Abstract
Background
Falls are a common and costly problem, with poor balance a significant contributor. Wobble boards are commonly used for balance enhancement. However, the efficacy of wobble board training is not well understood, particularly in the older adult.
Objectives
To appraise and synthesise literature pertaining to the effect of wobble board training on balance in older adults.
Methods
A systematic search of Medline, Scopus, EBSCO, CINAHL, Science Direct, and Google Scholar databases was conducted up to August 2020. Articles comparing balance before and after wobble board training were included and quality appraised using the modified Downs and Black checklist.
Results
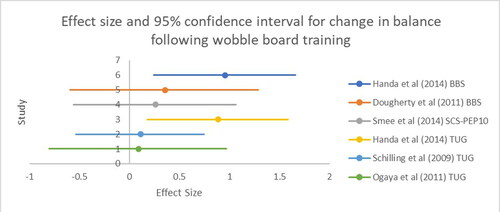
Six relevant studies (n = 129) were identified for review: four randomised-controlled-trials, one pilot-study and one repeated-measures design. The overall weighted average percentages, calculated from those studies where possible suggested an improvement in Berg Balance Scale (or similar) was 4.4% and for timed-up and go, 6.3%. Mean effect sizes ranged from 0.09 to 0.96. Overall, there is conflicting evidence to support wobble training for balance improvement in older adults. Magnitude of real change was often small questioning the impact of such small improvements on overall balance function. Effect sizes for balance enhancement through wobble board training were modest, with the largest effects on multi-modal balance outcome measures, such as the Berg Balance Scale. The results indicate that if wobble board programmes are simple and of a sufficient ‘within session’ duration, then some improvements in balance can be demonstrated within 3-weeks.
Conclusions
The evidence suggests conflicting results for the improvement of balance with wobble board training in older adults. Where effects were seen their magnitude was modest. Future studies should focus on determining the optimal wobble board programme to enhance balance.
Introduction
Falling is the second most common cause of accidental injurious death in adults over 65 years old [Citation1]. Thirty percent of this population fall at least once a year, increasing to 50% in the over 80 s [Citation2]. Associated injuries significantly impact quality of life, with the National Health Service spending around £2.3 billion annually on the treatment and management of falls in the United Kingdom alone [Citation2].
Postural balance refers to the ability to maintain the centre of a body’s mass within its base of support [Citation3]. The centre of mass (COM) represents the location where a body’s total mass acts to achieve balance [Citation4]. The maintenance of postural balance is vital to avoid slips, trips and falls, particularly in older adults. Training older adults to control their COM to rehabilitate and improve balance has been demonstrated to reduce falls risk [Citation5], and is a prevention strategy recommended by the American Geriatrics Society [Citation6]. Debate exists, however, as to how best to improve balance [Citation7], with many approaches relying on multi-modal exercise programmes over lengthy durations, typically resulting in poor completion and compliance rates [Citation8]. Scope, therefore, exists for improved, new and/or novel balance rehabilitation strategies.
Balance rehabilitation has long been considered an essential component of the Physiotherapist’s workload. Physiotherapists have adopted a range of techniques to assess and implement rehabilitation strategies for balance. One such technique is the utilisation of a wobble board, where a platform positioned on an unstable surface is used to challenge balance. Whilst wobble boards have been used effectively for injury prevention [Citation9], rehabilitation and balance enhancement [Citation10,Citation11], the mechanisms behind the efficacy of wobble board training are not well understood. Furthermore, these studies fail to integrate the older adult. Improvements in wobble board performance may be attributable to one or more of the following: muscle strengthening [Citation12], enhanced intersegmental coordination [Citation13], increase in brain activity in the supplementary motor area [Citation14] and/or enhanced feed-forward and feed-backward postural control mechanisms [Citation14]. To date, no systematic reviews explore the efficacy of wobble board training for enhancing balance performance in older adults. A contemporary synthesis is vital to the justification of wobble board intervention, the development of efficient rehabilitation strategies and selection of optimal training parameters.
This review will investigate wobble board intervention and training efficacy in older adults.
