Abstract
Corrosive chemical substance ingestions are a major problem, especially in developing countries, but also in developed countries such as the United States, France, and Belgium. Ingestions may be deliberate as suicide attempts (mostly in adolescents and adults) or accidental (mostly in children). The results can be devastating in terms of individual suffering and disability, but also in terms of resource utilization and costs. In developing countries, outcomes may be worse because of limited medical/surgical resources. Common sequelae include gastrointestinal (GI) tract (esophagus, stomach, pylorus, and duodenum) stricture formation, GI tract perforation, and hemorrhage. Systemic effects may also occur, such as disseminated intravascular coagulation (DIC), multi-organ system failure, and sepsis. Various interventions in the acute phase to reduce the severity of injury have been attempted, but there are no large controlled clinical trials to demonstrate efficacy. Dilation therapy in various forms is commonly used for the treatment of strictures and a variety of surgical procedures including esophagectomy and delayed replacement may be required in severe corrosive injury cases.
Introduction
The term “corrosive” rather than “caustic” is used in this review as it better reflects the totality of chemical ingestions that can cause acute injury to the esophagus, stomach, pylorus, duodenum, and sometimes other organs. The most commonly ingested corrosive chemicals are strong acids and bases (pH <2 or >12) which can rapidly penetrate the various layers of the esophagus (Poley et al. Citation2004; Cheng et al. Citation2008; Betalli et al. Citation2009; Chibishev et al. Citation2013; Ciammaichella et al. Citation2019), but other chemical substances can also cause such injuries (Wax and Yarema Citation2007; Chibishev et al. Citation2012; Ducoudray et al. Citation2016), for example, concentrated acetic acid (Chibishev et al. Citation2013). The extent of the tissue injury is dependent on such factors as the physical form of the ingested chemical substance, the type, amount, and concentration, the pre-ingestion condition of the tissues, and the duration of contact (Poley et al. Citation2004; Cheng et al. Citation2008; Betalli et al. Citation2009; Chibishev et al. Citation2013). Storage of corrosive chemical substances in water or soft drink containers in the home is a risk factor for accidental corrosive ingestion in children, particularly those less than 5 years of age (Botwe et al. Citation2015; Sabzevari et al. Citation2017). Education programs for storage of corrosive chemical substances in their original child-resistant containers might prevent some ingestion corrosive injuries (Uygun Citation2015).
The esophageal mucosal tissue is generally considered to be more resistant to the injurious effects of acids than alkalis, as the latter are often more viscous – with a potentially longer contact time – and also produce liquefaction rather than coagulation necrosis as with acids (Cheng et al. Citation2008; Ducoudray et al. Citation2016; Ciammaichella et al. Citation2019). The necrosis seen with acid ingestion forms a coagulum which serves to limit tissue penetration, whereas the liquefaction necrosis seen with alkalis does not (Wax and Yarema Citation2007).
No one particular symptom or symptom/sign set reliably – especially the presence or absence of oropharyngeal lesions – can predict the severity of the tissue injury following corrosive ingestion (Cello et al. Citation1980; Gaudreault et al. Citation1983; Crain et al. Citation1984; Satar et al. Citation2004; Wax and Yarema Citation2007; Lupa et al. Citation2009; Riffat and Cheng Citation2009; Millar and Cox Citation2015; Sabzevari et al. Citation2017). Therefore, the “gold standard” for determining the extent of tissue injury is esophagogastroduodenoscopy (EGD), generally referred to as “endoscopy” in this review (Wax and Yarema Citation2007; Cheng et al. Citation2008; Riffat and Cheng Citation2009). However, the DROOL Score has been proposed by a Turkish group (Uygun et al. Citation2012) and a “Med-TU” chart was devised by authors from Thailand who found that drooling of saliva, the severity of buccal mucosal injury, and white blood count were significant independent predictors of whether a patient is at risk to have a grade 2b or more severe GI tract injury (Havanond and Havanond Citation2007).
Some authors have suggested that asymptomatic patients who have ingested corrosive substances do not require endoscopy (Gupta et al. Citation2001; Lamireau et al. Citation2001; Bird et al. Citation2017), however, cautions on monitoring are recommended for pediatric patients (Bird et al. Citation2017). A recently published international consensus paper recommends that CT-scan may be a better option than EGD for guiding the decision of whether emergent surgical intervention is necessary (Bonavina et al. Citation2015).
Methods
A literature review on the topic of corrosive ingestions was performed in PubMed and Google using a variety of search terms including “caustic ingestion”, “corrosive ingestion”, “acid ingestion”, “base ingestion,” and “ingestion injury.” Standard Medical Toxicology textbooks were also consulted. The dates were generally confined to the 1970s and up to the present with the most recent publications given precedence. References retrieved were also perused for additional relevant reference citations. Emphasis was on human corrosive ingestion exposures rather than experimental animal studies.
Results
Review articles and textbook chapters, large and small case series, selected case reports, and a recent World Society of Emergency Surgery consensus paper on foregut corrosive injuries were retrieved and reviewed.
Scope of the problem
Dangerous commercial products are available in the home environment. In adults, ingestion of corrosives is mostly done by suicidal patients or those suffering from serious psychiatric disorders (Sarfati et al. Citation1984). Accidental ingestions are often benign, sometimes accompanied by acute alcohol intoxication. “Corrosive” is defined as any substance capable of causing tissue damage. Among the corrosives commonly found are oxidants such as bleach, hydrogen peroxide, or potassium permanganate, but also bases, often associated with surfactants in household products or unblocking furnace cleaners, drain cleaners, oven and grill cleaners, and acids such as sulfuric, nitric, and hydrochloric acids in toilet bowl cleaners, rust removers, automobile batteries, and finally in lesser quantities in solvents such as white spirit or formaldehyde.
More recently, laundry detergents and especially laundry pods represent a serious risk for ingestion by children (Valdez et al. Citation2014). During 2012–2013 in the USA, 17,230 children <6 years old were exposed to laundry detergent pods. In 79.7% of these cases, ingestion was the exposure route. A major medical outcome was noted in 7.5% of cases and 4.4% were hospitalized. The spectrum of clinical effects ranged from minor to serious, and there was one confirmed death (Valdez et al. Citation2014).
Following ingestion of corrosive chemical substances, the severity and location of GI lesions depend on the duration of contact, the corrosive strength of the chemical agent such as pH for acids and bases or oxidative potential, and chemical concentration. Viscosity may also play a role in the severity of chemical injury, as more viscous substances may adhere to the wall of the GI tract, increasing contact duration.
The ingested volume is also an aggravating factor for chemical GI injuries and when an amount equivalent to >/= 100 ml is ingested, the ingestion can be considered massive as it is in the case of suicide attempt. In cases of accidental ingestion, a sip is enough as the taste or odor can assist in identifying the mistake. Accidental ingestions can be due to decanting a corrosive chemical into an unlabeled or improperly labeled container such as a mineral water or soft drink bottle (Botwe et al. Citation2015; Marcuz de Souza Compos et al. Citation2017). Bleach can sometimes be mistaken for lemonade.
Substances anticipated not to be or only minimally corrosive or toxic
Laboratoire Prevor (Valmondois, France) provides the Prometra database, available without charge on the website http://www.prevor.com/fr/prometra. This database is currently available only in French, but it is proposed to have a French-to-English translation function in the near future. The following list of substances anticipated to not be corrosive or toxic or only minimally so was gleaned from the Prometra database:
Anionic and Nonionic Detergents
Artificial Sweeteners
Ballpoint Pen Ink
Barium Sulfate
Blackboard Chalk
Black Pepper
Carboxymethylcellulose
Children’s Crayons
Dichloral
Dry Cell Batteries
Glycerol
Glycerol Stearate
Glycerol Triacetate
Graphite
Gums (Acacia, Agar, Ghatti, etc.)
Hormones
Kaolin
Lanolin
Lauric Acid
Linoleic Acid
Linseed (Flax) Oil (Not Boiled)
Lipstick
Magnesium Silicate
Matches
Methylcellulose
Modeling Clay
Palmitic Acid
Pencil “Lead” (Graphite)
Polyethylene Glycol (Carbowax)
Polyethylene Stearate
Pure Castor Oil, Sulfurated
Putty
Silicone
Sorbitol
Stearic Acid
Tallow Candles
Titanium Oxide
Thermometer Liquid (Not Mercury)
Vasoline (Petrolatum Jelly)
Vitamins and Multivitamin Compounds (Not Containing Iron)
Wax Candles
AAPCC NPDS data
Some summary cases of corrosive ingestion are published by the American Association of Poison Control Centers in the National Poison Data System (NPDS) annual reports, the most recent of which at the time of this review were from 2013 (for the year of 2012), 2014 (for the year of 2013), 2015 (for the year of 2014), 2016 (for the year of 2015), 2017 (for the year of 2016), and 2018 (for the year of 2017) (Mowry et al. Citation2013, Citation2014, Citation2015, Citation2016; Gummin et al. Citation2017; Gummin et al. Citation2018). Overall, there were a total of 13,000,885 human poison exposures reported to this database during the 6-year period of 2012–2017.
With limited published details, during this 7-year time frame, there were a total (exposure route not specified) of 10,860 hydrochloric acid (HCl) exposures with 3808 patients evaluated in a Health Care Facility and 13 deaths. Of alkali poison exposures during this 6-year time frame, there were a total of 20,983 (exposure route not specified) with 9876 patients evaluated in a Health Care Facility and 5 deaths. Fatal corrosive ingestions were common among elderly patients and those adults intentionally committing suicide and were a combination of intentional (suicidal), unintentional, or unknown (excluding cases with co-ingestants) () (Mowry et al. Citation2013, Citation2014, Citation2015, Citation2016; Gummin et al. Citation2017; Gummin et al. Citation2018).
Table 1. Summary of fatal corrosive ingestions (2012–2017 AAPCC NPDS Data) (Mowry et al. Citation2013, Citation2014, Citation2015, Citation2016; Gummin et al. Citation2017, Citation2018).
Other scope of the problem data
A comprehensive review by Bonnici et al. (Citation2014) retrieved 277 published papers, of which 37 were relevant for analysis of whether CT-scan could replace fiberoptic endoscopy in evaluation of symptomatic patients with corrosive ingestions. These 37 papers reported 2375 adult patients, 2302 pediatric patients, and 489 patients for whom the age group was not specified, for a total of 5166 symptomatic corrosive substance ingestions (Bonnici et al. Citation2014).
In the course of a literature search as an internship report for Laboratoire Prevor, Valmondois, France, Weinrab (Citation2012) noted that there are approximately 15,000–20,000 cases of corrosive substance ingestion annually in France (Fuilla et al. Citation1996), and that in the USA there are between 5000 and 15,000 such cases per year, while some references state there might be >100,000 such ingestion cases per year in children (Rothstein Citation1986; Doğan et al. Citation2006; Weinrab Citation2012). Weinrab (Citation2012) noted that most published data concern cases from a single hospital or medical center. In Denmark, hospitalizations for corrosive substance ingestion were estimated to be 1/100,000 population in 1994 (Weinrab Citation2012). In Italy, in 2005, there were 225 corrosive substance ingestion hospitalizations, or 0.38/100,000 population (Robustelli et al. Citation2011), although Gambardella et al. (Citation2018) stated that there are 15,000 new such cases annually in Italy. In Saudi Arabia, there were an estimated 4/100,000 population corrosive ingestions in children (Al-Binali et al. Citation2009). Worldwide, children represent ∼80% of corrosive substances ingestions, and the majority of these are accidental (Contini and Scarpignato Citation2013).
Quoting data compiled by the World Health Organization, Lachaux et al. (Citation2011) described that the worldwide estimated incidence of corrosive ingestions is 110/100,000 persons annually. Incidences in various regions were the following: United States, 19/100,000 population; Eastern Mediterranean area, 187/100,000 population; Asia, 243/100,000 population. Worldwide corrosive ingestion mortality was 310,000 persons in 2004, or 4.8/100,000 population per year. Children accounted for approximately 30% of corrosive ingestion cases (Lachaux et al. Citation2011).
According to one reference, the economic cost of treatment of corrosive ingestions in the United States in 2009 was more than 22 Million dollars (Johnson and Brigger Citation2012).
Presenting signs and symptoms
Corrosive ingestions are commonly evaluated initially by presenting signs and symptoms and by fiberoptic endoscopy.
In a comprehensive review of the literature, Bonnici et al. (Citation2014) concluded that adult patients with presenting signs and symptoms of esophageal corrosive injuries such as drooling of saliva, vomiting, pain, or dysphagia require evaluation with fiberoptic endoscopy, and noted that a greater degree of caution should be applied in pediatric patients (Bonnici et al. Citation2014). These authors noted that early endoscopy (<12 h after corrosive ingestion) is indicated in symptomatic patients to grade the injury and determine whether surgical intervention is necessary (Lupa et al. Citation2009; Bonnici et al. Citation2014).
Some authors have noted that early symptoms and physical examination findings are unreliable in predicting the extent of GI tract injuries following corrosive substance ingestion (Lupa et al. Citation2009; Boskovic and Stankovic Citation2014; Ciammaichella et al. Citation2019), although a multi-center study of 356 patients with alkaline corrosive substance ingestion (pH >/= 12) found that all with a significant injury (grade 2 or 3) were symptomatic (Ferguson et al. Citation1989; Gorman et al. Citation1992).
Acute clinical characteristics of corrosive ingestion may include such findings as (Chibishev et al. Citation2012; Contini and Scarpignato Citation2013; Ciammaichella et al. Citation2019):
Painful and burning sensations in the mouth and throat
Retrosternal chest and upper abdominal pain
Nausea
Vomiting, often with hematemesis
Hypersalivation
Difficulty in swallowing secondary to edema
Ulcerations or whitish-appearing plaques in the mouth, oropharynx, or on the palate
Laryngospasm
Dysphonia/aphonia
Dyspnea
Gastrointestinal tract perforation
Aspiration of the corrosive substance with:
Endotracheal or endobronchial necrosis,
Mediastinits,
Which may result in a fatal outcome.
Late clinical findings may include (Eaton and Tennekoon Citation1972; Chibishev et al. Citation2012; Contini and Scarpignato Citation2013; Uygun Citation2015; Arnold and Numanoglu Citation2017; Ciammaichella et al. Citation2019):
Esophageal strictures/stenosis
Stenosis of the gastric antrum or pylorus (usually manifested as a sensation of a full stomach, nausea, vomiting, and weight loss)
Gastrointestinal reflux
Esophageal or gastric carcinoma (cicatricial carcinoma) appearing many years after corrosive substance ingestion (esophageal carcinoma occurs in perhaps 3% of patients; gastric carcinoma is very rare)
Following corrosive chemical ingestion, the following risk factors for late development of esophageal strictures were identified in a retrospective cohort study of 50 patients (Le Naoures et al. Citation2017):
Zargar endoscopic classification score +/> 2a
Ingestion of strong (concentrated) acidic or alkaline chemical substances
Elevated white blood cell count
Decreased prothrombin ratio
Thirty-eight Brazilian patients with a history of corrosive ingestions and esophageal stenosis >20 years previously were evaluated in an observational transitional trial, cross-sectional study to assess whether Lugol’s Iodine solution chemoendoscopy or Narrow Band Imaging were better for detecting of early esophageal cancer (Pennachi et al. Citation2017). Nine suspicious lesions were found with Narrow Band Imaging and 14 were found with Lugol’s solution chemoendoscopy. Five (13%) were noted with both techniques. Two (40%) of such lesions were confirmed as carcinomas on histopathological evaluation (Pennachi et al. Citation2017).
Among patients with grade 2b or 3 lesions, strictures develop in 71% and 100%, respectively. Esophageal neoplasms (adenocarcinomas and squamous cell carcinomas) occur at a rate 1000–3000 times higher than in persons of similar age. Such neoplasms have been reported to occur only one year post-ingestion, but more often occur at a rate of 2–3% with an interval of 1–3 decades post-ingestion (Contini and Scarpignato Citation2013).
The severity of gastrointestinal injuries as classified according to criteria established by Zargar et al. (Citation1991) was initially based on a case series of 81 corrosive ingestion patients who underwent a total of 381 endoscopic examinations ().
Table 2. Classification of mucosal injury (adapted from Zargar et al. Citation1991).
An alternative classification system proposed by Kikendall (Citation1991) has been used by some authors ().
Table 3. Classification of mucosal injury (adapted from Kikendall Citation1991).
There may be a 9-fold increase in patient mortality and morbidity with each increasing endoscopic lesion grade (De Lusong et al. Citation2017). In a 10-year cross-sectional study of 348 adult corrosive ingestion patients treated in an Iranian institution, important predictive factors for needed Intensive Care Unit admission, emergent surgical intervention, and fatality were the following: attempted suicide, higher Zargar score mucosal injuries, decreased level of consciousness, and higher respiratory rate (Alipour-Faz, Arsan, et al. Citation2017).
Summaries of case series
Pediatric patients
Bautista Casasnova et al. (Citation1997) published a retrospective 10-year study of ingestion of corrosive substances by 743 children in Galicia between 1981 and 1990. All corrosive substance ingestions seemed to be accidental. Of these 743 children, 20% had esophageal injuries as determined by endoscopy; 11.8% were the 1st degree, 3.1% were the 2nd degree, and 2.7% were the 3rd degree.
Bleach was ingested by 73% of patients. The next most common corrosive ingestant was sodium hydroxide. Alkaline chemical products were ingested by 681/743 children (92%) and were responsible for 87% of corrosive GI injuries. Acid chemical products accounted for only 16/743 cases (2%). Liquid chemical products accounted for 88% of the injuries (Bautista Casasnova et al. Citation1997).
On hospital presentation, 44% of children did not have any symptoms. Of symptomatic children, 39% had vomiting, 6% had excessive salivation, both vomiting and excessive salivation occurred in 5%, and 2.5% had hematemesis. Other symptoms such as coughing, prostration, retrosternal pain, and epigastric pain each occurred in less than 1%. These authors did not find any reliable predictive relationship between presenting clinical symptoms or signs and development of esophageal corrosive injuries (Bautista Casasnova et al. Citation1997).
Five percent of total patients developed an esophageal stricture, and this complication occurred in 39 of 63 (62%) of patients with grade 2 or 3 lesions. Of these 39 patients with strictures, 17 developed the stricture in association with esophagitis, 9 in association with gastroesophageal reflux, 2 with both esophagitis and reflux, and 10 developed the stricture alone. One patient who ingested an acid chemical substance had only a quite minimal esophageal stricture, but developed a severe pyloric stricture. Three percent of children with strictures were treated with esophageal dilation therapy. No surgical interventions were mentioned in this report (Bautista Casasnova et al. Citation1997).
de Jong et al. (Citation2001) performed a 30-year retrospective study of corrosive esophagitis in pediatric patients treated at the Hospital for Sick Children in Toronto, Ontario, Canada from 1965-1995. Eighty cases of corrosive ingestion were identified. Ages ranged from 1 month to 16 years. Of these, 63 children (78%) were between the ages of 1 and 3 years. Alkali chemical substances were ingested by 56 children (70%), while acids were ingested by only 11%. Various other potentially corrosive products were ingested by the remainder (de Jong et al. Citation2001).
First or second-degree mucosal injury was noted in 46 cases (58%), while more extensive second-degree injuries occurred in 26% and third-degree injuries were found in 16%. Endoscopy was performed in 35/80 cases (44%). In no case, did a perforation occur secondary to endoscopy. A barium swallow X-ray examination was done in 13/80 cases (16%). Antibiotics and corticosteroids were administered to only 18 children (22%). Twenty-three of these 80 children (29%) developed medical complication which included chemical pneumonitis, atelectasis, aspiration pneumonitis, and dysphagia associated with gastroesophageal reflux. One child developed a gastric ulcer associated with hemorrhage (de Jong et al. Citation2001).
Nineteen of these 24 children with medical complications (24%) required esophageal dilation or surgical procedures. Three of them required anti-reflux surgical procedures, 5 required repeated pro-grade dilation, 11 required gastrostomy and stringing with subsequent retrograde dilation, and these 11 children subsequently required esophageal replacement procedures at times post-ingestion ranging from 12 months to 14 years (mean: 5 years). One patient died 2 months after replacement surgery from a massive hemorrhage. One patient had a left vocal cord injury; a right recurrent laryngeal nerve injury occurred during the replacement surgical procedure and a permanent tracheostomy was required. These authors also noted the significant psychosocial, family, and financial impacts that ensue from such corrosive injuries (de Jong et al. Citation2001).
Turner and Robinson (Citation2005) performed a retrospective study of 32 cases of corrosive substance ingestion in 31 pediatric patients admitted to a children's hospital in Melbourne, Australia between 1993 and 2003. Patients had a median age of 2.6 years (range: 11 months–18 years). In 3 cases, adolescents ingested corrosive substances with deliberate self-harm intent. Most commonly ingested corrosive substances were dishwashing tablets/powders (31%) and household bleach (18%) (Turner and Robinson Citation2005).
The most common presenting signs were drooling and ulcerations of the oropharynx (62% of cases). Signs and symptoms of respiratory tract involvement such as stridor, wheezing, and the requirement for supplemental oxygen were rare. Two patients required endotracheal intubation and mechanical ventilation because of respiratory distress. Thirty patients (97%) underwent endoscopy within 24 h of ingestion. Of these, 64% had mucosal swelling and oropharyngeal ulceration, 45% had esophageal involvement with 77% having superficial inflammation and 23% having severe ulceration (Turner and Robinson Citation2005).
None of these pediatric patients had documented long-term respiratory sequelae. Two patients developed long-term GI complications of residual esophageal strictures requiring multiple dilations. One had accidentally ingested an industrial ammonia-based cleaning solution and the other had deliberately ingested a caustic dishwashing powder on 2 occasions within one month (Turner and Robinson Citation2005).
Contini et al. (Citation2009a) reported the cases of 148 pediatric patients (aged 14 months–15 years) with accidental corrosive chemical substance ingestion treated at a surgical center in Goderich, Sierra Leone, between 2005 and 2008. Of these patients, only 29 (19.5%) were admitted early, and of these 2 died of severe respiratory tract injury. Twenty of these children had no lesions and were released from the hospital. The other 119 were admitted to hospital as late as several days, weeks, or even months post-ingestion with severe dysphagia (Contini et al. Citation2009a).
A total of 126 of these children underwent esophageal dilation for the treatment of strictures, with a mean of 4.9 dilations (range: 1–23). Gastrostomy was performed in 92/126 children (73%). Fifty-four of 126 children (42.8%) had recurrent strictures and 24 of these were still being treated with a continuous dilation program at the time of the report. Three patients did not respond to dilation therapy and were referred elsewhere for esophageal replacement surgery. Perforations occurred in 3 children (5.6%) and resulted in 2 fatal outcomes, both occurring after a dilation procedure. Successful dilation treatment was noted in 96 of these children (76%). The overall death rate was 4% (5/126) (Contini et al. Citation2009a).
Riffat and Cheng (Citation2009) reported a retrospective series of 50 consecutive cases of pediatric corrosive ingestions. The majority of these cases were unintentional ingestions and children had a median age of 22 months. Ingested chemical substances were alkalis (74%) (mainly, dishwashing powders, disinfectants, and degreasers), acids (6%), and other substances including chlorine bleach being the remainder. Of those children who had grade 2 or greater injuries on endoscopy, 50% developed strictures and required multiple dilations. Of note, in 6 of these patients (12%), there was no oral injury whilst there was a significant esophageal injury (Riffat and Cheng Citation2009).
