Abstract
This paper describes the history of the development of taxonomies of psychoactive drug use, and discusses the conceptualization of three recent taxonomies: comparing their features, and considering their application in education, treatment, and harm reduction settings. Firstly, the Drugs Wheel was created in 2012, prompted by the emergence of New Psychoactive Substances and rapid developments in their legislative control. It was created in collaboration with health professionals and trainers in the drugs field, people who use drugs, and harm reduction non-government organizations, as a learning tool for NPS. Secondly, by contrast, the Drug Pyramid was an academic creation published in 2016 that aimed to conceptualize the multitude of NPS then being developed at a rate of two per week, as primarily an educational project. Finally, building from limitations identified in the previous two models, the Drugs Venn was created by the authors for the purpose of this paper and in consultation with staff at a drug checking service provider, with the intention of future application in delivery of drug checking consultations. Viewed together, each model addresses objections raised to its predecessor, and in doing so highlights the multi-dimensional nature of taxonomies, and their potential for generation of further hypotheses.
Introduction
Classification, in its simplest form, is concerned with the grouping together of items based on their similarities or differences. It has been described as a way of dealing with the complexities of the world around us, with Mercier (Citation1912, pp. 149-150) finding it ‘implied and involved in all thought… without classification, the Universe is chaos’. Classification is in some ways an arbitrary process, defined by the requirements of the environment in question, with its relevance mostly dependent on its setting (Gilmour & Walters, Citation1964). Where classification is the construction of classes, taxonomy can be viewed as the development of theories for separating items into different kinds, or the theory of classification. Taxonomy attempts to arrange items into a systematic framework, or conceptual organization, based on the relationships between items (McKelvey, Citation1978) and implies greater sophistication or detail than the one-dimensional approach of classification. Taxonomy is therefore both subjective and complex: a multi-dimensional scheme of classification influenced by many factors.
One of the earliest taxonomies of drugs was created by Lewin (Citation1924) who named his groups Euphorica (sedatives of mental activity, including opium and cocaine); Phantastica (drugs of illusion, including mescal buttons and cannabis); Inebriantia (created by chemical synthesis, such as alcohol or chloroform); Hypnotica (sleep-producing agents, such as chloral); and Excitantia (mental stimulants, of vegetable origin, such as caffeine or tobacco). By contrast, other categorizations have been proposed that are not taxonomies, for example Lingford-Hughes (Citation2004) and Leonard (Citation2010), whose approaches combined classes such as sedatives with individual substances such as cannabis, and drug groups such as opioids.
Constance (Citation1957, p. 88) suggested a fluid approach to taxonomy which could be visualized as a system of three-dimensional library shelves in which boxes containing information could be moved around, creating an ‘open, growing, vital taxonomic system’. As can be seen in the example of cocaine in Lewin’s model above, in which it was categorized as a sedative (and more recently would be classified as a stimulant), there is value to drug taxonomies being flexible, in order to respond to new scientific data, new political perspectives, or to the development of new compounds. In 1980, more than two decades before the emergence and explosion onto the illicit drug market of multiple new compounds, Fink predicted that ‘new psychoactive drug classes may yet be formed from the ongoing studies of the derivatives of tetrahydrocannabinol, [and] of stimulants which differ from the amphetamines’ (Fink, Citation1980, p. 499). His predictions turned out to be prescient: synthetic cannabinoid receptor agonists (SCRAs) and cathinones were seen more widely on the drug market from the late 2000s (EMCDDA, Citation2020), since when there has been a proliferation in the number and chemical makeup of new psychoactive compounds. Alongside terms such as ‘internet drugs’, ‘research chemicals’, and ‘legal highs’, the term novel, then New Psychoactive Substances (NPS) entered the popular vernacular (Liechti, Citation2015). Within the legal framework, the United Nations Office on Drugs and Crime defined NPS as 'substances of abuse, either in a pure form or a preparation, that are not controlled by the 1961 Single Convention on Narcotic Drugs or the 1971 Convention on Psychotropic Substances, but which may pose a public health threat' (UNODC, Citation2013, p. iv). The term came into common use to describe a broad spectrum of synthetic and plant-derived psychoactive substances that emerged from 2008 onwards. Marketed as ‘legal highs’, ‘research chemicals’, ‘plant food’, and ‘bath salts’, these were most usually sold on the internet and in ‘headshops’. NPS is therefore a wide-reaching term that can include newly discovered and manufactured synthetic drugs, pre-existing compounds only recently observed on the drug market, natural plants or their extracted products, and active pharmaceutical ingredients and medicinal products. NPS classifications have tended to focus on either their psychotropic effect (such as stimulants, depressants, or hallucinogens) or according to their chemical families (including phenethylamines, synthetic cathinones, piperazines, aminoindanes, benzofurans, cannabimimetics, and tryptamines) (Liechti, Citation2015; Measham, Citation2021). By 2012, 236 NPS had been identified by the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA, Citation2013), with this number having increased to 830 at the time of writing (EMCDDA, Citation2021). This posed challenges for public health, law enforcement, and also those working in the drugs education, prevention, treatment, and training fields who were attempting to provide accurate and appropriate services for people taking these drugs, whether inadvertently or by choice.
These same challenges were also faced by harm reduction and peer services for people who use drugs (PWUD). Harm reduction: a pragmatic approach to decreasing the negative consequences of drugs to users, communities, and wider society (Newcombe, Citation1987), such as safer consumption rooms, needle exchange, and drug checking, can provide PWUD with resources such as access to prescribing programs, injecting equipment, or drugs information (Pates & Riley, Citation2012). One source of information about NPS came from people who themselves were taking them for psychoactive exploration, or psychonauts, a term attributed to Jünger (Citation1970). Newcombe (Citation1999) described psychonauts who reported their experiences with NPS in trip reports, a self-report monitoring procedure employing observations of effects used by Shulgin and Shulgin (Citation1991) and others. Psychonauts not only provided information in person but also in discussions on global internet forums (Davey et al., Citation2012; Ruane, Citation2018) where information around effects, safety, and ‘an extensive and cumulative amount of knowledge about previously unfamiliar drugs’ was shared (Soussan & Kjellgren, Citation2014, p. 8).
As the number and variety of NPS grew, so did attempts to classify them, or integrate them into existing models. For example, Coulon and Gorji (Citation2016, p. 515) proposed a categorization which featured two ‘hazard groups’, and 13 categories based on neurobiological mechanisms of action, including synthetic cannabinoids. Others, for example those created by the United Nations Office on Drugs and Crime (UNODC, Citation2013) and King (Citation2013, p. 12) included a miscellaneous or other group that was used to contain drugs that did not fit into existing categories.
The Drugs Wheel
The Drugs Wheel was the product of an action research project to create a taxonomy to classify psychoactive drugs that encompassed both NPS and ‘established’ drugs (those not classed as NPS). Its first objective was to simplify the rapidly burgeoning psychoactive drug market; creating a comprehensive model that integrated information about drug effects and risks gathered from the experiences of people using NPS with emerging research about the actions of these drugs. Its second objective was to design a visually appealing and interactive taxonomy to maximize its effectiveness as an educational tool; increasing knowledge and reducing harm for people of all ages who used established drugs and/or NPS, wider communities, and support services.
