ABSTRACT
Objective
In psychotherapy, strength-based methods (SBM) represent efforts to build on patients’ strengths while addressing the deficits and challenges that led them to come to therapy. SBM are incorporated to some extent in all major psychotherapy approaches, but data on their unique contribution to psychotherapy efficacy is scarce.
Methods
First, we conducted a systematic review and narrative synthesis of eight process-outcome psychotherapy studies that investigated in-session SBM and their relation to immediate outcomes. Second, we conducted a systematic review and multilevel comparative meta-analysis contrasting strength-based bona fide psychotherapy vs. other bona fide psychotherapy at post-treatment (57 effect sizes nested in 9 trials).
Results
Despite their methodological variability, the pattern of results in the process-outcome studies was generally positive, such that SBM were linked with more favorable immediate, session-level patient outcomes. The comparative meta-analysis found an overall weighted average effect size of g = 0.17 (95% CIs [0.03, 0.31], p < .01) indicating a small but significant effect in favor of strength-based bona fide psychotherapies. There was non-significant heterogeneity among the effect sizes (Q(56) = 69.1, p = .11; I2 = 19%, CI [16%, 22%]).
Conclusion
Our findings suggest that SBMs may not be a trivial by-product of treatment progress and may provide a unique contribution to psychotherapy outcomes. Thus, we recommend integration of SBM to clinical training and practice across treatment models.
Clinical or methodological significance of this article: Strength-based methods highlight the importance of balancing responsiveness and capitalization on patients’ strengths while also addressing their weaknesses in therapy. Our systematic review suggests that strength-based methods contribute to positive in-session processes and treatment outcomes. The comparative meta-analysis indicates that strength-based methods may increase treatment efficacy of bona fide psychotherapy. Thus, strength-based methods should be incorporated in clinical trainings and practice across treatment modalities.
In their pioneering work, Cronbach and Snow (Citation1977) claimed that some treatments are more effective for particular individuals depending on their preexisting capabilities. In the context of educational sciences, the authors suggested optimal learning occurs in at least two different ways: compensating the individual’s deficits (e.g., support lessons for learners with poor grades) or capitalizing on the individual’s behaviors and capabilities (“strengths”) (e.g., choice of a profession related to personal skills and interests).
In psychotherapy, a skillful balance between using patient capitalization and compensation strategies within a collaborative therapeutic relationship has long been suggested to contribute to optimal treatment outcomes (e.g., Cheavens et al., Citation2012; Cronbach & Snow, Citation1977; Gelso & Woodhouse, Citation2003). In addition, strategies to capitalize on the therapist's abilities can also be used to increase the therapist's effectiveness (Constantino et al., Citation2021). For therapists, a first step in patient capitalization is to systematically assess patients’ existing strengths and form hypotheses about how these strengths can be addressed in therapy. During therapy, the therapist can identify and emphasize the patient’s strengths and use them as a catalyst for change.
Whereas mental health is often seen as a unidimensional dichotomy or continuum of psychological suffering (e.g., depression yes/no; mild, moderate, severe major depressive episode; 0–100 global assessment of functioning), a bi-dimensional conceptualization considers psychological strengths in addition to problems and suffering (e.g., Cacioppo et al., Citation2012). In the present systematic review, we use a working definition of mental health as actively and intentionally engaging fully in life as a mainly independent quality that is not exclusively due to the absence of suffering or a mental disorder. An example of a patient strength is resilience, that is, the capacity to cope adaptively with adversity with minimal psychological suffering (e.g., Bonanno, Citation2021; Lee et al., Citation2013). Other examples of human strength include well-being (e.g., Jebb et al., Citation2020; Tay & Diener, Citation2011), self-efficacy (Scholz et al., Citation2002), human agency (Bandura, Citation2006), meaning of life (e.g., Hill, Citation2018), resources (Hobfoll, Citation1989) or happiness (Helliwell et al., Citation2021).
Definitions and Clinical Description
In psychotherapy, strength-based methods (SBM) represent efforts to balance between enhancing patients’ strengths, while addressing their deficits and challenges. The term strength-based methods (also called positive interventions, resilience-based or resource-oriented) refers to therapist behaviors designed to acknowledge, validate, and foster the client’s strengths, capabilities, and motivational readiness for psychotherapy change. SBM are based on the premise that working with patient strengths is key to psychotherapeutic change. The unpleasant, unsatisfying, and maladaptive parts of behavior are integrated into a fuller picture of mental health by also including the pleasant, satisfying, and functional parts of behavior.
Strength-based psychotherapy refers to multiple treatment approaches. These include positive psychotherapy (Conoley & Scheel, Citation2018; Parks & Schueller, Citation2014; Rashid & Seligman, Citation2019), strength-based and/or resilience-focused cognitive–behavioral therapy (e.g., Cheavens et al., Citation2012; Padesky & Mooney, Citation2012; Willutzki et al., Citation2004), and psychotherapy integration (e.g., Flückiger et al., Citation2010, Citation2013; Grawe, Citation1997; Gelso & Woodhouse, Citation2003; Scheel et al., Citation2013).
SBM is incorporated to some extent in all major psychotherapy orientations. In cognitive–behavioral therapy (CBT), specific SBMs are designed to increase positive affect (Craske et al., Citation2019) or engagement in pleasurable activities (Solomonov et al., Citation2020); psychodynamic therapy promotes insight, meaning making (Wachtel, Citation2011), and thriving in relationships (Tolpin, Citation2002). SBM are identified as a basic component of counseling psychology and humanistic psychotherapy (e.g., Gelso & Woodhouse, Citation2003; Satir et al., Citation1991; Scheel et al., Citation2013). Resource activation as a therapeutic factor represents a collaborative process that (re)activates skills, behaviors, and motivation for further change in patients and the psychosocial environment to achieve treatment goals.
All SBM capitalize on patient strengths, but they vary in their specific clinical context. Below, we provide an overview of different ways in which SBM are conceptualized in psychotherapy practice:
- Therapist responsiveness to the patient self-directed strength AND/OR therapist strength-based instructions. SBM exist in transaction (at least a dyadic construct), that is, patients proactively contribute to their therapy (e.g., Bohart, Citation2007; Macdonald & Muran, Citation2020; Ryan & Deci, Citation2008). Some psychotherapies emphasize the therapist’s strength-based responsiveness to patients’ self-directed abilities and motivational readiness (Flückiger et al., Citation2021), whereas others highlight the therapist’s strength-based instructions and patient reactions to those instructions (Suhr et al., Citation2017). It is difficult to separate these two strength-based aspects in individual sessions, as patients, as part of their patient role, often are guided by therapists to emphasize positively valued aspects during sessions.
- Disorder-specific AND/OR general strength-based methods. While several clinician’s guides propose disorder-specific SBM (such as positive psychotherapy for psychosis; Riches et al., Citation2016), others highlight more generic SBM that include focusing more broadly on wellbeing and personal engagement (e.g., strength-based CBT to build on resilience; Padesky & Mooney, Citation2012).
- Trait AND/OR state strengths. Some SBM build on individual traits (e.g., character strengths; Niemiec, Citation2018) whereas others focus on the situational strengths in a particular therapeutic action or moment (Gonçalves et al., Citation2014).
- Capitalizing on preexisting strengths AND/OR building new strengths. Some SBM enhance preexisting abilities (e.g., proposing actions that correspond with the patients’ preexisting skills; Cheavens et al., Citation2012). Other methods highlight the development of new skills (e.g., building pleasure; Rashid & Seligman, Citation2019).
