Abstract
Purpose
Sensory hypersensitivity is a frequently reported complaint after acquired brain injury (ABI). This study explores patients’ perceptions of sensory hypersensitivity following ABI and its impact on everyday life.
Materials and Methods
Semi-structured interviews were conducted with 18 patients with ABI (stroke, brain tumour, TBI) who reported complaints of sensory hypersensitivity. Interview data were analysed using qualitative thematic analysis.
Results
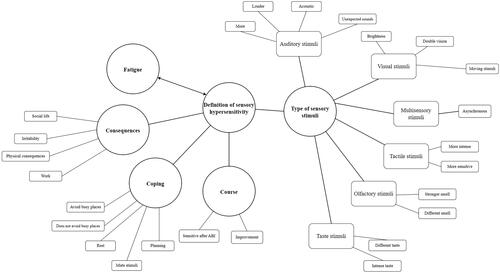
Six themes emerged from the data: (1) definition of sensory hypersensitivity, relating to individual perceptions of sensory hypersensitivity; (2) type of sensory stimuli, relating to the variety of stimuli that patients may be sensitive to; (3) course, relating to changes in sensory hypersensitivity following ABI; (4) fatigue, relating to its association with sensory hypersensitivity; (5) consequences of sensory hypersensitivity, relating to the physical, social and emotional impact of sensory hypersensitivity on patients’ lives; and (6) coping strategies, relating to behaviours used to cope with sensory hypersensitivity.
Conclusions
Sensory hypersensitivity can have a major impact on patients’ physical well-being, return to work and (social) participation after ABI. Characteristics of sensory hypersensitivity vary between patients with ABI. To develop treatments for sensory hypersensitivity, future studies should focus on cognitive (e.g., filtering information) and psychological factors (e.g., coping) in relation to sensory hypersensitivity.
IMPLICATIONS FOR REHABILITATION
Sensory hypersensitivity occurs in all types of acquired brain injury (ABI).
It is important to ask an ABI patient how sensory hypersensitivity is experienced.
It is recommended to investigate the physical (e.g., headache) and emotional (e.g., irritability, anger, frustration) consequences of sensory hypersensitivity and its impact on return to work and social participation.
When the patient mentions sensory hypersensitivity, also map cognition (with a focus on attention), fatigue, stress, and coping.
Introduction
More than 80% of patients with acquired brain injury (ABI) report experiencing sensory stimuli as very overwhelming since the injury [Citation1]. This increase in sensory sensitivity has a significant impact on their quality of life [Citation2–6]. Even though the term sensory hypersensitivity is often used to describe these complaints after ABI, there is no consensus or conceptual clarity on this phenomenon [Citation2,Citation7]. Moreover, information is lacking about how sensory hypersensitivity affects daily life functioning after ABI.
According to a previous systematic review of Thielen et al. [Citation2] research on sensory hypersensitivity after ABI is limited and primarily conducted in patients with traumatic brain injury and stroke [Citation8–10]. Moreover, the studies merely focused on sensitivity to light and noise. Sensitivity to gustatory, olfactory, tactile, vestibular, and multisensory stimuli is underexposed [Citation2]. One of the reasons hereof is that the majority of the studies use a post-concussion questionnaire (such as the Rivermead Post-Concussion Symptoms Questionnaire), which only use (single) items on hypersensitivity to light and noise [Citation11].
Little is also known about what mechanisms are responsible for sensory hypersensitivity after ABI. Some studies show associations between reduced information processing speed and an increase in sensory sensitivity [Citation12,Citation13]. Relationships to other behavioural mechanisms found in neurotypical and other clinical populations, such as attention deficits and changes in sensory thresholds, have not been found or investigated yet [Citation2]. At the neural level, there is evidence that sensory hypersensitivity after ABI is associated with insular lesions [Citation14,Citation15] and functional changes in brain activity [Citation16]. More extensive studies are however necessary to substantiate the causality in these associations.
