?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Aims
A novel professional training was developed to reduce stigma toward harm reduction and pharmacotherapy for substance use disorders.
Methods
The training was delivered over three sessions to n = 147 health professionals in Utah between 2019 and 2020, including n = 40 substance use disorder treatment professionals. Pre and post-training survey measures provided evaluation information on knowledge, attitudes, and planned action regarding harm reduction and pharmacotherapy. Items were grouped into a stigma score, and multilevel modeling, regression analyses, and McNemar tests were used to quantify changes in overall stigma toward harm reduction interventions both before and after the training.
Results
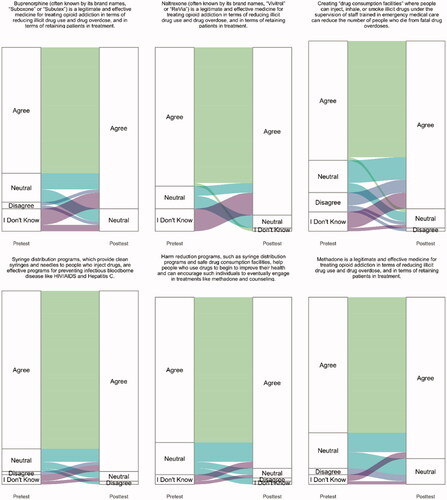
The training significantly decreased the total stigma score toward harm reduction (b = −0.09, p < .001, β = −0.34). At the individual item level, 6 of the 22 items showed significant change in reduced stigma (all p < .047), and all items moved in the direction of decreased stigma. These items include both attitudes and planned action aspects of the total stigma score.
Conclusions
This study suggests that education targeting prejudice and discriminatory actions against harm reduction and pharmacotherapy interventions among healthcare professionals may contribute to stigma reduction. These results provide a basis for intervention effectiveness, addressing preconceived ideas, and show community need for such substance use interventions, as a component of future stigma reduction efforts.
Introduction
Harm reduction refers to a range of evidence-based approaches that help to reduce the negative consequences of substance use. This includes pharmacotherapy for opioid use disorders (OUDs), especially opioid agonist treatments like methadone or buprenorphine, syringe distribution programs, and overdose reversal medication distribution. These approaches have a number of benefits, including a lowered risk of infectiousdisease transmission (Aspinall et al., Citation2014; MacArthur et al., Citation2012), reduced fatal overdoses (Doe-Simkins et al., Citation2014; Soyka et al., Citation2011; Walley et al., Citation2013), as well as retention in treatment programs (Bao et al., Citation2009; Kakko et al., Citation2003; Mattick et al., Citation2014).
Despite robust research demonstrating effectiveness, these interventions are not widely accepted or implemented. A possible explanation for this could be the presence of stigma toward implementing these interventions. Stigma is the process by which an attribute leaves one prone to prejudice and discrimination (Goffman, Citation1963). Stigma significantly affects the lives of people who use drugs by reducing access to care and housing (Couto e Cruz et al., Citation2018; Hatzenbuehler & Phelan, Citation2013;Lloyd, Citation2013; von Hippel et al., Citation2018; Yang et al., Citation2017). In this case, stigma attaches to substance use itself andaffects the harm reduction and pharmacotherapy services patients receive. Despite their evidence base, some health providers approach these treatments with skepticism.
In a process known as 'intervention stigma' (Madden, Citation2019), individuals involved with harm reduction services (Crawford et al., Citation2014; Gatewood et al., 2016) and medication treatment for OUDs, especially methadone and buprenorphine (Chaar et al., Citation2013; Gordon et al., 2011; Madden, Citation2019; Ramirez-Cacho et al., Citation2007), may also become the target of discrimination and prejudice. With intervention stigma, it is the provision of particular treatments or services that may subject individuals to mistreatment or stigma. Conversely, individuals who access abstinent-based services may not face similar prejudices (Hatcher et al., Citation2018; Madden, Citation2019).
Broadly speaking, health care professionals strive to be compassionate and show empathy when it comes to treatment, even for patients they find to be difficult (Sulzer et al., Citation2015; Sulzer et al., Citation2016). However, stigma toward harm reduction and pharmacotherapy persists among health care professionals. Studies of people who use drugs indicate experiences of discrimination and prejudice from health care providers when seeking syringes (Davidson et al., Citation2012), methadone (Harris & McElrath, Citation2012; Paquette et al., Citation2018), or buprenorphine (Allen & Harocopos, Citation2016). Specialized and non-specialized healthcare providers themselves also report stigmatizing attitudes and actions. These actions can include refusing to distribute syringes, assuming syringe distribution participation will result in increased drug use (Crawford et al., Citation2014), or believing that methadone and buprenorphine are illegitimate interventions and refusing to participate in pharmacotherapy (Chaar et al., Citation2013; Livingston et al., Citation2018; Madden, Citation2019). This 'provider-based stigma,' or stigma among individuals tasked with helping marginalized groups (Pescosolido & Martin, 2015) in the context of healthcare can create barriers to accessing high-quality health services, such as syringe programs (Davidson et al., Citation2012), medication treatment (Peterson et al., Citation2010), and non-specialized health services, including hospital-based carefor co-occurring conditions (McNeil et al., 2014; Kimmel et al., 2020).