Data to inform the creation of the model were drawn from multiple sources, and in consultation with DrugWatchUK (2021), an informal association of charities, organizations, and individuals who share an interest in establishing a robust early warning system in the UK for all types of drugs. Members of DrugWatchUK included a number of leading professionals within the drugs education, prevention, and training fields, who, having previously set up an informal network of professionals who were working with PWUD, added their expertise during the design of the model. This led to a dialectical interaction, in which professionals shared information on risks and effects of NPS being observed in practice.
In addition to these collaborations and exchanges, data were also collected from informal, unstructured discussions with users of forums including Bluelight (Citation2020), along with information garnered from users’ first-hand experiences with NPS collated in trip reports (e.g. Dondante, Citation2011; McHound, Citation2009; Mindspelunker, Citation2011). Additional data were collected from the emerging body of research on NPS (e.g. Deluca et al., Citation2012; Van Hout & Brennan, Citation2011), and their effects on neurotransmitter pathways (e.g. Möller et al., Citation2011; Schifano et al., Citation2011).
Conceptualization
In his Classification of Psychoactive Drugs, Leonard (Citation2010, p. 294) proposed a five-class system of sedatives, opiates, psychostimulants, cannabinoids, and hallucinogens, additionally suggesting that:
Psychotropic drugs may be classified (1) according to their chemical structure, (2) by their pharmacological actions on specific biological processes such as receptors, transporter, or ion channels, or (3) by their therapeutic actions.
The Drugs Wheel model built upon this system by adding two additional categories, empathogens and dissociatives, taking into account reported effects, emerging harm reduction information, and research on the effects of NPS on neurotransmitter pathways. The seven categories: stimulant, empathogen, psychedelic, dissociative, depressant, opioid, and cannabinoid, allowed for all psychoactive substances, both established and NPS, to fit within a category without the need for a miscellaneous or other group as found in many previous taxonomies and classifications (see for Drugs Wheel categories).
Table 1. The seven categories of the Drugs Wheel model, with a summary overview of reported effects, harms, and receptor activity (Abdulrahim & Bowden-Jones, 2015; Basavarajappa & Subbanna, Citation2019; Coulon & Gorji, Citation2016; Stolerman, Citation2010; Julien et al., Citation2011).
The empathogen category identified NPS that could be seen to ‘bridge the gap’ between stimulants and psychedelics, in some cases containing elements of both. While many empathogenic drugs such as MDMA have stimulant qualities, with activity on dopamine and noradrenaline pathways, they add additional effects such as being mildly hallucinogenic at certain doses and an ‘open mind state’ (Sáez-Briones & Hernández, Citation2013). Because of their additional serotonergic activity, empathogens may also carry a risk of harm from serotonin syndrome (Maier et al., Citation2018; Scotton et al., Citation2019), notably observed in compounds such as MDAI, MDMA, and 5-API (Páleníček et al., Citation2016; Parrott, Citation2002; Simmler & Liechti, Citation2018).
The dissociative category was, in a similar manner, included to identify specific receptor activity and reported risks of harm. While dissociative drugs such as ketamine, phencyclidine (PCP), methoxetamine (MXE), or diphenidine (DPH) also affect numerous other receptors (Morgan et al., Citation2010; Sahai et al., Citation2018), they act mainly as antagonists of the NMDA receptor (Baumeister et al., Citation2015; Herrling et al., Citation1997). This NMDA receptor activity can result in a ‘peculiar’ state of consciousness with altered perceptions of sound and reality, and feelings of detachment that differ from serotonergic psychedelic hallucinations experienced in drug groups such as tryptamines, lysergamides, and phenethylamines (Abdulrahim & Bowden-Jones, 2015; Corazza et al., Citation2012; Schifano et al., Citation2019). Harms specific to dissociatives include the risk of entering an anaesthetized state in higher doses, known colloquially as a ‘hole’, in which users find themselves experiencing an ‘out of body’ or ‘near death’ experience (Hearne & Van Hout, Citation2016): accidentally for many, deliberately sought after by some.
Adaptation
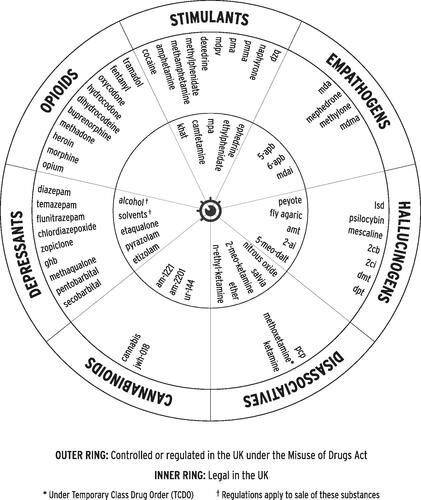
Inner and outer rings were added to the model (see , an early version of the Drugs Wheel from 2012) to allow for additional subdivision of the seven categories, and to facilitate adaptation to different settings. For example, subdividing the medicines categories into licensed and non-licensed medicines facilitated discussion around UK legislation, policy, and practice, while training sessions in which the Drugs Wheel’s categories were subdivided into higher and lower risk facilitated discussions about perceived risks, drug effects, facts, and myths. The inner and outer rings have also been used to separate the categories by legal status, as seen in the 2012 incarnation in , which included the legislative situation in the UK at that time, or separated by NPS and established drugs (see for the most recent adaptation, with established drugs in the outer ring, and NPS in the inner ring).
Figure 2. A more recent version of the Drugs Wheel (12 October 2021) with established drugs in the outer ring, and NPS in the inner ring.
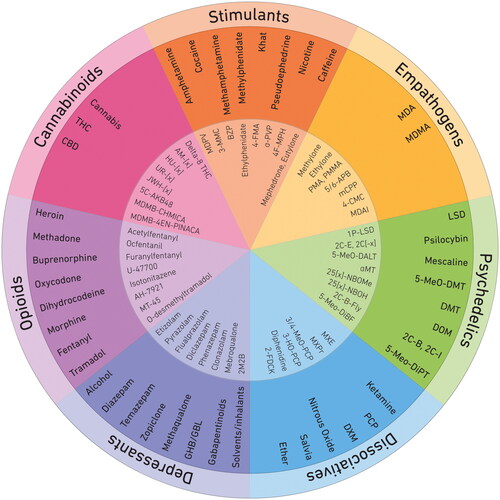
The positioning of categories was intentionally chosen, so that adjacent categories were linked: for example, many of the psychedelics share some neurotransmitter and/or subjective drug effects with both the empathogenic and dissociative groups. With the emergence of research highlighting both the direct and ‘downstream’ dopaminergic activity of some of the SCRAs (Basavarajappa & Subbanna, Citation2019; Fantegrossi et al., Citation2018), and the efficacy of cannabinoids as a treatment for pain relief (Johnson et al., Citation2010), the cannabinoid group was later repositioned between the opioid and stimulant groups (see ).