As a result of the limited knowledge of sensory hypersensitivity, these complaints are frequently overlooked in clinical care. Moreover, there are limited evidence-based treatments for these complaints after ABI.
The aim of this study is to explore patients’ perceptions of sensory hypersensitivity following ABI and its impact on everyday life. Insight from patients’ perspectives on the characteristics and factors related to sensory hypersensitivity after ABI might provide new directions for future research on the aetiology of sensory hypersensitivity and the development of evidence-based treatments for these complaints.
Materials and methods
Findings are reported in accordance with the consolidated criteria for reporting qualitative studies (COREQ).
Design
Sensory hypersensitivity is subjective and can therefore not be directly observed [Citation2]. Therefore, sensory hypersensitivity was examined through a qualitative research design. A strength of qualitative research is that it seeks to investigate the phenomenon from the patient’s perspective in the way they experience, interpret, and attach a meaning to it [Citation17].
Participants
The patients were included if they were above the age of 18, diagnosed with ABI (stroke, brain tumour or traumatic brain injury (TBI)) by a neurologist over three months ago, and had sufficient proficiency in the Dutch language. Exclusion criteria were diagnoses of a psychotic disorder, ADHD, ASD or a primary sensory deficit (e.g., hearing loss, deafness, visually impaired or blindness), since sensory hypersensitivity can be related to these disorders [Citation18–20]. Patients were recruited from the outpatient clinic of the department of Rehabilitation, Physical Therapy Science & Sport of the University Medical Centre of Utrecht in the period from December 2019 until February 2022. The inclusion of the patients was temporarily interrupted because of the COVID-19 pandemic. During the purposive sampling process, a female rehabilitation physician [J.M.A. Visser-Meily] selected patients whose sensory hypersensitivity was the main treatment goal in rehabilitation and met the in- and exclusion criteria of the study.
All 18 patients who received an email from the treating rehabilitation physician with an invitation to participate in the study gave consent. There were no withdrawals from the study.
Participant characteristics are described in . Participants were evenly distributed in terms of sex and had a mean age of 48 years with a range of 30–77. There were 18 candidates; 6 patients who had a stroke, 6 patients with a brain tumour, and 6 patients with TBI.
Table 1. Characteristics of ABI patients (n = 18).
Materials
Interviews were conducted using a semi-structured interview guide including open-ended and probing questions concerning demographics, different sensory domains, etc. The questions contained information about demographics, different sensory domains (auditory, visual, tactile, olfactory, taste, and multisensory), consequences, and coping. The interview questions were drafted by occupational therapists, rehabilitation physicians, clinical neuropsychologists, and the research team.
Procedure
Semi-structured interviews were used to explore perceptions of sensory hypersensitivity among patients with ABI. Patients were interviewed individually by the principal investigator [I.M.C. Huenges Wajer, a female clinical neuropsychologist with a PhD in ABI and ample experience with conducting interviews in clinical care]. She was not known to the patients involved in their care, hence she introduced herself (name and profession) before the interview and explained the purpose of the study. Whereas 17 interviews were conducted face-to-face in a quiet room in the hospital, one interview took place online (videocall) as it was too intensive for the patient to travel. Subsequently, patients were asked to provide informed consent to make an audio recording of the interview and to use the data for research. After informed consent was obtained, patients were asked about their complaints regarding sensory hypersensitivity and the impact on daily life activities. If desired, a break could be inserted during the interview. The duration of each interview was approximately 45 min. All interviews were audio-recorded and no repeat interviews were conducted.
Data analysis
Descriptive statistics were used for the demographics and ABI characteristics of the patients included in this study. Prior to the analysis, all interview transcripts of the audio recordings were anonymized and transcribed with Nvivo software (v12). After transcription, the audiotapes of the interviews were deleted. Due to the lack of existing theoretical frameworks to understand and describe sensory hypersensitivity in the context of ABI, interview transcripts were analysed using inductive thematic analysis wherein themes are generated directly from the data [Citation22]. Four authors, all female (AM de Sain; L.W.M. Pellikaan; J. van Voskuilen; M. Migdis) were involved in the open coding process. The four authors coded the interviews independently. The principal investigator was consulted during the coding process if there was no consensus on a particular code. We used researcher triangulation to reduce researcher bias and increase trustworthiness. Moreover, field notes were written after each interview.