Intervention stigma toward harm reduction and pharmacotherapy has gained significant attention as a barrier to care in recent years (Olsen & Sharfstein, 2014; Wakeman & Rich, Citation2018). Availability of harm reduction in the U.S. differs by geography (Cummings et al., 2014; Dick et al., 2015; Faul et al., 2015; Rosenblatt et al., Citation2015), and resistance to uptake may be partially tiedto stigma. Recent studies of both primary care providers (McGinty et al., 2020) and residential treatment programs (Beetham et al., 2020) for opioid use disorders show low participation in pharmacotherapy. In an audit study of residential treatment facilities, 21% of program representatives actively discouraged study callers from using pharmacotherapy for opioid use disorders (Beetham et al., 2020). Similarly, a nationally representative study of primary care providers indicated that one-third of providers did not agree that pharmacotherapy for opioid use disorders is more effective than nonmedication treatment (McGinty et al., 2020). Therefore, a significant percentage providers may benefit from education addressing negative perceptions of pharmacotherapy.
However, few studies examine how to address provider-based intervention stigma toward harm reduction and pharmacotherapy (Bland et al., Citation2001; Crapanzano et al., Citation2014). Extant studies on provider-based stigma and substance use focus largely on stigma toward people who use drugs but not on treatment modalities or other interventions used to address substance use. As such, they fail to acknowledge that providers may be more or less open-minded to different substance use interventions, regardless of the evidence base.
The few studies seeking to directly address provider-based intervention stigma have mixed outcomes (Crawford et al., Citation2014; Friedmann et al., Citation2015). For example, an intervention testing the effects of providing syringe distribution education and ongoing implementation support to community pharmacy personnel in New York found few changes to self-reported attitudes and no changes to pharmacy syringe distribution participation (Crawford et al., Citation2014). However, a study testing education and organizational linkages between U.S. medication treatment programs for OUDs and community corrections officials found increased intent to refer clients to pharmacotherapy for OUDs, greater familiarity with methadone, and reduced negative perceptions of pharmacotherapy among corrections personnel (Friedmann et al., Citation2015).
Other studies also suggest that misperceptions of harm reduction and pharmacotherapy may be drivers of provider-based stigma. Misperceptions can include the lack of familiarity among non-specialized providers in addressing substance use (Livingston et al., Citation2018) as well as beliefs that these harm reduction methods increase substance use (Knudsen et al., Citation2005; Winograd et al., Citation2017).
Changing stigmatizing attitudes may be possible with professional education, although the research is mixed. Education on pharmacotherapy for OUDs may produce greater stigma reductions than education on harm reduction interventions (Crawford et al., Citation2014; Friedmann et al., Citation2015). However, neither case explores how education may be effectively delivered to healthcare professionals working in the substance use disorder (SUD) treatment field. This population differs from community pharmacy personnel and corrections officials, who often do not have specialized training toward care for people who use drugs. SUD treatment professionals do have such training yet may still harbor intervention stigma toward pharmacotherapy for OUDs or harm reduction approaches (Madden, Citation2019; Olsen & Sharfstein, 2014; Knudsen et al., Citation2005).
This study explores the effect of a novel curriculum on reducing self-reported stigma toward harm reduction and opioid agonist (methadone and buprenorphine) and antagonist (naltrexone) treatment for OUDs among SUD treatment professionals. Given the strong evidence bases for pharmacotherapy for OUDs and harm reduction approaches, effective interventions that address provider-based stigma have the potential to improve services offered in marginalized communities. Reducing stigma toward harm reduction and pharmacotherapy may contribute to increased ability to promote patient-centered care by improving referrals to appropriate services, improving the ability to provide comprehensive patient education, and ultimately improving care quality for people who use drugs.
Methods
Curriculum design
The curriculum for this training was developed based on a forthcoming systematic review, and in collaboration with harm reduction professionals, people with substance use disorders, tribal community members, and a community advisory board in Utah. The systematic review identified drivers of intervention stigma toward harm reduction and pharmacotherapy for OUDs. These drivers included the following: 1) false ideas about the effects of pharmacotherapy and harm reduction on patients or communities; 2) lack of knowledge of the evidence base for interventions; and 3) lack of knowledge of the extent to which the local service population has poor substance use outcomes that could be addressed with specific harm reduction services or medication treatment.
To respond to the stigma factors identified in the systematic review, an eight-hour training was developed using an interactive contact-based educational session and a curriculum that explicitly addressed preconceived ideas about intervention effects, provided an overview of the science underlying harm reduction and pharmacotherapy, and provided local data and statistics about SUDs. The curriculum also included first-hand stories about the need for harm reduction in the local community. The senior author and a local harm reduction practitioner who recovered from a SUD co-taught the course. After the eight-hour training was delivered to providers for feedback, it was revised into a four-hour curriculum and delivered to additional groups of health professionals.
