers and patients [Citation10]. Evaluation of patient-reported quality has been reported elsewhere [Citation23]. In this study, we examined the provider-reported quality of rehabilitation.
The provider-reported questionnaire included 19 structure indicators, as presented in additional file 1. The QIs were related to written documents (procedures or method descriptions) being present and easily accessible at the rehabilitation center as a structural foundation for daily clinical practice [Citation10]. Ten QIs addressed the use and monitoring of standardized outcome measures, and six QIs addressed patient participation in goal setting, planning, and evaluating throughout the rehabilitation period and follow-up. Assessments of follow-up needs from next of kin or external services were covered in three items.
Between 6 and 8 weeks after adding the BRIDGE program, the leader of each center or another person familiar with the written procedures available for daily use, answered “yes” or “no” to each statement presented in additional file 1. The answers given at T2 were compared to the same measurement conducted at the beginning of T1. At both time points, data were collected in a telephone-based interview conducted by the central project coordinator (ALSS).
Data source 2: program-fidelity checklist (quantitative data, a questionnaire)
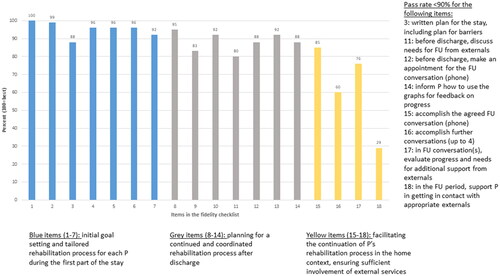
The fidelity checklist included measurable aspects of the elements intended to be delivered in the BRIDGE program. There were 18 items with response alternatives “yes” or “no” and a “not appropriate” alternative for two items (). During T2, the providers completed one checklist for each patient along with their ongoing rehabilitation process, starting with items for the establishment of the process at admission and ending with items for a mandatory follow-up conversation after discharge. Responders were members of the multidisciplinary teams, mainly local project coordinators, who were familiar with the content of the delivered rehabilitation process.
Table 1. Fidelity checklist for optimal delivery of the BRIDGE program.
The MI approach was expected to influence items in the checklist regarding goal setting, development of rehabilitation plans, and follow-up. To highlight these expectations, guiding information was included in the provider booklet (Additional file 2).
Data source 3: FGs (qualitative data)
We arranged three FGs with representation from all centers and all professional groups. The FG interviews were performed after the providers had completed all potential follow-up interventions for all patients, i.e., about 6 months after the discharge of the last patients in the intervention group (). The same interview guide (Additional file 3) was used in all groups and included questions about the providers’ impression of the program and their experiences translating it into their local setting. We included two group tasks in each FG to stimulate group interactions and give providers the opportunity to reflect on shared experiences or different viewpoints and express their beliefs, attitudes, questions, and concerns about program delivery [Citation24]. In the group tasks, the participants rated cards naming the elements and tools in the BRIDGE program from “less” to “more” important and useful in supporting the patients’ rehabilitation process. The rating scale was 0–10, with 10 indicating most important or useful (see Additional file 4 for details regarding the group tasks).
The FG conversations were audiotaped and carried out on the same day in three different rooms at the same location. Each group was facilitated by one moderator (ALSS, IK, or ASH [one of the site coordinators]) and supported by an assistant moderator (IJ, TND, HLV). The assistant moderator took brief field notes during the discussions to capture impressions and nonverbal observations, managed the material needed in the group tasks, and photographed the rating of the cards on the table.
To establish a purposive sample, we aimed to include men and women and at least one representative from all of the different professions delivering the BRIDGE program, such as a nurse, social worker, physiotherapist, occupational therapist, and sports educator. In dialogue with the local project coordinators, we recruited 15 professionals and deliberately assigned them to the groups to ensure three groups with mixed locations and professions represented.
Ethics
All participants provided written informed consent to participate, after reading the invitation letter that explained the purpose of this study. The Norwegian Regional Committee for Medical Research Ethics (REK South-East, 2017/665) approved the study. Provider representatives and two patient research partners were involved in all stages of the study.
Analyses
We used STATA/IC 14.0 and Microsoft Office Excel 2019 to analyze numeric data, and Nvivo 12 Plus for text data. Nvivo was not used as a codebook but rather as a way to facilitate the processes of clustering and meaning-mapping of textual data.
Quality indicator data
We considered a structure indicator as achieved if the item was answered “yes” and calculated the degree of achievement as pass rates (PRs). For each center, we calculated summary PR as PR total equal to “the total number of items achieved at this center” divided by “total number of items (=19).” In addition, we calculated PRs for single indicators across the centers as “the total number of centers that checked ‘yes’ for this item” divided by “total number of eligible centers (=number of centers that checked ‘yes’ or ‘no’ for this particular item).” The PR values were presented as percentages ranging from 0% to 100%, with 100% representing the best quality. We used descriptive statistics to compare changes in PR data between T1 and T2.