First, the researchers familiarised themselves with the interview transcripts. Second, they independently assigned codes (i.e., conceptual labels consisting of words or brief phrases) to relevant sentences or passages so as to systematically organised the data. Codes were modified and refined in discussion until consensus was reached on all codes. In the third step, codes were grouped into overarching themes and subthemes reflective of sensory hypersensitivity. Sampling continued until inductive thematic saturation was reached, which indicates that no new themes or codes were identified during analyses of the last three interviews [Citation23]. The coding scheme was made using the conventional approach. The codes were obtained directly from the data [Citation24].
Results
Six themes emerged from the data: (1) definition of sensory hypersensitivity, (2) type of sensory stimuli, (3) the course, (4) fatigue, (5) consequences of sensory hypersensitivity and (6) coping strategies. An overview of the themes and subthemes can be found in .
Figure 1. Thematic map of sensory hypersensitivity in patients with ABI.
Definition sensory hypersensitivity
Patients used different phrasing to describe how they experience sensory hypersensitivity:
Well sometimes I am sensitive for light stimuli, through sound and through crowds around me. Sometimes I can tolerate that and other times I cannot. (P1)
When I get really overstimulated, there’s actually two reactions. Either I just think; I need to get out of here now. Or I tend to when I’m overexcited to seek out even more stimuli … my head kind of races a lot more than it did before. So it is much harder, to turn my head off, as it was before the injury. (P2)
I am starting to notice it more and more. It is very difficult to describe, but I notice that my head fills up a bit more. And that I also get less and less energy, so it’s a kind of combination. And then I notice that everything that comes in has to be processed more and more and that it takes longer and longer and at a certain moment, if I do not say ‘stop’, then I just sort of get stuck in my head. (P11)
It is the intensity of stimuli. The brightness and color of some lights, bothers me the most. I have to put, for example, the brightness of the screen on my mobile phone to be as low as possible. But also in a shop, the lights can be annoying. I avoid these shops, or wear sunglasses when I go to these shops. (P8)
Type of sensory stimuli
Auditory stimuli
Sensory hypersensitivity to auditory stimuli was most frequently reported. A majority of the patients had the feeling that the sounds are louder. Other patients reported that the sounds enter as more. They have trouble distinguishing irrelevant sounds (i.e., background noise) from relevant sounds (i.e., conversation). Furthermore, almost half of the patients mention a feeling of vigilance and jumpiness as a reaction to auditory stimuli. In addition, unexpected sounds are perceived as louder, and are considered painful by the patients.:
If someone moves a bucket on the counter, it sounds like a bulldozer is passing by. Normally you focus on one sound and the rest is in the background, but now it is not in the background but just always present. (P9)
So if I am watching a volleyball match inside a hall where the sounds are very reflective, then it is not doable, but if I am on a field on a soccer field or something else then it’s doable, just fine. (P5)
Visual stimuli
Sensory hypersensitivity to visual stimuli was the second most frequently reported complaint. Moving lights seemed to bother patients the most:
Well at least I do experience it myself that if I am in a space where there are a lot of movements, for example if there are a lot of little children running around. That is what really gets into my head. (P12)
Multisensory stimuli
A majority of the patients explained that they were particularly bothered when stimuli were multisensory. For example, patients reported that they cannot watch television anymore, because of the sounds (auditory) and moving images (visual stimuli). Other places, such as shopping malls, hospitals, and birthday parties (sounds, running children, smells) are described as very intense.
So all stimuli are bad; sound, light, smell, heat or cold. The more there are, the worse it gets.(P2)
One patient mentioned that he had trouble with the synchronicity of auditory and visual stimuli:
When I get too tired. The mouth movements are not synchronous with the sounds anymore. It drives me crazy because it is very confusing. There can be a difference of 200 milliseconds sometimes.
