Abstract
Human milk oligosaccharides (hMOs) in mothers’ milk play a crucial role in guiding the colonization of microbiota and gut-immune barrier development in infants. Non-digestible carbohydrates (NDCs) such as synthetic single hMOs, galacto-oligosaccharides (GOS), inulin-type fructans and pectin oligomers have been added to infant formula to substitute some hMOs’ functions. HMOs and NDCs can modulate the gut-immune barrier, which is a multiple-layered functional unit consisting of microbiota, a mucus layer, gut epithelium, and the immune system. There is increasing evidence that the structures of the complex polysaccharides may influence their efficacy in modulating the gut-immune barrier. This review focuses on the role of different structures of individual hMOs and commonly applied NDCs in infant formulas in (i) direct regulation of the gut-immune barrier in a microbiota-independent manner and in (ii) modulation of microbiota composition and microbial metabolites of these polysaccharides in a microbiota-dependent manner. Both have been shown to be essential for guiding the development of an adequate immune barrier, but the effects are very dependent on the structural features of hMO or NDC. This knowledge might lead to tailored infant formulas for specific target groups.
Introduction
Human breastmilk is considered to be the gold standard for infant nutrition and is responsible for the guidance of gut microbiota colonization and the promotion of the development of a healthy immune system and gut barrier (Allan Walker Citation2013; Smilowitz et al. Citation2014; Walker Citation2010). Human milk oligosaccharides (hMOs) as the third most abundant nutrient after lactose and lipids in human milk are considered to be highly significant in this guidance (Allan Walker Citation2013; Smilowitz et al. Citation2014; Zuurveld et al. Citation2020). The majority of hMOs resist digestion by human enzymes in the upper part of the gastrointestinal (GI) tract and enter the colon where they are metabolized by microorganisms (Engfer et al. Citation2000). Many hMOs penetrate the gut (sub)mucosa and support the development of a healthy immune system (Zuurveld et al. Citation2020). HMOs are different in structure and have different functional groups. About 200 structurally distinct forms are currently identified (Zuurveld et al. Citation2020).
In case breastfeeding is not an option for newborns, feeding cow milk-derived infant formula is usually the only alternative (Akkerman, Faas, and de Vos Citation2019). However, due to the uniqueness and structural complexity of hMOs in mother milk, producing synthetic hMOs-like structures is difficult and expensive (Akkerman, Faas, and de Vos Citation2019). Currently, there are only a few commercially available synthetic hMOs which are 2′-fucosyllactose (2′-FL), 3-fucosyllactose (3-FL), 3′-sialyllactose (3′-SL), 6′-sialyllactose (6′-SL), and 3′-galactosyllactose (3′-GL) and lacto-N-neotetraose (LNnT) (Zuurveld et al. Citation2020). Therefore, most infant formulas contain more affordable alternatives for hMOs which are mostly non-digestible carbohydrates (NDCs) (Akkerman, Faas, and de Vos Citation2019). NDCs just like hMOs have impacts on gut microbiota and the development of the gut-immune barrier (Kong et al. Citation2020). Up to now, NDCs such as galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) are used to supplement cow milk-derived infant formulas (Akkerman, Faas, and de Vos Citation2019). Especially mixtures of GOS and FOS in a ratio of 9:1 are widely used in infant formula and have been shown to guide the formation of gut microbiota very similar to that of breastfed infants (Akkerman, Faas, and de Vos Citation2019; Böger et al. Citation2019). Pectin, another type of NDC, has received considerable scientific attention for its prebiotic properties and modulating effects on the gut immune barrier (Beukema, Faas, et al. Citation2020; Verkhnyatskaya et al. Citation2019). To supplement infant formula with functional oligosaccharides, pectin-derived acidic oligosaccharides (pAOS) are suggested as an alternative source of hMOs acidic oligosaccharides (Bode and Jantscher-Krenn Citation2012). Several clinical studies with infant have demonstrated that pAOS supplementation in infant formula exerts beneficial effects on both healthy term infants (Fanaro et al. Citation2005) and on preterm infants (Westerbeek et al. Citation2010; Westerbeek et al. Citation2011). Additionally, there is evidence that, depending on NDCs composition, the NDCs promoted either Th1, Th2, or Treg immune responses (Bermudez-Brito, Rösch, et al. Citation2015; Bermudez-Brito, Sahasrabudhe, et al. Citation2015).
In recent years, it has been shown that NDCs can have these beneficial effects in infants via at least two mechanisms. They can either interact (i) directly with the epithelium or immune cells in the digestive tract or (ii) they can support the development and colonization of gut microbiota in the large intestine (Cai et al. Citation2020). Only the NDCs that escape digestion by host enzymes and are not absorbed in the upper GI tract can transit to the large intestine (Louis et al. Citation2007) where the vast majority of gut microbiota is present (Heiss and Olofsson Citation2018). These NDCs can serve as the substrate for microbiota fermentation resulting in changes in microbiota composition which further stimulate the immune system (Rastall et al. Citation2022). Also, during the fermentation of NDCs, some metabolic end-products such as short-chain fatty acids (SCFAs) are formed which also have immunomodulatory functions (Rastall et al. Citation2022). Moreover, there is accumulating evidence demonstrating that the fermentation of hMOs and NDCs may also impact the bacterial generation of indole derivatives (Akkerman et al. Citation2022). Indole derivatives have been proven to play a crucial role in maintaining intestinal homeostasis (Ye et al. Citation2022).
During recent years we and others have shown that different compositions and structures of NDCs or hMOs may have different effects on either gut microbiota or on the intestinal immune barrier function. However, not many reviews have critically summarized and compared such effects in view of the application of these molecules in infant formula. Therefore, this manuscript focuses on reviewing current insight into the structure-relationship of commonly applied NDCs including pectins, GOS and inulin-type fructans (ITFs) on gut-immune barrier function in view of applicants in infant formula for stimulating the development of a healthy gut.
The gut barrier
The gut-immune barrier is considered to be the gatekeeper of the human body. It is an enormous interface separating the host from the luminal content of the intestine (Bischoff et al. Citation2014; Figueroa‐Lozano and de Vos Citation2019). Interestingly, the GI tract performs two opposite actions at the same time. It is selectively permeable for the body’s nutrients, water, and electrolytes that are present in the gut lumen but at the same time, it protects the host from the invasion of harmful substances such as pathogens and luminal proinflammatory factors (Assimakopoulos et al. Citation2018; König et al. Citation2016). To perform these tasks the intestinal immune barrier is composed of a multi-layered functional unit containing the gut bacteria, a mucus layer, epithelial cells, and immune cells in the lamina propria (Martel et al. Citation2022; Viggiano et al. Citation2015) ().
Figure 1. Structural components of the gut-immune barrier. The gut-immune barrier is a multi-layered structural unit consisting of gut microbiota, the internal mucus layer containing mucins, antimicrobial proteins, and immunoglobulin A (IgA), the epithelial monolayer with enterocytes, goblet cells, Paneth cells, and microfold (M) cells which are connected by tight junctions (TJs); and different immune cells within lamina propria, e.g., macrophages, dendritic cells (DCs), and T-cells. The mucus layer is the small intestine is composed of a single layer while in the large intestine it is composed of two layers. It starts with a loose, outer layer that serves as resident site for the gut microbiota and a firm inner layer in which bacteria are rare. This illustration depicts the barrier in the large intestine.
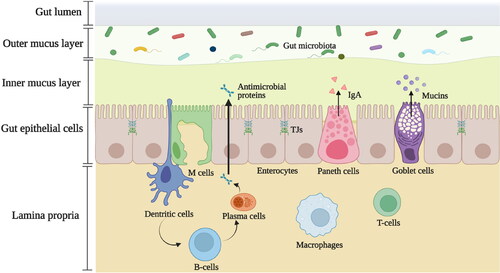
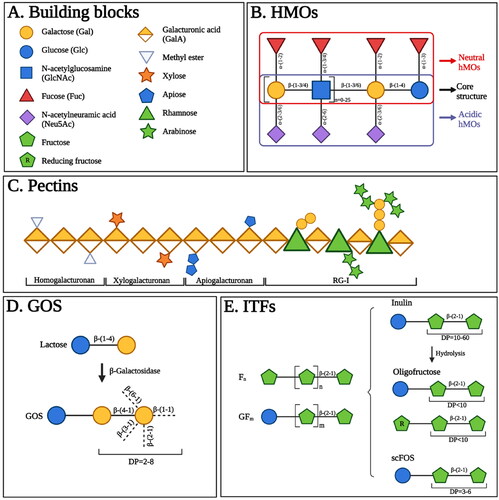
Figure 2. The structures of human milk oligosaccharides (hMOs), pectins, galacto-oligosaccharides (GOS), and inulin-type fructans (ITFs). (A). Main building blocks of hMOs, pectins, GOS and ITFs. (B). HMOs are composed of five building blocks, including glucose (Glc), galactose (Gal), N-acetylglucosamine (GlcNAc), fucose (Fuc), and N-acetylneuramic acid (Neu5Ac). Each hMO possesses a core structure, the Gal-GlcNAc-Gal-Glc unit. The addition of Fuc or Neu5Ac residues can further enrich the core structure of hMOs resulting in neutral hMOs or acid hMOs, respectively. (C). Pectins contain several structural components including homogalacturonan, xylogalacturonan, apiogalacturonan and rhamogalacturona I (RG-I). Homogalacturonan is made up of galacturonic acid (GalA). The GalA residues can be methyl-esterified and are displayed as methyl esters. Xylogalacturonan and apiogalacturonan are the homogalacturonan with attached xylose and apiose residues, respectively. RG-I consists of a backbone in which GalA and rhamnose are alternated, and contain branched chains containing galactose, arabinose, or a combination thereof. (D). GOS are synthesized via the enzymatic trans-galactosylation of lactose by β-galactosidase. GOS are made up of Gal units linked by diverse glycosidic bonds along with a Glc unit at the reducing end. The degree of polymerization (DP) of GOS ranges from 2-8. (E). ITFs mainly consist of fructose (Fn) and a starting Glc unit can be included as well (GFm). The magnitude of n and m determines the DP of ITFs. According to DP values, ITF is classified into inulin (DP = 10-60), oligofructose (DP < 10) derived from the hydrolysis of inulin; and short-chain fructooligosaccharides (scFOS) (DP = 3-6).
Gut microbiota
Gut microbiota composition in the GI tract
The adult human Gl tract harbors more than 1000 different bacterial species, including bacteria, protozoa, yeasts, and fungi (Rowland et al. Citation2018; Turner Citation2018), which forms a dynamic and complex community, collectively defined as the gut microbiota (Natividad and Verdu Citation2013). They establish a lifelong symbiotic association with human intestinal cells (Hooper Citation2009). During the postnatal period, the gut microbiota begins to colonize the newborn’s gut (Milani et al. Citation2017). In this early life phase, the majority of the microorganisms are exclusively anaerobic (Dieterich, Schink, and Zopf Citation2018). Microbiota diversity increases with age until the host matures to a stable microbiota composition predominated by three bacterial phyla, namely, Bacteroidetes, Firmicutes, and Proteobacteria (Dieterich, Schink, and Zopf Citation2018; Rinninella et al. Citation2019). Even though this overall profile keeps constant till and during adulthood, the diversity and quantity of intestinal microbes exhibit significant variations in the distribution along the longitudinal side of the GI tract (Jandhyala et al. Citation2015). To illustrate this variation; from the distal esophagus to the large intestine, the number of gut microorganisms increases from roughly ten per gram in the esophagus and stomach to around one trillion per gram in the colon and rectum (O’Hara and Shanahan Citation2006). Streptococcaceae is the dominant genus inhabiting the distal esophagus, duodenum, and jejunum while Helicobacter is the major resident of the stomach (Jandhyala et al. Citation2015). From the distal part of the small intestine to the colon, the main colonizing bacterial species change from Veillonella and Lactobacillus to Lachnospiraceae and the phyla Bacteroidetes (Dieterich, Schink, and Zopf Citation2018). However, also other species are present in the gut lumen as a wide variety of gut luminal microbes can be found in feces including Bacteroides, Bifidobacterium, Enterobacteriaceae, and Ruminococcus (Sekirov et al. Citation2010). Current insight is that the microorganisms contribute to the barrier for invading agents in several ways as will be explained in the next section.
Gut microbiota functions
The gut microbiota serves as a biological barrier and by that positively impacts intestinal health (Assimakopoulos et al. Citation2018; Jandhyala et al. Citation2015). Gut microbes via their structural components induce the production of antimicrobial proteins (AMP) released by Paneth cells (Thursby and Juge Citation2017). Moreover, some intestinal microorganisms, such as Bacteroides, can activate gut dendritic cells (DCs), which stimulate plasma cells to produce secretory immunoglobulin A (SIgA) (Jandhyala et al. Citation2015). In addition, the gut microbiota ferments molecules that are indigestible by human enzymes, such as dietary fibers. During this process, a variety of metabolites are produced, such as SCFAs (Valdes et al. Citation2018). Generally, the production of SCFA exerts beneficial physiological effects. SCFAs, are for example an energy substrate for enterocytes (Wozniak et al. Citation2022) and can be quickly absorbed from the intestinal lumen (Hamer et al. Citation2008). SCFAs promote epithelial cell proliferation and enforce barrier function by strengthening connections between epithelial cells. Also, they regulate immune response (Parada Venegas et al. Citation2019).
Gut mucus layer
Gut mucus composition
The mucus layer makes up the first line of physical defense to protect the underlying cells of the digestive tract (Vancamelbeke and Vermeire Citation2017). From the upper part to the lower part of the digestive tract, the mucus layer becomes progressively thicker (Atuma et al. Citation2001). The small intestine only has one layer of mucus while the large intestine is composed of two layers: an inner layer, closely attached to the epithelial cells without bacterial inhabitants, and an outer layer, which is thicker and looser and colonized by commensal microbiota (Viggiano et al. Citation2015). The goblet cells synthesize and release the mucus. This forms the mucus layer which is a watery but viscous secretion product containing more than 95% water, along with electrolytes and lipids. About 1 to 5% is highly glycosylated mucus protein which plays a functional role in mucus-function (Bansil and Turner Citation2018; Pelaseyed et al. Citation2014). Together they form a gel-like sieve structure covering the gut epithelial cells (Vancamelbeke and Vermeire Citation2017). Mucin 2 (MUC2) is the most prevalent mucus glycoprotein in the small and large intestine (Vancamelbeke and Vermeire Citation2017). A previous study has found that colitis occurred in Muc2 knock-out mice, illustrating the importance of MUC2 expression for intestinal health (Van der Sluis et al. Citation2006). Moreover, some mucins are solely expressed in specific sites of the GI tract, for example, MUC5AC mucin is predominant in the gastric glands, MUC6 is expressed in Brunner’s gland of the duodenum and MUC5B is marginally expressed in the colon (Paone and Cani Citation2020). In addition to these gel-forming mucins, gut epithelial cells also express transmembrane mucins such as MUC1, MUC4, MUC13, and MUC16 (Cornick, Tawiah, and Chadee Citation2015; Vancamelbeke and Vermeire Citation2017). These mucins are not responsible for mucus gel production but instead responsible for protecting cells or are involved in some signaling pathways linked to tumor occurrence (Cornick, Tawiah, and Chadee Citation2015; Paone and Cani Citation2020). However, their specific functions are still not fully elucidated (Cornick, Tawiah, and Chadee Citation2015).
Gut mucus functions
The gut mucus has multiple beneficial functions to maintain intestinal homeostasis. It acts as a humectant to prevent dehydration of epithelial cells and as a lubricant for intestinal motility (Paone and Cani Citation2020; Viggiano et al. Citation2015). Furthermore, the gut mucus layer works as a dynamic semi-permeable barrier that selectively allows the diffusion of nutrients, water, and ions (Cone Citation2009). But, at the same time, as part of the innate gut mucosal barrier prevents diffusion of undesirable molecules (e.g., antigens) and pathogens from directly contacting the intestinal epithelium (Corfield Citation2015). The mucus layer also displays antimicrobial properties due to the presence and action of Paneth cell-derived AMP (Allam-Ndoul, Castonguay-Paradis, and Veilleux Citation2020). Finally, mucus can regulate immunity as mucin glycans can bind to lectin-like receptors on immune cells and exerts direct immunological effects (Paone and Cani Citation2020).
Gut epithelium
Gut epithelial cells
The gut epithelium is a single layer consisting of different columnar intestinal epithelial cells (IECs). It includes enterocytes, goblet cells, enteroendocrine cells, tuft cells, microfold (M) cells, and Paneth cells (Ghosh et al. Citation2021; Ulluwishewa et al. Citation2011). These IECs cooperatively create a physical barrier dividing the luminal contents from the lamina propria (Beukema, Faas, et al. Citation2020). The cells are functionally diverse and imperative for deleting numerous antigens in the gut lumen, thereby enhancing gut barrier defense (Goto Citation2019).
Enterocytes, as the most dominant cell type compromise over 80% of all IECs (Ulluwishewa et al. Citation2011), generate AMP such as Ly6/PLAUR domain containing 8 (Lypd8), C-type lectin and regenerating islet-derived 3-gamma (RegIIIγ) in both small intestine and colon (Goto Citation2019; Peterson and Artis Citation2014). Enterocytes also assist plasma cells in the lamina propria to produce SIgA. On the basal side of the enterocyte membrane, polymeric immunoglobulin receptors (pIgR) are expressed and bind to dimeric immunoglobulin A (IgA). The IgA molecules are produced by plasma cells and released into the lumen (Goto Citation2019).