Material and methods
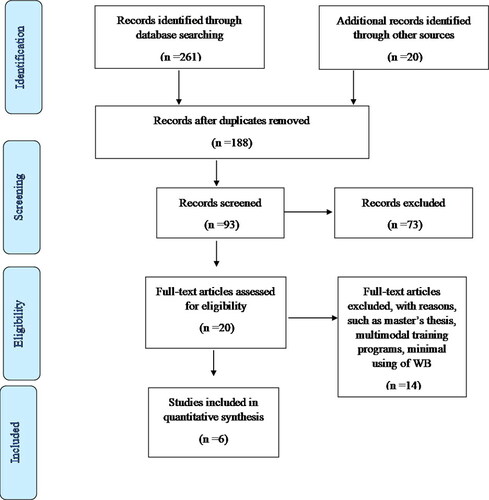
This review was conducted in accordance to the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). In addition, the PICO approach to question setting and data extraction was adopted.
Search strategy
A systematic literature search of electronic databases (Medline, Scopus, EBSCO, CINAHL, Science Direct, and Google Scholar) was conducted by two authors (MA and JW) in July 2020 using Boolean logic and the key terms listed in .
Table 1. Search terms using Boolean logic.
The search was limited to peer-reviewed journals and English language articles only, as no translational services were available. Reference lists were also screened for additional relevant articles. In total, 261 relevant articles were identified following duplicate removal. Titles and abstracts were screened for suitability, removing 241 as irrelevant to the research question. The remaining 20 articles were independently screened by two authors against pre-determined inclusion and exclusion criteria. Full details of the implemented search strategy are outlined in the PRISMA flow diagram (see ).
Inclusion and exclusion criteria
Only studies involving healthy older adults (aged 60 years old and above) were included in this review. Studies needed to clearly describe the wobble board training intervention and have at least one specific balance outcome measure. No a-priori decisions were made regarding inclusion or omission of balance outcome measure and all balance outcomes reported by the studies were included in this review. Multi-modal intervention studies were excluded, as were those investigating participants with any declared neurological, rheumatological, vestibular, vascular or musculoskeletal disorder likely to affect balance. Theses, conference proceedings and discussion pieces were also excluded. No studies were excluded based of methodological quality.
Quality index and data extraction
The selected studies were assessed for methodological quality using the modified Downs and Black checklist [Citation15], a robust and valid literature appraisal tool that can be applied to both randomised and non-randomised studies [Citation15]. The checklist was modified by replacing the final question’s scoring with a 1 or a 0, ensuring equal weighting as applied previously [Citation16,Citation17]. Two authors performed a blinded quality appraisal, with results compared and any discrepancies resolved by consensus. The quality index scores for the six reviewed papers are listed in . As the focus of this review was to determine the efficacy of wobble board training programmes as means to improve the balance of healthy older adults, data extraction highlighted wobble board design, duration of intervention and balance measurement utilised (see ).
Table 2. Methodological quality assessment results using a modified version of the Downs and Black appraisal tool [Citation15].
Table 3. Data extraction.
Synthesis
Quantitative synthesis was completed by effect size calculation (Cohen’s d) with 95% confidence intervals and forest plots, along with weighted averages to address differing balance outcome measures.
Results
Study selection and characteristics
The search strategy identified six relevant studies for review: four randomised controlled trials [Citation18–21], one pilot study [Citation22] and one repeated measures single-subject design [Citation23]. In total, the studies described 129 healthy older adults, aged 60 years old and above. The studies were performed in Australia, Canada, America, Japan, the Netherlands and India.
Interventions
The wobble board training comprised horizontal and lateral rocking, attempting to achieve and maintain a level wobble board, using the wobble board to follow an on-screen cursor, using the wobble board as an input into exercise-gaming or performing closed kinetic chain exercises (e.g. squats, lunges). A wobble board was used in all the studies with the exception of Dougherty et al. [Citation22], who used an IndoFLO balance board. This device contains a flat board on which the individual stands and an unstable base onto which the board is placed. The result is an unstable platform on which to train with a similar action to a standard wobble board, therefore, this was included in the current study. Wobble board training periods ranged from 3 to 16 weeks, with a mean of 8 weeks. Training frequency ranged from 3 to 4 sessions per week, with a mean of 3 sessions per week. Single training session durations ranged from 6 to 30 min, with a mean of 15 min.