Program fidelity data
The fidelity checklist contained 18 eligible items. If the response option “not appropriate” was used once or twice, the number of eligible items was 17 or 16, respectively. We calculated a summary fidelity score for care provided to each patient, as “the number of items adhered to for this patient” divided by “the number of eligible items for this particular patient’s rehabilitation process.” At the group level, we calculated the fidelity score for single items in the checklist, equal to “the total number of ‘yes’ for this item” divided by “the total number of eligible cases for this particular item.” We presented the results in percentages ranging from 0% to 100%, with 100% representing the highest fidelity, and used descriptive statistics to calculate the median, maximum, and minimum values.
FG data
The audio recordings were transcribed by the researcher mainly responsible for the FG analyses (ALSS). Data relevant to our research questions were extracted from the FG transcripts and field notes and analyzed using a reflexive thematic analysis [Citation25]. The researcher (ALSS) did not differentiate among the three FGs but rather analyzed for recurring patterns across the entire transcript material. Categories and themes developed early in the process were refined, replaced, or expanded as other passages from the transcripts were analyzed or when transcripts or passages were revisited several times.
Initial categories and preliminary themes (generated by ALSS) were presented and discussed at an overarching level with the local site coordinators and the wider research group (GJA, MA, GB, AMB, TD, CE, IJ, HLV, IK) early in the process and later discussed in more detail with a second researcher (HLV). The further process was driven by one researcher (ALSS) as an interpretative reflexive process [Citation25–26]. First, patterns of shared meaning were developed inductively based on the content of the data. Then, existing concepts and ideas from relevant literature [Citation27–28] were added to the interpretation process to expand understanding of the providers’ reflections and behaviors when delivering the BRIDGE program in their routine clinical settings. Titles of the final themes were formulated as first-person wordings, as spoken by the providers, reflecting patterns identified during the iterative process back and forth between raw data, categories, theories, and themes. Illustrative quotations (Q) have been edited for readability.
Integration
We compared the results from the different data sets to determine how they converged, diverged, or expanded each other [Citation19]. To illustrate how the data related, we used a joint display figure for the overall results and a joint display table for details.
Results
Changes measured by the structure indicators
There were no missing data for the QI questionnaire. The median PR total increased from 53% at T1 to 90% at T2, calculated for all of the centers as a whole sample. At T2, the PRs for single indicators were 100% for all of the indicators, except for the two indicators related to written documents addressing possible attendance in meetings for next of kin or external services (PR ≤ 25%; see additional file 5 for details about changes measured by the indicators).
Fidelity of program delivery
The checklist was answered by the providers regarding the rehabilitation processes for 156/168 patients (93%) receiving the BRIDGE program. The fidelity of program delivery was high, with a median summary score of 94% (range 6%–100%). The fidelity score for single items differed according to phases in the rehabilitation process from admission to the follow-up period. More specifically, initial goal setting was delivered with higher fidelity compared with tailored follow-up across levels of care. Intervention content addressing the time after discharge and involvement of next of kin or external services was delivered with less fidelity than the inpatient parts of the program (; see Additional file 6 for details about the measured program fidelity).
Figure 2. Fidelity scores for single items in the providers’ checklist for fidelity in the BRIDGE trial. HP: health professionals; rehab: rehabilitation; P: patient; PR: pass rate; FU: follow-up.
Results from FGs
A total of 15 providers of the BRIDGE program participated in the FGs. In , we present details of participant characteristics and group composition. Approximately 2 hours of discussion in each group were audiotaped and transcribed verbatim. In the following quotations, the symbol * indicates work experience over the median experience among the FG participants.
Table 2. Characteristics of the participants and composition of the focus groups.
The analysis of the providers’ descriptions and reflections on practicing BRIDGE led to an understanding that optimal program delivery depended on four themes, as described from the provider perspective:
Improving my professional skills
This theme reflected the providers’ perceived competence when practicing elements in the program. Statements suggested that parts of the BRIDGE program implied improvements in the providers’ behaviors and conversation skills, compared to the delivery of their traditional programs.
Paying attention to my professional toolbox
This theme comprised the providers’ attention towards supporting material and practical objects available in the BRIDGE program, developed to guide or facilitate the interacting phases in each patient’s rehabilitation process.
Expressing my professional mind
This theme addressed the providers’ professional understanding of the program and their theory-based accounts for use of the elements comprising it. Several statements suggested that the BRIDGE program evoked the providers’ consciousness about core values and important activities in rehabilitation, as one stated: “[BRIDGE was] like ‘this is what we should be excellent in’ [as rehabilitation experts]” (Q 56).
Optimizing the organization at my workplace
This theme comprised the contextual factors at each center, influencing the delivery of the BRIDGE program. As a pattern, the providers’ statements pointed to a mutual influence between the elements of the program and the contextual settings at each center, such as the organization of meetings and time schedules, or human contextual factors related to the individual team members, the local research coordinator, or the leader of the center. The context modified the delivery of BRIDGE, and vice versa.
