Abstract
Rotaviruses, double-stranded, non-enveloped RNA viruses, are a global health concern, associated with acute gastroenteritis and secretory-driven watery diarrhoea, especially in infants and young children. Conventionally, rotavirus is primarily viewed as a pathogen for intestinal enterocytes. This notion is challenged, however, by data from patients and animal models documenting extra-intestinal clinical manifestations and viral replication following rotavirus infection. In addition to acute gastroenteritis, rotavirus infection has been linked to various neurological disorders, hepatitis and cholestasis, type 1 diabetes, respiratory illness, myocarditis, renal failure and thrombocytopenia. Concomitantly, molecular studies have provided insight into potential mechanisms by which rotavirus can enter and replicate in non-enterocyte cell types and evade host immune responses. Nevertheless, it is fair to say that the extra-intestinal aspect of the rotavirus infectious process is largely being overlooked by biomedical professionals, and there are gaps in the understanding of mechanisms of pathogenesis. Thus with the aim of increasing public and professional awareness we here provide a description of our current understanding of rotavirus-related extra-intestinal clinical manifestations and associated molecular pathogenesis. Further understanding of the processes involved should prove exceedingly useful for future diagnosis, treatment and prevention of rotavirus-associated disease.
Introduction
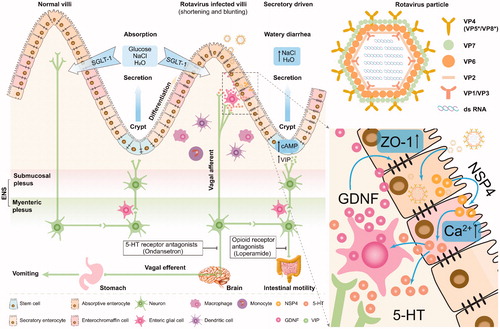
Rotaviruses (RVs) are non-enveloped double-stranded RNA (dsRNA) viruses that belong to the Reoviridae family (Trask et al. Citation2012). Their genome comprises 11 segments of dsRNA encoding six viral structural proteins (VP1 to VP4, VP6 and VP7) and six non-structural proteins (NSP1 to NSP6) (Trask et al. Citation2012) (). Up to now, ten rotavirus species (A to J) have been identified. Four of these (A, B, C, and H) cause human disease, with the rotavirus A species [featuring strains Wa, DS-1 and AU-1 (Matthijnssens et al. Citation2008)] being the most significant in this respect (Crawford et al. Citation2017). Human rotaviruses are important enteric pathogen, infecting the epithelial compartment of the small intestine, and are a major cause of gastroenteritis in infants and young children (Crawford et al. Citation2017; Bányai et al. Citation2018). Although the introduction of anti-rotavirus vaccines (Rotateq and Rotarix, two live-attenuated oral vaccines) has raised hopes that the virus can eventually be constrained (Burnett et al., Citation2020; Simsek et al. Citation2021), clinical management of rotavirus-associated disease is complicated by the absence of specific antiviral therapy (Crawford et al. Citation2017; Bányai et al. Citation2018). The canonical view is that rotavirus infection is restricted to the intestine, but this notion has become challenged (Kraft Citation1958; Blutt and Conner Citation2007; Ramig Citation2007; Gómez-Rial et al. Citation2019). During the acute phase of rotavirus infection, both antigenemia and viremia are readily detected in both experimental animals and children, demonstrating that the virus can reach a multitude of potential host compartments (Blutt et al. Citation2003; Citation2007; Ramig Citation2007; Gómez-Rial et al. Citation2019). In apparent agreement, the presence of either rotaviral RNA, protein or infectious particles during human or animal infection, has been documented in brain, liver, spleen, lung, heart, kidney, pancreas, thymus, adrenal gland, bladder testis and immune cells (Kraft Citation1958; Crawford et al. Citation2006; Blutt and Conner Citation2007; Ramig Citation2007). Accordingly, extra-intestinal complications during rotavirus therapy have been widely reported (Mossel and Ramig Citation2003; Ramig Citation2007; Gómez-Rial et al. Citation2019). Nevertheless, it is fair to say that the extra-intestinal aspect of rotavirus infection is largely ignored by the biomedical community. This prompted us to assess the evidence for non-intestinal diseases associated with rotavirus infection, the possible size of the clinical problem associated with such infection, and the pathological mechanisms driving extra-intestinal rotavirus-associated disease.
Figure 1. Rotavirus infection-induced acute gastroenteritis. The rotavirus particle contains 11 segments of dsRNA as its genome, and the capsid consists of three layers. The intestinal epithelium is characterized by the villi and crypt. Mature enterocytes locate at the top and middle of villi allow SGLT-1-mediated absorption of water and salt. The ECs locate at the middle of villi are highly specialized cells with endocrine function. Stem cells and Paneth cells locate in the crypt are functionally responsible for differentiation and secretion, respectively. Thus, under normal conditions, the intact intestinal membrane barrier can keep homeostasis (absorption and secretion). While rotavirus infection in mature enterocytes causes absorptive enterocyte death and secretory Paneth cell replacement, leading to shortening and blunting of villi, and increasing infiltration of inflammatory cells in the lamina propria. The NSP4 stimulates the epithelium and ECs to increase intracellular calcium, which further induces the secretion of 5-HT from ECs through a calcium-dependent manner. The secreted 5-HT activates EGCs to increase release of GDNF which induces the expression of tight junction-associated protein ZO-1 in infected and bystander cells. Thus neurotrophic factors and 5-HT can protect the intestinal barrier function during rotavirus insult. Moreover, the number of enterocytes remaining following infection is functionally sufficient to allow SGLT-1-mediated absorption of water and salt. However, 5-HT can also activate the intrinsic primary afferent nerves of the myenteric plexus. Such activation activates the nerves of the submucosal plexus and leads to increase of intestinal motility which can be attenuated by an opioid-receptor-antagonist (Loperamide). The activation of submucosal nerves further induce VIP release from nerve endings adjacent to crypt cells. Then, VIP induces crypt cells to secret NaCl and water into the intestinal lumen by increasing cellular cAMP levels, which ultimately leading to secretory diarrhoea. During these processes, the stimulated afferent vagal signalling activates the nausea and vomiting centre of the brain to generate efferent vagal signalling which then results in vomiting by stimulating a nerve-muscle vomiting reflex in the stomach. This event can be attenuated by 5-HT receptor antagonists (Ondansetron). Finally, intestinal rotavirus infection results in secretory-driven watery diarrhoea accompanying by vomiting. dsRNA: double-stranded RNA; VPs: rotavirus structural proteins (VP4 is cleaved into VP5* and VP8*); NSP4: rotavirus non-structural protein; ENS: enteric nervous system; NaCl: sodium chloride; Ca2+: calcium ions; SGLT-1: sodium/glucose cotransporter 1; 5-HT: 5-hydroxytryptamine (serotonin); VIP: vasoactive intestinal peptide; ECs: enterochromaffin cells; EGCs: enteric glial cells; GDNF: glial cell-derived neurotrophic factor; ZO-1: zona occludens 1; cAMP: cyclic adenosine monophosphate.
Rotavirus-induced gastrointestinal disease
Acute gastroenteritis
Before considering potential extra-intestinal rotavirus infection, it is important to review the conventional presentation of the disease, acute gastroenteritis ( and ). About 258 million diarrhoea episodes and 129 000–200 000 associated deaths per year are attributed to rotavirus infection, making it the leading cause of gastroenteritis in young children (Tate et al. Citation2016; Crawford et al. Citation2017; Bányai et al. Citation2018; Hartman et al. Citation2019). As the vast majority of cases occurs in developing countries, rotavirus infection is seen as a global health concern, but also in developing countries rotavirus associated gastroenteritis remains a major cause of hospitalization in children (Crawford et al. Citation2017). Following the introduction of anti-rotavirus vaccination, hospitalizations and mortality has shown a 25–55% decline (Crawford et al. Citation2017; Troeger et al. Citation2018; Aliabadi et al. Citation2019; Burke et al. Citation2019; Burnett et al., Citation2020). Nonetheless, 8–10% of all children with gastroenteritis and 35–40% of hospitalized children are positive for rotavirus (Bányai et al. Citation2018). Compounding the clinical problem is that children often suffer from multiple episodes of rotavirus infection as multiple serotypes are present in the population and both vaccine and prior disease fail to provide full immunity (36 G genotypes and 51 P genotypes have been classified in species A rotavirus binary serotype system based on the two outer capsid proteins VP4 and VP7 (Crawford et al. Citation2017; Simsek et al. Citation2021), respectively), even if subsequent infections are less severe than first infections (Velázquez et al. Citation1996; Mormile Citation2016). By the age of five, nearly every child in the world will have been infected with rotavirus at least once (Tate et al. Citation2012).
Figure 2. Rotavirus-related systemic diseases and proposed mechanisms. The primary infection of rotavirus in the intestine leads to acute gastroenteritis. However, the tropism and pathogenetic role of rotavirus infection is not only limited to the gastrointestinal tract. The extra-intestinal dissemination and infection of rotavirus in non-intestinal tissues such as the spleen, liver, heart, lung, kidney, testis, bladder, adrenal gland, pancreas and brain have been confirmed, which may sometimes lead to additional extra-intestinal complications. Here we present rotavirus-induced acute gastroenteritis and the frequently reported complications related to rotavirus extra-intestinal spread and propose the potential mechanisms. RV: rotavirus; VP7: viral structural protein; NSP4: non-structural protein; ENS: enteric nervous system; NO: nitric oxide; IFN-γ: interferon gamma.