Outcome measures
Various balance outcome measures were applied across the studies. The Berg Balance Scale (BBS) was used in two studies [Citation18, Citation23], Continuous Scale-Physical Functional Performance 10 (SCS-PEP10) [Citation21] and the Timed Up and Go test (TUG) in three studies [Citation18–20]. Postural sway was measured in two studies [Citation19,Citation20], including tasks ranging from single leg stance [Citation19,Citation20], tandem stance and double leg stance [Citation20].
Methodological quality
Independent assessment, performed using the Downs and Black quality appraisal checklist, scored all studies between 15 and 23. Whilst many studies shared common threats to validity, no studies were excluded due to poor methodological quality.
Overall, the studies demonstrated that wobble board training resulted in an improvement in at least one outcome measure relating to balance. However, as the effect was not distributed across all balance outcome measures, the collated results demonstrate conflicting evidence concerning whether or not wobble board training can improve balance in older adults [Citation24].
The overall weighted average percentages were calculated from those studies where data could be extracted and for those variables where more than one article reported the result. The weighted average percentage improvement in BBS (or similar) was 4.4% and for TUG, 6.3%. Effect sizes (ES) were calculated with mean ES ranging from 0.09 [Citation19] to 0.96 [Citation18], see forest plot ().
Discussion
This review is the first to assess wobble board training efficacy for rehabilitating balance in the older adult population. Despite wobble boards being widely used in numerous physical therapy environments, only six articles were identified that addressed this question. These articles shared common threats to validity. All studies failed to blind participants, which is important to minimise systematic effects of experimentation and limit the effects of participant bias. Such blinding is challenging in exercise-based studies, given that the intervention is normally fundamentally different to the control group, however, this mirrors current Physical Therapy practice and so these results remain highly relevant to clinicians. All studies also failed to blind the outcome assessors and therefore, may potentially threaten internal validity, since assessors may be biased towards an intervention, thereby inadvertently influencing the outcome. In these studies, many balance outcome assessments were computationally automated (e.g. force plate with standardised outputs), minimising the potential influence of assessor bias, therefore, these data remain clinically relevant.
The articles contained multiple outcome measures under the construct of balance and not all findings were universal. Four studies utilised a multi-dimensional balance outcome measure, i.e. the BBS, or the continuous-scale physical function performance test 10 (CS-PFP10) [Citation18, Citation21, Citation23]. A weighted average improvement of 4.4% was observed across those studies using this outcome measure and with a 0.61 weighted average effect size. This suggests an overall moderate effect of wobble board training on BBS (or similar). Wobble board training demonstrated improvements in balance between 1.6% [Citation22] and 6.3% [Citation21], however, the multi-dimensional nature of these outcome measures and the lack of detailed reporting, prevents identifying the improved element/s. The minimal clinically important difference in healthy older adults has not been established, however ranged from 5% in people with multiple sclerosis [Citation25] to 21% in older adults recovering from hip fracture [Citation26].
Two studies utilised the Timed Up and Go tests (TUG) as an outcome measure, reporting no significant difference after wobble board training [Citation19,Citation20]. Despite this, wobble board training resulted in a weighted average improvement of 6.3% and a 0.40 weighted effect size. The initial and spread of values are interesting across the two papers, since participants recruited by Schilling et al. [Citation20] had a mean baseline TUG time of 5.6 s. This would place them in the top 5th percentile of TUG performance [Citation27], allowing little room for improvement, regardless of intervention. Furthermore, the standard deviation for TUG time, as reported by Ogaya et al. [Citation19] (13.6 s on a mean of 14.7 s) suggests high variability across the recruited participants. It is unclear how or whether, outliers were identified or managed, however, this variability is likely to negatively influence the ability to detect significant differences. Only Handa et al. [Citation18] produced a significant improvement in TUG, with a real change of 1.7 s across a sample of healthy older adults. This could represent an important clinical change, given for example, that 1.4 s represents a clinically important difference in older adults with hip osteoarthritis [Citation28].
