Abstract
Context: Pain and depression are two prevalent secondary complications associated with spinal cord injury (SCI) that negatively impact health and well-being. Self-management strategies are growing in popularity for helping people with SCI to cope with their pain and depression. However, there is still a lack of research on which approaches are best suited for this population.
Objective: The aim of this scoping review was to determine what is known about the self-management of pain and depression through the use of pharmacological and non-pharmacological therapies in adults with SCI.
Methods: Seven electronic databases were searched for articles published between January 1, 1990 and June 13, 2017. Grey literature was searched and additional articles were identified by manually searching the reference lists of included articles.
Results: Overall, forty-two articles met the inclusion criteria; with the majority reporting on the self-management of pain, rather than on depression or on both complications. Non-pharmacological interventions were more likely to include self-management strategies than pharmacological interventions. A limited number of studies included all of the core self-management tasks and skills.
Conclusions: There are significant knowledge gaps on effective self-management interventions for pain and depression post-SCI. There is a need to develop interventions that are multi-faceted, which include both pharmacological and non-pharmacological therapies to address multimorbidity.
Introduction
A spinal cord injury (SCI) is a devastating injury with damage to the spinal cord that occurs from either a traumatic or non-traumatic event.Citation1 Damage to the spinal cord can result in paraplegia or tetraplegia, but the severity of the injury depends on the cause and location of the damage.Citation2,Citation3 There are debilitating secondary complications associated with SCI, often caused by the partial or complete loss of motor and sensory functions and the inability to control bodily functions.Citation4,Citation5 Common secondary complications include pain,Citation6 depression,Citation7 anxiety,Citation8 cardiovascular complications,Citation9 pressure ulcers,Citation10 respiratory complications,Citation11 spasticity,Citation12 urinary and bowel complicationsCitation9 and fractures.Citation12
Importantly, secondary complications of a disabling condition, such as a SCI, can be reduced by incorporating self-management tasks and skills into daily life.Citation13 For this reason, programs involving self-management are becoming increasingly common.Citation14 Self-management has been commonly defined using Barlow’s definition as,
an individual’s ability to manage the symptoms, treatment, physical and psychosocial consequences and lifestyle changes inherent in living with a chronic condition. Efficacious self-management encompasses ability to monitor one’s condition and to affect the cognitive, behavioural and emotional responses necessary to maintain a satisfactory quality of life (p. 178).Citation15
Lorig and Holman identify three main categories of self-management tasks: medical management, role management and emotional management and six core skills: problem solving, decision making, using resources, communicating with healthcare providers, taking action and self-tailoring.Citation16 Self-management strategies have shown positive outcomes in individuals with chronic conditions.Citation15,Citation17,Citation18 However, in individuals with multiple chronic conditions (e.g. multimorbidity), including persons with SCI, self-management is more complex than in individuals with one chronic condition because the dominant condition is often prioritized for management.Citation19
Pain and depression are among the most common chronic complications of SCI, co-occur frequently, and have overlapping implications for well-being. The majority of persons with SCI report experiencing some type of pain,Citation20 with about half endorsing neuropathic pain.Citation21 SCI-related pain correlates with multiple adverse effects on physical,Citation9 emotional,Citation22,Citation23 and social health.Citation24,Citation25 These include: depression,Citation6,Citation26 unemployment,Citation27 reduced function,Citation28 social isolationCitation28 and decreased quality of life.Citation29 Similarly, approximately a quarter of persons with SCI experience depression,Citation30 a rate that is substantially higher than the general population worldwide prevalence of 3.2%.Citation31 As with pain, depression in persons with SCI represents a major concern because it is connected to multiple negative health outcomes including: urinary tract infections, poor social and community integration, decreased self-appraised health, pressure ulcers, fewer leisure activities, the lack of meaningful social pursuits and mortality.Citation32 Depression may also interfere with the physical rehabilitation process.Citation33
Several self-management interventions and programs have highlighted positive outcomes in individuals with pain and/or depression.Citation34,Citation35 A recent longitudinal study (n = 250) published in 2016 identified that primary care patients with comorbid musculoskeletal pain and depression (receiving antidepressant therapy and a pain self-management program) had greater self-efficacy for managing their pain and depression when compared to the group receiving usual care (advised to seek care from their primary care provider).Citation35 Similarly, a randomized controlled trial (N = 60) of an online pain self-management program conducted among patients with chronic non-cancer pain demonstrated similar positive results.Citation34 Participants in the intervention group had lower pain severity, pain interference, opioid misuse and depressive symptoms, as well as increased pain self-efficacy. Despite the positive results of self-management programs for addressing pain and depression in the general population,Citation34,Citation35 little is known about the use of self-management strategies for pain and depression among adults with SCI.
Given the benefits of self-management strategies for the management of SCI,Citation36,Citation37 as well as the prevalence and complexity of pain and depression, there is a need to improve our knowledge on existing self-management strategies and interventions to help people with SCI better cope with these significant complications. An individual’s ability to self-manage their pain may be hindered by comorbid depression.Citation35 Thus, when developing and implementing self-management strategies, pain and depression might be better considered in conjunction, rather than separately. Currently there is a lack of research on self-management strategies for pain and depression among persons with SCI.
While self-management approaches have been used extensively in other conditions with pain and depression, the potential value for people with SCI remains in its infancy with key questions still unanswered. Key issues include, but are not limited to: what types of interventions work best for SCI?; when and where should these interventions be delivered?; who should deliver these interventions?; and what formats and supports are considered useful by those undergoing the intervention and those implementing them? The purpose of this scoping review was to examine the literature to determine what is known about the self-management of pain and depression through the use of pharmacological and non-pharmacological therapies in adults with SCI. In addition to identifying what is known, suggestions for future research were developed in order to fill gaps in the literature.