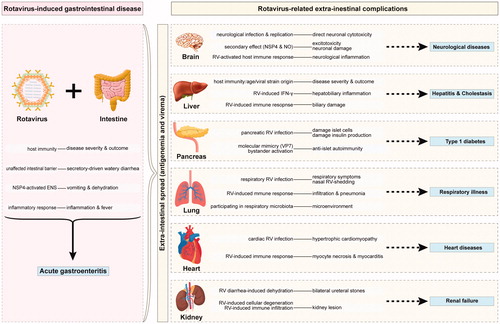
The primary outcome of rotavirus infection is acute gastroenteritis. Its clinical features range from subclinical infection and mild watery diarrhoea to severe diarrhoea with vomiting and fever that can result in dehydration with shock, electrolyte imbalance, and death (Hjelt et al. Citation1985; Haffejee and Moosa Citation1990; Leung et al. Citation2005; Parashar et al. Citation2013; Esona and Gautam Citation2015) (). The importance of antiviral immunity in controlling disease is highlighted by the observation that the symptomology is more severe in children with more immature immune systems (Crawford et al. Citation2017; Bányai et al. Citation2018), with disease being the worst in the youngest children, where as severe dehydration, electrolyte disturbances and emesis are not uncommon following rotavirus infection (Leung et al. Citation2005; Parashar et al. Citation2013; Hartman et al. Citation2019). In both humans and animal models (piglets, calves, lambs and mice) rotavirus infection may provoke histological and functional alterations changes in the small intestine, which include intestinal wall hypotrophy, loss of epithelial microvilli, villous atrophy and intraepithelial lymphocytosis, and loss of disaccharidase activity (Dharakul et al. Citation1988; Haffejee and Moosa Citation1990; Crawford et al. Citation2017) (). Examination of intestinal biopsies from rotavirus-infected children, however, show poor correlation between histological abnormalities and diarrhoea (Köhler et al. Citation1990; Ramig Citation2004; Hagbom et al. Citation2016). Interestingly, rotavirus-induced anatomical changes were linked to the slightly increased intussusception (a serious condition where an intestinal segment folds into an adjacent part of the intestine) observed primarily in application of the first-generation vaccine, but more substantial evidence has demonstrated that neither natural rotavirus infection nor vaccination are significantly associated with intussusception (Robinson et al. Citation2004; Lu et al. Citation2019; Burnett et al., Citation2020). In general, rotavirus-induced gastrointestinal disease manifests as acute gastroenteritis is associated with watery diarrhoea, low-grade fever, vomiting, low inflammation, and intestinal wall damage (Hagbom et al. Citation2020).
Table 1. Clinical manifestation and evidence summary of rotavirus-related systemic diseases.
The pathogenesis of rotavirus gastroenteritis is multifactorial ( and ). Conventionally, gastroenteritis is viewed as the consequence of rotavirus infecting mature enterocyte and enterochromaffin cells (ECs, one type of enteroendocrine cell) at the tip and the body of intestinal villi, causing loss of enterocytes and secondary expansion of the Paneth cell compartment. Consequently, secretion of digestive enzymes and disaccharidase is impaired, in turn increasing osmolarity of the intestinal lumen and thus provoking diarrhoea and malabsorption (Colbère-Garapin et al. Citation2007; Hagbom et al. Citation2016). This concept has been challenged by observation in experimental rodents that show that the number of enterocytes remaining following infection is functionally sufficient to allow sodium/glucose cotransporter (SGLT-1)-mediated absorption of water and salt (Hagbom et al. Citation2011; Citation2012; Citation2016). Thus it has been proposed that the diarrhoea is an active defense mechanism controlled by neurotrophic factors and the serotonin 5-hydroxytryptamine (5-HT) (Istrate et al. Citation2014; Hagbom et al. Citation2020), in which the enteric nervous system is activated as Loperamide (an opioid receptor agonist) appears to attenuate rotavirus-induced diarrhoea (Li et al. Citation2007; Hagbom et al. Citation2012). The notion that diarrhoea is an active process and not the result from loss of absorptive function is supported by the success of rehydration in rotavirus-induced diarrhoea (Rautanen et al. Citation1997; Hagbom et al. Citation2012) or the observation that zinc-mediated inhibition of cAMP-dependent chloride secretion counteracts rotavirus-induced diarrhoea (Baqui et al. Citation2002; Dalgic et al. Citation2011; Hagbom et al. Citation2012). Altogether, these studies indicate that rotavirus-induced watery diarrhoea is of a secretory nature.
At the molecular level, rotavirus replication in enterocytes and ECs results in expression and release of the rotaviral non-structural protein 4 (NSP4), which is a major viral enterotoxin due to its virporin activity and subsequently provoked increased levels of intracellular Ca2+ (Van Den Brink et al. Citation1999; Hagbom et al. Citation2012; Hyser et al. Citation2012). This provokes release of 5-HT by the EC compartment, in turn activating the primary afferent nerves of the myenteric plexus of the enteric nervous system (ENS) (Hagbom et al. Citation2011; Citation2012; Citation2016; Crawford et al. Citation2017). The resulting neurotransmission in turn is responsible for increased intestinal motility as well as the release of vasoactive intestinal peptide (VIP) from synaptic terminals located adjacent to crypt cells (Hagbom et al. Citation2012; Citation2016; Crawford et al. Citation2017). As a hormone, VIP stimulates secretion of sodium, chloride, potassium and indirectly of water into the small intestine diarrhoea through increased cAMP production (Hagbom et al. Citation2012; Citation2016; Crawford et al. Citation2017). During this process the afferent component of the nervus vagus becomes stimulated, and this provokes vomiting through a reflex relay to the stomach (Hagbom et al. Citation2011; Citation2012; Citation2016; Crawford et al. Citation2017), again 5-HT being a prominent neurotransmitter in thus process as evident by the attenuation of emesis following the use of receptor antagonist (Ondansetron) (Yamashiro et al. Citation1989; Kordasti et al. Citation2004; Hagbom et al. Citation2012; Crawford et al. Citation2017). Apart from provoking 5-HT release, NSP4 also stimulates production of nitric oxide (NO) release and this also modulates ENS signalling (Hagbom et al. Citation2012). Thus the notion that rotavirus-provoked diarrhoea is secretory in nature can be mechanistically substantiated.
Apart from diarrhoea, rotavirus infection provokes systemic activation of immunity as for instance evident from the fever that often accompanies disease (). Clinical studies show that rotavirus gastroenteritis is associated with increased levels of the pro-inflammatory cytokines interleukin-1β (IL-1β), IL-6, IL-8 and interferon gamma (IFN-γ) (Mormile Citation2016; Crawford et al. Citation2017), which have been linked to fever and malaise. Much of the tissue damage observed in rotavirus gastroenteritis may be secondary to immune cell activation by such cytokines and not as much from direct viral cytopathic effects (Mormile Citation2016). Especially serum IL-8 appears a distinctive biomarker for clinical rotavirus-mediated disease (Chen et al. Citation2014; Mormile Citation2016). IFN-γ production may well be instrumental in inducing clearance of virus as it is a canonical mediator of cell autonomous and T cell-mediated immune responses (Mormile Citation2016). Indeed, adult life is characterized by stronger IFN-γ production and subsequent T cells activation, as compared to infants, which fits well with the decreased susceptibility of adults to rotavirus infection as compared to children (Mormile Citation2016). While we understand the interaction of rotavirus with mucosal immunity fairly well, potential interactions outside the intestine are, however, less well understood.
Rotavirus-related extra-intestinal complications
Central nervous system diseases
Extra-intestinal manifestations reported following paediatric rotavirus infection in infants and children most commonly involve the central nervous system (CNS) (Ramig Citation2007; Gómez-Rial et al. Citation2019). Following early reports from East Asia, also Western countries reported cases apparently rotavirus-related cases of neurological disorders, such as seizures, meningitis, encephalopathy, encephalitis, and cerebellitis (Wong et al. Citation1984; Ushijima et al. Citation1986; Nishimura et al. Citation1993; Lynch et al. Citation2001; Iturriza-Gómara et al. Citation2002; Fukuda et al. Citation2009; Takanashi et al. Citation2010; Karampatsas et al. Citation2015; Laizane et al. Citation2019). The severity of the disease varies widely from well-tolerated seizures and mild encephalitis/encephalopathy concomitant with cerebellitis to death, corresponding to neurological manifestations ranging from benign convulsions and reversible white matter injury to fatal Reye’s syndrome (Lynch et al. Citation2001; Karampatsas et al. Citation2015) (). Seizures presenting as benign convulsions are the most commonly reported. Neurological manifestations of rotavirus may be underestimated as rotavirus stool levels in newborn infants presenting convulsion were considerably higher than the healthy control group or rotavirus-negative control groups, whereas co-presentation of convulsion and acute gastroenteritis in children is higher as expected when compared to other aetiologies (Herrmann et al. Citation1993; Wong Citation2001; Yeom et al. Citation2019). Rotavirus infection represents an independent risk factor for neonatal seizure increasing risk by four times (Yeom et al. Citation2019). Strikingly, in paediatric rotavirus gastroenteritis, the incidence of seizures ranges from 2 to 8% (Iturriza-Gómara et al. Citation2002; Lloyd et al. Citation2010; Pardo-Seco et al. Citation2015).