Content related to each theme are briefly labeled (i) skills, (ii) tools, (iii) mind, and (iv) organization. To enhance readability, the following presentation of details about the FG results are structured along the phases in the rehabilitation process from goal setting to follow-up.
Skills
Initial goal setting and tailored rehabilitation process during the first part of the stay
Several providers stated that guiding the patients in formulating written goals was more difficult than making oral agreements. To be more confident, some providers prepared for the goal setting by reading about goal-setting techniques in the provider booklet. For others, the booklet was perceived to include too much information covering all stages in the rehabilitation process. Therefore, they used the booklet infrequently as support for the development of goal-setting skills.
Planning for a continued and coordinated rehabilitation process
The use of written rehabilitation plans in the BRIDGE program implied the need to invite the patients to reflect not only on actions needed for goal achievement but also on potential barriers and strategies for overcoming them. The latter represented a more advanced aspect of planning compared with traditional practice, and one provider stated: “We developed tailored plans, but we did not talk about barriers…I do not think I have the talent needed to do that task” (Q 105). Others explained how they tailored phrases to their everyday vocabulary, resulting in improved confidence: “…for me, it became easier when I just invited [the patient] to develop a good plan B instead of using the barrier word or other complicated words” (Q 103*). Training of skills to identify strategies for barriers could be motivated by positive experiences in interaction with their patients, as stated by this provider: “…those dialogues [planning for barriers] were useful…most patients could imagine potential barriers, such as how to manage if it is a rainy day or I am worn-out or I am too busy” (Q 99*).
Some providers described the use of MI rating scales as more difficult and advanced than basic parts of MI, such as reflections, empathy, and positive affirmations. Their stated reasons for infrequent use or non-use of the MI rating scales were partly related to the providers’ role-identities. For example, some providers associated “learning new provider skills” with “being less competent than I was when delivering the traditional program,” as illustrated in this quotation: “I did not use the MI rating scales, but some of my colleagues who are more familiar with MI did, but for me…I was not comfortable. For me, it is important to be competent and good in interaction with my patients, and therefore I have to be comfortable with what I practice” (Q 89*).
Facilitate continuation in the home context and sufficient involvement of external services after discharge
Some providers highlighted the benefit of dedicated time to practice and develop conversation skills, in terms of team-based workshops, peer-to-peer learning, or guidance from the local site coordinator. However, the content in such initiatives mostly addressed goal setting and MI used in the initial parts of the rehabilitation process. Similar leader-led initiatives to empower clinicians’ practicing of tailored feedback on progress or cooperation with next of kin or external services were not described.
Tools
Initial goal setting and tailored rehabilitation process during the first part of the stay
All providers rated the reflection task, “The shoe” (Additional file 7), as the most useful tool to support the patient’s initial rehabilitation process. “The shoe” was a drawing designed to stimulate the development of goals for each patient. Different parts of the surface of a shoe represent potential headings for rehabilitation goals for people with RMDs. In line with the Norwegian saying “Where the shoe pinches”, the patients considered their everyday situation according to the topics written on “the shoe”. Providers stated that this task worked as a quick and “to-the-point” preparation for goal setting for patients. Additionally, the task seemed to widen the scope of topics for rehabilitation goals, reaching beyond or supplementing the more frequently occurring topic “physical training.” The consequence was that different professions were invited to engage in goal setting, such as social worker or a nurse: “They [the patients] said they experienced a new way of thinking about factors influencing it [their health and pain], and difficult things became easier to talk about because ‘the shoe’ influenced the patients’ mental process in a way (-)” (Q 69*).
Planning for a continued and coordinated rehabilitation process
Less attention to tools, such as MI rating scales or smartphone applications relevant to support health-related behavior changes, was explained by forgetfulness and delay in changing routines. Some providers used an available tool a few times and experienced benefit in interaction with their patients but did not automatically change their habitual practice.
Facilitate continuation in the home context and sufficient involvement of external services after discharge
A few statements outlined the importance of feedback on progress (the digital graphs as a tool): “I rated the graph [as] highly important [to support the process] because I saw how the patients responded to the document…the visual effect…so concrete…for some patients, the graph illustrated well the fluctuations [of their symptoms or activity problems], and they wanted to present it to the general practitioner” (Q 7). Hence, experienced effectiveness was a prominent reason for rating the graphs or other BRIDGE tools as highly useful.
Mind
In general, the providers’ theoretical grounding of activities in the BRIDGE program could vary along a continuum from not verbally expressed to evoked and expressed. The degree of theoretical grounding could improve by peer-to-peer learning or individual self-reflections, as part of the dialogues within the FGs.
Initial goal setting and tailored rehabilitation process during the first part of the stay
Goal setting and MI were collectively rated as highly important to support the rehabilitation process. Provider explanations for why those elements were important typically addressed theoretical concepts, such as patient autonomy, motivation, and responsibility: “BRIDGE is about the patient being responsible for his own rehabilitation process, and I think that is great, because the likelihood of goal attainment increases when the patient talks and reflects, and we are more in the background…and we use the right tools, such as MI, to listen and reveal the patients’ actual meanings and wishes” (Q 68).