The proportion of goblet cells gradually increases along the GI tract. It makes up around at most 10% and even over 20% of all IECs in the upper small intestine and distal colon, respectively (Mowat and Agace Citation2014). Goblet cells secrete mucus but also release anti-inflammatory molecules beneficial for gut defense. This includes trefoil factor 3 (TFF3), and resistin-like molecule-β (RELMβ) (Goto Citation2019; Shemtov et al. Citation2022). TFF3 promotes mucus layer integrity by supporting mucin cross-linking and serves as a tissue protective molecule that inhibits apoptosis and facilitates epithelial repair (Goto Citation2019; Peterson and Artis Citation2014). RELMβ encourages MUC2 secretion and modulates macrophage and adaptive T-cell responses during inflammation (Peterson and Artis Citation2014). Moreover, goblet cells act as antigen-presenting cells (APCs) and present luminal antigens to CD103+ DCs stimulating Treg cells development (McDole et al. Citation2012).
Enteroendocrine cells are present in both the small intestine and colon (Ghosh et al. Citation2021). They secrete hormones glucagon-like peptide-2 (GLP-2) which has a positive effect on intestinal integrity (Ghosh et al. Citation2021). GLP-2 stimulates tight junction (TJ) proteins like occludin and attenuates TNF-α induced alterations in TJ proteins along the colonic epithelial cells (Ghosh et al. Citation2021). Tuft cells are present in lower numbers in between both the small and large intestinal epithelium, but are crucial in anti-helminthic immunity (Hendel et al. Citation2022). They recognize luminal helminths through their GTP-binding protein, α-gustducin, and subsequently release IL-25 and thymic stromal lymphopoietin (TSLP) to stimulate a Th2 immune response preventing helminth infection (Goto Citation2019).
M cells are present only in the small intestine (Ghosh et al. Citation2021). They are enriched in the follicle-associated epithelium on the luminal surface of intestinal lymphoid structures, like Peyer’s patches (PPs) (Mabbott et al. Citation2013). They are responsible for sampling the luminal antigens followed by presenting them to the underlying mucosal immune system (Mabbott et al. Citation2013). Paneth cells only exist in the small intestine (Ghosh et al. Citation2021). They have antibacterial effects through AMP release such as α-defensins, lysozyme, antimicrobial lectins (RegIIIβ and RegIIIγ) (Clevers and Bevins Citation2013), and secretory phospholipase A2 (sPLA2) (Goto Citation2019), which supports the gut innate defense (Ayabe et al. Citation2004).
The epithelial cells also express several pattern recognition receptors (PRRs) involving Toll-like receptors (TLRs) and nucleotide-binding oligomerization domain-containing protein 2 (NOD2) (Shi et al. Citation2017). Through the PRRs, microbes can initiate the release of molecules such as chemokines, and pro- and anti-inflammatory cytokines, which are vital for adaptive immunity and for preventing autoimmunity (Shi et al. Citation2017).
Junctional complexes between gut epithelial cells
Neighboring epithelial cells are firmly connected by intercellular junctional complexes. These connections safeguard paracellular transport pathways while simultaneously maintaining the integrity of the gut barrier (Lee, Moon, and Kim Citation2018; Ulluwishewa et al. Citation2011). The junctional complexes include tight junctions (TJs), adherents junctions (AJs), gap junctions, and desmosomes (Farquhar and Palade Citation1963). TJs are situated on the apical side of the epithelium, where they form a ring-like structure through the linkage of transmembrane proteins and intracellular scaffold proteins (Ghosh et al. Citation2021; Schulzke and Fromm Citation2009). Transmembrane proteins contain claudins, occludin, tricellulin, and junctional adhesion molecules (JAM), and the intracellular cytoskeletal proteins are composed of zonula occludens (ZO-1, ZO-2, and ZO-3) (Ghosh et al. Citation2021). AJs are located underneath the TJs (Ulluwishewa et al. Citation2011). The formation of AJs is also related to the actin cytoskeleton by a mechanism involving two adherent junctional proteins (Ulluwishewa et al. Citation2011; Viggiano et al. Citation2015). Specifically, cadherins are attached to the actin cytoskeleton via catenins (Viggiano et al. Citation2015). Gap junctions and desmosomes contribute to intracellular interaction and cell-cell binding, respectively (Garrod and Chidgey Citation2008; Sosinsky and Nicholson Citation2005). These complicated multiprotein structures strengthen the resistance of the gut epithelial barrier to potentially harmful molecules and pathogens in the lumen (Allam-Ndoul, Castonguay-Paradis, and Veilleux Citation2020). Partial or complete destruction of the junctions leads to an increase in gut permeability which permits undesired luminal components to invade the systemic circulation resulting in gut health issues (Allam-Ndoul, Castonguay-Paradis, and Veilleux Citation2020).
Gut immune system
Up to 70% of the body’s immune cells are located in the GI tract which makes the intestine the largest immunological organ of the human body (Pabst, Russell, and Brandtzaeg Citation2008; Viggiano et al. Citation2015). Intraepithelial lymphocytes (IELs) located in between the epithelium have a regulatory function. IELs can release IFN-γ and keratinocyte growth factors to prevent epithelial cells from injury (Shi et al. Citation2017). Besides, a large number of immune cells are organized in gut-associated lymphoid tissue (GALT), which contains the lamina propria, PPs, and mesenteric lymph nodes (MLNs) (Beukema, Faas, et al. Citation2020; Viggiano et al. Citation2015).
The lamina propria located below the gut epithelial cells provides a homing area for innate immune cells, including innate lymphocytes (ILCs), DCs, macrophages, as well as adaptive immune cells, such as T cells and B cells (Mowat and Agace Citation2014; Shi et al. Citation2017). ILCs generate IL-22 after activation, which contributes to homeostasis and healing during intestinal infections (Shi et al. Citation2017). DCs and macrophages identify luminal antigens after PRR-binding and present antigens to adaptive immune cells in the GALT, which activates the differentiation of B cells into plasma cells to secrete IgA or promote the differentiation of naive T cells into regulatory T cells or effector T cells (Th1, Th2, Th9, Th17 or Th22) (Beukema, Faas, et al. Citation2020). In addition, DCs penetrate the TJs between gut epithelial cells and enter the lumen directly to phagocytose pathogens such as E. coli and Salmonella (Rescigno et al. Citation2001).
PPs are scattered along the small intestine and are found beneath the epithelium where M cells are present (Reboldi and Cyster Citation2016). PPs receive antigens from M cells to initiate a proper immune response (Shi et al. Citation2017). PPs provide sites for the activation of B cells supporting the production of IgA-producing plasma cells (Shi et al. Citation2017). Secreted IgA exerts a protective effect on the intestinal barrier (Carasi et al. Citation2015). T cells and B cells return to the lamina propria after activation to take part in a specific immune response (Kuhn, Pedraza, and Demoruelle Citation2014).
Both the small and large intestines contain MLNs, which are crucial locations for T-cell activation (Houston et al. Citation2016). DCs move from intestinal tissues to MLNs where they present antigens and regulate the development, movement, and functional differentiation of adaptive immune system cells (Houston et al. Citation2016).
The effect of different structures of hMOs and NDCs on the gut-immune barrier
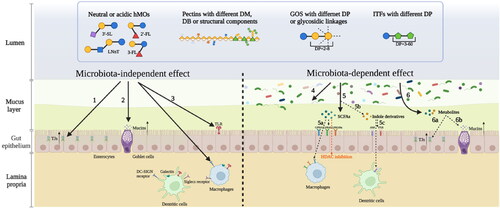
In this section, an overview is given of how different structures of hMOs and NDCs influence the intestinal barrier in microbiota-independent and microbiota-dependent manners with a focus on hMOs and three types of NDCs which are pectins, GOS, and ITFs.
Different structures of hMOs, pectins, GOS and ITFs ()
Human milk oligosaccharides
HMOs are unique for human milk and are composed of five types of monosaccharide units, including glucose (Glc), galactose (Gal), N-acetylglucosamine (GlcNAc), fucose (Fuc), and sialic acid with N-acetylneuramic acid (Neu5Ac) (Bode Citation2012). Each hMO possesses a core structure, namely the lactose unit which is a Gal-Glc unit connected by a β-(1-4) glycosidic linkage (Smilowitz et al. Citation2014). Lacto-N-biose or N-acetyllactosamine through β-(1-3) or β-(1-6) glycosidic bonds extend the lactose unit resulting in a linear or branched core structure (Ayechu-Muruzabal et al. Citation2018; Smilowitz et al. Citation2014). Lacto-N-biose or N-acetyllactosamine is the combination of Gal and GlcNAc linked by a β-(1-3) or β-(1-6) linkage, respectively (Bode Citation2012). The addition of Fuc or Neu5Ac residues can further enrich the core structure of hMOs (Ayechu-Muruzabal et al. Citation2018). Normally, the Fuc residues are attached to the core structure via α-(1-2), α-(1-3) or α-(1-4) linkages and the Neu5Ac residues are connected via α-(2-3) or α-(2-6) linkages (Smilowitz et al. Citation2014). There are three main kinds of hMOs: (1) Neutral (fucosylated) hMOs such as 2′-FL and Lactodifucopentaose; (2) Neutral N-containing hMOs such as LNnT and lacto-N-tetraose; (3) Acidic (sialylated) hMOs such as 2′-sialyllactose (2′-SL) and 3′-sialyllactose (3′-SL) (Wiciński et al. Citation2020).
Pectins
Pectins are structurally complex acidic heteropolysaccharides widely found in primary and secondary cell walls of plants (BeMiller Citation2018; Beukema, Faas, et al. Citation2020; Rastall et al. Citation2022). Their chemical structures are diverse and determined by their origin, location in the plant, and extraction method (Rastall et al. Citation2022). It contains linear stretches mainly made of galacturonic acid (GalA) linked by α-(1–4) glycosidic bonds (Beukema, Faas, et al. Citation2020; Blanco-Pérez et al. Citation2021). This is hypothesized to resemble the Sia residues in hMOs (Verkhnyatskaya et al. Citation2019). The GalA residues can be free or methyl-esterified via its carboxyl groups at C-6 and can then be displayed as methyl esters (Blanco-Pérez et al. Citation2021). The proportion of methyl-esterified GalA groups to the total GalA groups is defined as the degree of methyl-esterification (DM). According to this property, pectins are categorized as high DM pectin (DM > 50%) and low DM pectin (DM < 50%) (Liang et al. Citation2012). Pectins have several structural components which are homogalacturonan, xylogalacturonan, apiogalacturonan, rhamogalacturona I (RG-I), and rhamogalacturona II (RG-II). Homogalacturonan regions made up of only GalA are the major constituent in commercial pectin. The structures of xylogalacturonan and apiogalacturonan are the homogalacturonan with attached xylose and apiose residues, respectively. RG-I consists of a backbone in which GalA and rhamnose are alternated, and contain branched chains containing galactose, arabinose, or a combination thereof. The structures of RG-II are more complex, containing a GaLA-formed skeleton with up to 12 sugar residues located in its branched chains. (Beukema, Faas, et al. Citation2020) Another structural property determining functionality of pectins is the degree of blockiness (DB) which indicates the distribution of non-esterified GalA. Low DB pectins have a more random distribution of non-esterified GalA, while high DB pectins have a more blockwise distribution of non-esterified GalA (Beukema, Faas, et al. Citation2020).
Galacto-oligosaccharides
GOS are short-chain, non-digestible carbohydrates (Ibrahim Citation2018; Maráz et al. Citation2022). GOS can be synthesized through the enzymatic trans-galactosylation of lactose (Lac) by the microbial enzyme β-galactosidase derived from bacteria, yeasts, and fungi (Ibrahim Citation2018; Maráz et al. Citation2022). The typical structure of GOS is made up of galactose (Gal) units linked by diverse glycosidic bonds, including β-(1-1), β-(1-2), β-(1-3), β-(1-4), and β-(1-6), along with a glucose (Glc) unit at the reducing end (de Almeida and Maitan-Alfenas Citation2021). The degree of polymerization (DP) of GOS varies from 2 to 8 (Böger et al. Citation2019). However, as the enzymatic conversion of Lac-producing GOS is incomplete, most GOS also contain Lac and the Lac content may vary in different commercial GOS preparations (Figueroa-Lozano et al. Citation2020). Furthermore, there is a kind of plant-based GOS present in legume seeds, which structure contains a terminal sucrose unit connected by the Glc to Gal via α-(1-6) linkages (Marín-Manzano et al. Citation2020). Irrespective of its source the structures and composition of GOS are diverse due to variations in DP, glycosidic linkage types, and the content of oligosaccharide (Ambrogi et al. Citation2023; Figueroa-Lozano et al. Citation2020).
Inulin-type fructans
ITFs are natural components present in vegetables and fruits (e.g. onions, garlic, wheat, and bananas) (Roberfroid Citation2004). They are linear polydisperse carbohydrates that mainly consist of fructose monomers linked by β-(2-1) glycosidic linkages. A starting α-D-glucose moiety can be included as well (Jackson et al. Citation2022). They represent two structures, i.e., Fn and GFm, respectively. The G is the glucosyl moiety. F is the fructosyl moiety, and n or m refers to the amount of the fructosyl moieties (Roberfroid, Van Loo, and Gibson Citation1998). The magnitude of n and m determines the DP of ITFs. In other words, the DP represents the number of sugars in the polymer chain. Higher DP ITFs have a longer chain length and a larger molecular weight (Payling et al. Citation2020). According to DP values, ITF is classified into inulin (DP = 10-60) primarily from chicory root extraction, oligofructose (DP < 10) derived from the hydrolysis of inulin; and short-chain fructooligosaccharides (scFOS) (DP = 3-6) are usually synthesized from sucrose (Liu et al. Citation2016; Rastall et al. Citation2022).
The processes for manufacturing hMOs, pectins, GOS and ITFs
Human milk oligosaccharides
HMOs currently applied in products are predominantly produced by enzymatic in vitro reactions from lactose, by genetically modified microorganisms, or by chemical synthesis (Zeuner et al. Citation2019). HMOs structures can be extended from lactose at the non-reducing end and this process are catalyzed by glycosyltransferase (Chen Citation2015). For example, some sialylated hMOs, such as 3′-SL, 6′-SL, and disialyllacto-N-tetraose are synthesized by sialyltransferases with different specificities (Zeuner et al. Citation2019). 2 ‘-FL and LNnT were the first industrial-scale hMOs obtained from genetically engineered E. coli. HMO structures that are not yet on the market, such as LNT and difucosyllactose can also be produced in this way (Bych et al. Citation2019). Chemical synthesis of hMOs is less commonly used for large-scale production as it is time-consuming and associated with lower yields. Lacto-N-fucopentaose, LNT and 2-FL can be produced by this method but is not very cost-effective for inclusion in consumer products (Zeuner et al. Citation2019).
Pectins
Chemical extraction by acids is the most commonly applied method for pectin isolation from fruits or vegetables (Morales-Medina et al. Citation2022; Robledo and Vázquez Citation2019). Due to the high molecular weight and complex structure of pectins, their bioavailability is limited (Zhi et al. Citation2017). Therefore, modification of pectins is important for functionality. This involves the addition of new functional groups into natural pectins or the change of molecular weight and structures of pectins by several modification methods. This process can significantly influence pectin’s properties. Pectin modification includes chemical methods such as esterification and acetylation as well as physical methods such as pectin depolymerization by ultrasound and high pressure. Also, enzymatic modification using esterase, hydrolase, and lyase are commonly applied (Jiao et al. Citation2023). PAOS are produced by enzymatic hydrolysis of pectin, and their size depends on the enzyme used and the duration of the reaction (Fanaro et al. Citation2005).
Galacto-oligosaccharides
GOS synthesis depends on reactions such as lactose hydrolysis and transgalactosylation. A lactose unit reacts with the β-galactosidase to form a galactosyl-enzyme complex while releasing a glucose molecule. The transition intermediate then reacts with another lactose molecule to form a Gal-Gal-Glu trisaccharide (GOS-DP3). GOS-DP3 in turn can act as an acceptor of the galactosyl-enzyme complex to form a Gal-Gal-Gal-Glu tetrasaccharide (GOS-DP4). By analogy, GOS can be produced with a higher number of galactose units such as GOS-DP5 and GOS-DP6 (Vera et al. Citation2016).
Inulin-type fructans
Inulin-type fructans are extracted from chicory roots for commercial use and are marketed as native inulin with a DP of 2-60 (Kelly Citation2008; Logtenberg Citation2020). With the aid of enzymes including fructosyltransferases and B-d-fructofuranosidases, native inulin can be further hydrolyzed to produce fructooligosaccharides (FOS) with a DP of 2-10 (Picazo et al. Citation2019). FOS can also be isolated from inulin-rich plant materials or synthesized enzymatically from sucrose (Picazo et al. Citation2019). Long-chain inulin (DP 10-60) is produced by physically separating native inulin, and it is usually applied in infant formulas in combination with either GOS or FOS (Logtenberg Citation2020).
