Abstract
Purpose
The effects of physical activity on health are well-established for chronic diseases such as multiple sclerosis (MS), Alzheimer’s disease (AD), and ischaemic heart disease (IHD). However, sustaining physical activity in everyday life is difficult. Lifeworld knowledge can help qualify interventions aimed at resolving this public health issue, but there is a gap in regard to synthesized research on peoples’ experiences with integrating and sustaining physical activity. Hence, the purpose of this review is to explore and present the available evidence on experiences with integrating and sustaining physical activity in a lived life with MS, AD, and IHD.
Methods
We conducted a scoping review with qualitative analysis and narrative syntheses in accordance with PRISMA-ScR. Based on SPIDER we ran a systematic search in Cinahl, Embase, Medline, and PsychInfo for primary qualitative research papers published until December 2022.
Results
43 papers were included. A thematic content analysis found that individuals who have MS, AD or IHD find integrating and sustaining physical activity in everyday life meaningful on several levels: Physical activity can facilitate meaningful movement with outcomes of physical, psychosocial, and existential importance.
Conclusion
The research literature presents a meaning to physical activity that extends the idea of physical fitness to one of existential movement and personal growth. In addition, our review finds that people are more likely to integrate and sustain physical activity if they feel acknowledged, supported and believe that physical activity has a meaningful purpose reflecting their sense of self. Taking a more person-centred approach in rehabilitative care might help qualify the content of physical activity in terms of integration into everyday life, but more research is needed on how to implement a person-centred approach in practice.
The research literature presents an experiential meaning to physical activity that extends the idea of physical fitness to one of more existential movement and personal growth.
To ensure the integration of physical activity in people’s everyday life, future rehabilitation interventions might benefit from adapting a more person-centred approach.
People are more likely to sustain physical activity when they feel acknowledged, supported through social relationships, can access activities adapted to their specific needs and preferences, and believe that physical activity has a meaningful purpose reflecting their sense of self.
IMPLICATIONS FOR REHABILITATION
Introduction
Physical inactivity is a major cause of at least 35 chronic diseases [Citation1] and chronic diseases are responsible for more than 86% of all deaths across the world, causing 550,000 premature deaths every year in the EU alone and costing approximately €700 billion [Citation2,Citation3].
Physical activity is defined as any bodily movement produced by skeletal muscles that results in energy expenditure [Citation4]. This could be structured and repetitive exercise such as scheduled workouts or an unstructured physical activity related to everyday life such as gardening or walking the dog. Physical activity has been shown to have a positive impact on overall health [Citation5,Citation6], and exercise represents a pillar in the treatment, prevention, and rehabilitation of many chronic diseases [Citation1,Citation7,Citation8].
Long-term exercise adherence is essential for sustaining health benefits [Citation9], and the Exercise is Medicine (EIM) initiative was introduced to advance the implementation of physical activity as a standard part of health care for the prevention and treatment of noncommunicable diseases [Citation8]. However, a significant percentage of patients undergoing a rehabilitation program for their chronic diseases drop out or do not maintain an active lifestyle after the program [Citation10–13]. This suggests that integrating and sustaining physical activity in everyday life is challenging for people with chronic diseases, and an extended understanding of their experiences seems necessary.
Some reviews have looked into patient experiences with interventions to increase physical activity in people with, e.g., multiple sclerosis [Citation14,Citation15], or acute coronary syndrome [Citation16]. However, we have not found any synthesis that maps the experiences of people with chronic diseases integrating and sustaining physical activity in everyday life. Such a study would be of value in terms of providing lifeworld perspectives on this public health challenge and providing a reference for future interventions to support long-term physical activity behaviour.
Lifeworld is a phenomenological concept built on the idea that the world is lived through experienced phenomena, making it essential to explore and present these experiences [Citation17]. Therefore, we conducted a scoping review with the aim of presenting published research findings on personal experiences and perspectives about integrating and sustaining physical activity in life while coping with chronic illnesses such as multiple sclerosis (MS), Alzheimer’s disease (AD) and ischaemic heart disease (IHD).
These diseases were chosen because they are diverse regarding underlying causes, disease onset, clinical manifestations, and symptoms affecting experiences with physical activity in everyday life.
MS is believed to be an autoimmune disease but the pathogenesis of MS is complex [Citation18]. The onset of MS often occurs in early adult life characterized by episodes of relapses with a clinical manifestation such as reduced muscular strength, coordination, energy, and cognitive function. Especially fatigue presents a barrier to physical activity [Citation19]. Furthermore, as people are often at the beginning of their adult life with what that entails of plans for the future (hopes, family, work, etc.), MS means major costs both for the individual and for society [Citation20–22].
AD is a dementia disorder that causes brain cells to die [Citation23]. The origin is thought to be a combination of genetic, lifestyle, and environmental factors [Citation24]. Age is the greatest known risk factor for AD and the age-specific prevalence almost doubles every five years after age 65 [Citation25]. AD causes cognitive impairment making it difficult to make plans and decisions in everyday life. This effects the level of physical activity in everyday life [Citation26].
IHD is often diagnosed based on an acute cardiac event that has been described as an embodied experience of pain and relief, vulnerability, loss of control on various aspects of life, and the existential challenge of a changed future [Citation27,Citation28]. People with IHD often experience a fear of being physically active [Citation29].
Furthermore, the positive effects on symptoms, progression of disease, and quality of life from physical activity are well documented for these diseases [Citation7,Citation30,Citation31]. Synthesizing experienced knowledge on physical activity from these diverse diseases provides insights within the nuances of lifeworld knowledge relevant when planning rehabilitation to a greater variety of diseases and people.
Methods
Study design
According to Peters et al. [Citation32], the indications for scoping reviews can, among other things, identify the types of evidence available in a given field, identify and analyse knowledge gaps, clarify key concepts and definitions in the literature, and identify key characteristics related to a concept. This study used the scoping review design to identify available studies and synthesize findings on the experiences and perspectives people with MS, AD, and IHD about integrating and sustaining physical activity in everyday life.
The review process was guided by the updated methodological framework for scoping reviews developed by the Joanna Briggs Institute (JBI) [Citation32] and the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [Citation33].