Usta et al. (Citation2014) reported a series of 83 pediatric patients from developing countries with grade 2b esophageal injuries following ingestion of corrosive substances. Following an otherwise similar treatment regimen, 42 children received high-dose methylprednisolone for 3 d and 41 children did not receive this intervention. On endoscopic evaluation, stricture formation was noted in 4 patients (10.8%) in the methylprednisolone group and in 12 patients (30%) in the non-methylprednisolone group (p < 0.004), strongly suggesting that this intervention may be beneficial for such patients (Usta et al. Citation2014). However, other studies have not found evidence of clinical benefit from corticosteroid administration in such cases, particularly in patients with second and third-degree esophageal corrosive substance chemical injuries (Ferguson et al. Citation1989; Mamede and De Mello Filho Citation2002; Caravati Citation2014; Pelclová and Navrátil Citation2005; Fulton and Hoffman Citation2007; Wax and Yarema Citation2007; Chibishev et al. Citation2012).
In three publications, Contini et al. (Citation2007, Citation2009b, Citation2011) described the features and management of corrosive substance lesions in 175 consecutive pediatric patients from Sierra Leone. Of these, 57.7% were admitted to hospital at >1 month after ingestion. Esophageal dilation procedures were performed in 77.7%. Gastrostomy was done in 64%. Perforations occurred in 4.5%, and 2.8% of patients had a fatal outcome. More than 7 dilations each were required in 62 patients (35.4%). However, maintenance of a satisfactory luminal diameter was not possible in 15 patients (8.5%). Only 52.7% of patients were available for follow-up for a median of 7 months (range: 1–36 months) and long-term success of dilation (ability to swallow, improved nutritional status with weight gain, sustained esophageal patency) was only noted in 16% of patients Contini et al. Citation2007, Citation2009b, Citation2011).
Tewfik and Schloss (Citation1980) reviewed 86 pediatric cases of corrosive substance ingestion admitted to the Montreal, Quebec, Canada Children’s Hospital over a 10-year period. Of these, 62 children (72%) were <4 years old. Esophageal lesions defined by endoscopy were found in 35/86 cases (40%) and 6 children developed esophageal strictures requiring treatment with bougienage (Tewfik and Schloss Citation1980).
Temiz et al. (Citation2012a) reported a series of 14 pediatric patients with pyloric stenosis, 8 of whom had a history of corrosive substance ingestion. All patients were evaluated by endoscopy, and endoscopic balloon dilation was attempted in 12. This intervention was successful in 6 patients; the remaining 8 required surgical intervention (Temiz et al. Citation2012a).
Kaya et al. (Citation2010) retrospectively reviewed a series of 134 consecutive pediatric patients evaluated for corrosive substance ingestion over a 1-year period. These children were divided into low-grade and high-grade corrosive esophageal injury groups. A majority of patients (70%) had no symptoms on initial evaluation, while saliva drooling and oral lesions were more common in children with high-grade injuries. Clinical findings were evaluated for sensitivity, specificity, and predictive values. None of these were found valuable for estimating the severity of esophageal injury. These authors concluded that endoscopic direct esophageal visualization is required to make a definitive diagnosis (Kaya et al. Citation2010).
Gün et al. (Citation2007) reported a series of 91 pediatric patients treated with dilation therapy for esophageal strictures out of a total of 296 children admitted for ingestion of corrosive chemical substances during the period of 1990–2005. Of these, 43/91 (47%) were admitted immediately following corrosive ingestion and 48/91 (53%) were referred with esophageal strictures after having been treated for 6–12 weeks in other facilities. Treatments included esophageal rest, IV fluids, broad-spectrum antibiotics, single-dose corticosteroids, and IV ranitidine. After 3 weeks, patients with demonstrated esophageal stricture on barium swallow underwent esophageal dilation. Patients admitted immediately post-ingestion had better dilation response rates and 60% recovered within 1 year. Patients admitted late after corrosive substance ingestion had increased rates of esophageal perforation and none recovered during the first year post-ingestion (Gün et al. Citation2007).
Doğan et al. (Citation2006) performed a retrospective review of 473 children admitted to hospital for corrosive substance ingestion from 1995 to 2003. Household bleaches (36.6%) and oven cleaning products (23%) were the most common ingestants. Esophageal lesions were noted in 379/473 (80%) of these pediatric patients and 81/473 (17%) had gastric lesions. On follow-up, the following sequelae were noted: esophageal stricture (11 cases; 2%), esophageal perforation (1 case), gastric outlet obstruction (2 cases). Ingestion of alkaline oven cleaners appeared to result in more severe injures (Doğan et al. Citation2006).
Lamireau et al. (Citation1997) reported a case series of 65 children who underwent esophagoscopy following ingestion of corrosive chemical substances. These authors classified the children into 3 groups based on endoscopic findings: no lesion; minimal lesions; severe lesions. Corrosive ingestants included: dishwasher detergents (n = 14), oven cleaners (n = 10), bleach (n = 9), washing powder (n = 4), and others (n = 20). The ingestants were more often liquids (n = 37) rather than solids (n = 28). Children were asymptomatic in 57% of cases. Emesis (n = 20) or abdominal pain (n = 10) were not correlated with endoscopic findings. Hematemesis (n = 3) and respiratory distress (n = 4) were only noted in children with severe lesions. Of the 17 children with severe lesions, 8 (47%) developed strictures. Seven of these were long strictures which necessitated esophageal replacement, and one short stricture was treated with repeated dilation (Lamireau et al. Citation1997).
Balderas et al. (Citation2018) performed a descriptive-analytical study of 133 children aged <16 years who presented to the emergency department following ingestion of a corrosive substance (acids in 41%; alkaline in 59%). Muriatic acid was the most common specific substance ingested (36.8%). Caustic soda (sodium hydroxide) was the most common alkaline substance ingested (41.4%).
An esophageal injury was the most common following lesion following caustic soda (sodium hydroxide) ingestion compared to the other corrosive ingestants (p < 0.001) and muriatic acid ingestion compared to other ingestants was the most common cause of gastric lesions (p < 0.001) and duodenal lesions (p < 0.002). Children younger than 5 years of age comprised 93.2% of the total corrosive substance ingestions (Balderas et al. Citation2018).
Patients were evaluated between 6 and 24 h after ingestion with endoscopy. Injury grades for alkaline substances ingestion were the following: grade 1 25 (51%), grade 2a 12 (46.1%), grade 2b 10 (55.5%), and grade 3a 1 (50%). There were no grade 3b lesions in this group. In the alkaline ingestion group, there were 6 (37.5%) grade 1 gastric lesions, 1 (14.3%) grade 2a lesions, and 1 (100%) grade 3a lesions. There were no grade 3b gastric lesions. One patient (14.2%) had a grade 1 duodenal lesion (Balderas et al. Citation2018).
In those patients ingesting acids, the esophageal injury grades were the following: grade 1 18 (36.7%), grade 2a 11 (42.3%), grade 2b 5 (27.7%), grade 3a 1 (50%), and grade 3b 1 (100%). Gastric lesions in the acid-ingesting group were the following: grade 1 10 (62.5%), grade 2a 5 (71.4%), and grade 3b 1 (100%). There were 5 (85.7% grade 1 duodenal lesions and 1 (100%) grade 2a lesions. The authors concluded that, in this study, alkaline ingestions caused injuries in the upper gastrointestinal tract and esophagus, while acid ingestions damaged the stomach and duodenum (Balderas et al. Citation2018).
A retrospective review of 41 pediatric patients with corrosive ingestion evaluated over a 2-year period in Iran was done by Dehghani et al. (Citation2018). Accidental corrosive chemical substances wee noted in 96.1% and 68.3% happened in the home. Chemical substances involved were acidic in 19 children (46.3%) and 17 (41.5%) were alkaline substances. Symptomatic children comprised 24.3% of patients with drooling (34.14%), dysphagia (26.8%), oral ulcers (7.3%), abdominal pain (7.3%), elevated temperature (4.8%), and hematemesis (2.4%). Of these children, normal endoscopy findings were found in 14 (34.1%), 6 (14.6%) had grade 1 injuries, 8 (19.5%) had grade 3 injuries.
Children with normal or grade 1 endoscopic findings were clinically observed and then discharged from hospital with a 4-week follow-up. Proton pump inhibitors were initially prescribed for all patients, and corticosteroids and antibiotics were administered to all children with grade 2 injuries (29.3%). Of children with acid ingestion, 36% of children had injuries of the esophagus and 26.3% had gastric lesions. Of pediatric ingestions of alkaline substances and developing grade 3 lesions, 100% developed esophageal strictures. One such child died (Dehghani et al. Citation2018).
In a single case report, Johnson and Bruno (Citation2018) described the use of ophthalmic pH paper in the evaluation of a 3-year-old child who subsequently was found to be the victim of deliberate child abuse from forced ingestion of an industrial bleach solution. Emesis pH was 9.0 (Johnson and Bruno Citation2018).
Sabzevari et al. (Citation2017) performed a retrospective cross-sectional study of 54 children who ingested corrosive substances during 2011–2013. Acidic chemical substances were ingested by 36 children and base substances were ingested by the remaining 16. In 77.5% of cases the corrosive substances were not in standard containers. At endoscopy, 50 of 54 children were found to have esophageal lesions: grade 1 in 6 cases, grade 2a in 15 cases, grade 2b in 27cases, and grade 3a in 2 cases. Gastric lesions ranging from mild erythema to mild or severe ulcers were present at endoscopy in 34 cases. These authors found no significant relationship between presenting initial clinical findings and lesion severity (Sabzevari et al. Citation2017).
A retrospective study of 75 Iranian pediatric patients having ingested corrosive chemical substances between 2006 and 2011 was performed by Honar et al. (Citation2017). The most common presenting symptoms were drooling, vomiting, lesions in the oral cavity, and dysphagia. By 3-month post-ingestion follow-up, 20% of these children had developed an esophageal stricture. Ingestions comprised both acidic and base chemical substances, but gastric lesions were more common following acidic substances ingestion (Honar et al. Citation2017).
Kucuk et al. (Citation2017) reported a case series of 154 pediatric patients in whom endoscopy was performed because of corrosive chemical ingestion. Corrosive substances involved were the following: descalers, degreasers, bleach (unlabeled), drain cleaners, kitchen cleaners, dishwasher rinsing substances, and hydrochloric acid. Oropharyngeal lesions were present in 63% of patients. On endoscopy, 63 of these children had mucosal injuries found at initial endoscopy, and 40 had severe lesions. Twenty of these children developed esophageal strictures and were treated with dilation, 14 of whom had both dilation and intralesional steroid injection. Three children each required surgical colonic interposition and 3 had surgical intervention with laparoscopic gastroduodenostomy and gastrojejunostomy (Kucuk et al. Citation2017).
In a retrospective case series of 635 endoscopies in children with corrosive chemical substance ingestion between the years of 2000 and 2015, there were five with grade 2a and 15 with grade 2b lesions. Those who developed esophageal strictures were treated with endoscopic balloon dilation. The duration of treatment for children with grade 2a lesions was an average of 7 balloon dilations over a period of 15 months and those with grade 2b lesions had balloon dilation treatment over a period of 18.8 months (Taşkinlar et al. Citation2017).
Adult patients
Cheng et al. (Citation2008) performed a retrospective medical records review of 273 patients with corrosive ingestions admitted to a teaching hospital in Taiwan between 1999 and 2006. Of 273 patients whose medical records could be analyzed, a Zargar et al. (Citation1991) grade 3b lesion was the most common (n = 82; 30.03%), and a grade 2b injury was the next most common (n = 62; 22.71%). The most common complication was esophageal stricture formation (n = 66; 24.18%), followed by aspiration pneumonitis (n = 31; 11.36%), and respiratory failure (n = 21; 7.69%) (Cheng et al. Citation2008).
When compared to patients with a grade 3a injury, those with a grade 3b injury had a greater risk of prolonged hospital stays, admissions to an Intensive Care Unit (ICU), and systemic or GI complications. The upper GI complications noted were bleeding, perforation, and stricture formation. Systemic complications were renal insufficiency, liver injury, and disseminated intravascular coagulation (DIC). The majority of patients had ingested industrial cleaning agents containing alkaline substances (n = 131; 47.99%) or strong acids (n = 95; 34.80%) (Cheng et al. Citation2008).
Severe injuries were found in the stomach (n = 116; 30.04%); duodenum (n = 120; 43.1%), and esophagus (n = 71; 26%). The mean hospital stay was 8 d (range: 0–90 d), 29 patients were admitted to the intensive care unit, and in-hospital mortality was 6.59% (18/273 patients). Deaths were attributable to esophageal perforation (n = 1), tracheal perforation with hemorrhage (n = 1), hematemesis and sudden onset of apnea (n = 4), lung cancer (n = 1), and multiple organ system failure (n = 11) (Cheng et al. Citation2008).
Formation of strictures was the most common GI complication amongst all patients (n = 66; 24.18%) and in patients with grade 3b injuries (n = 44; 53.66%). Strictures most commonly occurred 2 weeks after corrosive ingestion. Stricture treatments included: gastrojejunostomy (n = 24), endoscopic dilation (n = 21), medical treatment (n = 10), esophagectomy (n = 5), esophageal-colonic bypass in 1 patient, and nasogastric feeding in 1 patient with a past history of a cerebrovascular accident. Of the 21 patients treated with endoscopic dilation, 11 later required surgical intervention for esophageal or pyloric perforation (n = 3) or dilation failure (n = 8). A total of 51 patients were treated surgically for perforation (n = 6) and stricture formation (n = 34). This total includes the 11 patients described above (Cheng et al. Citation2008).
In a retrospective 10-year study of 84 Macedonian patients who ingested concentrated acetic acid (>30%) between 2002 and 2011, Chibishev et al. (Citation2013) found that in addition to severe upper GI tract damage and other systemic complications, 28/56 patients (approximately 50%) developed renal function impairment. There were 11 deaths amongst these patients (13%). These data were taken from a total group of 932 patients with corrosive substance ingestions. In the acetic acid subgroup, there were complications of esophageal stenosis (n = 5), gastric stenosis (n = 22), combined esophageal and gastric stenosis (n = 11), acute kidney failure (n = 28), combined acute renal failure and liver failure (n = 23), and combined acute renal failure, liver failure, and DIC (n = 17). Systemic complications were more common amongst patients who had serious upper GI tract injuries, and the death rate in this subgroup was approximately 39% (Chibishev et al. Citation2013).
In a 16-year retrospective Danish study, 179 patients with corrosive ingestions between 1976 and 1991 were reviewed (Henrik and Christensen Citation1994). Of the 75 adult patients, 61% ingested corrosive substances in a suicide attempt and 61% of these were women. Over half of the suicide attempts were in patients with a history of psychiatric illnesses. When hydrochloric acid (HCl) was ingested by adults, it was fatal in 6/12 patients (50%). In this case series, two patients died before endoscopy could be performed. Eleven patients had no signs or symptoms and endoscopy was not done. One patient eventually developed an esophageal stricture. The average hospital stay for adults was 10 d (range: 1–107 d). Patients had upper GI tract injuries (n = 63; 84%) and/or esophageal chemical injuries (79%). Of the ingested corrosive substances, 94% were liquids, 55% were acids, 50% were “strong” acids, and 29% were “strong” alkalis. A 7th patient died 14 d after ingestion of liquid sodium hydroxide (Henrik and Christensen Citation1994).
Thomas et al. (Citation2009) performed a multi-center prospective study of 78 cases of corrosive chemical esophageal injuries treated over a 10-year period from 1996 to 2006 in the metropolitan area of Lagos, Nigeria. There were a total of 78 patients (61 males; 17 females). Acid chemical substances were ingested in 55.1% of cases, an alkali substance was ingested in 35.9%, and the ingestion was accidental in 62 of 78 patients (79%). Six patients underwent endoscopy in the acute phase. Of these, 4 had oral burns and the other 2 had mid-esophageal injuries (Thomas et al. Citation2009).
A total of 47 patients had emesis in the acute phase (60%), and 12 patients had specific treatment with naso-gastric tubes, antacids, H2-blockers, and/or corticosteroids. Barium swallow X-ray examinations were used to determine the location and extent of strictures. Of 52 patients ingesting acids (52.5%), 3 developed pharyngo-esophageal strictures, 2 had upper 1/3 esophageal strictures, 23 had middle 1/3 strictures, 17 had lower 1/3 strictures, and 7 developed gastric strictures. Of those who ingested alkalis, 1 had an upper 1/3 esophageal stricture, 33 had middle 1/3 strictures, 6 had lower 1/3 strictures, and none developed gastric strictures. The authors did not report whether or not dilation or surgical procedures were utilized for treatment (Thomas et al. Citation2009).
Adedeji et al. (Citation2013) published the results of a retrospective 7-year study of all patients treated for corrosive chemical ingestions in a university teaching hospital in Osogbo, Nigeria between 2005 and 2011. There were a total of 28 patients (21 adults; 7 children). Alkali chemical substances were ingested by 78.6% of these patients. Suicidal ingestion was the cause in 71.4% of patients, especially amongst adults, while accidental ingestion was the cause in 28.6%. Nearly 2/3 of patients presented to hospital >48 h after ingestion. Patients presenting to hospital early were managed with conservative therapy, while those arriving late received fluid and nutritional rehabilitation. There were two deaths from esophageal perforation complicated by sepsis. Esophageal strictures developed in 42.9% of patients. These were managed with esophageal dilation if the strictures were short; patients with long or multiple segment strictures were referred to cardiothoracic surgeons for management (Adedeji et al. Citation2013).
Havanond and Havanond (Citation2007) performed a prospective study of 148 patients who ingested corrosive substances in Thailand between 2000 and 2004. The most commonly ingested substance (62%) was a toilet disinfectant containing a strong acid. The reason for ingestion was deliberate suicide attempt in 92% of patients; in only 8% was the ingestion accidental. The presenting signs/symptoms were as follows: nausea or vomiting (84%); a depressed or drowsy general appearance (10%); hoarseness (14%); stridor (2%); visible lesions of the lips (33%), tongue (44%), buccal mucosa (43%), or palate (49%); slight abdominal guarding (2%) or tenderness (34%) (Havanond and Havanond Citation2007).
While all of these patients had superficial oral ulcerations, none required admission to the Intensive Care Unit. Endoscopic examination revealed the following: negative in 7 cases (4.7%); grades 1 or 2a in 122 cases (82.4%); grade 2b or more severe in 19 cases (12.8%). All patients found to have grade 2a lesions were seen in follow-up 2 weeks after hospital discharge and they were all healthy and having no swallowing difficulties. The site of more severe lesions (grade 2b or more severe) involved: gastric antrum (1 case); gastric body (2 cases); gastroesophageal junction (5 cases); multiple lesion sites (11 cases) (Havanond and Havanond Citation2007). These authors did not report what treatments were administered or whether any surgical procedures were performed in this study group.
Radenkova-Saeva et al. (Citation2014) conducted a 3-year prospective study of 43 patients with acute ingestions of corrosive substances hospitalized in Sophia, Bulgaria during 2010–2013. All ingestions were of alkaline chemical substances and all were intentional. In 82% of cases, complications including severe bleeding, perforation, and formation of strictures and/or fistulas. Two patients required surgical intervention with coloesophagoplasty, but had satisfactory recoveries (Radenkova-Saeva et al. Citation2014).
Jalal et al. (Citation2014) reported the results of a retrospective series of 1360 cases of ingestion of household corrosive hydrochloric acid products in Morocco. Ingestions were with suicidal intent in 45% of cases and were accidental in 54%. Gastroesophageal symptoms occurred in 96% of cases, with a favorable outcome in 89%. Sequelae (not specified) occurred in 4.6% of cases and 7.1% of such patients had a fatal outcome (Jalal et al. Citation2014).
Diliwari et al. (Citation1984) reported a case series of 16 adult patients with corrosive ingestions in Chandigarh, India over 3 years from 1978 to 1980. Of these patients, 10 ingested sulfuric acid and 3 had ingested hydrochloric acid; the rest (1 patient each) had ingested nitric acid, formic acid, and chromic acid. All patients developed injuries of the esophagus and stomach while the duodenum was not injured in the majority. No mild (grade 1) injuries occurred, but 5 patients had moderate (grade 2) lesions and 10 had grade 3 lesions. Three patients with grade 3 injuries died (Diliwari et al. Citation1984).
Epigastric pain and vomiting occurred in 14 of 15 patients, respectively. Hematemesis and oropharyngeal lesions were found in 12 patients. The single patient who ingested chromic acid developed renal failure and intravascular hemolysis. These authors noted that the amount of acid said to have been ingested did not correlate with the severity of GI tract injuries. Late complications developed in the six patients who were available for follow-up evaluation, consisting of esophageal structure (n = 4) and antral stenosis (n = 2). One of the 4 patients with esophageal stricture had a surgical colonic bypass procedure and two had successful endoscopic dilation. The fourth patient had such a significant stricture that even a guide wire could not be passed, refused surgical intervention, left the hospital against medical advice, and was lost to follow-up. Two of the patients with gastric antral stenosis had relief of gastric outlet obstruction following surgical resection (Diliwari et al. Citation1984).
Hawkins et al. (Citation1980) reviewed the cases of 214 patients with a history of corrosive substance ingestion. Of these, 65 (30%) had penetrating mucosal injuries. Children <5 years old accounted for 39% of hospital admissions, but only 8% required treatment. In contrast, 48% of patients admitted to hospital were adults and 81% of such patients required treatment. Thirty-one patients (48%) with penetrating mucosal lesions developed complications. Of these latter, all but one were secondary to ingestion of lye or acids (Hawkins et al. Citation1980).
Rajan et al. (Citation1985) reported 53 cases of formic acid ingestion (used in agriculture) in Karala State, South India, during the 3-year period 1980–1982. Of these, there were 38 survivors and 15 fatalities. Lesions present included circumferential facial chemical injuries, ulcerations of the oral and pharyngeal mucosa, abdominal pain with hematemesis and dysphagia, contractures and keloid formation on exposed skin, and esophageal strictures requiring surgical intervention. Respiratory tract lesions included inhalation pneumonitis with coughing, dyspnea, and cyanosis followed by infection and respiratory failure. Hematuria occurred in the first few hours and was followed by renal failure (renal biopsies showed toxic tubular necrosis) (Rajan et al. Citation1985).
Of complications, 16 patients (30%) developed esophageal strictures, 45 (84%) had inhalation pneumonitis, 20 (38%) had renal failure, 17 (32%) had hypotension, and 9 (17%) were unconscious. Ingestion of as little as 10 ml could be lethal with death occurring within hours regardless of treatment. Patients ingesting 15 ml or more were most often found dead. Of the 15 deaths (28%), 6 died of severe hypotension and respiratory arrest, 4 died of acute renal failure, and 5 died of GI hemorrhage (Rajan et al. Citation1985).
Wilson and Wormald (Citation1995) reported a series of 27 South African adults who attempted suicide by ingesting battery acid (30% sulfuric acid) over a 3-year period. A high rate of mortality was not observed, but 4 patients (15%) required surgical intervention for development of esophageal strictures (Wilson and Wormald Citation1995).