- Building patients’ individual strengths AND/OR building social and community strengths. SBM are based on multiple levels of social networks. Some aim to build on the patients’ individual strengths (e.g., fostering own gratitude practice, Emmons & Stern, Citation2013), some on interpersonal relationships, and still others on community or environmental strengths (e.g., fostering social support; Hirani et al., Citation2018; Li et al., Citation2021).
- SBM in the therapy room AND/OR outside of the therapy room. Strength-based methods can be focused on in-session (micro-) skills (e.g., Flückiger et al., Citation2009) but also outside of the therapy room via strength-based homework and augmented online tools (e.g., De Vries et al., Citation2020; Scheel et al., Citation2004).
Overall, SBM are based on a common premise that the general positive quality of SBM contributes to treatment progress, while also maintaining a clear focus on the patients’ difficulties (Yulish et al., Citation2017).
Assessments
Assessment of Strength-Based Therapist and Patient Behaviors
There are several video-rating systems to measure therapists’ in-session use of SBM. These include overall rating of the positivity/resource activation at the end of sessions (von Consbruch et al., Citation2013), a moment-to-moment coding system where innovative moments of the patient change process are assessed (Gonçalves et al., Citation2011), and resource-oriented micro-process analysis (ROMA-T/P, e.g., Flückiger et al., Citation2009), where strength-based therapist and patient behaviors are assessed separately during 1-minute segments.
As an example, the ROMA-Therapist version assesses the following strength-based categories (Flückiger & Grosse Holtforth, Citation2008b): (i) immediate reinforcement of specific strengths, (ii) emphasis on patients’ self-directed change, (iii) expression of confidence for improvement, (iv) focus of personal skills, (v) emphasis on positive emotions, (vi) focus on interpersonal skills and social support, (vii) focus on physical health, (viii) emphasis on positive therapeutic process and relationship, (ix) focus on treatment goals, (x) emphasis on solutions to problems, (xi) emphasis on self-directed choice, (xii) pick up a positive patients’ metaphors, (xiii) exploring exceptions, and (xiv) normalizing and reframing a targeted problem. An overall minute-by-minute rating of the quality of strength-based methods is evaluated from −2 (e.g., therapist ignores positive aspects mentioned by the patient for at least several minutes) to +2 (e.g., therapist explores in detail strengths for more than several minutes) and as a further category +3 (e.g., too excessive positivity, therapist appears overly enthusiastic or disingenuous). Corresponding with the therapist categories, ROMA-Patient rating system assesses the strength-based categories of the patient on a minute-to-minute level.
ROMA-T/P does not differentiate who initiates the strength-based therapeutic focus; it is assumed that both therapist and patient contribute to strength-based therapeutic talks and the sum of the therapist’s SBM may help to keep a strength-based focus across several minutes. For example, a therapist may ask an open question and the patient may respond in a manner where the therapist starts to explore and reflect positive aspects more precisely. What matters is that therapist and patient successively include and appreciate strength-based aspects in the sessions.
Strength-Based Assessments Post-Session, Between Sessions, and Treatment Progress
The definition, repeated assessment and monitoring of strength-based concepts is a SBM itself; for example, the repeated assessment of strengths increases patient awareness for strength. There are post-session reports where strength-based in-session experiences are assessed from the patient and therapist perspectives (e.g., Flückiger et al., Citation2010; Mander et al., Citation2015). Patients’ positive experiences of well-being may also be assessed outside of the therapy room, for example, using inter-session diaries or ecological momentary assessments/interventions (e.g., De Vries et al., Citation2020; Suhr et al., Citation2017; Vîslă et al., Citation2021).
Patient strength may be optimally assessed in a broad battery of measures that evaluates various domains of functioning including physical and mental health, such as psychological and social well-being, positive affectivity, self-esteem, self-efficacy, and social support (e.g., Probst et al., Citation2022; Schürmann-Vengels et al., Citation2022). Further, the items and answer formats of clinical questionnaires can be systematically discussed in terms of patients’ strength, abilities, skills, needs and motivation (e.g., item of the Beck Depression Inventory: “I have as much energy as ever.”.
Many have also suggested using individualized assessments of progress toward mutually developed and well-defined treatment goals (e.g., criterion-oriented outcomes such as Goal Attainment Scaling, Kiresuk & Sherman, Citation1968, or Target Complaints, Battle et al., Citation1966). A strength-based formulation of treatment goals would cover both maladaptive domains that should be targeted (e.g., fewer symptoms, fewer interpersonal problems) as well as positive behaviors and functioning that should be enhanced (e.g., Grosse Holtforth & Grawe, Citation2002). Finally, reviewing satisfaction with the therapist and therapy (e.g., Seligman, Citation1995; Wampold & Flückiger, Citation2023) is a critical SBM to validate patient-centered outcomes.
Previous Meta-Analyses
summarizes prior meta-analyses on treatment outcomes of strength-based psychotherapies, with the majority comparing strength-based psychotherapies with control conditions on distal (not disorder-specific) outcomes. The majority of these contrasts indicated small to medium effects in favor of the positive/strength-based approaches. However, all meta-analyses investigated the efficacy of SBM vis-à-vis control conditions that were not designed to be fully therapeutic (i.e., that were not bona fide psychotherapy; Wampold & Imel, Citation2015). Thus, prior studies do not provide information on whether SBM increase or decrease the efficacy of preexisting bona fide psychotherapy. To the best of our knowledge, this is the first comparative meta-analysis that investigates the potential added contribution of SBM to bona fide psychotherapy outcomes.
Table I. Prior meta-analyses of strength-based treatments.
Research Review
The goal of this systematic review and meta-analysis was two-fold. First, we reviewed the research evidence on strength-based process-outcome studies. We conducted a narrative review of studies that assess in-session SBM (comparable to the above-mentioned ROMA-rating) under bona fide psychotherapy conditions and its contribution to immediate outcomes. Second, we conducted a comparative meta-analysis of trials that contrasted strength-based psychotherapies vs. other bona fide psychotherapies. Most of these trials contrasted SBM with more problem-focused methods within the same orientation, sometimes even using the same treatment manual/approach, but contrasting different degrees of implementing SBM during sessions.
Inclusion Criteria
The inclusion criteria include: (a) the study author(s) referred to the individual psychotherapy as “strengths based” or “solution focused” or “resource oriented” or “resilience based;” (b) patients had a current mental health diagnosis; (c) treatments were bona fide psychotherapy, and (d) comparable amount of treatment, supervision and training sessions across the conditions. Studies were excluded if: (a) the trials focused on children (< 13 years) or couples or family therapy; (b) the study design focused on prevention, after-care or at-risk programs; (c) the trials were preliminary pilot studies with less than 10 patients per group or with less than 3 therapists. When multiple treatments were available in the same study, we selected only those that met our criteria outlined above (e.g., medication conditions were excluded). For the process-outcome studies, we included studies that directly assessed SBM at the in-session level (e.g., using ratings of video-/audio recordings). We excluded studies that assessed strength-based session experiences only as overall ratings at post-session (e.g., using post-session reports).
The following criteria were used for bona fide psychotherapy (Wampold et al., Citation1997; Wampold & Imel, Citation2015): psychotherapists with at least a master’s degree delivered the treatment, patients met diagnostic criteria, and two of the following four criteria were satisfied: (a) treatments were generally recognized as legitimate treatment, such as CBT or psychodynamic therapy and therapists were not proscribed from well-accepted therapeutic actions, such as psychoeducation, being empathic, providing a treatment rationale; (b) description of treatment contained a reference to a psychological mechanism (e.g., operant conditioning); (c) a treatment manual/guide was used; and (d) treatment contained an active component that appeared in the psychological literature.