Planning for a continued and coordinated rehabilitation process
Less priority was given to BRIDGE elements if the added tasks were perceived to be too time-consuming or less important: “We do plan for goal-attainment after discharge, but not necessarily as a written plan…writing requires additional time, and is not necessarily a must…for some patients, I think the good conversation is most helpful” (Q 108*). However, the group discussions about the BRIDGE elements could result in new understanding or evoke professional reasoning: “First I rated it [written rehabilitation plan] as less important, but now [after reflections in the FG], I will say it is very important. I need something written–reflecting the patients’ own words and statements–to evaluate if we have a similar understanding of the situation and to have some written agreements to give feedback on–or adjust–during the process” (Q 149).
Some providers linked the use of written rehabilitation plans to theoretical concepts such as the patients’ coping skills and sufficient self-efficacy towards goal-directed plans and actions. They described the MI rating scales as valued tools to support the patient’s reflections on their confidence and readiness for change and to facilitate agreements on a written rehabilitation plan comprising tailored goal-directed actions. When listening to others’ reflections during the FGs, some providers realized the potential in forgotten or unused tools, as illustrated in the following dialogue: Informant 3: “I am surprised, because I realize–while we are talking–that during the BRIDGE, I forgot the possibility of using available applications from the list (laughing)….” Informant 4: “Agree, I know the feeling…(more laughing)…I realize I could have been more conscious regarding the applications, and also the MI rating scales…we could have used these tools more often.” Informant 5*: “I think–after our discussions–that in my unit, we could have used the introduction video about rehabilitation goals…from now, I will consider to use the video-presentation at our unit” (Q 39).
Facilitate continuation in the home context and sufficient involvement of external services after discharge
Some providers linked the use of feedback and follow-up after discharge to theoretical concepts such as patients’ self-management over time and their ability to solve problems during their own rehabilitation process: “It [BRIDGE] was a reminder of the patients’ further process after discharge, and [a reminder of] the contrast related to a few weeks in our unit and plenty of weeks in the home setting…therefore, the patients’ ability to solve problems and manage is most important…and [involvement of] relevant collaborators after discharge” (Q 133*). Experienced benefit from the mandatory phone call after discharge could also lead to a high rating of follow-up as an important tool to support the patients’ process: “The patients described that they were motivated to engage in the agreed actions due to a sense of responsibility…they knew that someone would keep in touch and call them…prior to that, they would try to comply with their [rehabilitation] plan” (Q 116).
The reasons for lower ratings were either diffuse or characterized by anticipated low effectiveness in spite of limited or no experience with the tool, as illustrated in the following: “I do not know (laughing), I am not sure what I was thinking” (Q 74), and “I do not know [but have not checked] if the patients read the written plan [or used the digital graphs] afterwards” (Q 125).
Organization
Initial goal setting and tailored rehabilitation process during the first part of the stay
The introduction video about goals was a frequently omitted tool. Existing organization at the centers was in some cases suitable for the presentation of the video: “We added the video about rehabilitation goals in the first group education [a routine meeting already established in the center]” (Q 44*), and in other cases, it was not: “Admission is one by one [at our center], not groups…I did not use the video about goals, individuals could have used the tablet to watch the video alone, but…no” (Q 52*). In general, the providers’ ability to deliver the BRIDGE program was influenced by leader-led changes in schedules, for instance, to reorganize the sequence, duration, or content of goal-setting meetings during the patients’ first days after admission, and to decide which parts of the interventions were suitable in group versus individual interaction with the patients.
At some centers, the program delivery was driven only by the local coordinator and a few team members. At other centers, in contrast, the topic for current institutional quality initiatives coincided with one or several elements in BRIDGE, such as goal setting (at one center) or MI (at two centers): “As decided by the leaders, all professionals providing rehabilitation services at our workplace attended MI seminars in this period…[] to strengthen MI knowledge in the team…and [the leaders organized] a better structure in our schedules to pay more attention to goal setting, the patients’ motivation and so on” (Q 90*).
Planning for a continued and coordinated rehabilitation process
At some centers, the written rehabilitation plans improved the organization and cooperation within the team, as one provider observed: “A great benefit in our team was that the content in our meeting became more focused due to actions and goals written in the rehabilitation plan…we kind of…organized the meetings around each plan” (Q 152). Another provider noted: “…even the doctors ask for the patient’s goals now…that really did not happen earlier [prior to BRIDGE]. In addition, the work done by the occupational therapist or the nutritionist …contributions from different disciplines became more visible and specific, when reported in the template [rehabilitation plan] and we use the template every Friday [at the team meetings]” (Q 153).