Adjusting the inner and outer rings of the Drugs Wheel in response to legislative change allowed the model to be rapidly updated during a period of particularly frenetic activity in the UK in relation to drug control, which has been characterized as a series of ‘cat-and-mouse’ responses between legislators and NPS manufacturers, or a tightening of the drug policy ratchet (Stevens & Measham, Citation2014). As each new NPS appeared in the UK that was not yet covered by legislation, from 2011 its importation, production, and supply could be temporarily banned using a Temporary Class Drug Order, and from 2016 the production, sale, and supply of all but a handful of exempted psychoactive substances were permanently banned by the Psychoactive Substances Act (Home Office, Citation2018), in addition to the established process of review and legislative control under the Misuse of Drugs Act 1971. Between its creation in 2012 and the passing of the Psychoactive Substances Act four years later, a total of 27 revisions were made to the Drugs Wheel to reflect legislative changes.
Utility
It is beginning to emerge that, in many fields of medicine, a system- and mechanism-based approach is much more useful than the traditional organ- and disease-specific approach… This strategy can and should be readily expanded to pharmacology as a whole and psychopharmacology in particular.
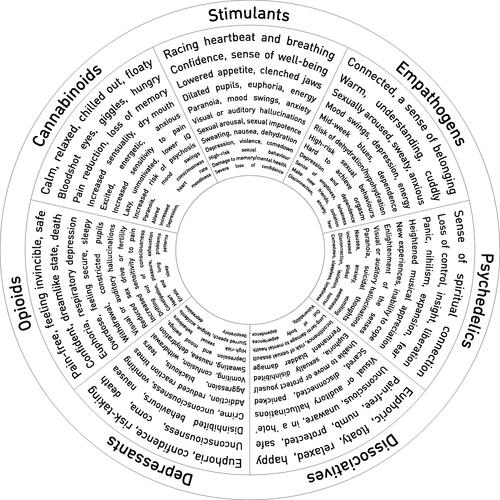
This quote from Seifert and Schirmer (Citation2020, p. 1337) encapsulates the rationale behind the categories used in the Drugs Wheel. Rather than adopting a single method of classification it took a ‘whole systems’ approach: integrating drug effects and action on receptor pathways with harm reduction information specific to each group (see : The Effects Wheel).
Figure 3. The Effects Wheel: drug effects and risks, allowing for harm reduction information to be given by category.
The model was implemented as a harm reduction tool in the form of the Drugs Wheel game. Piloted with young people in school and community youth offending settings, the game was designed to simplify the number and range of psychoactive drugs, allowing for harm reduction information to be given by category, rather than by individual substance, thereby helping both PWUD and support services to make sense of the hundreds of emergent NPS. To play the game, a group was divided into teams, and points were allocated to correct responses to create an element of competition. Teams were initially asked to match key words (e.g. + pain-free, relaxed, - dependent, overdose) with categories on the Wheel (e.g. opioids). While many of the terms, such as relaxed, could be applied to multiple categories, there were nuances in the combinations of the terms that led to discussion about the different categories. Teams were then assigned printed cards with images of NPS and established drugs that they were asked to place in their correct category, with inner and outer rings of the Wheel used to add additional categorization, initially of legal status. The game contained a printed board, instructions, drug descriptions, and labels, and was available in both commercial and free-to-download versions, along with instructional videos (Adley, 2012).
In 2018 and in partnership with Adley, The Loop (a harm reduction non-government organization) adapted the Drugs Wheel into the Club Drugs Wheel (Adley & The Loop, Citation2018), specifically for use by the Loop and the Loop Australia, making use of the model’s inner and outer rings to allow for the categories to be split into further sections according to UK and Australian national laws. The Loop’s Club Drugs Wheel was then used for a variety of educational and harm reduction activities including training of Loop volunteers, students, university staff, and staff in nightlife, events, hospitality and local authority sectors, as well as being printed and displayed in large format at festivals and nightclubs (see ). It was also printed in small format as materials for harm reduction information sessions during the healthcare interventions delivered by health staff to Loop drug checking service users in festivals (Measham, Citation2019; Measham & Turnbull, Citation2021) and city centers (Measham, Citation2020a). The Drugs Wheel’s Creative Commons licensing terms has led to its adaptation for use in different countries and languages, at time of print: Arabic, Australian, Bulgarian, Dutch, French, Italian, Latvian, Polish, Portuguese, Russian, and Spanish versions. Additionally, the Australian Alcohol and Drug Foundation (Citation2019) created an interactive digital version for the Drug Facts section of their website, with a tutorial video by the Drug Education Network (Citation2020).
Figure 4. The Drugs Wheel on display outside The Loop's drug checking service at Boomtown Fair festival, UK, 2017.

Potter and Chatwin (Citation2018, p. 331) questioned the rationale behind complex systems that sub-categorized NPS, such as that proposed by the UNODC (Citation2013), suggesting that ‘the vast majority of NPS could be incorporated into an existing system such as [the Drugs Wheel]’. Fletcher et al. (Citation2016) and Bennett et al. (Citation2017) used the Drugs Wheel’s classifications to categorize the NPS identified in their studies, while Gilani (Citation2015) found it a useful method of classification. Its application as a harm reduction and educational tool is further demonstrated by its inclusion in materials produced by the EMCDDA (Citation2019b), and the English and Scottish Governments (Home Office, Citation2015; MacLeod et al., Citation2016); it has also been used to illustrate journal articles on ‘party drugs’ (Sammut & Craig, Citation2019), and is included in a textbook on psychiatry (Marwick, Citation2019, p. 82).
Limitations
In his book on teenage substance use, aimed primarily at those working with young people, Macdonald (Citation2019, p. 95) described the Drugs Wheel as a ‘comprehensive depiction of a wide range of drugs according to their specific effects, legal status and risks’. However, he found it to be ‘far too detailed and unworkable at a universal level’, and suggested instead using the three main psychopharmacological categories of stimulant, depressant, and hallucinogen, an approach also supported by Measham and Newcombe (Citation2016), discussed further below.
The classification of empathogens, as with many of the drugs in the Drugs Wheel, is a matter of debate, and the rationale for their categorization in the Drugs Wheel has been criticized. One such query was raised by Bowden-Jones, a consultant psychiatrist and Lead Clinician for the Club Drug Clinic (personal communication, 15/03/2016), who commented that the drugs contained in this category were better included within the stimulant group. While many empathogens can indeed induce traditionally stimulant effects (Sainsbury et al., Citation2011), there are exceptions. Drugs such as mCPP (Bossong et al., Citation2005) and the aminoindane MDAI have serotonergic action with minimal activity on the dopamine system and without notable stimulant effect found in humans, with MDAI described as being ‘inactive in terms of locomotor activity’ (Brandt et al., Citation2013, p. 11). Sainsbury et al. (Citation2011, p. 80) noted the predominantly serotonergic action of the aminoindanes, finding that MMAI, MDAI, and 5-IAI ‘appear to affect the 5-HT system, but have an absence of action on dopamine and noradrenaline receptors’. Additional support for the creation of the empathogenic category came from Bedi et al. (Citation2010, p. 521) who argued that the unique pharmacological properties of MDMA were ‘different from those of structurally related stimulants and hallucinogens'. In this way, the empathogen category not only provided a bridge between the stimulant and psychedelic categories in the Drugs Wheel, but its inclusion in the model allowed for a wider discussion about the potential risks of serotonin syndrome.