Search Strategy
For the systematic review and comparative meta-analysis, we located comparative trials of strength-based approaches under bona fide psychotherapy conditions, and we inspected the above-mentioned prior comparative meta-analyses on positive psychotherapy (Carter et al., Citation2016 (s = 8); Chakhssi et al., Citation2018 (s = 30); Munder et al., Citation2019 (s = 10); White et al., Citation2019 (s = 51/39); Zheng et al., Citation2016 (s = 6); Hoppen & Morina, Citation2021 (s = 20)). Furthermore, to broaden the scope, we searched (via EBSCO) the PsycINFO, ERIC, MEDLINE, and PSYNDEX databases with the keywords «psychotherapy OR treatment» AND «strength based OR solution focused OR resource oriented OR resilience based» AND «RCT OR randomized control trial OR randomized controlled trial OR clinical trial» AND «disorder» in March, 2021. For the process-outcome studies, we examined the introduction and reference sections of included studies to detect further process-outcome studies. Furthermore, we checked the hits of a further systematic review with the keywords «resource activation OR Ressourcenaktivierung OR resource realization OR Ressourcenrealisierung» in April 2021.
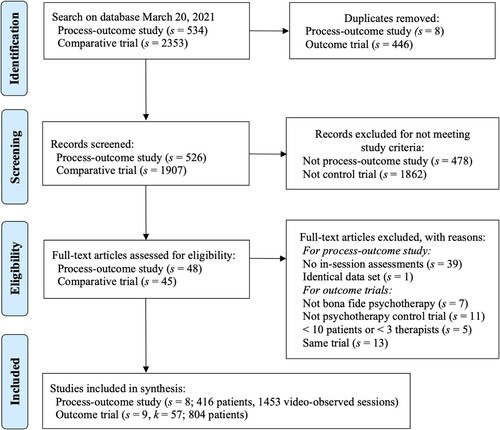
flowchart provides an overview of the extraction procedure. From the 534 and 2,353 articles respectively (8 and 446 were duplicates), we identified eight process-outcome studies (representing 416 patients) and nine comparative trials (reporting 57 effect sizes at post assessment representing 804 patients with an average of 89 patients per study). The eight process-outcome studies and nine clinical trials are summarized in and (for bona fide criteria and Risk of Bias 2 see https://osf.io/s7z2w/). Agreement between raters of bona fide criteria for strength-based treatments and contrasting treatments was 92%. Coding disagreements were discussed and resolved by reaching consensus. Effect size extractions and sample characteristics were coded, double-checked, and collaboratively discussed between the first and second author.
Figure 1. Flowchart of the included process-outcome studies and comparative trials (s = studies, k = effect sizes).
For the nine comparative trials, data included both peer-reviewed manuscripts (s = 8) and one dissertational thesis without peer-review (s = 1, i.e., Kosfelder, Citation2000), data collected from randomized controlled trials (s = 7) and from trials where patients were not randomized, but grouped using propensity score methods on the basis of previously collected data (s = 2; i.e., Flückiger & Grosse Holtforth, Citation2008a; Kosfelder, Citation2000). No trial with Positive Psychotherapy as a specific strength-based approach met the inclusion criteria (potential trials that did not meet the inclusion criteria: Andrewes et al., Citation2014 and Asgharipoor et al., Citation2012 treated 5 clients in the CBT control condition, Fava et al., Citation2005 and Chaves et al., Citation2017 considered less than 3 therapists; Uliaszek et al., Citation2016 investigated a subclinical student population; in Furchtlehner et al., Citation2020 group leaders were not psychotherapists).
Review of In-Session SBM and Their Relation to Immediate Outcomes
Studies on therapist in-session use of SBM, as assessed with video-based observer ratings, and their relation to outcomes are summarized in . Video-ratings in all reviewed process-outcome studies are primarily based on the theoretical framework initiated by Grawe (Citation1997) in which SBM are operationalized as a general positivity factor (e.g., ROMA-P/T overall quality ratings). A representative example is provided by Smith and Grawe (Citation2003, Citation2005), who used an advanced analytic methods of decision trees (a machine learning algorithm). The authors analyzed SBM in a sample of 613 sessions of 128 different patients to predict a composite score of session productivity evaluated at post-session (2829 strength-based ratings of 10-min sequences) in integrative CBT. The authors documented positive associations between strength-based therapist methods and immediate outcomes during the course of treatment. They concluded that when a proposed therapeutic procedure was tailored to the individual skills and strengths of the patient so that they became actively involved, the likelihood that the patient evaluated the session as productive was higher (60.8%) compared to methods where patients were unable to respond adequately (20.9%). However, even in these less-optimal sequences, a subsequent discussion about the patient’s positive skills and abilities enhanced the likelihood of a session to be rated as productive (51.1% of the 20.9%). This finding may suggest that SBMs are experienced by patients as helpful and therapeutic. Of course, the correlative nature of the study precludes a definite causal interpretation.
Table II. Summary of strengths-based process-outcome studies investigating bona fide psychotherapy.
Table III. Comparative trials contrasting strength-based methods with bona fide psychotherapy.
The reviewed studies in varied in use of methods and samples (e.g., selection of particular sessions over a treatment course). Given their methodological heterogeneity, it is not surprising that the effects of SBM on the session level may be highly situational. Descriptively, an inspection of these studies reveal that therapists use SBM with multiple client populations, across theoretical orientations, and with a range of mental health conditions. Notably, despite their methodological variability, the general pattern of results was uniformly positive in that SBM was linked with more favorable immediate, session-level patient outcomes. SBM consistently emerged as a therapeutic factor that is related to treatment progress across sessions. At the same time, and somewhat unexpectedly, therapists’ use of SBM was also evident in situations where treatment relapse was evident (Gassmann & Grawe, Citation2006; Schilling et al., Citation2021). In these situations, the therapeutic function of SBM may be less straightforward as in successful sessions.
Comparison of Strength-Based Psychotherapies to Other Bona Fide Psychotherapies
For the comparative multi-level meta-analysis, we used random-effects restricted maximum-likelihood estimator. This analysis is based on the assumption that studies in this meta-analysis were randomly sampled from a population of studies. Effect sizes were generated using the R statistical software “compute.es” package (Del Re, Citation2013), and the multi-level meta-analytic models and meta-analytic diagnostics (i.e., tests for outliers) used the R “metafor” package (Viechtbauer, Citation2010; for the forest plot: Fernández-Castilla et al., Citation2020).
To account for multiple outcomes per study (i.e., within-study effect sizes nested in a trial), we conducted multi-level meta-analytic models with 3 levels, where sampling variance of the extracted effect sizes at Level 1 were nested in k measures at Level 2 and s studies at Level 3 (e.g., Assink & Wibbelink, Citation2016; Raudenbush & Bryk, Citation2002). The use of multi-level models in meta-analytic research enables integration of multiple outcomes and accounts for their interdependency as correlations between outcomes are rarely reported in primary studies and therefore difficult to obtain. In addition, the three-level approach allows examining outcome variance within studies (i.e., within-study heterogeneity) as well as between studies (i.e., between-study heterogeneity).
For the specific treatment contrasts, overall heterogeneity was assessed with the Q and I2 statistics (Higgins & Thompson, Citation2002). I2 is calculated as the percentage of variability due to true differences among effect sizes. We also tested whether within-study heterogeneity (i.e., various measures nested in a study) explained a significant proportion of the overall heterogeneity by comparing the full model with a reduced model, where the within-study variance was fixed as zero (Assink & Wibbelink, Citation2016).
We estimated power based on Jackson and Turner’s (Citation2017) recommendation using “metapower” package in R (Griffin, Citation2021). Given a small effect of d of 0.10, an average group size across studies of n = 80 patients, and some heterogeneity of I2 = 20%, the power for meta-analytic random effects models was 0.86 for 57 effect sizes. That indicated that there was sufficient power to detect treatment differences.