He reported having trouble with the synchronicity of movements of the mouth and speech.
Tactile stimuli
A part of the patients reported a sensory hypersensitivity to tactile stimuli. Patients described experiencing heat and cold as more intense when they take a shower. Patients also reported that they are more sensitive to intimate touch. For example, a patient reported that she is more frightened when being touched. Especially after a busy day, when she is very hypersensitive, the patient described that her head is full and she cannot tolerate any more stimuli such as touch. Moreover, patients indicated that they were more sensitive to clothes and fabric:
I have a lot of cycling clothes. I like good clothing. I used to just leave the labels in. Nowadays I have to cut everything out, because it starts to irritate me. (P12)
I find the fabric of the duvet covers too rigid, which causes me to sleep restlessly. (P17)
Olfactory stimuli
Most patients did not report sensory hypersensitivity to olfactory stimuli. Patients had a stronger smell than before ABI, without distinguishing between nice smells and bad smells. One patient described that the smell of a fish stall has become very intense. Other patients mentioned a change in odour:
Sometimes when I’ve been working out and I’m sweating, I smell orange. (P12)
Taste stimuli
Sensory hypersensitivity in taste stimuli was the least reported. Flavours became more intense. One patient described that the taste of sauerkraut has become even tastier than before. Another patient stated a change in taste:
There are flavours that I don’t recognize anymore, like a specific drink. (P4).
Course
All the patients expressed that they became more sensitive to sensory stimuli since the ABI. The majority of the patients noticed a decrease in sensory hypersensitivity complaints in the following months after the ABI. However, the sensory hypersensitivity did not disappear completely. A part of these patients indicated that the sensory hypersensitivity bothered less because they learned how to deal with it. Some patients described that they noticed an increase in sensory hypersensitivity directly after ABI:
The first few weeks were very bad, which makes sense. The sensory sensitivity has become less, but I think I got used to it. (P7)
Fatigue
Most of the patients indicated that fatigue plays a role in sensory hypersensitivity. Patients describe that they experience more fatigue after ABI. Moreover, patients described that when they are tired, they are more sensitive for sensory stimuli. Moreover, sensitivity causes them to be more tired. Therefore, it is a reciprocal relationship. Also, even when they are not tired, they are still sensitive to sensory stimuli:
I am always sensitive for stimuli. When I get too tired, I react more violently. And when I am really, really tired, then I somehow switch everything off because then want to rest. (P3)
Consequences of sensory hypersensitivity
The patients reported many consequences of sensory hypersensitivity. These consequences can be divided into the domains of work, physical consequences, irritability, and social life.
A majority of the patients mentioned that they are not able to work anymore because of sensory hypersensitivity. A patient described that he cannot image that he used to work 40 h a week. Another patient indicated that adjustments have been made in the office:
I really need to learn to dose and I really need to avoid things that I used to do. Currently, I work four hours a week in a quiet space. I do not work in the big office garden anymore, there is no music, there is no walking through the corridor. So all of that has already been taken into account. These are all things that make it more manageable. (P5).
I never go to birthday parties anymore, or just parties. And I never do anything with more than a few people at a time. It is doable if you have a conversation with four people. If the group gets bigger. I just can’t stand that, then the people are all talking at the same time. (P17).
Coping
Patients developed different kinds of coping mechanisms for themselves in order to deal with sensory hypersensitivity. Patients use (noise cancelling) headphones or earplugs to shut themselves off from the environment, they use sunglasses to decrease the effect of visual stimuli.
To save energy, patients sleep for a few hours during the day. Patients also rest when they feel that there were too many sensory stimuli.
What I do is … rest a few times a day. Then I find a dark room. In that way, my head and my eyes actually get some rest. (P16).