Grouping psychoactive drugs by neurotransmitter activity is also open to criticism due to the complexity of these actions and interactions. Receptor systems can exert influence over one another (Di Matteo et al., Citation2008), with Julien et al. (Citation2011, p. 70) summarizing that:
It would be nice if there were a single receptor type for each specific neurotransmitter. In actuality, virtually every transmitter binds to several distinct receptor subtypes. For example, norepinephrine, serotonin, and dopamine bind to multiple presynaptic and postsynaptic receptors as well as their specific presynaptic transporter.
In addition to these overlaps, and the shared effects of many psychoactive drugs on the brain, there is still considerable individual variability between drug classes, their mechanisms of action, and physical and psychological effects. These effects can be highly subjective, depending on a wide range of factors, summarized by the ‘drug, set and setting’ model proposed by Zinberg (Citation1984); integrating these subjective experiences into the design of a taxonomy of psychoactive drugs is not without criticism. Becker (Citation1967) identified a number of concerns about the inclusion of subjective reports into research, among them: that drugs have multiple effects, and people using them might single out a particular desirable or undesirable effect, or attribute effects to other causes; and the impact of prior knowledge, and expectation. Newcombe (Citation1999) questioned the lack of methodological standardization and terminology for studying subjective drug effects, proposing a standardized approach based around a 10-dimensional model of drug effects exploring factors relating to consumption, intoxication, physical, and psychological effects and experience. By contrast others have noted the essentially subjective and non-verbal nature of the psychoactive experience (Moore & Measham, Citation2011; Sumnall et al., Citation2006) and the futility of attempting to standardize or verbalize such an experience (Díaz, Citation1979, p. 71). More recently however, subjective experiences of use of psychoactive drugs have been included in guidance such as the NEPTUNE Expert Group (Abdulrahim & Bowden-Jones, 2015) and research tools such as the Drug Effects Questionnaire (Morean et al., Citation2013), aligned with Becker who in 1967 (p. 164) opined that ‘the subjective changes produced by a drug can be ascertained only by asking the subject, in one way or another, how he [sic] feels’.
The Drugs Pyramid
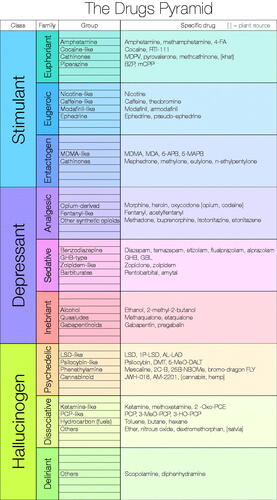
In parallel with the Drugs Wheel, the Drugs Pyramid (Measham & Newcombe, Citation2016) was created in response to the emergence of NPS and the perceived need to order and classify the multitude of diverse substances that appeared from 2008 onwards. While the number of NPS identifications peaked in 2014 at approximately two per week, there was still an average of one new NPS per week identified by the EMCDDA in 2018 (EMCDDA, Citation2019a; Measham, Citation2020b), with around 400 previously unreported NPS detected in Europe every year since 2005 (EMCDDA, Citation2021). Unlike the Drugs Wheel, however, the aim of the Drugs Pyramid was primarily an intellectual exercise rather than an education, prevention, or treatment-oriented tool. The Drugs Pyramid used a four-tiered model taking the three categories of stimulant, depressant, or hallucinogen as the initial classification, then sorting these three categories of NPS into nine families of psychoactive effect, a further 37 chemical groups, and finally itemizing examples of the hundreds of NPS into these chemical groups.
The Drugs Pyramid provided an expandable, tiered model. This adaptability meant it could be both succinct and comprehensive, as its number of levels could be adapted for use with specific populations: for example, the model could be limited to one or two tiers when working with those with less interest in, or knowledge of the more detailed classifications. However, while the Drugs Pyramid offered a comprehensive taxonomy, the authors acknowledge an element of subjectivity to the classification, meaning that some drugs could be classified under alternate headings. The entactogen family, for example, could be included within either the hallucinogen or stimulant groups. Also the Drugs Pyramid, in contrast with the Drugs Wheel, does not include legislative status but focuses instead on psychoactive effects. Whilst more limited in scope, therefore, it also requires less regular updating, does not need to be adapted to different legislative contexts and countries, and potentially this simplicity and utility can make it more accessible and appealing to a wider range of lay audiences.
For the purposes of this paper, and future application with The Loop’s drug checking services, the authors began the process of adapting the Drugs Pyramid from its 2016 NPS-focused version to one which included established drugs. This process was not without its challenges however, and resulted in some drug groups being split among different families. For example, some drugs in the phenylethylamine group were contained both in the Stimulant-Entactogen family (e.g. MDMA) and the Hallucinogen-Psychedelic category (e.g. mescaline), while the tropane group spanned both the Stimulant-Euphoriant and Hallucinogen-Psychedelic categories. To navigate around this issue, some of the more technical terms for group names in the original model, such as lysergamides, were replaced with more generic names such as ‘LSD-like’. illustrates the end result: the ‘de-chemicalized’ 2021 version of the Drugs Pyramid.
However, when distributed to colleagues for evaluation, the rigid structure of the Pyramid was called into question. Requests were made for a version which acknowledged the overlapping nature of drug effects, allowing drugs to span more than one category.
Thesis/antithesis/synthesis: the Drugs Venn model
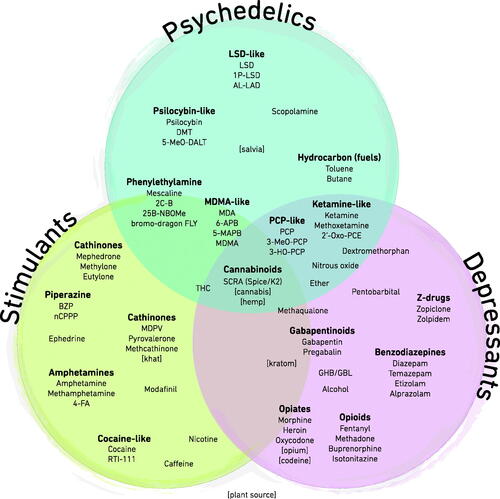
Based on an original idea by Derek Snider, the Drugs World Venn diagram visualization (McCandless, Citation2010) features four overlapping circles containing stimulants, depressants, hallucinogens, and anti-psychotics (see ).
Figure 6. The Drugs World Venn diagram: reprinted from www.InformationIsBeautiful.net with kind permission.