An earlier publication by these same authors (Wormald and Wilson Citation1993) appears to be a subset of the above patients who ingested battery acid. In this retrospective review of 18 patients, there was no correlation between symptom severity and extent of esophageal injury. It required ingestion of >200 ml to result in a significant GI tract injury. Esophageal injuries occurred in 10/18 patients (55%), and deep rather than circumferential injuries resulted in the formation of strictures. The most significant injury site was the gastric antrum, with 4 patients (23%) needing surgical intervention (Wormald and Wilson Citation1993).
Mamede and De Mello Filho (Citation2002) reported a 37-year historical review of 239 corrosive substance ingestion patients admitted to a teaching hospital between 1957 and 1994. Suicidal intent was the cause in 60% of cases and ingested amount was greater in such patients than in cases where ingestion was accidental. Among 215 of these patients for whom complications information was available, 190 (88.4%) developed esophageal lesions, 73% developed esophageal strictures, and 10.6% had no complications. Death during the acute phase occurred in 1% of patients (Mamede and De Mello Filho Citation2002).
Arici et al. (Citation2012) analyzed a series of adult and pediatric ingestions of corrosive substances and household detergents admitted to a university hospital emergency service between 1993 and 2008. Corrosive substances ingestion involved 1160 cases (8.5% of total emergency service admissions) in adults and 1988 cases (4.1% of total emergency service admissions) in children. Among patients aged 19–29 years, intentional ingestions were common. Ingested corrosive substances were alkaline (106 cases; 58.3%), acidic (47 cases; 25.8%), and household detergents (28 cases; 15.4%). Common clinical signs and symptoms were vomiting (35.7%), nausea (14.8%), and sore throat (13.1%). In patients evaluated with endoscopy, first-degree esophageal injury was noted in 58.7%. One adult patient died following intentional hydrochloric acid ingestion (Arici et al. Citation2012).
Tohda et al. (Citation2008) reported a series of 95 consecutive adult patients admitted for corrosive substance ingestion to an urban emergency hospital over a 28-year period. The ingestion was a suicide attempt in 49/95 (52%) and was accidental in 47/95 (49%). No esophageal mucosal injury was noted on endoscopy in 10/95 (11%), while 47/95 (49%) had grade 1 injuries, 25/95 (26%) had grade 2 injuries, and 11/95 (12%) had grade 3 injuries. Endoscopic findings were predictive of development of complications. There was one fatality in a patient with grade 3 esophageal injury, multiple co-morbidities, and multiorgan system failure (Tohda et al. Citation2008).
Arévalo-Silva et al. (Citation2006) conducted a retrospective cohort study of 50 cases of corrosive substance ingestion treated in a tertiary medical center from 1988 to 2003. There was a biphasic patient distribution with half being children <5 years of age and the rest were adults (overall age range: 5 months–71 years). Alkaline corrosive substances were ingested by 42%, acidic substances by 32%, and chlorine bleach by 26%. Accidental ingestion was more frequent (67%) than attempted suicidal ingestions (33%). All of the latter occurred in adults. Rigid esophagoscopy findings in 36 patients revealed 1st-degree injuries in 16 (44%), 2nd-degree injuries in 6 (17%), 3rd-degree injuries in 7 (19%), and 4th-degree injuries in 6 (17%); one patient had normal esophagoscopy findings. In this case series, ingestion of acidic corrosive substances caused worse esophageal mucosal injuries than did alkaline substances. As noted in other case series, injuries were worse following attempted suicidal ingestion than accidental ingestion (Arévalo-Silva et al. Citation2006).
Christesen (Citation1994) performed a retrospective review of 179 patients hospitalized in Denmark following ingestion of corrosive substances. Adults >15 years of age comprised 75/179 (42%) of cases. Adult suicide attempts accounted for 61% of adult corrosive substance ingestions, and more than half of these patients had a history of psychiatric illnesses. The majority (94%) of ingestants were liquids. Of 12 adults ingesting hydrochloric acid (HCl), there were 6 fatalities (Christesen Citation1994).
de Ferron et al. (Citation1987) conducted a retrospective study of 193 adult patients ingesting liquid chlorine bleach, comprising 37% of all corrosive ingestions treated in the authors’ hospital. All patients underwent fiberoptic endoscopy on the day of ingestion and 38% were found to have serious grade 2 or 3 corrosive lesions. Emergent surgical intervention was required for 10 patients who developed complications within the first 3 weeks post-ingestion. Surgical intervention was required 6 months post-ingestion in 6 patients who developed strictures. These authors noted that ingestion of liquid chlorine bleach mainly causes gastric lesions and perforation from secondary necrosis may occur after a latent period of 2–26 d (de Ferron et al. Citation1987).
Sarfati et al. (Citation1987) reported a series of 484 adults who ingested corrosive substances. There were 250 patients who developed superficial esophageal, gastric, or duodenal lesions, but had healing without sequelae. Emergent surgical intervention was required in 44 patients (9%) and 24 of these died. Of the remaining 190 patients (39%) who had esophageal or gastric ulceration without necrosis, 92 (48%) recovered without sequelae, 3 died of aorto-esophageal fistulas, 12 (6%) survived after undergoing surgical intervention for complications, and 83 (44%) developed esophageal or gastric strictures requiring endoscopic or surgical treatment (Sarfati et al. Citation1987).
Meredith et al. (Citation1988) reported a case series of 9 youths who ingested concentrated sodium hydroxide (lye), mistaking it for wine. There were no fatalities. Patients (n = 3) with second degree oral injuries did not require surgical intervention. Of the other 6 patients, all required laparotomy with gastrostomy or jejunostomy, 1 required immediate esophagogastrectomy, and 3 required subtotal or total gastrectomy. Three of these 6 patients subsequently underwent esophageal replacement while the other 3 required repeated dilations. All 9 patients were found to be able to maintain oral nutritional status at 2-year follow-up. These authors concluded that liquid lye (NaOH) ingestion requires a much more aggressive approach to diagnosis and treatment than is generally recommended for ingestion of other corrosive substances (Meredith et al. Citation1988).
In a descriptive study of 91 Spanish adult patients, Rodriguez Vargas et al. (Citation2016) noted that ingested corrosive chemical substances were the following: bleach (sodium hypochlorite) ingested by 71 of 91 patients (78%), hydrochloric acid (muriatic acid) ingested by18 of 91 patients (20%), and sodium hydroxide (caustic soda) ingested by2 patients (2%). Mean volume of ingested corrosive chemical substances was 16 ml (range: 30-500 ml) (Rodriguez Vargas et al. Citation2016).
Sore throat, nausea, vomiting, and abdominal pain were the most frequently noted symptoms on presentation. Lesions developed in 46% of patients: acid ingestions, 100%; alkaline ingestions, 33%. Of those patients who developed lesions, oropharyngeal lesion occurred in 5 patients (5%), esophageal lesions in 24 patients (26%), gastric lesions in 36 patients (40%), and duodenal lesions in 12 patients (13%) (Rodriguez Vargas et al. Citation2016).
On endoscopy, 10 patients (11%) had Zargar classification grade 1 lesions, 16 patients (18%) had had grade 2 lesions, and 15 patients had grade 3 lesions. Those patients ingesting acidic corrosive substances, 12 patients had grade 3 lesions. Complications included esophageal stricture in 2 patients (2%), gastric stenosis in 7 patients (8%), and both esophageal and gastric stenosis in 3 patients (3%). Two patients were treated with dilation and 10 patients had surgical intervention (Rodriguez Vargas et al. Citation2016).
Struck et al. (Citation2016) reported a case series of 28 patients treated in their institution over a 10-year period from 2005 to 2014. Acidic chemical substances were ingested by 6 patients (21%) and base chemical substances were ingested by 22 patients (79%). Suicide attempt resulted in ingestion in 18 patients (64%); 9 of these patients (50%) had a prior history of psychiatric disorders (depression, schizophrenia) and 6 of them had a history of prior suicide attempts (Struck et al. Citation2016).
Treatment in the Intensive Care Unit was required in 20 patients (71%). Fourteen patients required endotracheal intubation and ventilator support; 3 of these presented difficult airway management. Tracheotomy for airway management was required in7 cases (25%); one of which was an emergency awake procedure mandated by progressive upper airway obstruction. EGD was done in 21 cases (75%). CT-scanning was done in 11 cases (39%). Emergent surgical procedures were necessary in 5 cases (18%). Mortality was 60% in the emergent surgery cases.
Fatality in the total study group was 18%. Predictors for mortality in these patients were associated with: requirement for endotracheal intubation (p = 0.012), abnormal CT-scan findings (p = 0.001), necessity for tracheostomy (p = 0.048), higher Zargar scores on endoscopy (p = 0.006), and requirement for emergent surgical intervention (p = 0.005) (Struck et al. Citation2016).
Wijeratna et al. (Citation2015) described 9 adult cases of acid ingestion (sulfuric acid, n = 5; acetic acid, n = 1; unknown acid, n = 2) in Sri Lanka. The acute stage management was not specified except in 1 case where gastric perforation and peritonitis occurred. All patients presented with gastric outlet obstruction (Wijeratna et al. Citation2015).
Surgical interventions included the following: repair of the damaged stomach and loops of small bowel in the one fatal acute case; retro-colic iso-peristaltic gastro-jejunostomy; gastric resection with sparing of an uninjured fundus area and iso-peristalic jejunal loop reconstruction; gastric outlet junction injury with fistula closure, distal stomach resection, and proximal gastro-jejunostomy followed by right colonic transposition due to first surgical failure (fatal case); gastrectomy with retro-colic jejunal anastomosis; distal stomach strictures resection and retro-colic loop gastro-jejunostomy; ante-colic iso-peristaltic proximal gastrojejunostomy; esophageal dilation and pyloroplasty; proximal gastrojejunostomy; balloon dilation of the esophagus and proximal anticolic gastrojejunostomy (fatal case) (Wijeratna et al. Citation2015).
Selected case reports of interest
Pediatric patients
A 7-month-old male bit into a laundry detergent pod. Initial symptoms were crying and occasional coughing. Vomiting occurred during EMS transport to hospital. On hospital presentation, the child was noted to have somnolence, upper airway wheezing with retractions, and moderate respiratory distress with oxygen desaturation (%O2 saturation in the 80s). The child was profoundly acidotic with an arterial pH of 6.50. Chest X-ray showed a right upper lobe infiltrate. A seizure occurred and the child had a cardiac arrest 3 h after exposure and could not be resuscitated. Autopsy findings included mild hyperemia of the oropharynx and trachea without burns or ulcerations, a small amount of greenish-brown gastric contents, right-sided pulmonary congestion, and cerebral edema (Mowry et al. Citation2014).
Gharib et al. (Citation2016) reported the case of a 1.5-year-old child who ingested an alkaline drain cleaning substance. The child had corrosive lesions in his mouth, upper chest, and buttock that appeared to be caused by the corrosive agent. The delay to hospital admission was 12 h. Endoscopy revealed a circumferential ulcer with necrosis and a grade 3 esophageal corrosive lesion. A barium swallow examination on post-ingestion revealed gastrointestinal reflux but no major stricture formation (Gharib et al. Citation2016).
Kua et al. (Citation2015) reported the case of a 16-month-old male who accidentally ingested a granular product containing sodium hydroxide and sodium carbonate. The child presented with necrotic lesions on the lips and oral mucosa. Endoscopy found erythema and deep ulcerations from the oral cavity to the first section of the duodenum. Laryngoscopy on day 2 found white and charred lesions of the epiglottis and the anterior first third of the vocal cords. At 1 week postingestion, repeat laryngoscopy found complete destruction of the vocal cords and the epiglottic cartilage was denuded. Supportive care was with parenteral nutrition and ventilatory management through a tracheostomy (Kua et al. Citation2015).
Andrade et al. (Citation2016) reported the case of a child from a developing country with accidental acid ingestion. This child developed gastric outlet obstruction as a complication. The gastric outlet obstruction was successfully treated with endoscopic balloon dilation (Andrade et al. Citation2016).
An 8-½-year old male with Down syndrome and a prior history of gastric and cardiac corrective surgery for congenital abnormalities accidentally ingested battery acid (concentrated sulfuric acid). Severe corrosive injuries of the esophagus and stomach resulted. Dilation procedures (32 procedures over 15 months) and stenting were not successful, while salivary fistula surgery was suggested, in the interim the patient was treated with a nasogastric tube with perforations above the stenotic area for passage of fluid and saliva. These authors then developed a new type of double lumen nasogastric tube for protection of the esophageal closure and which placement was associated with decreased needs for additional endoscopic procedures and hospitalization (Woynarowski et al. Citation2014).
Adult patients
Tseng et al. (Citation2011) reported an unusual case of corrosive injury of the esophagus and stomach. An 84-year-old woman with dementia was admitted to the emergency department 9 h after ingesting a hand-warmer packet which contained activated charcoal, a salt, vermiculite, and 50% iron powder. Abdominal X-ray showed radiopaque material in the upper abdomen. Endoscopy revealed a confluent black mass with iron adherent to the esophageal and gastric mucosa. The mucosa was also friable, had erosions, and was bleeding. The adherent coating mass could not be removed with the endoscope. Proton pump inhibitors (PPI) were administered intravenously. Serum iron was elevated and was attempted to be treated with intravenous deferoxamine (desferrioxamine). The patient survived and was discharged from the hospital after 84 h of observation (Tseng et al. Citation2011).
Keh et al. (Citation2006) reported two cases of corrosive ingestion with injury to the upper gastrointestinal tract. The first patient was a 23-year-old male with a learning disability who accidentally ingested a cupful of 30% caustic soda (sodium hydroxide) and had vomited nearly immediately. On admission to the hospital, he had a hoarse voice, was short of breath, and drooling. Physical examination revealed an erythematous, swollen tongue and an inflamed and edematous oropharynx. After transfer to the intensive care unit following endotracheal intubation, he was treated with a PPI and total parenteral nutrition (TPN). On endoscopic examination 2 d later, he was found to have a grade 3 esophageal injury. A barium swallow study two weeks after ingestion revealed a long stricture from just distal to the hypopharynx to the esophageal-gastric junction. Treatment was with progressively time-spaced dilation (bougienage) using a guide wire under fluoroscopy (Keh et al. Citation2006).
The second patient was a 33-year-old male with a past medical history of overdose and assaults who was admitted to the emergency department after ingesting approximately 40 ml of battery acid in a deliberate self-harm attempt (Keh et al. Citation2006). CT-scan of the chest and abdomen showed a thickened distal esophagus and stomach, but no evidence of perforation; there were small bilateral pleural effusions. Endoscopy performed early in the clinical course revealed inflammation and ulceration of the esophagus and pharynx with bleeding and circumferential ulceration of the esophageal mucosa at 23 cm; the stomach was filled with blood. Acute treatments included PPI, TPN, corticosteroids, and broad-spectrum antibiotics. After attempts of conservative therapy, it became necessary to perform a surgical Roux-en-Y gastrojejunostomy to bypass the stricture (Keh et al. Citation2006).
Six fatality case reports from the AAPCC NPDS database had more clinical details (Mowry et al. Citation2013, Citation2014, Citation2016).
A woman aged 69 years intentionally ingested a glass of muriatic acid (most often 30–35% hydrochloric acid) in a successful suicide attempt. Initial symptoms/signs were dysphonia and mild abdominal distress. The clinical course progressed to multi-organ system failure and demise (Mowry et al. Citation2013).
A man aged 32 years ingested an unknown amount of an industrial-strength drain cleaner (acid/alkali not reported). Copious bloody vomiting occurred during EMS transport and in the ED. Difficulty swallowing and abdominal pain were noted. Necrotic tissue was found on limited endoscopy. An esophageal-left bronchus fistula developed and the patient died (Mowry et al. Citation2013).
A 22-year-old male with a history of bipolar disorder and previous suicide attempts ingested an alkali-containing drain cleaner, slit his writs, and jumped out of a 2nd story window. On evaluation, findings were the following: right lower lobe aspiration pneumonitis and pneumomediastinum with extensive intraperitoneal hemorrhage consistent with esophageal and gastric perforation. At emergent exploratory surgery, there was extensive liquefaction necrosis of nearly all abdominal organs; non-survivable findings. The patient died 15 h after emergency department admission (Mowry et al. Citation2016).
A 43-year-old female ingested a sulfuric acid-containing drain cleaner and ethanol for intentional suicide. Initial findings were oropharyngeal burns and mild ulceration. The patient subsequently developed airway compromise and died. At autopsy, there was non-survivable necrosis of the stomach and intestines (Mowry et al. Citation2016).
An 81-year-old female with dementia ingested a laundry detergent pod. Initial findings were a swollen tongue and difficulty swallowing. The patient died approximately 36 h after emergency department admission. No autopsy was performed (Mowry et al. Citation2016).
Following an intentional ingestion of 16 oz of a hydrochloric acid based toilet bowl cleaner, a 68-year-old female presented to hospital 2 h later (Gummin et al. Citation2017). Findings in the Emergency Department included hematemesis, respiratory distress, bloody secretions in the oropharynx, coarse wet rales throughout the lung fields, diffuse abdominal tenderness, metabolic acidosis, dark brown aspirates from both nasogastric and endotracheal tubes, and right lung opacification on chest X-ray. Endoscopy revealed hypopharynx ulceration, necrotic esophageal lesions, and diffuse gastric necrosis. The patient died 12 h post-admission (Gummin et al. Citation2017).
Nguyen et al. (Citation2014) reported a case of accidental laundry detergent pod ingestion causing esophageal and gastric injury in an adult. After ingestion, a grade 2a esophageal injury as well as erythema and ulcerations of the gastric mucosa ensued (Nguyen et al. Citation2014).
Furukawa et al. (Citation2014) reported the fatal case of an 88-year-old woman who accidentally ingested approximately 1/3 of a bottle of a liquid neutral detergent containing a surface active agent (40 w/w%). At autopsy, what seems to have been aspiration of this substance caused congested and edematous lungs with corrosive changes in the bronchi (Furukawa et al. Citation2014).
While ingestions of household bleach (sodium hypochlorite at concentrations of <6%) are usually considered to be benign, a 32-year-old female who ingested approximately 240 ml of such a product developed a grade 1 esophageal lesion and severe gastric necrosis (Jacobs et al. Citation2014).
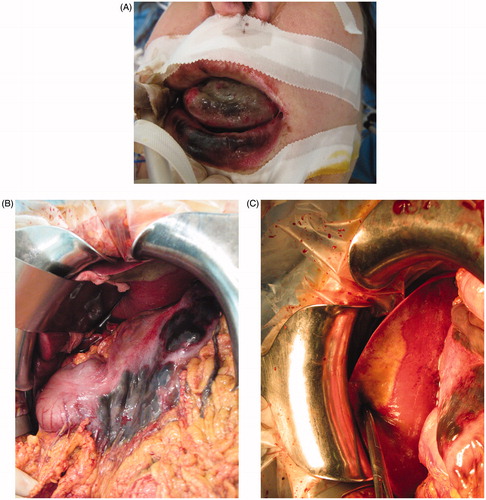
Jacquemin (Citation2014) described the case of a 52-year-old man who ingested approximately 500 ml of caustic soda (sodium hydroxide; Destop®) in a suicide attempt. The patient also had skin exposure on the face, neck () and right arm, and was admitted to the Burn Center about 4-½ h post-ingestion. Despite having had water skin decontamination, no improvement was achieved before hospital admission. The skin and the mouth were immediately decontaminated with Diphoterine® solution (Laboratoire Prevor, Valmondois, France) (Lynn et al. Citation2016). Gastroscopy done on admission revealed extensive necrosis of the esophagus along all its length, stage 3b.
Figure 1. (a) Sodium hydroxide (caustic soda; Destop®) ingestion. Additional skin exposure on face, neck, and right arm. 4-½ hours post-ingestion. (b and c) 8 d post-ingestion. The facial and oral lesions are completely healed.

The stomach appeared erythematous with congestive areas and areas with petechia on the large curvature. There were also many superficial ulcers, stage 2a. No attempt was made to decontaminate the esophagus. Bronchoscopy did not reveal any lesions. Skin lesions on the arm were dressed with sulfadiazine and those on the face with bacitracin/polymixin. Emergent esophagostomy, gastrostomy, and esophageal stripping were performed. Three weeks after admission, excision of necrotic skin tissue and mesh autograft transplantation was done, and the wounds healed adequately within 8 d. At this time, the facial and oral lesions were completely healed () (Jacquemin Citation2014).
A 53-year-old woman ingested about 200 ml of caustic soda (sodium hydroxide) in a suicide attempt. Her husband tried to make her to vomit before bringing her to hospital (Jacquemin Citation2014). On admission (), the lips and the tongue were injured. Gastroscopy showed edema of the esophagus, the mucosa was inflammatory without ulceration, and the fundus was necrotic. Abdominal CT-scan revealed pneumoperitoneum and extensive necrosis of the gastric wall at the fundus. Emergent surgical intervention was performed; however, there was necrosis of the anterior wall of the stomach with perforation (), edema of the duodenum, and injury of segment II of the liver (). Esophagectomy and jejunostomy were performed. Twelve days after admission, bronchoscopy revealed necrosis of the carina and of the posterior wall of the trachea. The patient developed mediastinitis and died 16 d after admission (Jacquemin Citation2014).
Figure 2. (a) Caustic soda (sodium hydroxide) ingestion. Lips and tongue injuries. (b) At emergent surgery, necrosis of the anterior stomach wall with perforations. (c) At emergent surgery, duodenal edema and injury of segment II of the liver.
Boonekamp et al. (Citation2018) reported the case of a man aged 65 years who accidentally ingested a 5-g sodium hypochlorite solid pellet. Six hours after ingestion, the patient developed aphonia and severe dyspnea, prompting evaluation by nasofibroscopy which revealed necrosis and edema of the glottis and supraglottic area. Intravenous corticosteroids were administered, the patient was endotracheally intubated, and underwent a tracheotomy. Treatment included administration of a proton pump inhibitor (esomeprazol) and antibiotics for a respiratory infection. Favorable clinical progress permitted removal of the tracheotomy cannula after 17 d (Boonekamp et al. Citation2018).
Menéndez et al. (Citation2015) reported the case of a 32-year-old male who ingested ferric chloride. On presentation, the patient had decreased sensorium and erosions in the buccal cavity and oropharynx. Metabolic acidosis was present and blood ferritin level was 1400 mg/dL. Abdominal and pelvic CT-scan revealed extensive pneumoperitoneum and free fluid in the abdominal cavity. Emergent surgical intervention consisted of an exploratory laparotomy, total gastrectomy and esophagectomy, and placement of a feeding jejunostomy tube, as well as washing and drainage because of perforated necrosis of the stomach (Menéndez et al. (Citation2015)).
Wijeratna et al. (Citation2015) reported a case series of 9 patients with corrosive acid ingestion. Complications noted were gastric outlet obstruction. This was treated with a bypass surgical procedure in 5 patients and resection in 4 patients. Outcomes were successful in all cases (Wijeratna et al. Citation2015).
Gastocele occurred as a complication in 8 corrosive ingestion patients with grade 3b lesions who did not receive early surgical intervention. Surgical treat was with a two-step partial gastrectomy (antrectomy) and later esophageal treatment performed an average of 2 and 8 months post-ingestion. No post-operative deaths occurred and the long-term survival rate was 83% (Zerbib et al. Citation2014).