Gut-microbiota-independent effects of different structures of hMOs, pectins, GOS and ITFs
Direct effects on the gut barrier and their immunomodulatory effects
HMOs and NDCs can directly protect the host by several mechanisms such as by strengthening the mucus layer or by enhancing gut-immune barrier integrity. This modulation may be different with hMOs and NDCs with different structures (Rastall et al. Citation2022). In addition, different structures of hMOs or NDCs have different degrees of affinity for receptors expressed on the surface of immune cells, which in turn might lead to different immune responses (Rastall et al. Citation2022).
HMOs
HMOs can directly contribute to enforce intestinal epithelial barrier function by promoting the synthesis of intestinal mucus and by supporting the development of a well-connected gut epithelium (Zuurveld et al. Citation2020). HMOs stimulate the protein expression of molecules related to mucus function to enhance the integrity of the mucus layer (Zuurveld et al. Citation2020). The expression of MUC2, the major protein in mucus was improved after goblet cells were exposed to hMOs extracted from human breastmilk in vitro (Wu et al. Citation2018). Some individual, single hMO preparations can strengthen mucus barrier function by directly regulating the mucus-secreting goblet cells under different conditions, but the magnitude of the effects is structure‐dependent. This was illustrated in a study with LS174T goblet cells that were exposed to two individual hMOs, 2′-FL and 3-FL, and the hMO’s acid hydrolysis product LNT2. Under steady-state and inflammatory conditions, 3-FL and LNT2 showed upregulating effects on Muc2 and Tff3 genes. TFF3 protein is responsible for mucosa protection and mucus healing. Under allergic condition, 2′-FL, 3-FL, and LNT2 all significantly enhanced the expression of Muc2. (Cheng et al. Citation2020)
In addition to stimulating mucus secretion, hMOs can facilitate epithelial barrier maturation and prevent the gut barrier from dysfunctioning (Holscher, Bode, and Tappenden Citation2017; Varasteh et al. Citation2019; Wu et al. Citation2018). An in vitro study proved that LNnT enhanced the transepithelial electrical resistance (TEER) of Caco‐2Bbe cells (Holscher, Davis, and Tappenden Citation2014). This protective effect was also found in vivo work. HMOs derived from human breast milk that not only supported intestinal barrier function in vivo in mice but also rescued barrier disruption caused by enteric pathogens in vitro (Wu et al. Citation2018). Similarly, the hMO 3′-galactosyl-lactose (3′-GL) prevented deoxynivalenol (DON)-induced disruption of the intestinal barrier in intestinal epithelial monolayers in vitro (Varasteh et al. Citation2019). This protective effect, however, was hMO-structure dependent. Galactosyllactose with a 1-3 glycosidic linkage effectively mitigated gut barrier integrity loss, whereas galactosyllactose without a 1-3 glycosidic linkage did not (Varasteh et al. Citation2019). Moreover, the hMOs facilitate the development of the epithelial glycocalyx in a structure-dependent manner. The glycocalyx is important for microbial colonization in the gut. 3-FL enhanced albumin uptake and the production of heparan sulfate (HS) and hyaluronic acid (HA) in the glycocalyx of Caco-2 cells to a greater extent than 2′-FL (Kong et al. Citation2019).
HMOs have immunomodulatory effects and specific structures of hMOs can bind to receptors expressed on innate as well as on adaptive immune cells and on epithelial cells (Zuurveld et al. Citation2020). The affinity of receptors for hMOs is influenced by hMOs structures. HMOs interact with the glycan receptors, also known as lectin receptors involving C-type lectin receptor DC-SIGN, galectin receptor, and Siglecs receptor (Zuurveld et al. Citation2020). The neutral (fucosylated) hMOs, can interact with the DC-SIGN receptors on macrophages and DCs to prevent allergic reactions (Huang, Liao, and Yu Citation2018; Noll et al. Citation2016). Galectin receptors expressed by immune cells have been associated with the binding of neutral N-containing hMOs (Rapoport, Kurmyshkina, and Bovin Citation2008; Zuurveld et al. Citation2020). This binding can inhibit inflammatory cytokines release (Rousseaux et al. Citation2021). Siglecs receptors on DCs and neutrophils show an affinity for acid (sialylated) hMOs (O’Reilly and Paulson Citation2009; Triantis, Bode, and Van Neerven Citation2018). The activation of this process also attenuate inflammation (O’Reilly and Paulson Citation2009).
Pectins
Pectins directly strengthen the mucus layer and protect the integrity of epithelium to enhance gut barrier function in a structure-dependent manner. Low DM and high DM pectins affect mucin secretion by different mechanisms. The negative charge of the non-esterified GalA residues of low DM pectin cannot react with the negative charge of mucins, so it passes through the mucus layer and directly stimulates the goblet cells to synthesize mucus. In contrast, high DM pectins can form hydrogen bonds to interact with mucin to form gels that enhance the barrier function of the mucus layer (Beukema, Faas, et al. Citation2020). Furthermore, pectins with different structures influence muco-adhesive properties. The pectin structures with a high degree of methyl-esterification, branching, or non-linear backbone are considered to have low muco-adhesive properties (Rastall et al. Citation2022). The protective effect on the intestinal barrier is however very DM dependent. Lemon pectins with three distinct DM (30, 56, and 74) were compared to investigate their differences in gut barrier protection. It was shown that DM30 and DM74 pectins had a significant protective impact on the intestinal barrier compared to that of DM56 pectin (Vogt et al. Citation2016).
Pectins directly influence immune cell responses through interacting with pattern recognition receptors (PRRs) expressed on epithelial cells and mucosal immune cells (Blanco-Pérez et al. Citation2021). Toll-like receptors (TLRs) as the best-characterized PRRs in the gut and have been shown to be influenced by many dietary fibers including by pectins (Sahasrabudhe et al. Citation2018; Vogt et al. Citation2013). Several studies demonstrate that pectins with different DM or DB can inhibit the proinflammatory TLR-2/TLR-1 pathway resulting in the attenuation of inflammatory events (Beukema, Jermendi, et al. Citation2020; Beukema et al. Citation2021; Sahasrabudhe et al. Citation2018). The pectins with lower DM suppressed TLR-2 and particularly inhibited the proinflammatory TLR-2/TLR-1 pathway, leaving the tolerogenic TLR-2/TLR-6 pathway unchanged (Sahasrabudhe et al. Citation2018). The effect was most pronounced with pectins with a DM lower than 22 (Sahasrabudhe et al. Citation2018). Also, it was shown that the addition of calcium during incubation decreased TLR-2 inhibition. Calcium reduced the inhibition of TLR-2 by low DM8 and intermediate DM52 pectins, but calcium showed a lower effect on TLR-2 inhibition induced by high DM69 pectins. Furthermore, DM18 and DM52 substantially inhibited and bound to TLR-2 without the presence of calcium (Beukema, Jermendi, et al. Citation2020). DB levels of pectins are also important for the suppression of the TLR2-1 pathway. Low DM and intermediated DM pectins with high DB inhibit the TLR-2/TLR-1 pathway stronger and enhanced the release of anti-inflammatory cytokine IL-6 in human macrophages (Beukema et al. Citation2021).
GOS
GOS can strengthen gut barrier function by directly inducing the production of mucus and by modulating mucus associated genes in goblet cells (CitationFigueroa-Lozano et al. 2020). A recent study revealed that oligosaccharide content and glycosidic linkages of GOS influence mucus related gene expression in goblet cells. Lac-containing β-(1-4) GOS upregulated the expression of Muc2, Tff3, and Relmβ in goblet cells, whereas Lac-free β-(1-4) GOS did not affect the expression of these genes. Additionally, it was shown that a novel Lac-derived oligosaccharide mixture containing α-linkages significantly promoted the expression of Muc2, Tff3, and Relmβ compared to β-(1-3/4) GOS or β-(1-4) GOS (CitationFigueroa-Lozano et al. 2020).
GOS with specific structures also protect against intestinal barrier destruction and regulate the immune response (Akbari et al. Citation2017; Wang et al. Citation2021). Akbari et al. (Citation2017) compared the direct effects of different structures of GOS on barrier function of intestinal Caco-2 cells in vitro. They chose Vivinal® GOS (VGOS) and purified Vivinal® GOS (PGOS) which both are oligosaccharide mixtures with a DP of mainly 2-6. PGOS purified from VGOS had a lower content of glucose, galactose, lactose, and GOS-DP2 than VGOS. The results showed that VGOS was more effective than PGOS in improving the impaired integrity of the Caco-2 cells monolayer and in inhibiting the release of the inflammatory marker CXCL8. However, this effect was not attributed to the oligosaccharides in VGOS but to GOS-DP2. Subsequently they isolated GOS fractions of different DPs from VGOS and found that DP2 and DP3 fractions prevented disruptor-induced barrier impairment more effectively than DP-fraction equal to or larger than 4. Another study illustrating the structure dependent effects was an in vivo study in mice that demonstrated that the supplementation of GOS mainly containing DP3 and DP4 fractions attenuated gut barrier damage and inflammatory responses caused by lipopolysaccharide (LPS). The expression of gut TJ proteins like ZO-1, Occludin, and Claudin-1 increased, by the DP3 and DP4 fraction as well as the expression of pro-inflammatory cytokines including IL-1β, IL-6, IFN-γ, and TNF-α (Wang et al. Citation2021).
ITFs
A study performed in a mouse model demonstrated that long-chain ITFs (DP = 10-60) strengthen gut barrier function through enhancing the expression of TJ proteins including Occludin and Claudin-2 and the production of AMP whereas short-chain ITFs (DP = 2-25) did not have such effects (Chen et al. Citation2017). This was not corroborated by Vogt et al. (Citation2014) and Akbari et al. (Citation2017). Vogt et al. (Citation2014) investigated the impact of the chain length of ITFs on the intestinal barrier. Short-chain ITFs (DP < 10) and long-chain ITFs (DP > 10) were cultured with gut T84 epithelial cells before being stimulated with the barrier disrupting agent. TEER of T84 cells was measured to quantify the protective effects of ITFs with different DPs. The finding revealed that short-chain ITFs exhibited a protective effect on the integrity of gut epithelial cell monolayer, while long-chain ITFs did not. Akbari et al. (Citation2017) incubated FOS and inulin with Caco2 cells followed by stimulation with the fungal barrier disruptor deoxynivalenol (DON) and quantified intestinal barrier integrity via measuring TEER and intercellular lucifer yellow permeability. They found that ITFs with a lower DP (FOS) contributed more to protecting the barrier integrity than those with a higher DP (inulin).
ITFs exert different immunomodulatory effects according to their different chain lengths. To study this ITFs with different chain lengths were incubated with human peripheral mononuclear cells in vitro. TLR-2 on the immune cells was activated and induced cytokine-release. Short-chain FOS stimulated a more regulatory cytokine balance compared to long-chain inulin (Vogt et al. Citation2013). In a germ-free mouse model, both short-chain FOS and long-chain inulin enhanced T-helper cells in PPs, while only short-chain FOS activated regulatory T cells and a subclass of DCs in MLNs (Fransen et al. Citation2017).
Gut microbiota-dependent effects of different structures of hMOs, pectins, GOS and ITFs
HMOs and NDCs can serve as the substrate for microbiota fermentation resulting in changes in microbiota composition and beneficial microbial metabolites (Rastall et al. Citation2022). During fermentation of NDCs, some metabolic end-products (e.g., SCFAs) are formed which have immunomodulatory or barrier modifying functions (Rastall et al. Citation2022). Also, several recent studies have shown that the intake of NDCs affects bacterial tryptophan (Trp) metabolism, thereby increasing the circulating levels of indole derivatives (Kundi et al. Citation2021; Qi et al. Citation2022; Tuomainen et al. Citation2018). Indole derivatives have been proven to be essential for maintaining intestinal homeostasis (Ye et al. Citation2022). Therefore, in this part of this manuscript, the influences of hMOs and NDCs on gut microbiota composition, gut barrier function, and the immune system are reviewed.
Modulation of microbiota communities
A balanced composition of the gut microbiota is essential for maintaining intestinal health. This composition is primarily determined by the composition of the microbiota that colonize the intestine immediately after birth but can also be partially regulated by certain compounds in the diet (Roberfroid Citation2004), or by hMOs, pectins, GOS and ITFs. These molecules have during the past decade been shown to be instrumental in the final composition of the microbiota in early life (Akkerman, Faas, and de Vos Citation2019; Kong et al. Citation2020).
HMOs
HMOs are resistant to degradation by human enzymes in the proximal intestine and can be utilized by the microbiota in the distal intestine (Al-Khafaji et al. Citation2020). HMOs are metabolized differently by different bacterial species and strains (Al-Khafaji et al. Citation2020). Neutral (fucosylated) hMOs including 2′-FL, 3-FL, and lactodifucopentaose stimulate mostly Bifidobacteria and Bacteroides growth. Also, 2′-FL and 3-FL show a mild promoting effect on the growth of Lactobacillus delbrueckii, Enterococcus faecalis, and Streptococcus thermophilus (Yu, Chen, and Newburg Citation2013). Besides, Bifidobacterium breve is only abundant in presence of neutral N-containing HMOs, like laco-N-tetraose (LoCascio et al. Citation2007). Another lacto-N-neotetraose (LNnT) acid hydrolysis product, lacto-N-triaose II facilitates growth of Collinsella and Bifidobacterium (Kong et al. Citation2021). The acid (sialylated) hMOs including 3′-sialyllactose (3′-SL) and 6′-SL moderately support growth of Bifidobacterium longum, Bacteroides vulgatus, and Bacteroides thetaiotaomicron (Yu, Chen, and Newburg Citation2013). Probably other hMOs support gut bacteria as well but this has not been studied in much detail up to now.
Pectins
Pectins are fermented in the colon by several bacterial genera and support their growth (Blanco-Pérez et al. Citation2021). The regulation of the intestinal microbiota composition varies with different types of pectins. Several studies have shown that pectins with distinct DM levels or with variations in RG-I structures can lead to different gut microbial communities (Beukema, Faas, et al. Citation2020; Blanco-Pérez et al. Citation2021; Rastall et al. Citation2022). Low DM pectins increased the abundance of Bifidobacteria and Bacteroides while high DM pectins induced the growth of Prevotella and Ruminococcus (Beukema, Faas, et al. Citation2020; Blanco-Pérez et al. Citation2021). The in vitro fermentation of RG-I-rich structures of pectins increased the levels of Bifidobacterium and Lactobacillus (Rastall et al. Citation2022). Some studies also demonstrate the relationship between the structural properties of pectins and microbial abundances (Larsen et al. Citation2019; Walters, Xu, and Knight Citation2014). Pectins with a higher proportion of monosaccharides, a lower GalA fraction, and a lower DM increased the growth of Firmicutes and Bacteroidetes (Larsen et al. Citation2019). In addition, there was a positive correlation between the abundances of Faecalibacterium prausnitzii and Ruminococcaceae and the GalA content and DM levels of pectins (Walters, Xu, and Knight Citation2014).
GOS
Structurally different GOS-structures or mixtures can induce varying gut microbiota enrichment depending on the GOS composition applied. GOS with relatively higher DP (DP = 3 or 4) induce Bifidobacterium abundance, while Lactobacillus preferentially utilize GOS with lower DP (DP = 2) (Böger et al. Citation2019; Gopal, Sullivan, and Smart Citation2001). When compared to GOS with β-(1-4) linkages, GOS with β-(1-6) linkages showed a comparatively higher prebiotic index (PI) value (Li et al. Citation2015). PI represents the relationship between beneficial and undesirable microbiota based on the change in the total number of bacteria. Higher PI values indicate the growth of more advantageous microbiota and relative lower amounts of unfavorable microbiota (Li et al. Citation2015). Additionally, α-GOS containing α-(1-6) linkages (DP = 3 and 4) and β-GOS containing β glycosidic linkages (DP = 3-6) both stimulated the enrichment of Bifidobacterium. β-GOS significantly decreased the Enterobacteria abundance while α-GOS did not (Marín-Manzano et al. Citation2020). In the case of disturbed intestinal flora, different DP components of GOS can also promote the enrichment of different microbiota. DP4-6 fractions of GOS were found to stimulate recovery of Bifidobacteria and butyrate-producing bacteria after amoxicillin treatment of the host, while DP2 and DP3 of GOS did not have such an effect (Ladirat et al. Citation2014).
ITFs
ITFs are composed of linear polymers of monosaccharides and have variations in DP (Yeung et al. Citation2021). The degree of DP of ITF determines the composition of the intestinal flora when administered in food or feed (Li et al. Citation2020; Paßlack et al. Citation2012; Zhu et al. Citation2017). Higher polymerization degrees (DP ≥ 10) enhance gut microbiota diversity to a higher extent than lower degrees of polymerization (e.g. FOS) (Asto et al. Citation2019). In a study comparing the impact of inulin with different DPs in mice, short-chain inulins (DP = 4-5) favorably induced the growth of Bifidobacterium, Faecalibaculum, Oscillibacter, and other bacterial genera (Li et al. Citation2020). However, long-chain inulin (DP= 23-25) had some different effects and stimulated the growth of bacterial species capable of degradation of complex polysaccharides such as Bacteroides, Parasutterella, and Erysipelatoclostridium (Li et al. Citation2020). In another study, mice were fed with FOS (DP = 2-9, DPaverage = 4) and inulin (DP = 2-60, DPaverage = 10) for 6 weeks (5 g/kg/day). In this study the FOS group showed a higher abundance of Lactobacillaceae, Bifidobacteriaceae and Akkermansia muciniphila than the longer DP inulin group (Zhu et al. Citation2017). Another in vivo study in piglets illustrated that inulin with an average DP of 57 induced higher bacterial abundance than inulin with an average DP of 31. This included a higher enrichment of Enterococcus, Bifidobacterium, and Lactobacillus mucosae in the ileum (Paßlack et al. Citation2012). Furthermore, IFT with a wider DP distribution had a higher impact on beneficial microbiota growth. Native chicory inulin (DP = 2-60) and synthetic inulin (DP = 5-30) were fermented by swine fecal cultures in vitro. Compared to synthetic inulin, native chicory inulin promoted more Bifidobacterium (B. catenulatum, B. dentium) and Lactobacillus (L. reuteri) growth (Nakayama et al. Citation2020).