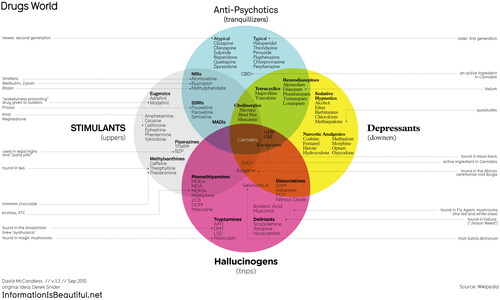
We aimed to simplify this model by integrating the less-technical terms from the revised Drugs Pyramid above, removing the anti-psychotic category, and renaming hallucinogens as psychedelics in response to feedback from academics and practitioners in the field (see ). This version synthesized elements from three previous models: incorporating (i) miniature Drugs Wheels, (ii) the three main categories of the Pyramid model, and (iii) adding a new element, that of the overlapping areas within the Venn diagram that was found in neither of the other two models, but drew on the McCandless Venn diagram discussed above.
Strengths and limitations
Díaz (Citation1979) highlighted the challenges of creating a taxonomy of psychoactive drugs that is generally acceptable, due to the diversity in backgrounds of specialists working with these substances, while in the 1959 bulletin for the World Health Organization, Jacobsen (Citation1959, p. 465) concluded that groups of psychotropic drugs are ‘merely to be considered as general characterizations which make it possible to provide short descriptions of old or newly discovered compounds’. In turn, there are valid criticisms aimed at each of the three models in this paper: the seven categories of the Drugs Wheel can be seen to add unnecessary complexity to drug classification, and its definition between drug categories can be seen to disregard the often-overlapping nature of drug effects. The Drugs Pyramid’s and Drug Venn’s adherence to the stimulant/depressant/hallucinogen (or psychedelic) model can in turn raise questions about the placement of certain drugs such as SCRA, and some dissociative and empathogenic drugs. There are both advantages and disadvantages to the inclusion or exclusion of legislative context in the three models. Taken together and through their dialectical interactions, however, each model addresses the objections raised by its predecessor, and by being both complementary and contradictory illustrate the very nature of taxonomies.
There are challenges in attempting to categorize and simplify a psychoactive experience that is both subjective and non-verbal: taxonomies will never be complete, final, or perfect. Much like a language, in which there will almost invariably be irregular verbs, there will almost invariably be outliers in any model; it is however the comparison of where an object belongs within a taxonomy, and where it does not, that adds value. As Christiansen (Citation1994, p. 4) found, observation of these differences can result in the generation of hypotheses to explain them, and these differences ‘are heuristic, in that they stimulate informed inquiry’. It is hoped that the inclusion of these three models serves a similar purpose, and that rather than each proposing to be the ‘perfect’ drug taxonomy, that discussion over their differences and their utility to education, prevention, and treatment can lead to further debate.
Conclusion
There is no perfect taxonomy, as illustrated by this often-referenced quote by Box et al. (Citation2011, p. 61) which, although related to statistical and engineering processes, may be of relevance across multiple fields of study:
All models are approximations… but some models are useful. So the question you need to ask is not “Is the model true?” (it never is) but “Is the model good enough for this particular application?”
Much like psychoactive drugs, taxonomies are not detached objective conundrums; within the drugs field they reflect and are embedded within the changing landscape of drug use and drug markets, that themselves respond to changes in policy and socio-cultural contexts, manufacturing processes, and psychoactive exploration and exploitation around the world. They are specific to, and relevant to disciplines and practices; one of their purposes is to be of use to their target audiences, for example the pharmacologically-driven nomenclature to aid clinicians in prescribing psychotropic drugs proposed by Zohar et al. (Citation2014). Complex models that classify drugs by group, or action on neurotransmitter sites, may require an understanding of chemistry that is beyond the knowledge base or utility of many lay audiences, while taxonomies which aim to simplify the intricate actions and effects of psychoactive drugs can be criticized for being too naive. The Drugs Wheel is symptomatic of this binary, having been criticized both for being too simple and too complex. Despite its criticisms, however, it provides a popular interactive and educational approach to drug taxonomy that can potentially encompass existing and future psychoactive drugs. As a taxonomy, it has progressed beyond an intellectual exercise to facilitate a wide range of educational, treatment, and training opportunities with a harm reduction ethos in a number of countries and languages. Its design and ongoing adaptation have been notably collaborative: drawn from contributions from PWUD, academics, and professionals working in the health and substance misuse fields, while its Creative Commons license has allowed for its continued development and adaptation around the world (Creative Commons, Citation2021).
Acknowledgements
With thanks to: Russell Newcombe for his contribution to the Drugs Pyramid; members of UK and Ireland DrugWatch for their work on the Drugs Wheel; Michael Linnell for contributing images to the Drugs Wheel game; InformationIsBeautiful.net for permission to use the Drugs World image; and to Newcastle University for providing Open Access publishing. This work includes material that is based (wholly or partially) on data sets obtained from Bluelight.org. Bluelight.org is a non-profit online community dedicated to reducing drug-related harm. This work was conducted with authorization from Bluelight.org. The content is solely the responsibility of the authors and does not necessarily represent the official views of Bluelight.org.
Disclosure statement
Fiona Measham is founding Director, and Guy Jones is senior chemist, with The Loop, a non profit non government organisation providing drug checking and harm reduction services www.wearetheloop.org
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Adley, M. (2012). The Drugs Wheel Game. Retrieved 16 December 2020 from http://www.thedrugswheel.com/?page=game
- Adley, M, & The Loop (2018). The Club Drugs Wheel. Retrieved 12 December 2020 from http://www.thedrugswheel.com/?page=clubdrugswheel
- Alcohol and Drug Foundation (2019). Drug Facts: Drug Wheel. Retrieved 12 December 2020 from https://adf.org.au/drug-facts/#wheel
- Basavarajappa, B. S., & Subbanna, S. (2019). Potential mechanisms underlying the deleterious effects of synthetic cannabinoids found in spice/k2 products. Brain Sciences, 9(1), 14. https://doi.org/10.3390/brainsci9010014
- Baumeister, D., Tojo, L. M., & Tracy, D. K. (2015). Legal highs: staying on top of the flood of novel psychoactive substances. Therapeutic Advances in Psychopharmacology, 5(2), 97–132. https://doi.org/10.1177/2045125314559539
- Becker, H. S. (1967). History, culture and subjective experience: an exploration of the social bases of drug-induced experiences. Journal of Health and Social Behavior, 8(3), 163–176. https://doi.org/10.2307/2948371
- Bedi, G., Hyman, D., & de Wit, H. (2010). Is ecstasy an “empathogen”? Effects of ±3, 4-methylenedioxymethamphetamine on prosocial feelings and identification of emotional states in others. Biological Psychiatry, 68(12), 1134–1140. https://doi.org/10.1016/j.biopsych.2010.08.003
- Bennett, K. H., Hare, H. M., Waller, R. M., Alderson, H. L., & Lawrie, S. (2017). Characteristics of NPS use in patients admitted to acute psychiatric services in Southeast Scotland: a retrospective cross-sectional analysis following public health interventions. BMJ Open, 7(12), e015716. https://doi.org/10.1136/bmjopen-2016-015716
- Bluelight (2020). Retrieved 12 December 2020 from https://www.bluelight.org/xf/
- Bossong, M., Van Dijk, J., & Niesink, R. (2005). Methylone and mCPP, two new drugs of abuse? Addiction Biology, 10(4), 321–323. https://doi.org/10.1080/13556210500350794
- Box, G. E. P., Luceno, A., & del Carmen Paniagua-Quinones, M. (2011). Statistical control by monitoring and adjustment. (2nd ed., Vol. 700). John Wiley & Sons.