Vewzakis et al. (Citation2016) reported 3 illustrative cases showing the spectrum of adult suicidal corrosive chemical ingestion. The first case was a 77-year-old female with a prior history of depression. She ingested an unknown corrosive chemical substance in a suicide attempt and presented with dyspnea, chest and abdominal pain, and progressive respiratory failure. Airway management and chest and abdominal CT-scanning were done. Endoscopy revealed a Zargar scale IIIB injury with perforation. Emergent surgery was accomplished, but the patient died on post-operative day 1 (Vewzakis et al. Citation2016).
The second patient was a 46-year-old female with a prior history of depression who ingested an acidic household cleaning product. She presented with nausea, vomiting, and respiratory distress. Evaluation found a Zargar grade 3a lesion with intraperitoneal perforation. Emergent exploratory laparotomy was done and later restoration with colonic interposition. At follow-up, this patient was healthy and functional (Vewzakis et al. Citation2016).
The third patient was a 33-year-old female with no prior psychiatric history who ingested an acidic household cleaning product and also jumped from a height, resulting in multiple orthopedic injuries. Endoscopy showed only a Zargar grade 1 mucosal injury. The patient developed esophageal and pyloric stenosis, successfully treated with dilation therapy. On follow-up, this patient was healthy and functional (Vewzakis et al. Citation2016).
Pathophysiology of corrosive ingestion injuries
The extent of GI tract injury following ingestion of a corrosive substance depends on a number of factors, including: ingested product formulation, concentration, ingested volume, pH, viscosity, mucosal surface contact duration, and the absence or presence of food in the stomach (Caravati Citation2014; Wax and Yarema Citation2007; Betalli et al. Citation2009; Contini and Scarpignato Citation2013). Corrosive substances may also cause injury to any tissue(s) they come in contact with, such as the skin, eyes, mucous membranes, and lungs (Caravati Citation2014; Betalli et al. Citation2009).
Alkali corrosive substances cause a saponification or liquefaction necrosis and do not form a coagulum as do acid corrosive substances (Caravati Citation2014; Wax and Yarema Citation2007; Betalli et al. Citation2009; Contini and Scarpignato Citation2013; Bonavina et al. Citation2015; De Lusong et al. Citation2017; Grossi et al. Citation2017). They can, therefore, penetrate more deeply into exposed GI tract tissues and tend to cause more severe injuries than do acids (Caravati Citation2014; Wax and Yarema Citation2007; Betalli et al. Citation2009; Contini and Scarpignato Citation2013; Bonavina et al. Citation2015). With acid corrosive ingestions, the esophageal injuries tend to be less severe, but injuries to the stomach, pylorus, and duodenum are more common (Caravati Citation2014; Wax and Yarema Citation2007; Betalli et al. Citation2009; Contini and Scarpignato Citation2013; Grossi et al. Citation2017). However, ingestion of either alkaline or acidic corrosive substances can result in significant adverse effects such as stricture formation, perforation, and potentially fatal bleeding (Caravati Citation2014; Wax and Yarema Citation2007; de Lusong et al. Citation2017).
Four stages in the natural history of corrosive ingestions have classically been described. The first stage is one of necrosis when tissue invasion with bacteria and polymorphonuclear leukocytes occurs. Following this, increased tissue damage is caused by vascular thrombosis. Sloughing of superficial tissues then occurs over the subsequent 2–5 d, with the tensile strength of such damaged tissue being low for as long as 3 weeks. This latter can predispose patients to delayed GI tract perforation which may occur up to 14 d or more after the initial insult. Then, formation of collagen deposition, granulation tissue, and re-epithelization occur as part of the healing process, unfortunately sometimes resulting in esophageal stricture development from scar contraction which may be noted over a period of weeks to years (Caravati Citation2014; Wax and Yarema Citation2007; Lupa et al. Citation2009; De Lusong et al. Citation2017).
Children with unintentional corrosive ingestions and psychiatric patients with intentional corrosive ingestions seem to be at special risk of serious complications (Wax and Yarema Citation2007; Contini and Scarpignato Citation2013).
In a cohort of 100 Egyptian children (mean age: 5.9 ± 2.6 years) with a history of ingestion of a corrosive chemical substance (90% of whom ingested potassium hydroxide in household cleaning products) and developed esophageal strictures were evaluated with endoscopic biopsies (Eskander et al. Citation2019). These children had undergone between 16 and 100 endoscopic dilation sessions (mean: 37.2 ± 14.9). Microscopic histological evaluation revealed that 85% of these children had evidence of chronic esophagitis (hyperkaratosis, hyperplasia, subepithial fibrosis), 13% had reactive atypia (severe neutrophilic intraepithelial inflammatory cellular infiltration), and 2 patients (2%) were found to have mild squamous cell dysplasia (Eskander et al. Citation2019).
Clinical aspects of corrosive substances ingestion
Upper airway compromise is a life-threatening early manifestation of corrosive substance ingestion. Laryngeal edema may necessitate the need for endotracheal intubation or creation of a surgical airway by cricothyrotomy or tracheostomy (Caravati Citation2014; Wax and Yarema Citation2007). Rarely, a traacheoesophageal fistula may develop (Gupta et al. Citation2015).
In the acute phase, common complaints are oral pain, vomiting, abdominal pain, and drooling. Various other signs and symptoms include respiratory distress, crying, coughing, dysphagia, odynophagia, hematemesis, wheezing, coughing, and stridor. Such signs and symptoms as pain, crying, dysphagia, and drooling tend to be more correlated with buccal mucosal injury, and are not predictive of injuries lower in the GI tract. It is difficult to predict significant GI tract lesions from particular signs/symptoms, although prolonged dysphagia and drooling were more predictive in some studies and vomiting and stridor were more predictive of more significant GI lesions than oropharyngeal tissue injury (Wax and Yarema Citation2007).
GI tract perforation or hemorrhage in the acute phase may require emergent surgical intervention (Wax and Yarema Citation2007). It is of note that respiratory function abnormalities following corrosive substances ingestion are more common in children than adults (Betalli et al. Citation2009).
For those patients who survive the acute phase, more long-term complications include esophageal stricture formation (more common in those with circumferential corrosive chemical injuries), quite delayed cicatricial carcinomas (usually developing 30–50 years after initial exposure), pyloric and gastric antrum stenosis, and duodenal atonicity (Caravati Citation2014; Keh et al. Citation2006; Wax and Yarema Citation2007; Contini and Scarpignato Citation2013; de Lusong et al. Citation2017).
No specific laboratory testing is useful in patients with corrosive ingestions, although some standard tests may be useful in assisting symptomatic and supportive care (Wax and Yarema Citation2007; Contini and Scarpignato Citation2013; de Lusong et al. Citation2017). A chest X-ray and abdominal film may be useful in the acute phase to look for stigmata of perforation, such as peritoneal or mediastinal free air or pleural effusion (Caravati Citation2014; de Lusong et al. Citation2017). CT-scan may also be useful for such purposes (Caravati Citation2014; Contini and Scarpignato Citation2013; Jagpal et al. Citation2014; Gill et al. Citation2019). The best method for determining the severity and location of tissue injuries is EGD with a flexible fiberoptic scope which should be performed in the initial 12–24 h, as later evaluations carry a greater risk of perforation (Caravati Citation2014; Wax and Yarema Citation2007; Lupa et al. Citation2009). Those procedures performed earlier than 12 h may not disclose the full extent of injury and performing endoscopy later than 48 h post-ingestion is not recommended because of the increased of esophageal perforation (Wax and Yarema Citation2007; Lupa et al. Citation2009).
Prognostic value of early upper GI tract endoscopy
Pediatric patients
Betalli et al. (Citation2008) performed an observational multicenter study of the medical records of 162 children who presented to hospital with accidental corrosive ingestions, asking the question: “Is endoscopy always indicated?” These authors divided presenting signs and symptoms into minor (oral and/or pharyngeal lesions, vomiting) and major (dyspnea, drooling, hematemesis) categories. All patients were evaluated using endoscopy within the first 12–24 h post-ingestion. Mild esophageal lesions were noted in 143/168 (88.3%) of patients. Severe (third-degree) lesions were found in only 19 patients (11.7%). When signs and/or symptoms were not present, the risk of severe esophageal lesions was very low. In this case series, the presence of 3 or more signs and/or symptoms was an important predictor of severe corrosive esophageal lesions (Betalli et al. Citation2008).
Temiz et al. (Citation2012b) conducted a study of 206 children evaluated by EGD for corrosive substances ingestion. Ingestants were acidic in 72 (34.9%) of cases, alkaline in 56 (27.2%), liquid household bleach in 62 (30.1%), and unknown in 16 (7.8%). These authors noted that many studies of pediatric corrosive substances ingestion have focused mainly on esophageal lesions, so they proposed to evaluate gastric lesions as well. Positive clinical findings were considered to be: hematemesis, oropharyngeal fibrinous lesions, severe mucosal edema, vomiting, drooling, oropharyngeal hyperemia, and respiratory distress, and were noted in 149 (72.3%) of patients. Fifty-seven patients (27%) were asymptomatic (Temiz et al. Citation2012b).
EGD findings were grade 0 (no lesions) in 86 (41.7%) of patients, grade 1 in 49 (23.8%), grade 2a in 42 (20.4%), grade 2b in 28 (13.6%), and grade 3a in 1 (0.5%) patient. An esophageal stricture developed in 13/35 patients (37%) of patients with grade 2a, 2b, or 3a lesions. There was no significant difference in the rate of esophageal stricture development between patients who ingested acid as opposed to alkali corrosive substances. A severe gastric injury was found in 38 (18.5%) of patients and was significantly more common in the group with acidic ingestions. Among the 149 patients with clinical findings as listed above, 49 (32.9%) had no esophageal lesions and 117 (78.5%) had no gastric lesions (Temiz et al. Citation2012b).
However, among patients with no symptoms 20 (35.1%) had esophageal lesions and 8 (14%) had severe gastric lesions, underlining the generally recognized fact that clinical findings are not reliable predictors of the presence of corrosive upper GI tract lesions. Six patients developed pyloric stenosis, only 2 of whom responded to balloon dilation. These authors concluded that EGD is an effective method for diagnosing the presence of upper digestive tract lesions and can help avoid unnecessary treatment in patients having no or only mild corrosive injuries (Temiz et al. Citation2012b).
Betalli et al. (Citation2009) stated that endoscopy can be done earlier, but not later, than 24 h post-ingestion. Initial endoscopy is indicated in all symptomatic children, but the indications in asymptomatic children remain controversial. Repeat endoscopy is indicated for monitoring the evolution of lesions and for possible stricture development (Betalli et al. Citation2009). A French SFED consensus publication states that the initial endoscopy should be done between 6 and 24 h postingestion (Lachaux et al. Citation2011).
Based on a review of 458 pediatric corrosive substance ingestion patients, Bosnali et al. (Citation2017) in dividing the specific type of corrosive ingestant into 8 groups of increasing corrositivity, noted that endoscopy was not necessary if the ingestant was in a lower corrosivity group and the patient could be fed easily, endoscopy was not necessary. However, in those patients ingesting substances in the higher corrosivity groups, endoscopy could decrease duration of hospitalization (Bosnali et al. Citation2017).
In 2014, the American Society for Gastrointestinal Endoscopy (ASGE) published modifications in endoscopic practice for pediatric patients (ASGE Standards of Practice Committee et al. Citation2014). These recommendations are the following:
Endoscopy in children should be done by those trained in pediatric procedures, whenever possible
When endoscopy must be performed by those trained in adult procedures, coordination with pediatricians and pediatric specialists is recommended
Endoscopy should be performed within the first 24 h following ingestion of a corrosive substance
Age-appropriate procedural and resuscitation equipment should be available
Personal trained in pediatric life support including airway management should be readily available during procedures performed under sedation
For infants and children weighing <10 kg, an endoscopy scope <6 mm diameter should be used
A standard adult endoscope should be used in children weighing at least 10 kg
Percutaneous endoscopic 12F or 16F gastrostomy tubes should be placed in children weighing <50 kg.
An ESPGHAN (European Society for Paedatric Gastroenterology Hepatology and Nutrition) guideline for pediatric gastrointestinal endoscopy was published in 2017 with reference to endoscopic evaluation of infants, children and adolescents (ages 0–18 years) (Trangali et al. Citation2017). In this guideline, diagnostic indications include caustic ingestion and therapeutic indications include dilation of esophageal or upper gastrointestinal tract strictures and perforation. Signs and symptoms prompting endoscopy include dysphagia, odynophagia, chest pain, feeding difficulties, and suspicion of corrosive chemical substance ingestion (Trangali et al. Citation2017).
Adult patients
Poley et al. (Citation2004) retrospectively reviewed the cases of 179 adolescent and adult patients with corrosive substance ingestion evaluated in a hospital in Rotterdam, The Netherlands between 1980 and 2002. Of the total, 153 patients, 85% deliberately ingested the corrosive substance in a suicide attempt. All patients underwent endoscopy within 8 h of admission. Of those patients ingesting acids, more than 85% ingested glacial acetic acid which seemed to cause more severe local mucosal tissue damage than other acids and also more commonly resulted in systemic toxicity (Poley et al. Citation2004).
Patients ingesting acids had significantly longer periods of hospitalization and were more frequently admitted to the Intensive Care Unit than were patients ingesting other corrosive substances. Systemic complications developed more frequently in acid-ingesting patients (20/85; 24%) than in alkali-ingesting patients (3/94; 3%). Systemic complications were most often multiple. Mucosal injury was more common in the acid-ingesting group as compared to the alkali-ingesting group (median grade 2 with acid ingestion versus median grade 1 with alkali). More patients who ingested acids had at least grade 2 mucosal lesions (60/85; 71%) compared to the alkali-ingesting group (46/94; 49%). There was an overall mortality rate of 14/179 (8%), especially in the acid-ingesting group (14% versus 2% for the alkali-ingesting group). Most patients who died had systemic complications including intractable hemorrhaging secondary to DIC and hemolysis, multiorgan system failure, sepsis, or a combination of such complications. Deaths most often occurred within a period of 24–48 h after Intensive Care Unit admission. In 3 cases, death was due to GI tract perforation (Poley et al. Citation2004).
Sites of GI tract lesions were most commonly the esophagus (n = 141; 79%), followed by the stomach and especially the gastric fundus and body (n = 91; 51%); duodenal lesions were not common (n = 11; 6%). While stricture formation was similar in the acid-ingesting and alkali-ingesting groups, perforations occurred only in the acid-ingesting group. Strictures developed in 29 patients (32 strictures), generally at 6–12 weeks post-ingestion. One such patient died of systemic complications before dilation treatment could be initiated. The rest of the patients were treated either with dilation or surgical intervention. The majority of strictures were esophageal (n = 25), followed by gastric strictures (n = 5), but were rare in the duodenum (n = 2). Some patients had more than one stricture (Poley et al. Citation2004).
Patients were initially treated with dilation (21/29; 72%). Seven patients with strictures had primary surgical intervention because it was judged that the probability of successful dilation therapy was low, either because of the length (extent) of the stricture or because more than one stricture was present. The 21 patients initially treated with dilation therapy comprised 10/21 (34%) with dilation alone, but in 11 cases (38%) surgical intervention was done because dilation was unsuccessful. The number of dilatation therapy sessions was a median of 6 (range: 1–84). No perforations occurred during dilation therapy (Poley et al. Citation2004).
These authors found by logistic regression analysis that the severity of mucosal lesions as determined by endoscopy was the most predominant predictive factor for systemic complications and fatal outcomes. As the severity of mucosal lesions increased by grade, so did the incremental risk increase by a factor of 9 (Poley et al. Citation2004).
Cabral et al. (Citation2012) reviewed the cases of 315 patients referred for corrosive injuries of the upper gastrointestinal tract between 2002 and 2007. Endoscopy was performed emergently on admission. Those patients with grades 1–3a lesions were managed non-operatively, while emergent surgical intervention was performed for those patients with grades 3b and 4 lesions. Esophageal reconstruction was performed in those patients having had emergent esophageal resection and for those who developed esophageal strictures not responsive to dilation (Cabral et al. Citation2012).
On initial endoscopy, no lesions were found in 73 (23%), mild injuries suitable for non-operative management were noted in 158 (50%), and severe injuries requiring surgical intervention were found in 84 (27%). Surgical procedures performed were exploration in 88 (28%) of patients and resection in 76/88 (86%). Emergent mortality occurred in 7% of patients who all had severe corrosive injuries. These authors concluded that emergent endoscopic injury grading is the main factor in predicting outcome (Cabral et al. Citation2012).
In a retrospective cross-sectional study, Alipour-Faz et al. (Citation2017b) evaluated the accuracy of endoscopy’s ability to predict the depth of esophageal injury in 54 adult patients with corrosive ingestions evaluated over a 7-year period. Patients with either grade 1 injuries or obvious emergent indications for surgery (grade 4) were excluded. Mean mucosal injury evaluated by primary endoscopy using the Zargar scale was compared with histological findings. The primary endoscopic findings found grade 2 injuries in 28 patients (51.85%) and grade 3 injuries in 19 patients (35.18%). However, tissue biopsy pathologic findings reviewed by blinded pathologists revealed 21 patients (38.88%) having grade 1 injuries, 14 patients (25.92%) having grade 2 injuries, and 19 patients (35.18%) having grade 3 injuries. Initial endoscopy sensitivity and specificity of endoscopy were, for grade 2 injuries, respectively, 50.00 (23.01–76.96) and 47.50 (23.04–63.97). These same values for grade 3 injuries were, respectively, 100.00 (82.35–100) and 80.00 (63.06–91.56) (Alipour-Faz et al. Citation2017b).
The overall accuracy for initial endoscopy for predicting the depth of mucosal lesions following corrosive substance ingestion, based on the Zargar scale, was good for grade 3 lesions (87%), but did not have good accuracy for grade 2 lesions (48%). These authors urge caution in developing treatment plans for such patients based only on endoscopic findings (Alipour-Faz et al. Citation2017b).
In patients aged >14 years with ammonia ingestions, Gelu-Simeon et al. (Citation2018) found that in a case series of 43 patients that on endoscopic evaluation, submucosal hematoma of the gastric wall was a distinctive clinical sign in 15 cases (34.8%). Of these 43 patients, oropharyngeal lesions were present in 30 (69.8%) and associated with attempted suicidal ingestions in 18 of these patients. Such submucosal hematomas should be differentiated from gastric necrosis to preclude confusion with gastric necrosis which might be an indication for surgical intervention (Gelu-Simeon et al. Citation2018).
Lu et al. (Citation2014) conducted a seven-year retrospective study of 108 adult patients who ingested corrosive substances in an attempt to identify predictive factors for the development of esophageal stricture and gastric outlet obstruction utilizing a modified Zargar endoscopic mucosal injury grading scale. All patients were evaluated with endoscopy within 24–48 h of the ingestion. Esophageal and gastric lesions were evaluated separately (Lu et al. Citation2014).
Of the 108 medical records examined retrospectively, ingestions substances were mainly acidic (90 cases) with 18 cases of alkaline substance ingestion. Ten patients died during the acute injury phase, 2 from esophageal perforation, 1 from hematemesis with apnea, and 7 from aspiration pneumonitis. Of the 98 survivors, endoscopy showed grade 3 mucosal lesions in the esophagus (n = 43; 39.8%), in the stomach (n = 58; 53.7%), and in the duodenum (n = 13; 12%). Of those patients having grade 3 or worse mucosal injuries in the esophagus, were more likely to develop esophageal strictures (58.6% versus 43.5% for those with lesser injuries; p < 0.046). Of those patients with grade 3 or worse gastric or duodenal mucosal injuries compared to those with lesser injuries, patients were more likely to develop gastric outlet obstruction (stomach injuries (100% versus 43.5% p < 0.001; duodenal injuries, 43.8% versus 8%, p < 0.001). Age greater than 60 years was an independent risk for from mortality following corrosive chemical substance ingestion (Lu et al. Citation2014).
Relook endoscopy (endoscopy on day 1 following corrosive substance ingestion compared to the same procedure on day 5) was evaluated by Kochhar et al. (Citation2017). In 62 adult patients, the relook endoscopy on day 5 had a higher specificity (83 versus 65%) and a higher Positive Predictive Value (60 versus 41%) for predicting the risk of developing an esophageal stricture. These authors concluded that endoscopy on day 5 post-ingestion is a more effective predictor of development of esophageal stricture and gastric scarring, and that the day 1 endoscopy over-predicts the grade of such injuries (Kochhar et al. Citation2017).
In a retrospective nation-wide database analysis of 21,682 patients, Abbas et al. (Citation2017) evaluated whether there was an association between patients having early endoscopy following corrosive chemical substances (24–48 h) and those having later (>48 h) post-ingestion. These authors evaluated the relationships in the 2 groups for clinical outcome (poor clinical outcome: systemic complications of fatality), economic factors (prolonged hospitalization and cost of treatment), and various clinical factors.
Of these 21,862 patients, 6,011 (37%) with the majority undergoing endoscopy within 24–48 h post-ingestion and 17% having the procedure at >48 h post-ingestion comparison of the 2 groups showed that the late endoscopy group had a 3-fold increased poor clinical response (Odds Ratio = 2.7; p < 0.001), a 4-fold increase in higher-cost hospitalization (Odds Ratio = 4.6; p < 0.001), and a 5-fold increased long-term hospitalization (Odds Ratio= 4.9; p < 0.001). No significant clinical outcomes difference was noted in those undergoing endoscopy within 24 h post-ingestion and those having the procedure from 24 to 48 h post-ingestion. These authors concluded that early endoscopic evaluation could potentially result in better clinical outcomes and decreased economic costs (Abbas et al. Citation2017).
Contrast-enhanced radiographic imaging
Acutely, contrast-enhanced radiographic imaging (barium swallow) is generally not recommended for initial evaluation of patients with corrosive substance ingestion because it is usually not sensitive enough to detect injury to the mucosa. Barium swallow may be useful after the third post-ingestion week to identify stricture development (Ciammaichella et al. Citation2019).
99mTC-Pertechnate or sucralfate scintigraphy
While acknowledging that endoscopy is the “gold standard” in the evaluation of gastric mucosal injury following corrosive chemical substance ingestion, Rai et al. (Citation2013) suggested that 99m TC Pertechnate scintigraphy may be useful in the evaluation of gastric viability after such ingestions (Rai et al. Citation2013). However, in an observational study of 197 children with corrosive substances ingestions, 40 patients had both endoscopy grading and underwent 99mTc sucralfate scanning (Nondela et al. Citation2018).
Twenty-seven children (68%) had low-grade adhesions on 99mTc sucralfate scan and all had low-grade endoscopic lesions (Zargar scale). None of these children developed residual esophageal strictures. Thirteen children (23%) had high-grade 99mTC sucralfate scan adhesions, had high-grade endoscopic lesions (Zargar scale), and 3 of these (23%) had stricture formation. These authors concluded that endoscopy is not required for pediatric patients with low-grade 99mTc sucralfate scan adhesions. However, those with high-grade 99mTc sucralfate scan adhesions should undergo esophagoscopy (Nondela et al. Citation2018).