Wobble board training is reported to positively influence the BBS and TUG balance outcome measures, however, the magnitude of change of BBS was small with the largest post-training change being three points. As the minimal detectable change has been suggested in the BBS at four points [Citation22], it is unclear whether these changes were beyond the natural variation expected with repeated testing. Additionally, as these scales subjectively assess performance of daily physical functions (e.g. transferring from bed to chair), assessor bias may have influenced scoring success.
Furthermore, it remains unclear if and how wobble board training influenced the static or dynamic balance components of BBS. Such small improvements may also be due to a ceiling effect, whereby baseline scores are close to the maximum value, leaving no opportunity to demonstrate balance improvement. The baseline scores for BBS range from 49 to 53, thus, these individuals already had scores close to the maximum of 56.
The reasoning behind the contrast in findings between the TUG and BBS is not immediately apparent. There are several similarities between the BBS and the TUG, namely the components such as sit to stand, turning etc. Two of the three studies using the TUG did not identify a statistically significant effect, but this may be due to measuring a fundamentally different functional construct. The TUG test measures the duration of time for completing linked tasks, whilst the BBS measures quality subjectively. Twenty-two percent of TUG variability can be explained by BBS performance, however, 78% is not explained, suggesting these are largely independent balance measures [Citation29]. This supports the concept of different underlying constructs, suggesting that wobble board training may not develop universal improvement in all balance constructs.
The similar outcomes of two studies suggest wobble board training does not improve postural sway [Citation19, Citation23]. Ogaya et al. [Citation19] utilised bilateral stance, calculating root mean square area and single leg stance duration, with both metrics failing to demonstrate a significant difference post-training. Similar findings regarding lack of effect, were also reported for tandem stance and single leg stance duration [Citation23]. These findings suggest that wobble board training has little or no influence on these postural sway tests. Therefore, it seems possible that wobble board training does not target those specific physiological constructs that determine postural sway performance. Tests such as these have been described as static balance tests, in which the challenge is the ability to remain ‘relatively’ still, while responding to an intrinsically derived postural challenge [Citation30]. This contrasts with the wobble board’s externally driven perturbation, therefore, perhaps the conflict in training specificity can explain the lack of effect of wobble board training on postural sway.
In summary, balance, post- wobble board training, is likely to be significantly improved when analysed via multi-modal assessment (e.g. BBS), however, it remains unclear whether enhancement extends beyond natural variability. A moderate effect size can be expected for change in BBS following wobble board training and a small effect size for change in TUG from wobble board training. Postural sway appears to be unaffected by wobble board training.
All the wobble board training programmes involved the completion of prescribed exercises over a duration of between 6 and 30 min, 2 − 3 times per week. It is noteworthy, however, that no evidence was presented to justify the selection of these parameters. This may reflect a wider lack of evidence across the literature for optimal wobble board or balance training regimens. The American College of Sports Medicine [Citation31] often provides positional statements related to optimal training programme design based on evidence synthesis, however they fail to offer detailed guidelines for balance exercise prescription beyond only basic principles. Based on the findings of this review, it appears greater effect sizes were demonstrable from studies using session durations up to 30 min, the ceiling included for this review. Thirty minutes of wobble board training in a single session would significantly challenge a number of mechanisms that could affect balance. Neuromuscular adaptation is likely to be affected by wobble board training. Previous studies have provided evidence for this with improvements in proprioception [Citation32] and improved latency times following wobble board training [Citation33]. Furthermore, it has been demonstrated that wobble board training results in significant improvements in lower limb muscle strength [Citation12], however, the largest effect sizes seem to relate to shorter programmes [Citation18, Citation22]. Such short training stimuli are associated with neuromuscular changes rather than muscle hypertrophy [Citation12, Citation34]. Additionally, improvement after unstable training is due to enhanced foot proprioception and muscle mechanoreceptors [Citation35], as well as other components of the somatosensory system, such as joint receptors, ligaments and tendons [Citation35].