Patients also mentioned that they need to plan more in their lives. They expressed that there is no more spontaneity. Before undertaking an activity they have to make a schedule:
Every day I am waking up in the morning thinking, what do we eat, what do I have? Oh no I still have to do this or that. Every day is a consideration; what am I going to do? (P16).
Discussion
This study aimed to explore patients’ perspectives on sensory hypersensitivity after ABI and its impact on their daily life activities. Patients mentioned sensory hypersensitivity in different modalities (auditory, visual, tactile, olfactory, taste or multisensory modalities) and gave different descriptions of how they experienced sensory hypersensitivity. Furthermore, results showed that sensory hypersensitivity can have physical (e.g., headache, nausea) and emotional (e.g., irritability, angry, frustrated) consequences. In addition, sensory hypersensitivity can have a major impact on (social) activities and return to work. Coping strategies and the course of sensory hypersensitivity were also identified.
In line with the systematic review of Thielen et al. [Citation2] sensory hypersensitivity in auditory and visual modalities are the most pronounced complaints among ABI patients. Patients reported that they perceive the sounds as louder and that characteristics of the stimuli (fluorescent light/blue light) and the situation or environment (acoustics) matter. In addition, a large part of the patients described that the acoustics of the environment matters. It was easier to tolerate the sounds outside in comparison with the inside because the sounds disappeared in the environment. A majority of the patients also mentioned that, in particular, multisensory stimuli (e.g., sound and visual) cause limitations in daily life. For example, it is harder to watch television. Other patients reported sensory hypersensitivity to tactile stimuli. They experience these stimuli as more intense. Boucher et al. [Citation14] found hypersensitivity to painful tactile stimulation. However, the number of studies that investigated hypersensitivity to tactile stimuli is very limited [Citation2].
A minority of the patients reported sensory hypersensitivity to olfactory and taste stimuli. A stronger smell, a more intense taste, and changes in odour were described. This is in line with the study of Mak et al. [Citation25], which showed that changes in intensity were most reported for unpleasant odours and stronger tastes.
Beside the differences in the type of sensory stimuli, patients also gave different descriptions of the process that characterises sensory hypersensitivity. It was frequently mentioned that sensory stimuli were perceived as more intense. But patients also reported that sensory hypersensitivity meant that they registered all the stimuli in the environment, both relevant and irrelevant. An increase in the intensity of sensory stimuli might be a result of a lowered neurologic threshold. A lower threshold causes the patients to respond more easily to stimuli [Citation26]. Moreover, having trouble with selecting the correct stimuli could potentially point to problems in attention. The model of Broadbent [Citation27] states that all stimuli from the environment are processed in a sensory buffer. After this sensory buffer, a part of the stimuli passes through the more advanced stage, and will eventually enter the working memory [Citation28]. This selection process, or filter, that determines of which stimuli someone will become consciousness aware, might be affected in patients with ABI. Therefore, they cannot differentiate between relevant and irrelevant stimuli.
With respect to the course of sensory hypersensitivity, most of the patients that are interviewed in this study indicated that the complaints of sensory hypersensitivity were more severe in the first weeks after the ABI. They experienced an improvement in tolerating sensory stimuli in the following months. This is in line with previous research [Citation29,Citation30]. The recovery of sensory hypersensitivity after acquired brain injury can however show some inter- and intra-individual variation [Citation4,Citation31,Citation32], which could be influenced by other factors such as medical history, coping strategies, and comorbid symptomatology.
Sensory hypersensitivity is often a persistent complaint and has multiple consequences in daily life activities. The majority of the patients in this study can for example not work because of the sensory hypersensitivity in the work environment. Furthermore, certain busy places such as restaurants are avoided because of the crowdedness, noise, and loudness. Literature has shown a similar impact of sensory changes in daily life activities in stroke survivors [Citation4].