- Brandt, S. D., Braithwaite, R. A., Evans-Brown, M., & Kicman, A. T. (2013). Aminoindane Analogues. In P. I. Dargan & D. M. Wood (Eds.), Novel psychoactive substances: classification, pharmacology and toxicology. (pp. 261–283). Academic Press. https://doi.org/10.1016/b978-0-12-415816-0.00011-0
- Christiansen, C. (1994). Classification and study in occupation a review and discussion of taxonomies. Journal of Occupational Science, 1(3), 3–20. https://doi.org/10.1080/14427591.1994.9686382
- Constance, L. (1957). Plant taxonomy in an age of experiment. American Journal of Botany, 44(1), 88–92. https://doi.org/10.2307/2438350
- Corazza, O., Schifano, F., Simonato, P., Fergus, S., Assi, S., Stair, J., Corkery, J., Trincas, G., Deluca, P., Davey, Z., Blaszko, U., Demetrovics, Z., Moskalewicz, J., Enea, A., Melchiorre, G., Mervo, B., Furia, L., Farre, M., Flesland, L., … Scherbaum, N. (2012). Phenomenon of new drugs on the Internet: the case of ketamine derivative methoxetamine. Human psychopharmacology, 27(2), 145–149. https://doi.org/10.1002/hup.1242
- Coulon, P., & Gorji, A. (2016). Tightrope or slackline? The neuroscience of psychoactive substances. Trends in Pharmacological Sciences, 37(7), 511–521. https://doi.org/10.1016/j.tips.2016.04.004
- Creative Commons (2021). Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International. Retrieved 16 December 2020 from https://creativecommons.org/licenses/by-nc-sa/4.0/legalcode
- Davey, Z., Schifano, F., Corazza, O., Deluca, P., & Group, P. W. M, Psychonaut Web Mapping Group (2012). e-Psychonauts: conducting research in online drug forum communities. Journal of Mental Health, 21(4), 386–394. https://doi.org/10.3109/09638237.2012.682265
- Deluca, P., Davey, Z., Corazza, O., Di Furia, L., Farre, M., Flesland, L. H., Mannonen, M., Majava, A., Peltoniemi, T., Pasinetti, M., Pezzolesi, C., Scherbaum, N., Siemann, H., Skutle, A., Torrens, M., van der Kreeft, P., Iversen, E., & Schifano, F. (2012). Identifying emerging trends in recreational drug use; outcomes from the Psychonaut Web Mapping Project. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 39(2), 221–226. https://doi.org/10.1016/j.pnpbp.2012.07.011
- Díaz, J. L. (1979). Ethnopharmacology and Taxonomy of Mexican Psychodysleptic Plants. Journal of Psychedelic Drugs, 11(1-2), 71–101. https://doi.org/10.1080/02791072.1979.10472094
- Di Matteo, V., Di Giovanni, G., Pierucci, M., & Esposito, E. (2008). Serotonin control of central dopaminergic function: focus on in vivo microdialysis studies. Progress in Brain Research, 172, 7–44. https://doi.org/10.1016/s0079-6123(08)00902-3
- Dondante (2011). (25C-NBOMe/500 µg) First time: Van-Goghian masterpiece. https://www.bluelight.org/xf/threads/25c-nbome-500-%C2%B5g-first-time-van-goghian-masterpiece.564781/
- DrugWatchUK (2021). UK and Ireland DrugWatch. Retrieved from December 06, 2021 from https://michaellinnell.org.uk/drugwatch.html
- Drug Education Network (2020). Exploring the Drug Wheel. Retrieved 06 February 2021 from https://www.youtube.com/watch?v=ETDuFgZosWw
- EMCDDA (2013). EU Drug Markets Report: a strategic analysis. European Monitoring Centre for Drugs and Drug Addiction, Publications Office of the European Union. https://www.emcdda.europa.eu/system/files/publications/741/TD3112366ENC_406102.pdf
- EMCDDA (2019a). EU Drug Markets Report 2019. European Monitoring Centre for Drugs and Drug Addiction: Publications Office of the European Union. https://www.emcdda.europa.eu/system/files/publications/12078/20192630_TD0319332ENN_PDF.pdf
- EMCDDA (2019b). European Prevention Curriculum: a handbook for decision-makers, opinion-makers and policy-makers in science-based prevention of substance use. European Monitoring Centre for Drugs and Drug Addiction. https://www.emcdda.europa.eu/publications/manuals/european-prevention-curriculum_en
- EMCDDA (2020). New psychoactive substances: global markets, glocal threats and the COVID-19 pandemic. European Monitoring Centre for Drugs and Drug Addiction: Publications Office of the European Union. https://www.emcdda.europa.eu/system/files/publications/13464/20205648_TD0320796ENN_PDF_rev.pdf
- EMCDDA (2021). European drug report 2021: Trends and developments. European Monitoring Centre for Drugs and Drug Addiction: Publications Office of the European Union. https://www.emcdda.europa.eu/system/files/publications/13838/TDAT21001ENN.pdf
- Fantegrossi, W. E., Wilson, C. D., & Berquist, M. D. (2018). Pro-psychotic effects of synthetic cannabinoids: interactions with central dopamine, serotonin, and glutamate systems. Drug Metabolism Reviews, 50(1), 65–73. https://doi.org/10.1080/03602532.2018.1428343
- Fink, M. (1980). An objective classification of psychoactive drugs. Progress in Neuro-Psychopharmacology, 4(4-5), 495–502. https://doi.org/10.1016/0364-7722(80)90019-3
- Fletcher, E. H., Tasker, S. M., Easton, P., & Denvir, L. (2016). Improving the help and support provided to people who take new psychoactive substances ('legal highs')). Journal of Public Health (Oxford, England), 38(4), e489–e495. https://doi.org/10.1093/pubmed/fdv191
- Gilani, F. (2015). Legal highs’: Novel psychoactive substances. InnovAiT: Education and Inspiration for General Practice, 8(12), 717–724. https://doi.org/10.1177/1755738015612509
- Gilmour, J. S., & Walters, S. M. (1964). Philosophy and Classification. In W. B. Turrill (Ed.), Vistas in Botany. (pp. 1–22). Pergamon Press.
- Hearne, E., & Van Hout, M. C. (2016). "Trip-Sitting" in the black hole: a netnographic study of dissociation and indigenous harm reduction. Journal of Psychoactive Drugs, 48(4), 233–242. https://doi.org/10.1080/02791072.2016.1207827
- Herrling, P. L., Emre, M., & Watkins, J. (1997). D-CPPene (SDZ EAA-494)—a competitive NMDA antagonist: pharmacology and results in humans. In P. L. Herrling (Ed.), Excitatory Amino Acids. (pp. 7–21). Academic Press.