Wobble board training duration is not necessarily a good indicator of training intensity (the energy expended, etc.), and measuring this variable may undermine attempted correlations with balance rehabilitation. The greatest effect size was reported by Handa et al. [Citation18], investigating the relatively simple tasks of side-to-side and forward-backwards rocking, and cursor matching tasks. Similar programmes, however, reported only modest effect sizes. The most complex programme included wobble board -based squats, lunges and reaching tasks, though achieved only a very small effect (e.g. Schilling et al. [Citation20]). It is possible that this effect occurred due to focus, or attention. Previous research has demonstrated superior performance when an individual focusses or attends to the outcome of one’s actions, rather than the specific inputs (movements) [Citation36]. Therefore, if an individual focusses on performing additional tasks whilst on the wobble board, such as squats, lunges etc., this could then serve to distract the focus from controlling the tilt of the wobble board, and lead to poor wobble board performance reducing balance enhancement. Therefore, it appears a high degree of complexity is not warranted when the objective is improving balance as measured in the studies included in this review. It is possible that the requirement to focus on maintaining the board level and controlling the degree of tilt, either through specific verbal commands or by following a cursor on a screen, affords sufficient stimulus to improve balance.
Wobble board training efficacy may also be influenced by additional factors, for example a fear of falling may affect wobble board performance. Performance tasks, including those in BBS and TUG are affected by a fear of falling, possibly explaining 36 − 94% of the variance of BBS performance [Citation37,Citation38] and up to 90% of the variance in TUG performance [Citation38]. Fear of falling among the elderly can lead them to reduce their activity and alter their gait, as noted in the balance assessments that examined activity and gait such as BBS and TUG [Citation38]. An individual with fear of falling demonstrates reduced speed to complete tasks, potentially as a mechanism to enhance their safety and reduce the risk of falling. Rapidly moving one’s centre of mass will potentially tax the balance system's equilibrium to a greater extent and require a more rapid and larger muscle response to maintain balance. Therefore, individuals with a more exaggerated fear of falling often complete tasks more slowly. Only two studies investigated the effect of wobble board training on balance confidence, as measured via the Activities Specific Balance Confidence questionnaire, with conflicting results. Dougherty et al. [Citation22] failed to demonstrate any significant changes or report actual values. Schilling et al. [Citation20] demonstrated a small improvement with a magnitude of just 3.8 points (4%), which is questionable when compared to the minimal detectable change equal to 15 [Citation39]. If fear is part of the explanatory mechanism informing the effect of older adult wobble board training, such as wobble board training reducing fear of falling, then future investigations should consider exercise prescriptions that target fear of falling.
In summary, this review has highlighted the role of wobble board training programmes in providing simple tasks to enhance multi-modal balance outcome measures. Focus and attention on wobble board tilt should be encouraged, and training session durations extending to 30 min, 2–3 times per week for at least 3 weeks.
This work is limited by including only studies written in English, raising the potential for selection bias. Only a small number of studies were included and offered only small sample sizes, reducing the impact of synthesis and minimising the generalisability. Furthermore, this study was confined to investigating healthy older adults only.
Conclusion
This review overall demonstrates conflicting evidence in support of wobble board training for balance enhancement. When effective, wobble board training demonstrated modest effect sizes for balance enhancement, with the largest effects on multi-modal balance outcome measures, such as BBS. Consensus from the literature on optimal prescription of wobble board activities is lacking and future studies should focus on targeting specific interventional manipulations to more fully understand optimal prescriptions.
Acknowledgements
The first author gratefully acknowledges the Princess Nourah Bint Abdulrahman University for funding her PhD programme at Cardiff University and Eleanor Daniel for her helpful comments on an earlier draft of this manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Madawi A. ALJawaee
Madawi ALJawaee is a Physiotherapy Lecturer at Princess Nourah bint Abdulrahman, Riyadh, Saudi Arabia. She holds a professional fellowship in teaching and learning from Advance Higher Educational academy in UK and is currently a PhD student within the School of Engineering, Cardiff University, UK.