The study followed an iterative process that allowed the revisitation of earlier phases when encountering unexpected findings and gaining new insights. The scoping review study is not subject to ethical restrictions. A protocol is registered in the Open Science Framework [Citation34].
Searches and information sources
The search strategy aimed to identify published peer-reviewed primary studies about the personal experiences with integrating and sustaining physical activity from adult participants living with MS, IHD, or AD. The strategy was developed and aligned with the research aim and questions guided by the SPIDER search strategy tool [Citation35], as shown in Box 1.
An initial search in Cochrane was used to search for current reviews and explore search and index terms. These keywords and index terms were then tailored to each information source: Cinahl, Embase, Medline, and PsychInfo. The search was done on the 7th, 9th, and 15th of December 2022 respectively. For detailed searches in every database, see Appendix A–D in the supplementary material. Two information specialists peer-reviewed the search strategy following the PRESS guidelines [Citation36]. In addition, the reference lists of the included papers were hand-screened for additional records and run through the Web of Science, adding a snowballing effect to the database search. No filters were set on the search.
Eligibility criteria
We included papers if they comprised research findings on personal experiences of physical activity in life with a chronic illness such as MS, AD, and IHD. As our aim revolves around integration and sustainability, we specifically focused on papers attentive to experiences in everyday life and strategies to remain physically active.
Search data from databases can be found in the supplementary material. Reviews, opinion pieces, editorials, conference proceedings or similar proceedings, and publications of abstracts only were excluded.
Selecting, extracting and analysing evidence
For the management and screening process, the search results were uploaded to Covidence (https://www.covidence.org/home). Duplicates were removed automatically using the software Covidence and followed up in the screening process. In the first step of screening, two reviewers (SGR, SW) independently screened the articles according to the inclusion/exclusion criteria. If the inclusion of a study was unclear from the title and abstract, the paper was moved on to full-text screening. To validate the process, the reviewers (SGR, SW) met after screening the first 100 papers and adjusted the screening process accordingly.
In the second step of screening, four reviewers (SGR, SW, GZ, SRM) independently read full-text versions of identified articles to assess their final inclusion or exclusion, and every paper was assessed by two different reviewers. The first author (SGR) read all papers. Some papers sparked a discussion, and consensus was reached by discussing the paper with one of the other reviewers. Records of the database searches, screening, eligibility, and final inclusion of articles were logged in Covidence.
Given the nature of this review and following guidelines for scoping reviews, no critical appraisal was required [Citation32]. However, as we hoped to use results in the development of a practice, we used the Let Evidence Guide Every New Decision (LEGEND) process, an evidence appraisal of a single study focused on meaning, knowledge, attitudes, and beliefs [Citation37]. Two reviewers (SGR, SW) appraised the first 5 papers until a consensus was reached, and then the first author performed the rest of the appraisals. These findings are available in Table S1 in the supplementary material but will not be addressed in this article.
A predetermined extraction template was developed in Covidence. The template was piloted in 10 studies, discussed with an additional reviewer, and adjusted as needed. Then, data extraction from five articles was carried out independently by two researchers. Once consensus was reached on what and how to extract, the first author carried out the rest of the extractions. Details of extraction, adapted from JBI [Citation32], include bibliographic details and characteristics of the evidence source and details and results extracted from the evidence source (see Box 2).
Details on these extractions are presented in a tabular format accompanied by narrative descriptions (see Table S1 in supplementary material).
Extracted data were then further explored using qualitative thematic content analysis with inspiration from Miles, Huberman, and Saldaña; this included the close reading and rereading of the articles and the development of themes through a coding process [Citation38]. The first author (SGR) took the lead on the analysis and discussed emerging themes with the other authors. Themes are presented with narrative descriptions.
Results
A scope of published research on experiences with integrating and sustaining physical activity
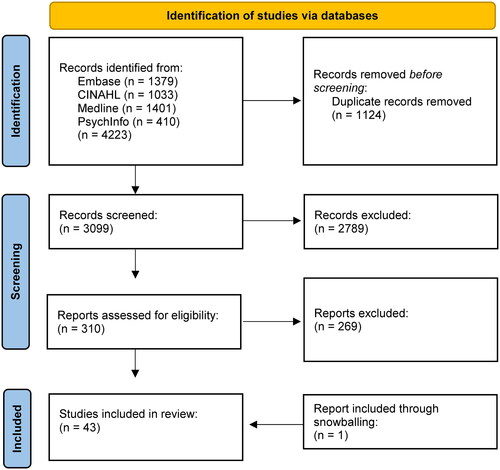
As presented in , the database search produced 3099 papers after duplicates were removed. In all, 310 papers were full text-screened, and 43 papers were included in the final review. These papers represent data from the USA [Citation39–53], UK [Citation54–64], Canada [Citation65–70], New Zealand [Citation71–73], Australia [Citation74–76], Sweden [Citation77,Citation78], Norway [Citation79], Malaysia [Citation80] and Hong Kong [Citation81]. In total, this review synthesized data from 26 studies including 459 participants with MS [Citation39–42,Citation44–52,Citation54,Citation58–60,Citation63–65,Citation67,Citation68,Citation71–73,Citation75], 12 studies including 198 participants with IHD [Citation43,Citation53,Citation55–57,Citation62,Citation70,Citation74,Citation76,Citation79–81] and 5 studies including 56 participants with AD [Citation61,Citation66,Citation69,Citation77,Citation78].
Figure 1. PRISMA Flowchart.
According to the inclusion criteria, all studies applied qualitative methods to explore experiences with physical activity, and eight also used surveys [Citation48,Citation51,Citation70–72,Citation74,Citation76,Citation80]. Fourteen studies included an intervention [Citation41,Citation47,Citation50,Citation54,Citation56,Citation58–60,Citation63,Citation65,Citation67,Citation76,Citation79,Citation81] and all but one [Citation60] of these had a focus on structured exercise. The focus on physical activity ranged from attention on activities associated with everyday life [Citation61,Citation62,Citation66,Citation69,Citation77,Citation78] to a combination of both unstructured activity and structured exercise [Citation40,Citation44–46,Citation51,Citation52,Citation57,Citation60,Citation64,Citation67,Citation71–74,Citation80] to attention only on structured exercise [Citation39,Citation41,Citation42,Citation47–50,Citation53,Citation55,Citation58,Citation59,Citation63,Citation68,Citation70,Citation75,Citation76,Citation79].