Materials and methods
Scoping reviews are conducted to analyze the extent, range and nature of available research, determine if a systematic review is feasible, summarize and disseminate research findings and identify gaps in the literature.Citation38 This review was conducted using the six stage methodological framework of scoping reviews presented by Levac and colleagues.Citation39
Stage 1 – Identifying the research question
The research question leading this scoping review was: What is known about the self-management of pain and depression through the use of pharmacological and non-pharmacological therapies in adults with SCI? Through this scoping review we identified: (1) types of research studies on this topic and described various methods of pain and depression management being used; (2) characteristics of adults with SCI included in studies (e.g. etiology and level of injury, functional status, etc.); and (3) characteristics of interventions and outcomes (e.g. knowledge, attitudes and behaviors regarding self-management).
Stage 2 – Identifying relevant studies
The search strategy, developed in consultation with a Medical Librarian in Rehabilitation Sciences at the University of Toronto, included literature between January 1, 1990 and June 13, 2017 using the following electronic databases: MEDLINE (Ovid Interface), EMBASE (Ovid Interface), PsycINFO (Ovid Interface), AMED (Ovid Interface), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO Interface), SPORTDiscus (EBSCO Interface) and Cochrane Library. Grey literature was searched on TSpace, Spinal Cord Injury Research Evidence, the Rick Hansen Institute, Spinal Cord Injury Ontario and the World Health Organization websites. A manual search of the included article reference lists was also performed to ensure all relevant articles were included.
The search strategy (Supplemental Material A) was developed based on appropriate indexing and command line syntax for each database. Relevant articles were identified by searching the following keywords using Boolean operators, truncation, wild cards and proximity operators: spinal cord injuries, self care, self-management, medication adherence, pain, depression. A previously published and recommended ‘gold standard’ search strategy for identifying spinal cord damage (not due to trauma) was adapted for each database and incorporated into our search.Citation40
Stage 3 – Study selection
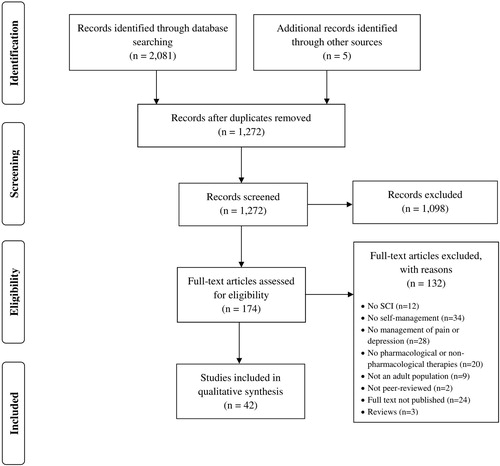
Study selection was guided by Bramer’s three stage methodCitation41 and managed using a reference manager software system (EndNote X8 software). Bramer’s three stage method is used for the de-duplication process; and the stages consist of (1) changing settings for displayed fields and installing custom export filters and formats; (2) importing articles from the seven databases into a temporary library, exporting them in an adapted format and importing them into a new library; and (3) modifying the settings for fields to detect and remove duplicates.Citation41 The initial searches identified 2,081 articles, but after importing the articles to EndNote and removing duplicates using Bramer’s three stage method, 1,267 articles remained for further assessment (see ).
Included studies met the following criteria: (1) adults older than 18 years of age with SCI; (2) focused on self-management, which included concepts defined by Barlow and the categories of self-management described by Lorig and Holman;Citation15,Citation16 (3) related to pain or depression; (4) peer-reviewed or grey literature; and (5) published from January 1, 1990 to June 13, 2017. To meet criteria two (focus on self-management), the article was required to mention or discuss one of the concept’s defined in Barlow’s definition of self-management (e.g. managing symptoms and treatment, psychosocial support, physical consequences, and lifestyle changes due to pain or depression) or at least one component of Lorig and Homan’s self-management framework. Lorig and Holman’s self-management framework describes the three self-management tasks and six self-management skills when implementing self-management education into healthcare systems (see Supplemental Material B).Citation16 The criteria for self-management were intentionally kept broad, as one of the purposes of this review was to characterize the types of self-management approaches in the literature for pain and depression.
Studies were excluded if they met any of the following criteria: (1) books, book chapters, opinion pieces, editorials, case studies/reports, case laws, trial papers, narratives; (2) published before January 1, 1990; (3) studies on animals; (4) population younger than 18 years of age; or (5) conference and poster abstracts without a published full-text article. Articles were excluded prior to 1990 given that the majority of research on self-management occurred after this date.Citation15
The title and abstract screening was completed using a study-specific form to determine study eligibility and identify discrepancies between reviewers. Prior to beginning, 20 articles were independently screened by all three reviewers (LC, CD, SJTG); disagreements were discussed until consensus was reached. Two reviewers then independently screened the next 110 articles (LC and CD). The overall kappa agreement was 0.91; which is greater than the commonly accepted threshold of 0.80 for high agreement.Citation42 The remaining articles were screened by a single reviewer (LC). After the title and abstract screening, 169 articles were imported into Covidence (a software system for article review and data extraction) for full-text review. Two reviewers (LC and CD) independently screened ten full-text articles, with a kappa agreement of 1.0 the remaining articles were screened by a single reviewer (LC). Following full-text analysis, 42 articles were included in the scoping review.
Stage 4 – Charting the data
A single reviewer (LC) charted the data using a data extraction form in Microsoft Excel. Questions that arose during data extraction were discussed with the core team (LC, SJTG, CD) who met on a weekly basis. The data extraction form was adapted from two frameworks: 1) Lorig and Holman’s components of self-management framework as previously describedCitation16 and 2) Ogallo and Kanter’s framework.Citation43 Ogallo and Kanter’s framework for medication therapy management was developed based on the parent models of medication therapy management service and chronic care.Citation43 The collated data included general information, study characteristics, study population, population characteristics, intervention characteristics, self-management characteristics, and study outcomes and findings.