Supporting a neurological substrate for rotavirus replication is that rotavirus particles, antigens, antibodies and RNA have been detected in cerebrospinal fluid (CSF) (Wong et al. Citation1984; Keidan et al. Citation1992; Pager et al. Citation2000; Lynch et al. Citation2001; Iturriza-Gómara et al. Citation2002). Indeed, study showed that neurons can sustain infection with rhesus rotavirus (RRV), NSP4 protein being detectable in dendritic processes (Weclewicz et al. Citation1998). In vivo data in animals are more ambiguous but brain cell cultures from pigs and mice inoculated with heterologous RRV (MMU-18006, species A, serotype G3) or homologous murine strain (EDIM-5099) respectively, showed productive infection (Kraft Citation1958; Janke et al. Citation1988; Czech-Schmidt et al. Citation2001). Accordingly, in the USA and Spain, rotavirus vaccination has resulted in reduced incidence of paediatric seizures (Payne et al. Citation2014; Pardo-Seco et al. Citation2015; Burke et al. Citation2018), although later studies failed to detect such an effect (Biggart et al. Citation2018; Orrico-Sánchez et al. Citation2018; Gómez-Rial et al. Citation2019). Hence, the overall contribution of rotavirus neuronal infection as a trigger for seizures remains unclear.
Four hypotheses have been brought forward for explaining neurological manifestations of rotavirus infection (). The presence of rotavirus in the CSF, which is mostly documented by reverse transcription-polymerase chain reaction (RT-PCR) data (presence of viral genome), and the infectious capacity of neurons to sustain rotavirus infection points towards direct rotavirus-mediated neuronal cytotoxicity (Kraft Citation1958; Wong et al. Citation1984; Keidan et al. Citation1992; Czech-Schmidt et al. Citation2001; Lynch et al. Citation2001; Iturriza-Gómara et al. Citation2002; Ramig Citation2007; Nakano et al. Citation2011), but it also possible that the rotavirus presence signals the presence of other pathogens that mediate the actual neurotoxicity (e.g. zika virus, influenza virus, or adenovirus) (Karampatsas et al. Citation2015). A further alternative is that the neuronal damage is the consequence of circulating NSP4, possibly in conjunction with NO generation (DiFazio et al. Citation2007). NSP4 can act as a virporin and thus provoke Ca2+-mediated excitotoxicity (Hagbom et al. Citation2012; Citation2016; Crawford et al. Citation2017), whereas NO production (which is a reactive free radical (Goldwater et al. Citation2001)) may further provoke neuronal damage. Interestingly, a significant elevation of NO was observed in the spinal fluid of patients suffering from rotavirus-induced seizures (DiFazio et al. Citation2007). Finally, rotavirus-activated host immune responses may provoke neurological damage as well. A pilot study showed that the expression of monocyte chemoattractant protein-1 and macrophage inflammatory protein-1β was higher in rotavirus-infected newborns with white matter injury than in newborns without such damage or in healthy controls (Yeom et al. Citation2019). Another small study reported elevated levels of IL-6, IL-10 and IFN-γ and immune cells in the CSF of rotavirus-infected patients with mild encephalopathy (Miyata et al. Citation2012; Karampatsas et al. Citation2015). Thus the neurological manifestations of rotavirus infection may well relate to multiple aetiological mechanisms.
Hepatobiliary diseases
An increasing body of evidence relates rotavirus to acute and chronic liver disease and to cholestatic disease (Ramig Citation2007). Rotavirus-induced acute and chronic hepatitis usually results in liver dysfunction, and rotavirus-induced cholestasis often leads to obstructive jaundice. Biliary atresia (BA), characterized by perinatal progressive obliteration of the extrahepatic bile duct, is one of the most frequent causes of neonatal cholestasis and will progress as biliary cirrhosis and end-stage liver disease requiring liver transplantation (Shivakumar et al. Citation2004; Allen et al. Citation2007). A diagnosis of acute hepatitis, prompted by elevated alanine aminotransferase (ALT), aspartate aminotransferase (AST) and gammaglutamyl transferase (GGT) levels, in children with rotavirus-gastroenteritis has been reported () and associated with the presence of hepatic positivity for rotaviral non-structural proteins in immunostaining (Gilger et al. Citation1992; Teitelbaum and Daghistani Citation2007; Nakano et al. Citation2011). Especially, in immunocompromised or immunodeficient children with rotavirus infection, liver involvement is often obvious (Gilger et al. Citation1992; Ramig Citation2007). A significant association between rotavirus and cholestatic disease was also reported, in which species C rotavirus RNA was detected in liver biopsy samples of extrahepatic BA (EHBA) infants (Riepenhoff-Talty et al. Citation1996). Recently it was shown that human liver organoids are highly susceptible to simian rotavirus (SA11, species A, serotype G3) infection and sustain the entire life cycle of the virus (Chen et al. Citation2020). In the liver of severe combined immunodeficiency (SCID) mice and immunocompetent BALB/c mice, the heterologous RRV (MMU-18006) provoked hepatitis, the immunocompetent BALB/c mice more resistant to this effect, in line with human data (Uhnoo et al. Citation1990; Ramig Citation2007). Thus host immunity appears to be a critical factor with respect to the development of rotavirus-induced hepatobiliary diseases (Uhnoo et al. Citation1990; Shivakumar et al. Citation2004; Mack et al. Citation2006) (). Importantly, high incidence of cholestasis (over 80%) and mortality (over 90%) due to obstruction of extrahepatic bile ducts was observed in neonatal mice following inoculation of the animals with RRV (MMU-18006) and with an apparent tropism to the bile duct (Shivakumar et al. Citation2004; Ramig Citation2007). Furthermore, in neonatal BALB/c mice infected with two hepatobiliary-tropic RV strains (HCR-3 and RRV, species A), active virus replication was detected in the biliary tract and liver as early as two days after inoculation (Riepenhoff-Talty et al. Citation1993), and later jaundice, acholic stool and other hallmarks of BA were present as well (Riepenhoff-Talty et al. Citation1993; Petersen et al. Citation1997; Ramig Citation2007). In apparent agreement, transcriptomic analysis of BA infants finds evidence of ongoing inflammation and activation of IFN-γ-mediated antiviral immunity (Bezerra et al. Citation2002), whereas in experimental animals adoptive transfer of B cells into rotavirus-infected B cell-deficient mice was essential for biliary damage (Bednarek et al. Citation2018). Thus a role for rotavirus infection in the development of BA either through direct cytopathy or indirect through immunological damage have been proposed.
An underappreciated aspect with regard to the discussion on the role of rotavirus in BA development is that biliary and hepatic manifestations of the infection appear highly strain and context dependent. Whereas inoculation of experimental rodents with the bovine (WC3), human (Wa) strains or the murine strain EDIM-5099 provoked no sign of hepatobiliary disease (Uhnoo et al. Citation1990; Allen et al. Citation2007), in the same model the simian rotavirus strain (SA11-SM) produces hepatocyte infection but not cholangiocyte infection and the SA11-FM strain (identical to SA11-SM except for the presence of the bovine rotavirus VP4 protein gene) targets biliary epithelial cells causing bile duct obstruction and high mortality (). Furthermore, disease outcome in rotavirus-infected mouse models are highly age-dependent: whereas rotaviral infection of neonatal mice (<2 days of age) results in hepatobiliary inflammation and obstruction, such infection in adult mice is asymptomatic (Riepenhoff-Talty et al. Citation1993; Shivakumar et al. Citation2004; Mack et al. Citation2006; Hertel and Estes Citation2012). Experiments in which effect of rotavirus infection in foetal and adult liver organoids are contrasted may shed light on to which extent the outcome of cholangiocyte infection are host age mediated (Saxena et al. Citation2016; Ramani et al. Citation2018). Notably, immunization against rotavirus in female mice protects newborn mice from developing rotavirus-induced cholestasis and EHBA (Czech-Schmidt et al. Citation2001). It is thus well possible that rotavirus vaccination of pregnant women will substantially reduce the incidence of neonatal BA.