Facilitate continuation in the home context and sufficient involvement of external services after discharge
Although standardized instruments for baseline assessments and outcome monitoring were included in the program, participants in the FGs focused relatively less on this topic. Some providers stated that the digital solution of data collection in the RCT required additional time and efforts in comparison with T1. Two providers described how they included evaluation of the patient’s progress on goal attainment in the mandatory follow-up conversation. Beyond that, little information was present in the transcripts regarding how or if providers used the results from the outcome measures in interactions with patients.
In a few examples, some providers outlined positive experiences when inviting persons from the patient’s work or social services to meetings before discharge. Others stated that “what we can do while the patient is here [at the institution] is to guide the patient to… better ability to self-manage, but at home…what happens when they return home…we do not know” (Q 141*). In general, information about the organization of cooperation and dialogues with next of kin or external services was scarce in the transcripts.
Integration of results from questionnaires and FGs
Evidence in the quantitative findings indicated that the structure dimension of quality of a continued and coordinated rehabilitation process were improved as intended from T1 to T2, in terms of a higher degree of available written procedures, templates, and other supporting material relevant for the interacting phases in the rehabilitation process. Furthermore, evaluation of the measurable part of the process dimension of rehabilitation quality indicated that the providers delivered most of the elements of the BRIDGE program to most of their patients. Integrating the results from the FGs led to expanded insights into how the BRIDGE program was delivered, depending on the features of the institution, the team, and/or the individual providers. The integrated results are presented in (joint display, figure). In additional file 8 (joint display, table), we present more details about how the quantitative and qualitative findings for each element in the quality improvement program are related.
Figure 3. Joint display of intended program delivery confirmed by quantitative and qualitative results, and potentials for improvements suggested by the results from at least one database. FU: follow-up; P: patient; MI: motivational interviewing.
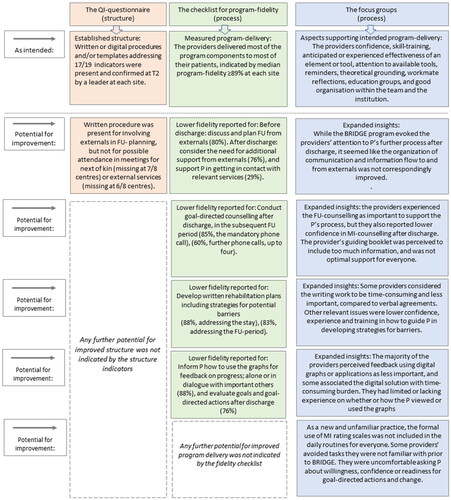
High program fidelity, as measured quantitatively, seemed to correspond with qualitative findings reflecting the providers’ confidence that they were suitably skilled to deliver what was intended and their consciousness about the components’ theoretical grounding or potential effectiveness. Other corresponding data addressed the presence of learning possibilities within the team or the institution, collective efforts to build confidence and seek experience with new tasks, and leaders who reorganized the routines and schedules to facilitate the delivery of the BRIDGE program. Conversely, lower program fidelity seemed to correspond with qualitative findings covering the same features, but then as being lacking or present to a lower degree within individuals, teams, or institutions.
Of note, the integrated view pointed to the highest quality during patient-centered goal setting and the initial phases of the rehabilitation process. It also indicated the highest potential for quality improvements regarding the use of written plans for rehabilitation, strategies for overcoming potential barriers, feedback on progress on standardized outcome measures, involvement of next of kin and external services, and tailored follow-up. Although the BRIDGE program was intended to bridge gaps between care levels, we found that this intention seemed not to be fulfilled: The quality indicators addressing next of kin and external services had the lowest pass rates, the check list items regarding involvement of next of kin and external services revealed less program fidelity, and reflections within the FGs were scarce regarding cooperation or dialogues with next of kin or external services.
Discussion
In this convergent mixed methods study, we investigated the provider perspective on how the BRIDGE program, designed to improve the quality of the rehabilitation process from admission to follow-up, was delivered and perceived by members of multidisciplinary teams from different sites. After the addition of the BRIDGE program, structural differences in quality (measured by the QIs) were improved to a high-quality level across all centers in terms of written documents for each phase in the rehabilitation process and electronic records for the standardized outcome measures being present and accessible at every site. Comparing these results with the overall high program fidelity (measured with the fidelity checklist) and statements (provided by the FGs) on improved practicing of tasks and dialogues with patients, we suggest that the BRIDGE program had the intended positive influence on both the structure and process dimensions of quality of rehabilitation for patients with RMDs. However, the further integration of FG results indicated that delivery of the BRIDGE program could be considered as a continuum from lower to higher rehabilitation quality, depending on contextual factors, such as the influence of the individual providers, team leaders, and local institutional settings. These results underline the importance of paying attention to contextual features in future quality improvement research and practice, also in the field of rehabilitation [Citation29].