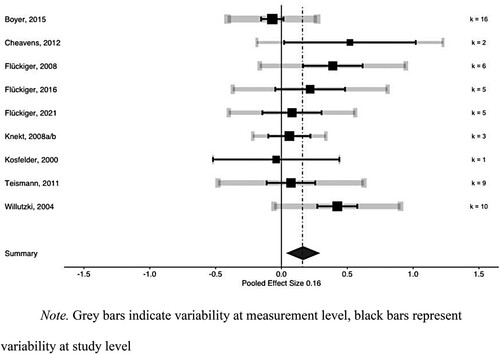
The overall weighted effect size contrasting strength-based psychotherapies vs. bona fide psychotherapies based on 57 effect sizes nested in 9 trials was g = 0.166 (95% CIs [0.027, 0.305], p < .01) in favor of strength-based psychotherapies. The omnibus effect size was computed while accounting for the sample size of each study, as well as within-study dependence between outcome measures. The forest plot () depicts the 57 effect sizes nested in 9 studies. There was non-significant heterogeneity among the effect sizes (Q(56) = 69.1, p = .11; I2 = 19%, CI [16, 22]). A small portion of heterogeneity was primarily impacted by between-study variance (sigma2 level 3 = .03), whereas within-study variance across particular outcome measures was marginal (sigma2 level 2 = .00). That is, the small heterogeneity observed in this meta-analysis was primarily based on the various study contexts and relatively independent from the particular outcome measure used within studies.
Figure 2 Forest plot - Relative efficacy in favor of strength-based methods vis à vis bona fide psychotherapy (s = 9 studies, k = 57 effect sizes, 804 patients).
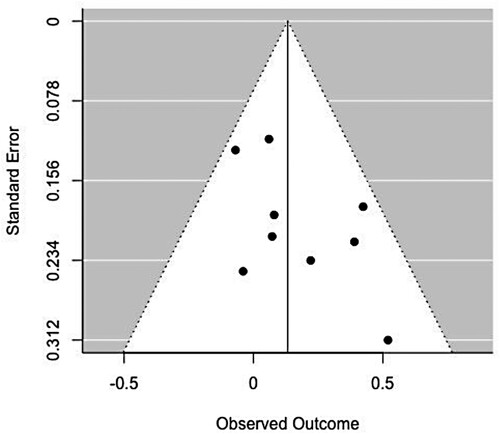
The funnel plot () is a diagram that plots the standard error on the Y-axis and the effect size on the X axis. Due to the relatively small proportion of within-study heterogeneity, we provided the study-level estimates for illustrative purposes (s = 9). In the presence of bias, the plot would show a higher concentration of studies on one side of the mean than the other. There was no indication of publication bias in our sample (asymmetry, p > .48; trim and fill missing studies: 0). As well, we computed how many unpublished non-significant studies it would take to reduce the overall effects size to g = 0. In this dataset, this failsafe value was greater than 11 additional non significant studies.
Moderators of meta-analysis
We analyzed disorder-specific outcomes as a potential moderator in the meta-analysis (1: targeted disorder-specific outcome measure, 0: general outcome). We considered that the disorder-specific measures (e.g., Beck Depression Inventory in depressed patients) might differ from overall distress measures (e.g., Symptom Check List-90, Working Ability Index). As a trend, targeted disorder-specific outcomes (g = 0.178 (95% CIs [0.025, 0.332], p < .05, k = 28)) revealed marginally higher effect sizes in strength-based conditions than general outcomes (g = 0.155 (95% CIs [0.003, 0.306], p < .05; k = 29; moderator: F(2/55) = 2.95, p < .06)).
To summarize, our meta-analysis of comparative trials indicated an additional small but significant benefit of SBM in comparison to other bona fide psychotherapies with a less systematized focus on SBM. Based on 57 effect sizes nested in 9 trials, the effect size on distal, end-of-treatment outcomes was 0.166 in favor of strength-based psychotherapies. In all these trials, SBM were used as augmentation strategies within bona fide psychotherapies. The results of the comparative trials indicate that SBMs may not be a trivial by-product of treatment progress and may provide a unique contribution to psychotherapy outcomes.
Limitations of the Research
This article is based on a systematic synthesis of the research. While we used gold-standard methods to identify any available research on SBM in psychotherapy, no systematic review or meta-analysis is truly exhaustive. To address the complexity in the comparative meta-analysis, we selected only comparative trials with treatment contrasts where the comparison groups were conducted under minimal standards of (bona fide) psychotherapy.
Limitations of our review of process-outcome studies include a relatively small number of studies that met our criteria of direct SBM assessments. Further, most of the reviewed process-outcome studies used correlational designs and could not rule out alternative explanations for their findings (e.g., confound of SBM with other therapist or treatment variables such as general treatment progress). There is little knowledge about the potential short-time impact of strength-based micro methods using analog experiments (see Murphy et al., Citation2022; Strauman et al., Citation2015 for exceptions). Finally, from a methodological perspective, there is a lack of qualitative process studies (see Scheel et al., Citation2013, for an exception).
With respect to the comparative meta-analysis, although most studies have used both disorder-specific and general outcomes, we were not able to investigate particular strength-based outcomes such as treatment satisfaction (Seligman, Citation1995) or individual goal attainment (Kiresuk & Sherman, Citation1968), as they were not collected in the studies. Furthermore, potential serious adverse effects generally were not systematically assessed (e.g., Klatte et al., Citation2022, for exceptions see Flückiger et al., Citation2016, Citation2021). Thus, there is a need for research on a broader range of strength-based as well as disorder-specific outcomes including long-term follow-up. The reviewed studies primarily were conducted in Europe and there is need for comparative trials under bona fide conditions outside of Europe (see Cheavens et al., Citation2012, for an exception, also see Hendriks et al., Citation2018).
Training Implications
SBM are rarely emphasized explicitly in clinical training (Jankowski et al., Citation2020). One possible reason is that they are often perceived as a professional competence of developing positive attitudes toward patients, rather than specific skills that can be taught (e.g., Gelso & Woodhouse, Citation2003; Scheel et al., Citation2013). However, training programs can incorporate an explicit focus on SBM, through the use of structured assessments (e.g., ROMA-T) as well as technical skills and therapeutic strategies to promote strength building. Many psychotherapy approaches emphasize SBM, including positive psychotherapy (e.g., Conoley & Scheel, Citation2018; Parks & Schueller, Citation2014; Rashid & Seligman, Citation2019), strength-based cognitive–behavioral therapy (Cheavens et al., Citation2012; Padesky & Mooney, Citation2012), and resource activation (Flückiger et al., Citation2010; Willutzki & Teismann, Citation2013). Based on these models, we offer the following pantheoretical training recommendations:
Include education regarding the risk of a bias toward negative information in clinical populations (Smith et al., Citation2006).
Address in clinical training SBMs with both long-term perspectives (e.g., matching treatments to patients’ preexisting capabilities and motivational readiness) and short-term perspectives (detection of strengths during sessions, applying methods that foster wellbeing and positive qualities).
Consider discussions on the situation-specific nature of strengths, as certain qualities can be adaptive and healthy in certain situations but maladaptive in others.
Teach strength-based (micro-)skills by means of deliberate practice and using video-based feedback.
Train students to monitor and balance their emphasis on distress and problems with their focus on client strengths. Psychotherapeutic methods should integrate both problem-focused and strength-based perspectives.
Encourage trainees to be responsive to patients’ expressions of their own strengths, while leaving space to discuss their distress when needed.