Patients developed different coping strategies to deal with sensory hypersensitivity. Most of the patients mute the stimuli. For example, they use sunglasses when the light is too bright. Some patients mention that they avoid crowded places, like supermarkets. However, other patients describe that they do not avoid these places on purpose. They want to expose themselves to the situation. Although there is an unclear causal relationship between sensory stimuli and maladaptive coping, literature shows that coping can influence sensory hypersensitivity after ABI. For instance, the anxiety hypothesis suggests that sympathetic over-arousal, which is frequently linked to stress, can lead to hypervigilance for stimuli in the environment [Citation13]. Stress was not explicitly mentioned by the patients in the current study but was also not questioned in the interviews. Patients did mention a feeling of vigilance and jumpiness, which could potentially have a relationship with stress. Literature shows that symptoms of stress could to an elevated state of arousal, which could potentially contribute to sensory hypersensitivity in the long term [Citation26,Citation33–35]. Given the unclear causal relationship between stress and sensory changes, it could be interesting to investigate this in future research. Moreover, a reciprocal relationship with fatigue was found in the current study. Patients described that when they are tired, they are more sensitive for sensory changes. Also, sensory hypersensitivity causes them to be more tired. Mental fatigue is a common long-lasting symptom after traumatic brain injury, stroke and brain tumour [Citation36,Citation37]. One of the characteristics of this fatigue is that patients with ABI need a relatively longer time to recover from mentally exhausting activities [Citation36].
Strengths and limitations
Previous research on sensory hypersensitivity in patients with acquired brain injury focused mainly on stroke and traumatic brain injury. A strength of this study, therefore, was the diversity of the study population, in terms of multiple types of ABI, age range and gender. Moreover, this is one of the first studies to investigate a patients’ perspective on sensory hypersensitivity. However, the generalisability of these findings may be limited due to selection bias. Because the study was performed at the rehabilitation outpatient clinic, only ADL-independent ABI patients participated in this study. In addition, there were relatively many highly educated patients. Therefore, it could be questioned whether the verbalisation of the complaints is different among lowly qualified patients. Moreover, in the interviews, patients had to be able to understand the questions, express themselves and refer to examples from their daily life. Patients with severe aphasia of (severe) amnesia, were therefore not included in this study. Furthermore, no cognitive data of the patients was available.
Conclusion
In conclusion, there is no single definition of sensory hypersensitivity after ABI. ABI patients describe sensory hypersensitivity as stimuli being more intense, and/or as the inability to filter relevant from irrelevant stimuli in the environment. Moreover, patients mentioned sensory hypersensitivity in different modalities, of which sensitivity to auditory and visual stimuli was most present. In most of the interviewed patients, sensory hypersensitivity increases when stimuli are multisensory. Besides the sensory modality, other characteristics of the stimuli or environment in which the stimuli are perceived (e.g., brightness, colour, movement and acoustics) play a role. Sensory hypersensitivity is present as an acute change in sensory sensitivity since the ABI. The severity of these complaints decreases in most patients in the following months after ABI. Hypersensitivity has a major impact on social relationships, (social) activities, and return to work. Furthermore, patients report a reciprocal relationship with fatigue. The change in intensity of sensory stimuli and problems with filtering stimuli that patients experience in relationship to sensory hypersensitivity implicate that sensory hypersensitivity after ABI might be explained by different cognitive processes (e.g., change in sensory threshold or attention). In addition, psychological factors (e.g., stress) and coping strategies can be related. A broad investigation in the future is therefore recommended for a better understanding of the underlying mechanisms of sensory hypersensitivity after ABI. To develop treatments for sensory hypersensitivity, future studies should therefore focus on cognitive (e.g., filtering information) as well as psychological factors (e.g., coping) in relation to sensory hypersensitivity.
Ethical approval
This research project did not belong to the regimen of the Dutch Act on Medical Research Involving Human Subjects, and therefore there was no need for approval of a Medical Ethics Committee. Moreover, the Ethics Committee of the Faculty of Social and Behavioural Sciences of Utrecht University approved the study.
Supplemental Material
Download MS Word (34.9 KB)Acknowledgement
We thank the participants for sharing their stories and experiences.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Research data are not shared due to privacy restrictions.