Participants
The training consists of a one-time session, and was delivered three times between July 2019 and June 2020. It was delivered twice at in-person training sessions in Utah (once in a rural county and once in an urban county), and delivered once in a synchronous online session that included participants from geographic locations across the United States. Participants were primarily from the target population of SUD counselors (n = 40); however, 38% of attendees were other health and public health professionals, including primary care providers and County and State Department of Health employees. The (redacted for blind review) IRB determined the training evaluation to be non-human subjects research.
Measures
A survey measuring stigma toward harm reduction and pharmacotherapy for OUDs (methadone, buprenorphine, and naltrexone) was delivered prior to the training and immediately following the training to assess knowledge, attitudes, and intention to act. Eight of the survey questions gathered demographic and professional data. Twenty-four Likert scale questions assessed agreement with stigmatizing attitudes toward harm reduction or pharmacotherapy (e.g. 'Patients who take methadone or buprenorphine are no different than people who still use illicit opioids like heroin'), knowledge of factual or non-factual statements about harm reduction approaches (e.g. 'Creating drug consumption facilities where people can use illicit drugs under the supervision of trained staff will increase addiction rates'), and intention to act (e.g. 'I intend to promote harm reduction or correct myths in conversations with my colleagues at my work site in the next six months') (See Appendix 1 for complete survey). The responses were coded so that a higher score indicated greater stigma and disagreement with harm reduction principles and evidence. A mean score was then calculated across items to create a total stigma score. This total score treated 'I don't know' responses as non-data points.
The items used for the "total score" were selected with guidance from the systematic review of research on stigma toward harm reduction and pharmacotherapy. Attitude statements were drawn from research on stigma toward harm reduction and pharmacotherapy that identified common negative perceptions held by individuals averse to these interventions (e.g. Livingston et al., Citation2018; Smye et al., Citation2011). Knowledge questions were also drawn from research in the review indicating common misperceptions of these interventions (e.g. Rieckmann et al., Citation2007; Rieckmann et al., Citation2014). Questions about participation in harm reduction and pharmacotherapy were likewise drawn from research on enacted stigma among professionals (e.g. Crawford et al., Citation2014; Livingston et al., Citation2018; Rieckmann et al., Citation2007). To assess its ability to measure the intended constructs in this sample, internal consistency, construct validity, and face validity were tested. For internal consistency, Cronbach's alpha was used, with any value above .80 having high reliability. For face validity, the team that reviewed the survey included members of the target group. Lastly, for construct validity, the team assessed its relationship to well-known correlates (e.g. experience in harm reduction) as well as variables with which it should not correlate (e.g. race, gender).
Data analysis
To assess the impact of the program, three main analyses were used: 1) descriptive statistics, 2) multilevel modeling, and 3) linear regression. Descriptive statistics were used to understand the characteristics of the participants. Multilevel modeling, specifically linear mixed-effects modeling, was used to assess the impact of the program from pre-training to post-training. For this, the total score was the dependent variable with the time point (i.e. pretest or posttest) the main independent variable. The model can be expressed as:
where
is the total score for person i at time t,
is the estimate of interest,
is the random intercept by participant, and covariates being training setting (i.e. in-person or virtual) and participant professional characteristics (i.e. SUD professional, harm reduction experience).
Linear regression was then used to assess whether there were any differential impacts by participant characteristics. These analyses assessed whether any participant characteristics predicted the change in stigma score from pretest to posttest. Specifically, the models assessed posttest scores predicted by whether the respondent was a SUD professional, their years of professional treatment experience, and whether they had previous harm reduction experience, while controlling for pre-training scores. Due to heteroskedasticity of the residuals, the robust standard error (i.e. the White Heteroskedasticity adjustment) was used. In addition to these core analyses, a series of McNemar tests were used to understand the individual features that showed change from pretest to posttest.
All participants who had pre-training and post-training survey scores were included in the analyses. Assumptions of the models were checked for each approach. All analyses were done in the R statistical environment (R Core Team, Citation2020; RStudio Team, Citation2019) using the tidyverse (Wickham et al., Citation2019), gtsummary (Sjoberg et al., Citation2020), lme4 (Bates et al., 2015), lmtest (Zeileis & Hothorn, Citation2002), sandwich (Zeileis, Citation2004), and ggalluvial (Brunson, 2017) packages. All code and output, including all linear mixed effect models and regression tables, are available at https://osf.io/vygeh/.
Results
A total of 147 individuals participated in the trainings, with 110 responding to at least one of the surveys. Note that ten individuals did not respond to the surveys and 27 were not provided the pretest survey and as such were not included in the 110 participants. Of these 110 participants, 65 responded to both the pre-training and post-training surveys. Given that the core question was the training's effects on self-reported stigma, it was essential to analyze participant responses from both the pre- and post-training surveys. For this reason, only participants with complete pre- and post-training data were used in this analysis. Of the 110 that did not respond, 2 did not respond to the pretest and 43 did not respond to the posttest. Those 43 that provided demographic information were compared to the remaining sample of 65. Compared to the sample of 65 used in the study, those missing were more likely to be women (62% in complete sample vs. 82% in the missing sample, p = .005) but otherwise did not differ from the sample analyzed.