Several contextual features seem to have influenced the program delivery, and some of them are worth special attention. First, some BRIDGE tasks entailed changes in the providers’ behaviors and improved conversation skills, and results from the qualitative analyses indicated that delivery of these parts of the program depended on the extent of such preparation or training. Corresponding item scores in the fidelity checklist (quantitative findings), indicated that the program fidelity was lower for the use of rehabilitation plans including strategies for barriers, feedback on progress, and MI-guided counseling after discharge. Additionally, in the qualitative findings, the providers’ statements indicated a lower perceived competence in measuring the patients’ self-efficacy in completing goal-directed actions, either during the stay or after discharge. Our results confirm previous findings by Scobbie and colleagues in 2013 [Citation30]. Although those authors included diseases other than RMDs, their evaluation pointed to the same provider challenges with the goal-setting process as we identified here, namely barriers and coping planning, appraisal and feedback, and measuring patient confidence in goal-directed actions [Citation30]. Almost 10 years ago, these aspects were perceived as novel additions to rehabilitation practice for long-term conditions [Citation30]. Our findings highlight that these aspects are still perceived as difficult to practice in daily routines. In the future, efforts are needed to improve provider competence along with suggested ways to address these difficulties.
Second, our qualitative findings indicated that high program fidelity was supported by the providers’ understanding and beliefs about the components included in the BRIDGE program. The highest fidelity in the quantitative findings addressed goal setting and the early stages of the rehabilitation process. Based on results from the FGs, the same topics were perceived as most important to support the patients’ rehabilitation process and were most frequently discussed within the team or the institution in education sessions during T2. However, as others have indicated, skilled behavior-change counseling includes, but is not restricted to, goal setting [Citation30–33]. Therefore, institutional initiatives in training and education also should address providers’ confidence and competency in action and coping planning, feedback on behavior and outcomes, and ways to build patient self-efficacy and ability to engage and sustain healthy behaviors over time, also in the face of barriers [Citation30–33]. Taken together, a set of coordinated activities is needed for providers to guide the patients towards their goals. Suboptimal attention towards some steps or aspects may influence and weaken the whole intervention.
Third, when comparing quantitative and qualitative results for similarities, we also found an apparent need for professional initiatives to discuss and establish the sufficient degree of involvement of external services and/or next of kin. It has been suggested that patients with RMDs prefer to self-manage without support from others, but their needs for tailored, supported self-management are also well documented in the literature [Citation34–38]. Therefore, providers should guide patients in problem-solving skills and strategies for coping with their challenges in daily life. Simultaneously, providers should help patients find and express their individual need for support in follow-up and maintain suitable and sufficient continuity after discharge. A variety of preferred supports are documented for people with RMDs, such as health professionals, fellow patients, employers, colleagues, stakeholders from labor and welfare services, the education system, neighbors, friends, and relatives [Citation34–38]. Active involvement of next of kin is highlighted as relevant, not only for potential support but also because of necessary adjustments between the patient and near relatives in their daily life, both at emotional and practical levels [Citation38–39].
Finally, it could be argued that the delivery of the BRIDGE program was challenged by the program itself, which comprised several interacting elements and required a number of tasks and behaviors from both providers and patients. This complexity was reflected in the relatively high number of structure indicators and items in the fidelity checklist. However, rehabilitation, by nature, is a complex and lengthy process, and the stages and components included in the program were intended to build on each other and were assumed to be equally important. In the current study, a higher program fidelity seemed to be facilitated not only by new knowledge but also by evoking knowledge established prior to BRIDGE. Some providers described this as evoking “sleeping” or “dimmed” knowledge. The providers’ expressed theoretical grounding seemed to be positively influenced by self-reflection on recommended routine practice, workmate reflections, team-based or institutional education initiatives, and reminders. The BRIDGE program was perceived as a reminder of core values in rehabilitation and seemed to motivate providers to practice tasks that they associated with high-quality rehabilitation. Also, the checklist, some passages in the guidance booklets, and other preferred BRIDGE tools seemed to prompt the providers to prepare and perform central aspects of the complex intervention. As others have indicated, providing reminders to healthcare professionals may lead to improved processes of care [Citation40–41]. The use of provider reminders seems to be of special importance for overcoming problems with information overload, time constraints, or unconscious omissions of one or several components when delivering complex interventions [Citation40–41]. Such knowledge is highly relevant to improving the quality of the complex, interacting components included in the rehabilitation process.
Strengths and limitations
The mixed methods approach was considered a strength because it resulted in expanded insight into the delivery of the quality improvement program, allowing us to focus on what was delivered as well as how it was delivered in different settings. This dual focus was made possible because the quantitative and qualitative results both addressed the concept of quality of program delivery, and we could draw inferences from the integrated data.
This study also has some limitations. First, the PR changes measured by the structure indicators at T2 might have been a response to the T1 measures, i.e., changes because of leader-initiated improvements motivated by the T1 results at each site, rather than by improvements caused by the added quality improvement program. However, in the interview-based data collection, local leaders explained to the researcher (ALSS) that written and digital BRIDGE material supplemented some lacking documents in their exisiting procedures, leading to high fulfillment of QIs at T2. We do not know to what degree local institutions developed their own written or digital documents when the BRIDGE trial was completed.