Comparison of endoscopy and chest/abdominal CT-scan
Wightman et al. (Citation2016) suggest radiography and CT-scan (chest and abdominal) may be useful to determine the extent of injury in some cases.
Lurie et al. (Citation2013) performed a retrospective study of 23 adult Israeli patients with corrosive ingestion admitted to a hospital in Haifa between 2000 and 2012 in order to compare the ability of chest/abdominal CT-scan with EGD to predict the severity of injury and the need for emergency laparotomy.
Ingested corrosive chemical substances were acids (12/23; 52.2%), alkalis (6/23; 26.1%), household bleach (3/23; 13%), and unspecified corrosive substances (2/23; 8.7%). Intentional ingestions comprised 18/23 (78.3%) and the remaining five patients had unintentional ingestions. Of these 23 patients, 7 (30.4%) underwent emergent laparotomy: 6 because of necrosis of the esophageal or gastric wall, and 1 with a hyperemic gastric wall. Twelve patients required mechanical ventilation. There were 5 deaths during the hospital stay (21.7%) (Lurie et al. Citation2013).
Comparing CT-scan to endoscopy, the endoscopy grading of lesion severity was higher than the CT-scan grading in 14/23 patients (60.8%). Of note, 8 patients (66.6%) with grade 3 lesions as assessed by endoscopy had only grade 1 lesions as assessed by CT-scan. In 2 cases (8.7%), the CT-scan lesion grading was higher than the grading by endoscopy, and in 5 cases (21.7%) the grading by both modalities was comparable. In the 5 fatal cases, endoscopy gradings were the following: 2 were grade 3a, 1 was grade 3b, and in 2 cases the endoscopy could not be completed secondary to severe edema. The CT-scan gradings in these 5 cases were the following: 1 was grade 0, 2 were grade 1, and 3 were grade 3. Overall, CT-scan was less sensitive and more specific than endoscopy and had higher positive predictive values and lower negative predictive values (Lurie et al. Citation2013).
Also noted on CT-scan were pulmonary infiltrates compatible with aspiration pneumonitis in 11 patients (48%), while for 3 of these patients same-day chest X-ray did not reveal such infiltrates. Overall, these authors concluded that chest/abdominal CT-scan as compared to endoscopy tends to underestimate prediction of severe outcomes such as the requirement for emergent laparotomy or death during the acute phase of corrosive chemical substance ingestion. They recommend that CT-scan should not be the only basis for the decision of whether to perform emergent surgery (Lurie et al. Citation2013).
Two Letters to the Editor were published in January 2014 in the medical journal Clinical Toxicology. The first was a comment on the above study and the second was the authors' reply (Fil et al. Citation2014; Bentur et al. Citation2014). The Fil et al. (Citation2014) Letter essentially asked a number of questions of the authors, especially for more data on patient characteristics, and did note that there are several factors which might delay endoscopy, while CT-scan perhaps maybe a more readily available means of evaluation.
Bentur et al. (Citation2014) provided as much of the requested additional information as possible. Inclusion criteria included performing both endoscopy and CT-scan within 24 h of admission, although in some cases the history of the time of ingestion was not reliable which precluded using time of ingestion as an inclusion criterion. Regarding additional patient characteristics, more severe endoscopic findings and worse outcomes were found in patients with intentional ingestion. For those patients found to have grade 2b or 3 lesions on endoscopy (n = 14), 5 died and 7 underwent emergent laparotomy (Bentur et al. Citation2014).
Of the total 14 patients with more severe lesions, 6 ingested acid, 5 ingested alkali, 1 ingested bleach, and 2 ingested an unspecified corrosive substance. Of those patients who died, 3 ingested acid and 2 ingested alkali. Of those patients who required emergent laparotomies, 5 ingested acid and 2 ingested alkali. All 5 patients who died had intentionally ingested the corrosive substances. Of those requiring emergent laparotomies, 6 had intentional ingestions and 1 had an unintentional ingestion. Of the total 14 patients with grade 2 b and 3 lesions, 12 had intentional ingestions and 2 had unintentional ingestions (Bentur et al. Citation2014).
Median times from hospital admission to both endoscopy and CT-scan in the 14 patients with grade 2b and 3 lesions were not statistically different, so time spans between the two tests cannot explain the lesion severity underestimation by CT-scan. At all times during the study, CT-scan devices were of third generation, so poor quality of CT-scans also cannot explain the underestimation of lesion severity by this modality (Bentur et al. Citation2014).
Ryu et al. (Citation2010) retrospectively reviewed a series of 49 patients with corrosive ingestions evaluated between 1998 and 2009. Severity of esophageal injury was graded from thoracoabdominal CT-scans based on the extent of edema of the esophageal wall and adjacent tissue damage. Esophageal stricture formation was determined by esophagoscopy (Ryu et al. Citation2010).
Using a CT-scan grading scale, grade 3 injury was the most common finding (n = 20; 40.8%). Grades 1, 2, and 4 injuries were as follows: grade 4 (n = 14; 28.6%); grade 2 (n = 9; 18.4%); grade 1 (n = 6; 12.2%). CT-scan grading for esophageal stricture resulted in a slightly larger detection rate as compared with an endoscopic grading system. These authors concluded that noninvasive CT-scans could be useful in estimating the occurrence of esophageal stricture formation in patients with corrosive substance ingestions (Ryu et al. Citation2010).
Bonnici et al. (Citation2014) retrieved 277 published papers regarding corrosive substance ingestion in a comprehensive literature search. Of these, 37 published papers were relevant to the question of “should computerized tomography replace endoscopy in the evaluation of symptomatic ingestion of corrosive substances?” The above-described two retrospective studies did not convince these authors that CT-scan should replace early (<12 h postingestion) fiberoptic eophagoscopy in the evaluation of patients with corrosive substance ingestion (Bonnici et al. Citation2014).
More recent publications including a consensus report from a comprehensive literature review and 2 international conferences which included anesthesiologists, endoscopists, surgeons, and toxicologists have stated that CT-scans may indeed be of use in the clinical decision of whether to perform emergent esophagectomy or other surgical procedures (Bonavina et al. Citation2015; Chirica et al. Citation2016).
In a prospective cross-sectional study 34 adult patients with corrosive ingestions were studied for comparative results of CT-scan and endoscopy in predicting the extent of upper gastrointestinal tract damage (Bahrami-Motlagh et al. Citation2017). Agreement rates between these two assessment modalities for esophageal and gastric injuries were, respectively, moderate (K = 0.38; p = 0.001) and fair (K = 0.17; p = 0.038). Sensitivity and specificity of CT-scan for diagnosis of esophageal injury were, respectively, 96.29 (79.11–00.80) and 57.14 (20.23–88.19).
These authors concluded that CT-scan and endoscopy findings correlation as pertains to injury grading is not sufficient to preclude the need for endoscopy (Bahrami-Motlagh et al. Citation2017). Other authors have stated that esophageal and gastric CT-scan is better than traditional endoscopy for the purpose of triaging patients for emergent surgical intervention or observation (Chirica et al. Citation2017; Methasate and Lohsiriwat Citation2018) and for assessing the risk of stricture formation (Gill et al. Citation2019).
Bruzzi et al. (Citation2018) compared the accuracy of CT-scan versus endoscopy in the acute evaluation of 152 adult patients at risk of developing esophageal stricture formation following corrosive chemical substance ingestion. In this study, CT-scan was more efficacious than acute endoscopy for predicting which patients were at risk for developing esophageal strictures and alone was equal to a combined CT-scan-endoscopy protocol. These authors concluded that CT-scan was more efficacious for predicting which corrosive substance ingestion patients were at risk for developing esophageal strictures and commented that endoscopy might be dispensed with (Bruzzi et al. Citation2018).
Yonemaru et al. (Citation2016) described the case of a 77-year-old female with a prior history of lower urinary tract cancer treated with chemotherapy that ingested 100 ml of a toilet bowl cleaner containing 9.5% hydrochloric acid in a suicide attempt. Endoscopy was deferred because of the rick of iatrogenic esophageal perforation. Repeated contrast-enhanced CT-scanning revealed edematous abnormalities but no evidence of perforation. A repeat Ct-scan on day 2 postingestion found mediastinal emphysema. The patient did require tracheostomy and mechanical ventilation for some time because of development of glottic edema noted on fiberoptic bronchoscopy. Conservative and supportive treatment resulted in a reasonably good outcome and the patient could be discharged from the surgical ward on post-ingestion day 21 (Yonemaru et al. Citation2016).
The DROOL score
Based on a prospective review of 202 children with a history of corrosive substance ingestion within the preceding 48 h admitted to a hospital in Anatolia, Turkey, between 2004 and 2011, Uygun et al. (Citation2012) proposed the DROOL Score () as a means of initial assessment.
Table 4. The DROOL score (adapted from Uygun et al. Citation2012).
In this case series of 202 pediatric patients, a DROOL Score </= 4 was a good predictor of esophageal stricture formation (100% sensitivity; 96.63% specificity; 85% Positive Predictive Value; 100% Negative Predictive Value). All patients in this study with esophageal stricture were treated with orogastic balloon dilation. Of 249 sessions with such treatment, there were 4 esophageal perforations, and all were treated conservatively (Uygun et al. Citation2012).
The issues of decontamination measures
The current treatment for corrosive chemical GI injuries is to observe the evolution of the lesions and to intervene as indicated. There are no specific proven medications or decontamination measure(s) to stop or limit lesion evolution. However, it is strictly not recommended to induce emesis, as this could expose the esophagus twice to the corrosive chemical with the risk of additional tissue injury.
Controversy exists about dilution and neutralization therapy (Ciammaichella et al. Citation2019). In vitro experiments showed that dilution does not provide any benefit (Maull et al. Citation1985). There is also the possibility that neutralization might result in an exothermic reaction with heat release which could add a thermal injury to the chemical injury. Rumack and Burrington (Citation1977) used vinegar (dilute acetic acid) to neutralize sodium hydroxide. While there was no difference for solid sodium hydroxide, an increase of heat was observed with dissolved sodium hydroxide (Rumack and Burrington Citation1977). In the study by Maull et al. (Citation1985), a minor temperature change was observed while a good effect on pH was measured. Dilute acetic acid was also used in a study in cats (Leape Citation1974); half of the experimental animals’ deaths were observed when diluted acetic acid was used to neutralize a 5% potassium hydroxide injury.
In humans, dilution with milk or water immediately after corrosive ingestion remains quite controversial and is likely of little clinical value (Mamede and De Mello Filho Citation2002; Wax and Yarema Citation2007; Chibishev et al. Citation2012). Other GI decontamination measures such as induced emesis with sirup of ipecac, gastric lavage, and administration of activated charcoal have fallen into disfavor over a number of years due to the potential risks and lack of substantiating evidence of efficacy (Wu and Lai Citation1993; Wax and Yarema Citation2007; Lachaux et al. Citation2011; Ciammaichella et al. Citation2019); some authors state that these are contraindicated (Riffat and Cheng Citation2009; Chibishev et al. Citation2012). Attempting neutralization by oral administration of mild vinegar, lemon juice, or orange juice for alkali ingestions or milk, eggs, or antacids for acid ingestions is also considered to be contraindicated by some authors (Chibishev et al. Citation2012).
Overall, standard gastric decontamination measures are unlikely to be efficacious and innovative therapy(ies) to stop or limit a chemical agent’s diffusion and corrosive potential has yet to be elucidated.
Other potential therapeutic measures
Administration of corticosteroids in an attempt to prevent stricture formation has remained controversial for many years (Lupa et al. Citation2009; Lachaux et al. Citation2011; Vandenplas Citation2017). Conflicting data have been published, and evidence of efficacy from prospective clinical trials is mostly lacking (Ferguson et al. Citation1989; Mamede and De Mello Filho Citation2002; Caravati Citation2014; Fulton and Hoffman Citation2007; Wax and Yarema Citation2007; Chibishev et al. Citation2012; Ormeño Julca Citation2016; Katibe et al. Citation2018). One 3-year study including 24 patients with penetrating mucosal lesions secondary to ingestion of lye or acids found that methylprednisolone administration was beneficial in moderately severe injuries following solid lye ingestion, but was not beneficial for severe injuries following ingestion of liquid lye or acids (Hawkins et al. Citation1980).
A randomized pediatric clinical trial published by Anderson et al. (Citation1990) noted that administration of corticosteroids did not produce a significant difference in esophageal stricture formation. The number of patients enrolled in this study, however, was rather low (Anderson et al. Citation1990). A meta-analysis of 572 adult corrosive ingestion patients found no difference in the incidence of esophageal stricture formation in patients with second- and third-degree mucosal injuries (Pelclová and Navrátil Citation2005).
In a preliminary survey of members of the World Society of Emergency Surgery, 25% or respondents recommended corticosteroid administration to all patients, 29% recommended corticosteroids for some patients depending on severity of lesions, and 46% did not recommend corticosteroids for any patients (Kluger et al. Citation2015). A search in the US National Library of Medicine Clinical Trials.gov (accessed 9 July 2019) did not retrieve any ongoing studies on this issue.
Antibiotics are considered to only be administered in cases where there is evidence of perforation or infection; prophylactic use is not recommended (Caravati Citation2014; Wax and Yarema Citation2007; Chibishev et al. Citation2012; Lu et al. Citation2014). In a review of recommendations for pediatric corrosive substances ingestion, Betalli et al. (Citation2009) recommended antibiotic administration only for patients with grade 3 lesions.
In a preliminary survey of members of the World Society of Emergency Surgery, 34% of respondents recommended antibiotic administration for all patients, 32% recommended antibiotics only for patients requiring surgical intervention, and 34% recommended antibiotic administration depending on the severity of lesions (Kluger et al. Citation2015). A French SFED consensus publication recommended antibiotic treatment with cephalosporins and gentamicin (Lachaux et al. Citation2011).
Administration of sucralfate, H2 antagonists, and/or proton pump inhibitors (PPIs) has been advocated by some authors, particularly for patients with grade 2 and 3 lesions (Betalli et al. Citation2009; Riffat and Cheng Citation2009; Lachaux et al. Citation2011; Chibishev et al. Citation2012; Lu et al. Citation2014; Struck et al. Citation2016). PPIs reduce the amount of acid in the stomach by blocking the enzyme hydrogen-potassium ATPase, with the intention of allowing already present ulcers in the esophagus, stomach, or duodenum to heal (MedicineNet.com Citation2014).
In a prospective study of 13 adult patients with corrosive ingestion, administration of the PPI, omeprazole combined with withholding oral intake until their condition stabilized, there was a significant difference in healing as shown by endoscopy before and after omeprazole administration. There was no hospital mortality during follow-up (Cakal et al. Citation2013).
Topical mitomycin-C and intralesional triamcinolone have been administered during dilation procedures in attempts to reduce post-dilation recurrence of esophageal strictures (Shub Citation2015; Nijhawan et al. Citation2016; Arnold and Numanoglu Citation2017; Vandenplas Citation2017; Methasate and Lohsiriwat Citation2018). One study compared these 2 interventions (Méndez-Nieto et al. Citation2015). The mitomycin-C group was collected from a non-randomized, prospective, longitudinal study compromising 16 patients from 2009 to 2012. The intralesional triamcinolone group for comparison was from a retrospective cohort of 34 patients treated from 2002 to 2009 (Méndez-Nieto et al. Citation2015). A second study described 21 pediatric patients with long-segment esophageal strictures treated with topical mitomycin C after endoscopic esophageal dilatation on multiple occasions. Resolution of dysphagia was noted after 14.3 ± 5.7 dilations with topical mitomycin C applied on two to six occasions. There was no recurrence at short- or mid-term follow-up (El-Asmar et al. Citation2015). However, in one study of 11 pediatric cases treated with topical mitomycin C, 5 of 11 patients (45%) did not respond favorably to this treatment and two of them required re-do esophageal surgery (Madadi-Sanjani et al. Citation2018).
Comparing the number of dilation procedures required, those patients administered intralesional triamcinolone required a medium number of 11 dilations (range: 4–24), while those treated with topical mitomycin-C required a median of 4.5 (range: 3–8) of such procedures (p < 0.001) (Méndez-Nieto et al. Citation2015). These authors concluded that topical mitomycin-C administration can be recommended to reduce the number of dilation procedures required in patients with esophageal 99mTcstricture following corrosive chemical ingestion (Méndez-Nieto et al. Citation2015).
A systematic review and meta-analysis performed by Katibe et al. (Citation2018) of 763 publication from which 244 patients were included in randomized clinical trials concluded that there was no benefit of corticosteroid administration in preventing development of esophageal stricture formation
Stents and nasogastric tubes
When esophageal stricture formation following corrosive chemical ingestion does not respond satisfactorily to dilation measures, an esophageal stent maybe placed (Martin Cano et al. Citation2012; Shub Citation2015; Methasate and Lohsiriwat Citation2018). Three types of esophageal stents are available: self-expandable plastic stents (SEPS), fully-covered self-expandable metallic stents (FCSEMS), and biodegradable stents. SEPS and FCEMS are left in place for 6 weeks and removed by 12 weeks post-insertion. Biodegradable stents do not require removal (Methasate and Lohsiriwat Citation2018).
Esophageal stents can migrate with an incidence of 40%. Clinical efficacy assessed by relief of dysphagia is approximately 33% and may not last long-term. Therefore, placing an esophageal stent is considered a last resort for treating recalcitrant esophageal stricture (Methasate and Lohsiriwat Citation2018).
Nutrition
Because of GI tract injury following corrosive substance ingestion, normal nutrition may be compromised or impossible. Patients may thus develop a hypercatabolic state with a negative alkali balance (Chibishev et al. Citation2012). Artificial nutrition may be required based on the extent of esophageal or gastric injury found by flexible endoscopy.
For patients with grades 1 and 2a lesions, total parenteral nutrition (TPN) can be begun during the first 24–48 h, followed by institution of a liquid diet on about the 10th day, which can be advanced toward a regular diet as tolerated (Chibishev et al. Citation2012). Patients with grade 2b and 3 lesions require “esophageal rest” with no intake by mouth. In a Turkish study of 202 pediatric corrosive ingestions, TPN was only used for children with GI tract perforation (Uygun et al. Citation2012).
Nutrition can be provided by several means: nasogastric or nasoenteral tube, gastrostomy or jejunostomy tube, or central venous TPN (Chibishev et al. Citation2012). Such measures may – but are not conclusively proven to – reduce the risk of post-corrosive ingestion stenosis and strictures (Chibishev et al. Citation2012). A French SFED consensus publication noted that enteral nutrition administered by nasogastric tube is as efficacious and well-tolerated as that by jejunostomy (Lachaux et al. Citation2011).
A retrospective study of 30 Spanish patients who ingested corrosive substances over a 7-year period between 2000 and 2007 found an overall mortality of 43.3% (Muñoz Botero et al. Citation2010). Weight loss was noted in 46.9% of these patients and a negative nitrogen balance in 62.5%. Sixteen of these patients were managed with a combination of enteral or parenteral nutrition over a mean time of 24 ± 22 d. Mortality, duration of hospitalization, and final albumin values were significantly different between the moderate versus severe GI tract injury groups (Muñoz Botero et al. Citation2010). Some of these patients had surgical procedures for perforation or hemorrhage (n = 3), esophago-gastropancreatico-duodenumectomies (n = 3), esophagectomies (n = 2), total gastrectomies (n = 1), subtotal gastrectomies (n = 1), partial duodenumectomy (n = 1), and jejunumectomy (n = 1) (Muñoz Botero et al. Citation2010).
Follent et al. (Citation2017) discussed two pediatric cases illustrative of dysphagia and deficient feeding skills following alkaline substance ingestion. In both cases, abnormal outcomes consisting of delayed oral motor skills, a restricted variety of dietary intake, and difficult mealtime behaviors were present, resulting in delayed recovery of oral intake consistent with age. At 2-year post-ingestion follow-up, both children required modification of oral food and fluid intake and supplemental gastrostomy feedings. Consultation with a feeding specialist may assist in evaluation and early development of targeted dietary rehabilitation (Follent et al. Citation2017).
Early bougienage
Pediatric patients
When corrosive chemical GI tract exposures induce narrowing of the esophageal lumen or decreased motility in the distal esophagus, physicians may introduce a plastic or metal cylinder into and through the esophagus to limit stricture formation.
Tiryaki et al. (Citation2005) retrospectively compared the results of early prophylactic bougienage with those of dilation begun after the onset of stricture formation in 125 children with corrosive ingestions admitted to a hospital in Ankara, Turkey between 2000 and 2003. Severity of corrosive lesions was determined by early rigid endoscopy under general anesthesia using the Zargar grading scale. The patients' ages ranged from 7 d to 13 years and 27% were symptomatic at the time of admission. The main presenting symptom was dysphagia. The most common corrosive substances ingested were potassium hydroxide, sodium hydroxide, and sulfuric acid which were sold locally in both solid and liquid forms for household use; the most significant injuries occurred following ingestion of corrosive liquid substances (Tiryaki et al. Citation2005).
Of the 125 pediatric patients, 71 (57%) had no mucosal injury as determined by rigid endoscopy. Of the remainder, 11 had grade 1 lesions, 15 had grade 2a lesions, 23 had grade 2b lesions, and 5 had grade 3 lesions. Thus, esophageal corrosive mucosal injuries were found in 54 patients and 32 (26%) later developed esophageal strictures that were successfully managed with dilation therapy (Tiryaki et al. Citation2005).
Patients with grade 1 injuries did not require any specific treatment. Four patients with grade 2a injuries had only minimal stricture formation that resolved following 1-5 dilations. Of patients with grade 2b injuries, 4 had mild, 13 had moderate, and 6 had severe strictures. Those patients with grade 3 injuries all had severe esophageal stricture formation. Of the 20 patients treated with an early bougienage protocol, the strictures resolved over a 6-month period. In the 8 patients treated with dilation only after strictures developed, the strictures resolved over 1 year of dilations in 5 patients, and over 6, 18, and 24 months of dilation in the other 3 patients. Two patients treated with early bougienage had perforations, but did not require surgical intervention (Tiryaki et al. Citation2005).
Surgical intervention with gastrostomy was performed in 3 patients with esophageal perforation and in 5 patients with severe strictures, but these could be closed within 12 months. Two patients developed pyloric stenosis and pyloroplasties were performed. Dysphagia was present in 5 patients with severe mucosal injuries even though strictures had resolved. Esophageal dilation therapy was continued infrequently in these 5 patients with good results. There were no fatalities in this case series (Tiryaki et al. Citation2005).
Thus, early bougienage helps to decrease development of esophageal strictures.
Adult patients: long-term self-bouginage
A case of an 82-year-old patient treated over a 40-year period for esophageal stricture with self-bouginage was reported by Gambardella et al. (Citation2018). This patient had ingested caustic soda (sodium hydroxide) in a suicide attempt at age 23 years and for 40 years had done reasonably well, when emergency department presentation for esophageal obstruction prompted endoscopic removal of a food fragment. Later, the patient developed dysphagia, heartburn, and nocturnal reflux. Barium swallow examination revealed stenosis of the middle and lower third of the esophagus and delayed emptying. Endoscopic bougie dilations were thus performed at monthly intervals, with significant relief of symptoms (Gambardella et al. Citation2018).