The principles of the strength-based approach are relevant not only for therapy, but equally for creating optimal learning conditions in training and supervision. Strength-based approaches are best exemplified in the interaction with and supervision of trainees.
Therapeutic Practices
Our systematic review of strength-based in-session studies and meta-analysis of comparative trials suggests that SBM can increase psychotherapy effects. The meta-analytic evidence presented in this article indicates that strength-based psychotherapies prove as efficacious, and sometimes slightly more efficacious, than other bona fide psychotherapies. Based on this research evidence, we recommend that practitioners:
Consider incorporating SBM throughout the treatment phases.
Integrate the assessment of strengths into the clinical interview and standardized assessment and discuss weaknesses and strengths explicitly with the patient.
Integrate weaknesses and strengths in case formulation to derive a more balanced and comprehensive understanding of patients’ narrative and needs.
Be aware that the assessment of positive constructs might identify problematic aspects of functioning (e.g., low self-esteem, hope, gratitude, kindness).
Collaborate with patients in defining and amplifying their strengths. Therapists and patients may disagree on the value or meaning of certain strengths and their role in patients’ functioning. A culturally sensitive approach is crucial here.
Consider obtaining an outside perspective from a significant other on the patients’ strengths; it can sometimes provide beneficial information of which the patient is unaware.
Use SBM to improve and broaden therapy success in terms of the WHO mental health definition (e.g., symptom reduction, wellbeing, social integration).
Create wording or therapist slang that communicates inclusiveness and positive regard (e.g., “You just said highlight moment. What does this mean to you?”, “This voice of your silly old man, does it have something wise to say or is it just silly?”).
Monitor and validate positive change across the whole psychosocial functioning during therapy.
Identify and discuss with the patient functional aspects in behaviors that may easily dismissed as dysfunctional (by either you or the patient).
Identify preexisting problem-solving strategies to facilitate behavioral change and use them to build new skills.
Incorporate patient strengths into homework assignments (e.g., observation of positive moments or experiences during a week, planning enjoyment) and in fostering activities outside of the therapy room (e.g., recreation, physical movement, social support).
Note that sometimes emphasizing strengths may be mistuned with the patient’s experience. For example, a therapist who is overwhelmed by the patient’s despair may try to “cheer them up” and “focus on the positive.” This could cause the patient to feel invalidated and alone if their distress is not address properly.
Acknowledgement
This article is adapted, by special permission of Oxford University Press, by the same authors in C. E. Hill & J. C. Norcross (Eds.) (2023), Psychotherapy skills and methods that work. New York: Oxford University Press. The interorganizational Task Force on Psychotherapy Methods and Skills was cosponsored by the APA Division of Psychotherapy/Society for the Advancement of Psychotherapy.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
*Study included in the process-outcome review and comparative meta-analysis.
- Andrewes, H. E., Walker, V., & O'Neill, B. (2014). Exploring the use of positive psychology interventions in brain injury survivors with challenging behaviour. Brain Injury, 28(7), 965–971. https://doi.org/10.3109/02699052.2014.888764
- Asgharipoor, N., Asgharnejad Farid, A., Arshadi, H., & Sahebi, A. (2012). A comparative study on the effectiveness of positive psychotherapy and group cognitive-behavioral therapy for the patients suffering from major depressive disorder. Iranian Journal of Psychiatry and Behavioral Sciences, 6(2), 33–41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940016/
- Assink, M., & Wibbelink, C. J. M. (2016). Fitting three-level meta-analytic models in R: A step-by-step tutorial. The Quantitative Methods for Psychology, 12(3), 154–174. https://www.tqmp.org/RegularArticles/vol12-3/p154/. https://doi.org/10.20982/tqmp.12.3.p154
- Bandura, A. (2006). Toward a psychology of human agency. Perspectives on Psycholgical Science, 1(2), 164–180. https://doi.org/10.1111/j.1745-6916.2006.00011.x
- Battle, C. C., Imber, S. D., Hoehn-Saric, R., Nash, E. R., & Frank, J. D. (1966). Target complaints as criteria of improvement. American Journal of Psychotherapy, 20(1), 184–192. https://doi.org/10.1176/appi.psychotherapy.1966.20.1.184.
- Bohart, A. C. (2007). Insight and the active client. In L. G. Castonguay, & C. Hill (Eds.), Insight in psychotherapy (pp. 257–277). American Psychological Association. https://doi.org/10.1037/11532-012
- Bolier, L., Haverman, M., Westerhof, G. J., Riper, H., Smit, F., & Bohlmeijer, E. (2013). Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health, 13(1), 119. https://doi.org/10.1186/1471-2458-13-119
- Bonanno, G. A. (2021). The end of trauma: How the new science of resilience is changing ho to think about PTSD. Basic Books.
- *Boyer, B. E., Geurts, H. M., Prins, P. J., & Van der Oord, S. (2015). Two novel CBTs for adolescents with ADHD: The value of planning skills. European Child & Adolescent Psychiatry, 24(9), 1075–1090. https://doi.org/10.1007/s00787-014-0661-5
- Cacioppo, J. T., Berntson, G. G., Norris, C. J., & Gollan, J. K. (2012). The evaluative space model. In P. A. M. Van Lange, A. W. Kruglanski, & E. T. Higgins (Eds.), Handbook of theories of social psychology (pp. 50–72). Sage. https://doi.org/10.4135/9781446249215.n4
- Carter, T., Morres, I. D., Meade, O., & Callaghan, P. (2016). The effect of exercise on depressive symptoms in adolescents: A systematic review and meta-analysis. Journal of the American Academy of Child and Adolescent Psychiatry, 55(7), 580–590. https://doi.org/10.1016/j.jaac.2016.04.016
- Chakhssi, F., Kraiss, J. T., Sommers-Spijkerman, M., & Bohlmeijer, E. T. (2018). The effect of positive psychology interventions on wellbeing and distress in clinical samples with psychiatric or somatic disorders: A systematic review and meta-analysis. BMC Psychiatry, 18(1), 211. https://doi.org/10.1186/s12888-018-1739-2
- Chaves, C., Lopez-Gomez, I., Hervas, G., & Vazquez, C. (2017). A comparative study on the efficacy of a positive psychology intervention and a cognitive behavioral therapy for clinical depression. Cognitive Therapy and Research, 41(3), 417–433. https://doi.org/10.1007/s10608-016-9778-9
- *Cheavens, J. S., Strunk, D. R., Lazarus, S. A., & Goldstein, L. A. (2012). The compensation and capitalization models: A test of two approaches to individualizing the treatment of depression. Behaviour Research and Therapy, 50(11), 699–706. https://doi.org/10.1016/j.brat.2012.08.002
- Conoley, C. W., & Scheel, M. J. (2018). Goal focused positive psychotherapy: A strength-based approach. Oxford University Press.
- Constantino, M. J., Boswell, J. F., Coyne, A. E., Swales, T. P., & Kraus, D. R. (2021). Effect of matching therapists to patients vs assignment as usual on adult psychotherapy outcomes: A randomized clinical trial. JAMA Psychiatry, 78(9), 960–969. https://doi.org/10.1001/jamapsychiatry.2021.1221
- Craske, M. G., Meuret, A. E., Ritz, T., Treanor, M., Dour, H., & Rosenfield, D. (2019). Positive affect treatment for depression and anxiety: A randomized clinical trial for a core feature of anhedonia. Journal of Consulting and Clinical Psychology, 87(5), 457. https://doi.org/10.1037/ccp0000396
- Cronbach, L. J., & Snow, R. E. (1977). Aptitudes and instructional methods: A handbook for research on interactions. Irvington.