Regarding the date of publication, 10 papers were published from 2018 to 2022, 19 from 2010 to 2017, three from 2006 to 2009 and one in 1999.
Twenty-four papers used theoretical frameworks or theory to guide their study and/or to discuss their findings [Citation40,Citation41,Citation43,Citation45–49,Citation52,Citation53,Citation55,Citation56,Citation62,Citation66,Citation70–72,Citation76–81]. Furthermore, the theories were applied to understand physical activity behaviour [Citation40,Citation41,Citation43,Citation45–50,Citation56,Citation76], experiences [Citation55,Citation62,Citation66,Citation79], meaning [Citation77,Citation78], thoughts and attitude [Citation71,Citation72,Citation81], resilience processes [Citation52] and adherence [Citation53,Citation70].
A thematic scope of experiences of integrating and sustaining physical activity
The major theme developed from the content analysis is “Physical activity as a facilitator for meaningful movement”, which shows how physical activity can facilitate meaningful movement with physical, psychosocial, and existential outcomes. In this case, “meaning” and “meaningful” is not understood simply in positivist terms but in particular as phenomenological term related to the meaning people recover when being physically active. The subsequent themes of “the meaning of the self”, “the meaning of others” and “the meaning of the outside” are all interrelated and clarify how multiple factors influence the integration and sustainability of the physical activity.
Physical activity as a facilitator for meaningful movement
Numerous papers show how illness was experienced as a disruptor in life [Citation46,Citation57,Citation58,Citation68,Citation75,Citation76] and how integrating physical activity in everyday life could facilitate physical outcomes of strength and energy [Citation50,Citation51,Citation53,Citation58,Citation65,Citation68,Citation75,Citation76,Citation81] but also outcomes of psychosocial and existential nature such as perceived social impact, regained control in life and renewed or maintained sense of self [Citation40,Citation42,Citation47,Citation48,Citation52,Citation54,Citation58,Citation61,Citation64,Citation81].
These interpreted outcomes were often strengthened by theory. An example of this is Cedervall et al., who applied Harré’s theory on selfhood to their data and interpreted how physical activity was a means of maintaining selfhood when living with AD [Citation78]. Their interpretation suggested that by being physically active, the participants focused more on physical capability and activity routines and less on their illness [Citation78]. However, they found that the meaningful outcome was not an improvement of physical capacity but rather of well-being and a preserved sense of self [Citation78].
Another example is Birtwistle et al. [Citation55]. Their findings captured the sense of interrelatedness between existential and physical movement. They defined this meaningful movement as a “journey” characterized by three overlapping stages from “I can’t do what I was doing before (physically)” to “finding my way” to “accepting this way” [Citation55]. Against the backdrop of social cognitive theory and self-determination theory, they showed how these stages were very closely linked to existence and identity, especially if the participants identified themselves as physically active persons. Through different activities, these participants started to establish new parameters and understand their bodies’ capabilities, which ultimately led to a new sense of self and acceptance [Citation55].
Several other papers found experiences of increased confidence to engage in everyday life and participating in the world outside with a better social life and quality of life as outcomes [Citation50,Citation56,Citation63,Citation65,Citation66,Citation68,Citation70,Citation79]. For instance, Giacobbi et al. evaluated the quality of life after a progressive resistance training program for individuals with MS and found that enhanced muscle endurance and strength had a positive psychosocial impact on participants’ confidence in performing everyday tasks and making new friends [Citation50]. Another such example came from Horton, who found the meaningful outcomes of independence and overcoming social isolation were key motivators for sustaining physical activity: “This program, it’s not just the exercise, even though it’s a big thing… I felt like a prisoner in my own home the last year before I started the program. I had anger issues. I had frustration issues” [Citation68].
The meaning of The self
The realization of integrating and sustaining physical activity and experience of meaningful movement was influenced by a sense of self-encompassing intrinsic factors such as beliefs and knowledge about physical activity, earlier experience, positive feelings and outlook on life [Citation46,Citation49,Citation51,Citation55,Citation58,Citation62–64,Citation66,Citation68,Citation71–74,Citation77,Citation80].
An example of this was from Moore et al. [Citation62] that drew on work by Giddens and Foucault to show how what they called “engaged self-managers” had both knowledge and self-discipline for success. These participants overcame obstacles to regain confidence and independence by drawing on their own resources and experiences but also relational support. In contrast, “burdened patients” had few positive experiences to draw from and were often compromised by personal circumstances that reduced their opportunities to seek help or develop positive relationships for an improved health outcome [Citation62].
Kayes et al. even found a perceived “pointlessness” to physical activity [Citation73]. They described a fine line between the beliefs of exercise as damaging and beneficial and physical activity as a waste of time: “It’s like having a tin can with holes punched in it, no matter how much water you pour into it, it is still pouring out” [Citation73].
On the other hand, an illustration of how positive thinking could influence the integration of physical activity in life with MS was found in Hall-McMaster et al. [Citation71,Citation72]. They described how positive thinking and purposeful goals are central to motivation but also how physical activity can lead to positive thoughts and feelings, generating a positive spiral for sustaining physical activity [Citation71,Citation72].
The meaning of others
Other key elements to this meaningful movement are the psychosocial factors of support and social relations with others, such as family or peers.
Ten papers focused specifically on the family or spouses [Citation44,Citation45,Citation55,Citation56,Citation61,Citation66–69,Citation77]. The papers all agreed that family is important for integrating and sustaining physical activity, but their involvement is not without costs.
For instance, Phinney found that in an effort to help the person with AD remain involved in the world, three supportive strategies stood out [Citation69]. The families tried to reduce demands of participation, guided the person through the activity, and ensured involvement by accompanying them to activities [Citation69]. However, this level of commitment had consequences for some family caregivers who discounted their own preferences for being physically active [Citation69].