Additional information
Funding
References
- Thielen H, Huenges Wajer IMC, Tuts N, et al. The multi-modal evaluation of sensory sensitivity (MESSY): assessing a commonly missed symptom of acquired brain injury. Clin Neuropsychol. 2023;8:1–35. doi: 10.1080/13854046.2023.2219024.
- Thielen H, Tuts N, Welkenhuyzen L, et al. Sensory sensitivity after acquired brain injury: a systematic review. J Neuropsychol. 2022;00:1–31.
- Shepherd D, Landon J, Kalloor M, et al. The association between health-related quality of life and noise or light sensitivity in survivors of a mild traumatic brain injury. Qual Life Res. 2020;29(3):665–672. doi: 10.1007/s11136-019-02346-y.
- Alwawi DA, Dean E, Heldstab A, et al. A qualitative study of stroke survivors’ experience of sensory changes. Can J Occup Ther. 2020;87(4):298–306. doi: 10.1177/0008417420941975.
- Carlsson GE, Möller A, Blomstrand C. A qualitative study of the consequences of ‘hidden dysfunctions’ one year after a mild stroke in persons <75 years. Disabil Rehabil. 2004;26(23):1373–1380. doi: 10.1080/09638280400000211.
- Carlsson GE, Möller A, Blomstrand C. Managing an everyday life of uncertainty- -a qualitative study of coping in persons with mild stroke. Disabil Rehabil. 2009;31(10):773–782. doi: 10.1080/09638280802638857.
- Scheydt S, Müller Staub M, Frauenfelder F, et al. Sensory overload: a concept analysis. Int J Ment Health Nurs. 2017;26(2):110–120. doi: 10.1111/inm.12303.
- Nelson LD, Kramer MD, Patrick CJ, et al. Modeling the structure of acute sport-related concussion symptoms: a bifactor approach. J Int Neuropsychol Soc. 2018;24(8):793–804. doi: 10.1017/S1355617718000462.
- Chung SM, Song BK. Evaluation of sensory processing abilities following stroke using the adolescent/adult sensory profile: implications for individualized intervention. J Phys Ther Sci. 2016;28(10):2852–2856. doi: 10.1589/jpts.28.2852.
- Knoll RM, Lubner RJ, Brodsky JR, et al. Auditory quality-of-life measures in patients with traumatic brain injury and normal pure tone audiometry. Otolaryngol Head Neck Surg. 2020;163(6):1250–1254. doi: 10.1177/0194599820933886.
- King NS, Crawford S, Wenden FJ, et al. The rivermead post concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242(9):587–592. doi: 10.1007/BF00868811.
- Kumar S, Rao SL, Nair RG, et al. Sensory gating impairment in development of post- concussive symptoms in mild head injury. Psychiatry Clin Neurosci. 2005;59(4):466–472. doi: 10.1111/j.1440-1819.2005.01400.x.
- Shepherd D, Landon J, Kalloor M, et al. Clinical correlates of noise sensitivity in patients with acute TBI. Brain Inj. 2019;33(8):1050–1058. doi: 10.1080/02699052.2019.1606443.
- Boucher O, Turgeon C, Champoux S, et al. Hyperacusis following unilateral damage to the insular cortex: a three-case report. Brain Res. 2015;1606:102–112. doi: 10.1016/j.brainres.2015.02.030.
- Cantone M, Lanza G, Bella R, et al. Fear and disgust: case report of two uncommon emotional disturbances evoked by visual disperceptions after a right temporal- insular stroke. BMC Neurol. 2019;19(1):193. doi: 10.1186/s12883-019-1417-0.
- Astafiev SV, Zinn KL, Shulman GL, et al. Exploring the physiological correlates of chronic mild traumatic brain injury symptoms. Neuroimage Clin. 2016;11:10–19. doi: 10.1016/j.nicl.2016.01.004.