Stage 5 – Collating, summarizing, and reporting results
The data was extracted and entered into Microsoft Excel which allowed for analysis and comparison of different variables across multiple studies. Qualitative studies were reviewed to identify major themes.
Results
Of the 174 full-text articles reviewed, 132 were excluded and 42 articles met the inclusion criteria (see ). Of the included studies, 38 were identified from the literature search and four were found from other sources. Three literature reviews were identified (one literature review and two systematic reviews). These reviews were not included in the final data extraction, but their reference lists were searched for relevant articles.
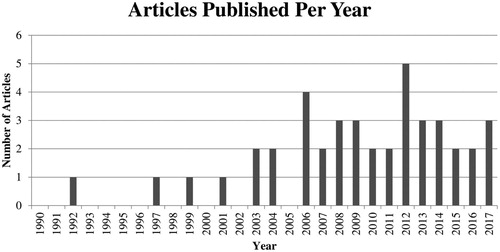
Key study characteristics of included articles are summarized in . The included articles consisted of seven qualitative studies, 28 quantitative studies and seven mixed method studies. These studies were conducted in seven countries: United States (n = 17), Canada (n = 6), Sweden (n = 6), Netherlands (n = 5), United Kingdom (n = 4), Australia (n = 3) and Hungary (n = 1). As seen in , from 1990 to 2002, a small number of studies (n = 4) were published on the self-management of pain and/or depression in adults with SCI. There has been an upward trend since 2003, with 38 articles published on this topic in the last 15 years.
Table 1 Study characteristics identified in scoping review of articles January 1, 1990 to June 13, 2017.
The overall sample sizes of the included studies were relatively small, with an average of 118 participants and median of 38 participants across all 42 studies. The variation in sample size was large, ranging from 7 participants to 526 participants. On average, the breakdown of the population based on sex was 69.6% male and 30.4% female. There were only three studies that had a greater percent of female participants than male.Citation44,Citation49,Citation71 Approximately three quarters of the studies reported the type of SCI (n = 31) and the level of injury (n = 32), with slightly more than half (n = 25) reporting the participant’s functional status. Of the 31 studies that reported the type of SCI, 20 studies had participants with both traumatic and non-traumatic injuries,Citation44,Citation47,Citation49,Citation51,Citation53,Citation56–59,Citation61,Citation63–65,Citation67,Citation69,Citation73,Citation77,Citation79,Citation80,Citation85 10 studies had participants with only traumatic injuriesCitation45,Citation62,Citation66,Citation70,Citation72,Citation74–76,Citation81,Citation84 and 1 included participants with only non-traumatic injuries.Citation55 None of the studies reported if the participants were diagnosed with other comorbidities.
Approximately half (n = 20) of the studies discussed or evaluated interventions (n = 11 pain; n = 7 depression; n = 2 both), as seen in . Of the studies involving interventions, the method of delivery mostly included in-person (n = 16), technology (e.g. online books with reflective responses and telephone counseling; n = 3) and 1 using both in-person and technological components (e.g. self-hypnosis began with in-person sessions then used a compact disc (CD) recording and telephone interviews to assess pain intensity). Based on the description and content of the interventions, about half (n = 11) were single-component (e.g. yoga), while the other half (n = 9) were multi-component (e.g. included several components such as cognitive behavioral therapy (CBT) that consists of educational, cognitive, and behavioral elements). Approximately one quarter (n = 6) used a multidisciplinary team to facilitate the intervention.
Table 2 Intervention characteristics identified in scoping review of articles January 1, 1990 to June 13, 2017.
The majority of articles (n = 31) focused on the self-management of pain. The most commonly used scales for measuring pain were the Numeric Rating Scale, Visual Analogue Scale, Brief Pain Inventory, Multidimensional Pain Inventory and the Chronic Pain Grade Scale. There were 11 studies that evaluated interventions for pain (), with the majority involving an in-person intervention (n = 10). The majority (n = 9) of these interventions focusing on pain had favorable outcomes, while two of the interventions showed no improvements in pain intensity. The two interventions (yoga and a pain management programCitation44,Citation61) that showed no improvements in pain intensity, did show favorable outcomes in mood, quality of sleep, self-compassion and symptoms of depression. There were seven qualitative studies identified, all of which focused on the self-management of pain. The qualitative studies highlighted the following themes: living with and the impact of pain, coping strategies, understanding pain, informal and formal support systems, and the importance of empowerment and autonomy with self-management.
Of all the included articles, only seven focused on the self-management of depression. The most frequently used measurements for depression were the Beck Depression Inventory, the Hospital Anxiety and Depression Scale and the Center for Epidemiological Studies – Depression Scale. As seen in , just under half of the interventions (n = 3) for depression used technological components (e.g. telephone counseling and CD recordings for self-hypnosis), while just over half (n = 4) included in-person components. All of the depression interventions demonstrated improvements in depression or depressive symptoms, psychological well-being, emotional state or mood. One of the interventions targeting both pain and depression resulted in reduced pain and depression, while the other had no significant effect on either. There were no qualitative studies identified on the self-management of depression.
Only four studies included all of Lorig and Holman’s core self-management tasks and skills (). Of the core tasks, all identified medical management (n = 42), just over half identified emotional management (n = 23) and only one quarter identified role management (n = 11). The types of medical management consisted of non-pharmacological therapies (n = 27) or a combination of non-pharmacological and pharmacological therapies (n = 15). The most common types of non-pharmacological therapies discussed were exercise (n = 16), massage (n = 13), relaxation (n = 10), acupuncture (n = 9) and Transcutaneous Electrical Nerve Stimulation (TENS) (n = 9). Antidepressants (n = 6), anticonvulsants (n = 5), opioids (n = 4) and non-steroidal anti-inflammatory drugs (NSAIDs) (n = 4) were the most commonly reported pharmacological therapies.