- Home Office (2015). New Psychoactive Substances (NPS) Resource Pack for informal educators and practitioners. https://www.gov.uk/government/publications/new-psychoactive-substances-nps-resource-pack
- Home Office (2018). Review of the Psychoactive Substances Act 2016. Crown Copyright. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/756902/Review_of_the_Psychoactive_Substances_Act__2016___print_-_content_.pdf
- Jacobsen, E. (1959). The comparative pharmacology of some psychotropic drugs. Bulletin of the World Health Organization, 21(4-5), 411–493.
- Johnson, J. R., Burnell-Nugent, M., Lossignol, D., Ganae-Motan, E. D., Potts, R., & Fallon, M. T. (2010). Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC:CBD extract and THC extract in patients with intractable cancer-related pain. Journal of Pain and Symptom Management, 39(2), 167–179. https://doi.org/10.1016/j.jpainsymman.2009.06.008
- Julien, R. M., Advokat, C. D., & Comaty, J. E. (2011). A Primer of Drug Action: A comprehensive guide to the actions, uses, and side effects of psychoactive drugs, revised and updated. (12 ed.). Worth.
- Jünger, E. (1970). Annäherungen: Drogen und Rausch. Klett-Cotta. https://libcom.org/files/Approaches%20-%20Drugs%20and%20Ecstatic%20Intoxication%20-%20Ernst%20Junger_1.pdf
- King, L. A. (2013). Novel psychoactive substances classification, pharmacology and toxicology. In P. I. Dargan & D. M. Wood (Eds.), Novel psychoactive substances: classification, pharmacology and toxicology. Academic Press.
- Leonard, B. E. (2010). Classification of psychoactive drugs. In I. Stolerman (Ed.), Encyclopedia of Psychopharmacology. (pp. 293–302). Springer.
- Lewin, L. (1924). Phantastica: Die betaubenden und erregenden Genussmittel. Georg Stilke. https://publikationsserver.tu-braunschweig.de/receive/dbbs_mods_00036941
- Liechti, M. E. (2015). Novel psychoactive substances (designer drugs): overview and pharmacology of modulators of monoamine signaling. Swiss Medical Weekly, 145, w14043. https://doi.org/10.4414/smw.2015.14043
- Lingford-Hughes, A. (2004). Drugs of abuse. In I. M. Anderson & I. C. Reid (Eds.), Fundamentals of Clinical Psychopharmacology. (2nd ed., pp. 114–127). Taylor & Francis.
- Macdonald, I. (2019). Teen Substance Use, Mental Health and Body Image: Practical Strategies for Support. Jessica Kingsley Publishers.
- MacLeod, K., Pickering, L., Gannon, M., Greenwood, S., Liddel, L, Smith, A., Johnstone, L., & Burton, G. (2016). Understanding the patterns of use, motives, and harms of new psychoactive substances in Scotland. Final report to the Scottish Government. https://www.gov.scot/publications/understanding-patterns-use-motives-harms-new-psychoactive-substances-scotland/
- Maier, J., Mayer, F. P., Luethi, D., Holy, M., Jäntsch, K., Reither, H., Hirtler, L., Hoener, M. C., Liechti, M. E., Pifl, C., Brandt, S. D., & Sitte, H. H. (2018). The psychostimulant (±)-cis-4,4'-dimethylaminorex (4,4'-DMAR) interacts with human plasmalemmal and vesicular monoamine transporters. Neuropharmacology, 138, 282–291. https://doi.org/10.1016/j.neuropharm.2018.06.018
- Marwick, K. (2019). Crash Course Psychiatry. (5th ed.). Elsevier.
- McCandless, D. (2010). Drugs World. Retrieved 30 May 2021 from https://www.informationisbeautiful.net/visualizations/drugs-world/
- McHound (2009). 5-MEO-DALT. https://drugs-forum.com/threads/5-meo-dalt-experiences.40544/page-4#post-904818
- McKelvey, B. (1978). Organizational systematics: Taxonomic lessons from biology. Management Science, 24(13), 1428–1440. https://doi.org/10.1287/mnsc.24.13.1428
- Measham, F. (2019). Drug safety testing, disposals and dealing in an English field: Exploring the operational and behavioural outcomes of the UK's first onsite 'drug checking' service. The International Journal on Drug Policy, 67, 102–107. https://doi.org/10.1016/j.drugpo.2018.11.001
- Measham, F. (2020a). City checking: Piloting the UK's first community-based drug safety testing (drug checking) service in 2 city centres. British Journal of Clinical Pharmacology, 86(3), 420–428. https://doi.org/10.1111/bcp.14231
- Measham, F. (2020b). The NPS imposters, merging and emerging drug markets and the contribution of drug checking. In D. Bewley-Taylor & K. Tinasti (Eds.), Research Handbook on International Drug Policy. (pp. 341–354). Edward Elgar Publishing.
- Measham, F. (2021). Social issues in the use of novel psychoactive substances: differentiated demand, displacement and adulteration. In P. Dargan & D. Wood (Eds.), Novel Psychoactive Substances: Classification, Pharmacology and Toxicology. (2nd ed., pp. 105–127). Elsevier.
- Measham, F., & Newcombe, R. (2016). What's so 'new' about new psychoactive substances? Definitions, prevalence, motivations, user groups and a proposed new taxonomy. In T. Kolind, B. Thom, & G. Hunt (Eds.), The SAGE handbook of drug alcohol studies - social science approaches. (pp. 576–596). SAGE Publications Ltd. https://doi.org/10.4135/9781473921986.n33
- Measham, F., & Turnbull, G. (2021). Intentions, actions and outcomes: A follow up survey on harm reduction practices after using an English festival drug checking service. The International Journal on Drug Policy, 95, 103270. https://doi.org/10.1016/j.drugpo.2021.103270
- Mercier, C. A. (1912). A new logic. Open Court Publishing Company.
- Mindspelunker (2011). Into the M-Hole. https://www.erowid.org/experiences/exp.php?ID=90865
- Möller, I., Wintermeyer, A., Bender, K., Jübner, M., Thomas, A., Krug, O., Schänzer, W., & Thevis, M. (2011). Screening for the synthetic cannabinoid JWH‐018 and its major metabolites in human doping controls. Drug Testing and Analysis, 3(9), 609–620. https://doi.org/10.1002/dta.158
- Moore, K., & Measham, F. (2011). Impermissible pleasures in UK leisure: Exploring policy developments in alcohol and illicit drugs. In C. Jones, E. Barclay, & R. Mawby (Eds.), The Problem of Pleasure: Leisure, Tourism and Crime. (pp. 62–76). Willan.