- Ochieng PA. An analysis of the strengths and limitation of qualitative and quantitative research paradigms. Probl. Educ. 21st Century. 2009;13:13–18.
- Bijlenga D, Tjon-Ka-Jie JYM, Schuijers F, et al. Atypical sensory profiles as core features of adult ADHD, irrespective of autistic symptoms. Eur Psychiatry. 2017;43:51–57. doi: 10.1016/j.eurpsy.2017.02.481.
- Landon J, Shepherd D, McGarry M, et al. When it’s quiet, it’s nice: noise sensitivity in schizophrenia. (2016). Am. J. Psychiatr. 2016;19(2):122–135.
- Tavassoli T, Hoekstra RA, Baron-Cohen S. The sensory perception quotient (SPQ): development and validation of a new sensory questionnaire for adults with and without autism. Mol Autism. 2014;5(1):29. doi: 10.1186/2040-2392-5-29.
- Verhage F. Intelligentie en Leeftijd Onderzoek bij Nederlanders Van Twaalf tot Zevenenzeventig Jaar [Intelligence and Age Research with Dutch People Aged Twelve to Seventyseven Years]. Assen: Van Gorcum Prakke en Prakke; 1964.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual. Res. in Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa.
- Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687.
- Mak YE, Simmons KB, Gitelman DR, et al. Taste and olfactory intensity perception changes following left insular stroke. Behav Neurosci. 2005;119(6):1693–1700. doi: 10.1037/0735-7044.119.6.1693.
- Dunn W. The impact of sensory processing abilities on the daily lives of young children and their families: a conceptual model. Infants Young Child. 1997;9(4):23–35. doi: 10.1097/00001163-199704000-00005.
- Broadbent DE. Perception and communication. Oxford, UK: Oxford University Press;1958
- Carrasco M. Visual attention: the past 25 years. Vision Res. 2011;51(13):1484–1525. doi: 10.1016/j.visres.2011.04.012.
- Shepherd D, Heinonen-Guzejev M, Heikkilä K, et al. Sensitivity to noise following a mild traumatic brain injury: a longitudinal study. J Head Trauma Rehabil. 2021;36(5):289–301.
- Barker-Collo S, Theadom A, Starkey N, et al. Factor structure of the rivermead post- concussion symptoms questionnaire over the first year following mild traumatic brain injury. Brain Inj. 2018;32(4):453–458. doi: 10.1080/02699052.2018.1429659.
- Rabinowitz AR, Fisher AJ. Person-specific methods for characterizing the course and temporal dynamics of concussion symptomatology: a pilot study. Sci Rep. 2020;10(1):1248. doi: 10.1038/s41598-019-57220-1.
- Truong JQ, Ciuffreda KJ, Han MH, et al. Photosensitivity in mild traumatic brain injury (mTBI): a retrospective analysis. Brain Inj. 2014;28(10):1283–1287. doi: 10.3109/02699052.2014.915989.
- Callahan ML, Storzbach D. Sensory sensitivity and posttraumatic stress disorder in blast exposed veterans with mild traumatic brain injury. Appl Neuropsychol Adult. 2019;26(4):365–373. doi: 10.1080/23279095.2018.1433179.
- Elliott JE, Opel RA, Weymann KB, et al. Sleep disturbances in traumatic brain injury: associations with sensory sensitivity. J Clin Sleep Med. 2018;14(7):1177–1186. doi: 10.5664/jcsm.7220.
- Harvey AG, Bryant RA. Acute stress disorder: a synthesis and critique. Psychol Bull. 2002;128(6):886–902. doi: 10.1037/0033-2909.128.6.886.
- Johansson B, Ronnback L. Evaluation of the mental fatigue scale and its relation to cognitive and emotional functioning after traumatic brain injury or stroke. Int. J. Phys. Med. Rehabil. 2014;2(01):572–573.
- Asher A, Fu JB, Bailey C, et al. Fatigue among patients with brain tumors. CNS Oncol. 2016;5(2):91–100. doi: 10.2217/cns-2015-0008.