Table 3 Components of self-management identified in scoping review of articles January 1, 1990 to June 13, 2017+*
✓ – identified in article; X – not identified.
The studies that included all of the self-management tasks and skills were two CBT programs,Citation73,Citation85 a pain management programCitation44 and a multidisciplinary program.Citation67 CBT programs are comprised of educational, cognitive and behavioral elements in order to improve coping skills for individuals with SCI. One CBT programCitation85 was conducted by a psychologist and a trainer at a rehabilitation center once per week for ten weeks. The program included a personal workbook that consisted of all of the program components such as: goal setting, information on relaxation techniques and communication. This program resulted in improved pain cognitions and pain coping strategies. The other CBT program that included all self-management tasks and skills was conducted by a psychologist at a rehabilitation center biweekly for an average of 11 session, which resulted in improved depression scores.Citation73 A key component of the CBT program was the development of coping skills including problem solving, cognitive appraisal skills and behavioral activation which align with the components of self-management. The pain management program was comprised of educational sessions, behavioral therapy, light exercise, relaxation techniques, stretching, and body awareness training to assess its effect on a number of different outcomes (pain intensity, sleep quality, mood, life satisfaction, health-related quality of life and sense of coherence).Citation44 The specific self-management components of the program were goal setting and continuing home assignments. This program consisted of two sessions per week for ten weeks and resulted in improved mood and quality of sleep, but had no reduction in pain intensity. The multidisciplinary program was delivered by a physical therapist, nurse and psychologist and consisted of education, cognitive and behavioral elements that target patients coping with chronic neuropathic SCI pain.Citation67 A workbook was provided to each participant with information and exercises on goal-setting, communication, relaxation techniques and relationships. This program occurred once per week for ten weeks and displayed favorable long-term outcomes on pain intensity, pain-related disability, anxiety and participation in activities.
Another important finding in this review is the concentration of studies focused on non-pharmacological therapies, instead of evaluating self-management through the use of pharmacological treatments and perhaps more importantly, using both. In our review of the qualitative studies (see ) challenges with pharmacotherapies were highlighted. Common challenges included multiple drug treatments, reliance on medication and ineffective drug treatments. Of the 20 interventions identified in this review, only one included both pharmacological and non-pharmacological components to managing pain.Citation44
Table 4 Themes from qualitative studies identified in scoping review of articles January 1, 1990 to June 13, 2017.
Discussion
This scoping review analyzed the extent, range and nature of available research on what is known about the self-management of pain and depression through the use of pharmacological and non-pharmacological therapies in adults with SCI. Our findings showed that the majority of studies have focused on the self-management of pain, with a minimal number focusing on the self-management of depression or both pain and depression. All of the included articles focused on the core task of medical management with fewer focused on core tasks of emotional and role management. Our review highlighted a need for future research to address the following: (1) incorporate all three core self-management tasks (medical management, emotional management and role management); (2) utilize a multidisciplinary approach focusing both on pain and depression; (3) evaluate both pharmacological and non-pharmacological therapies; and (4) describe more details about population demographics and clinical characteristics.
Given the complexity of SCI, it is important for self-management interventions to address all three key domains of self-management.Citation86 In a recent systematic review of qualitative studies, Liddy et al. examined the perspectives of patients with multiple chronic conditions and the challenges with self-management.Citation86 The complexity of self-managing multiple chronic conditions was highlighted, as symptoms are often independent, such as pain and depression.Citation86 The coexistence of pain and depression often results in more negative clinical outcomes, health utilization and overall health and well-being.Citation87–89 The interdependency of symptoms highlights the need for self-management interventions to be multi-faceted and comprehensive. In particular, most of the challenges identified in Liddy et al.’s review were related to medical and emotional management of symptoms. Given that persons with SCI often have multiple chronic conditions,Citation90,Citation91 findings from this review reinforce the need for self-management interventions to target not only medical management, but also emotional and role management.
Similarly, there is evidence to support multidisciplinary approaches for persons with multimorbidity.Citation92,Citation93 Of the included articles, slightly less than half of the interventions reported using multidisciplinary teams to facilitate interventions. Psychologists, physical therapists and nurses were common members of the multidisciplinary teams identified in our scoping review. In our scoping review, the interventions with a multidisciplinary team facilitating the intervention were effective in the improvement of pain, depressive symptoms, coping strategies, sense of control and socialization. These positive outcomes suggest the need for more research to be done in this area. Previous research has highlighted the importance of a multidisciplinary team approach for managing SCI and secondary complications.Citation94,Citation95 For example, Derakhshanrad and colleagues found that the use of a multidisciplinary team comprised of a neurosurgeon, urologist, occupational therapist, coloproctologist, psychologist, physiatrist and nurse specialist was effective in improving the functional outcome, as measured by the Spinal Cord Independence Measure, in patients with SCI.Citation95 In addition to improving patient outcomes, Alizo et al., recently demonstrated that a multidisciplinary team consisting of a physical therapist, occupational therapist, respiratory therapist, nutritionist, pharmacist, wound care specialist and neurosurgical and orthopedic services for persons with traumatic SCI improved hospital outcomes and reduced the length of hospital stays.Citation96
In addition to using multidisciplinary approaches, there is evidence to support the use of technology for individuals with multimorbidity. Our scoping review identified a total of four interventions that included a technological component. The technologies used for the interventions identified in this review include: online books with reflective responses, two telephone counseling programs and self-hypnosis which incorporated a CD recording. In particular, the use of telephone-based counseling is attractive for this population since there is evidence showing that this modality can improve coping skills, increase levels of community integration and reduce depression in adults with physical disabilities. Similarly, a systematic review by Dorstyn, Mathias and Denson identified that telecounselling services following SCI can improve the management of pain and sleep difficulties.Citation97 As technology continues to increase in popularity for self-management, technological interventions for individuals with SCI should be investigated.