- Del Re, A. C. (2013). compute.es: Compute Effect Sizes. https://cran.rproject.org/package=compute.es
- De Vries, L. P., Baselmans, B. M. L., & Bartels, M. (2020). Smartphone-based ecological momentary assessment of wellbeing: A systematic review and recommendations for future studies. Journal of Happiness Studies: An Interdisciplinary Forum on Subjective Wellbeing, 22(5), 2361–2408. https://doi.org/10.1007/s10902-020-00324-7
- Emmons, R. A., & Stern, R. (2013). Gratitude as a psychotherapeutic intervention. Journal of Clinical Psychology, 69(8), 846–855. https://doi.org/10.1002/jclp.22020
- Fava, G. A., Ruini, C., Rafanelli, C., Finos, L., Salmaso, L., Mangelli, L., & Sirigatti, S. (2005). Wellbeing therapy of generalized anxiety disorder. Psychotherapy and Psychosomatics, 74(1), 26–30. https://doi.org/10.1159/000082023
- Fernández-Castilla, B., Declercq, L., Jamshidi, L., Beretvas, N., Onghena, P., & Van den Noortgate, W. (2020). Visual representations of meta-analyses of multiple outcomes: Extensions to forest plots, funnel plots, and caterpillar plots. Methodology, 16(4), 299–315. https://doi.org/10.5964/meth.4013
- *Flückiger, C., Caspar, F., Holtforth, M. G., & Willutzki, U. (2009). Working with patients’ strengths: A microprocess approach. Psychotherapy Research, 19(2), 213–223. https://doi.org/10.1080/10503300902755300
- *Flückiger, C., Forrer, L., Schnider, B., Bättig, I., Bodenmann, G., & Zinbarg, R. E. (2016). A single-blinded, randomized clinical trial of How to implement an evidence-based treatment for generalized anxiety disorder [IMPLEMENT]–effects of three different strategies of implementation. EBioMedicine, 3, 163–171. https://doi.org/10.1016/j.ebiom.2015.11.049
- *Flückiger, C., & Grosse Holtforth, M. (2008a). Focusing the therapist's attention on the patient's strengths: A preliminary study to foster a mechanism of change in outpatient psychotherapy. Journal of Clinical Psychology, 64(7), 876–890. https://doi.org/10.1002/jclp.20493
- Flückiger, C., & Grosse Holtforth, M. (2008b). Ressourcenorientierte Mikroprozess-Analyse (ROMA) - Ressourcendiagnostik und Ressourcenaktivierung im Therapieprozess. Klinische Diagnostik und Evaluation, 1(2), 171–185.
- Flückiger, C., Grosse Holtforth, M., Del Re, A. C., & Lutz, W. (2013). Working along sudden gains - responsiveness on small and subtle early changes and exceptions. Psychotherapy, 50(3), 292–297. https://doi.org/10.1037/a0031940
- *Flückiger, C., & Studer, R. (2009). Bern Strength Task force - Resource activation and problem actuation as interdependent processes (Die Berner- Ressourcen Taskforce - Ressourcenaktivierung und Problembearbeitung unter der Lupe). Verhaltenstherapie & psychosoziale Praxis (VPP), 41(4), 829–839. Tübingen: DGVT-Verlag.
- *Flückiger, C., Vîslă, A., Wolfer, C., Hilpert, P., Zinbarg, R. E., Lutz, W., Grosse Holtforth, M., & Allemand, M. (2021). Exploring change in cognitive-behavioral therapy for generalized anxiety disorder-A two-arms ABAB crossed-therapist randomized clinical implementation trial. Journal of Consulting and Clinical Psychology, 89(5), 454–468. https://doi.org/10.1037/ccp0000639
- Flückiger, C., Wüsten, G., Zinbarg, R. E., & Wampold, B. E. (2010). Resource activation – Using clients’ own strengths in psychotherapy and counseling. Hogrefe.
- *Flückiger, C., Zinbarg, R. E., Znoj, H., & Ackert, M. (2014). Resource activation in generalized anxiety - An observer-based microprocess analysis of patients’ in-session outcomes. Psychotherapy, 51(4), 535–545. https://doi.org/10.1037/a0034119
- Furchtlehner, L. M., Schuster, R., & Laireiter, A.-R. (2020). A comparative study of the efficacy of group positive psychotherapy and group cognitive behavioral therapy in the treatment of depressive disorders: A randomized controlled trial. Journal of Positive Psychology, 15(6), 832–845. https://doi.org/10.1080/17439760.2019.1663250
- *Gassmann, D., & Grawe, K. (2006). General change mechanisms: The relation between problem activation and resource activation in successful and unsuccessful therapeutic interactions. Clinical Psychology & Psychotherapy, 13(1), 1–11. https://doi.org/10.1002/cpp.442
- Gelso, C. J., & Woodhouse, S. (2003). Toward a positive psychotherapy: Focus on human strength. In W. B. Walsh (Ed.), Counseling psychology and optimal human functioning (pp. 171–197). Lawrence Erlbaum Associates Publishers.
- Gonçalves, M. M., Gabalda, I. C., Ribeiro, A. P., Pinheiro, P., Borges, R., Sousa, I., & Stiles, W. B. (2014). The innovative moments coding system and the assimilation of problematic experiences scale: A case study comparing two methods to track change in psychotherapy. Psychotherapy Research, 24(4), 442–455. https://doi.org/10.1080/10503307.2013.835080
- Gonçalves, M. M., Ribeiro, P. A., Mendes, I., Matos, M., & Santos, A. (2011). Tracking novelties in psychotherapy process research: The innovative moments coding system. Psychotherapy Research, 21(5), 497–509. https://doi.org/10.1080/10503307.2011.560207
- Grawe, K. (1997). Research-informed psychotherapy. Psychotherapy Research, 7(1), 1–19. https://doi.org/10.1080/10503309712331331843
- Grawe, K., Regli, D., Smith, E., & Dick, A. (1999). Currative factor analysis (Wirkfaktorenanalyse). Verhaltenstherapie und psychosoziale Praxis, 31, 201–225.
- Grawe, K. (2004). Psychological Therapy. Bern: Hogrefe.
- Griffin, J. (2021). Metapower – Computing and visualizing statistical power for meta-analysis. https://cran.r-project.org/web/packages/metapower/index.html.
- Grosse Holtforth, M., & Grawe, K. (2002). Bern inventory of treatment goals: Part 1 - development and first application of a taxonomy of treatment goal themes. Psychotherapy Research, 12(1), 79–99. https://doi.org/10.1080/713869618
- Helliwell, J. F., Layard, R., Sachs, J., De Neve, J.-E., Aknin, L. B., & Wang, S. (2021). World happiness report 2021. Sustainable Development Solutions Network.
- Hendriks, T., Schotanus-Dijkstra, M., Hassankhan, A., Graafsma, T., Bohlmeijer, E., & de Jong, J. (2018). The efficacy of positive psychology interventions from non-Western countries: A systematic review and meta-analysis. International Journal of Wellbeing, 8(1), 71–98. https://doi.org/10.5502/ijw.v8i1.711
- Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. https://doi.org/10.1002/sim.1186
- Hill, C. E. (2018). Meaning in life: A therapist’s guide. American Psychological Association.