Michael D. Jones
Dr Mike Jones has a keen interest in applying engineering principles to the investigation of the causation of injury. This extends to penetrative wounding and blunt force trauma, falls, playground accidents, sports related head injuries, sub concussive brain injuries, non-accidental injuries; including vehicular impacts, short fall impacts and inertial injuries, such as those believed to be a result of shaking. He is a consultant to several UK's government agencies and routinely advises multi agency investigations on the biomechanical engineering aspects of murder, assault, accident and suicide.
Peter S. Theobald
Dr Peter Theobald is a Biomechanical Engineer with an interest in quantifying human movement. His other works include capturing spinal movement and estimating head/brain kinematics, typically within a sports and exercise environment.
Jonathan M. Williams
Dr Jonathan Williams is a Principal Academic in Physiotherapy with a strong interest in Biomechanics. His research focusses on real world instrumentation of human movement within sporting and clinical practice.
References
- Wang X, Ellul J, Azzopardi G. Elderly fall detection systems: a literature survey. Front Robot Ai. 2020;7(71):71–23.
- National Institute for Health and Care Excellence (NICE). Falls in older people: assessing risk and prevention [internet]. London: NICE; 2013. NICE guideline CG161. [cited 2020 Oct 10]. Available from: https://www.nice.org.uk/guidance/cg161/chapter/Introduction.
- Gosine P, Komisar V, Novak AC. A kinematic analysis of balance recovery following an unexpected forward balance loss during stair descent. Appl Ergon. 2021;92:1–9.
- Erdmann W. Center of mass of the human body helps in analysis of balance and movement. Appl Bionics Biomech. 2018;2(2):144–148.
- Melzer I, Benjuya N, Kaplanski J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing. 2004;33(6):602–607.
- Health in aging organsiation [internet]. New York: American Geriatrics Society: Geriatrics healthcare professionals; 2020. [cited 2020 Oct 7]. Available from: https://www.healthinaging.org/a-z-topic/falls-prevention/causes
- Lesinski M, Hortobágyi T, Muehlbauer T, et al. Effects of balance training on balance performance in healthy older adults: a systematic review and Meta-analysis. Sports Med. 2015;45(12):1721–1738.
- Kohler A, Kressig RW, Schindler C, et al. [Adherence rate in intervention programs for the promotion of physical activity in older adults: a systematic literature review]. Praxis (Bern 1994). 2012;101(24):1535–1547.
- Emery CA, van den Berg C, Richmond SA, et al. Implementing a junior high school-based programme to reduce sports injuries through neuromuscular training (iSPRINT): a cluster randomised controlled trial (RCT). Br J Sports Med. 2020;54(15):913–919.
- Fusco A, Giancotti GF, Fuchs PX, et al. Wobble board balance assessment in subjects with chronic ankle instability. Gait Posture. 2019;68:352–356.
- Williams J, Bentman S. An investigation into the reliability and variability of wobble board performance in a healthy population using the SMART wobble instrumented wobble board. Phys Ther Sport. 2014;15(3):143–147.
- Balogun JA, Adesinasi C, Marzouk D. Effects of wobble board exercise training program on static balance performance and strength of lower extremity muscles. Physiother Can. 1992;44(4):23–30.
- Urs G, Gruber M, Gollhofer A. Effects of sensorimotor training on postural control in older men. Dtsch Z Sportmed. 2009;60(21):387–393.
- Thomas E, Battaglia G, Patti A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Medicine (Baltimore). 2019;98(27):e16218.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- Cooper T, Williams J. Does an exercise programme integrating the nintendo Wii-Fit balance board improve balance in ambulatory children with cerebral palsy? Phys Ther Rev. 2017;22(5-6):229–237.
- Lien-Iversen T, Morgan DB, Jensen C, et al. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? A systematic review and meta-analysis. Br J Sports Med. 2020;54(10):592–598.
- Hande DK, Parab KN, Subhash K. Effectiveness of progressive stepping program on balance performance in geriatrics: a randomised controlled trial. Rom J Physical Ther. 2014;20(33):51–59.