Of the participants that had pretest and posttest data, more than half were SUD professionals, with an average of 9 (SD = 7) years of work experience. Only 22% had prior experience in harm reduction. The average age of the sample was 41 (SD = 11). provides more detail on the characteristics of the participants.
Table 1. Demographic characteristics of the sample.
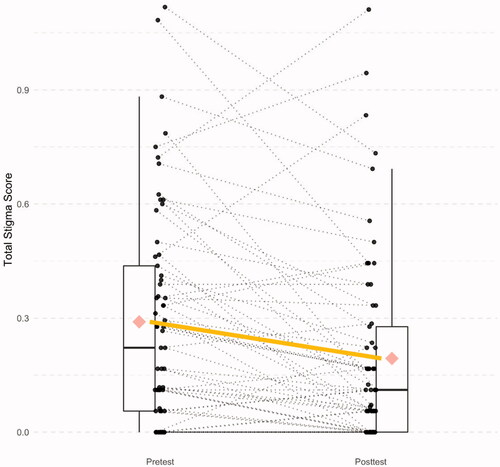
The total stigma score ranged from 0 to 1.1 and had high internal consistency (Cronbach's alpha = .83). It matched expectations for construct validity with correlations to having experience in harm reduction (rho = .247), being a SUD professional (rho = .161), and having more education (.144). Further, as expected, the total stigma score lacked correlations with age, race, and gender (all rho < .045). The effect of the training from pretest to posttest is illustrated in , which shows that the majority of individuals exhibited decreases in stigma from pre-training to post-training survey responses. This finding was corroborated by the multilevel model: the training significantly reduced total stigma scores from pretest to posttest, with a small-to-moderate standardized effect size (b = −0.09, p < .001, β = −0.34). This effect was still significant when controlling for training setting (i.e. in-person or virtual) and participant professional characteristics. Neither the participants' status as SUD professional or nonprofessional, nor their previous experience in harm reduction impacted overall scores (both p > .08).
Figure 1. Changes from pretest to posttest, where the solid thick line is the average change and the dotted lines are the individual changes.
Analyses also examined whether the training had a differential effect for particular groups of participants. This analysis provides information on predictors of change from pretest to posttest. Specifically, differences in posttest (when controlling for pretest scores) were tested for whether the respondent was a SUD professional, their years of professional treatment experience, and whether they had previous harm reduction experience. The analysis also compared the delivery mechanism (online vs. in-person). None of these variables significantly predicted change (all p > .30).
At the individual survey item level, six of the 22 items showed significant change (all p < .047). These items included agreement with statements regarding methadone, buprenorphine, naltrexone, syringe distribution, and safe drug consumption facilities. shows the responses to these items and how they changed from pretest to posttest. These responses consistently demonstrated reduced stigma in post-training surveys. In general, individuals who responded 'I don't know' or 'Neutral' in pre-training surveys tended to agree with the statement in the post-training survey. Very few disagreement responses were seen for pretest or posttest. All other items did not show significant change from pretest to posttest. For many of these remaining items, there was no change because the participants already held the attitudes and beliefs that the course was designed to promote.
Discussion
The novel training developed and tested in this study shows promising preliminary evidence of reducing stigma toward several harm reduction interventions and pharmacotherapy for OUD among healthcare providers. Previous research on addressing stigma has focused on reducing prejudicial attitudes toward people who use drugs (Livingston et al., 2012). Still, there is very limited research on stigma toward harm reduction interventions and medication treatment modalities.
Our curriculum draws from a comprehensive literature search and operationalizes the guidance and feedback of scholars at the forefront of this field, along with input from tribal and community advisory board members. The reduction in stigma from the delivery of this curriculum suggests that we have successfully operationalized the best recommendations of the field. The results of this educational intervention study may indicate that misinformation and lack of knowledge of substance use harm reduction and pharmacotherapy for OUDs are significant drivers of provider-based stigma; however, such causal claims cannot be established with the current study design. While we anticipate additional improvements can be made to our curriculum and approach across time, it is notable that we were able to identify such a clear and positive trend from the first iterations of the training onwards. The evidence from this study suggests that the findings of the systematic review upon which this training has been based can be operationalized into real-world contexts.
Best practices for effectively addressing intervention stigma toward harm reduction and pharmacotherapy will likely require a multi-pronged approach that includes structural change through policy and resource investment, as well as organizational and professional-level education efforts for people working in the health sector. By significantly decreasing stigma toward harm reduction, this training provides one of the first models of what professional education targeting stigma may look like in the context of substance use harm reduction and OUD pharmacotherapy treatment. This is a crucial development, given the substantial evidence of the efficacy of these interventions, and the persistent stigmas toward them that continue today among many providers.
Our training was undoubtedly improved by pairing a harm reduction science expert with a practicing harm reduction activist. This likely made participants from a variety of backgrounds comfortable asking questions and engaging with the material. This pairing may also have demonstrated an underlying assumption of the value of lived experience and knowledge. Combining these epistemological orientations may have made the training more accessible to people from a variety of backgrounds, especially given that this is a sensitive topic prone to stigmatizing beliefs. In fact, two of the health professionals who joined our trainings were from law enforcement, and we anticipate that it would be well-received among that population.