- Hirani, S. S., Norris, C. M., Van Vliet, K. J., Van Zanten, S. V., Karmaliani, R., & Lasiuk, G. (2018). Social support intervention to promote resilience and quality of life in women living in Karachi, Pakistan: A randomized controlled trial. International Journal of Public Health, 63(6), 693–702. https://doi.org/10.1007/s00038-018-1101-y
- Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524. https://doi.org/10.1037/0003-066X.44.3.513
- Hoppen, T. H., & Morina, N. (2021). Efficacy of positive psychotherapy in reducing negative and enhancing positive psychological outcomes: A meta-analysis of randomised controlled trials. BMJ Open, 11(9), e046017. https://doi.org/10.1136/bmjopen-2020-046017
- Jackson, D., & Turner, R. (2017). Power analysis for random-effects meta-analysis. Research Synthesis Methods, 8(3), 290–302. https://doi.org/10.1002/jrsm.1240
- Jankowski, P. J., Sandage, S. J., Bell, C. A., Davis, D. E., Porter, E., Jessen, M., Motzny, C. L., Ross, K. V., & Owen, J. (2020). Virtue, flourishing, and positive psychology in psychotherapy: An overview and research prospectus. Psychotherapy, 57(3), 291–309. https://doi.org/10.1037/pst0000285
- Jebb, A. T., Morrison, M., Tay, L., & Diener, E. (2020). Subjective wellbeing around the world: Trends and predictors across the life span. Psychological Science, 31(3), 293–305. https://doi.org/10.1177/0956797619898826
- *Kech, S. (2008). Einflussfaktoren auf den Behandlungserfolg der Interpersonellen Psychotherapie bei stationären Depressionspatienten: Analyse der Wirkmechanismen [Unpublished dissertational thesis]. University of Freiburg, Germany.
- Kiresuk, T. J., & Sherman, R. E. (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal, 4(6), 443–453. https://doi.org/10.1007/BF01530764
- Klatte, R., Strauss, B., Flückiger, C., Färber, F., & Rosendahl, J. (2022). Defining and assessing adverse events and harmful effects in psychotherapy study protocols: A systematic review. Psychotherapy. Advance online publication. https://doi.org/10.1037/pst0000359
- *Knekt, P., Lindfors, O., Härkänen, T., Välikoski, M., Virtala, E., Laaksonen, M. A., Marttunen, M., Kaipainen, M., Renlund, C., & Helsinki Psychotherapy Study Group. (2008). Randomized trial on the effectiveness of long-and short-term psychodynamic psychotherapy and solution-focused therapy on psychiatric symptoms during a 3-year follow-up. Psychological Medicine, 38(5), 689–703. https://doi.org/10.1017/S003329170700164X
- Knekt, P., Lindfors, O., Sares-Jäske, L., Virtala, E., & Härkänen, T. (2013). Randomized trial on the effectiveness of long- and short-term psychotherapy on psychiatric symptoms and working ability during a 5-year followup. Nordic Journal of Psychiatry, 67(1), 59–68. https://doi.org/10.3109/08039488.2012.680910
- Knekt, P., Heinonen, E., Härkäpää, K., Järvikoski, A., Virtala, E., Rissanen, J., Lindfors, O., & Helsinki Psychotherapy Study Group. (2015). Randomized trial on the effectiveness of long- and short-term psychotherapy on psychosocial functioning and quality of life during a 5-year follow-up. Psychiatry Research, 229(1-2), 381–388. https://doi.org/10.1016/j.psychres.2015.05.113
- *Kosfelder, J. (2000). Handlungsorientierung durch Lösungsfokus. Eine klinisch-psychologische Interventionsstudie. Der Andere Verlag.
- Lee, J. H., Nam, S. K., Kim, A-R, Kim, B., Lee, M. Y., & Lee, S. M. (2013). Resilience: A meta-analytic approach. Journal of Counseling & Development, 91(3), 269–279. https://doi.org/10.1002/j.1556-6676.2013.00095.x
- Li, F., Luo, S., Mu, W., Li, Y., Ye, L., Zheng, X., Xu, B., Ding, Y., Ling, P., Zhou, M., & Chen, X. (2021). Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry, 21(1), 16. https://doi.org/10.1186/s12888-020-03012-1
- Macdonald, J., & Muran, C. J. (2020). The reactive therapist: The problem of interpersonal reactivity in psychological therapy and the potential for a mindfulness-based program focused on “mindfulness-in-relationship” skills for therapists. Journal of Psychotherapy Integration, 31(4), 452–467. https://doi.org/10.1037/int0000200
- Mander, J., Schlarb, A., Teufel, M., Keller, F., Hautzinger, M., Zipfel, S., Wittorf, A., & Sammet, I. (2015). The individual therapy process questionnaire: Development and validation of a revised measure to evaluate general change mechanisms in psychotherapy. Clinical Psychology & Psychotherapy, 22(4), 328–345. https://doi.org/10.1002/cpp.1892
- Munder, T., Flückiger, C., Leichsenring, F., Abbass, A. A., Hilsenroth, M. J., Luyten, P., Rabung, S., Steinert, C., & Wampold, B. E. (2019). Let’s distinguish relative and absolute efficacy to move psychotherapy research forward. Zeitschrift fur Psychosomatische Medizin und Psychotherapie, 65(2), 178–182. https://doi.org/10.13109/zptm.2019.65.2.178
- Murphy, S. T., Cheavens, J. S., & Strunk, D. R. (2022). Framing an intervention as focused on one's strength: Does framing enhance therapeutic benefit? Journal of Clinical Psychology, 78(6), 1046–1057. https://doi.org/10.1002/jclp.23302
- Niemiec, R. M. (2018). Character strengths interventions: A field guide for practitioners. Hogrefe Publishing.
- Padesky, C. A., & Mooney, K. A. (2012). Strength-based cognitive-behavioural therapy: A four-step model to build resilience. Clinical Psychology & Psychotherapy, 19(4), 283–290. https://doi.org/10.1002/cpp.1795
- Parks, A. C., & Schueller, S. M. (2014). The Wiley Blackwell handbook of positive psychological interventions. Hoboken (NJ): Wiley.
- Probst, G., Vîslă, A., & Flückiger, C. (2022). Patients’ symptoms and strengths as predictors of long-term outcomes of CBT for generalized anxiety disorder - A three-level, multi-predictor analysis. Journal of Anxiety Disorders 92:102635. https://doi.org/10.1016/j.janxdis.2022.102635
- Rashid, T., & Seligman, M. E. P. (2019). Positive psychotherapy. Oxford University Press.
- Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models. Sage.
- *Regli, D., Bieber, K., Mathier, F., & Grawe, K. (2000). Beziehungsgestaltung und Aktivierung von Ressourcen in der Anfangsphase von Therapien. Verhaltenstherapie und Verhaltensmedizin, 21(4), 399–420.
- Riches, S., Schrank, B., Rashid, T., & Slade, M. (2016). WELLFOCUS PPT: Modifying positive psychotherapy for psychosis. Psychotherapy, 53(1), 68–77. https://doi.org/10.1037/pst0000013
- Ryan, R. M., & Deci, E. L. (2008). A self-determination theory approach to psychotherapy: The motivational basis for effective change. Canadian Psychology/Psychologie Canadienne, 49(3), 186–193. https://doi.org/10.1037/a0012753
- Satir, V., Banmen, J., Gerber, J., & Gomori, M. (1991). The Satir Model: Family therapy and beyond. Science and behavior books. Palo Alto (CA): Science & Behavior Books.