Type 1 diabetes
Type 1 diabetes (T1D) is an autoimmune disease characterized by the destruction of insulin-producing pancreatic β cells, and is frequently and also increasingly diagnosed in children in the USA (Rogers et al. Citation2017; Burke et al. Citation2020). Although the aetiology of T1D is not fully understood yet, links with different pathogens are well-recognized (Filippi and von Herrath Citation2008; Rewers and Ludvigsson Citation2016; Burke et al. Citation2020). Rotavirus has been proposed as an etiologic trigger for T1D (), but also for other autoimmune disease such as coeliac disease (Smatti et al. Citation2019; Burke et al. Citation2020; Gómez-Rial et al. Citation2020). Support for rotavirus as a potential causative agent in the development of T1D comes from the observation that incidence of T1D decreased by 3–14% in rotavirus-vaccinated children aged 0–4 years in the USA and Australia (Perrett et al. Citation2019; Burke et al. Citation2020; Gómez-Rial et al. Citation2020). However, Finnish studies in children up to 10 years and American studies in children with follow-up of 5–12 years, failed to detect association between rotavirus vaccination and T1D development (Vaarala et al. Citation2017; Hemming-Harlo et al. Citation2019; Burke et al. Citation2020; Glanz et al. Citation2020). Animal studies, however, largely support the idea that rotavirus infection can be a trigger of T1D. Both in vitro as well in neonates in vivo, infection by rotavirus of Non-Obese Diabetic (NOD) mouse islet cells has been convincingly demonstrated (Ramig Citation2007; Graham et al. Citation2008; Pane and Coulson Citation2015) and results in transient (pre-)diabetic symptoms like hyperglycaemia, pancreatic cell death and reduced insulin production (Honeyman et al. Citation2014). Mechanistically, this effect may linked to the spread of rotavirus in infected NOD mice to the pancreatic lymph nodes (PLN) and mesenteric lymph nodes (MLN) (Webster et al. Citation2013) where the infection leads to the activation of antigen presenting cells and accumulation of autoreactive lymphocytes (Graham et al. Citation2008; Pane et al. Citation2014; Pane and Coulson Citation2015), which may provoke T1D development (Burke et al. Citation2020) (). The induction of anti-islet autoimmunity may be further stimulated by similarity of the rotavirus VP7 protein to two T1D-associated autoantigens, glutamic acid decarboxylase (GAD65) and insulinoma antigen 2 (IA-2) protein. Support for this notion comes from the observation that the presence of anti-GAD65 antibody levels in children shows positive correlation with anti-rotavirus IgG levels (Burke et al. Citation2020). With the more widespread introduction of anti-virus vaccination around the globe, the overall contribution of rotavirus to the aetiology of T1D should become more evident.
Although a rare complication, various cases of acute pancreatitis, accompanied by diarrhoea, abdominal pain and elevated serum pancreatic enzymes, following an earlier rotavirus gastroenteritis have been reported in children (Nigro Citation1991; Parri et al. Citation2010; Basturk et al. Citation2017) (). The role for rotavirus in the pancreatitis is supported by the presence of stool rotavirus particles and the absence of other pathogens therein. Also, in two cases of pancreatitis-associated paediatric fatalities, rotavirus antigen and RNA was detected in the pancreas (Lynch et al. Citation2003; Ramig Citation2007). Hence, paediatricians should be aware of the possibility that severe rotavirus-mediated gastroenteritis can become complicated by the development of acute pancreatitis.
Respiratory illness
Spreading of rotavirus infection is classically attributed solely to fecal-oral transmission (Esona and Gautam Citation2015). Nevertheless, the possibility of a contribution of respiratory rotavirus transmission cannot be discounted (Goldwater et al. Citation1979). Indeed, occurrence of respiratory symptoms (rhinorrhea, nasal congestion, coughing, vomiting or pneumonia; ) shortly after or concomitant with rotavirus gastroenteritis appears common in infants and children (30–65%) (Goldwater et al. Citation1979; Gurwith et al. Citation1981; Santosham et al. Citation1983; Fragoso et al. Citation1986; Zhaori et al. Citation1991; Brouard et al. Citation2000; Sharma et al. Citation2002; Grimprel et al. Citation2008; Yu et al. Citation2012). Furthermore, rotavirus antigen was found in oropharyngeal, nasopharyngeal and tracheal aspirates (Yolken and Murphy Citation1982; Fragoso et al. Citation1986; Zhaori et al. Citation1991; Zheng et al. Citation1991), and RT-PCR detected rotavirus RNA in the lungs from a patient with fatal diarrhoea-associated disease (Lynch et al. Citation2003). Also, with the advent of metagenomics, the rotavirus genome is frequently found in tracheal aspirates or throat and nasal swabs from patients with respiratory tract infections, concurrently with bona-fide respiratory viruses (adenovirus, influenza A virus, respiratory syncytial virus and rhinovirus) and bacteria (CitationTaboada et al. 2014; Madi et al. Citation2018; Thi Kha Tu et al. Citation2020). In apparent agreement, in Sus scrofa intranasal inoculation with virulent human rotavirus (HRV, Wa) was not inferior to oral or gavage inoculation with regard to provoking diarrhoea, and viremia relative to oral or gavage-mediated inoculation, and provoked nasal viral shedding (Azevedo et al. Citation2005). In Bos bovis, colostrum-deprived and thus infection-prone calves were orally inoculated with the bovine rotaviruses (GARVs, KJ9-1, species A) and developed transient interstitial pneumonia accompanied by the presence of GARV antigen and viral RNA in the pneumocytes and lung lymphocytes (Kim et al. Citation2011). Analogously, in neonatal rats, replicating RRV was detected in alveolar macrophages and pneumocytes (Crawford et al. Citation2006). The latter study described that rotavirus antigen levels in the lower respiratory tract and stomach showed strong correlation and thus proposed that rotavirus was released into respiratory secretions and swallowed. Also in newborn mice, following murine rotavirus or heterologous RRV infection, viral RNA, NSP4 protein and viral particles were found in lung tissues (Fenaux et al. Citation2006), whereas it has also been shown that intranasal immunization of mice with inactivated RRV protects against subsequent rotavirus challenge (Coffin and Clark Citation2001). Intriguingly, oral immunization was not protective, possibly suggesting alternative handling of the rotavirus vaccine by the bronchial and intestinal mucosal immune system. In toto, there seems to be a contribution of the respiratory compartment in rotavirus-provoked pathogenesis, even while it remains unclear whether respiratory illness provokes susceptibility to rotavirus infection or rotavirus infection can provoke respiratory illness (CitationTaboada et al. 2014; Madi et al. Citation2018; Thi Kha Tu et al. Citation2020) ().
Other extra-intestinal complications
A number of case reports have described additional extra-intestinal complications of rotavirus infection, including myocarditis, renal failure and thrombocytopenia (Ramig Citation2007) ( and ). Indeed, both autopsy examinations and animal studies have described the presence of rotavirus RNA, antigens and replication in heart and kidney (Cioc and Nuovo Citation2002; Lynch et al. Citation2003; Crawford et al. Citation2006; Ramig Citation2007). Post-mortem histopathological reports showed that cardiac rotavirus infection could contribute to hypertrophic cardiomyopathy with focal disorganized myocardial architecture, myocyte necrosis and myocarditis (Grech et al. Citation2001; Cioc and Nuovo Citation2002; Nakano et al. Citation2011). Prominent lymphocytic infiltration was found in the myocardium in cases of rotavirus myocarditis, suggesting that antiviral immunity may provoke myocardial damage (Cioc and Nuovo Citation2002) and indeed rotavirus infection has been associated to increased Creatine Kinase-MB signalling damage to the heart during infection (Zheng et al. Citation2017).
With respect to renal manifestations, interpretation is complicated by that the rotavirus diarrhoea-induced dehydration can lead to pre- and post-renal failure and thus renal problems following infection may not reflect direct infection of the kidneys (Fujinaga et al. Citation2005; Ashida et al. Citation2012; Shirasu et al. Citation2015; Kira et al. Citation2016; Tsukida et al. Citation2018). Nevertheless, although direct rotavirus damage to renal epithelial cells has not been reported, kidney lesions due to cellular degeneration and mild infiltration of mononuclear cells have been identified in mice infected with rotavirus (Kashyap et al. Citation2018). The fact that monkey kidney cells (secondary and permanent cell lines) are highly susceptible for RV infection in vitro is compatible with the view that kidneys can be productively infected in vivo (Ward et al. Citation1984; Gilger et al. Citation1992; Lynch et al. Citation2003; Crawford et al. Citation2006; Fenaux et al. Citation2006).
In addition to the kidneys and the heart, also the bone marrow may be affected following rotavirus infection. Thrombocytopenia and significantly lower mean platelet volume (MPV) are more common in children with rotavirus gastroenteritis than in controls (Mete et al. Citation2014; Tanju et al. Citation2014; Ai et al. Citation2016), but as there is no significant association between MPV and gastroenteritis score (Mete et al. Citation2014; Tanju et al. Citation2014), the relation may be indirect, for instance relating to disturbed vitamin uptake.
Conclusions
As the leading cause of severe acute gastroenteritis, rotavirus infection has a substantial effect on morbidity and mortality in infants and young children. Rotavirus primarily infects the intestinal enterocytes and induces secretory-driven watery diarrhoea. In addition, both human and animal experimentation demonstrates that extra-intestinal tissue can be susceptible to rotavirus infection in turn provoking further pathology, which may be the consequence of virus-mediated destruction of the cells involved, or indirect secondary to anti-viral immune responses. Nevertheless, the involvement of rotavirus in extra-intestinal tissue damage is much better documented in animal models than in humans, and there are gaps in the understanding of mechanisms of pathogenesis. It is to be expected that together with rotavirus-mediated gastroenteritis such extra-intestinal manifestations will become less prevalent as consequence from the introduction of anti-rotavirus vaccination. For now, however, clinicians, particularly paediatricians caring for rotavirus-infected children should be aware of the possible extra-intestinal complications of rotavirus infection.