The production of SCFAs
HMOs and NDCs are fermented by gut microbiota to form a variety of microbial metabolites, among which SCFAs, such as acetate, propionate, and butyrate (Cummings et al. Citation1987). Acetate can be synthesized by many different genera, but mainly by Bifidobacteria and Lactobacilli. Propionate is mainly formed by Bacteroidetes and Firmicutes. Butyrate is reported to be produced by some Clostridia, Faecalibacterium prausnitzii, Roseburia intestinalis, and Eubacterium rectale (Blanco-Pérez et al. Citation2021). Microbial fermentation of structurally different hMOs and NDCs may influence the profiles of SCFAs production in the digestive tract.
HMOs
Kong et al. (Citation2021) fermented 3-FL and LNT2 in vitro using infant fecal microbiota and found that 3-FL exhibited slower fermentation and was less utilized compared to LNT2. Besides, 3-FL induced acetic acid production and LNT2 stimulated acetic and butyric acid formation (Kong et al. Citation2021). The hMO 2′-FL was also slowly fermented and enhanced acetate formation, but its fermentability could be improved when it was fermented with readily fermentable molecules such as GOS and native inulin (Akkerman et al. Citation2021; Kong et al. Citation2021).
Pectins
Pectins with different structural characteristics generate different SCFAs profiles. Also, quantitatively there are differences depending on the type of pectin consumed. E.g. homogalacturonan-type pectins with a lower molecule weight induced a higher total amount of SCFAs production (Zhao et al. Citation2021). Pectins with higher fractions of rhamnose and fucose induces more propionate formation (Blanco-Pérez et al. Citation2021). In vitro fermentation of RG-I-type pectins enhanced production of propionate and butyrate (Larsen et al. Citation2019). Low DM pectins promoted the production of acetate and butyrate, while high DM pectin enhanced the synthesis of acetate and propionate (Huang et al. Citation2022; Larsen et al. Citation2019).
GOS
There are structure-based differences in the microbial fermentation and production of metabolites from GOS. The lower DP fractions (DP = 2 and 3) were preferentially degraded by adult microbiota as well as by infant intestinal flora compared to the higher DP fractions (DP = 4-6) in GOS (Akkerman et al. Citation2022; Ladirat Citation2014). Fermentation of GOS together with 2′-FL by infant microbiota accelerated the fermentation of GOS compared to the fermentation of GOS alone, but the fermentation rate was not DP-dependent (Akkerman et al. Citation2022). GOS-DP2 containing β-(1-4) and β-(1-6) linkages were the most easily fermented while β-(1-1) linkages were more resistant to fermentation. However, in the DP3 fraction of GOS, the presence of a β-(1-1) linkage resulted in faster fermentation of adjacent β-(1-4) linkages (Ladirat et al. Citation2014). Acetate was the major SCFA produced during microbial fermentation of β-GOS as well as of α-GOS (Marín-Manzano et al. Citation2020). A higher DP component in GOS, with DP greater than 3, encouraged the production of butyrate by either healthy microbiota or amoxicillin-treated microbiota (Ladirat et al. Citation2014).
ITFs
ITFs with linear structures are somewhat simpler to ferment for the gut microbiota than more complex molecules such as the aforementioned pectins (Yeung et al. Citation2021). However, the rate of fermentation and the location where fermentation occurs in the hindgut vary with the DP levels of the ITF. In general, ITF with a lower DP (DP = 3-10) is readily metabolized in the proximal colon, while ITF with a higher DP (DP > 20) resists fermentation and is fermented gradually along the distal colon (Vogt et al. Citation2015). The rate of fermentation may result in differences in SCFA formation between different ITF types (Logtenberg et al. Citation2020; Macfarlane and Macfarlane Citation2003). Higher acetate formation was observed with native inulin (DP = 16) after fermentation in vitro by infant fecal microbiota than with fermentation of FOS (DP = 3-8) (Logtenberg et al. Citation2020).
The effect of SCFAs on the gut barrier and their immunomodulatory effects
SCFAs, including acetate, propionate, and butyrate exert health benefits for the gut (Cummings et al. Citation1987). Butyrate, as an energy substrate, is mostly utilized by the gut epithelial cells (Hamer et al. Citation2008). Instead, acetate and propionate can pass through the epithelial barrier and be absorbed into the circulation (Rastall et al. Citation2022; Zuurveld et al. Citation2020). The synthesis of SCFAs reduces the luminal PH of the gut thus favoring or inhibiting colonization of different taxa of microbiota, which contributes to gut health (Tramontano et al. Citation2018). SCFAs may also guide the gut barrier and immune response (Blanco-Pérez et al. Citation2021). This can be done in several ways. SCFAs have been shown to increase mucus secretion and thereby improve gut barrier function (Burger-van Paassen et al. Citation2009; Zuurveld et al. Citation2020). Acetate may facilitate the differentiation of goblet cells (Zuurveld et al. Citation2020). Propionate and butyrate have been shown to induce and enhance the expression of MUC2 (Burger-van Paassen et al. Citation2009). Another mechanism by which SCFAs regulate intestinal barrier function is by stimulating epithelial cells to strengthen TJs and reduce intestinal permeability (Feng et al. Citation2018; Suzuki, Yoshida, and Hara Citation2008). SCFAs or individual SCFAs increase the TEER and lower Lucifer yellow paracellular transport of intestinal epithelium (Suzuki, Yoshida, and Hara Citation2008). Butyrate has been shown to upregulate the expression of Occludin, Claudin-3, and ZO-1 proteins in gut epithelial cells in vivo and in vitro (Feng et al. Citation2018).
SCFAs not only directly stimulate the intestinal epithelial cell to grow but also stimulate their production of antimicrobial peptides, and they promote the proliferation of innate lymphoid cells (ILC3) to release IL22 (Wiertsema et al. Citation2021). IL22 indirectly promotes epithelial cell production of antibacterial compounds (Wiertsema et al. Citation2021). SCFAs also attenuate too strong activation of APCs such as DCs and macrophages and are important in support of the development of Treg cells (Beukema, Faas, et al. Citation2020; Blanco-Pérez et al. Citation2021; Wiertsema et al. Citation2021). These SCFAs’ immunomodulatory effects and promotion of intestinal homeostasis occur predominantly through two different signaling pathways in the hosts (Rastall et al. Citation2022). SCFAs activate G protein-coupled receptors (GPCRs) on intestinal epithelial cells and immune cells, such as GPCR41, GPCR43, and GPCR109a, to exert entero-protective effects (Cai et al. Citation2020; Zuurveld et al. Citation2020). Several studies show that SCFAs can protect against inflammation by interaction with GPCR41and GPCR43 (Maslowski et al. Citation2009; Masui et al. Citation2013; Trompette et al. Citation2014). Propionate reduce Th2 effector function in a GPCR41-dependent manner (Trompette et al. Citation2014), and SCFAs stimulate Treg cell differentiation in a GPR43-dependent manner in mice (Smith et al. Citation2013). However, GPCR109a is only having affinity for butyrate (Brosseau et al. Citation2019). By that butyrate can induce GPCR109a signaling pathways and trigger anti-inflammatory effects in macrophages and DCs in the colon, along with the stimulation of Treg and IL-10-producing T cell differentiation (Singh et al. Citation2014). Knockdown of GPCR109a in Caco-2 cells inhibited butyrate-induced expression of Claudin-3 and therewith impacted barrier function (Feng et al. Citation2018). Another mechanism by which SCFA can support gut-immune barrier function is by suppressing the activity of histone deacetylases (HDACs) to inhibit the production of pro-inflammatory cytokines in intestinal macrophages and to induce the lgA production by B cells. This is especially done by butyrate and to a lesser extent by proprionate which regulate by this mechanism intestinal immunity and intestinal homeostasis (Cai et al. Citation2020; Sun et al. Citation2017).
The effect of indole derivatives on the gut barrier and their immunomodulatory effects
SCFAs have gained much attention of the scientific community in the past decade but cannot explain all the beneficial effects of food components on the GI immune barrier (Gasaly, de Vos, and Hermoso Citation2021). The dietary essential amino acid Trp is the main precursor of indole production by gut microbiota (Scott, Fu, and Chang Citation2020; Ye et al. Citation2022). The majority of the Trp is absorbed in the small intestine, and approximately 5% of the Trp is metabolized into indole by the gut microbiota in the colon (Ye et al. Citation2022). Bacteroides, Clostridium, and Escherichia coli can convert Trp into indole by tryptophanase (Roager and Licht Citation2018). Trp can also be metabolized into some indole-related compounds by gut microbiota such as indole-3-pyruvate (IPyA), indole 3-propionic acid (IPA), indole-3-acrylate (IA), indole-3-aldehyde (I3A), indoleacetic acid (IAA), indole-3-ethanol (IE) and skatole (Su, Gao, et al. Citation2022; Tennoune, Andriamihaja, and Blachier Citation2022).
Indole and indole-related compounds regulate the gut barrier mainly through two signaling pathways. The first pathway is by activating aromatic hydrocarbon receptors (AhR) in epithelial cells and immune cells which has a direct positive impact on the intestinal barrier function and mucosal immune responses (Scott, Fu, and Chang Citation2020; Ye et al. Citation2022). IPyA, I3A, and IE signal via AhR and have been shown to preserve the integrity of the apical junction complexes and its related actin regulatory proteins (Scott, Fu, and Chang Citation2020). Additionally, indole and indole derivatives induce IL-10 and IL-22 production which have a regulatory effect on gut immunity (Alexeev et al. Citation2018; Powell et al. Citation2020; Zelante et al. Citation2013). These actions are all induced through the activation of AhR (Ye et al. Citation2022). IAA also acts as an AhR ligand to promote the expression of the antimicrobial lectins RegIIIγ and exert anti-inflammatory effects (Shi et al. Citation2020). The second pathway by interaction of indols with pregnancy-X receptors (PXR) expressed in gut tissues to control mucosal integrity and maintain intestinal homeostasis (Ye et al. Citation2022). IPA activates PXR resulting in the down-regulation of enterocyte-derived TNF-α and up-regulation of connexin-coding mRNA (Venkatesh et al. Citation2014). IAA induces IL-35+ B cells to generate the anti-inflammatory cytokine IL-35 through stimulating PXR (Su, Zhang, et al. Citation2022).
IPA was shown to strengthen the intestinal barrier in a Caco-2/HT29 cell culture model (Li et al. Citation2021). It enhanced the mucus barrier by inducing MUC2, MUC4, TFF3, and RELMβ. In addition, the TEER of the co-culture cells monolayer increased and induced the expression of TJ proteins Claudin-1, Occludin, and ZO-1 (Li et al. Citation2021). IPA and IA promote the release of IL-10, which plays an essential role in maintaining mucus secreted by goblet cells (Alexeev et al. Citation2018; Wlodarska et al. Citation2017).
Current insight in how hMOs, pectins, GOS and ITFs impact the gut-immune barrier
To date, several studies have explored how fermentation product such as SFCA produced from hMOs, pectins, GOS and ITFs influence the gut-immune barrier. However, especially in recent years more and more insight has been generated that confirm that not only direct effects on immune cells of hMOs and NDCs are responsible for improving the gut-immune barrier but that also fermentation products have beneficial effects. Also, a few studies suggest that the fermentation of NDCs may also impact the generation of indole derivatives that are beneficial to the intestinal barrier (Akkerman et al. Citation2022).
Human milk oligosaccharides
Šuligoj et al. (Citation2020) illustrate that the microbial fermentation products of 2′-FL alone or in a mixture of 2′-FL and LNnT significantly reduced the permeability of Caco-2 cell monolayers, and simultaneously increased the expression of Claudin-8. In addition, microbial metabolites produced by 2′-FL promoted production of Claudin-5 in human organoids from proximal, transverse, and distal colon biopsies (Šuligoj et al. Citation2020). Recently, it was demonstrated that fermentation of a mixture of hMOs can prevent gut barrier disruption. An in vitro model was designed to evaluate the effects of fermentation products of 2′FL, 2′FL + LNnT, and a mixture of six hMOs (HMO6: composed of 2′FL, LNnT, diucosyllactose, lacto-N-tetraose, 3′-SL and 6′-SL) on barrier function of gut epithelial cells. The products from fermented HMO6 significantly increased the TEER of gut epithelium. After simulating inflammatory conditions, fermented 2′FL + LNnT, and HMO6 prevented a decrease in TEER, and the fermentation products of the groups combintly significantly reduced intestinal permeability. This illustrated that combining hMO mixture may work synergistically and better protect the intestinal barrier from proinflammatory imbalances than single molecules alone. (Natividad et al. Citation2022)
The fermentation products of hMOs can also have beneficial effects by supporting the adhesion of commensal microbiota to gut epithelial cells. This, however, depends on the hMOs’ structures. The fermentation products of LNT2 significantly enhanced the adhesion of L.plantarum WCFS1 to Caco-2 cells, whereas the fermentation products of 3-FL did not exert this effect (Kong et al. Citation2021). These studies illustrate that health effects of hMOs might be very specific for individual types of hMOs.
Pectins
Fermentation of pectins may contribute to gut barrier integrity as well as to anti-inflammatory effects. Bacterial metabolites produced from carrot-derived RG-I pectins increased the TEER of a Caco-2/peripheral blood mononuclear cells (PBMC) co-cultured monolayer. Furthermore, fermented RG-I suppressed the release of the pro-inflammatory cytokines including IL-9, IL-4, and IL-17a as well as enhanced the production of the anti-inflammatory cytokines IL-10 (Van den Abbeele et al. Citation2020). Microbial metabolites produced from pectins with different levels of DM and DB activate AhR to varying degrees which impact immunomodulatory effects of pectins. Fecal samples from mice supplemented with DM19 (high DB) pectin for one week showed the strongest activation of AhR, followed by DM49 (low DB) pectin (Beukema et al. Citation2022). Metabolites from DM43 (high DB) pectin also induced activation of AhR after four weeks of pectin supplementation in mice, but this effect was not as strong as for DM19 (high DB) and DM49 (low DB) pectins. This had a remarkable effect as supplementation with these three pectins increased the production of Rorγt+ Tregs in MLNs (Beukema et al. Citation2022). Rorγt+ Tregs can suppress the immune responses of effector T cells and therewith avoid intestinal inflammation (Yang et al. Citation2016). However, SCFAs in metabolites were not enhanced by structural-diverse pectins supplementation illustruing that effects were more indole than SCFA dependent. An increase in the abundance of Lachnospiraceae associated with the production of indole derivatives was found (Amaretti et al. Citation2019). It was therefore suggested that that microbial-produced indole derivatives that activate AhRs may be responsible for enhanced Rorγt+ Treg levels (Beukema et al. Citation2022).
Galacto-oligosaccharides
There is some evidence that the fermentation of GOS affects the intestinal barrier and immune cell response (Akkerman et al. Citation2022; Gao et al. Citation2021). In a porcine study in vivo, lipopolysaccharide (LPS) injection resulted in decreased TJ protein expression of Claudin-1 and ZO-1 in the colonic mucosa. GOS feeding recovered the TJs expression resulting in the upregulation of Claudin-1 and ZO-1(Gao et al. Citation2021). In another study it was shown that GOS and 2 ‘-FL, either fermented separately or combined, attenuated cytokine responses of DCs in an AhR-receptor-dependent manner. This may be attributed to AhR-receptor agonists, such as indole derivatives, formed during NDCs fermentation. In this study DCs were stimulated with fermentation digesta of GOS, 2′-FL, or a mixture of GOS/2′-FL. After the addition of AhR-receptor blockers, the fermentation digesta of all groups induced higher levels of cytokine secretion in DCs compared to normal conditions. This indicated that GOS fermentation produced ligands that activated and bind to AhR, which could attenuate immune activation of DCs. (Akkerman et al. Citation2022).
Inulin-type fructans
Some studies suggest that the fermentation of ITFs promotes intestinal barrier function (Logtenberg et al. Citation2020; Pham et al. Citation2018; Uerlings et al. Citation2020). Caco-2/HT29-MTX intestinal epithelial cells were stimulated by fermentation digesta of dried chicory root containing 75% inulin or 90% inulin, and a significant increase in TEER was found compared with cells exposed to unfermented inulins. When a barrier disrupting stressor was added to the apical part of the gut epithelial layer, the fermentation of dried chicory roots containing 75% inulin significantly improved intestinal barrier integrity (Pham et al. Citation2018). Fermentation digesta of inulin was also shown to induce expression of TJ proteins (Claudin-1, −3, ZO-1) and AJ protein (CDH1) as well as the Muc1 gene in pig intestinal epithelial cells (IPEC-J2) (Uerlings et al. Citation2020). Moreover, fermented ITFs with higher DP showed stronger anti-inflammatory effects than fermented ITFs with lower DP. Fermented FOS and native inulin all decreased pro-inflammatory cytokine generation in DCs, while fermented native inulin had an even more pronounced attenuating effect (Logtenberg et al. Citation2020) ().