Second, the fidelity checklist was developed for the BRIDGE project and has not been tested for psychometric properties, such as test-retest reliability and validity.
Third, the fact that study researchers mentored the FGs could have led to a response bias from participants, such as under-reporting of undesirable delivery or of critical opinions about the BRIDGE program. However, the qualitative data were rich and represented various attitudes, indicating the likelihood that statements were honest and dialogues were spontaneous among the FG participants.
This study was designed to investigate quality improvements in a national RMD rehabilitation context, but the generic nature of the multidisciplinary goal-setting and self-management processes indicates that the results, knowledge, and understanding may be transferable beyond this specific project. Future studies should include patient perspectives on receiving similar programs.
Conclusion
We found that the delivery of a quality improvement program designed to enhance continuity and coordination in rehabilitation processes depended on the providers’ professional skills, their attention towards supporting tools developed to facilitate the rehabilitation process, and their professional mind in terms of theoretical grounding of activities in the rehabilitation program. Also important were organizational factors in their teams or institutions. Planning or evaluating the delivery of rehabilitation processes requires attention both to program components that can be measured quantitatively and to qualitative aspects of how to deliver them, at the levels of individual providers, teams, and institutions. Such approaches may promote equal attention to each phase from goal setting to tailored follow-up, decrease the risk of suboptimal support of patient self-management strategies over time, and reduce undesired variability in program delivery among providers and institutions.
Authors contributions
ALSS drafted the article. All authors were involved in revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. ALSS had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. Study conception and design: ALSS, GB, GJA, MA, AMB, TND, CE, IJ, HLV, HD, IK. Acquisition of data: ALSS, TND, IJ, HLV, IK. Analysis and interpretation of data: ALSS, GB, GJA, MA, AMB, TND, CE, IJ, HLV, HD, IK
Additional_file_8.pdf
Download PDF (165.8 KB)Additional_file_7.pdf
Download PDF (136.8 KB)Additional_file_6.pdf
Download PDF (102.2 KB)Additional_file_5.pdf
Download PDF (119.2 KB)Additional_file_4.pdf
Download PDF (143.7 KB)Additional_file_3.pdf
Download PDF (161.2 KB)Additional_file_2.pdf
Download PDF (142.8 KB)Additional_file_1.pdf
Download PDF (117.5 KB)Acknowledgements
The authors would like to thank all of the health professionals at the participating rehabilitation centers for their contribution to the original data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2021;396(10267):2006–2017.
- Meyer T, Gutenbrunner C, Bickenbach J, et al. Towards a conceptual description of rehabilitation as a health strategy. J Rehabil Med. 2011;43(9):765–769.
- Gimigliano F, Negrini S. The world health organization rehabilitation 2030: a call for action. Eur J Phys Rehabil Med. 2017;53(2):155–168.
- Wade D. Rehabilitation-a new approach. Overview and part one: the problems. Clin Rehabil. 2015;29(11):1041–1050.
- Norwegian Directorate of Health. Clarification of responsibilities and tasks sharing between municipalities and the specialist health care in the rehabilitation area; no. IS -947. Oslo, Norway: Norwegian Directorate of Health, 2012.
- Office of the Auditor General. The Office of the Auditor General’s investigation into rehabilitation in the health service. Document 3: 11(2011–2012). Norway: Office of the Auditor General; 2012.
- Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15(6):523–530.
- Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748.
- Jesus TS, Hoenig H. Postacute rehabilitation quality of care: toward a shared conceptual framework. Arch Phys Med Rehabil. 2015;96(5):960–969.
- Johansen I, Klokkerud M, Anke A, et al. A quality indicator set for use in rehabilitation team care of people with rheumatic and musculoskeletal diseases; development and pilot testing. BMC Health Serv Res. 2019;19(1):265.
- Liu LH, Choden S, Yazdany J. Quality improvement initiatives in rheumatology: an integrative review of the last 5 years. Curr Opin Rheumatol. 2019;31(2):98–108.
- Verburg AC, van Dulmen SA, Kiers H, et al. Patient-reported outcome-based quality indicators in Dutch primary care physical therapy for patients with nonspecific low back pain: a cohort study. Phys Ther. 2021;101(8):pzab118.
- Becker M, Breuing J, Nothacker M, et al. Guideline-based quality indicators-a systematic comparison of German and international clinical practice guidelines: protocol for a systematic review. Syst Rev. 2018;7(1):5.
- Hagen KB, Smedslund G, Østerås N, et al. Quality of community-based osteoarthritis care: a systematic review and meta-analysis. Arthritis Care Res. 2016;68(10):1443–1452. Oct
- Mahmood S, van Oosterhout M, de Jong S, et al. Evaluating quality of care in rheumatoid arthritis: the patient perspective. RMD Open. 2017;3(1):e000411.