Malthouse et al. found that a loss of freedom associated with AD affected the activity levels of both people with AD and their spouses and was accompanied by feelings of blame, guilt, and worry [Citation61]. Being unable to leave the house alone meant that the spouse had to take more responsibility and could experience that their own social life grew smaller [Citation61].
Although the papers focused mostly on the positive effect of family support, carers could both facilitate and restrict physical activity out of concern and beliefs about the benefits of physical activity. This was evident in Thompson et al., who showed how a lack of knowledge could lead to “wrapping in cotton” protection and an attempt to discourage the loved one from being active [Citation56].
Support from peers came across in different ways across different studies [Citation39,Citation40,Citation43,Citation47,Citation48,Citation50,Citation52,Citation54,Citation70,Citation80]. It could be through a sense of companionship [Citation76,Citation81], camaraderie [Citation54], or fellowship [Citation53] in lifestyle changes and shared experiences.
Fasczewski et al. portrayed a feeling of important social connection and community through shared experiences about MS [Citation47]. In this study, the authors took a phenomenological approach to explore motives for participation in a “Bike MS” event. They found that participants experienced important social bonds and raised awareness of life with MS. In turn, they experienced motivation for long-term physical activity participation and outcomes of increased quality of life [Citation47].
Another example of peer support is from Rogerson et al. [Citation74]. They found that peers were experienced as positive role models and provided a sense of “if he can do it, surely I can too”, as a participant expressed it [Citation74]. In addition, these social bonds through physical activity proved to have a cyclical meaning in regard to meaningful movement because, as mentioned earlier, establishing social connections could have a meaningful psychosocial outcome for participants.
The meaning of the outside
Extrinsic factors incontrollable by the person with the illness, such as available activities, the ecological environment, and trainers’ skills and knowledge, were also reported as experiential factors related to integrating and sustaining physical activity [Citation39,Citation42,Citation43,Citation50,Citation51,Citation54,Citation56–59,Citation61,Citation67,Citation76].
The clinical manifestations of the disease itself were shown to be a factor for accessibility to activities. This was especially evident in studies on MS and AD. An example is Learmonth et al. [Citation51], who performed a study on people with MS using mobility devices. They found that a triad of strategies, such as mobility devices, equipment adaptations, and tangible support from caregivers, maximized meaningful participation in everyday activities in the family but reduced participation in organized physical activities. The physical and social spaces around available activities were seldom adapted appropriately to the needs of people with chronic diseases [Citation51].
An example of the meaning of environmental factors is presented by Traywick et al. [Citation43]. They found that physical structure, outdoor conducive spaces, weather, and a sense of safety all influenced whether participants with IHD found it meaningful to engage in physical activity [Citation43]. In regard to MS, heat is a known trigger for an attack during physical activity [Citation82]. This means that warm weather and the temperature in the gym or of the water in the pool is a factor for being physically active.
Some studies identified skills and knowledge such as personalized exercise advice through a therapeutic relationship as a key component [Citation57,Citation58,Citation60,Citation75]. An example was given by Crank et al. [Citation58], who found that building rapport with an exercise specialist who was able to adapt exercises to physical limitations while providing knowledge about safe and effective activities and suitable progression was important.
In short, the papers showed how the right activity, at the right time, is of importance and that it is imperative for the person with a disease to feel acknowledged and in competent hands. “Individualised practices are a necessary component of managing chronic illness in the lifeworld” [Citation62].
Discussion
With this review, we systematically found, synthesized, and analysed qualitative research on experiences integrating and sustaining physical activity in everyday life across chronic diseases such as MS, AD, and IHD.
The content analysis demonstrated that integration of physical activity is more likely when people feel acknowledged, experience being supported through social relationships, can access activities adapted to their specific needs and preferences, and believe that physical activity has a meaningful purpose reflecting their sense of self. Moreover, when physical activity is successfully integrated it shows meaningful outcomes of physical, psychosocial, and existential nature.
This resonate well with the aim of increasing public health through strategies such as the Exercise is Medicine (EIM) initiative [Citation8]. EIMs consist of three modules integrating clinical and community resources via the use of health technologies. The clinical module has three steps: assessment of physical activity, prescription of physical activity, and referral of patients to self-management. The community module focuses on the development of a community referral network, and active health technology with real-time feedback is used throughout the process to engage patients [Citation8].
However, our findings raise a discussion of (in)compatibility between a complex phenomenon of integrating and sustaining physical activity in life with disease and a health care strategy dominated by personal responsibility and self-management such as EIM.
In the academic literature, there is an ongoing discussion regarding the role of responsibility for illness in health care resource allocation due to increasingly scarce resources [Citation83] Responsibility within health care can mean lowering priorities for those who are blamed for their illness, penalizing those who fail to meet certain health standards or incentivizing those who do [Citation84].
An obvious argument for EIM is that it is evidence-based and cost-effective, and moreover, it is a treatment that enables people to take control and manage their own health [Citation8].
A concern could be that this puts so much emphasis on personal responsibility so that those who are not able to meet the required elements and recommendations are shamed, either by the health care system, by social constructs or by themselves. Cairney, McGannon, and Atkinson share this concern about EIM: “The onus for disease prevention is placed squarely on the individual, whose behaviour (or failure to behave correctly) becomes, itself, a cause of disease.” [Citation85].
Strengthened by a multitude of included studies grounded in theory [Citation40,Citation41,Citation46–48,Citation50,Citation52,Citation53,Citation55,Citation56,Citation62,Citation66,Citation70–72,Citation76–80], this review has shown that a health behaviour such as physical activity is influenced by intrinsic, extrinsic and social factors. Therefore, responsibility cannot be placed solely on the individual. For instance, not everyone is in a life situation where they (or their family) are capable of managing their illness and planning a structured physical activity routine. In these situations, health care professionals might take a very practical supporting role and plan with the patient. In other words, if one area of influencing factors is weak, the others might need to be that much stronger to ensure balance.