Figure 3. Different structures of individual hMOs and commonly applied NDCs in infant formulas regulate the intestinal immune barrier in a microbiota-independent and microbiota-dependent manner. According to the microbiota-independent effects, they directly 1. support the gut integrity by enhancing tight junctions (TJs); 2. strengthen the mucus layer by stimulating the goblet cells to release mucins; 3. modulate the immune response by interacting with receptors expressed on epithelial cells or immune cells such as Toll-like receptors (TLRs), DC-SIGN receptors, galectin receptors, and Siglecs receptors. These complex carbohydrates can also regulate the intestinal immune barrier in a microbiota-dependent way. 4. They directly modulate the gut microbiota composition. 5. They are fermented by gut microbiota resulting in the production of short-chain fatty acids (SCFAs). 5a. SCFAs exert immunomodulatory effects by interacting with G protein-coupled receptors (GPCRs) or inhibiting histone deacetylases (HDACs). 5b. The intake of hMOs or NDCs may influence the production of indole derivatives. 5c. Indole derivatives also have immunomodulatory functions by interacting with aromatic hydrocarbon receptors (AhR) or pregnancy-X-receptors (PXR). 6. These metabolites such as SCFAs and indoles can improve the gut barrier by upregulating TJs (6a) and enhance the mucus layer by increasing mucins secretion (6b).
Clinical trials on the supplementation of infant formula with synthetic oligosaccharides
The combination of 90% short-chain GOS (scGOS) and 10% long-chain FOS (lcFOS) monomers is commonly applied in infant formula in Europe since 2000 (Veereman Citation2007). When 4.5 g of the inulin/GOS mixture was supplemented daily to infants between the ages of 4-6 months for 6 weeks, the number of Bifidus in the fecal flora increased (Scholtens et al. Citation2006). Infants who received the inulin/GOS mixture for a full year experienced a marked decrease in the episodes of GI and respiratory infection occurrences (Bruzzese et al. Citation2006). Besides, the European Food Safety Authority (EFSA) and US Food and Drug Administration (FDA) permit several synthetic hMOs (2′-FL, LNnT, LNT, 2′-FL + difucosyllactose, 3′-SL and 6′-SL) for infant formula (Bührer et al. Citation2022). However, there are only a few clinical studies that did test these hMOs. A clinical trial show that infants fed with a formula containing 2′-FL during the first 4 months of life compared with breastfed infants showed no significant difference in growth performance which included head circumference, height, or weight (Marriage et al. Citation2015). Infants who received formula supplemented with 2′-FL had lower inflammatory cytokine levels and the levels were similar to that of infants who were breastfed (Goehring et al. Citation2016). Another study shows that infants fed formula supplemented with 2′-FL and LnNT had fewer respiratory infections in the first year of life compared to infants fed a formula without hMOs supplementations (Puccio et al. Citation2017). Pectin hydrolysates pAOS is an alternative source of hMOs acidic oligosaccharides for use in infant formula (Garthoff et al. Citation2010). A randomized, double-blind study found that healthy infants born at term and receiving infant formula with the supplementation of pAOS with or without scGOS + lcFOS for 6 weeks did not affect growth, crying, vomiting, and regurgitation patterns compared with the placebo group (Fanaro et al. Citation2005). Preterm infants receiving a combination of scGOS + lcFOS + pAOS decreased stool pH and viscosity with a tendency to increase stool frequency as well as reduced pro-inflammatory cytokine levels (Westerbeek et al. Citation2011). Also a decrease of endogenous infections were observed when adequate amounts of scGOS + lcFOS + pAOS were given to premature infants (Westerbeek et al. Citation2010). A clinical study showed that cotton-boll pectins added to the infant diet improved the nutritional status, physical development, and erythrocytic system of infants (Salomov et al. Citation1994).
Concluding remarks and future perspectives
The regulation of the intestinal barrier such as strengthening the mucus layer and gut epithelial barrier integrity has been shown to be very dependent on the structural features of hMO or NDCs. For instance, 3-FL was more effective in promoting gut epithelial glycocalyx development than 2′-FL (Kong et al. Citation2019). The protective effect of pectins on the intestinal barrier was highly dependent on the DM content in pectins (Vogt et al. Citation2016). Lactose-containing GOS was a stronger upgrader of expression of genes related to mucus layer integrity than lactose-free GOS (CitationFigueroa‐Lozano and de Vos 2019). Short-chain ITFs were more protective for intestinal barrier integrity than long-chain ITFs (Akbari et al. Citation2017; Vogt et al. Citation2014). These all have important implications for finding more suitable NDCs for application in infant formula to support barrier function development. Until now only a few molecules are added to infant formulas such as 2′-FL, pAOS, GOS, and FOS. Meanwhile, more and more promising NDCs with specific health benefits are proposed to be added such as pectins. Also, recent research has illustrated that many more tailored health benefits can be achieved by combining specific chemistries of these molecules. For example, under inflammatory conditions, 3-FL and LNT2 can strengthen the mucus layer by increasing the expression of goblet cell secretory-related genes. Under allergic conditions, 2′-FL, 3-FL and LNT2 all can increase the mucus-secreting related genes expression (Cheng et al. Citation2020). Also, it has been shown that immune responses such as stimulation or inhibition of different receptors on immune cells can be achieved by specific chemistries of hMOs and NDCs and that this results in different immune responses in vitro and in vivo. Fucosylated hMOs interact with DC-SIGN receptors on immune cells and can prevent allergic reactions (Huang, Liao, and Yu Citation2018; Noll et al. Citation2016). Neutral N-containing hMOs and salicylated hMOs bind to galectin receptors and Siglecs receptors on immune cells, respectively, and can inhibit the release of inflammatory cytokines (O’Reilly and Paulson Citation2009; Rapoport, Kurmyshkina, and Bovin Citation2008; Zuurveld et al. Citation2020). Pectins with low DM and high DB can inhibit the pro-inflammatory TLR-2/TLR-1 pathway, leading to an increase in anti-inflammatory cytokine release (Beukema et al. Citation2021). GOS mainly containing DP3 and DP4 fractions attenuate gut inflammatory responses (Wang et al. Citation2021). Short-chain ITFs have a stronger anti-inflammatory induction compared to long-chain ITFs (Vogt et al. Citation2013). These different effects of the molecules have possibly important implications for the development of tailored infant formula when they are combined. For example, prematures are born with a more proinflammatory phenotype and might have other needs than term-born infants (Sharma et al. Citation2012; Strunk et al. Citation2011). For allergy-prone infants, other needs and adapted infant formula may lead to better health (Pickett-Bernard Citation2006). Besides tailoring for specific target groups current insight is that we might adapt infant formula to meet the different requirements of infants during lactation. Mother milk usually adapts its composition according to the needs of the baby (Ballard and Morrow Citation2013). By generating more knowledge on the immunomodulating impact of different types of NDCs we might be able to better steer the development of infants and design age-matched infant formula.
Furthermore, our review hopefully leads to more and dedicated research on the metabolites made of hMOs and NDCs. SCFAs, one of the microbial metabolites of NDCs or hMOs by bacteria, can contribute directly to mucus production, and enhance epithelial integrity to facilitate the development of the intestinal barrier. They also exert an immune response through different receptor signaling mechanisms in the host. Besides, indoles, another fermentation metabolite that plays a beneficial role in the regulation of intestinal barrier function, have received increasing attention recently. The fermentation of individual hMOs, GOS, and pectin has been proven to activate the AhR-receptor of immune cells and exert an immunomodulatory effect. However, only a few studies have been conducted on the role of fermented hMOs or NDCs on gut epithelial barrier and the regulation of intestinal immunity (Natividad et al. Citation2022). The role of development and guidance of colonization of gut microbes are also vital for maintaining homeostasis in the gut (Zheng, Liwinski, and Elinav Citation2020). More research is recommended focusing on the fermentation kinetics of non-digestible carbohydrates and the effect of fermentation products on gut health. This ultimately will lead to the required insights and knowledge for designing better combinations of NDCs that support microbiota and immune barrier function in infants.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Akbari, P., J. Fink-Gremmels, R. H. A. M. Willems, E. Difilippo, H. A. Schols, M. H. C. Schoterman, J. Garssen, and S. Braber. 2017. Characterizing microbiota-independent effects of oligosaccharides on intestinal epithelial cells: insight into the role of structure and size. European Journal of Nutrition 56 (5):1919–30. doi: 10.1007/s00394-016-1234-9.
- Akkerman, R., M. J. Logtenberg, M. Beukema, B. J. de Haan, M. M. Faas, E. G. Zoetendal, H. A. Schols, and P. de Vos. 2022. Combining galacto-oligosaccharides and 2′-fucosyllactose alters their fermentation kinetics by infant fecal microbiota and influences AhR-receptor dependent cytokine responses in immature dendritic cells. Food & Function 13 (12):6510–21. doi: 10.1039/d2fo00550f.
- Akkerman, R., M. J. Logtenberg, M. Beukema, B. J. De Haan, M. M. Faas, E. G. Zoetendal, H. A. Schols, and P. de Vos. 2021. Chicory inulin enhances fermentation of 2′-fucosyllactose by infant fecal microbiota and differentially influences immature dendritic cell and T-cell cytokine responses under normal and Th2-polarizing conditions. Food & Function 12 (19):9018–29. doi: 10.1039/d1fo00893e.
- Akkerman, R., M. M. Faas, and P. de Vos. 2019. Non-digestible carbohydrates in infant formula as substitution for human milk oligosaccharide functions: Effects on microbiota and gut maturation. Critical Reviews in Food Science and Nutrition 59 (9):1486–97. doi: 10.1080/10408398.2017.1414030.
- Alexeev, E. E., J. M. Lanis, D. J. Kao, E. L. Campbell, C. J. Kelly, K. D. Battista, M. E. Gerich, B. R. Jenkins, S. T. Walk, D. J. Kominsky, et al. 2018. Microbiota-derived indole metabolites promote human and murine intestinal homeostasis through regulation of interleukin-10 receptor. The American Journal of Pathology 188 (5):1183–94. doi: 10.1016/j.ajpath.2018.01.011.
- Al-Khafaji, A. H., S. D. Jepsen, K. R. Christensen, and L. K. Vigsnæs. 2020. The potential of human milk oligosaccharides to impact the microbiota-gut-brain axis through modulation of the gut microbiota. Journal of Functional Foods 74:104176. doi: 10.1016/j.jff.2020.104176.
- Allam-Ndoul, B., S. Castonguay-Paradis, and A. Veilleux. 2020. Gut microbiota and intestinal trans-epithelial permeability. International Journal of Molecular Sciences 21 (17):6402. doi: 10.3390/ijms21176402.
- Allan Walker, W. 2013. Initial intestinal colonization in the human infant and immune homeostasis. Annals of Nutrition and Metabolism 63 (Suppl. 2):8–15. doi: 10.1159/000354907.
- Amaretti, A., C. Gozzoli, M. Simone, S. Raimondi, L. Righini, V. Pérez-Brocal, R. García-López, A. Moya, and M. Rossi. 2019. Profiling of protein degraders in cultures of human gut microbiota. Frontiers in Microbiology 10:2614. doi: 10.3389/fmicb.2019.02614.
- Ambrogi, V., F. Bottacini, L. Cao, B. Kuipers, M. Schoterman, and D. van Sinderen. 2023. Galacto-oligosaccharides as infant prebiotics: Production, application, bioactive activities and future perspectives. Critical Reviews in Food Science and Nutrition. Taylor & Francis 63 (6):753–66. doi: 10.1080/10408398.2021.1953437.
- Assimakopoulos, S. F., C. Triantos, I. Maroulis, and C. Gogos. 2018. The role of the gut barrier function in health and disease. Gastroenterology Research 11 (4):261–3. doi: 10.14740/gr1053w.
- Asto, E., I. Mendez, M. Rodriguez-Prado, J. Cune, J. Espadaler, and A. Farran-Codina. 2019. Effect of the degree of polymerization of fructans on ex vivo fermented human gut microbiome. Nutrients 11 (6):1293. doi: 10.3390/nu11061293.
- Atuma, C., V. Strugala, A. Allen, and L. Holm. 2001. The adherent gastrointestinal mucus gel layer: Thickness and physical state in vivo. American Journal of Physiology. Gastrointestinal and Liver Physiology 280 (5):G922–G929. doi: 10.1152/ajpgi.2001.280.5.g922.
- Ayabe, T., T. Ashida, Y. Kohgo, and T. Kono. 2004. The role of paneth cells and their antimicrobial peptides in innate host defense. Trends in Microbiology 12 (8):394–8. doi: 10.1016/j.tim.2004.06.007.
- Ayechu-Muruzabal, V., A. H. van Stigt, M. Mank, L. E. M. Willemsen, B. Stahl, J. Garssen, and B. Van’t Land. 2018. Diversity of human milk oligosaccharides and effects on early life immune development. Frontiers in Pediatrics 6:239. doi: 10.3389/fped.2018.00239.
- Ballard, O., and A. L. Morrow. 2013. Human milk composition: Nutrients and bioactive factors. Pediatric Clinics of North America 60 (1):49–74. doi: 10.1016/j.pcl.2012.10.002.
- Bansil, R., and B. S. Turner. 2018. The biology of mucus: Composition, synthesis and organization. Advanced Drug Delivery Reviews 124:3–15. doi: 10.1016/j.addr.2017.09.023.
- BeMiller, J. N. 2018. Carbohydrate chemistry for food scientists. Amsterdam, The Netherlands: Elsevier. doi: 10.1016/C2016-0-01960-5.
- Bermudez-Brito, M., C. Rösch, H. A. Schols, M. M. Faas, and P. de Vos. 2015. Resistant starches differentially stimulate toll-like receptors and attenuate proinflammatory cytokines in dendritic cells by modulation of intestinal epithelial cells. Molecular Nutrition & Food Research 59 (9):1814–26. doi: 10.1002/mnfr.201500148.
- Bermudez-Brito, M., N. M. Sahasrabudhe, C. Rösch, H. A. Schols, M. M. Faas, and P. de Vos. 2015. The impact of dietary fibers on dendritic cell responses in vitro is dependent on the differential effects of the fibers on intestinal epithelial cells. Molecular Nutrition & Food Research 59 (4):698–710. doi: 10.1002/mnfr.201400811.
- Beukema, M., É. Jermendi, H. A. Schols, and P. de Vos. 2020. The influence of calcium on pectin’s impact on TLR2 signalling. Food & Function 11 (9):7427–32. doi: 10.1039/d0fo01703e.
- Beukema, M., É. Jermendi, M. A. van den Berg, M. M. Faas, H. A. Schols, and P. de Vos. 2021. The impact of the level and distribution of methyl-esters of pectins on TLR2-1 dependent anti-inflammatory responses. Carbohydrate Polymers 251:117093. doi: 10.1016/j.carbpol.2020.117093.
- Beukema, M., É. Jermendi, M. M. P. Oerlemans, M. J. Logtenberg, R. Akkerman, R. An, M. A. van den Berg, E. G. Zoetendal, T. Koster, C. Kong, et al. 2022. The level and distribution of methyl-esters influence the impact of pectin on intestinal T cells, microbiota, and AHR activation. Carbohydrate Polymers 286:119280. doi: 10.1016/j.carbpol.2022.119280.
- Beukema, M., M. M. Faas, and P. de Vos. 2020. The effects of different dietary fiber pectin structures on the gastrointestinal immune barrier: impact via gut microbiota and direct effects on immune cells. Experimental & Molecular Medicine 52 (9):1364–76. doi: 10.1038/s12276-020-0449-2.
- Bischoff, S. C., G. Barbara, W. Buurman, T. Ockhuizen, J. D. Schulzke, M. Serino, H. Tilg, A. Watson, and J. M. Wells. 2014. Intestinal permeability–a new target for disease prevention and therapy. BMC Gastroenterology 14 (1):25. doi: 10.1186/s12876-014-0189-7.
- Blanco-Pérez, F., H. Steigerwald, S. Schülke, S. Vieths, M. Toda, and S. Scheurer. 2021. The dietary fiber pectin: Health benefits and potential for the treatment of allergies by modulation of gut microbiota. Current Allergy and Asthma Reports 21 (10):1–19. doi: 10.1007/s11882-021-01020-z.
- Bode, L. 2012. Human milk oligosaccharides: Every baby needs a sugar mama. Glycobiology 22 (9):1147–62. doi: 10.1093/glycob/cws074.
- Bode, L., and E. Jantscher-Krenn. 2012. Structure-function relationships of human milk oligosaccharides. Advances in Nutrition (Bethesda, MD) 3 (3):383S–91S. doi: 10.3945/an.111.001404.
- Böger, M., S. S. van Leeuwen, A. Lammerts van Bueren, and L. Dijkhuizen. 2019. Structural identity of galactooligosaccharide molecules selectively utilized by single cultures of probiotic bacterial strains. Journal of Agricultural and Food Chemistry 67 (50):13969–77. doi: 10.1021/acs.jafc.9b05968.