This scoping review highlights a lack of studies that focus on self-management through the use of pharmacological treatments, as the primary concentration is on non-pharmacological treatments. While pharmacological treatments are commonly recommended and prescribed,Citation98 there is limited published literature to date on how adults with SCI self-manage their pain and/or depression through the use of medications (e.g. knowledge, attitudes and beliefs about medication, how persons are communicating about medications with care providers, monitoring side effects and outcomes). While it is known that when used in conjunction, pharmacological and non-pharmacological therapies are beneficial for the management of pain,Citation99,Citation100 our review highlighted a gap in interventions using both, as there was only one intervention that incorporated both for the management of pain.Citation44 This gap further emphasizes the importance for future research to incorporate self-management strategies that focus on both pharmacological and non-pharmacological components.
Finally, we found a lack of consistency in reporting on sociodemographic and clinical characteristics of the study populations. Characteristics that were often not reported or not consistently reported include: income, ethnicity, use of mobility devices, employment status, type of SCI, level of injury, functional status and geographic location. There were 11 studies in this review that neglected to classify the type of injury as traumatic or non-traumatic. Of the 31 studies that did specify the type of injury, the majority did not examine how the self-management strategies or intervention outcomes differed by type of injury. Given the differences in age and sex profiles for persons with traumatic SCI and non-traumatic SCI, with an older and more even sex distribution among the latter group,Citation101 it is important to understand how population characteristics may impact self-management strategies which may inform the tailoring of programs to specific populations for optimal success.
Based on our scoping review, there have been no peer-reviewed studies to date on the SCI population regarding sex and gender differences in self-management. This review highlighted a gap in the literature examining self-management among women with SCI, with a bias for research among men with SCI, as we only identified two of the included articles to have more female participants. The two articles with more female participants were Curtis et al.’s yoga program and Norrbrink Budh and Lundeberg’s cross-sectional study assessing what non-pharmacological treatments have been and are being used.Citation49,Citation71 Moreover, men and women also have different responses to multimodal pain management programs that consist of individual treatments (doctor’s appointments, physical therapy and psychotherapy) and group treatments (relaxation techniques, physical therapy, CBT, pain education, nutrition advice and social counseling).Citation102 Furthermore, future research should investigate self-management interventions with a focus on strategies for women with SCI in managing their pain and depression.
Limitations
Despite an exhaustive search of seven electronic databases and grey literature, it is possible that relevant articles were missed and therefore, not included in the review. In order to minimize the possibility of missed articles, our search strategy was adapted to search text words and keywords that included all key concepts relating to SCI, self-management, pain and depression. It is possible we missed studies that focused on self-management for SCI in general and may have discussed pain and depression but were not flagged with our search strategy. In addition, we conducted a manual search of the reference lists of included articles. Results of self-management tasks and skills were limited to studies that explicitly mentioned, incorporated as part of the intervention, or evaluated as an outcome. It is possible that studies were measuring more self-management tasks or skills, but they were not explicitly mentioned. Since this is a scoping review, there is no assessment of the quality of the interventions discussed.
Conclusion
This scoping review analyzed the extent, nature and range of available research pertaining to the topic of the self-management of pain and depression in adults with SCI. Multiple gaps were revealed as the extent of information was limited in several areas; thus leading to the following recommendations for future research: self-management interventions should incorporate components of emotional, role and medical management; interventions should be multifaceted and evaluate both pharmacological and non-pharmacological therapies; and interventions should address multimorbidity and ways to support the self-management of co-existing pain and depression. Additionally, a lack of consistency in reporting sociodemographic and clinical characteristics was identified. Having an understanding of these characteristics of the SCI populations would allow for the gathering of clues about potential differences between groups (e.g. women vs. men, those of low vs. high level of education or income status, those living in an urban vs. rural area, those with traumatic SCI vs. non-traumatic SCI) and preferences for types of delivery (e.g. face to face or telephone/internet-based, mobile apps), and by whom (e.g. multidisciplinary team). By focusing future research in the recommended areas, improvements can be made in the understanding of how self-management strategies impact pain and depression for adults with SCI.
Disclaimer statements
Contributors None.
Funding This project was funded by a Connaught New Investigator Award (University of Toronto), Craig H. Neilsen Foundation (Psychosocial Research Pilot grant [#441259]), and the Graduate Department of Pharmaceutical Sciences (Undergraduate Summer Research Program and Dean’s Fund) at the Leslie Dan Faculty of Pharmacy, University of Toronto. Dr. Guilcher is supported by a Canadian Institutes for Health Research Embedded Clinician Scientist Salary Award on Transitions of Care (2016–2020).
Declaration of interest None.
Conflict of interest statement There are no conflicts of interest to report. The opinions, results and conclusions reported herein are those of the authors and are independent from the funding sources.
Acknowledgements
The authors would like to thank the University of Toronto librarians, especially Erica Lenton and Gail Nichol for their expertise and assistance with literature syntheses.
ORCID
Lauren Cadel http://orcid.org/0000-0001-6925-8163
Sander L. Hitzig http://orcid.org/0000-0002-9139-9250
Tanya L. Packer http://orcid.org/0000-0003-4831-7691
Aisha K. Lofters http://orcid.org/0000-0002-7322-0894
Tejal Patel http://orcid.org/0000-0003-3002-8306
Sara J. T. Guilcher http://orcid.org/0000-0002-9552-9139
References
- Fatehi D, Naleini F, Salehi M, Afshari D, Mirfendereski SAM, Farzizadeh M, et al. Traumatic spinal cord injury; theranostic applications of advanced MRI techniques. Biomed Pharmacol J 2015;8(2):891–903.
- Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003;26(sup1):S50–6.
- Crewe N, Krause J. Medical, Psychosocial and Vocational Aspects of Disability. 3 ed. 2009:282–300.
- World Health Organization. Spinal cord injury (Fact Sheet N°384) 2013. Available from http://www.who.int/mediacentre/factsheets/fs384/en/.
- SCI Ontario. What is an SCI? 2014. Available from https://sciontario.org/support-services/resources/living-with-an-sci/what-is-an-sci/.
- Tate DG, Forchheimer MB, Karana-Zebari D, Chiodo AE, Kendall Thomas JY. Depression and pain among inpatients with spinal cord injury and spinal cord disease: differences in symptoms and neurological function. Disabil Rehabil 2013;35(14):1204–12.
- Krause JS, Kemp B, Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil 2000;81(8):1099–109.
- Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000;81(7):932–7.
- Sezer N. Chronic complications of spinal cord injury. World J Orthop 2015;6(1):24–33.
- McKinley WO, Jackson AB, Cardenas DD, De Vivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999;80(11):1402–10.
- Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG. Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998;36(1):45–50.
- McKinley WO, Gittler MS, Kirshblum SC, Stiens SA, Groah SL. Spinal cord injury medicine. 2. Medical complications after spinal cord injury: identification and management. Arch Phys Med Rehabil 2002;83(3 Suppl 1):S58–64, S90–8.
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part I). Health Promot Pract 2005;6(1):37–43.
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA 2002;288(19):2469–75.
- Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 2002;48(2):177–87.
- Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26(1):1–7.
- National Guideline Centre UK. Multimorbidity: assessment, prioritisation and management of care for people with commonly occurring multimorbidity. National Institute for Health and Care Excellence 2016. p. 370–95.
- Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health 2014;104(8):e25–31.
- Bratzke LC, Muehrer RJ, Kehl KA, Lee KS, Ward EC, Kwekkeboom KL. Self-management priority setting and decision-making in adults with multimorbidity: a narrative review of literature. Int J Nurs Stud 2015;52(3):744–55.
- van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain 2015;19(1):5–14.
- Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain 2017;21:29–44.
- Boldt I, Eriks-Hoogland I, Brinkhof MWG, de Bie R, Joggi D, von Elm E. Non-pharmacological interventions for chronic pain in people with spinal cord injury. Cochrane Database Syst Rev 2014;11: CD009177.
- Putzke JD, Richards JS, Hicken BL, DeVivo MJ. Interference due to pain following spinal cord injury: important predictors and impact on quality of life. Pain 2002;100(3):231–42.
- Rick Hansen Institute. Facts about SCI Vancouver, BC2014. Available from http://www.rickhanseninstitute.org/resource/sci/what-is-sci.
- Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res 2016;9:457–67.
- Khazaeipour Z, Norouzi-Javidan A, Kaveh M, Khanzadeh Mehrabani F, Kazazi E, Emami-Razavi S-H. Psychosocial outcomes following spinal cord injury in Iran. J Spinal Cord Med 2014;37(3):338–45.
- Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain 1992;50(2):133–49.
- Harris RA. Chronic pain, social withdrawal, and depression. J Pain Res 2014;7:555–6.
- McCarberg BH, Nicholson BD, Todd KH, Palmer T, Penles L. The impact of pain on quality of life and the unmet needs of pain management: results from pain sufferers and physicians participating in an internet survey. Am J Ther 2008;15(4):312–20.
- Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil 2015;96:133–40.
- Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health 2013;34:119–38.
- Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil 2011;92(3):411–18.
- Aoki T, Hosaka T, Ishida A. Psychiatric evaluation of physical rehabilitation patients. Gen Hosp Psychiatry 1995;17(6):440–3.
- Wilson M, Finlay M, Orr M, Barbosa-Leiker C, Sherazi N, Roberts MLA, et al. Engagement in online pain self-management improves pain in adults on medication-assisted behavioral treatment for opioid use disorders. Addict Behav 2018;86:130–7.
- Damush TM, Kroenke K, Bair MJ, Wu J, Tu W, Krebs EE, et al. Pain self-management training increases self-efficacy, self-management behaviours and pain and depression outcomes. Eur J Pain 2016;20(7):1070–8.
- Meade MA, Trumpower B, Forchheimer M, DiPonio L. Development and feasibility of health mechanics: a self-management program for individuals with spinal cord injury. Top Spinal Cord Inj Rehabil 2016;22(2):121–34.
- Houlihan BV, Brody M, Everhart-Skeels S, Pernigotti D, Burnett S, Zazula J, et al. Randomized trial of a peer-led, telephone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management. Arch Phys Med Rehabil 2017;98(6):1067–76.e1.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19–32.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69–77.
- New PW, Delafosse V. What to call spinal cord damage not due to trauma? Implications for literature searching. J Spinal Cord Med 2012;35(2):89–95.
- Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016;104(3):240–3.
- Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 2014;5(4):371–85.
- Ogallo W, Kanter AS. Using natural language processing and network analysis to develop a conceptual framework for medication therapy management research. AMIA Annu Symp Proc 2016;2016:984–93.
- Norrbrink Budh C, Kowalski J, Lundeberg T. A comprehensive pain management programme comprising educational, cognitive and behavioural interventions for neuropathic pain following spinal cord injury. J Rehabil Med 2006;38(3):172–80.