Comparison of antegrade versus retrograde dilation methods
Hawkins (Citation1988) reviewed 59 patients who had a total of 687 esophageal dilation procedures over a 17-year period. Of these, 79% of strictures were secondary to ingestion of corrosive substances and accounted for 89% of the dilation procedures. Antegrade procedures were performed 389 times (57%) resulting in 7 cases of iatrogenic esophageal perforation. Retrograde procedures were performed 298 times (43%) and no iatrogenic perforations occurred. This author concluded that retrograde dilation procedures were safer (Hawkins Citation1988).
Endoscopic balloon dilation therapy for gastric outlet obstruction
Balloon dilation seems to be as efficacious as other dilation techniques and has a lower iatrogenic perforation risk (Shub Citation2015). Kochhar and Kochhar (Citation2010) reviewed the use of endoscopic balloon dilation for all types of benign gastric outlet obstruction, including those caused by ingestion of corrosive substances. Approximately 1/3 of patients who ingest strong acidic or alkaline corrosive substances develop gastric outlet obstruction. While surgical intervention has most often been the treatment for corrosive substance ingestion-induced gastric outlet obstruction, there is a place for treatment with endoscopic balloon dilation in such patients. These authors also note that, as compared to gastric outlet obstruction secondary to peptic ulcer disease, patients with corrosive substance ingestion have more recurrences and require a larger number of dilation treatments (Kochhar and Kochhar Citation2010).
Uygun et al. (Citation2013) reported a retrospective study of 38 pediatric patients with corrosive esophageal strictures treated with fluoroscopic balloon dilation over an 8-year period from 2004 to 2012. Patients were divided into 2 groups: those who began fluoroscopic-guided balloon dilation early (a mean of 15 d post-ingestion); and those who began the same treatment later (a mean of 34 d post-ingestion. Strictures were defined as short or long. Balloon sizes were gradually increased (Uygun et al. Citation2013).
Overall, 369 balloon dilations were done in these 38 pediatric patients (median age: 3.5 years; range: 14 months–14 years). Six patients were still receiving dilation procedures at the time of publication, 1 patient was lost to follow-up, a child treated with a stent was excluded from analysis, and 3 children were transferred back to their referring hospitals, leaving 27 patients successfully treated with fluoroscopic-guided balloon dilation (Uygun et al. Citation2013).
Those children treated early (n = 16) had significantly shorter courses of balloon dilation that those treated late (n = 11). In those with short esophageal strictures, required balloon dilation treatment was significantly shorter than in those with long strictures. Six patients developed iatrogenic esophageal perforations during treatment, but all were managed conservatively and no fatalities occurred. These authors recommended that fluoroscopically-guided balloon dilation has a high success rate (100%) and is safe. Such treatment should be begun early post-ingestion and should use a gentle technique with gradually increasing appropriately sized balloons (Uygun et al. Citation2013).
Surgical interventions
If free air, hemorrhage, severe abdominal or chest pain, or peritonitis are apparent in the acute phase following corrosive substance ingestion, emergent surgery is indicated (Caravati Citation2014; Wax and Yarema Citation2007; Chibishev et al. Citation2012). For late complications, repeated bougienage may be indicated, although repeated procedures carry a risk of late perforation. Other surgical procedures that may be considered include esophageal stent placement, colonic interposition procedures, and either dilation or surgical correction of gastric outlet obstruction (Wax and Yarema Citation2007; Lupa et al. Citation2009; Chibishev et al. Citation2012).
Surgery is indicated for complications such as complete stenosis not treatable by usual conservative methods, a defect of the esophagus or stomach detected by radiographic examinations, or fistula formation (Chibishev et al. Citation2012). To replace the esophagus, currently the jejunum, stomach, or colon can be surgically adapted. Esophagectomy with colon interposition is most commonly done, although gastric transposition is more often recommended for children despite a mortality rate of 5%, anastomotic leakage in 12%, and the need for postoperative dilation for stricture formation in 20% (Chibishev et al. Citation2012).
Surgical interventions for patients with corrosive substance ingestion were reviewed by Zwischenberger et al. (Citation2001) as part of an overall review on the surgical aspects of esophageal disease. They note that esophageal perforation is an emergent condition because survival is decreased when there is a delay in surgical intervention. Causes of esophageal perforation are spontaneous, traumatic, and iatrogenic (with endoscopic procedures being the most common cause) (Zwischenberger et al. Citation2001).
Symptoms and signs of esophageal perforation include pain, vomiting, hematemesis, dysphagia, tachypnea, fever, emphysema, cardiac crunch, chest dullness or hypersonarity, and vary with the perforation site (cervical, thoracic, or abdominal). Chest X-ray can be suggestive in up to 90% of cases, but may appear normal immediately after the perforation. Chest CT-scan may reveal mediastinal fluid and free air at the site of the perforation. Esophagoscopy may reveal the perforation site, but the perforation may be missed if it is hidden in a mucosal fold and endoscopy is therefore not recommended as a primary diagnostic modality (Zwischenberger et al. Citation2001). Early surgical intervention can have a fundamental role in the prevention of acute hemorrhages and complications of perforation (Andreoni et al. Citation1995, Citation1997).
Of iatrogenic esophageal perforations which may be noted immediately during endoscopic procedures, those patients with cervical esophageal perforations have a 94% survival rate, those with thoracic perforations have a 66% survival rate, and those with abdominal perforations have a 71% survival rate (Zwischenberger et al. Citation2001).
Surgical interventions that may be required for patients with corrosive substance ingestion include (Zwischenberger et al. Citation2001; Chiba and Brichkov Citation2014; Ezemba et al. Citation2014; Benjamin et al. Citation2016; Gonzalez et al. Citation2016; Marchesi et al. Citation2016; Tirelli et al. Citation2017; Tannuri and Tannuri Citation2017; Braghetto et al. Citation2018; Predescu and Constantinoiu Citation2018):
Elective gastrostomy with placement of a nasogastric string for retrograde esophageal dilation (often done in pediatric patients)
Intraluminal stent placement plus gastrostomy
Esophagectomy
Insertion of a salivary bypass tube
Exploratory laparoscopy if perforation occurs with resection of all injured organs to prevent injury extension
Esophagectomy with delayed reconstruction
Endoscopic rendez-vous technique for reconstrustion of total esophageal disruption
Emergent pulmonary patch repair for tracheobronchial necrosis
Pharyngo-ileo-colo-anastomosis with vascular blood supply augmentation for complete esophago-gastric necrosis
Pedicled colon interposition
Gastric esophageal reconstruction
Pharyngoplasty with complete esophageal substitution
Chirica et al. (Citation2015a) compared short- and long-term outcomes in patients who underwent reconstruction of the digestive tract following corrosive substance ingestion. Surgical procedures were either colopharyngoplasty (n = 116) or esophagocoloplasty (n = 122) performed between 1993 and 2012. The overall Kaplan–Meyer survivals at 1, 5, and 10 years after colopharyngoplasty were, respectively, 92%, 74%, and 67%. Following esophagocoloplasty, survivals were, respectively, 92%, 83%, and 73%. These percentage survivals were not significantly different. After colopharyngoplasty, quality of life and functional results were impaired compared to esophagocoloplasty (success: 57% versus 95%; p < 0.001). Failure of the surgical procedures was associated with older age and colopharyngoplasty, with only 1/15 (7%) of patients operated after the age of 55 years being self-sufficient for eating and breathing. There was no influence on success rates if the larynx had to be resected during colopharyngoplasty. These authors concluded that a need to associate pharyngeal reconstruction during esophageal reconstruction for corrosive substance injuries had a long-term negative impact on functional outcome (Chirica et al. Citation2015a).
Chirica et al. (Citation2014) compared the outcomes of patients undergoing emergent esophagogastrectomy (n = 14) or total gastrectomy with immediate esophagojejunostomy (n = 12) performed between 1987 and 2013 for full thickness corrosive necrosis of the stomach and mild esophageal injuries. These authors compared early and long-term outcomes in the groups having the two surgical procedures and found no significant difference in emergent morbidity, mortality, or re-operation rates. Length of hospitalization was significantly longer in patients having esophagogastrectomy performed. Functional success was similar between the two groups. These authors concluded that immediate esophagojejunostomy can be performed safely following total gastrectomy for corrosive ingestion injuries and decreases the need for further esophageal reconstruction surgery (Chirica et al. Citation2014).
Chirica et al. (Citation2012) reviewed the outcomes (survival, functional outcomes) of patients who underwent surgical treatment between 1987 and 2006 for severe corrosive injuries (n = 268) or late-onset sequelae (n = 79). The overall Kaplan–Meyer survivals in the severe corrosive injuries group at years 1, 5, 10, and 20 were, respectively, 76.4%, 63.6%, 53.9%, and 44.1%. Advanced age, extended resection, emergent esophagectomy, and tracheobronchial injuries were found to be independent negative predictors of survival. Among the group treated emergently for severe corrosive injuries, 147 (56%) had noted functional success (nutritional autonomy after removal of jejunostomy and tracheostomy tubes). The group treated surgically with esophageal reconstruction for late sequelae had significantly better survival rates and functional success. These authors concluded that when surgery is required to be performed for corrosive substances injuries, it has a persistent long-term negative impact on functional outcome and survival (Chirica et al. Citation2012).
Chirica et al. (Citation2009) noted that retrosternal coloplasty is the “gold standard” for reconstruction of the esophagus in patients with severe lesions following ingestion of corrosive substances. The choice of the left or right colon depends on blood supply and the surgeon’s preference. Attention to associated laryngeal and pharyngeal lesions is required at the time of reconstruction. Mortality is usually <5%, but such post-operative complications as graft necrosis, leakage, and stricture formation at anastomotic sites are common. After coloplasty, 60–80% of patients achieve nutritional autonomy (Chirica et al. Citation2009).
In a series of 12 patients requiring esophageal and gastric resection following corrosive substance ingestion between 1988 and 2001, Munoz-Bongrand et al. (Citation2003) found that the lesions extended to the duodenum and pancreatic head (n = 6), jejunum (n = 4), colon (n = 2), spleen (n = 2), or pancreatic body (n = 1). In these 12 patients, the mean duration of hospitalization was 50 d (range: 15–152). Complications developed in all patients. Re-operation was required in 6 patients who developed extension of corrosive lesions to the colon (n = 4), small bowel (n = 2), and pancreas (n = 2). Three fatalities occurred on post-operative days 17, 20, and 130. Eight patients (75%) subsequently underwent substernal right ileocoloplasty, and 6 (50%) survived the initial resection and subsequent esophageal reconstruction. At follow-up (mean: 5 months; range: 7–87 months), 4 patients (33%) were able to eat normally. These authors concluded that extension of corrosive injuries to surrounding organs is associated with high morbidity and mortality and that massive small bowel or colon extension may be the reasonable limit for surgical resection (Munoz-Bongrand et al. Citation2003). An earlier report from this same group of authors of 9 cases (apparently 9 of the 12 described above) reported similar findings (Cattan et al. Citation2000). Ingested corrosive substances were caustic soda (sodium hydroxide)-based strong alkalis (n = 6), chlorine (n = 1), ammonia (n = 1), and hydrochloric acid (n = 1) (Cattan et al. Citation2000).
Braghetto et al. (Citation2018) described surgical intervention with pharyngo-ileo-colo-anastomosis with micro-vascular blood supply augmentation after esophago-gastrectomy in a 41-year-old patient who ingested an alkaline solution containing sodium hydroxide in a suicide attempt and developed complete esophageal and gastric necrosis. Acutely, after esophago-gastrectomy, enteral nutrition was provided through a jejunostomy. Three years later because of poor management of nutrition and poor quality-of-life, the surgical procedure was performed. Parenteral nutrition and jejunostomy feeding was done post-operatively and after one month oral nutrition was adequate and the jejunostomy tube was removed. At one-year follow-up, the patient continued with oral nutrition with vitamin supplementation (Braghetto et al. Citation2018).
A preliminary survey of members of the World Society of Emergency Surgery reported the following (Kluger et al. Citation2015): emergency surgery was recommended by all survey participants when there were finding of esophageal perforation, free air, or peritonitis. Fifty-two percent of participants recommended laparotomy, while 48% recommended possible laparoscopic procedures. Thirty-one percent of respondents recommended urgent surgical reconstruction for unstable patients, while 69% recommended that urgent reconstruction procedures no be undertaken (Kluger et al. Citation2015).
Rajabi et al. (Citation2015) reviewed the surgical management of upper gastrointestinal tract corrosive injuries in 14 adult patients treated from 1993 to 2011. Six patients had accidental ingestions and 8 were suicide attempts. Ingested corrosive chemicals were the following: nitric acid (n = 4), hydrochloric acid (n = 7), sulfuric acid (n = 2), and a strong base in 1 case. Lesions were noted in the esophagus (n = 13), stomach (n = 7), and pharynx (n = 2) (Rajabi et al. Citation2015).
An acute abdomen developed in 2 patients, and was treated with emergent total gastrectomy and blunt esophagectomy. Other surgical interventions were: substernal esophageal bypass (n = 2), esophageal resection and surgical replacement (n = 9), and gastroenterostomy (n = 1). Mortality (n = 2) was from mediastinitis following esophageal replacement. Esophageal strictures developed in 2 patients with hypopharyngeal reconstructive surgical intervention, one treated with dilation and one with KTP laser treatment and stenting. Five patients developed post-operative complications including proximal anastomotic stricture, regurgitation and salivary fistula, pyloric stenosis, superglottic stricture, left subdiaphragmatic abscess, and anastomotic fistula of the neck (Rajabi et al. Citation2015).
Based on a Delphi technique used by a multipledisciplinary Interacting Group Method, Rollin et al. (Citation2015) proposed a diagnostic and treatment algorithm with the successive questions to be answered: (1) Is a functional larynx present?; (2) Is a patent larynx present; (3) Is a patent esophagus present?; and (4) Is a viable or salvageable stomach present? Based on yes or no answers to these four questions, the algorithm suggests various diagnostic and therapeutic measures that require the participation of a multidisciplinary team (Rollin et al. Citation2015). A similar approach was undertaken in the case of a 10-year-old child with injury of the tongue base, hypopharynx, cricopharyngeus, and esophagus following corrosive chemical substance ingestion (Miller et al. Citation2016).
Awad and Jaffray (Citation2017) reported the outcomes of gastric esophageal replacement in ten pediatric patients, of which two cases were due to corrosive substance ingestions. They noted that among the 8 survivors, all patients developed complications (Awad and Jaffray Citation2017).
Those having early onset of complications postoperatively had anastomotic leahage (2 cases) and stomach compression of the lung (1 case). Those who developed late complications had anemia (8cases), stricture of the anastomosis (7 cases), esophagitis (5 cases), dumping syndrome (2 cases), paragastric hiatal hernia (1 case), gastric outlet obstruction (1 case), Barrett’s esophagus (1 case), long-term inability to swallow (1 case), and recurrent infections of the lower respiratory tract (1 case). In their literature review, these authors found that of 57 publications on this topic, only 3 reported long-term followup which could mask the serious complication of gastric replacement of the esophagus (Awad and Jaffray Citation2017).
For pediatric patients with both esophageal injury/stricture formation and airway injury, an interdisciplinary team approach (Pulmonology, Gastroenterology, and Speech Therapy) has been recommended (Lobeck et al. Citation2016). These authors reported eleven pediatric patients with long gap esophageal atresia (27%; n = 3), tracheoesophageal fistula (18%; n = 2), and necrotizing pharyngitis (9%; n = 1). Surgical intervention was with colonic interposition and major airway reconstruction. Six patients (54%) developed postoperative esophageal stricture, but all patients were able to take some or full oral nutrition (Lobeck et al. Citation2016).
Naamee et al. (Citation2015) reported the case of a 32-year-old male who underwent emergent total esogastrectomy, tracheostomy, and feeding jejunostomy following ingestion of a corrosive chemical substance. Ten days postoperative, bronchoscopy revealed complete tracheal mucosal destruction, extending from the tracheostomy to the carina. Under veno-venous extracorporeal; membrane oxygenation, tracheal reconstruction was performed using a pedicled intercostal muscle flap. A flap biopsy specimen obtained 7 months postoperatively revealed ciliated neoepithelium (Naamee et al. Citation2015).
Ananthakrishnan et al. (Citation2014) reported a series of 105 patients with corrosive substance ingestions treated surgically with esophageal bypass without resection of the damaged esophagus between 1977 and 2008, noting that ingestion of acidic substances was the most common (70% of patients). Substernal bypass using the left colic vessel was performed in 89 patients, while the subcutaneous route was chosen for the remaining 16 patients.
Three fatalities occurred postoperatively. Postoperative complications were necrosis of the conduit (1 patient), pneumothorax (15 patients), cervical anastomotic stenosis (1 patient), cervical anastomotic leak (13 patients), and recurrent laryngeal nerve palsy (6 patients). Seventy-two patients could swallow normally following the procedure, while 33 had some occasional problems swallowing solid food (Ananthakrishnan et al. (Citation2014).
Di Saverio et al. (Citation2015) described two approaches for management of corrosive ingestion depending on whether the endoscopic classification was Zargar’s grade 3a or grade 3b. For patients with grade 3a gastric lesions and equivocal peritoneal signs, emergency diagnostic laparoscopy can be performed in stable patients. For patients with grade 3b gastric lesions with complications of perforation, diffuse peritonitis, and unstable hemodynamic instability, an optional approach to mitigate the extent of injury is “4-tubes ostomy”. The aim of this procedure is to wash out the corrosive substance from the duodenum and jejunum and to avoid primary duodenal closure and performing jejuno-jejunal anastomosis over injured tissues (Di Saverio et al. Citation2015).
A tracheoesophageal fistula may rarely develop following ingestion of corrosive chemical substances. Gupta et al. (Citation2015) reported 3 adolescent cases in whom 5, 9, and 30 mm tracheoesophageal fistulas developed following ingestion of aluminum phosphide (2 cases) or sodium hydroxide (caustic soda) (1 case). Surgical intervention was with neomembranous trachea in all 3 cases, with reinforcement by a pleural flap in 2 cases and an intercostal muscle flap in the third case. Colon interposition was required in two patients and the third had a short-segment resection. All 3 patients were doing well on follow-up visits (Gupta et al. Citation2015).
In a retrospective study of 112 corrosive substance ingestion patients, 23 required emergent surgical intervention (Chang et al. (Citation2018). Those patients who had emergent surgery had the most severe lesions at endoscopy and a fatal outcome in 12 of 23 (47.8%). Factors predicting a fatal outcome were gastrointestinal tract perforation (Odd Ratio = 13.5; p = 0.011) and the need for an unscheduled re-operation (Odds Ratio = 13.2; p = 0.033) (Chang et al. Citation2018).
Montalva et al. (Citation2017) described 7 pediatric patients with corrosive substance ingestion treated surgically with total laparoscopic transhiatal esophagectomy and Gavriliu’s esophagoplasty. Of these children, 2 were able to resume oral feeding following barium swallow evaluation on post-operative day 7. Frequent immediate complications were anastomotic or gastric tube leakage in 57%. This was successfully treated in all cases (100%) with placement of a metallic self-expanding stent. Seventy-one percent of these children developed a stricture which was successfully treated with pneumatic dilation in 67% of patients. Repeated surgical intervention was needed in 43% of these children because of a nonfunctional gastric tube of for anastomosis revision. At 51-month follow-up, 85.7% of these patients were tolerating oral feeding (Montalva et al. Citation2017).
Transoral CO2 laser microsurgery was described in a pediatric case of corrosive chemical substance ingestion who developed pharyngolaryngeal stenosis. Following this procedure, oral feeding was able to be resumed after only one day (Berlucchi et al. Citation2014).
Age as an outcome predictive factor in adult corrosive substances ingestions
Chang et al. (Citation2011) performed a retrospective study of 389 Taiwanese adult patients aged 17–107 years admitted to hospital between the years of 1999 and 2009. Patients were divided into 2 groups according to age: non-elderly (< 65 years; 321 patients; 82.5%), and elderly (>/= 65 years; 68 patients; 17.5%). GI tract mucosal injury was graded using EGD within the first 24 h. Evaluated parameters were the following: gender, ingestion intent, ingested chemical substance, GI and systemic complications, systemic and psychological co-morbidities, mucosal injury severity, and time to death (Chang et al. Citation2011).
Psychological co-morbidities were more common in the non-elderly group. Systemic co-morbidities, severity of mucosal injury, and systemic complications were more common in the elderly group. Systemic complications noted included: aspiration pneumonitis, respiratory failure, DIC, and liver failure. GI tract complications included: hemorrhage, perforation, stricture formation, and fistula formation. Treatment was based upon individual factors, but included medical treatment(s), dilation, and a variety of surgical interventions such as feeding jejunostomy, subtotal gastrectomy, esophagectomy, esophageal reconstruction, and Whipple procedure for perforation (Chang et al. Citation2011).
The necessity for Intensive Care Unit (ICU) admissions and deaths were more common in the elderly group (29.4% versus 8.1% in the non-elderly group), and the cumulative survival rate was lower. Causes of death in the non-elderly group were the following: DIC (3 cases); hemoptysis (4 cases); tracheal perforation (1 case); and respiratory failure (4 cases). In the elderly group, causes of death were the following: DIC (2 cases); hemoptysis (1 case); perforation (1 case); and respiratory failure (8 cases). Those elderly patients with systemic complications had the greatest risk of mortality following corrosive chemical substance ingestion. The GI tract injury severity did not appear to have an impact on the survival of elderly patients (Chang et al. Citation2011).
Caganova et al. (Citation2017) compared the clinical outcomes of corrosive chemical ingestions in 176 adult elderly (>/= 60 years of age) and non-elderly (<60 years of age) patients with corrosive chemical substance ingestions reported to a National Toxicological Information Center is Slovakia from 1998-2015. Mortality in the elderly group was higher than in the non-elderly group (23.0% versus 11.3%; p = 0.041). Fatality in the elderly group was associated with acid and particularly hydrochloride acid ingestion and respiratory complications. Those elderly patients with respiratory complications had the worst clinical outcomes (Caganova et al. Citation2017).
Risk scoring system
A retrospective study by Rigo et al. (Citation2002) of 210 patients with corrosive substance ingestion admitted to a hospital in Modena, Italy between 1982 and 1999 evaluated the use of endoscopy and selected clinical parameters to determine their usefulness in predicting the risk of death. Of these 210 patients, 13 underwent emergent surgical procedures (6.2%) and 25 (11.9%) died.
These authors devised a risk scoring system with values ranging from 1-16, including such factors as ingestion of strong acids, white blood cell count on hospital admission >/= 20,000 cells/mm3, presence of gastric necrosis, deep gastric ulcers, and age. No patient scoring <10 on this risk score system died, and just 1 of the patients scoring > 14 survived (Rigo et al. Citation2002).
The types of corrosive substances ingested were strong acids (28.1%), strong alkalis (17.1%), ammonia (6.7%), bleach (31.0%), and other corrosive or unknown substances (17.1%). Of the 59 patients ingesting a strong acid, 20 died (33.9%). Four of 140 patients ingesting other corrosive substances died (2.9%). The ingestion was intentional in 127 cases (60.5%) and 24 of 25 of the noted deaths followed intentional ingestion. There were no deaths among patients who accidentally ingested a strong acid. Of those who accidentally ingested a corrosive chemical substance other than a strong acid, 1/67 died, whereas 3/73 patients with deliberate ingestion died. Nine of 13 (69.2%) of patients undergoing surgical procedures died, compared to 16/197 (8.1%) treated without surgical intervention (Rigo et al. Citation2002).