- Ogaya S, Ikezoe T, Soda N, et al. Effects of balance training using wobble boards in the elderly. J Strength Cond Res. 2011;25(9):2616–2622.
- Schilling BK, Falvo MJ, Karlage RE, et al. Effects of unstable surface training on measures of balance in older adults. J Strength Cond Res. 2009;23(4):1211–1216.
- Smee DJ, Berry HL, Waddington GS, et al. A balance-specific exercise intervention improves falls risk but not total physical functionality in community-dwelling older adults. Phys Occup Ther Geriatr. 2014;32(4):310–320.
- Dougherty J, Kancel A, Ramar C, et al. The effects of a multi-axis balance board intervention program in an elderly population. Mo Med. 2011;108(2):128–132.
- Kosse NM, Caljouw SR, Vuijk PJ, et al. Exergaming: interactive balance training in healthy community-dwelling older adults. J Cyber Ther Rehabil. 2011;4(3):399–407.
- van Tulder M, Furlan A, Bombardier C, Editorial Board of the Cochrane Collaboration Back Review Group, et al. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–1299.
- Gervasoni E, Jonsdottir J, Montesano A, et al. Minimal clinically important difference of berg balance scale in people with multiple sclerosis. Arch Phys Med Rehabil. 2017;98(2):337–340.e2.
- Tamura S, Miyata K, Kobayashi S, et al. Minimal clinically important difference of the berg balance scale score in older adults with hip fractures. Disabil Rehabil. 2021;19:1–6.
- Pondal M, Delser T. Normative data and determinants for the timed “up and go” test in a population-based sample of elderly individuals without gait disturbances. J Geriatr Phys Ther. 2008;31(2):57–63.
- Wright AA, Cook CE, Baxter GD, et al. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41(5):319–327.
- Bennie S, Bruner K, Dizon A, et al. Measurements of balance: comparison of the timed "up and go" test and functional reach rest with the berg balance scale. J Phys Ther Sci. 2003;15(2):93–97.
- Haines T, Kuys SS, Morrison G, et al. Development and validation of the balance outcome measure for elder rehabilitation. Arch Phys Med Rehabil. 2007;88(12):1614–1621.
- Riebe D, Ej Liguori G, and, Magal M. American college of sports medicine, ACSM's guidelines for exercise testing and prescription. 10th ed. Philadelphia (PA): Wolters Kluwer; 2018.
- Waddington G, Adams R. The effect of a 5-week wobble-board exercise intervention on ability to discriminate different degrees of ankle inversion, barefoot and wearing shoes: a study in healthy elderly. J Am Geriatr Soc. 2004;52(4):573–576.
- Akhbari B, Ebrahimi T, Salavati M, et al. A 4-week biodex stability exercise program improved ankle musculature onset, peak latency and balance measures in functionally unstable ankles. Phys Ther Sport. 2007;8(3):117–129.
- Schoenfeld B. The mechanisms of muscle hypertrophy and their application to resistance training. J Strength Cond Res. 2010;24(10):2857–2872.
- Mohammadian Z, Rajabi R, Minoonejad H, et al. Effect of a 6-week balance training program with shuttle balance on balance, gait speed, and fear of falling in elderlies. EHJ. 2019;5(2):72–78.
- Lohse KR, Sherwood DE, Healy AF. How changing the focus of attention affects performance, kinematics, and electromyography in dart throwing. Hum Mov Sci. 2010;29(4):542–555.
- McAuley E, Mihalko SL, Rosengren K. Self-efficacy and balance correlates of fear of falling in the elderly. J Aging Phys Act. 1997;5(4):329–340.
- Kumar SVV, Awasthi S, Tiwari M, et al. Relationship between fear of falling, balance impairment and functional mobility in community dwelling elderly. IJPMR. 2008;19(2):48–52.
- Wang Y-C, Sindhu B, Lehman L, et al. Rasch analysis of the Activities-Specific balance confidence scale in older adults seeking outpatient rehabilitation services. J Orthop Sports Phys Ther. 2018;48(7):574–583.