- Molton IR, Jensen MP, Nielson W, Cardenas D, Ehde DM. A preliminary evaluation of the motivational model of pain self-management in persons with spinal cord injury-related pain. J Pain 2008;9(7):606–12.
- Buscemi V, Cassidy E, Kilbride C, Reynolds FA. A qualitative exploration of living with chronic neuropathic pain after spinal cord injury: an Italian perspective. Disabil Rehabil 2017;40(5):577–86.
- Norrbrink C, Lundeberg T. Acupuncture and massage therapy for neuropathic pain following spinal cord injury: an exploratory study. Acupunct Med 2011;29(2):108–15.
- Rodgers ML, Strode AD, Norell DM, Short RA, Dyck DG, Becker B. Adapting multiple-family group treatment for brain and spinal cord injury intervention development and preliminary outcomes. Am J Phys Med Rehabil 2007;86(6):482–92.
- Curtis K, Hitzig S, Leong N, Wicks C, Ditor D, Katz J. An evaluation of a modified yoga program for spinal cord injury. Ther Recreation J 2015;49 (2):97–117.
- Nawoczenski DA, Ritter-Soronen JM, Wilson CM, Howe BA, Ludewig PM. Clinical trial of exercise for shoulder pain in chronic spinal injury. Phys Ther 2006;86(12):1604–18.
- Perry KN, Nicholas MK, Middleton JW. Comparison of a pain management program with usual care in a pain management center for people with spinal cord injury-related chronic pain. Clin J Pain 2010;26(3):206–16.
- Stuntzner SM. Comparison of two self-study on-line interventions to promote psychological well-being in people with spinal cord injury: a forgiveness intervention and a coping effectively with spinal cord injury intervention. Diss Abstr Int 2008;68(8-B):5595–6011.
- Henwood P, Ellis J, Logan J, Dubouloz C-J, D'Eon J. Acceptance of chronic neuropathic pain in spinal cord injured persons: a qualitative approach. Pain Manag Nurs 2012;13(4):215–22.
- Kratz AL, Hirsh AT, Ehde DM, Jensen MP. Acceptance of pain in neurological disorders: associations with functioning and psychosocial well-being. Rehabil Psychol 2013;58(1):1–9.
- Smith R, Jones G, Murphy H, Curtis A, Flint G. Are established methods of physiotherapeutic management for long-term neurological conditions applicable to ‘orphan’ conditions such as syringomyelia? J Physiother 2015;101:eS1412–eS13.
- Löfgren M, Norrbrink C. “But I know what works” – patients’ experience of spinal cord injury neuropathic pain management. Disabil Rehabil 2012;34(25):2139–47.
- Henwood P, Ellis JA. Chronic neuropathic pain in spinal cord injury: the patient's perspective. Pain Res Manag 2004;9(1):39–45.
- Heutink M, Post MWM, Wollaars MM, Van Asbeck FWA. Chronic spinal cord injury pain: pharmacological and non-pharmacological treatments and treatment effectiveness. Disabil Rehabil 2011;33(5):433–40.
- Dorstyn D, Mathias J, Denson L, Robertson M. Effectiveness of telephone counseling in managing psychological outcomes after spinal cord injury: a preliminary study. Arch Phys Med Rehabil 2012;93(11):2100–08.
- Jensen MP, Barber J, Romano JM, Hanley MA, Raichle KA, Molton IR, et al. Effects of self-hypnosis training and EMG biofeedback relaxation training on chronic pain in persons with spinal-cord injury. Int J Clin Exp Hypn 2009;57(3):239–68.
- Curtis K, Hitzig SL, Bechsgaard G, Stoliker C, Alton C, Saunders N, et al. Evaluation of a specialized yoga program for persons with a spinal cord injury: a pilot randomized controlled trial. J Pain Res 2017;10:999–1017.
- Guest RS, Klose KJ, Needham-Shropshire BM, Jacobs PL. Evaluation of a training program for persons with SCI paraplegia using the Parasteprho1 ambulation system: part 4. Effect on physical self-concept and depression. Arch Phys Med Rehabil 1997;78(8):804–07.
- Burns AS, Delparte JJ, Ballantyne EC, Boschen KA. Evaluation of an interdisciplinary program for chronic pain after spinal cord injury. PM R 2013;5(10):832–8.
- Zsoldos A, Sátori Á, Zana Á. Impact of animal-assisted intervention on rehabilitation of patients with spinal cord injury. Orv Hetil 2014;155(39):1549–57.
- Hearn JH, Cotter I, Fine P, Finlay KA. Living with chronic neuropathic pain after spinal cord injury: an interpretative phenomenological analysis of community experience. Disabil Rehabil 2015;37(23):2203–11.
- Widerström-Noga E, Anderson KD, Perez S, Hunter JP, Martinez-Arizala A, Adcock JP, et al. Living with chronic pain after spinal cord injury: a mixed-methods study. Arch Phys Med Rehabil 2017;98(5):856–65.
- Heutink M, Post MW, Luthart P, Schuitemaker M, Slangen S, Sweers J, et al. Long-term outcomes of a multidisciplinary cognitive behavioural programme for coping with chronic neuropathic spinal cord injury pain. J Rehabil Med 2014;46(6):540–5.
- Widerström-Noga E, Felix ER, Adcock JP, Escalona M, Tibbett J. Multidimensional neuropathic pain phenotypes after spinal cord injury. J Neurotrauma 2016;33(5):482–92.
- Norrbrink C, Löfgren M. Needs and requests – patients and physicians voices about improving the management of spinal cord injury neuropathic pain. Disabil Rehabil 2016;38(2):151–8.
- Taylor J, Huelbes S, Albu S, Gómez-Soriano J, Peñacoba C, Poole HM. Neuropathic pain intensity, unpleasantness, coping strategies, and psychosocial factors after spinal cord injury: an exploratory longitudinal study during the first year. Pain Med 2012;13(11):1457–68.