- Brosseau, C., A. Selle, D. J. Palmer, S. L. Prescott, S. Barbarot, and M. Bodinier. 2019. Prebiotics: Mechanisms and preventive effects in allergy. Nutrients 11 (8):1841. doi: 10.3390/nu11081841.
- Bruzzese, E., M. Volpicelli, F. Salvini, M. Bisceglia, P. Lionetti, M. Cinquetti, G. Iacono, and A. Guarino. 2006. Early administration of GOS/FOS prevents intestinal and respiratory infections in infants. Journal of Pediatric Gastroenterology and Nutrition 42 (5):LWW:E95.
- Bührer, C., R. Ensenauer, F. Jochum, H. Kalhoff, B. Koletzko, B. Lawrenz, W. Mihatsch, C. Posovszky, and S. Rudloff. 2022. Infant formulas with synthetic oligosaccharides and respective marketing practices: Position statement of the German Society for Child and Adolescent Medicine EV (DGKJ), Commission for Nutrition. Molecular and Cellular Pediatrics 9 (1):14. doi: 10.1186/s40348-022-00146-y.
- Burger-van Paassen, N., A. Vincent, P. J. Puiman, M. van der Sluis, J. Bouma, G. Boehm, J. B. Van Goudoever, I. Van Seuningen, and I. B. Renes. 2009. The regulation of intestinal mucin MUC2 expression by short-chain fatty acids: Implications for epithelial protection. The Biochemical Journal 420 (2):211–9. doi: 10.1042/BJ20082222.
- Bych, K., M. H. Mikš, T. Johanson, M. J. Hederos, L. K. Vigsnæs, and P. Becker. 2019. Production of HMOs using microbial hosts—from cell engineering to large scale production. Current Opinion in Biotechnology 56:130–7. doi: 10.1016/j.copbio.2018.11.003.
- Cai, Y., J. Folkerts, G. Folkerts, M. Maurer, and S. Braber. 2020. Microbiota‐dependent and‐independent effects of dietary fibre on human health. British Journal of Pharmacology 177 (6):1363–81. doi: 10.1111/bph.14871.
- Carasi, P., S. M. Racedo, C. Jacquot, D. E. Romanin, M. A. Serradell, and M. C. Urdaci. 2015. Impact of Kefir derived lactobacillus kefiri on the mucosal immune response and gut microbiota. Journal of Immunology Research 2015:1–12. doi: 10.1155/2015/361604.
- Chen, K., H. Chen, M. M. Faas, B. J. de Haan, J. Li, P. Xiao, H. Zhang, J. Diana, P. de Vos, and J. Sun. 2017. Specific inulin‐type fructan fibers protect against autoimmune diabetes by modulating gut immunity, barrier function, and microbiota homeostasis. Molecular Nutrition & Food Research 61 (8):1601006. doi: 10.1002/mnfr.201601006.
- Chen, X. 2015. Human milk oligosaccharides (HMOS): Structure, function, and enzyme-catalyzed synthesis. Advances in carbohydrate chemistry and biochemistry 72:113–90. doi: 10.1016/bs.accb.2015.08.002.
- Cheng, L., C. Kong, M. T. C. Walvoort, M. M. Faas, and P. Vos. 2020. Human milk oligosaccharides differently modulate goblet cells under homeostatic, proinflammatory conditions and ER stress. Molecular Nutrition & Food Research 64 (5):1900976. doi: 10.1002/mnfr.201900976.
- Clevers, H. C., and C. L. Bevins. 2013. Paneth Cells: Maestros of the small intestinal crypts. Annual Review of Physiology 75:289–311. doi: 10.1146/annurev-physiol-030212-183744.
- Cone, R. A. 2009. Barrier properties of mucus. Advanced Drug Delivery Reviews 61 (2):75–85. doi: 10.1016/j.addr.2008.09.008.
- Corfield, A. P. 2015. Mucins: A biologically relevant glycan barrier in mucosal protection. Biochimica Et Biophysica Acta 1850 (1):236–52. doi: 10.1016/j.bbagen.2014.05.003.
- Cornick, S., A. Tawiah, and K. Chadee. 2015. Roles and regulation of the mucus barrier in the gut. Tissue Barriers 3 (1–2):e982426. doi: 10.4161/21688370.2014.982426.
- Cummings, J. H., E. W. Pomare, W. J. Branch, C. P. Naylor, and G. T. MacFarlane. 1987. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 28 (10):1221–7. doi: 10.1136/gut.28.10.1221.
- de Almeida, M. N., and G. P. Maitan-Alfenas. 2021. Production of Oligosaccharides by fungi or fungal enzymes. In Encyclopedia of Mycology, 385–93. Amsterdam, The Netherlands: Elsevier. doi: 10.1016/B978-0-12-819990-9.00037-8.
- Dieterich, W., M. Schink, and Y. Zopf. 2018. Microbiota in the gastrointestinal tract. Medical Sciences 6 (4):116. doi: 10.3390/medsci6040116.
- Engfer, M. B., B. Stahl, B. Finke, G. Sawatzki, and H. Daniel. 2000. Human milk oligosaccharides are resistant to enzymatic hydrolysis in the upper gastrointestinal tract. The American Journal of Clinical Nutrition 71 (6):1589–96. doi: 10.1093/ajcn/71.6.1589.
- Fanaro, S., J. Jelinek, B. Stahl, G. Boehm, R. Kock, and V. Vigi. 2005. Acidic oligosaccharides from pectin hydrolysate as new component for infant formulae: effect on intestinal flora, stool characteristics, and PH. Journal of Pediatric Gastroenterology and Nutrition 41 (2):186–90. doi: 10.1097/01.mpg.0000172747.64103.d7.
- Farquhar, M. G., and G. E. Palade. 1963. Junctional complexes in various epithelia. The Journal of Cell Biology 17 (2):375–412. doi: 10.1083/jcb.17.2.375.
- Feng, W., Y. Wu, G. Chen, S. Fu, B. Li, B. Huang, D. Wang, W. Wang, and J. Liu. 2018. Sodium butyrate attenuates diarrhea in weaned piglets and promotes tight junction protein expression in colon in a GPR109A-dependent manner. Cellular Physiology and Biochemistry: International Journal of Experimental Cellular Physiology, Biochemistry, and Pharmacology 47 (4):1617–29. doi: 10.1159/000490981.
- Figueroa‐Lozano, S., and P. de Vos. 2019. Relationship between oligosaccharides and glycoconjugates content in human milk and the development of the gut barrier. Comprehensive Reviews in Food Science and Food Safety 18 (1):121–39. doi: 10.1111/1541-4337.12400.
- Figueroa-Lozano, S., C. Ren, H. Yin, H. Pham, S. van Leeuwen, L. Dijkhuizen, and P. de Vos. 2020. The Impact of Oligosaccharide Content, Glycosidic Linkages and Lactose Content of Galacto-Oligosaccharides (GOS) on the Expression of Mucus-Related Genes in Goblet Cells. Food & Function 11 (4):3506–15. doi: 10.1039/d0fo00064g.
- Fransen, F., N. M. Sahasrabudhe, M. Elderman, M. Bosveld, S. El Aidy, F. Hugenholtz, T. Borghuis, B. Kousemaker, S. Winkel, C. van der Gaast-de Jongh, et al. 2017. 1-fructans modulate the immune system in vivo in a microbiota-dependent and-independent fashion. Frontiers in Immunology 8:154. doi: 10.3389/fimmu.2017.00154.
- Gao, R., S. Tian, J. Wang, and W. Zhu. 2021. Galacto-oligosaccharides improve barrier function and relieve colonic inflammation via modulating mucosa-associated microbiota composition in lipopolysaccharides-challenged piglets. Journal of Animal Science and Biotechnology 12 (1):16. doi: 10.1186/s40104-021-00612-z.
- Garrod, D., and M. Chidgey. 2008. Desmosome structure, composition and function. Biochimica Et Biophysica Acta 1778 (3):572–87. doi: 10.1016/j.bbamem.2007.07.014.
- Garthoff, J. A., S. Heemskerk, R. A. Hempenius, B. A. R. Lina, C. A. M. Krul, J. H. Koeman, and G. J. A. Speijers. 2010. Safety evaluation of pectin-derived acidic oligosaccharides (PAOS): Genotoxicity and sub-chronic studies. Regulatory Toxicology and Pharmacology: RTP 57 (1):31–42. doi: 10.1016/j.yrtph.2009.12.004.
- Gasaly, N., P. de Vos, and M. A. Hermoso. 2021. Impact of bacterial metabolites on gut barrier function and host immunity: A focus on bacterial metabolism and its relevance for intestinal inflammation. Frontiers in Immunology 12:658354. doi: 10.3389/fimmu.2021.658354.
- Ghosh, S., C. S. Whitley, B. Haribabu, and V. R. Jala. 2021. Regulation of intestinal barrier function by microbial metabolites. Cellular and Molecular Gastroenterology and Hepatology 11 (5):1463–82. doi: 10.1016/j.jcmgh.2021.02.007.
- Goehring, K. C., B. J. Marriage, J. S. Oliver, J. A. Wilder, E. G. Barrett, and R. H. Buck. 2016. Similar to those who are breastfed, infants fed a formula containing 2′-fucosyllactose have lower inflammatory cytokines in a randomized controlled trial. The Journal of Nutrition 146 (12):2559–66. doi: 10.3945/jn.116.236919.
- Gopal, P. K., P. A. Sullivan, and J. B. Smart. 2001. Utilisation of galacto-oligosaccharides as selective substrates for growth by lactic acid bacteria including bifidobacterium lactis DR10 and lactobacillus rhamnosus DR20. International Dairy Journal 11 (1-2):19–25. doi: 10.1016/S0958-6946(01)00026-7.
- Goto, Y. 2019. Epithelial cells as a transmitter of signals from commensal bacteria and host immune cells. Frontiers in Immunology 10:2057. doi: 10.3389/fimmu.2019.02057.
- Hamer, H. M., D. Jonkers, K. Venema, S. Vanhoutvin, F. J. Troost, and R.-J. Brummer. 2008. Review article: The role of butyrate on colonic function. Alimentary Pharmacology & Therapeutics 27 (2):104–19. doi: 10.1111/j.1365-2036.2007.03562.x.
- Heiss, C. N., and L. E. Olofsson. 2018. Gut microbiota-dependent modulation of energy metabolism. Journal of Innate Immunity 10 (3):163–71. doi: 10.1159/000481519.
- Hendel, S. K., L. Kellermann, A. Hausmann, N. Bindslev, K. B. Jensen, and O. H. Nielsen. 2022. Tuft cells and their role in intestinal diseases. Frontiers in Immunology 13:822867. doi: 10.3389/fimmu.2022.822867.
- Holscher, H. D., L. Bode, and K. A. Tappenden. 2017. Human milk oligosaccharides influence intestinal epithelial cell maturation in vitro. Journal of Pediatric Gastroenterology and Nutrition 64 (2):296–301. doi: 10.1097/MPG.0000000000001274.
- Holscher, H. D., S. R. Davis, and K. A. Tappenden. 2014. Human milk oligosaccharides influence maturation of human intestinal Caco-2Bbe and HT-29 cell lines. The Journal of Nutrition 144 (5):586–91. doi: 10.3945/jn.113.189704.
- Hooper, L. V. 2009. Do symbiotic bacteria subvert host immunity? Nature Reviews. Microbiology 7 (5):367–74. doi: 10.1038/nrmicro2114.
- Houston, S. A., V. Cerovic, C. Thomson, J. Brewer, A. M. Mowat, and S. Milling. 2016. The lymph nodes draining the small intestine and colon are anatomically separate and immunologically distinct. Mucosal Immunology 9 (2):468–78. doi: 10.1038/mi.2015.77.
- Huang, F., E. Liao, and S. Yu. 2018. House dust mite allergy: Its innate immune response and immunotherapy. Immunobiology 223 (3):300–2. doi: 10.1016/j.imbio.2017.10.035.
- Huang, W., Q. Fang, L. Fan, T. Hong, H. Tan, and S. Nie. 2022. Pectin with various degrees of esterification differentially alters gut microbiota and metabolome of healthy adults. eFood 3 (1–2):e5. doi: 10.1002/efd2.5.
- Ibrahim, O. O. 2018. Functional oligosaccharides: Chemicals structure, manufacturing, health benefits, applications and regulations. Journal of Food Chemistry and Nanotechnology 4 (4):65–76. doi: 10.17756/jfcn.2018-060.
- Jackson, P. P. J., A. Wijeyesekera, S. Theis, J. van Harsselaar, and R. A. Rastall. 2022. Food for thought! inulin-type fructans: does the food matrix matter? Journal of Functional Foods 90:104987. doi: 10.1016/j.jff.2022.104987.
- Jandhyala, S. M., R. Talukdar, C. Subramanyam, H. Vuyyuru, M. Sasikala, and D. N. Reddy. 2015. Role of the normal gut microbiota. World Journal of Gastroenterology 21 (29):8787–803. doi: 10.3748/wjg.v21.i29.8787.
- Jiao, X., F. Li, J. Zhao, Y. Wei, L. Zhang, W. Yu, and Q. Li. 2023. The preparation and potential bioactivities of modified pectins: A review. Foods 12 (5):1016. doi: 10.3390/foods12051016.
- Kelly, G. 2008. Inulin-type prebiotics–a review: Part 1. Alternative Medicine Review 13 (4):315–29.
- Kong, C., M. Elderman, L. Cheng, B. J. de Haan, A. Nauta, and P. de Vos. 2019. Modulation of intestinal epithelial glycocalyx development by human milk oligosaccharides and non‐digestible carbohydrates. Molecular Nutrition & Food Research 63 (17):1900303. doi: 10.1002/mnfr.201900303.
- Kong, C., M. M. Faas, P. de Vos, and R. Akkerman. 2020. Impact of dietary fibers in infant formulas on gut microbiota and the intestinal immune barrier. Food & Function 11 (11):9445–67. doi: 10.1039/d0fo01700k.
- Kong, C., R. Akkerman, C. E. Klostermann, M. Beukema, M. M. P. Oerlemans, H. A. Schols, and P. de Vos. 2021. Distinct fermentation of human milk oligosaccharides 3-FL and LNT2 and GOS/inulin by infant gut microbiota and impact on adhesion of lactobacillus plantarum WCFS1 to gut epithelial cells. Food & Function 12 (24):12513–25. doi: 10.1039/d1fo02563e.
- König, J., J. Wells, P. D. Cani, C. L. García-Ródenas, T. MacDonald, A. Mercenier, J. Whyte, F. Troost, and R. J. Brummer. 2016. Human intestinal barrier function in health and disease. Clinical and Translational Gastroenterology 7 (10):e196. doi: 10.1038/ctg.2016.54.
- Kuhn, K. A., I. Pedraza, and M. K. Demoruelle. 2014. Mucosal immune responses to microbiota in the development of autoimmune disease. Rheumatic Diseases Clinics of North America 40 (4):711–25. doi: 10.1016/j.rdc.2014.07.013.
- Kundi, Z. M., J. C. Y. Lee, J. Pihlajamäki, C. B. Chan, K. S. Leung, S. S. Y. So, E. Nordlund, M. Kolehmainen, and H. El‐Nezami. 2021. Dietary fiber from oat and rye brans ameliorate western diet–induced body weight gain and hepatic inflammation by the modulation of short‐chain fatty acids, bile acids, and tryptophan metabolism. Molecular Nutrition & Food Research 65 (1):1900580. doi: 10.1002/mnfr.201900580.
- Ladirat, S. E. 2014. Galacto-oligosaccharides to counter the side effects of antibiotic treatments. Wageningen, The Netherlands: Wageningen University.
- Ladirat, S. E., H. A. Schols, A. Nauta, M. H. Schoterman, F. H. Schuren, and H. Gruppen. 2014. In vitro fermentation of galacto-oligosaccharides and its specific size-fractions using non-treated and amoxicillin-treated human inoculum. Bioactive Carbohydrates and Dietary Fibre 3 (2):59–70. doi: 10.1016/j.bcdf.2014.02.002.
- Larsen, N., C. Bussolo de Souza, L. Krych, T. Barbosa Cahú, M. Wiese, W. Kot, K. M. Hansen, A. Blennow, K. Venema, and L. Jespersen. 2019. Potential of pectins to beneficially modulate the gut microbiota depends on their structural properties. Frontiers in Microbiology 10:223. doi: 10.3389/fmicb.2019.00223.
- Lee, B., K. M. Moon, and C. Y. Kim. 2018. Tight junction in the intestinal epithelium: its association with diseases and regulation by phytochemicals. Journal of Immunology Research 2018:1–11. doi: 10.1155/2018/2645465.
- Li, J., L. Zhang, T. Wu, Y. Li, X. Zhou, and Z. Ruan. 2021. Indole-3-propionic acid improved the intestinal barrier by enhancing epithelial barrier and mucus barrier. Journal of Agricultural and Food Chemistry 69 (5):1487–95. doi: 10.1021/acs.jafc.0c05205.
- Li, L., Y. Wang, L. Zhu, Z. Liu, C. Ye, and S. Qin. 2020. Inulin with different degrees of polymerization protects against diet-induced endotoxemia and inflammation in association with gut microbiota regulation in mice. Scientific Reports 10 (1):12. doi: 10.1038/s41598-020-58048-w.