Additionally, this training was offered effectively both in-person and online. Our results showed no meaningful difference in our measures regardless of delivery modality. This is notable, especially in the COVID-19 era. With evidence that online delivery provides a comparable stigma reduction result, this training may be a promising option for more widespread online delivery in the future.
There were some limitations to this study, including the number of participants who did not fully complete both a pre- and post-training survey. Additionally, the lack of a control arm prevents inference regarding whether a training on a related matter could have similarly reduced some amount of stigma. Lastly, the face-to-face trainings were conducted exclusively within one region of the United States and may not be translatable across other contexts. It is possible that bias toward OUD pharmacotherapy and substance use harm reduction approaches may have considerable geographic and cultural variations. Research already shows geographic, socioeconomic, and racial/ethnic differences in methadone versus buprenorphine treatment (Hansen et al., 2013), and that access to syringe programs is concentrated in urban areas (Des Jarlais et al., 2015). This indicates that sociodemographic differences affect the utilization of pharmacotherapy and the provision of some harm reduction services. The extent to which prejudicial attitudes and discriminatory actions related to harm reduction and pharmacotherapy may also vary by these factors, and thus lead to differential outcomes for educational approaches, such as the training tested in this study, must still be investigated.
Future research should replicate this novel curriculum delivery across larger and more diverse groups of providers and evaluate the effects of the training with a waitlist control arm done simultaneously with the course to further validate the quality of this training. This study provides sufficient evidence to merit ongoing investigation of its benefits at reducing stigma toward interventions within the spectrum of harm reduction and treatment for SUDs.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Allen, B., & Harocopos, A. (2016). Non-prescribed buprenorphine in New York City: Motivations for use, practices of diversion, and experiences of stigma. Journal of Substance Abuse Treatment, 70, 81–86. https://doi.org/10.1016/j.jsat.2016.08.002
- Aspinall, E. J., Nambiar, D., Goldberg, D. J., Hickman, M., Weir, A., Velzen, E. V., Palmateer, N., Doyle, J., Hellard, M., & Hutchinson, S. J. (2014). Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol, 43(1), 235–248. https://doi.org/10.1093/ije/dyt243
- Bao, Y.-P., Liu, Z.-M., Epstein, D. H., Du, C., Shi, J., & Lu, L. (2009). A meta-analysis of retention in methadone maintenance by dose and dosing strategy. The American Journal of Drug and Alcohol Abuse, 35(1), 28–33. https://doi.org/10.1080/00952990802342899
- Bland, E., Oppenheimer, L. W., Oppenheimer, L., Brisson-Carroll, G., Morel, C., Holmes, P., & Gruslin, A. (2001). Influence of an educational program on medical students' attitudes to substance use disorders in pregnancy. The American Journal of Drug and Alcohol Abuse, 27(3), 483–490. https://doi.org/10.1081/ADA-100104513
- Brunson, J. C. (2020). ggalluvial: layered grammar for alluvial plots. Journal of Open Source Software, 5(49), 2017. https://doi.org/10.21105/joss.02017
- Chaar, B. B., Wang, H., Day, C. A., Hanrahan, J. R., Winstock, A. R., & Fois, R. (2013). Factors influencing pharmacy services in opioid substitution treatment. Drug and Alcohol Review, 32(4), 426–434. https://doi.org/10.1111/dar.12032
- Couto e Cruz, C., Salom, C. L., Dietze, P., Lenton, S., Burns, L., & Alati, R. (2018). Frequent experience of discrimination among people who inject drugs: Links with health and wellbeing. Drug Alcohol Depend, 190, 188–194. https://doi.org/10.1016/j.drugalcdep.2018.06.009
- Crapanzano, K., Vath, R. J., & Fisher, D. (2014). Reducing stigma towards substance users through an educational intervention: Harder than it looks. Academic Psychiatry, 38(4), 420–425. https://doi.org/10.1007/s40596-014-0067-1
- Crawford, N. D., Amesty, S., Rivera, A. V., Harripersaud, K., Turner, A., & Fuller, C. M. (2014). Community impact of pharmacy-randomized intervention to improve access to syringes and services for injection drug users. Health Education & Behavior, 41(4), 397–405. https://doi.org/10.1177/1090198114529131
- Davidson, P. J., Lozada, R., Rosen, P. C., Macias, A., Gallardo, M., & Pollini, R. A. (2012). Negotiating access: Social barriers to purchasing syringes at pharmacies in Tijuana, Mexico. International Journal of Drug Policy, 23(4), 286–294. https://doi.org/10.1016/j.drugpo.2012.05.001
- Doe-Simkins, M., Quinn, E., Xuan, Z., Sorensen-Alawad, A., Hackman, H., Ozonoff, A., & Walley, A. Y. (2014). Overdose rescues by trained and untrained participants an change in opioid use among substance-using participants in overdose education and naloxone distribution programs: a retrospective cohort study. BMC Public Health, 14(1), 297. https://doi.org/10.1186/1471-2458-14-297
- Friedmann, P. D., Wilson, D., Knudsen, H. K., Ducharme, L. J., Welsh, W. N., Frisman, L., Knight, K., Lin, H.-J., James, A., Albizu-Garcia, C. E., Pankow, J., Hall, E. A., Urbine, T. F., Abdel-Salam, S., Duvall, J. L., & Vocci, F. J. (2015). Effect of an organizational linkage intervention on staff perceptions of medication-assisted treatment and referral intentions in community corrections. Journal of Substance Abuse Treatment, 50, 50–58. https://doi.org/10.1016/j.jsat.2014.10.001
- Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. Simon & Schuster.