Despite an objective to present findings across dissimilar diagnoses, some differences are interesting to mention. We found that especially for MS and AD the clinical manifestations of the disease itself had an impact on people’s physical activity experiences, specifically the accessibility of activities that matched their needs [Citation51,Citation61]. In addition, we found that the active participation of family members played an especially important role for people with AD [Citation61,Citation66,Citation69,Citation77]. On the other hand, only studies on MS and IHD mentioned the importance of peer support [Citation40,Citation47,Citation54,Citation65,Citation79]. From our clinical experience peers play an important supporting role for people with AD and we were surprised to find this evidence gap.
Identifying subjective differences significant for the individual’s experience of physical activity requires an understanding of the person with the illness, his/her lifeworld, resources, and needs (physical, psychosocial, and existential). An understanding that could be achieved by shifting from the present dominating patient-centred approach to a more person-centred approach in rehabilitation. Person-centred care puts a strong philosophical emphasis on personhood and in a review of reviews from 2018 Eklund and colleagues argue that whereas the patient-centred approach has functional life as a main goal, the person-centred approach has a meaningful life as a main goal [Citation86]. This echoes with our findings and provides clinical implications for future rehabilitation intervention. Unfortunately, we found no studies on how to implement a person-centred approach in the promotion of the physical activity.
Limitations
Although we performed this scoping review in accordance with the extended PRISMA-ScR guidelines, it has certain methodological limitations. As already highlighted, the concept of integrating and sustaining physical activity in everyday life is elusive. We found it difficult to develop search terms that were broad enough for scoping purposes but narrow enough to ensure focus. In addition, we chose not to conduct a search for grey literature, as it was not feasible to search outside a Danish setting. With these choices, we anticipate that we may have missed certain relevant studies.
One thing that surprised us was the relatively small number of 12 studies involving IHD and five on AD in opposition to 26 studies on MS. We submit that age could be a factor here because when looking at the age of the participants throughout the included studies, participants in the MS studies are by far the youngest.
MS is a disease that typically is diagnosed in early adulthood, when people are starting a family, beginning their careers, and making plans for their futures. This makes a strong argument for conducting research that focuses on everyday life and lived experiences in this population because everyday life and the promise of a future suddenly present itself differently than before such a diagnosis.
Another factor could be feasibility. We know that studies involving AD patients are notoriously difficult due to their cognitive state [Citation87], but this is not necessarily true for IHD.
IHD is a disease on a global pandemic scale, and the research literature is full of studies on cardiac rehabilitation. How have so few studies focused on participants’ experiences with integrating and sustaining physical activity? We contemplate that a historic dominant focus on effect measures of treatment and rehabilitation has left little room for more philosophical paradigms in cardiac research. The acknowledgement of patients’ perspectives as evidence in health care was first acknowledged in 2010 [Citation88]. This is reflected in the date of publication of included studies in this review.
However, again, a simple explanation could be that our search strategy has missed important studies due to the difficult task of defining the phenomenon of integrating and sustaining physical activity.
Another limitation concerns the screening and extraction process. We did not calculate the inter-rater reliability and only one reviewer extracted data. However, reviewers piloted the in- and exclusion criteria thoroughly in the beginning of the process. Likewise, two reviewers abstracted data from the first five papers and when consensus was reached, one reviewer completed the data extraction.
For this review, our focus was on the experiences of people with MS, AD, and IHD, but this leaves out important studies concerning the experiences of other groups suffering from chronic disease. Nevertheless, we have limited the search to these diseases, as they are meaningfully different in how they affect everyday life and might provide knowledge that can be used to understand the experiences of integrating and sustaining physical activity from people with other diseases.
Last, the scoping review method has both strengths and weaknesses. It is much broader than a systematic review but less detailed and critical [Citation89]. Despite these limitations, we still consider this review to have provided a descriptive synthesis of experiences with integrating and sustaining physical activity in the lives of persons with MS, AD and IHD.
Conclusion and perspective
Current literature presents experiential meanings of physical activity as a concept of meaningful movement that extends the concepts of physical fitness to include psychosocial, existential, and personal growth benefits. This is important to acknowledge in rehabilitative care as the current dominating patient-centred approach aims for a functional life, whereas our findings suggest that meaningful movement enables a meaningful life.
When people feel acknowledged, experience being supported through social relationships, can access activities adapted to their specific needs and preferences, and believe that physical activity has a meaningful purpose reflecting their sense of self, then they are more likely to integrate and sustain physical activity in their life with meaningful outcomes of physical, psychosocial and existential nature.
Further development to support the integration of meaningful movement may benefit from a more person-centred approach in rehabilitative care acknowledging peoples’ lifeworld resources and needs. This however, requires more research focused on how to implement a person-centred approach. In addition, it might be necessary to perform contextual qualitative studies if the goal is to change practices, as this requires local cultural contextual knowledge.
Supplemental Material
Download Zip (116.5 KB)Acknowledgements
The authors would like to thank the following people for their contributions:
Trine G. Hamborg, MSc for her work with the search.
Graziella Zangger, PhD student for her help with screening.
Sofie R. Mortensen, PhD student, for her help with screening.
Disclosure statement
Dr. Skou is the developer of the Good Life with Osteoarthritis in Denmark (GLA:D) program, a not-for-profit initiative to implement clinical guidelines in primary care. The authors have no other conflicts of interest to declare.
Box 1. Search strategy using SPIDER.
Box 2. Extract template.
Additional information
Funding
References
- Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. doi:10.1002/cphy.c110025.
- The European Commission. [Internet]. 2022. Available from: https://ec.europa.eu/health/non_communicable_diseases/overview_en.
- European Commision. Economics of chronic diseases. 2015.[Internet]. Available from: http://www.econdaproject.com/publications_23_4222484709.pdf.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131.
- Ruegsegger GN, Booth FW. Health benefits of exercise. Cold Spring Harb Perspect Med. 2018;8:a029694. doi:10.1101/cshperspect.a029694.
- Fernández-Bustos JG, Infantes-Paniagua Á, Cuevas R, et al. Effect of physical activity on self-concept: theoretical model on the mediation of body image and physical self-concept in adolescents. Front Psychol. 2019;10:1537. doi:10.3389/fpsyg.2019.01537.