The risk scoring system developed by these authors is shown below (adapted from Rigo et al. Citation2002):
Survival varied by the risk scoring value as follows: <10, 166 survivors and no fatalities; 10–11.9, 7/13 (53.8%) non-survivors; 12–13.9, 7/9 (77.8%) non-survivors; >14, 10/11 non-survivors (90.9%). In this study, increasing age was associated with an Odds Ratio for fatality of 2.37 (95% confidence interval, 1.37–4.10) (Rigo et al. Citation2002).
Recent consensus statement and other recent data
More recent data have indicated that CT-scans are a better clinical choice than traditional EGD for deciding if emergent surgery is needed for patients ingesting corrosive substances (Chirica et al. Citation2015a, Citation2015b, Citation2016). A consensus paper reporting the results of the World Society of Emergency Surgery comprehensive literature research and discussed in two international symposia in Italy and Israel has recently been published (Bonavina et al. Citation2015). It is freely available from the National Library of Medicine’s website (http://www.nlm.nih.gov).
Conclusion
Ingestion of corrosive chemical substances can result in devastating GI tract injuries with the risk of perforation and/or hemorrhage and sometimes potentially fatal systemic complications. All current treatment modalities are unsatisfactory, especially in the acute phase where some efficacious measure(s) to prevent sequelae from developing would be highly desirable.
Declaration of interest
The regular employment affiliation of the authors is shown on the cover page. Alan H. Hall, Danièle Henny, and Laurence Mathieu were compensated by Laboratoire Prevor either as consultants or employees for preparation of this review. Diphoterine® solution, developed and marketed by Laoratoire Prevor, Valmondois, France is reviewed in this paper. None of the other authors, Denise Jacquemin, Patrice Josset, Bernard Meyer, have any interest to declare. The preparation of the review, conclusions drawn, and the recommendations made are the exclusive work product of the authors and may not necessarily be those of the employers or financial sponsor of the review. None of the authors have participated in legal or regulatory proceedings during the past five years related to the contents of the paper.
Acknowledgements
The authors thank the anonymous peer reviewers for constructive criticism and suggested additions. These have all been addressed and have significantly improved the article.
References
- Abbas A, Brar TS, Zori A, Estores DS. 2017. Role of early endoscopic evaluation in decreasing morbidity, mortality, and cost after caustic ingestion: a retrospective nationwide database analysis. Dis Esophagus. 30(6):1–11.
- Adedeji TO, Tobih E, Olaosun AO, Sogebi OA. 2013. Corrosive oesophageal injuries: a preventable menace. Pan Afr Med J. 15:11.
- Al-Binali AM, Al-Shehri MA, Abdelmoneim I, Shomrani AS, Al-Fifi SH. 2009. Pattern of corrosive ingestion in Southwestern Saudi Arabia. Saudi J Gastroenterol. 15(1):15–17.
- Alipour-Faz A, Arsan F, Peyvandi M, Oroei M, Shafagh O, Youselfi M, Peyvandi H. 2017a. Epidemiologic features and outcomes of caustic ingestions: a 10-year cross-sectional study. Emergency. 5(1):e56.
- Alipour-Faz A, Yousefi M, Peyvandi H. 2017b. Accuracy of endoscopy in predicting the depth of mucosal injury following caustic ingestion; a cross-sectional study. Emergency. 5(1):e72.
- Anderson KD, Rouse TM, Randolph JG. 1990. A controlled trial of corticosteroids in children with corrosive injury of the esophagus. N Engl J Med. 323(10):637–640.
- Ananthakrishnan N, Subbarao KS, Parthasarathy G, Kate V, Kalayarasan R. 2014. Long term results of esophageal bypass for corrosive strictures without esophageal resection using a modified left colon esophagocoloplasty-a report of 105 consecutive patients from a single unit over 30 years. Hepatogastroenterology. 61(132):1033–1041.
- Anderson KD, Randolph JG, Lilly JR. 1975. Peptic ulcer in children with gastric tube interposition. J Pediatr Surg. 10(5):701–707.
- Andrade M, Sawamura R, Cupo P, Lopes Del Ciampo IR, Fernandes MIM. 2016. Endoscopic treatment of gastric outlet obstruction secondary to accidental acid ingestion in a child. J Pediatr Gastroenterol Nutr. 62(1):90–92.
- Andreoni B, Farina ML, Biffi R, Crosta C. 1997. Esophageal perforation and caustic injury: emergency management of caustic ingestion. Dis Esophagus. 10(2):95–100.
- Andreoni B, Marini A, Gavinelli M, Biffi R, Tiberio G, Farina ML, Rossi A. 1995. Emergency management of caustic ingestion in adults. Surg Today. 25(2):119–124.
- Arévalo-Silva C, Eliashar R, Wohlgelernter J, Elidan J, Gross M. 2006. Ingestion of caustic substances: a 15-year experience. Laryngoscope. 116:1422–1426.
- Arici MA, Ozdemir P, Oray NC, Buyudkeligoz M, Tuncok Y, Kalkan S. 2012. Evaluation of caustics and household detergents exposures in an emergency service. Hum Exp Toxicol. 31:533–538.
- Arnold M, Numanoglu A. 2017. Caustic ingestion in children-A review. Semin Pediatr Surg. 26(2):95–104.
- ASGE Standards of Practice Committee, Lightdale JR, Acosta R, Shergill AK, Chandrasekhara V, Chathadi K, Early D, Evans JA, Fanelli RD, Fisher DA, Fonkalsrud L, et al. 2014. Modifications in endoscopic practice for edatric patients. Gastrointest Endosc. 79(5):699–710.
- Awad K, Jaffray B. 2017. Oesophagealreplacement with stomach: a personal series and review of published experience. J Paediatr Child Health. 53(12):1159–1166.
- Bahrami-Motlagh H, Hadizadeh-Neisanghalb M, Peyvandi H. 2017. Diagnostic accuracy of computed tomography scan in detection of upper gastrointestinal tract injuries following caustic ingestion. Emergency (Tehran). 5(1):e61.
- Balderas AB, Ascves MR, Ramirez PC, Rodriguez FG, Marin J. 2018. Endoscopic findings in the digestive tract secondary to caustic ingestion in children seen at the Emergency Department. Arch Argent Pediatr. 116(6):409–414.
- Bautista Casasnova A, Estevez Martinez E, Varela Cives R, Villanueva R, Villaneuva Jeremias A, Tojo Sierra R, Cadranel S. 1997. A retrospective analysis of ingestion of caustic substances by children. Ten-year statistics in Galicia. Eur J Pediatr. 156:410–414.
- Benjamin B, Agueb R, Vuarnesson H, Tranchart H, Bongrand NM, Sarfati E, Cattan P, Chirica M. 2016. Tracheobronchial necrosis after caustic ingestion. Ann Surg. 264:808–813.
- Bentur Y, Slotky M, Fischer D, Shreter R, Lurie Y. 2014. The role of chest and abdominal computed tomography in assessing the severity of acute corrosive ingestion [Letter]. Clin Toxicol. 52(1):83–83.
- Berlucchi M, Barbieri D, Garofolo S, Stefini S, Peretti G. 2014. Case report: pharyngolaryngeal stenosis in a child due to caustic ingestion treated with transoral CO2 laser microsurgery. Ann Otol Rhinol Laryngol. 123(12):847–851.
- Betalli P, Falchetti D, Giuliani S, Pane A, Dall'Oglio L, de' Angelis GL, Caldore M, Romano C, Gamba P, Baldo V. 2008. Caustic Ingestion Italian Study Group. The results of an Italian multicenter observational study. Caustic ingestion in children: is endoscopy always indicated? Gastrointest Endosc. 68(3):434–439.
- Betalli P, Ross A, Bini M, Bacis G, Borelli O, Cutrone C, Dall’Oglio L, d’Angelis GL, Falchetti D, Farina ML. 2009. Update on management of caustic substance and foreign body ingestion in children. Diag Ther Endosc. Article ID 9698852009;
- Bird JH, Kumar S, Paul C, Ramsden JD. 2017. Controversies in the management of caustic ingestion injury: an evidence-based review. Clin Otolaryngol. 42(3):701–708.
- Bonavina L, Chirica M, Skrobic O, Kluger Y, Andreollo NA, Contini S, Simic A, Ansaloni L, Catena F, Fraga GP, et al. 2015. Foregut caustic injuries: results of the World Society of Emergency Surgery consensus conference. World J Emerg Surg. 10(1):44.
- Bonnici KS, Wood DM, Dargan PI. 2014. Should computerized tomography replace endoscopy in the evaluation of symptomatic ingestion of corrosive substances? Clin Toxicol. 52(9):911–925.
- Boonekamp C, Voruz F, Fehlmann C. 2018. Accidental aspiration of a solid tablet of sodium hypochlorite. BMJ Case Rep. 2018:bcr2018224213.
- Boskovic A, Stankovic I. 2014. Predictability of gastroesophageal caustic injury from clinical findings: is endoscopy mandatory in children? Eur J Gastroenterol Hepatol. 26(5):499–503.
- Bosnali O, Moralioglu S, Celayir A, Pektas OZ. 2017. Is rigid endoscopy necessary with childhood corrosive ingestion? A retrospective comparative analysis of 458 cases. Dis Esophagus. 30(3):1–7.
- Botwe BO, Anim-Sampong S, Sarkodie BD, Antwi WK, Obeng-Nkansah J, Ashong G. 2015. Caustic soda ingestion in children under-5 years presenting for fluoroscopic examinations in an academic hospital in Ghana. BMC Res Notes. 8(1):684.
- Braghetto I, Figueroa M, Sanhueza B, Lanzarini E, Sepulveda S, Erazo C. 2018. Pharyngo-ileo-colo-anastomosis with micro-vascular blood supply augmentation for esophago-gastric replacement due to esophago-gastric necrosis after caustic ingestion. Arq Bras Cir Dig. 31(2):e1381.
- Bruzzi M, Chirica M, Resche-Rigon M, Corte H, Voron T, Safarti E, Zagdanski AM, Cattan P. 2018. Emergency computed tomography predicts caustic esophageal stricture formation. Ann Surg Mar. 12:109–114.
- Cabral C, Chirica M, de Chaisemartin C, Gornet M, Munoz-Bongrand N, Halimi B, Cattan P, Sarfati E. 2012. Caustic injuries of the upper gastrointestinal tract: a population observational study. Surg Endosc. 26(1):214–221.
- Caganova B, Foltanova T, Puchon E, Ondriasova E, Plackova S, Fazekas T, Kuzelova M. 2017. Caustic ingestions in the elderly: influence of age on clinical outcome. Molecules. 22(10):1726.
- Cakal B, Akbal E, Köklü S, Babali A, Koçak E, Taş A. 2013. Acute therapy with a S, Fazekas T, Kuzelova Mintravenous omeprazole on caustic esophageal injury: a prospective case series. Esophagus. 26:22–26.
- Caravati EM. 2014. Acids, and alkali (Chapters 201 and 202). In: Dart RC, editor. Medical toxicology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; p. 1294–1303, 1304–1309.
- Cattan P, Munoz-Bongrand N, Berney T, Halim B, Celerier M. 2000. Extensive abdominal surgery after caustic ingestion. Ann Surg. 213:519–523.
- Cello JP, Fogel RP, Boland CR. 1980. Liquid caustic ingestion. Spectrum of injury. Arch Intern Med. 140(4):501–504.
- Chang J-M, Liu N-J, Pai B-J, Liu Y-H, Tsai M-H, Lee C-S, Chu Y-Y, Lin C-C, Chiu C-T, Cheng HT. 2011. The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol. 11(1):72.
- Chang YH, Chien CY, Chen CC, Fu CY, Hsieh CH, Liao CH. 2018. The surgical strategy in massive corrosive injury in digestive tract: is the extensive surgery appropriate? World J Surg. 42(7):2028–2035.
- Chávez-Aguilar AH, Silva-Báez H, Sánchez-Rodríguez YB, Esparza-Ponce C, Zatarain-Ontiveros MÁ, Barrera de León JC. 2015. [Early complications with colon esophageal substitution for children via retrosternal] [Spanish]. Gac Med Mex. 151(3):323–328.
- Cheng HT, Cheng CL, Lin CH, Tang JH, Chu YY, Liu NJ, Chen PC. 2008. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 8(1):31.
- Chiba S, Brichkov I. 2014. Pulmonary patch repair of tracheobronchial necrosis with perforation secondary to caustc ingestion. Ann Thorac Surg. 97(6):2205–2207.
- Chibishev A, Pereska Z, Chibisheva V, Simonovska N. 2012. Corrosive poisoning in adults. Mater Sociomed. 24(2):125–130.
- Chibishev A, Sikole A, Pereska Z, Chibisheva V, Simonovska N, Orovchanec N. 2013. Severe renal function impairment in adult patients acutely poisoned with concentrated acetic acid. Arh Hig Rada Toksikol. 64(1):153–158.
- Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. 2017. Caustic ingestion. Lancet. 389(10083):2041–2052.
- Chirica M, Brette MD, Faron M, Munoz-Bongrand N, Halimi B, Laborde C, Sarfati E, Cattan P. 2015a. Upper digestive tract reconstruction for caustic injuries. Ann Surg. 261(5):894–901.
- Chirica M, de Chaisemartin C, Munoz-Bongrand N, Halimi B, Célérier M, Cattan P, Sarfati E. 2009. [Colonic interposition for esophageal replacement after caustic ingestion] [French]. J Chir. 146(3):240–249.
- Chirica M, Kraemer A, Petrascu E, Vuarnesson H, Pariente B, Halimi B, Munoz-Bongrand N, Sarfati E, Cattan P. 2014. Esophagojejunostomy after total gastrectomy for caustic injuries. Dis Esophagus. 27(2):122–127.
- Chirica M, Resche-Rigon M, Bongrand NM, Zohar S, Halimi B, Gornet JM, Sarfati E, Cattan P. 2012. Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg. 256(6):994–1001.
- Chirica M, Resche-Rigon M, Pariente B, Fieux F, Sabatier F, Loiseaux F, Munoz-Bongrand N, Gornet JM, Brette M-D, Sarfati E, et al. 2015b. Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg Endosc. 29(6):1452–1461.
- Chirica M, Resche-Rigon M, Zagdanski AM, Bruzzi M, Bouda D, Roland E, Sabatier F, Bouhidel F, Bonnet F, Munoz-Bongrand N. 2016. Computed tomography evaluation of esophagogastric necrosis after caustic ingestion. Ann Surg. 254:107–113.
- Christesen HB. 1994. Caustic ingestion in adults–epidemiology and prevention. J Toxicol Clin Toxicol. 32(5):557–568.
- Ciammaichella MM, Galanti C, Rossi C. 2019. Caustic ingestion. [Accessed 03/21/2019]. http://www.emjournal.net/htdocs/pages/art/47-caul.html.
- Contini S, Garatti M, Swarray-Deen A, Depetris N, Cecchini S, Scarpignato C. 2009a. Corrosive oesophageal strictures in children: outcomes after timely or delayed dilation. Dig Liver Dis. 41(4):263–268.
- Contini S, Scarpignato C, Rossi A, Strada G. 2011. Features and management of esophageal corrosive lesions in children from Sierra Leone: lessons learned from 175 consecutive patients. J Pediatr Surg. 46(9):1739–1745.
- Contini S, Swarray-Deen A, Scarpignato C. 2009b. Oesophageal corrosive injuries in children: a forgotten social and health challenge in developing countries. Bull World Health Org. 87(12):950–954.
- Contini S, Tesfaye M, Picone P, Pacchione D, Kuppers B, Zambianchi C, Scarpignato C. 2007. Corrosive esophageal injuries in children. A short lived experience in Sierra Leone. Int J Pediatr Otorhinolaryngol. 71(10):1597–1604.
- Contini S, Scarpignato C. 2013. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 19:3818–3930.
- Crain EF, Gershel JC, Mezey AP. 1984. Caustic ingestions: symptoms as predictors of esophageal injury. Am J Dis Child. 138(9):863–865.
- de Ferron P, Gossot D, Sarfati E, Célérier M. 1987. Esogastric lesions caused by ingestion of liquid chlorine bleach in adults [French]. Presse Med. 16:2110–2112.
- de Jong AL, Macdonald R, Ein S, Forte V, Turner A. 2001. Corrosive esophagitis in children: a 30-year review. Int J Pediatr Otorhinolaryngol. 57(3):203–211.
- de Lusong MAA, Timbol ABG, Tuazon DJS. 2017. Management of esopheagel caustic injury. WJGPT. 8(2):90–98.
- Dehghani SM, Bahmanyar M, Javaherizadeh H. 2018. Caustic ingestion in children in South of Iran: a two-year single center study. Middle East J Dig Dis. 10(1):31–34.
- Di Saverio S, Biscardi A, Piccini A, Mandrioli M, Tugnoli G. 2015. Different possible surgical managements of caustiv ingestion: diagnostic laparoscopy for Zargar’s grade 3a lesions and a new technique of “duodenal damage control”with “4-tubes ostomy” and duodenal wash-out as an option from extensive 3b lesions in unstable patients. Updates Surg. 67(3):313–320.
- Diliwari JB, Singh S, Rao PN, Anand BS. 1984. Corrosive acid ingestion in man – a clinical and endoscopic study. Gut. 25:183–187.
- Doğan Y, Erkan T, Çokuğraş FÇ, Kutlu T. 2006. Caustic gastroesophageal lesions in childhood: an analysis of 473 cases. Clin Pediatr (Phila). 45(5):435–438.
- Ducoudray R, Mariani A, Corte H, Kraemer A, Munoz-Bongrand N, Sarfati E, Cattan P, Chirica M. 2016. The damage pattern to the gastrointestinal tract depends on the nature of the ingested caustic agent. World J Surg. 40(7):1638–1634.
- Eaton H, Tennekoon GE. 1972. Squamous cancinoma of the stomach following corrosive acid burns. Br J Surg. 59(5):382–387.
- El-Asmar KM, Hassan MA, Abdelkader HM, Hamza AF. 2015. Topical mitomycin C can effectively alleviate dysphagia in children with long-segment caustic esophageal strictures. Dis Esophagus. 28(5):422–427.
- Eskander A, Ghobrial C, Mohsen NA, Mounir B, EL-Kareem DA, Tarek S, El-Shabrawi MH. 2019. Histopathological changes is the oesophageal mucosa in Egyptian children with corrosive stricture: a single-center vast experience. WJG. 25(7):870–879.
- Ezemba N, Eze JC, Nwafor IA, Etukokwu KC, Orakwe OI. 2014. Colon interposition graft for corrosive esophagealstricture: midterm functional outcome. World J Surg. 38(9):2352–2357.
- Ferguson MK, Migliore M, Staszak VM, Little AG. 1989. Early evaluation of therapy for caustic esophageal injury. Am J Surg. 157(1):116–120.
- Fil LJ, Verma G, Hoffman RS. 2014. Clarifying a study: computed tomography and assessing the severity of acute corrosive ingestion [Letter]. Clin Toxicol. 52:82.
- Follent AM, Rumbach AF, Ward EC, Marshall J, Dodrill P, Lewindon P. 2017. Dysphagia progression and feeding skills following pediatric alkali ingestion injury: two case reports. Disabil Rehabil. 39(23):2452–2459.
- Fuilla C, Richter F, Desportes JC, Michel A. 1996. Ingestion de produits caustiques en région Parisienne. Étude épidémiologique dans le secteur de reponsibalité de la Brigade de Sapeurs Pompiers de Paris [Ingestion of caustic products in the Paris region. Epidemiological study in the section of responsibility of the Paris Fire Brigade] [French].
- Fulton JA, Hoffman RS. 2007. Steroids in second degree burns of the esophagus: a systematic pooled analysis of 50 years of human data: 1956–2006. Clin Toxicol. 45(4):402–408.
- Furukawa S, Morita S, Okunaga H, Yamamoto Y, Nishi K. 2014. A case of death associated with ingestion of a neutral detergent [EAPCC XXXIV Congress Abstract]. Clin Toxicol. 52:428.
- Gambardella C, Allaria A, Siciliano G, Mauriello C, Patrone R, Avenia N, Polistena A, Sanguinetti A, Napolitano S, Conzo G. 2018. Recurrent esophageal stricture from previous caustic ingestion treated with 40-year self-dilation: case report and review of literature. BMC Gastroenterol. 18(1):68.
- Gaudreault P, Parent M, McGuigan MA, Chicoine L, Lovejoy FH. 1983. Predictability of esophageal injury from signs and symptoms: a study of caustic ingestion in 378 children. Pediatrics. 71(5):767–770.
- Gelu-Simeon M, Chuong A-P, Saliba F, Thiery G, Laurent M, Vilain C, Borel M, Amaral L, Alexis M, Saint-Georges G, et al. 2018. Submucosal hematoma: a new distinctive sign during emergency upper digestive endoscopy for ammonia ingestion. BMC Gastroenterol. 18(1):92.
- Gharib B, Mohammadpour M, Yaghmaie B, Sharifzadeh M, Mehdizadeh M, Zamani F, Edalatkhah R, Mohsenipour R. 2016. Caustic agent ingestion by a 1.5-year-old boy. Acta Med Iran. 54(7):465–470.
- Gill M, Tee D, Chinnaratha MA. 2019. Caustic ingestion: has the role of the gastroenterologist burnt out? Emerg Med Australas. 31(3):479–482.
- Gonzalez JM, Vanbiervliet G, Gasmi M, Grimaud JC, Barthet M. 2016. Efficacy of the endoscopic rendez-vous technique for the reconstruction of complete esophageal disruptions. Endoscopy. 48(2):179–183.
- Gorman RL, Khin-Maung-Gyi MT, Klein-Schwartz W, Oderda GM, Benson B, Litovitz T, McCormick M, McElwee N, Spiller H, Krenzelok E. 1992. Initial symptoms as predictors of esophageal injury in alkaline corrosive ingestions. Am J Emerg Med. 10(3):189–194.
- Grossi L, Francesco Ciccaglioni A, Marzio M. 2017. Esophagitis and its causes: who is “guilty” when acid is found “not guilty”? World J Gastroenterol. 23(17):3011–3016;
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2017. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol. 55(10):1072–1254.
- Gummin DD, Mowry JB, Spyker DA, Brooks DE, Osterthaler KM, Banner W. 2018. 2017 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th Annual Report. Clin Toxicol. 56(12):1213–1415.
- Gün F, Abbasoğlu L, Celik A, Salman ET. 2007. Early and late term management in caustic ingestion in children: a 16-year experience. Acta Surg Belg. 107:49–52.
- Gupta SK, Croffie JM, Fitzgerald JF. 2001. Is esophagogastroduodenoscopy necessary in all caustic ingestions? J Pediatr Gastroenterol Nutr. 32(1):50–53.
- Gupta V, Kurdia KC, Sharma A, Mishra AK, Yadav TD, Kochhar R. 2015. Treacheoesophageal fistula in adults due to corrosive ingestion: challenges in management. Updates Surg. 67(1):75–81.
- Havanond C, Havanond P. 2007. Initial signs and symptoms as prognostic indicators of severe gastrointestinal tract injury due to corrosive ingestion. J Emerg Med. 33(4):349–353.