Author contributions
Q.P. and Z.M. designed and directed the project; Z.D. wrote the manuscript with support from M.P., Y.S., G.Z. and Y.X.; X.F. and X.Y. searched and reviewed the literatures, and they aided in interpreting the results. Z.D., Y.S., X.F. and X.Y. assessed the screened literatures; Z.M. designed the figures; G.Z. and Y.X. drew the figures; Q.P. and M.P. directed the revision of the manuscript; all authors provided critical feedback and contributed to the final version of the manuscript.
Acknowledgments
The authors thank freepik and edraw for their assistance with regard to graphic illustrations.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Ai Q, Yin J, Chen S, Qiao L, Luo N. 2016. Rotavirus-associated immune thrombocytopenic purpura in children: a retrospective study. Exp Ther Med. 12:2187–2190.
- Aliabadi N, Antoni S, Mwenda JM, Weldegebriel G, Biey JNM, Cheikh D, Fahmy K, Teleb N, Ashmony HA, Ahmed H, et al. 2019. Global impact of rotavirus vaccine introduction on rotavirus hospitalisations among children under 5 years of age, 2008-16: findings from the Global Rotavirus Surveillance Network. Lancet Glob Health. 7:e893–e903.
- Allen SR, Jafri M, Donnelly B, McNeal M, Witte D, Bezerra J, Ward R, Tiao GM. 2007. Effect of rotavirus strain on the murine model of biliary atresia. J Virol. 81:1671–1679.
- Ashida A, Fujieda M, Ohta K, Nakakura H, Matsumura H, Morita T, Igarashi T, Tamai H. 2012. Clinical characteristics of obstructive uropathy associated with rotavirus gastroenteritis in Japan. Clin Nephrol. 77:49–54.
- Azevedo MS, Yuan L, Jeong KI, Gonzalez A, Nguyen TV, Pouly S, Gochnauer M, Zhang W, Azevedo A, Saif LJ, et al. 2005. Viremia and nasal and rectal shedding of rotavirus in gnotobiotic pigs inoculated with Wa human rotavirus. J Virol. 79:5428–5436.
- Bányai K, Estes MK, Martella V, Parashar UD. 2018. Viral gastroenteritis. Lancet. 392:175–186.
- Baqui AH, Black RE, El Arifeen S, Yunus M, Chakraborty J, Ahmed S, Vaughan JP. 2002. Effect of zinc supplementation started during diarrhoea on morbidity and mortality in Bangladeshi children: community randomised trial. BMJ. 325:1059.
- Basturk A, Artan R, Yilmaz A. 2017. Rotavirus gastroenteritis and a rare case accompanying acute pancreatitis. Prz Gastroenterol. 12:68–69.
- Bednarek J, Traxinger B, Brigham D, Roach J, Orlicky D, Wang D, Pelanda R, Mack CL. 2018. Cytokine-producing B cells promote immune-mediated bile duct injury in murine biliary atresia. Hepatology. 68:1890–1904.
- Bezerra JA, Tiao G, Ryckman FC, Alonso M, Sabla GE, Shneider B, Sokol RJ, Aronow BJ. 2002. Genetic induction of proinflammatory immunity in children with biliary atresia. Lancet. 360:1653–1659.
- Biggart R, Finn A, Marlow R. 2018. Lack of impact of rotavirus vaccination on childhood seizure hospitalizations in England – an interrupted time series analysis. Vaccine. 36:4589–4592.
- Blutt SE, Conner ME. 2007. Rotavirus: to the gut and beyond! Curr Opin Gastroenterol. 23:39–43.
- Blutt SE, Kirkwood CD, Parreño V, Warfield KL, Ciarlet M, Estes MK, Bok K, Bishop RF, Conner ME. 2003. Rotavirus antigenaemia and viraemia: a common event? Lancet. 362:1445–1449.
- Blutt SE, Matson DO, Crawford SE, Staat MA, Azimi P, Bennett BL, Piedra PA, Conner ME. 2007. Rotavirus antigenemia in children is associated with viremia. PLoS Med. 4:e121.
- Brouard J, Freymuth F, Vabret A, et al. 2000. Viral co-infections in immunocompetent infants with bronchiolitis: prospective epidemiologic study] Co-infections virales lors des bronchiolites du nourrisson immunocompétent: étude prospective épidémiologique. Arch Pediatr. 7:531s–535s.
- Burke RM, Tate JE, Dahl RM, Aliabadi N, Parashar UD. 2018. Rotavirus vaccination is associated with reduced seizure hospitalization risk among commercially insured US children. Clin Infect Dis. 67:1614–1616.
- Burke RM, Tate JE, Dahl RM, Saydah S, Imperatore G, Gregg EW, Parashar UD. 2020. Rotavirus Vaccination and Type 1 Diabetes Risk Among US Children With Commercial Insurance. JAMA Pediatr. 174:383–385.
- Burke RM, Tate JE, Jiang B, et al. 2020. Rotavirus and type 1 diabetes-is there a connection? A synthesis of the evidence. J Infect Dis. 222:1076–1083.
- Burke RM, Tate JE, Kirkwood CD, Steele AD, Parashar UD. 2019. Current and new rotavirus vaccines. Curr Opin Infect Dis. 32:435–444.
- Burnett E, Parashar UD, Tate JE. 2020. Associations of intussusception with adenovirus, rotavirus, and other pathogens: a review of the literature. Pediatr Infect Dis J. 39:1127–1130.
- Burnett E, Parashar UD, Tate JE. 2020. Real-world effectiveness of rotavirus vaccines, 2006-19: a literature review and meta-analysis. Lancet Glob Health. 8:e1195–e1202.
- Chen S, Li P, Wang Y, Yin Y, de Ruiter PE, Verstegen MMA, Peppelenbosch MP, van der Laan LJW, Pan Q. 2020. Rotavirus infection and cytopathogenesis in human biliary organoids potentially recapitulate biliary atresia development. mBio. 11:e01968-20.
- Chen SM, Lin CP, Tsai JD, Chao YH, Sheu JN. 2014. The significance of serum and fecal levels of interleukin-6 and interleukin-8 in hospitalized children with acute rotavirus and norovirus gastroenteritis. Pediatr Neonatol. 55:120–126.
- Cioc AM, Nuovo GJ. 2002. Histologic and in situ viral findings in the myocardium in cases of sudden, unexpected death. Mod Pathol. 15:914–922.
- Coffin SE, Clark SL. 2001. Induction of intestinal rotavirus-specific antibodies in respiratory, but not gut, lymphoid tissues following mucosal immunization of mice with inactivated rotavirus. Virology. 291:235–240.
- Colbère-Garapin F, Martin-Latil S, Blondel B, Mousson L, Pelletier I, Autret A, François A, Niborski V, Grompone G, Catonnet G, et al. 2007. Prevention and treatment of enteric viral infections: possible benefits of probiotic bacteria. Microbes Infect. 9:1623–1631.
- Coulson BS, Witterick PD, Tan Y, Hewish MJ, Mountford JN, Harrison LC, Honeyman MC. 2002. Growth of rotaviruses in primary pancreatic cells. J Virol. 76:9537–9544.
- Crawford SE, Patel DG, Cheng E, Berkova Z, Hyser JM, Ciarlet M, Finegold MJ, Conner ME, Estes MK. 2006. Rotavirus viremia and extraintestinal viral infection in the neonatal rat model. J Virol. 80:4820–4832.
- Crawford SE, Ramani S, Tate JE, Parashar UD, Svensson L, Hagbom M, Franco MA, Greenberg HB, O'Ryan M, Kang G, et al. 2017. Rotavirus infection. Nat Rev Dis Primers. 3:17083–17083.
- Czech-Schmidt G, Verhagen W, Szavay P, Leonhardt J, Petersen C. 2001. Immunological gap in the infectious animal model for biliary atresia. J Surg Res. 101:62–67.
- Dalgic N, Sancar M, Bayraktar B, Pullu M, Hasim O. 2011. Probiotic, zinc and lactose-free formula in children with rotavirus diarrhea: are they effective? Pediatr Int. 53:677–682.
- Dharakul T, Riepenhoff-Talty M, Albini B, Ogra PL. 1988. Distribution of rotavirus antigen in intestinal lymphoid tissues: potential role in development of the mucosal immune response to rotavirus. Clin Exp Immunol. 74:14–19.
- DiFazio MP, Braun L, Freedman S, Hickey P. 2007. Rotavirus-induced seizures in childhood. J Child Neurol. 22:1367–1370.
- Esona MD, Gautam R. 2015. Rotavirus. Clin Lab Med. 35:363–391.
- Fenaux M, Cuadras MA, Feng N, Jaimes M, Greenberg HB. 2006. Extraintestinal spread and replication of a homologous EC rotavirus strain and a heterologous rhesus rotavirus in BALB/c mice. JVI. 80:5219–5232.
- Filippi CM, von Herrath MG. 2008. Viral trigger for type 1 diabetes: pros and cons. Diabetes. 57:2863–2871.
- Fragoso M, Kumar A, Murray DL. 1986. Rotavirus in nasopharyngeal secretions of children with upper respiratory tract infections. Diagn Microbiol Infect Dis. 4:87–88.
- Fujinaga S, Kaneko K, Ohtomo Y, Takada M, Kobayashi K, Tada M, Yamashiro Y. 2005. Acute renal failure due to obstructive uric acid stones associated with rotavirus gastroenteritis. Pediatr Nephrol. 20:239–240.