- Morean, M. E., de Wit, H., King, A. C., Sofuoglu, M., Rueger, S. Y., & O'Malley, S. S. (2013). The drug effects questionnaire: psychometric support across three drug types. Psychopharmacology, 227(1), 177–192. https://doi.org/10.1007/s00213-012-2954-z
- Morgan, C. J., Muetzelfeldt, L., & Curran, H. V. (2010). Consequences of chronic ketamine self‐administration upon neurocognitive function and psychological wellbeing: a 1‐year longitudinal study. Addiction (Abingdon, England), 105(1), 121–133. https://doi.org/10.1111/j.1360-0443.2009.02761.x
- Newcombe, R. (1987). High time for harm reduction. Druglink, 2(1), 10.
- Newcombe, R. (1999). Psychonautics: A model and method for exploring the subjective effects of psychoactive drugs. Club Health 2000 – First International Conference on Nightlife and Substance Use. https://www.researchgate.net/publication/268576819_Psychonautics_a_model_and_method_for_exploring_the_subjective_effects_of_psychoactive_drugs
- Páleníček, T., Lhotková, E., Žídková, M., Balíková, M., Kuchař, M., Himl, M., Mikšátková, P., Čegan, M., Valeš, K., Tylš, F., & Horsley, R. R. (2016). Emerging toxicity of 5,6-methylenedioxy-2-aminoindane (MDAI): Pharmacokinetics, behaviour, thermoregulation and LD50 in rats. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 69, 49–59. https://doi.org/10.1016/j.pnpbp.2016.04.004
- Parrott, A. C. (2002). Recreational Ecstasy/MDMA, the serotonin syndrome, and serotonergic neurotoxicity. Pharmacology Biochemistry and Behavior, 71(4), 837–844. https://doi.org/10.1016/S0091-3057(01)00711-0
- Pates, R., & Riley, D. M. (2012). Harm reduction in substance use and high-risk behaviour international policy and practice. Wiley-Blackwell.
- Potter, G. R., & Chatwin, C. (2018). Not particularly special: critiquing ‘NPS’ as a category of drugs. Drugs: Education, Prevention and Policy, 25(4), 329–336. https://doi.org/10.1080/09687637.2017.1411885
- Ruane, D. (2018). Field experiments: psychonauts' efforts to reduce the harm of old and new drugs at music festivals. Drugs: Education, Prevention and Policy, 25(4), 337–344. https://doi.org/10.1080/09687637.2017.1418836
- Sáez-Briones, P., & Hernández, A. (2013). MDMA (3, 4-methylenedioxymethamphetamine) analogues as tools to characterize MDMA-like effects: an approach to understand entactogen pharmacology. Current Neuropharmacology, 11(5), 521–534. https://doi.org/10.2174/1570159X11311050007
- Sahai, M., Davidson, C., Dutta, N., & Opacka-Juffry, J. (2018). Mechanistic Insights into the Stimulant Properties of Novel Psychoactive Substances (NPS) and Their Discrimination by the Dopamine Transporter—In Silico and In Vitro Exploration of Dissociative Diarylethylamines. Brain Sciences, 8(4), 63. https://doi.org/10.3390/brainsci8040063
- Sainsbury, P., Kicman, A., Archer, R., King, L., & Braithwaite, R. (2011). Aminoindanes—the next wave of ‘legal highs’? Drug Testing and Analysis, 3(7-8), 479–482. https://doi.org/10.1002/dta.318
- Sammut, D., & Craig, C. (2019). Bitter pill: Testing times for party drugs. Chemistry in Australia.
- Schifano, F., Albanese, A., Fergus, S., Stair, J. L., Deluca, P., Corazza, O., Davey, Z., Corkery, J., Siemann, H., Scherbaum, N., Farre', M., Torrens, M., Demetrovics, Z., & Ghodse, A. H., ReDNet Research Groups (2011). Mephedrone (4-methylmethcathinone; 'meow meow'): chemical, pharmacological and clinical issues. Psychopharmacology, 214(3), 593–602. https://doi.org/10.1007/s00213-010-2070-x
- Schifano, F., Napoletano, F., Chiappini, S., Orsolini, L., Guirguis, A., Corkery, J. M., Bonaccorso, S., Ricciardi, A., Scherbaum, N., & Vento, A. (2019). New Psychoactive Substances (NPS), psychedelic experiences and dissociation: clinical and clinical pharmacological issues. Current Addiction Reports, 6(2), 140–152. https://doi.org/10.1007/s40429-019-00249-z
- Scotton, W. J., Hill, L. J., Williams, A. C., & Barnes, N. M. (2019). Serotonin syndrome: pathophysiology, clinical features, management, and potential future directions. International Journal of Tryptophan Research : IJTR, 12, 1178646919873925. https://doi.org/10.1177/1178646919873925
- Seifert, R., & Schirmer, B. (2020). A simple mechanistic terminology of psychoactive drugs: a proposal. Naunyn-Schmiedeberg's Archives of Pharmacology, 393(8):1331–1339. https://doi.org/10.1007/s00210-020-01918-x
- Shulgin, A., & Shulgin, A. (1991). PIKHAL: A Chemical Love Story. Transform Press.
- Simmler, L. D., & Liechti, M. E. (2018). Pharmacology of MDMA- and Amphetamine-Like New Psychoactive Substances. In H. Maurer & S. Brandt (Eds.), New Psychoactive Substances. Handbook of Experimental Pharmacology. (Vol. 252, pp. 143–164). Springer International Publishing. https://doi.org/10.1007/164_2018_113
- Soussan, C., & Kjellgren, A. (2014). Harm reduction and knowledge exchange-a qualitative analysis of drug-related Internet discussion forums. Harm Reduct J, 11(1), 25–25. https://doi.org/10.1186/1477-7517-11-25
- Stevens, A., & Measham, F. (2014). The ‘drug policy ratchet’: why do sanctions for new psychoactive drugs typically only go up? Addiction, 109(8), 1226–1232. https://doi.org/10.1111/add.12406
- Stolerman, I. (Ed.) (2010). Encyclopedia of psychopharmacology. Berlin: Springer Science & Business Media.
- Sumnall, H. R., Cole, J. C., & Jerome, L. (2006). The varieties of ecstatic experience: an exploration of the subjective experiences of ecstasy. Journal of Psychopharmacology (Oxford, England), 20(5), 670–682. https://doi.org/10.1177/0269881106060764
- UNODC (2013). The challenge of new psychoactive substances: a Report from the Global SMART Programme. https://www.unodc.org/unodc/en/scientists/the-challenge-of-new-psychoactive-substances–-global-smart-programme.html
- Van Hout, M. C., & Brennan, R. (2011). Heads held high’: an exploratory study of legal highs in pre-legislation Ireland. Journal of Ethnicity in Substance Abuse, 10(3), 256–272. https://doi.org/10.1080/15332640.2011.600210
- Zinberg, N. E. (1984). Drug set and setting: the basis for controlled intoxicant use. Yale University Art Gallery.
- Zohar, J., Nutt, D. J., Kupfer, D. J., Moller, H.-J., Yamawaki, S., Spedding, M., & Stahl, S. M. (2014). A proposal for an updated neuropsychopharmacological nomenclature. European Neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology, 24(7), 1005–1014. https://doi.org/10.1016/j.euroneuro.2013.08.004