- Scheel M.J., Davis C.K., & Hederson J.D. (2013). Therapist use of client strengths: A qualitative study of positive processes. The Counseling Psychologist 41(3), 392–427. https://doi.org/10.1177/0011000012439427
- Scheel, M. J., Hanson, W. E., & Razzhavaikina, T. I. (2004). The process of recommending homework in psychotherapy: A review of therapist delivery methods, client acceptability, and factors that affect compliance. Psychotherapy: Theory, Research, Practice, Training, 41(1), 38–55. https://doi.org/10.1037/0033-3204.41.1.38
- *Schilling, V. N. L. S., Boyle, K. S., Rubel, J. A., Flückiger, C., Zimmermann, D., & Lutz, W. (2021). Patients’ and therapists’ actions on the precipice of change: Session processes before sudden gains and sudden losses. Journal of Psychotherapy Integration, 31(3), 238–256. https://doi.org/10.1037/int0000242
- Scholz, U., Doña, B. G., Sud, S., & Schwarzer, R. (2002). Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment, 18(3), 242–251. https://doi.org/10.1027//1015-5759.18.3.242
- Schürmann-Vengels, J., Appelbaum, S., Apel, M.-K., Trimpop, L., Muermans, M. M., Ostermann, T., Teismann, T., & Willutzki, U. (2022). Association of patients’ pre-therapy strengths and alliance in outpatient psychotherapy: A multilevel growth curve analysis. Psychotherapy Research. Advance online publication. https://doi.org/10.1080/10503307.2022.2146543
- Seligman, M. E. (1995). The effectiveness of psychotherapy. The consumer reports study. The American Psychologist, 50(12), 965–974. https://doi.org/10.1037/0003-066X.50.12.965
- Sin, N. L., & Lyubomirsky, S. (2009). Enhancing wellbeing and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. https://doi.org/10.1002/jclp.20593
- *Smith, E. C., & Grawe, K. (2003). What makes psychotherapy sessions productive? A new approach to bridging the gap between process research and practice. Clinical Psychology and Psychotherapy, 10(5), 275–285. https://doi.org/10.1002/cpp.377
- *Smith, E. C., & Grawe, K. (2005). Which therapeutic mechanisms work when? A step towards the formulation of empirically validated guidelines for therapists’ session-to-session decisions. Clinical Psychology and Psychotherapy, 12(2), 112–123. https://doi.org/10.1002/cpp.427
- Smith, N. K., Larsen, J. T., Chartrand, T. L., Cacioppo, J. T., Katafiasz, H. A., & Moran, K. E. (2006). Being bad isn’t always good: Affective context moderates the attention bias toward negative information. Journal of Personality and Social Psychology, 90(2), 210–220. https://doi.org/10.1037/0022-3514.90.2.210
- Solomonov, N., Victoria, L. W., Dunlop, K., Respino, M., Hoptman, M. J., Zilcha-Mano, S., Oberlin, L., Liston, C., Areán, P. A., Gunning, F. M., & Alexopoulos, G. S. (2020). Resting state functional connectivity and outcomes of psychotherapies for late-life depression. The American Journal of Geriatric Psychiatry, 28(8), 859–868. https://doi.org/10.1016/j.jagp.2020.04.008
- Strauman, T. J., Socolar, Y., Kwapil, L., Cornwell, J. F., Franks, B., Sehnert, S., & Higgins, E. T. (2015). Microinterventions targeting regulatory focus and regulatory fit selectively reduce dysphoric and anxious mood. Behaviour Research and Therapy, 72, 18–29. https://doi.org/10.1016/j.brat.2015.06.003
- Suhr, M., Risch, A. K., & Wilz, G. (2017). Maintaining mental health through positive writing: Effects of a resource diary on depression and emotion regulation. Journal of Clinical Psychology, 73(12), 1586–1598. https://doi.org/10.1002/jclp.22463
- Tay, L., & Diener, E. (2011). Needs and subjective wellbeing around the world. Journal of Personality and Social Psychology, 101(2), 354–365. https://doi.org/10.1037/a0023779
- *Teismann, T., Dymel, W., Schulte, D., & Willutzki, U. (2011). Ressourcenorientierte Akutbehandlung unipolarer Depressionen: Eine randomisierte kontrollierte Psychotherapiestudie. Psychotherapie, Psychosomatik und Medizinische Psychologie, 61(7), 295–302. https://doi.org/10.1055/s-0030-1270453
- Tolpin, M (2002). Doing psychoanalysis of normal development: Forward edge transferences. In A. Goldberg (Ed.), Postmodern self psychology (pp. 167–190). The Analytic Press/Taylor & Francis Group.
- Uliaszek, A. A., Rashid, T., Williams, G. E., & Gulamani, T. (2016). Group therapy for university students: A randomized control trial of dialectical behavior therapy and positive psychotherapy. Behaviour Research and Therapy, 77, 78–85. https://doi.org/10.1016/j.brat.2015.12.003
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. https://doi.org/10.18637/jss.v036.i03
- Vîslă, A., Zinbarg, R. E., Hilpert, P., Allemand, M., Flückiger, C. (2021). Worry and positive episodes in the daily lives of individuals with generalized anxiety disorder: An ecological momentary assssment study. Frontiers in Psychology – Psychology for Clinical Settings, 12, 722881. https://doi.org/10.3389/fpsyg.2021.722881
- von Consbruch, K., Flückiger, C., Stangier, U., Beutel, M. E., Herpertz, S., Hoyer, J., Leibing, E., Leichsenring, F., Salzer, S., Strauß, B., & Wiltink, J. (2013). WIFA-k: Ein neues Messinstrument zur zeitökonomischen Erfassung allgemeiner Wirkfaktoren nach Grawe [Assessing common factors in psychotherapy: Psychometric properties of a new time-economic instrument (WIFA-k)]. PPmP: Psychotherapie Psychosomatik Medizinische Psychologie, 63(7), 286–289. https://doi.org/10.1055/s-0032-1331206
- Wachtel, P. L. (2011). Therapeutic communication: Knowing what to say when (2nd ed.). Guilford.
- Wampold, B. E., Mondin, G. W., Moody, M., Stich, F., Benson, K., & Ahn, H.-n. (1997). A metaanalysis of outcome studies comparing bona fide psychotherapies: Empiricially, "all must have prizes." Psychological Bulletin, 122(3), 203–215. https://doi.org/10.1037/0033-2909.122.3.203
- Wampold, B. E., & Flückiger, C. (2023). The alliance in mental health care: Conceptualization, evidence and clinical application. World Psychiatry, 22(1), 1–17. https://doi.org/10.1002/wps.21035
- Wampold, B. E., & Imel, Z. E. (2015). The great psychotherapy debate: The evidence for what makes psychotherapy work (2nd ed.). Routledge/Taylor & Francis Group.
- White, C. A., Uttl, B., & Holder, M. D. (2019). Meta-analyses of positive psychology interventions: The effects are much smaller than previously reported. PloS one, 14(5), e0216588. https://doi.org/10.1371/journal.pone.0216588
- *Willutzki, U., Haas, H., Neumann, B., Koban, C., & Schulte, D. (2004). Zur Psychotherapie sozialer Ängste: Kognitive Verhaltenstherapie im Vergleich zu einem kombiniert ressourcenorientierten Vorgehen. Eine randomisierte kontrollierte Interventionsstudie. Zeitschrift für Klinische Psychologie und Psychotherapie, 33(1), 42–50. https://doi.org/10.1026/0084-5345.33.1.42
- Willutzki, U., & Teismann, T. (2013). Ressourcenaktivierung in der Psychotherapie. Hogrefe.
- Yulish, N. E., Goldberg, S. B., Frost, N. D., Abbas, M., Oleen-Junk, N. A., Kring, M., Chin, M. Y., Raines, C. R., Soma, C. S., & Wampold, B. E. (2017). The importance of problem-focused treatments: A meta-analysis of anxiety treatments. Psychotherapy, 54(4), 321–338. https://doi.org/10.1037/pst0000144
- Zheng, W., Li, Q., Lin, J., Xiang, Y., Guo, T., Chen, Q., Cai, D., & Xiang, Y. (2016). Tai Chi for schizophrenia: A systematic review. Shanghai Archives of Psychiatry, 28(4), 185–194. https://doi.org/10.11919/j.issn.1002-0829.216051