- Harris, J., & McElrath, K. (2012). Methadone as social control: Institutionalized stigma and the prospect of recovery. Qualitative Health Research, 22(6), 810–824. https://doi.org/10.1177/1049732311432718
- Hatcher, A. E., Mendoza, S., & Hansen, H. (2018). At the expense of a life: Race, class, and the meaning of buprenorphine in pharmaceuticalized "care." Substance Use & Misuse, 53(2), 301–310. https://doi.org/10.1080/10826084.2017.1385633
- Hatzenbuehler, M. L., Phelan, J. C., & Link, B. G. (2013). Stigma as a Fundamental Cause of Population Health Inequalities. Am J Public Health, 103(5), 813–821. https://doi.org/10.2105/AJPH.2012.301069
- Kakko, J., Svanborg, K. D., Kreek, M. J., & Heilig, M. (2003). 1-year retention and social function after buprenorphine-assisted relapse prevention treatment for heroin dependence in Sweden: A randomised, placebo-controlled trial. The Lancet, 361(9358), 662–668. https://doi.org/10.1016/S0140-6736(03)12600-1
- Knudsen, H. K., Ducharme, L. J., Roman, P. M., & Link, T. (2005). Buprenorphine diffusion: The attitudes of substance abuse treatment counselors. Journal of Substance Abuse Treatment, 29(2), 95–106. https://doi.org/10.1016/j.jsat.2005.05.002
- Livingston, J. D., Adams, E., Jordan, M., MacMillan, Z., & Hering, R. (2018). Primary care physicians' views about prescribing methadone to treat opioid use disorder. Substance Use & Misuse, 53(2), 344–353. https://doi.org/10.1080/10826084.2017.1325376
- Lloyd, C. (2013). The stigmatization of problem drug users: A narrative literature review. Drugs Education Prevention Policy, 20(2), 85–95. https://doi.org/10.3109/09687637.2012.743506
- MacArthur, G. J., Minozzi, S., Martin, N., Vickerman, P., Deren, S., Bruneau, J., Degenhardt, L., & Hickman, M. (2012). Opiate substitution treatmentand HIV transmission in people who inject drugs: a systematic review and meta-analysis. BMJ, 345, e5945. https://doi.org/10.1136/bmj.e5945
- Madden, E. F. (2019). Intervention stigma: How medication-assisted treatment marginalizes patients and providers. Social Science & Medicine, 232, 324–331. https://doi.org/10.1016/j.socscimed.2019.05.027
- Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database of Systematic Reviews, 2, Art. No.: CD002207. https://doi.org/10.1002/14651858.CD002207.pub4
- Paquette, C. E., Syvertsen, J. L., & Pollini, R. A. (2018). Stigma at every turn: Health services experiences among people who inject drugs. International Journal of Drug Policy, 57, 104–110. https://doi.org/10.1016/j.drugpo.2018.04.004
- Peterson, J. A., Schwartz, R. P., & Mitchell, S. G. (2010). Why don't out-of-treatment individuals enter methadone treatment programs? International Journal on Drug Policy, 21(1), 36–42. https://doi.org/10.1016/j.drugpo.2008.07.004
- R Core Team. (2020). R: A language and environment for statistical computing. https://www.R-project.org/
- Ramirez-Cacho, W. A., Strickland, L., Beraun, C., Meng, C., & Rayburn, W. F. (2007). Medical students' attitudes toward pregnant women with substance use disorders. American Journal of Obstetrics and Gynecology, 196(1), 86.e1–86.e5. https://doi.org/10.1016/j.ajog.2006.06.092
- Rieckmann, T. R., Abraham, A. J., Kovas, A. E., McFarland, B. H., & Roman, P. M. (2014). Impact of research network participation on the adoption of buprenorphine for substance abuse treatment. Addictive Behaviors, 39(5), 889–896. https://doi.org/10.1016/j.addbeh.2014.01.016
- Rieckmann, T., Daley, M., Fuller, B. E., Thomas, C. P., & McCarty, D. (2007). Client and counselor attitudes toward the use of medications for treatment of opioid dependence. Journal of Substance Abuse Treatment, 32(2), 207–215. https://doi.org/10.1016/j.jsat.2006.09.002
- Rosenblatt, R. A., Andrilla, C. H. A., Catlin, M., & Larson, E. H. (2015). Geographic and specialty distribution of U.S. physicians trained to treat opioid use disorder. Annals of Family Medicine, 13(1), 23–26. https://doi.org/10.1370/afm.1735
- RStudio Team. (2019). RStudio: Integrated development for R. RStudio, Inc. http://www.rstudio.com/
- Sjoberg, D. D., Hannum, M., Whiting, K., Zabor, E. C. (2020). Gtsummary: Presentation-ready data summary and analytic result tables. https://CRAN.R-project.org/package=gtsummary
- Smye, V., Browne, A. J., Varcoe, C., & Josewski, V. (2011). Harm reduction, methadone maintenance treatment and the root causes of health and social inequities: An intersectional lens in the Canadian context. Harm Reduction Journal, 8(1), 17. https://doi.org/10.1186/1477-7517-8-17