- Pedersen BK, Saltin B. Exercise as medicine - Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1–72. doi:10.1111/sms.12581.
- Lobelo F, Stoutenberg M, Hutber A. The exercise is medicine global health initiative: a 2014 update. Br J Sports Med. 2014;48(22):1627–1633. doi:10.1136/bjsports-2013-093080.
- Marcus BH, Dubbert PM, Forsyth LH, et al. Physical activity behavior change: issues in adoption and maintenance. Health Psychol. 2000;19(1S):32–41. doi:10.1037/0278-6133.19.suppl1.32.
- Bricca A, Harris LK, Jäger M, et al. Benefits and harms of exercise therapy in people with multimorbidity: a systematic review and meta-analysis of randomised controlled trials. Ageing Res Rev. 2020;63:101166. doi:10.1016/j.arr.2020.101166.
- Juhl C, Christensen R, Roos EM, et al. Impact of exercise type and dose on pain and disability in knee osteoarthritis a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014; 66(3):622–636. doi:10.1002/art.38290.
- Dalal HM, Doherty P, McDonagh STJ, et al. Virtual and in-person cardiac rehabilitation. BMJ. 2021;373:n1270. doi:10.1136/bmj.n1270.
- Heesen C, Bruce J, Gearing R, et al. Adherence to behavioural interventions in multiple sclerosis: follow-up meeting report (AD@MS-2). Mult Scler J Exp Transl Clin. 2015;1:2055217315585333. doi:10.1177/2055217315585333.
- Dennett R, Gunn H, Freeman JA. Effectiveness of and user experience with web-based interventions in increasing physical activity levels in people with multiple sclerosis: a systematic review. Phys Ther. 2018;98(8):679–690. doi:10.1093/ptj/pzy060.
- Learmonth YC, Motl RW. Physical activity and exercise training in multiple sclerosis: a review and content analysis of qualitative research identifying perceived determinants and consequences. Disabil Rehabil. 2016;38(13):1227–1242. doi:10.3109/09638288.2015.1077397.
- Guo P, Harris R. The effectiveness and experience of self-management following acute coronary syndrome: a review of the literature. Int J Nurs Stud. 2016;61:29–51. doi:10.1016/j.ijnurstu.2016.05.008.
- Galanti Grollo S. Rethinking husserl’s lifeworld: the many faces of the world in heidegger’s early freiburg lecture courses. Cont Philos Rev. 2022;55(4):487–502. doi:10.1007/s11007-022-09565-0.
- Khorooshi R, Asgari N, Morch MT, et al. Hypersensitivity responses in the central nervous system. Front Immunol. 2015;6:517. doi:10.3389/fimmu.2015.00517.
- Correale L, Martinis L, Tavazzi E, et al. Barriers to exercise and the role of general practitioner: a cross-sectional survey among people with multiple sclerosis. Front Neurol. 2022;13:1016143. doi:10.3389/fneur.2022.1016143.
- Chalmer TA, Buron M, Illes Z, et al. Clinically stable disease is associated with a lower risk of both income loss and disability pension for patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2020;91(1):67–74. doi:10.1136/jnnp-2019-321523.
- Berg J, Lindgren P, Fredrikson S, et al. Costs and quality of life of multiple sclerosis in Sweden. Eur J Health Econ. 2006;7(Suppl 2):S75–S85. doi:10.1007/s10198-006-0379-5.
- Carney P, O’Boyle D, Larkin A, et al. Societal costs of multiple sclerosis in Ireland. J Med Econ. 2018;21(5):425–437. doi:10.1080/13696998.2018.1427100.
- The Alzheimer’s Association. 2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 2020;16:390–460.
- Mayo Clinic. Alzheimers disease. [Internet]. [cited 2021 Sep 8]. Available from: https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/symptoms-causes/syc-20350447.
- Qiu C, Kivipelto M, Von Strauss E. Epidemiology of Alzheimer’s disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009;11(2):111–128. doi:10.31887/dcns.2009.11.2/cqiu.
- Gebhard D, Mir E. What moves people living with dementia? Exploring barriers and motivators for physical activity perceived by people living with dementia in care homes. Qual Health Res. 2021;31(7):1319–1334. doi:10.1177/10497323211002822.
- Merlinsuja CRN, Susila C. Lived in experience of patients with first episode of myocardial infarction - Qualitative study. Int. J. Eng. Sci. Comput. (IJESC). 2017;7:12628–12630.
- Moeini M, Naseri N, Zargham-Boroujeni A. Lived experiences of women with ischemic heart disease. Iran J Nurs Midwifery Res. 2012;17(2 Suppl 1):S137–S42.
- Farris SG, Abrantes AM, Bond DS, et al. Anxiety and fear of exercise in cardiopulmonary rehabilitation: patient and practitioner perspectives. J Cardiopulm Rehabil Prev. 2019;39(2):E9–E13. doi:10.1097/HCR.0000000000000401.
- Hernández S, Sandreschi PF, Silva D, et al. What are the benefits of exercise for Alzheimer’s disease? A systematic review of the past 10 years. J Aging Phys Act. 2015;23(4):659–668. doi:10.1123/japa.2014-0180.
- Meng Q, Lin MS, Tzeng IS. Relationship Between exercise and alzheimer’s disease: a narrative literature review. Front Neurosci. 2020;14:131. doi:10.3389/fnins.2020.00131.
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. doi:10.11124/JBIES-20-00167.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi:10.7326/M18-0850.
- Roikjær SG, Skou ST, Walløe S, et al. OSF everyday experiences of integrating and sustaining PA in life with chronic illness – A scoping review protocol. Open Science Framework. 2021. Available from: https://osf.io/w2m4c.
- Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–1443. doi:10.1177/1049732312452938.
- McGowan J, Sampson M, Salzwedel DM, et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–46. doi:10.1016/j.jclinepi.2016.01.021.
- https://www.cincinnatichildrens.org/research/divisions/j/anderson-center/evidence-based-care/legend. [Internet]. Legend Evid. Apprais. a Single Study Meaning/KAB - Qual. study. CCHMC Evidence Collaboration; 2012 [cited 2022 Mar 7]. Available from: www.cincinnatichildrens.org/evidence.
- Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: a methods sourcebook. 3rd ed. Arizona: Sage Publications Inc.; 2014.
- Chard S. Qualitative perspectives on aquatic exercise initiation and satisfaction among persons with multiple sclerosis. Disabil Rehabil. 2017;39(13):1307–1312. doi:10.1080/09638288.2016.1194897.
- Chiu CY, Griffith D, Bezyak J, et al. Psychosocial factors influencing lifestyle physical activity engagement of african americans with multiple sclerosis: a qualitative study. J Rehabil. 2016;82:25–30.
- Plow MA, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. 2009;31(20):1652–1665. doi:10.1080/09638280902738375.
- Richardson EV, Barstow E, Motl RW. Exercise experiences among persons with multiple sclerosis living in the southeast of the United States. Disabil Rehabil. 2022;44(1):79–87. doi:10.1080/09638288.2020.1757767.
- Traywick LS, Schoenberg NE. Determinants of exercise among older female heart attack survivors. J Appl Gerontol. 2008;27(1):52–77. doi:10.1177/0733464807308604.
- Ware ME, McCully KK. Impact of marriage on physical activity behavior in women with multiple sclerosis. Disabil Rehabil. 2022;44(20):5941–5949. doi:10.1080/09638288.2021.1953622.
- Wood V, Kasser SL. Spousal support and self-determined physical activity in individuals with multiple sclerosis: a theory-informed qualitative exploration. Disabil Health J. 2020;13(1):100835. doi:10.1016/j.dhjo.2019.100835.
- Dlugonski D, Joyce RJ, Motl RW. Meanings, motivations, and strategies for engaging in physical activity among women with multiple sclerosis. Disabil Rehabil. 2012;34(25):2148–2157. doi:10.3109/09638288.2012.677935.
- Fasczewski KS, Cook HM, Campbell KE, et al. I ride for MS: the impact of bike MS participation on motivation for physical activity in individuals with multiple sclerosis. Disabil Health J. 2020;13(2):100853. doi:10.1016/j.dhjo.2019.100853.
- Fasczewski KS, Gill DL, Rothberger SM. Physical activity motivation and benefits in people with multiple sclerosis. Disabil Rehabil. 2018;40(13):1517–1523. doi:10.1080/09638288.2017.1300946.
- Fifolt M, Richardson EV, Barstow E, et al. Exercise behaviors of persons with multiple sclerosis through the stepwise implementation lens of social cognitive theory. Disabil Rehabil. 2020;42(7):948–956. doi:10.1080/09638288.2018.1514077.
- Giacobbi PRJ, Dietrich F, Larson R, et al. Exercise and quality of life in women with multiple sclerosis. Adapt Phys Activ Q. 2012;29(3):224–242. doi:10.1123/apaq.29.3.224.
- Learmonth YC, Rice IM, Ostler T, et al. Perspectives on physical activity among people with multiple sclerosis who are wheelchair users: informing the design of future interventions. Int J MS Care. 2015;17(3):109–119. doi:10.7224/1537-2073.2014-018.
- Martin S, Kasser SL. The role of resilience: Physical activity continuation after falling in adults with multiple sclerosis. Disabil Health J. 2021;14(2):101046. doi:10.1016/j.dhjo.2020.101046.
- Mitchell R, Muggli M, Sato A. Cardiac rehabilitation: participating in an exercise program in a quest to survive. Rehabil Nurs. 1999;24(6):236–239. doi:10.1002/j.2048-7940.1999.tb02189.x.
- Aubrey G, Demain S. Perceptions of group exercise in the management of multiple sclerosis. Int J Ther Rehabil. 2012;19(10):557–565. doi:10.12968/ijtr.2012.19.10.557.
- Birtwistle SB, Jones I, Murphy R, et al. “Do what you can with a happy heart”: a longitudinal study of patient and family members’ lived experiences of physical activity post-myocardial infarction. Disabil Rehabil. 2022;44(14):3661–3670. doi:10.1080/09638288.2021.1878560.
- Thompson G, Wilson IM, Davison GW, et al. “Why would you not listen? It is like being given the winning lottery numbers and deciding not to take them”: semi-structured interviews with post-acute myocardial infarction patients and their significant others exploring factors that influence participa. Disabil Rehabil. 2022;44(17):4750–4760. doi:10.1080/09638288.2021.1919213.
- Coull A, Pugh G. Maintaining physical activity following myocardial infarction: a qualitative study. BMC Cardiovasc Disord. 2021;21(1):105. doi:10.1186/s12872-021-01898-7.
- Crank H, Carter A, Humphreys L, et al. Qualitative investigation of exercise perceptions and experiences in people with multiple sclerosis before, during, and after participation in a personally tailored exercise program. Arch Phys Med Rehabil. 2017;98(12):2520–2525. doi:10.1016/j.apmr.2017.05.022.
- Dennett R, Coulter E, Paul L, et al. A qualitative exploration of the participants’ experience of a web-based physiotherapy program for people with multiple sclerosis: does it impact on the ability to increase and sustain engagement in physical activity? Disabil Rehabil. 2020;42(21):3007–3014. doi:10.1080/09638288.2019.1582717.
- Fortune J, Norris M, Stennett A, et al. “I can do this”: a qualitative exploration of acceptability and experiences of a physical activity behaviour change intervention in people with multiple sclerosis in the UK. BMJ Open. 2020;10(3):e029831. doi:10.1136/bmjopen-2019-029831.
- Malthouse R, Fox F. Exploring experiences of physical activity among people with alzheimer’s disease and their spouse carers: a qualitative study. Physiotherapy. 2014;100(2):169–175. doi:10.1016/j.physio.2013.10.002.
- Moore L, Frost J, Britten N. Context and complexity: the meaning of self-management for older adults with heart disease. Sociol Health Illn. 2015;37(8):1254–1269. doi:10.1111/1467-9566.12316.
- Powell L, Cheshire A. An individualized yoga programme for multiple sclerosis: a case study. Int J Yoga Therap. 2015;25(1):127–133. doi:10.17761/1531-2054-25.1.127.