- Fukuda S, Kishi K, Yasuda K, Sejima H, Yamaguchi S. 2009. Rotavirus-associated encephalopathy with a reversible splenial lesion. Pediatric Neurology. 40:131–133.
- Gilger MA, Matson DO, Conner ME, Rosenblatt HM, Finegold MJ, Estes MK. 1992. Extraintestinal rotavirus infections in children with immunodeficiency. J Pediatr. 120:912–917.
- Glanz JM, Clarke CL, Xu S, Daley MF, Shoup JA, Schroeder EB, Lewin BJ, McClure DL, Kharbanda E, Klein NP, et al. 2020. Association between rotavirus vaccination and type 1 diabetes in children. JAMA Pediatr. 174:455–462.
- Goldwater PN, Chrystie IL, Banatvala JE. 1979. Rotaviruses and the respiratory tract. Br Med J. 2:1551.
- Goldwater PN, Rowland K, Thesinger M, Abbott K, Grieve A, Palombo EA, Masendycz PJ, Wilkinson I, Bear J. 2001. Rotavirus encephalopathy: pathogenesis reviewed. J Paediatr Child Health. 37:206–209.
- Gómez-Rial J, Rivero-Calle I, Salas A, Martinón-Torres F. 2020. Rotavirus and autoimmunity. J Infect. 81:183–189.
- Gómez-Rial J, Sánchez-Batán S, Rivero-Calle I, Pardo-Seco J, Martinón-Martínez JM, Salas A, Martinón-Torres F. 2019. Rotavirus infection beyond the gut. Infect Drug Resist. 12:55–64.
- Graham KL, O'Donnell JA, Tan Y, Sanders N, Carrington EM, Allison J, Coulson BS. 2007. Rotavirus infection of infant and young adult nonobese diabetic mice involves extraintestinal spread and delays diabetes onset. J Virol. 81:6446–6458.
- Graham KL, Sanders N, Tan Y, Allison J, Kay TWH, Coulson BS. 2008. Rotavirus infection accelerates type 1 diabetes in mice with established insulitis. JVI. 82:6139–6149.
- Grech V, Calvagna V, Falzon A, Mifsud A. 2001. Fatal, rotavirus-associated myocarditis and pneumonitis in a 2-year-old boy. Ann Trop Paediatr. 21:147–148.
- Greenberg HB, Clark HF, Offit PA. 1994. Rotavirus pathology and pathophysiology. Curr Top Microbiol Immunol. 185:255–283.
- Grimprel E, Rodrigo C, Desselberger U. 2008. Rotavirus disease: impact of coinfections. Pediatr Infect Dis J. 27:S3–S10.
- Gurwith M, Wenman W, Hinde D, Feltham S, Greenberg H. 1981. A prospective study of rotavirus infection in infants and young children. J Infect Dis. 144:218–224.
- Haffejee IE, Moosa A. 1990. Rotavirus studies in Indian (Asian) South African infants with acute gastro-enteritis: II. Clinical aspects and outcome. Ann Trop Paediatr. 10:245–254.
- Hagbom M, De Faria FM, Winberg ME, Westerberg S, Nordgren J, Sharma S, Keita ÅV, Loitto V, Magnusson KE, Svensson L, et al. 2020. Neurotrophic factors protect the intestinal barrier from rotavirus insult in mice. mBio. 11:31964731.
- Hagbom M, Istrate C, Engblom D, Karlsson T, Rodriguez-Diaz J, Buesa J, Taylor JA, Loitto VM, Magnusson KE, Ahlman H, et al. 2011. Rotavirus stimulates release of serotonin (5-HT) from human enterochromaffin cells and activates brain structures involved in nausea and vomiting. PLoS Pathog. 7:e1002115.
- Hagbom M, Sharma S, Lundgren O, Svensson L. 2012. Towards a human rotavirus disease model. Curr Opin Virol. 2:408–418.
- Hagbom M, Svensson L, et al. 2016. Chapter 2.6 – Rotavirus disease mechanisms. In: Svensson L, Desselberger U, Greenberg HB, editors. Viral gastroenteritis. Boston (MA): Academic Press; p. 189–218.
- Hagbom M, Svensson L. 2016. Rotavirus disease mechanisms. In: Svensson L, Desselberger U, Greenberg HB, Estes MK, editors. Viral gastroenteritis. London (UK): Academic Press; p. 189–218.
- Hartman S, Brown E, Loomis E, Russell HA. 2019. Gastroenteritis in children. Am Fam Physician. 99:159–165.
- Hemming-Harlo M, Lähdeaho ML, Mäki M, Vesikari T. 2019. Rotavirus vaccination does not increase type 1 diabetes and may decrease celiac disease in children and adolescents. Pediatr Infect Dis J. 38:539–541.
- Herrmann B, Lawrenz-Wolf B, Seewald C, et al. 1993. [5th day convulsions of the newborn infant in rotavirus infections] 5-Tages-Krämpfe des Neugeborenen bei Rotavirusinfektionen. Monatsschr Kinderheilkd. 141:120–123.
- Hertel PM, Estes MK. 2012. Rotavirus and biliary atresia: can causation be proven? Curr Opin Gastroenterol. 28:10–17.
- Hjelt K, Krasilnikoff PA, Grauballe PC, Rasmussen SW. 1985. Clinical features in hospitalised children with acute gastroenteritis. Does the rotavirus syndrome exist? Acta Paediatr Scand. 74:96–101.
- Honeyman MC, Laine D, Zhan Y, Londrigan S, Kirkwood C, Harrison LC. 2014. Rotavirus infection induces transient pancreatic involution and hyperglycemia in weanling mice. PLoS One. 9:e106560.
- Hongou K, Konishi T, Yagi S, Araki K, Miyawaki T. 1998. Rotavirus encephalitis mimicking afebrile benign convulsions in infants. Pediatr Neurol. 18:354–357.
- Hyser JM, Collinson-Pautz MR, Utama B, Estes MK. 2010. Rotavirus disrupts calcium homeostasis by NSP4 viroporin activity. mBio. 1:e00265-10.
- Hyser JM, Utama B, Crawford SE, Estes MK. 2012. Genetic divergence of rotavirus nonstructural protein 4 results in distinct serogroup-specific viroporin activity and intracellular punctate structure morphologies. J Virol. 86:4921–4934.
- Istrate C, Hagbom M, Vikström E, Magnusson KE, Svensson L. 2014. Rotavirus infection increases intestinal motility but not permeability at the onset of diarrhea. J Virol. 88:3161–3169.
- Iturriza-Gómara M, Auchterlonie IA, Zaw W, Molyneaux P, Desselberger U, Gray J. 2002. Rotavirus gastroenteritis and central nervous system (CNS) infection: characterization of the VP7 and VP4 genes of rotavirus strains isolated from paired fecal and cerebrospinal fluid samples from a child with CNS disease. J Clin Microbiol. 40:4797–4799.
- Janke BH, Morehouse LG, Solorzano RF. 1988. Single and mixed infections of neonatal pigs with rotaviruses and enteroviruses: virological studies. Can J Vet Res. 52:360–363.
- Karampatsas K, Spyridou C, Morrison IR, Tong CYW, Prendergast AJ. 2015. Rotavirus-associated mild encephalopathy with a reversible splenial lesion (MERS)-case report and review of the literature. BMC Infect Dis. 15:446.
- Kashyap G, Singh R, Malik YS, Agrawal RK, Singh KP, Kumar P, Sahoo M, Gupta D, Singh R. 2018. Experimental bovine rotavirus-A (RV-A)infection causes intestinal and extra-intestinal pathology in suckling mice. Microb Pathog. 121:22–26.
- Keidan I, Shif I, Keren G, Passwell JH. 1992. Rotavirus encephalopathy: evidence of central nervous system involvement during rotavirus infection. Pediatr Infect Dis J. 11:773–775.
- Kim HJ, Park JG, Matthijnssens J, Lee JH, Bae YC, Alfajaro MM, Park SI, Kang MI, Cho KO. 2011. Intestinal and extra-intestinal pathogenicity of a bovine reassortant rotavirus in calves and piglets. Vet Microbiol. 152:291–303.
- Kira S, Mitsui T, Zakoji H, Aoki T, Sawada N, Miyamoto T, Takeda M. 2016. Postrenal failure due to urinary stones associated with acute viral gastroenteritis: three case reports. Case Rep Urol. 2016:1375923.
- Köhler T, Erben U, Wiedersberg H, et al. 1990. [Histological findings of the small intestinal mucosa in rotavirus infections in infants and young children] Histologische Befunde der Dünndarmschleimhaut bei Rotavirusinfektionen im Säuglings- und Kleinkindalter. Kinderarztl Prax. 58:323–327.
- Kordasti S, Sjövall H, Lundgren O, et al. 2004. Serotonin and vasoactive intestinal peptide antagonists attenuate rotavirus diarrhoea. Gut. 53:952–957.
- Kovacs A, Chan L, Hotrakitya C, Overturf G, Portnoy B. 1986. Serum transaminase elevations in infants with rotavirus gastroenteritis. J Pediatr Gastroenterol Nutr. 5:873–877.