- Soyka, M., Träder, A., Klotsche, J., et al. (2011). Six-year mortality rates of patients in methadone and buprenorphine maintenance therapy: Results from a nationally representative cohort study. Journal of Clinical Psychopharmacology, 31(5), 678–680. https://doi.org/10.1097/JCP.0b013e31822cd446
- Sulzer, S. H., Feinstein, N. W., & Wendland, C. L. (2015). Assessing empathy development in medical education: A systematic review. Medical Education, 50(3), 300–210. https://doi.org/10.1111/medu.12806
- Sulzer, S. H., Jackson, G., & Yang, A. (2016). Borderline personality disorder and the biomedical mismatch. In 50 years after deinstitutionalization: Mental illness in contemporary communities (Advances in Medical Sociology, Vol. 17) (pp. 263–290). Emerald Group Publishing Limited. https://doi.org/10.1108/S1057-629020160000017011
- von Hippel, C., Brener, L., & Horwitz, R. (2018). Implicit and explicit internalized stigma: Relationship with risky behaviors, psychosocial functioning and healthcare access among people who inject drugs. Addictive Behaviors, 76, 305–311. https://doi.org/10.1016/j.addbeh.2017.08.036
- Wakeman, S. E., & Rich, J. D. (2018). Barriers to medications for addiction treatment: How stigma kills. Substance Use & Misuse, 53(2), 330–333. https://doi.org/10.1080/10826084.2017.1363238
- Walley, A. Y., Xuan, Z., Hackman, H. H., et al. (2013). Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. BMJ, 346, f174. https://doi.org/10.1136/bmj.f174
- Wickham, H., Averick, M., Bryan, J., Chang, W., McGowan, L., François, R., Grolemund, G., Hayes, A., Henry, L., Hester, J., Kuhn, M., Pedersen, T., Miller, E., Bache, S., Müller, K., Ooms, J., Robinson, D., Seidel, D., Spinu, V., … Yutani, H., et al. (2019). Welcome to the tidyverse. Journal of Open Source Software, 4(43), 1686. https://doi.org/10.21105/joss.01686
- Winograd, R. P., Davis, C. S., Niculete, M., Oliva, E., & Martielli, R. P. (2017). Medical providers' knowledge and concerns about opioid overdose education and take-home naloxone rescue kits within Veterans Affairs health care medical treatment settings. Substance Abuse, 38(2), 135–140. https://doi.org/10.1080/08897077.2017.1303424
- Yang, L. H., Wong, L. Y., Grivel, M. M., & Hasin, D. S. (2017). Stigma and substance use disorders: An international phenomenon. Curr Opin Psychiatry, 30(5), 378–388. https://doi.org/10.1097/YCO.0000000000000351
- Zeileis, A. (2004). Econometric computing with H.C. and HAC covariance matrix estimators. Journal of Statistical Software, 11(1), 1–17. https://doi.org/10.18637/jss.v011.i10
- Zeileis, A., & Hothorn, T. (2002). Diagnostic checking in regression relationships. R News, 2(3), 7–10.
Appendix 1: Harm reduction training pre-survey
SUD-C Harm Reduction Training Pre-Training Survey
Start of block: Default question block
Q2 You are being asked to participate in a research project conducted by Utah State University Extension. The purpose of this project is to explore perceptions of interventions targeting opioid use disorders in order to best serve Utahns as we face the Opioid Crisis with the rest of the nation. Participating in this pre-training survey involves completing a survey that will take about 20 min of your time. This survey contains questions about things that may bring up negative emotions and feelings. There will not be any direct benefits to you unless health programs are created for rural communities as a result of this survey. There are no anticipated risks associated with taking part in this survey. COMPLETING THIS SURVEY IS COMPLETELY VOLUNTARY. You may choose to not participate or to not answer any question. You may skip any question you are not comfortable answering. It is very important that you answer all questions truthfully. It is better to skip a question than to answer it untruthfully. The only way for us to learn about how people in Utah feel about addiction interventions is if you answer the questions truthfully. There is no way for us to identify who answered the questions or how they answered them. Please be assured that all answers you provide are confidential and will be kept in the strictest confidentiality. Should you have questions about the study, please contact Sandra Sulzer, Health and Wellness Extension Specialist, or the Chair of the Institutional Review Board at Utah State University.
Q42 Please record your email address. This email address will be used to help us link the pre- and post-training survey responses for evaluation of the training. It will also be used to send you the 3–6 month post-training survey.