- Li, W., K. Wang, Y. Sun, H. Ye, B. Hu, and X. Zeng. 2015. Influences of structures of galactooligosaccharides and fructooligosaccharides on the fermentation in vitro by human intestinal microbiota. Journal of Functional Foods 13:158–68. doi: 10.1016/j.jff.2014.12.044.
- Liang, R., J. Chen, W. Liu, C. Liu, W. Yu, M. Yuan, and X. Zhou. 2012. Extraction, characterization and spontaneous gel-forming property of pectin from creeping fig (Ficus Pumila Linn.) seeds. Carbohydrate Polymers 87 (1):76–83. doi: 10.1016/j.carbpol.2011.07.013.
- Liu, T. W., K. D. Cephas, H. D. Holscher, K. R. Kerr, H. F. Mangian, K. A. Tappenden, and K. S. Swanson. 2016. Nondigestible fructans alter gastrointestinal barrier function, gene expression, histomorphology, and the microbiota profiles of diet-induced obese C57BL/6J mice. The Journal of Nutrition 146 (5):949–56. doi: 10.3945/jn.115.227504.
- LoCascio, R. G., M. R. Ninonuevo, S. L. Freeman, D. A. Sela, R. Grimm, C. B. Lebrilla, D. A. Mills, and J. B. German. 2007. Glycoprofiling of bifidobacterial consumption of human milk oligosaccharides demonstrates strain specific, preferential consumption of small chain glycans secreted in early human lactation. Journal of Agricultural and Food Chemistry 55 (22):8914–9. doi: 10.1021/jf0710480.
- Logtenberg, M. J. 2020. Bridging the immune gap between human milk and infant formula: Non-digestible oligosaccharides. Wageningen, The Netherlands: Wageningen University and Research.
- Logtenberg, M. J., R. Akkerman, R. An, G. D. A. Hermes, B. J. de Haan, M. M. Faas, E. G. Zoetendal, H. A. Schols, and P. de Vos. 2020. Fermentation of chicory fructo‐oligosaccharides and native inulin by infant fecal microbiota attenuates pro‐inflammatory responses in immature dendritic cells in an infant‐age‐dependent and fructan‐specific way. Molecular Nutrition & Food Research 64 (13):2000068. doi: 10.1002/mnfr.202000068.
- Louis, P., K. P. Scott, S. H. Duncan, and H. J. Flint. 2007. Understanding the effects of diet on bacterial metabolism in the large intestine. Journal of Applied Microbiology 102 (5):1197–208. doi: 10.1111/j.1365-2672.2007.03322.x.
- Mabbott, N. A., D. S. Donaldson, H. Ohno, I. R. Williams, and A. Mahajan. 2013. Microfold (M) cells: Important immunosurveillance posts in the intestinal epithelium. Mucosal Immunology 6 (4):666–77. doi: 10.1038/mi.2013.30.
- Macfarlane, S., and G. T. Macfarlane. 2003. Regulation of short-chain fatty acid production. The Proceedings of the Nutrition Society 62 (1):67–72. doi: 10.1079/pns2002207.
- Maráz, A., Z. Kovács, E. Benjamins, and M. Pázmándi. 2022. Recent developments in microbial production of high-purity galacto-oligosaccharides. World Journal of Microbiology and Biotechnology 38 (6):1–10. doi: 10.1007/s11274-022-03279-4.
- Marín-Manzano, M. C., O. Hernandez-Hernandez, M. Diez-Municio, C. Delgado-Andrade, F. J. Moreno, and A. Clemente. 2020. Prebiotic properties of non-fructosylated α-galactooligosaccharides from pea (Pisum Sativum L.) using infant fecal slurries. Foods 9 (7):921. doi: 10.3390/foods9070921.
- Marriage, B. J., R. H. Buck, K. C. Goehring, J. S. Oliver, and J. A. Williams. 2015. Infants fed a lower calorie formula with 2′ FL show growth and 2′ FL uptake like breast-fed infants. Journal of Pediatric Gastroenterology and Nutrition 61 (6):649–58. doi: 10.1097/MPG.0000000000000889.
- Martel, J., S. H. Chang, Y. F. Ko, T. L. Hwang, J. D. Young, and D. M. Ojcius. 2022. Gut barrier disruption and chronic disease. Trends in Endocrinology & Metabolism. Elsevier 33 (4):247–65. doi: 10.1016/j.tem.2022.01.002.
- Maslowski, K. M., A. T. Vieira, A. Ng, J. Kranich, F. Sierro, D. Yu, H. C. Schilter, M. S. Rolph, F. Mackay, D. Artis, et al. 2009. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461 (7268):1282–6. doi: 10.1038/nature08530.
- Masui, R., M. Sasaki, Y. Funaki, N. Ogasawara, M. Mizuno, A. Iida, S. Izawa, Y. Kondo, Y. Ito, Y. Tamura, et al. 2013. G protein-coupled receptor 43 moderates gut inflammation through cytokine regulation from mononuclear cells. Inflammatory Bowel Diseases 19 (13):2848–56. doi: 10.1097/01.MIB.0000435444.14860.ea.
- McDole, J. R., L. W. Wheeler, K. G. McDonald, B. Wang, V. Konjufca, K. A. Knoop, R. D. Newberry, and M. J. Miller. 2012. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature 483 (7389):345–9. doi: 10.1038/nature10863.
- Milani, C., S. Duranti, F. Bottacini, E. Casey, F. Turroni, J. Mahony, C. Belzer, S. Delgado Palacio, S. Arboleya Montes, L. Mancabelli, et al. 2017. The first microbial colonizers of the human gut: Composition, activities, and health implications of the infant gut microbiota. Microbiology and Molecular Biology Reviews 81 (4):e00036–17. doi: 10.1128/MMBR.00036-17.
- Morales-Medina, R., S. Drusch, F. Acevedo, A. Castro-Alvarez, A. Benie, D. Poncelet, M. M. Dragosavac, M. V. Defain Tesoriero, P. Löwenstein, V. Yonaha, et al. 2022. Structure, controlled release mechanisms and health benefits of pectins as an encapsulation material for bioactive food components. Food & Function 13 (21):10870–81. doi: 10.1039/d2fo00350c.
- Mowat, A. M., and W. W. Agace. 2014. Regional specialization within the intestinal immune system. Nature Reviews. Immunology 14 (10):667–85. doi: 10.1038/nri3738.
- Nakayama, Y., N. Kawasaki, T. Tamiya, S. Anzai, K. Toyohara, A. Nishiyama, and E. Kitazono. 2020. Comparison of the prebiotic properties of native chicory and synthetic inulins using swine fecal cultures. Bioscience, Biotechnology, and Biochemistry 84 (7):1486–96. doi: 10.1080/09168451.2020.1749553.
- Natividad, J. M., and E. F. Verdu. 2013. Modulation of intestinal barrier by intestinal microbiota: Pathological and therapeutic implications. Pharmacological Research 69 (1):42–51. doi: 10.1016/j.phrs.2012.10.007.
- Natividad, J. M., B. Marsaux, C. L. G. Rodenas, A. Rytz, G. Vandevijver, M. Marzorati, P. Van den Abbeele, M. Calatayud, and F. Rochat. 2022. Human milk oligosaccharides and lactose differentially affect infant gut microbiota and intestinal barrier in vitro. Nutrients 14 (12):2546. doi: 10.3390/nu14122546.
- Noll, A. J., Y. Yu, Y. Lasanajak, G. Duska-McEwen, R. H. Buck, D. F. Smith, and R. D. Cummings. 2016. Human DC-SIGN binds specific human milk glycans. The Biochemical Journal 473 (10):1343–53. doi: 10.1042/BCJ20160046.
- O’Hara, A. M., and F. Shanahan. 2006. The gut flora as a forgotten organ. EMBO Reports 7 (7):688–93. doi: 10.1038/sj.embor.7400731.
- O’Reilly, M. K., and J. C. Paulson. 2009. Siglecs as targets for therapy in immune-cell-mediated disease. Trends in Pharmacological Sciences 30 (5):240–8. doi: 10.1016/j.tips.2009.02.005.
- Pabst, R., M. W. Russell, and P. Brandtzaeg. 2008. Tissue distribution of lymphocytes and plasma cells and the role of the gut. Trends in Immunology 29 (5):206–8. doi: 10.1016/j.it.2008.02.006.
- Paone, P., and P. D. Cani. 2020. Mucus barrier, mucins and gut microbiota: The expected slimy partners? Gut 69 (12):2232–43. doi: 10.1136/gutjnl-2020-322260.
- Parada Venegas, D., M. K. De la Fuente, G. Landskron, M. J. González, R. Quera, G. Dijkstra, H. J. M. Harmsen, K. N. Faber, and M. A. Hermoso. 2019. Short chain fatty acids (SCFAs)-mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Frontiers in Immunology 10:277. doi: 10.3389/fimmu.2019.01486.
- Paßlack, N., M. Al-Samman, W. Vahjen, K. Männer, and J. Zentek. 2012. Chain length of inulin affects its degradation and the microbiota in the gastrointestinal tract of weaned piglets after a short-term dietary application. Livestock Science 149 (1–2):128–36. doi: 10.1016/j.livsci.2012.07.005.
- Payling, L., K. Fraser, S. M. Loveday, I. Sims, N. Roy, and W. McNabb. 2020. The effects of carbohydrate structure on the composition and functionality of the human gut microbiota. Trends in Food Science & Technology 97:233–48. doi: 10.1016/j.tifs.2020.01.009.
- Pelaseyed, T., J. H. Bergström, J. K. Gustafsson, A. Ermund, G. M. H. Birchenough, A. Schütte, S. van der Post, F. Svensson, A. M. Rodríguez-Piñeiro, E. E. L. Nyström, et al. 2014. The mucus and mucins of the goblet cells and enterocytes provide the first defense line of the gastrointestinal tract and interact with the immune system. Immunological Reviews 260 (1):8–20. doi: 10.1111/imr.12182.
- Peterson, L. W., and D. Artis. 2014. Intestinal epithelial cells: Regulators of barrier function and immune homeostasis. Nature Reviews. Immunology 14 (3):141–53. doi: 10.1038/nri3608.
- Pham, V. T., N. Seifert, N. Richard, D. Raederstorff, R. E. Steinert, K. Prudence, and M. H. Mohajeri. 2018. The effects of fermentation products of prebiotic fibres on gut barrier and immune functions in vitro. PeerJ 6:e5288. doi: 10.7717/peerj.5288.
- Picazo, B., A. C. Flores-Gallegos, D. B. Muñiz-Márquez, A. Flores-Maltos, M. R. Michel-Michel, O. de la Rosa, R. M. Rodríguez-Jasso, R. Rodríguez-Herrera, and C. N. Aguilar-González. 2019. Enzymes for fructooligosaccharides production: Achievements and opportunities. In Enzymes in food biotechnology, 303–20. Amsterdam, The Netherlands: Elsevier.
- Pickett-Bernard, D. 2006. Infant formula: Evaluating the safety of new ingredients. Journal of Human Lactation 22 (2):231. doi: 10.1177/089033440602200221.
- Powell, D. N., A. Swimm, R. Sonowal, A. Bretin, A. T. Gewirtz, R. M. Jones, and D. Kalman. 2020. Indoles from the commensal microbiota act via the AHR and IL-10 to tune the cellular composition of the colonic epithelium during aging. Proceedings of the National Academy of Sciences of the United States of America 117 (35):21519–26. doi: 10.1073/pnas.2003004117.
- Puccio, G., P. Alliet, C. Cajozzo, E. Janssens, G. Corsello, N. Sprenger, S. Wernimont, D. Egli, L. Gosoniu, and P. Steenhout. 2017. Effects of infant formula with human milk oligosaccharides on growth and morbidity: A randomized multicenter trial. Journal of Pediatric Gastroenterology and Nutrition 64 (4):624–31. doi: 10.1097/MPG.0000000000001520.
- Qi, Q., J. Li, B. Yu, J.-Y. Moon, J. C. Chai, J. Merino, J. Hu, M. Ruiz-Canela, C. Rebholz, Z. Wang, et al. 2022. Host and gut microbial tryptophan metabolism and type 2 diabetes: An integrative analysis of host genetics, diet, gut microbiome and circulating metabolites in cohort studies. Gut 71 (6):1095–105. doi: 10.1136/gutjnl-2021-324053.
- Rapoport, E. M., O. V. Kurmyshkina, and N. V. Bovin. 2008. Mammalian galectins: Structure, carbohydrate specificity, and functions. Biochemistry. Biokhimiia 73 (4):393–405. doi: 10.1134/s0006297908040032.
- Rastall, R. A., M. Diez-Municio, S. D. Forssten, B. Hamaker, A. Meynier, F. J. Moreno, F. Respondek, B. Stahl, K. Venema, and M. Wiese. 2022. Structure and function of non-digestible carbohydrates in the gut microbiome. Beneficial Microbes 13 (2):95–168. doi: 10.3920/BM2021.0090.
- Reboldi, A., and J. G. Cyster. 2016. Peyer’s patches: Organizing B‐cell responses at the intestinal frontier. Immunological Reviews 271 (1):230–45. doi: 10.1111/imr.12400.
- Rescigno, M., M. Urbano, B. Valzasina, M. Francolini, G. Rotta, R. Bonasio, F. Granucci, J. P. Kraehenbuhl, and P. Ricciardi-Castagnoli. 2001. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nature Immunology 2 (4):361–7. doi: 10.1038/86373.
- Rinninella, E., P. Raoul, M. Cintoni, F. Franceschi, G. A. D. Miggiano, A. Gasbarrini, and M. C. Mele. 2019. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms 7 (1):14. doi: 10.3390/microorganisms7010014.
- Roager, H. M., and T. R. Licht. 2018. Microbial tryptophan catabolites in health and disease. Nature Communications 9 (1):1–10. doi: 10.1038/s41467-018-05470-4.
- Roberfroid, M. B. 2004. Inulin-type fructans: Functional food ingredients. The Journal of Nutrition 137 (11):2493S–2502S. doi: 10.1093/jn/137.11.2493S
- Roberfroid, M. B., J. A. E. Van Loo, and G. R. Gibson. 1998. The bifidogenic nature of chicory inulin and its hydrolysis products. The Journal of Nutrition 128 (1):11–9. doi: 10.1093/jn/128.1.11.
- Robledo, V. R., and L. I. C. Vázquez. 2019. Pectin-extraction, purification, characterization and applications. In Pectins-extraction, purification, characterization and applications, 1–19. London, UK: intechopen.
- Rousseaux, A., C. Brosseau, S. Le Gall, H. Piloquet, S. Barbarot, and M. Bodinier. 2021. Human milk oligosaccharides: Their effects on the host and their potential as therapeutic agents. Frontiers in Immunology 12:680911. doi: 10.3389/fimmu.2021.680911.
- Rowland, I., G. Gibson, A. Heinken, K. Scott, J. Swann, I. Thiele, and K. Tuohy. 2018. Gut microbiota functions: Metabolism of nutrients and other food components. European Journal of Nutrition 57 (1):1–24. doi: 10.1007/s00394-017-1445-8.
- Sahasrabudhe, N. M., M. Beukema, L. Tian, B. Troost, J. Scholte, E. Bruininx, G. Bruggeman, M. van den Berg, A. Scheurink, H. A. Schols, et al. 2018. Dietary fiber pectin directly blocks toll-like receptor 2–1 and prevents doxorubicin-induced ileitis. Frontiers in Immunology 9:383. doi: 10.3389/fimmu.2018.00383.
- Salomov, I. T., A. R. Ashurov, O. KhM, U. I. Salomov, and B. M. Dzhalilov. 1994. Effect of pectin additives from cotton on the physical development, nutrition and erythrocytes in infants. Voprosy Pitaniia 6:16–8.
- Scholtens, P. A. M. J., M. S. Alles, J. G. Bindels, E. G. M. van der Linde, J. J. M. Tolboom, and J. Knol. 2006. Bifidogenic effects of solid weaning foods with added prebiotic oligosaccharides: a randomised controlled clinical trial. Journal of Pediatric Gastroenterology and Nutrition 42 (5):553–9. doi: 10.1097/01.mpg.0000221887.28877.c7.
- Schulzke, J. D., and M. Fromm. 2009. Tight junctions: Molecular structure meets function. Annals of the New York Academy of Sciences 1165 (1):1–6. doi: 10.1111/j.1749-6632.2009.04925.x.
- Scott, S. A., J. Fu, and P. V. Chang. 2020. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proceedings of the National Academy of Sciences of the United States of America 117 (32):19376–87. doi: 10.1073/pnas.2000047117.
- Sekirov, I., S. L. Russell, L. M. Antunes, and B. B. Finlay. 2010. Gut microbiota in health and disease. Physiological Reviews. American Physiological Society Bethesda, MD 90 (3):859–904. doi: 10.1159/000481627.
- Sharma, A. A., R. Jen, A. Butler, and P. M. Lavoie. 2012. The developing human preterm neonatal immune system: A case for more research in this area. Clinical Immunology 145 (1):61–8. doi: 10.1016/j.clim.2012.08.006.
- Shemtov, S. J., R. Emani, O. Bielska, A. J. Covarrubias, E. Verdin, J. K. Andersen, and D. A. Winer. 2022. The intestinal immune system and gut barrier function in obesity and ageing. The FEBS Journal 4:67. doi: 10.1111/febs.16558.