- Stennett A, De Souza L, Norris M. The meaning of exercise and physical activity in community dwelling people with multiple sclerosis. Disabil Rehabil. 2020;42(3):317–323. doi:10.1080/09638288.2018.1497715.
- Akbar N, Hazlewood S, Clement M, et al. Experiences and perceived outcomes of persons with multiple sclerosis from participating in a randomized controlled trial testing implementation of the Canadian physical activity guidelines for adults with MS: an embedded qualitative study. Disabil Rehabil. 2022;44(17):4663–4671. doi:10.1080/09638288.2021.1914199.
- Bechard LE, Beaton D, McGilton KS, et al. Physical activity perceptions, experiences, and beliefs of older adults with mild cognitive impairment or alzheimer’s disease and their care partners. Appl Physiol Nutr Metab. 2020;45(11):1216–1224. doi:10.1139/apnm-2019-0730.
- Fakolade A, Lamarre J, Latimer‐Cheung A, et al. Understanding leisure-time physical activity: voices of people with MS who have moderate-to-severe disability and their family caregivers. Health Expect. 2018;21(1):181–191. doi:10.1111/hex.12600.
- Horton S, MacDonald DJ, Erickson K, et al. A qualitative investigation of exercising with MS and the impact on the spousal relationship. Eur Rev Aging Phys Act. 2015;12:3. doi:10.1186/s11556-015-0148-5.
- Phinney A. Family strategies for supporting involvement in meaningful activity by persons with dementia. J Fam Nurs. 2006;12(1):80–101. doi:10.1177/1074840705285382.
- Sweet SN, Perrier M-JJ, Saunders C, et al. What keeps them exercising? A qualitative exploration of exercise maintenance post-cardiac rehabilitation. Int J Sport Exerc Psychol. 2019;17(4):381–396. doi:10.1080/1612197X.2017.136245810.1080/1612197X.2017.1362458.
- Hall-McMaster SM, Treharne GJ, Smith CM. ‘The positive feel’: unpacking the role of positive thinking in people with multiple sclerosis’s thinking aloud about staying physically active. J Health Psychol. 2016;21(12):3026–3036. doi:10.1177/1359105315592047.
- Hall-McMaster SM, Treharne GJ, Smith CM. Positive thinking and physical activity motivation for one individual with multiple sclerosis: a qualitative case-study. New Zeal J Physiother. 2016;44:26–32. doi:10.15619/NZJP/44.1.04.
- Kayes NM, McPherson KM, Taylor D, et al. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. 2011;33(8):625–642. doi:10.3109/09638288.2010.505992.
- Rogerson MC, Murphy BM, Bird S, et al. “I don’t have the heart”: a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140. doi:10.1186/1479-5868-9-140.
- Smith M, Neibling B, Williams G, et al. A qualitative study of active participation in sport and exercise for individuals with multiple sclerosis. Physiother Res Int. 2019;24(3):e1776. doi:10.1002/pri.1776.
- Tang CY, Blackstock FC, OʼHalloran PD, et al. A standard form of cardiac rehabilitation can improve Self-Reported positive behavior changes in the short- to Medium-Term. J Cardiopulm Rehabil Prev. 2019;39(3):175–180. doi:10.1097/HCR.0000000000000371.
- Cedervall Y, Åberg AC. Physical activity and implications on well-being in mild alzheimer’s disease: a qualitative case study on two men with dementia and their spouses. Physiother Theory Pract. 2010;26(4):226–239. doi:10.3109/09593980903423012.
- Cedervall Y, Torres S, Åberg AC. Maintaining well-being and selfhood through physical activity: experiences of people with mild alzheimer’s disease. Aging Ment Health. 2015;19(8):679–688. doi:10.1080/13607863.2014.962004.
- Morken IM, Norekvål TM, Isaksen K, et al. Increased confidence to engage in physical exertion: older ICD recipients’ experiences of participating in an exercise training programme. Eur J Cardiovasc Nurs. 2013;12(3):261–268. doi:10.1177/1474515111435885.
- Abu HB, Ludin SBM, Sowtali SNB. Understanding the development of self-efficacy for physical activity engagement in men after myocardial infarction: a preliminary qualitative study. J Public Health Res. 2021;10:2206. doi:10.4081/jphr.2021.2206.
- Wong EML, Zhong XB, Sit JWH, et al. Attitude toward the out-patient cardiac rehabilitation program and facilitators for maintenance of exercise behavior. Psychol Health Med. 2016;21(6):724–734. doi:10.1080/13548506.2015.1115107.
- Chacko G, Patel S, Galor A, et al. Heat exposure and multiple sclerosis—a regional and temporal analysis. Int J Environ Res Public Health. 2021;18:35962. doi:10.3390/ijerph18115962.
- Sharkey K, Gillam L. Should patients with self-inflicted illness receive lower priority in access to healthcare resources? Mapping out the debate. J Med Ethics. 2010;36(11):661–665. doi:10.1136/jme.2009.032102.
- Friesen P. Personal responsibility within health policy: Unethical and ineffective. J Med Ethics. 2018;44(1):53–58. doi:10.1136/medethics-2016-103478.
- Cairney J, McGannon KR, Atkinson M. Exercise is medicine: critical considerations in the qualitative research landscape. Qual Res Sport Exerc Heal. 2018;10(4):391–399. doi:10.1080/2159676X.2018.1476010.
- Eklund JH, Holmström IK, Kumlin T, et al. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ Couns. 2019;102(1):3–11. doi:10.1016/j.pec.2018.08.029.
- Beuscher L, Grando VT. Challenges in conducting qualitative research with individuals with dementia. Res Gerontol Nurs. 2009;2(1):6–11. doi:10.3928/19404921-20090101-04.
- Thorgaard K, Jensen UJ. Evidence and the end of medicine. Med Health Care Philos. 2011;14(3):273–280. doi:10.1007/s11019-011-9314-3.
- Anderson S, Allen P, Peckham S, et al. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst. 2008;6:7. doi:10.1186/1478-4505-6-7.