- Kraft LM. 1958. Observations on the control and natural history of epidemic diarrhea of infant mice (EDIM). Yale J Biol Med. 31:121–137.
- Laizane G, Smane L, Nokalna I, Gardovska D, Feemster KA. 2019. Rotavirus-associated seizures and reversible corpus callosum lesion. Acta Med Litu. 26:113–117.
- Leung AK, Kellner JD, Davies HD. 2005. Rotavirus gastroenteritis. Adv Ther. 22:476–487.
- Li ST, Grossman DC, Cummings P. 2007. Loperamide therapy for acute diarrhea in children: systematic review and meta-analysis. PLoS Med. 4:e98.
- Lloyd MB, Lloyd JC, Gesteland PH, Bale JF. 2010. Rotavirus gastroenteritis and seizures in young children. Pediatr Neurol. 42:404–408.
- Lu HL, Ding Y, Goyal H, Xu HG. 2019. Association between rotavirus vaccination and risk of intussusception among neonates and infants: a systematic review and meta-analysis. JAMA Netw Open. 2:e1912458.
- Lundgren O, Svensson L. 2001. Pathogenesis of rotavirus diarrhea. Microbes Infect. 3:1145–1156.
- Lynch M, Lee B, Azimi P, Gentsch J, Glaser C, Gilliam S, Chang H‐GH, Ward R, Glass RI. 2001. Rotavirus and central nervous system symptoms: cause or contaminant? Case reports and review. Clin Infect Dis. 33:932–938.
- Lynch M, Shieh WJ, Tatti K, Gentsch JR, Harris TF, Jiang B, Guarner J, Bresee JS, Greenwald M, Cullen S, et al. 2003. The pathology of rotavirus-associated deaths, using new molecular diagnostics. Clin Infect Dis. 37:1327–1333.
- Mack CL, Tucker RM, Lu BR, Sokol RJ, Fontenot AP, Ueno Y, Gill RG. 2006. Cellular and humoral autoimmunity directed at bile duct epithelia in murine biliary atresia. Hepatology. 44:1231–1239.
- Madi N, Al-Nakib W, Mustafa AS, Habibi N. 2018. Metagenomic analysis of viral diversity in respiratory samples from patients with respiratory tract infections in Kuwait. J Med Virol. 90:412–420.
- Matthijnssens J, Ciarlet M, Heiman E, Arijs I, Delbeke T, McDonald SM, Palombo EA, Iturriza-Gómara M, Maes P, Patton JT, et al. 2008. Full genome-based classification of rotaviruses reveals a common origin between human Wa-Like and porcine rotavirus strains and human DS-1-like and bovine rotavirus strains. J Virol. 82:3204–3219.
- Mete E, Akelma AZ, Cizmeci MN, Bozkaya D, Kanburoglu MK. 2014. Decreased mean platelet volume in children with acute rotavirus gastroenteritis. Platelets. 25:51–54.
- Miyata R, Tanuma N, Hayashi M, Imamura T, Takanashi JI, Nagata R, Okumura A, Kashii H, Tomita S, Kumada S, et al. 2012. Oxidative stress in patients with clinically mild encephalitis/encephalopathy with a reversible splenial lesion (MERS). Brain Dev. 34:124–127.
- Mormile R. 2016. Severe gastroenteritis and acute pancreatitis following rotavirus infection in children: the age-related failure of IFN-γ? Immunol Lett. 175:58–59.
- Mossel EC, Ramig RF. 2003. A lymphatic mechanism of rotavirus extraintestinal spread in the neonatal mouse. J Virol. 77:12352–12356.
- Nakano I, Taniguchi K, Ishibashi-Ueda H, Maeno Y, Yamamoto N, Yui A, Komoto S, Wakata Y, Matsubara T, Ozaki N, et al. 2011. Sudden death from systemic rotavirus infection and detection of nonstructural rotavirus proteins. J Clin Microbiol. 49:4382–4385.
- Nigro G. 1991. Pancreatitis with hypoglycemia-associated convulsions following rotavirus gastroenteritis. J Pediatr Gastroenterol Nutr. 12:280–282.
- Nishimura S, Ushijima H, Nishimura S, Shiraishi H, Kanazawa C, Abe T, Kaneko K, Fukuyama Y. 1993. Detection of rotavirus in cerebrospinal fluid and blood of patients with convulsions and gastroenteritis by means of the reverse transcription polymerase chain reaction. Brain Dev. 15:457–459.
- Operario DJ, Platts-Mills JA, Nadan S, Page N, Seheri M, Mphahlele J, Praharaj I, Kang G, Araujo IT, Leite JPG, et al. 2017. Etiology of severe acute watery diarrhea in children in the Global Rotavirus Surveillance Network using quantitative polymerase chain reaction. J Infect Dis. 216:220–227.
- Orrico-Sánchez A, López-Lacort M, Muñoz-Quiles C, Díez-Domingo J. 2018. Lack of impact of rotavirus vaccines on seizure-related hospitalizations in children under 5 years old in Spain. Hum Vaccin Immunother. 14:1534–1538.
- Osborne MP, Haddon SJ, Spencer AJ, Collins J, Starkey WG, Wallis TS, Clarke GJ, Worton KJ, Candy DC, Stephen J, et al. 1988. An electron microscopic investigation of time-related changes in the intestine of neonatal mice infected with murine rotavirus. J Pediatr Gastroenterol Nutr. 7:236–248.
- Pager C, Steele D, Gwamanda P, Driessen M. 2000. A neonatal death associated with rotavirus infection–detection of rotavirus dsRNA in the cerebrospinal fluid. S Afr Med J. 90:364–365.
- Pane JA, Coulson BS. 2015. Lessons from the mouse: potential contribution of bystander lymphocyte activation by viruses to human type 1 diabetes. Diabetologia. 58:1149–1159.
- Pane JA, Webster NL, Zufferey C, Coulson BS. 2014. Rotavirus acceleration of murine type 1 diabetes is associated with increased MHC class I-restricted antigen presentation by B cells and elevated proinflammatory cytokine expression by T cells. Virus Res. 179:73–84.
- Parashar UD, Nelson EA, Kang G. 2013. Diagnosis, management, and prevention of rotavirus gastroenteritis in children. BMJ. 347:f7204.
- Pardo-Seco J, Cebey-López M, Martinón-Torres N, Salas A, Gómez-Rial J, Rodriguez-Tenreiro C, Martinón-Sánchez JM, Martinón-Torres F. 2015. Impact of rotavirus vaccination on childhood hospitalization for seizures. Pediatr Infect Dis J. 34:769–773.
- Parri N, Innocenti L, Collini S, Bechi F, Mannelli F. 2010. Acute pancreatitis due to rotavirus gastroenteritis in a child. Pediatr Emerg Care. 26:592–593.
- Payne DC, Baggs J, Zerr DM, Klein NP, Yih K, Glanz J, Curns AT, Weintraub E, Parashar UD. 2014. Protective association between rotavirus vaccination and childhood seizures in the year following vaccination in US children. Clin Infect Dis. 58:173–177.
- Perrett KP, Jachno K, Nolan TM, Harrison LC. 2019. Association of rotavirus vaccination with the incidence of type 1 diabetes in children. JAMA Pediatr. 173:280–282.
- Petersen C, Biermanns D, Kuske M, Schäkel K, Meyer-Junghänel L, Mildenberger H. 1997. New aspects in a murine model for extrahepatic biliary atresia. J Pediatr Surg. 32:1190–1195.
- Ramani S, Crawford SE, Blutt SE, Estes MK. 2018. Human organoid cultures: transformative new tools for human virus studies. Curr Opin Virol. 29:79–86.
- Ramig RF. 2004. Pathogenesis of intestinal and systemic rotavirus infection. J Virol. 78:10213–10220.
- Ramig RF. 2007. Systemic rotavirus infection. Expert Rev anti Infect Ther. 5:591–612.
- Rautanen T, Kurki S, Vesikari T. 1997. Randomised double blind study of hypotonic oral rehydration solution in diarrhoea. Arch Dis Child. 76:272–274.
- Rewers M, Ludvigsson J. 2016. Environmental risk factors for type 1 diabetes. Lancet. 387:2340–2348.
- Reynolds DJ, Hall GA, Debney TG, Parsons KR. 1985. Pathology of natural rotavirus infection in clinically normal calves. Res Vet Sci. 38:264–269.
- Riepenhoff-Talty M, Gouvea V, Evans MJ, Svensson L, Hoffenberg E, Sokol RJ, Uhnoo I, Greenberg SJ, Schakel K, Zhaori G, et al. 1996. Detection of group C rotavirus in infants with extrahepatic biliary atresia. J Infect Dis. 174:8–15.
- Riepenhoff-Talty M, Schaekel K, Clark HF, Mueller W, Uhnoo I, Rossi T, Fisher J, Ogra PL. 1993. Group A rotaviruses produce extrahepatic biliary obstruction in orally inoculated newborn mice. Pediatr Res. 33:394–399.
- Robinson CG, Hernanz-Schulman M, Zhu Y, Griffin MR, Gruber W, Edwards KM. 2004. Evaluation of anatomic changes in young children with natural rotavirus infection: is intussusception biologically plausible? J Infect Dis. 189:1382–1387.