- Rademakers J, Delnoij D, de Boer D. Structure, process or outcome: which contributes most to patients’ overall assessment of healthcare quality? BMJ Qual Saf. 2011;20(4):326–331.
- Spitaels D, Vankrunkelsven P, Grypdonck L, et al. Quality of care for knee osteoarthritis in primary care: a patient’s perspective. Arthritis Care Res. 2020;72(10):1358–1366. Oct
- Toomey E, Matthews J, Hurley DA. Using mixed methods to assess fidelity of delivery and its influencing factors in a complex self-management intervention for people with osteoarthritis and low back pain. BMJ Open. 2017;7(8):e015452.
- Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Los Angeles: Sage; 2018.
- US National Library of Medicine. 2017. The BRIDGE Rehabilitation Trial (BRIDGE) [cited 2020 Mar 20]. Available from: https://beta.clinicaltrials.gov/study/NCT03102814?distance=50&term=the%20BRIDGE%20rehabilitation%20study&rank=1
- Berdal G, Sand-Svartrud AL, Linge AD, et al. Bridging gaps across levels of care in rehabiliation of patients with rheumatic and musculoskeletal diseases: results from a stepped-wedge cluster randomised controlled trial. Clin Rehabil. 2023. Epub ahead of print. DOI:10.1177/02692155231153341
- Sand-Svartrud AL, Berdal G, Azimi M, et al. A quality indicator set for rehabilitation services for people with rheumatic and musculoskeletal diseases demonstrates adequate responsiveness in a pre-post evaluation. BMC Health Serv Res. 2021;21(1):164.
- Sand-Svartrud A-L, Berdal G, Azimi M, et al. Associations between quality of health care and clinical outcomes in patients with rheumatic and musculoskeletal diseases: a rehabilitation cohort study. BMC Musculoskelet Disord. 2022;23(1):357.
- Liamputtong P. 2011. Focus group methodology: principles and practice. London: SAGE.
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–352.
- Thirsk LM, Clark AM. Using qualitative research for complex interventions: the contributions of hermeneutics. Int J Qual Methods. 2017;16(1):160940691772106.
- Kaplan HC, Provost LP, Froehle CM, et al. The model for understanding success in quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21(1):13–20.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of health care interventions: a theoretical framework and proposed research agenda. Br J Health Psychol. 2018;23(3):519–531.
- Coles E, Anderson J, Maxwell M, et al. The influence of contextual factors on healthcare quality improvement initiatives: a realist review. Syst Rev. 2020;9(1):94.
- Scobbie L, McLean D, Dixon D, et al. Implementing a framework for goal setting in community based stroke rehabilitation: a process evaluation. BMC Health Serv Res. 2013;13:190.
- Vallis M, Lee-Baggley D, Sampalli T, et al. Equipping providers with principles, knowledge and skills to successfully integrate behaviour change counselling into practice: a primary healthcare framework. Public Health. 2018;154:70–78.
- Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clin Rehabil. 2011;25(5):468–482.
- Scobbie L, Duncan EAS, Brady MC, et al. Facilitators and “deal breakers”: a mixed methods study investigating implementation of the goal setting and action planning (G-AP) framework in community rehabilitation teams. BMC Health Serv Res. 2020;20(1):791.
- Been-Dahmen JM, Walter MJ, Dwarswaard J, et al. What support is needed to self-manage a rheumatic disorder: a qualitative study. BMC Musculoskelet Disord. 2017;18(1):84.
- Fairley JL, Seneviwickrama M, Yeh S, et al. Person-centred care in osteoarthritis and inflammatory arthritis: a scoping review of people’s needs outside of healthcare. BMC Musculoskelet Disord. 2021;22(1):341.
- Chi-Lun-Chiao A, Chehata M, Broeker K, et al. Patients’ perceptions with musculoskeletal disorders regarding their experience with healthcare providers and health services: an overview of reviews. Arch Physiother. 2020;10:17.
- Valaas HL, Klokkerud M, Hildeskår J, et al. Follow-up care and adherence to self-management activities in rehabilitation for patients with rheumatic and musculoskeletal diseases: results from a multicenter cohort study. Disabil Rehabil. 2022;44:8001–8010.
- Bergström M, Larsson Ranada Å, Sverker A, et al. A dyadic exploration of support in everyday life of persons with RA and their significant others. Scand J Occup Ther. 2021:1–12. Epub ahead of print. DOI:10.1080/11038128.2021.2007997
- Bergström M, Sverker A, Larsson Ranada Å, et al. Significant others’ influence on participation in everyday life–the perspectives of persons with early diagnosed rheumatoid arthritis. Disabil Rehabil. 2020;42(3):385–393.
- Pantoja T, Grimshaw JM, Colomer N, et al. Manually-generated reminders delivered on paper: effects on professional practice and patient outcomes. Cochrane Database Syst Rev. 2019;12(12):CD001174.
- Arditi C, Rège-Walther M, Durieux P, et al. Computer-generated reminders delivered on paper to healthcare professionals: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;7(7):CD001175.