- Shi, J., P. Du, Q. Xie, N. Wang, H. Li, E. Smith, C. Li, F. Liu, G. Huo, and B. Li. 2020. Protective effects of tryptophan-catabolizing lactobacillus plantarum KLDS 1.0386 against dextran sodium sulfate-induced colitis in mice. Food & Function 11 (12):10736–47. doi: 10.1039/d0fo02622k.
- Shi, N., N. Li, X. Duan, and H. Niu. 2017. Interaction between the gut microbiome and mucosal immune system. Military Medical Research 4 (1):1–7. doi: 10.1186/s40779-017-0122-9.
- Singh, N., A. Gurav, S. Sivaprakasam, E. Brady, R. Padia, H. Shi, M. Thangaraju, P. D. Prasad, S. Manicassamy, D. H. Munn, et al. 2014. Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis. Immunity 40 (1):128–39. doi: 10.1016/j.immuni.2013.12.007.
- Smilowitz, J. T., C. B. Lebrilla, D. A. Mills, J. B. German, and S. L. Freeman. 2014. Breast milk oligosaccharides: Structure-function relationships in the neonate. Annual Review of Nutrition 34 (1):143–69. doi: 10.1146/annurev-nutr-071813-105721.
- Smith, P. M., M. R. Howitt, N. Panikov, M. Michaud, C. A. Gallini, M. Bohlooly-Y, J. N. Glickman, and W. S. Garrett. 2013. The microbial metabolites, short-chain fatty acids, regulate colonic T reg cell homeostasis. Science 341 (6145):569–73. doi: 10.1126/science.1241165.
- Sosinsky, G. E., and B. J. Nicholson. 2005. Structural organization of gap junction channels. Biochimica Et Biophysica Acta 1711 (2):99–125. doi: 10.1016/j.bbamem.2005.04.001.
- Strunk, T., A. Currie, P. Richmond, K. Simmer, and D. Burgner. 2011. Innate immunity in human newborn infants: Prematurity means more than immaturity. The Journal of Maternal-Fetal & Neonatal Medicine 24 (1):25–31. doi: 10.3109/14767058.2010.482605.
- Su, X., M. Zhang, H. Qi, Y. Gao, Y. Yang, H. Yun, Q. Zhang, X. Yang, Y. Zhang, J. He, et al. 2022. Gut microbiota–derived metabolite 3-idoleacetic acid together with lps induces IL-35+ B cell generation. Microbiome 10 (1):1–20. doi: 10.1186/s40168-021-01205-8.
- Su, X., Y. Gao, and R. Yang. 2022. Gut microbiota-derived tryptophan metabolites maintain gut and systemic homeostasis. Cells 11 (15):2296. doi: 10.3390/cells11152296.
- Šuligoj, T., L. K. Vigsnæs, P. V. Abbeele, A. Apostolou, K. Karalis, G. M. Savva, B. McConnell, and N. Juge. 2020. Effects of human milk oligosaccharides on the adult gut microbiota and barrier function. Nutrients 12 (9):2808. doi: 10.3390/nu12092808.
- Sun, M., W. Wu, Z. Liu, and Y. Cong. 2017. Microbiota metabolite short chain fatty acids, GPCR, and inflammatory bowel diseases. Journal of Gastroenterology 52 (1):1–8. doi: 10.1007/s00535-016-1242-9.
- Suzuki, T., S. Yoshida, and H. Hara. 2008. Physiological concentrations of short-chain fatty acids immediately suppress colonic epithelial permeability. The British Journal of Nutrition 100 (2):297–305. doi: 10.1017/S0007114508888733.
- Tennoune, N., M. Andriamihaja, and F. Blachier. 2022. Production of indole and indole-related compounds by the intestinal microbiota and consequences for the host: The good, the bad, and the ugly. Microorganisms 10 (5):930. doi: 10.3390/microorganisms10050930.
- Thursby, E., and N. Juge. 2017. Introduction to the human gut microbiota. The Biochemical Journal 474 (11):1823–36. doi: 10.1042/BCJ20160510.
- Tramontano, M., S. Andrejev, M. Pruteanu, M. Klünemann, M. Kuhn, M. Galardini, P. Jouhten, A. Zelezniak, G. Zeller, P. Bork, et al. 2018. Nutritional preferences of human gut bacteria reveal their metabolic idiosyncrasies. Nature Microbiology 3 (4):514–22. doi: 10.1038/s41564-018-0123-9.
- Triantis, V., L. Bode, and R. J. J. Van Neerven. 2018. Immunological effects of human milk oligosaccharides. Frontiers in Pediatrics 6:190. doi: 10.3389/fped.2018.00190.
- Trompette, A., E. S. Gollwitzer, K. Yadava, A. K. Sichelstiel, N. Sprenger, C. Ngom-Bru, C. Blanchard, T. Junt, L. P. Nicod, N. L. Harris, et al. 2014. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nature Medicine 20 (2):159–66. doi: 10.1038/nm.3444.
- Tuomainen, M., J. Lindström, M. Lehtonen, S. Auriola, J. Pihlajamäki, M. Peltonen, J. Tuomilehto, M. Uusitupa, V. D. de Mello, and K. Hanhineva. 2018. Associations of serum indolepropionic acid, a gut microbiota metabolite, with type 2 diabetes and low-grade inflammation in high-risk individuals. Nutrition & Diabetes 8 (1):1–5. doi: 10.1038/s41387-018-0046-9.
- Turner, P. V. 2018. The role of the gut microbiota on animal model reproducibility. Animal Models and Experimental Medicine 1 (2):109–15. doi: 10.1002/ame2.12022.
- Uerlings, J., M. Schroyen, E. Willems, S. Tanghe, G. Bruggeman, J. Bindelle, and N. Everaert. 2020. Differential effects of inulin or its fermentation metabolites on gut barrier and immune function of porcine intestinal epithelial cells. Journal of Functional Foods 67:103855. doi: 10.1016/j.jff.2020.103855.
- Ulluwishewa, D., R. C. Anderson, W. C. McNabb, P. J. Moughan, J. M. Wells, and N. C. Roy. 2011. Regulation of tight junction permeability by intestinal bacteria and dietary components. The Journal of Nutrition 141 (5):769–76. doi: 10.3945/jn.110.135657.
- Valdes, A. M., J. Walter, E. Segal, and T. D. Spector. 2018. Role of the gut microbiota in nutrition and health. BMJ (Clinical Research Ed.) 361:k2179. doi: 10.1136/bmj.k2179.
- Van den Abbeele, P., L. Verstrepen, J. Ghyselinck, R. Albers, M. Marzorati, and A. Mercenier. 2020. A novel non-digestible, carrot-derived polysaccharide (CRG-I) selectively modulates the human gut microbiota while promoting gut barrier integrity: An integrated in vitro approach. Nutrients 12 (7):1917. doi: 10.3390/nu12071917.
- Van der Sluis, M., B. A. E. De Koning, A. C. J. M. De Bruijn, A. Velcich, J. P. P. Meijerink, J. B. Van Goudoever, H. A. Büller, J. Dekker, I. Van Seuningen, I. B. Renes, et al. 2006. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology 131 (1):117–29. doi: 10.1053/j.gastro.2006.04.020.
- Vancamelbeke, M., and S. Vermeire. 2017. The intestinal barrier: A fundamental role in health and disease. Expert Review of Gastroenterology & Hepatology 11 (9):821–34. doi: 10.1080/17474124.2017.1343143.
- Varasteh, S., B. Van’t Land, I. Giziakis, M. Mank, B. Stahl, S. Wiertsema, G. Folkerts, J. Garssen, and S. Braber. 2019. Human milk oligosaccharide 3′-galactosyllactose can protect the intestinal barrier to challenges. Journal of Pediatric Gastroenterology and Nutrition 68:N–P–016. doi: 10.3390/nu13093190.
- Veereman, G. 2007. Pediatric applications of inulin and oligofructose. The Journal of Nutrition 137 (11 Suppl):2585S–9S. doi: 10.1093/jn/137.11.2585S.
- Venkatesh, M., S. Mukherjee, H. Wang, H. Li, K. Sun, A. P. Benechet, Z. Qiu, L. Maher, M. R. Redinbo, R. S. Phillips, et al. 2014. Symbiotic bacterial metabolites regulate gastrointestinal barrier function via the xenobiotic sensor PXR and toll-like receptor 4. Immunity 41 (2):296–310. doi: 10.1016/j.immuni.2014.06.014.
- Vera, C., A. Córdova, C. Aburto, C. Guerrero, S. Suárez, and A. Illanes. 2016. Synthesis and purification of galacto-oligosaccharides: State of the art. World Journal of Microbiology and Biotechnology 32 (12):1–20. doi: 10.1007/s11274-016-2159-4.
- Verkhnyatskaya, S., M. Ferrari, P. de Vos, and M. T. C. Walvoort. 2019. Shaping the infant microbiome with non-digestible carbohydrates. Frontiers in Microbiology 10:343. doi: 10.3389/fmicb.2019.00343.
- Viggiano, D., G. Ianiro, G. Vanella, S. Bibbò, G. Bruno, G. Simeone, and G. Mele. 2015. Gut barrier in health and disease: Focus on childhood. European Review for Medical and Pharmacological Sciences 19 (6):1077–85.
- Vogt, L. M., D. Meyer, G. Pullens, M. M. Faas, K. Venema, U. Ramasamy, H. A. Schols, and P. de Vos. 2014. Toll-like receptor 2 activation by B2→1-fructans protects barrier function of T84 human intestinal epithelial cells in a chain length-dependent manner. Journal of Nutrition 144 (7):1002–8. doi: 10.3945/jn.114.191643.
- Vogt, L. M., N. M. Sahasrabudhe, U. Ramasamy, D. Meyer, G. Pullens, M. M. Faas, K. Venema, H. A. Schols, and P. de Vos. 2016. The impact of lemon pectin characteristics on TLR activation and T84 intestinal epithelial cell barrier function. Journal of Functional Foods 22:398–407. doi: 10.1016/j.jff.2016.02.002.
- Vogt, L., D. Meyer, G. Pullens, M. Faas, M. Smelt, K. Venema, U. Ramasamy, H. A. Schols, and P. de Vos. 2015. Immunological properties of inulin-type fructans. Critical Reviews in Food Science and Nutrition 55 (3):414–36. doi: 10.1080/10408398.2012.656772.
- Vogt, L., U. Ramasamy, D. Meyer, G. Pullens, K. Venema, M. M. Faas, H. A. Schols, and P. de Vos. 2013. Immune modulation by different types of B2→1-fructans is toll-like receptor dependent. PLoS One 8 (7):e68367. doi: 10.1371/journal.pone.0068367.
- Walker, A. 2010. Breast milk as the gold standard for protective nutrients. The Journal of Pediatrics 156 (2 Suppl):S3–S7. doi: 10.1016/j.jpeds.2009.11.021.
- Walters, W. A., Z. Xu, and R. Knight. 2014. Meta-analyses of human gut microbes associated with obesity and IBD. FEBS Letters 588 (22):4223–33. doi: 10.1016/j.febslet.2014.09.039.
- Wang, G., W. Sun, X. Pei, Y. Jin, H. Wang, W. Tao, Z. Xiao, L. Liu, and M. Wang. 2021. Galactooligosaccharide pretreatment alleviates damage of the intestinal barrier and inflammatory responses in LPS-challenged mice. Food & Function 12 (4):1569–79. doi: 10.1039/d0fo03020a.
- Westerbeek, E. A. M., J. P. van den Berg, H. N. Lafeber, W. P. F. Fetter, G. Boehm, J. W. R. Twisk, and R. M. van Elburg. 2010. Neutral and acidic oligosaccharides in preterm infants: A randomized, double-blind, placebo-controlled trial. The American Journal of Clinical Nutrition 91 (3):679–86. doi: 10.3945/ajcn.2009.28625.
- Westerbeek, E. A. M., R. L. Hensgens, W. A. Mihatsch, G. Boehm, H. N. Lafeber, and R. M. Van Elburg. 2011. The effect of neutral and acidic oligosaccharides on stool viscosity, stool frequency and stool PH in preterm infants. Acta Paediatrica (Oslo, Norway: 1992) 100 (11):1426–31. doi: 10.1111/j.1651-2227.2011.02295.x.
- Wiciński, M., E. Sawicka, J. Gębalski, K. Kubiak, and B. Malinowski. 2020. Human milk oligosaccharides: Health benefits, potential applications in infant formulas, and pharmacology. Nutrients 12 (1):266. doi: 10.3390/nu12010266.
- Wiertsema, S. P., J. van Bergenhenegouwen, J. Garssen, and L. J. Knippels. 2021. The interplay between the gut microbiome and the immune system in the context of infectious diseases throughout life and the role of nutrition in optimizing treatment strategies. Nutrients 13 (3):886. doi: 10.3390/nu13030886.
- Wlodarska, M., C. Luo, R. Kolde, E. d’Hennezel, J. W. Annand, C. E. Heim, P. Krastel, E. K. Schmitt, A. S. Omar, E. A. Creasey, et al. 2017. Indoleacrylic acid produced by commensal peptostreptococcus species suppresses inflammation. Cell Host & Microbe 22 (1):25–37.e6. doi: 10.1016/j.chom.2017.06.007.
- Wozniak, H., T. S. Beckmann, L. Fröhlich, T. Soccorsi, C. Le Terrier, A. de Watteville, J. Schrenzel, and C. P. Heidegger. 2022. The central and biodynamic role of gut microbiota in critically ill patients. Critical Care 26 (1):1–12. doi: 10.1186/s13054-022-04127-5.
- Wu, R. Y., B. Li, Y. Koike, P. Määttänen, H. Miyake, M. Cadete, K. C. Johnson‐Henry, S. R. Botts, C. Lee, T. R. Abrahamsson, et al. 2018. Human milk oligosaccharides increase mucin expression in experimental necrotizing enterocolitis. Molecular Nutrition & Food Research 63 (3):1800658. doi: 10.1002/mnfr.201800658.
- Yang, B.-H., S. Hagemann, P. Mamareli, U. Lauer, U. Hoffmann, M. Beckstette, L. Föhse, I. Prinz, J. Pezoldt, S. Suerbaum, et al. 2016. Foxp3+ T cells expressing RORγt represent a stable regulatory T-cell effector lineage with enhanced suppressive capacity during intestinal inflammation. Mucosal Immunology 9 (2):444–57. doi: 10.1038/mi.2015.74.
- Ye, X., H. Li, K. Anjum, X. Zhong, S. Miao, G. Zheng, W. Liu, and L. Li. 2022. Dual role of indoles derived from intestinal microbiota on human health. Frontiers in Immunology 13:903526. doi: 10.3389/fimmu.2022.903526.
- Yeung, Y. K., Y. R. Kang, B. R. So, S. K. Jung, and Y. H. Chang. 2021. Structural, antioxidant, prebiotic and anti-inflammatory properties of pectic oligosaccharides hydrolyzed from okra pectin by fenton reaction. Food Hydrocolloids 118:106779. doi: 10.1016/j.foodhyd.2021.106779.
- Yu, Z., C. Chen, and D. S. Newburg. 2013. Utilization of major fucosylated and sialylated human milk oligosaccharides by isolated human gut microbes. Glycobiology 23 (11):1281–92. doi: 10.1093/glycob/cwt065.
- Zelante, T., R. G. Iannitti, C. Cunha, A. De Luca, G. Giovannini, G. Pieraccini, R. Zecchi, C. D’Angelo, C. Massi-Benedetti, F. Fallarino, et al. 2013. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity 39 (2):372–85. doi: 10.1016/j.immuni.2013.08.003.
- Zeuner, B., D. Teze, J. Muschiol, and A. S. Meyer. 2019. Synthesis of human milk oligosaccharides: protein engineering strategies for improved enzymatic transglycosylation. Molecules 24 (11):2033. doi: 10.3390/molecules24112033.
- Zhao, Y., J. Bi, J. Yi, X. Wu, Y. Ma, and R. Li. 2021. Pectin and homogalacturonan with small molecular mass modulate microbial community and generate high SCFAs via in vitro gut fermentation. Carbohydrate Polymers 269:118326. doi: 10.1016/j.carbpol.2021.118326.
- Zheng, D., T. Liwinski, and E. Elinav. 2020. Interaction between microbiota and immunity in health and disease. Cell Research 30 (6):492–506. doi: 10.1038/s41422-020-0332-7.
- Zhi, Z., J. Chen, S. Li, W. Wang, R. Huang, D. Liu, T. Ding, R. J. Linhardt, S. Chen, and X. Ye. 2017. Fast preparation of RG-I enriched ultra-low molecular weight pectin by an ultrasound accelerated fenton process. Scientific Reports 7 (1):1–11. doi: 10.1038/s41598-017-00572-3.
- Zhu, L., S. Qin, S. Zhai, Y. Gao, and L. Li. 2017. Inulin with different degrees of polymerization modulates composition of intestinal microbiota in mice. FEMS Microbiology Letters 364 (10):fnx075. doi: 10.1093/femsle/fnx075.
- Zuurveld, M., N. P. van Witzenburg, J. Garssen, G. Folkerts, B. Stahl, B. Van’t Land, and L. E. M. Willemsen. 2020. Immunomodulation by human milk oligosaccharides: The potential role in prevention of allergic diseases. Frontiers in Immunology 11:801. doi: 10.3389/fimmu.2020.00801.