- Rodriguez-Calvo T, Sabouri S, Anquetil F, von Herrath MG. 2016. The viral paradigm in type 1 diabetes: who are the main suspects? Autoimmun Rev. 15:964–969.
- Rogers MAM, Basu T, Kim C. 2019. Lower incidence rate of type 1 diabetes after receipt of the rotavirus vaccine in the United States, 2001-2017. Sci Rep. 9:7727.
- Rogers MAM, Kim C, Banerjee T, Lee JM. 2017. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. BMC Med. 15:199.
- Santosham M, Yolken RH, Quiroz E, Dillman L, Oro G, Reeves WC, Sack RB. 1983. Detection of rotavirus in respiratory secretions of children with pneumonia. J Pediatr. 103:583–585.
- Saxena K, Blutt SE, Ettayebi K, Zeng XL, Broughman JR, Crawford SE, Karandikar UC, Sastri NP, Conner ME, Opekun AR, et al. 2016. Human intestinal enteroids: a new model to study human rotavirus infection, host restriction, and pathophysiology. J Virol. 90:43–56.
- Sharma R, Hudak ML, Premachandra BR, Stevens G, Monteiro CB, Bradshaw JA, Kaunitz AM, Hollister RA. 2002. Clinical manifestations of rotavirus infection in the neonatal intensive care unit. Pediatr Infect Dis J. 21:1099–1105.
- Shaw DP, Morehouse LG, Solorzano RF. 1989. Rotavirus replication in colostrum-fed and colostrum-deprived pigs. Am J Vet Res. 50:1966–1970.
- Shepherd RW, Butler DG, Cutz E, Gall DG, Hamilton JR. 1979. The mucosal lesion in viral enteritis. Extent and dynamics of the epithelial response to virus invasion in transmissible gastroenteritis of piglets. Gastroenterology. 76:770–777.
- Shirasu A, Ashida A, Matsumura H, Nakakura H, Tamai H. 2015. Clinical characteristics of rotavirus gastroenteritis with urinary crystals. Pediatr Int. 57:917–921.
- Shivakumar P, Campbell KM, Sabla GE, Miethke A, Tiao G, McNeal MM, Ward RL, Bezerra JA. 2004. Obstruction of extrahepatic bile ducts by lymphocytes is regulated by IFN-gamma in experimental biliary atresia. J Clin Invest. 114:322–329.
- Simsek C, Corman VM, Everling HU, Lukashev AN, Rasche A, Maganga GD, Binger T, Jansen D, Beller L, Deboutte W, et al. 2021. At least seven distinct rotavirus genotype constellations in bats with evidence of reassortment and zoonotic transmissions. mBio. 12:e02755-20.
- Smatti MK, Cyprian FS, Nasrallah GK, Al Thani AA, Almishal RO, Yassine HM. 2019. Viruses and autoimmunity: a review on the potential interaction and molecular mechanisms. Viruses. 11:762.
- Taboada B, Espinoza MA, Isa P, Aponte FE, Arias-Ortiz MA, Monge-Martínez J, Rodríguez-Vázquez R, Díaz-Hernández F, Zárate-Vidal F, Wong-Chew RM, et al. 2014. Is there still room for novel viral pathogens in pediatric respiratory tract infections? PLoS One. 9:e113570.
- Takanashi J, Miyamoto T, Ando N, Kubota T, Oka M, Kato Z, Hamano S, Hirabayashi S, Kikuchi M, Barkovich AJ, et al. 2010. Clinical and radiological features of rotavirus cerebellitis. AJNR Am J Neuroradiol. 31:1591–1595.
- Tanju C, Ekrem G, Berksoy Emel A, et al. 2014. Mean platelet volume as a negative marker of inflammation in children with rotavirus gastroenteritis. Iran J Pediatr. 24:617–622.
- Tate JE, Burton AH, Boschi-Pinto C, et al. 2016. Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 62:S96–S105.
- Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD, WHO-coordinated Global Rotavirus Surveillance Network. 2012. 2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 12:136–141.
- Teitelbaum JE, Daghistani R. 2007. Rotavirus causes hepatic transaminase elevation. Dig Dis Sci. 52:3396–3398.
- Thi Kha Tu N, Thi Thu Hong N, Thi Han Ny N, My Phuc T, Thi Thanh Tam P, Doorn H. R v, Dang Trung Nghia H, Thao Huong D, An Han D, Thi Thu Ha L, et al. 2020. The virome of acute respiratory diseases in individuals at risk of zoonotic infections. Viruses. 12:960.
- Trask SD, McDonald SM, Patton JT. 2012. Structural insights into the coupling of virion assembly and rotavirus replication. Nat Rev Microbiol. 10:165–177.
- Troeger C, Khalil IA, Rao PC, Cao S, Blacker BF, Ahmed T, Armah G, Bines JE, Brewer TG, Colombara DV, et al. 2018. Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA Pediatr. 172:958–965.
- Tsukida K, Goto M, Yamaguchi N, Imagawa T, Tamura D, Yamagata T. 2018. Rotavirus gastroenteritis-associated urinary tract calculus in an infant. Turk J Pediatr. 60:769–770.
- Uhnoo I, Riepenhoff-Talty M, Dharakul T, Chegas P, Fisher JE, Greenberg HB, Ogra PL. 1990. Extramucosal spread and development of hepatitis in immunodeficient and normal mice infected with rhesus rotavirus. J Virol. 64:361–368.
- Ushijima H, Bosu K, Abe T, Shinozaki T. 1986. Suspected rotavirus encephalitis. Arch Dis Child. 61:692–694.
- Vaarala O, Jokinen J, Lahdenkari M, Leino T. 2017. Rotavirus vaccination and the risk of celiac disease or type 1 diabetes in Finnish children at early life. Pediatr Infect Dis J. 36:674–675.
- Van Den Brink GR, Bloemers SM, Van Den Blink B, Tertoolen LGJ, Van Deventer SJH, Peppelenbosch MP. 1999. Study of calcium signaling in non-excitable cells. Microsc Res Tech. 46:418–433.
- Velázquez FR, Matson DO, Calva JJ, Guerrero L, Morrow AL, Carter-Campbell S, Glass RI, Estes MK, Pickering LK, Ruiz-Palacios GM, et al. 1996. Rotavirus infection in infants as protection against subsequent infections. N Engl J Med. 335:1022–1028.
- Ward RL, Knowlton DR, Pierce MJ. 1984. Efficiency of human rotavirus propagation in cell culture. J Clin Microbiol. 19:748–753.
- Ward RL, McNeal MM, Sheridan JF. 1990. Development of an adult mouse model for studies on protection against rotavirus. J Virol. 64:5070–5075.
- Webster NL, Zufferey C, Pane JA, Coulson BS. 2013. Alteration of the thymic T cell repertoire by rotavirus infection is associated with delayed type 1 diabetes development in non-obese diabetic mice. PLoS One. 8:e59182.
- Weclewicz K, Svensson L, Kristensson K. 1998. Targeting of endoplasmic reticulum-associated proteins to axons and dendrites in rotavirus-infected neurons. Brain Res Bull. 46:353–360.
- Wong CJ, Price Z, Bruckner DA. 1984. Aseptic meningitis in an infant with rotavirus gastroenteritis. Pediatr Infect Dis. 3:244–246.
- Wong V. 2001. Acute gastroenteritis-related encephalopathy. J Child Neurol. 16:906–910.
- Yamashiro Y, Shimizu T, Oguchi S, Sato M. 1989. Prostaglandins in the plasma and stool of children with rotavirus gastroenteritis. J Pediatr Gastroenterol Nutr. 9:322–327.
- Yeom JS, Jo JY, Park JS, Kim YS, Chung JY, Han TH, Seo JH, Park ES, Lim JY, Woo HO, et al. 2019. Monocyte chemoattractant protein (MCP)-1 in rotavirus-associated white matter injury in newborns. Neuropediatrics. 50:228–234.
- Yeom JS, Park JS, Kim YS, Kim RB, Choi DS, Chung JY, Han TH, Seo JH, Park ES, Lim JY, et al. 2019. Neonatal seizures and white matter injury: role of rotavirus infection and probiotics. Brain Dev. 41:19–28.
- Yolken R, Murphy M. 1982. Sudden infant death syndrome associated with rotavirus infection. J Med Virol. 10:291–296.
- Yu TH, Tsai CN, Lai MW, Chen CC, Chao HC, Lin CW, Chiu CH, Chen SY. 2012. Antigenemia and cytokine expression in rotavirus gastroenteritis in children. J Microbiol Immunol Infect. 45:265–270.
- Zhaori GT, Fu LT, Xu YH, Guo YR, Peng ZJ, Shan WS. 1991. Detection of rotavirus antigen in tracheal aspirates of infants and children with pneumonia. Chin Med J. 104:830–833.
- Zheng BJ, Chang RX, Ma GZ, Xie JM, Liu Q, Liang XR, Ng MH. 1991. Rotavirus infection of the oropharynx and respiratory tract in young children. J Med Virol. 34:29–37.
- Zheng J, Zheng H, Gupta RK, Li H, Shi H, Pan L, Gong S, Liang H. 2017. Interrelationship of rotavirus infection and Creatine Kinase-MB isoenzyme levels in children hospitalized with acute gastroenteritis in Guangzhou, China, 2012-2015. Sci Rep. 7:7674.