______________________________________________________________
Q1 Please provide information about your professional background.
Q3 Are you a substance use disorder counselor or some other kind of addiction treatment professional?
^ Yes (1)
^ No (2)
Skip To: Q4 If Are you a substance use disorder counselor or some other kind of addiction treatment professional? = Yes
Skip To: Q6 If Are you a substance use disorder counselor or some other kind of addiction treatment professional? = No
Q4 What is your professional title?
______________________________________________________________
Q5 How many years have you been working in the addiction treatment field?
______________________________________________________________
Q6 Do you currently, or have you ever worked or volunteered in a harm reduction program, such as a methadone clinic or a needle and syringe distribution program?
^ Yes (1)
^ No (2)
Q7 Please provide demographic information.
Q8 What is your gender?
^ Woman (1)
^ Man (2)
^ Other (3)
Q9 What is your age?
______________________________________________________________
Q10 What is your race/ethnicity? Select all that apply.
⃞ Native American (1)
⃞ Non-Hispanic White (2)
⃞ Hispanic (3)
⃞ Asian American (4)
⃞ Pacific Islander (5)
⃞ Black/African American (6)
⃞ Middle Eastern or North African (7)
⃞ Other (8)
Q11 What is your highest level of education?
^ Did not finish high school (1)
^ High school diploma (2)
^ Some college (3)
^ Associate's degree (4)
^ Bachelor's degree (B.A., BS, BSN, etc.) (5)
^ Master's degree (MSN, MPH, MBA, MPA, MS, etc.) (6)
^ Advanced medical degree (M.D., PsyD, D.O., PA, DNP, PharmD) (7)
^ Other advanced degree (PhD, J.D., etc.) (8)
Q12 Indicate your level of agreement with the following statements:
Q13 Methadone is a legitimate and effective medicine for treating opioid addiction in terms of reducing illicit drug use and drug overdose, and in terms of retaining patients in treatment.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q14 Buprenorphine (often known by its brand names, 'Suboxone' or 'Subutex') is a legitimate and effective medicine for treating opioid addiction in terms of reducing illicit drug use and drug overdose, and in terms of retaining patients in treatment.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q15 Naltrexone (often known by its brand name, 'Vivitrol' or 'ReVia') is a legitimate and effective medicine for treating opioid addiction in terms of reducing illicit drug use and drug overdose, and in terms of retaining patients in treatment.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q16 Patients who take methadone or buprenorphine are no different than people who still use illicit opioids like heroin.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q17 I think patients using medications like methadone and buprenorphine for their opioid addiction should be allowed to access counseling, therapy, and residential treatment programs along with patients who are pursuing an abstinent (medication-free) treatment path.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q18 I would work at a clinic offering methadone, buprenorphine, and naltrexone to people with opioid addiction.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q19 Addiction treatment counselors should encourage patients with moderate or severe opioid addictions to get off medications for opioid use disorders like methadone and buprenorphine and instead only use behavioral therapy in their treatment.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q20 Creating "drug consumption facilities" where people can inject, inhale, or smoke illicit drugs under the supervision of staff trained in emergency medical care can reduce the number of people who die from fatal drug overdoses.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q21 Creating drug consumption facilities where people can use illicit drugs under the supervision of trained staff will increase addiction rates.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q22 I would work in a facility where people can use illicit drugs under supervision of trained staff.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q23 Naloxone (often known by its brand names, "Narcan" or "Evzio"), which is an opioid overdose reversal drug, is an effective medicine for preventing deaths due to opioid overdose.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q24 Distributing naloxone increases drug use rates because people feel like they can use as much opioids as they want without dying.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q25 I would be ok if naloxone was distributed by my place of work.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q26 "Good Samaritan Laws," which offer protection from criminal drugs charges to people who report an overdose, help reduce deaths due to opioid overdose because it encourages people to call 911.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q27 I support Good Samaritan Laws for my community.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q28 Syringe distribution programs, which provide clean syringes and needles to people who inject drugs, are effective programs for preventing infectious bloodborne disease like HIV/AIDS and Hepatitis C.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q29 Syringe distribution programs increase addiction rates in communities because they encourage injection drug use.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q30 I would work in a syringe distribution program.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q31 Harm reduction programs, such as syringe distribution programs and safe drug consumption facilities, help people who use drugs to begin to improve their health and can encourage such individuals to eventually engage in treatments like methadone and counseling.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q32 Counseling and therapy offered by trained behavioral health professionals is an effective treatment for opioid addiction.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q33 I would work at a counseling and therapy program for people with opioid addiction.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q34 I intend to promote harm reduction or correct myths in conversations with my colleagues at my work site in the next 6 months.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q35 I intend to inform clients/patients/community members who use drugs of the available harm reduction resources in our community during the next 6 months (such as where to get naloxone or unused needles).
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
Q36 I intend to primarily promote abstinence in my work with patients in the next 6 months.
^ Agree (1)
^ Neutral (2)
^ Disagree (3)
^ I don't know (4)
End of Block: Default Question Block
**Note, the post-training survey was identical except for eliminating demographic questions. Items 12–36 were replicated.