- Norrbrink Budh C, Lundeberg T. Non-pharmacological pain-relieving therapies in individuals with spinal cord injury: a patient perspective. Complement Ther Med 2004;12(4):189–97.
- Wilson MW. Perceived stress, pain coping strategies, pain interference, and social support: mediators and moderators of depression in a spinal cord injury sample with chronic pain. Diss Abstr Int 2008;68(10-B):6988–7097.
- Dorstyn DS, Mathias JL, Denson LA. Psychological intervention during spinal rehabilitation: a preliminary study. Spinal Cord 2010;48(10):756–61.
- Molton IR, Stoelb BL, Jensen MP, Ehde DM, Raichle KA, Cardenas DD. Psychosocial factors and adjustment to chronic pain in spinal cord injury: replication and cross-validation. J Rehabil Res Dev 2009;46(1):31–42.
- Radwanski M. Self-medicating practices for managing chronic pain after spinal cord injury. Rehabil Nurs 1992;17(6):312–8.
- McCasland LD, Budiman-Mak E, Weaver FM, Adams E, Miskevics S. Shoulder pain in the traumatically injured spinal cord patient: evaluation of risk factors and function. J Clin Rheumatol 2006;12(4):179–86.
- Wollaars MM, Post MWM, Van Asbeck FWA, Brand N. Spinal cord injury pain: the influence of psychologic factors and impact on quality of life. Clin J Pain 2007;23(5):383–91.
- Phillips VL, Vesmarovich S, Hauber R, Wiggers E, Egner A. Telehealth: reaching out to newly injured spinal cord patients. Public Health Rep 2001;116(1):94–102.
- Heutink M, Post MWM, Bongers-Janssen HMH, Dijkstra CA, Snoek GJ, Spijkerman DCM, et al. The CONECSI trial: results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal cord injury. Pain 2012;153(1):120–8.
- Norrbrink C. Transcutaneous electrical nerve stimulation for treatment of spinal cord injury neuropathic pain. J Rehabil Res Dev 2009;46(1):85–93.
- Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med 2006;29(2):109–17.
- Widerström-Noga EG, Turk DC. Types and effectiveness of treatments used by people with chronic pain associated with spinal cord injuries: influence of pain and psychosocial characteristics. Spinal Cord 2003;41(11):600–9.
- Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord 1999;37(3):191–5.
- Martin Ginis KAM, Latimer AE, McKechnie K, Ditor DS, McCartney N, Hicks AL, et al. Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol 2003;48(3):157–64.
- Heutink M, Post MW, Overdulve CW, Pfennings LE, van de Vis W, Vrijens NL, et al. Which pain coping strategies and cognitions are associated with outcomes of a cognitive behavioral intervention for neuropathic pain after spinal cord injury? Top Spinal Cord Inj Rehabil 2013;19(4):330–40.
- Liddy C, Blazkho V, Mill K. Challenges of self-management when living with multiple chronic conditions: systematic review of the qualitative literature. Can Fam Physician 2014;60(12):1123–33.
- Kroenke K, Shen J, Oxman TE, Williams JW, Dietrich AJ. Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain 2008;134(1):209–15.
- Nakagawa R, Yamaguchi S, Kimura S, Sadamasu A, Yamamoto Y, Sato Y, et al. Association of anxiety and depression with pain and quality of life in patients with chronic foot and ankle diseases. Foot Ankle Int 2017;38(11):1192–8.
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163(20):2433–45.
- Hitzig SL, Campbell KA, McGillivray CF, Boschen KA, Craven BC. Understanding age effects associated with changes in secondary health conditions in a Canadian spinal cord injury cohort. Spinal Cord 2010;48(4):330–5.
- Noreau L, Proulx P, Gagnon L, Drolet M, Laramée M-T. Secondary impairments after spinal cord injury: a population-based study. Am J Phys Med Rehabil 2000;79(6):526–35.
- Wallace E, Salisbury C, Guthrie B, Lewis C, Fahey T, Smith SM. Managing patients with multimorbidity in primary care. Br Med J 2015;350:h176–81.
- Smith SM, Wallace E, O'Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;14(3):CD006560.
- O'Connor RJ, Murray PC. Review of spinal cord injuries in Ireland. Spinal Cord 2006;44(7):445–8.
- Derakhshanrad N, Vosoughi F, Yekaninejad MS, Moshayedi P, Saberi H. Functional impact of multidisciplinary outpatient program on patients with chronic complete spinal cord injury. Spinal Cord 2015;53(12):860–5.
- Alizo G, Sciarretta JD, Gibson S, Muertos K, Holmes S, Denittis F, et al. Multidisciplinary team approach to traumatic spinal cord injuries: a single institution's quality improvement project. Eur J Trauma Emerg Surg 2018;44(2):245–50.
- Dorstyn D, Mathias J, Denson L. Applications of telecounselling in spinal cord injury rehabilitation: a systematic review with effect sizes. Clin Rehabil 2013;27(12):1072–83.
- Moulin DE, Boulanger A, Clark AJ, Clarke H, Dao T, Finley GA, et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian pain society. Pain Res Manag 2014;19(6):328–35.
- Chang K-L, Fillingim R, Hurley RW, Schmidt S. Chronic pain management: nonpharmacological therapies for chronic pain. FP Essent 2015;432:21–6.
- McCaffery M. Nursing approaches to nonpharmacological pain control. Int J Nurs Stud 1990;27(1):1–5.
- Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Front Hum Neurosci 2014;8(141):1–11.
- Pieh C, Altmeppen J, Neumeier S, Loew T, Angerer M, Lahmann C. Gender differences in outcomes of a multimodal pain management program. Pain 2012;153(1):197–202.