- Hawkins DB. 1988. Dilation of esophageal strictures: comparison morbidity of antegrade and retrograde methods. Ann Otol Rhinol Laryngol. 75:460–465.
- Hawkins DB, Demeter MJ, Barnett TE. 1980. Caustic ingestion: controversies in management: a review of 214 cases. Laryngoscope. 90(1):98–109.
- Henrik BT, Christensen MD. 1994. Caustic ingestion in adults – epidemiology and prevention. Clin Toxicol. 32:557–568.
- Honar N, Haghighat M, Mahmood S, Javaherizadeh H, Kalvandi G, Salimi M. 2017. Caustic ingestion in children in south of Iran. Retrospective study from Shiraz – Iran. Rev Gastroenterol Peru. 37(1):22–25.
- Jacobs D, Vearrier D, Greenberg MI. 2014. Severe gastric necrosis following household bleach ingestion [EAPCCT XXXVI Congress Abstract]. Clin Toxicol. 52:428.
- Jacquemin D. 2014. Medical and surgical treatment. In: Maibach HI, Hall AH, editors. Chemical skin injury: mechanisms, prevention, decontamination, treatment. Heidelberg: Springer; p. 162–170.
- Jagpal PS, Dawas K, Bradberry SM. 2014. Assessment of life-threatening sulphuric acid ingestion using computed tomography imaging. Clin Toxicol. 52:428–429.
- Jalal G, Windy M, Badrane N, Rhalem N, Soulaymani-Bencheikh R. 2014. Descriptive study of reported cases of intoxication by caustic household “hydrochloric acid” in Morocco [EAPCCT XXXVI Congress Abstract]. Clin Toxicol. 52:429.
- Johnson CM, Brigger MT. 2012. The public health impact of pediatric caustic ingestion injuries. Arch Otolaryngol Head Neck Surg. 138(12):1111–1115.
- Johnson NP, Bruno EC. 2018. Novel use of ophthalmic pH paper to diagnose malicious caustic ingestion in a pediatric patient. CPCEM. 2(1):39–42.
- Katibe R, Abdelgadr I, McGrogan P, Akobeng AK. 2018. Corticosteroids for preventing caustic esophageal strictures: systemic review and meta-analysis. J Pediatr Gastroenterol Nutr. 66(6):898–902.
- Kaya M, Ozdemir T, Sayan A, Arikan A. 2010. The relationship between clinical findings and esophageal injury severity in children with corrosive agent ingestion. Ulus Travma Acil Cerrah Derg. 16:537–540.
- Keh SM, Onyekwelu N, McManus K, McGuigan J. 2006. Corrosive injury to upper gastrointestinal tract: still a major surgical dilemma. World J Gastroenterol. 12(32):5223–5228.
- Kikendall JW. 1991. Caustic ingestion injuries. Gastroenterol Clin North Am. 20(4):847–857.
- Kluger Y, Ishay OB, Sartelli M, Katz A, Ansaloni L, Gomez CA, Biffl W, Catena F, Fraga GP, Di Saverio S, et al. 2015. Caustic ingestion management: World Society of Emergency Surgery: survey of expert opinion. World J Emerg Surg. 10(1):48.
- Kochhar R, Ashat M, Reddy YR, Dhaka N, Manrai M, Sinha SK, Dutta U, Yadav TD, Gupta V. 2017. Relook endoscopy predicts the development of esophageal and antropyloric stenosis better than immediate endoscopy in patients with caustic ingestion. Endoscopy. 49(7):643–650.
- Kochhar R, Kochhar S. 2010. Endoscopic balloon dilation for benign gastric outlet obstruction in adults. WJG. 2(1):29–35.
- Kua K, Jonas N, O'Donnell R. 2015. The larynx and caustic soda ingestion. Arch Dis Child. 100(6):570–570.
- Kucuk G, Gollu G, Ates U, Cakmak ZA, Kologlu M, Yagmurlu A, Aktug T, Dindar H, Cakmak AM. 2017. Evaluation of esophageal injuries secondary to ingesgtion of unlabeled corrosive substances: pediatric case series. Arch Argent Pediatr. 15(2):e85–e88.
- Lachaux A, Mas E, Breton A, Barange K, Heresbach D, Molard BR, commission recommandation de la SFED. 2011. Consensus en endoscopie digensive: prise en charge des oesophagaties caustiques [French]. Acta Endosc. 4:303–308.
- Lamireau T, Llanas B, Deprez C, El Hammar F, Vergnes P, Demarquez JL, Favarel-Garrigues JC. 1997. Severity of ingestion of caustic substances in children] [French]. Arch Pediatr. 4(6):529–534.
- Lamireau T, Rebouissoux L, Denis D, Lancelin F, Vergnes P, Fayon M. 2001. Accidental caustic ingestion in children: is endoscopy always mandatory? J Pediatr Gastroenterol Nutr. 33(1):81–84.
- Le Naoures P, Hamy A, Lerolle N, Metivier Lermite A, Venara A. 2017. Risk factors for symptomatic esophageal stricture after caustic ingestion: a retrospective review. Dis Esophagus. 40(6):1–6.
- Leape LL. 1974. New liquid lye drain cleaners. Clin Toxicol. 7(1):109–114.
- Lobeck I, Dupree P, Stoops M, de Alarcon A, Rutter M, von Allmen D. 2016. Interdisciplinary approach to esophageal replacement and major airway reconstruction. J Pediatr Surg. 51(7):1106–1109.
- Lu L-S, Tai W-C, Hu M-L, Wu K-L, Chiu Y-C. 2014. Predicting the progress of caustic injury to complicated gastric outlet obstruction and esophageal stricture, using modified endoscopic mucosal injury grading scale. BioMed Res Int. 2014:919870.
- Lupa M, Magne J, Guarisco L, Amedee R. 2009. Update on the diagnosis and treatment of caustic ingestion. Ochsner J. 9(2):54–59.
- Lurie Y, Slotky M, Fischer D, Shreter R, Bentur Y. 2013. The role of chest and abdominal computed tomography in assessing the severity of acute corrosive ingestion. Clin Toxicol. 51(9):834–837.
- Lynn DD, Zukin LM, Dellavalle R. 2016. The safety and efficacy of Diphoterine® for ocular and cutaneous burns in humans. Cutan Ocul Toxicol. 3:1–17.
- Madadi-Sanjani O, Zimmer J, Gosemann JH, Ure BM, Lacher M, Boehm R. 2018. Topical mitomycin C application in pediatric patients with recurrent esophageal strictures – report on unfavorable results. Eur J Pediatr Surg. 28(6):539–546.
- Mamede RC, De Mello Filho F. 2002. Treatment of caustic ingestion: an analysis of 239 cases. Dis Esophagus. 15(3):210–213.
- Marchesi F, Rapacchi C, Pattonieri V, Tartamella F, Mita MT, Cecchini S. 2016. Minimally invasive esophagectomy for caustic ingestion after 73 years and over 200 endoscopic dilations: Is it just a matter of time? Acta Biomed. 87(2):220–223.
- Marcuz de Souza Compos A, Bucaretchi F, Crista Rodriguez Fernandes L, Borrasca Fernandes C, M, de Copitani E, Medieros Beck AR. 2017. Toxic exposures in children involving legally and illegally commercialized household sanitizers. Rev Paul Pediatr. 35(1):11–17.
- Martin Cano F, Rodrigues Vargas J, Sánchez B, Herrera Montes I. 2012. [Use of self-expandable prosthesis in esophageal stenosis in children] [Spanish]. Cir Pediatr. 25(4):207–210.
- Maull KI, Osmand AP, Maull CD. 1985. Liquid caustic ingestions: an in vitro study of the effects of buffer, neutralization, and dilution. Ann Emerg Med. 14(12):1160–1162.
- MedicineNet.com 2014. Proton-pump inhibitors. [Accessed January 12, 2014]. http://MedicineNet.com.
- Méndez-Nieto CM, Zarate-Mondragón F, Ramírez-Mayans J, Flores-Flores M. 2015. Mitomicina C tópica contra triamcinolona intralesionalen el manejo de la esonosis esofágica por cáusticos [Spanish] [Topical mitomycin C versus intralesional triamcinolone in the management of esophageal stricture due to caustic ingestion]. Rev Gastroenterol México. 80(4):248–254.
- Menéndez AM, Abramson L, Vera A, Duza GE, Palermo M. 2015. Total gastrectomy due to ferric chloride intoxication. Acta Gastroenterol Latinoam. 45(3):212–216.
- Meredith JW, Kon ND, Thompson JN. 1988. Management of injuries from liquid lye ingestion. J Trauma. 28(8):1173–1180.
- Methasate A, Lohsiriwat V. 2018. Role of endoscopy in caustic injury of the esophagus. WJGE. 10(10):274–282.
- Millar AJ, Cox SG. 2015. Caustic injury of the esophagus. Pediatr Surg Int. 31(2):111–121.
- Miller CK, Rutter MJ, von Allmen D, Stoops M, Putnam P, Stevens L, Willging JP. 2016. Swallowing dynamics status post caustic ingestion in a pediatric patient: a multidisciplinary case report. Int J Pediatr Otorhinolargyngol. 86:4–8.
- Montalva L, Viala J, Michelet D, Frade F, Lardy H, Vitoux C, Bonnard A. 2017. Total laparoscopic approach for transhiatal esophagectomy and Gavriliu’s esagoplasty in children with caustic esophageal injuries. J Laparoendosc Adv Sury Tech A. 27(10):1085–1090.
- Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2015. 2014 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicol. 53(10):962–1146.
- Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2016. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol. 54(10):924–1109.
- Mowry JB, Spyker DA, Cantilena LR, Bailey JE, Ford M. 2013. 2012 Annual Report of the American Association of Poison Control Center's National Poison Data System (NDPS): 30th Annual Report. Clin Toxicol. 51:849–1229.
- Mowry JB, Spyker DA, Cantilena LR, McMillan N, Ford M. 2014. 2013 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol. 52(10):1032–1283.
- Muñoz Botero NA, Pérez Cano AM, Rodríquez Herrera R, Rojas Gómez MP, Soler Páez FA. 2010. Terapia nutricional en pacientes adultos con quermaduras del tracto gastrointestinal por cáuticos [Nutritional therapy in adult patients with caustic burns of the gastrointestinal tract] [Spanish]. Nutr Hosp. 25:231–237.
- Munoz-Bongrand N, Cattan P, de Chaisemartin C, Bothereau H, Honigman I, Sarfati E. 2003. Extensive digestive caustic burns – what are the limits for resection?] [French]. Ann Chir. 128(6):373–378.
- Naamee A, Galvaing G, Chadeyras JB, Farhat M, Page JP, Bony-Collangettes E, Tardy MM, Filaire M. 2015. Tracheoplasty with use of an intercostal muscle flap for caustic necrosis. Ann Thorac Surg. 100(5):e103–e105.
- Nguyen V, Kramer S, Wightman R, Nelson LS, Hoffman RS. 2014. Laundry detergent pod causing esophageal and gastric injury in an adult [EAPCCT XXXVI Congress Abstract]. Clin Toxicol. 52(2014):427–428.
- Nijhawan S, Udawat HP, Nagar P. 2016. Aggressive bougie dilation and intralesional steroids is effective in refractory benign esophageal strictures secondary to corrosive ingestion. Dis Esophagus. 29(8):1027–1031.
- Nondela BB, Cox SG, Brink A, Millar AJW, Numanoglu A. 2018. Correlation of 99mTc sucralfate scan and endoscopic grading in caustic esophageal injury. Pediatr Surg Int. 34(7):781–788.
- Ormeño Julca AJ. 2016. Use of corticosteroids in esophagitis caustic ingestion. Report of two cases [Spanish]. Rev Gastroenterol Peru. 36(3):256–259.
- Pelclová D, Navrátil T. 2005. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev. 24(2):125–129.
- Pennachi C, de Moura DTH, Amorim RBP, Guedes HG, Kumbhari V, de Moura EGH. 2017. Lugol’s iodine chemoendoscopy versus narrow band image enhanced endoscopy for the detection of esophageal cancer in patients with stenosis secondary to caustic/corrosive agent ingestion. Arg Gastroenterol. 54(3):250–254.
- Poley J-W, Steyerberg EW, Kuipers EJ, Dees J, Hartmans R, Tilanus HW, Siersema PD. 2004. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastointest Endosc. 60(3):372–377.
- Predescu D, Constantinoiu S. 2018. Esophageal reconstruction with the stomach: a functional dilemma: chr. 113(1):83–94.
- Radenkova-Saeva JV, Loukova A, Tzekov H. 2014. Intentional self-poisoning by alkaline corrosive agents: a study for the period 2010–2012. [EAPCCT XXXIV Congress Abstract]. Clin Toxicol. 52:310-311.
- Rai MB, Bhoil A, Kashyap R, Bhattacharya A, Dutta U, Kochlar R. 2013. 99m Tc-pertechnate scintilligraphy and endoscopy in assessment of caustic-induced gastric mucosal injury. Clin Nuclear Med. 38(3):e146-7.
- Rajabi MT, Maddah G, Bagheri R, Mehrabi M, Shabahang H, Lorestani F. 2015. Corrosive injury of the upper gastrointestinal tract: review of surgical management and outcome in 14 adult cases. Iran J Otorhinolaryngol. 27(1):78.
- Rajan N, Rahim R, Kumar SK. 1985. Formic acid poisoning with suicidal intent: a report of 53 cases. Postgrad Med J. 61(711):35–36.
- Riffat F, Cheng A. 2009. Pediatric caustic ingestion: 50 consecutive cases and a review of the literature. Dis Esophagus. 22(1):89–94.
- Rigo GP, Camellini L, Azzolini F, Guazzetti S, Bedogni G, Merighi A, Bellis L, Scarcelli A, Manenti F. 2002. What is the utility of selected clinical and endoscopic parameters in predicting the risk of death after caustic ingestion? Endoscopy. 34(4):304–310.
- Robustelli U, Bellotti R, Scardi F, Fortunato Armellino M, De Masi A, Forner AL, Riccio E, Manguso F. 2011. Management of corrosive injuries of the upper gastrointestinal tract. Our experience in 58 patients. G Chir. 32(4):188–193.
- Rodriguez Vargas BO, Monge Salgrado E, Montes Teves P, Salazar Ventura S, Guxmán Calderón E. 2016. Caustics injuries in the upper gastrointestinal tract: clinical and endoscopic features. Rev Gastroenterol Peru. 36(2):135–142.
- Rollin M, Jaulim A, Vaz F, Sandhu G, Wood S, Birchall M, Dáwas K. 2015. Caustic ingestion injury of the upper aerodigestive tract in adults. Annals. 97(4):304–307.
- Rothstein FC. 1986. Caustic injuries to the esophagus in children. Pediatr Toxicol Pediatr Clin North Am. 34:665–674.
- Rumack BH, Burrington JD. 1977. Caustic ingestions: a rational look at diluents. Clin Toxicol. 11(1):27–34.
- Ryu HH, Jeung KW, Lee BK, Uhm JH, Park YH, Shin MH, Kim HL, Heo T, Min YI. 2010. Caustic injury: can CT grading system enable prediction of esophageal stricture? Clin Toxicol. 48(2):137–142.
- Sabzevari A, Maamouri G, Kiani MA, Saeidi M, Kianifar H, Jafari SA, Ahanchian H, Jarahi L, Roudi E, Sharafkhani M. 2017. Clinical and endoscopic findings of children hospitalized in Qa’em Hospital of Mashhad due to caustic ingestion (2011–2013). Electron Physician. 9(4):4248–4250.
- Sarfati E, Gossot D, Assens P, Célérier M. 1987. Management of caustic ingestion in adults. Br J Surg. 74(2):146–148.
- Sarfati E, Gossot D, Assens P, Célérier M, Jadat R, Delcros J. 1984. Management of digestive lesions after ingestion of caustics [French]. Ann Chir. 38:651–658.
- Satar S, Topal M, Kozaci N. 2004. Ingestion of caustic substances by adults. Am J Ther. 11(4):258–261.
- Shub MD. 2015. Therapy of caustic ingestion: new treatment considerations. Curr Opin Pediatr. 27(5):609–613.
- Struck MF, Beilicke A, Hoffmeister A, Gockel I, Gries A, Wrigge H, Bernhard M. 2016. Acute emergency care and airway management of caustic ingestion in adults: single center observational study. Scand J Trauma Resusc Emerg Med. 24:45.
- Tannuri ACA, Tannuri U. 2017. Total esophageal substitution for combined hypopharyngeal and esophageal strictures after corrosive injury in children. J Pediatr Surg. 52(11):1742–1746.
- Taşkinlar H, Bahadir GB, Yiğit D, Erdoğan C, Avlan D, Nayci A. 2017. Effectiveness of endoscopic balloon dilation in grade 2a and 2b esophageal burns in children. Minim Invasive Ther Allied Technol. 26(5):300–306.
- Temiz A, Oguzkur P, Ezer SS, Ince E, Hicsinmez A. 2012a. Predictability of caustic ingestion by esophagogastroduodenoscopy in children. WJG. 18(10):1098–1103.
- Temiz A, Oguzkurt P, Ezer SS, Ince E, Gezer HO, Hicsonmez A. 2012b. Management of pyloric stricture in children: endoscopic balloon dilation and surgery. Surg Endosc. 26(7):1903–1908.
- Tewfik TL, Schloss MD. 1980. Ingestion of lye and other corrosive agents – a study of infant and child cases. J Otolaryngol. 9(1):72–77.
- Thomas MO, Ogunleye EO, Somefun O. 2009. Chemical injuries of the oesophagus: aetiopathological issues in Nigeria. J Cardiothorac Surg. 4(1):56.
- Tiedeken J, Uradomo L, Anderson KD, Brody F. 2012. Minimally invasive repair of a late stricture in a reversed gastric tube. J Pediatr Surg. 47(12):2321–2326.
- Tirelli G, Baruca R, Boscolo Nata F. 2017. Salivary bypass tube placement in esophageal stricture: a technical note and report of three cases. Auris Nasus Larynx. 44(6):758–761.
- Tiryaki T, Livanelioğlu Z, Atayurt H. 2005. Early bougienage for relief of stricture formation following caustic esophageal burns. Pediatr Surg Int. 21(2):78–80.
- Tohda G, Sugawa C, Gayer C, Chino A, McGuire TW, Lucas CE. 2008. Clinical evaluation and management of caustic injury in the upper gastrointestinal tract in 95 adult patients in an urban medical center. Surg Endosc. 22(4):1119–1125.
- Trangali A, Thomson M, Domonceau J-M, Taveras M, Tabbers MM, Fullano R. 2017. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (RSGE) and European Society for Paedric Gastroenterology Hepatology and Nutrition (ESPGHAN) guideline Executive Summary. Endoscopy. 49:83–91.
- Tseng J-Y, Chen C-H, Chen W-K, Dong-Zong H. 2011. Hand warmer corrosive injury. Clin Toxicol. 49(9):870–871.
- Turner A, Robinson P. 2005. Respiratory and gastrointestinal complications of caustic ingestion in children. Emerg Med J. 22(5):359–361.
- Usta M, Erkan T, Cokugras FC, Urganci N, Onal Z, Gulcan M, Kutlu T. 2014. High doses of methylprednisolone in the management of caustic esophageal burns. Pediatrics. 133(6):e1518–e1524.
- Uygun I. 2015. Caustic esophagitis in children: prevalence, the corrosive agents involved, and management from primary care through surgery. Curr Opin Otolaryngol Head Neck Surg. 23(6):423–432.
- Uygun I, Arslan MS, Aydogdu B, Okur MH, Otcu S. 2013. Fluorscopic balloon dilation for caustic esophageal stricture in children: an 8-year experience. J Pediatr Surg. 48(11):2230–2234.
- Uygun I, Aydogdu B, Okur MH, Arayici Y, Celik Y, Ozturk H, Otcu S. 2012. Clinico-epidemiological study of caustic substance ingestion accidents in children in Anatolia: The DROOL Score as a new prognostic tool. Acta Chir Belg. 112(5):346–354.
- Valdez AL, Casavant MJ, Spiller HA, Chounthirath T, Xiang H, Smith GA. 2014. Pediatric exposure to laundry detergent pods. Pediatrics. 134(6):1127–1135.
- Vandenplas Y. 2017. Management of benign esophageal stricture in children. Pediatr Gastroenterol Hepatol Nutr. 20(4):211–215.
- Vewzakis AI, Pantiora EV, Kontis EA, Sakellariou V, Theodoriou D, Gkiokas G, Polydorou AA, Fragullidas GP. 2016. Clinical spectrum and management of caustic ingestion: a case series presenting three opposing outcomes. Am J Case Rep. 17:340–346.
- Wax PW, Yarema M. 2007. Corrosives. In: Shannon MW, Borron SW, Burns MJ, editors. Haddad and Winchester's Clinical Management of Poisoning and Drug Overdose. 4th ed. Philadelphia: Saunders/Elsevier; p. 1407–1414.
- Weinrab A. 2012. Rapport du Stage: Dèvelopmment d’un produit de décontamination efficace dans le cas des ingestions de caustiques [Internship Report: Development of an efficacious product for cases of caustic ingestions] [French]. Laboratoire Prevor. Valmondois, France.
- Wightman RS, Read KB, Hoffman RS. 2016. Evidence-based managements of caustic esposures in the emergency department. Emerg Med Pract. 18(5):1–17.
- Wijeratna T, Ratnatunga C, Dharrmapala A, Samarasinghe T. 2015. Corrosive acid injury of the stomach. Ceylon Med J. 60(1):25–27.
- Wilson DA, Wormald PJ. 1995. Battery acid – an agent of attempted suicide in black South Africans. S Afr Med J. 85(6):529–531.
- Wormald PJ, Wilson DA. 1993. Battery acid burns of the upper gastro-intestinal tract. Clin Otolaryngol. 18(2):112–114.
- Woynarowski M, Dądalski M, Wojno V, Tiesseyre M, Szymczak M, Chyżyńska A, Hurkala L, Plowiecki E, Kmiotek J. 2014. Nasogastric tube as protection for recurrent oesophageal stricture: a case report. World J Gastroenterol. 20(16):4906–4910.
- Wu MH, Lai WW. 1993. Surgical management of extensive corrosive injuries of the alimentary tract. Surg Gynecol Obstet. 177(1):12–16.
- Yonemaru H, Karimata H, Shimoji H, Yamamoto K, Hanashiro K, Fukami M, Ouchi G, Tamaki Y, Kondo Y, Kukita I. 2016. Successful conservative management of a case of caustic esophagitis based on computed tomography assessment. Acute Med Surg. 3(2):147–151.
- Zargar SA, Kochhar R, Mehta S, Mehta SK. 1991. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classificatrion of burns. Gastrointest Endosc. 37:165–169.
- Zerbib P, Vinet A, Rogosnitzky M, Truant S, Chambon JP, Pruvot FR. 2014. Gastrocele complicated the course of non-operated severe caustic injuries: operative strategies. World J Surg. 38(5):1233–1237.
- Zwischenberger JB, Savage C, Bidani A. 2001. Surgical aspects of esophageal disease: perforation and caustic injury. Am J Respir Crit Care Med. 164:1037–1040.

