Abstract
Background
Millions of patients receive medications in the Emergency Medical Services (EMS) setting annually, and dosing safety is critically important. The need for weight-based dosing in pediatric patients and variability in medication concentrations available in the EMS setting may require EMS providers to perform complex calculations to derive the appropriate dose to deliver. These factors can significantly increase the risk for harm when dose calculations are inaccurate or incorrect.
Methods
We conducted a scoping review of the EMS, interfacility transport and emergency medicine literature regarding pediatric medication dosing safety. A priori, the authors identified four research topics: (1) what are the greatest safety threats that result in significant dosing errors that potentially result in harm to patients, (2) what practices or technologies are known to enhance dosing safety, (3) can data from other settings be extrapolated to the EMS environment to inform dosing safety, and (4) what impact could standardization of medication formularies have on enhancing dosing safety. To address these topics, 17 PICO (Patient, Intervention, Comparison, Outcome) questions were developed and a literature search was performed.
Results
After applying exclusion criteria, 70 articles were reviewed. The methods for the investigation, findings from these articles and how they inform EMS medication dosing safety are summarized here. This review yielded 11 recommendations to improve safety of medication delivery in the EMS setting.
Conclusion
These recommendations are summarized in the National Association of EMS Physicians® position statement: Medication Dosing Safety for Pediatric Patients in Emergency Medical Services.
NAEMSP Position Statement, Approved by the Board on July 1st, 2020
Inaccurate dosing of medications given to children receiving medical care is a known and frequent issue. Errors can include acts of commission and omission. Root causes of dosing errors are multifactorial and include provider inexperience, performing complex calculations in a stressful environment, and infrequent exposure to pediatric patients. These risks are known to exist across all phases of emergency care but may be magnified in the EMS setting. To mitigate the risk of medication dosing errors in pediatric encounters occurring in the EMS setting, the National Association of EMS Physicians endorses the following statements:
Performing mathematical dosing calculations at the bedside is an area at very high risk for error. EMS agencies and providers should utilize dose-derivation strategies that avoid use of calculations at the patient side (GRADE Moderate).
Tools that provide pre-calculated weight-based dosing and preclude the need for calculation by EMS providers can reduce dosing errors. Such tools should:
be approved by the local medical director to ensure concordance with the agency’s protocols and with the local agency’s usual and customary concentrations of medications in their supply.
be achieved through a standardized formulary which allows for pre-calculation of all drug dosing for children and adults.
report doses in volumetric units (mL) of medications in the concentration available in the agency formulary rather than mass-based units (mg, mcg).
be provided in preprinted or electronic formats that are immediately accessible at the point of care.
be able to be modified in a timely and system-wide manner when drug shortages force product substitutions
Kilograms should be the standard unit of weight used in the EMS setting (GRADE Moderate).
Pediatric patient weight should only be measured and/or recorded in EMS patient care records using kilograms. Electronic documentation platforms should default to automatic conversion of pounds to kilograms.
Where pediatric weights are previously expressed or reported in units other than kilograms, conversion templates, electronic patient care record platforms, or other pre-calculated tools should be utilized to convert units from pounds to kilograms.
Unaided conversions from pounds to kilograms by the paramedic in the field should be avoided.
Pediatric patient weight should be confirmed at the time care is delivered (GRADE Low).
Weight should not be visually estimated.
Weight may be estimated by asking a parent the child’s weight, using a validated weight-estimation tool based on a child’s length, preferentially, or by age (the least accurate method).
Weight-based dosing requires both cognitive and psychomotor skills that decline with infrequent use (GRADE Low).
Efforts should be made to increase opportunities for EMS providers to practice and perform pediatric weight-based-dosing using scenario-based simulation training and through increased supervised clinical exposure where available. Simulation should include the use of the same weight estimation tool and dosing aid that will be used clinically.
Engineering controls for human factors should be implemented in the labeling, packaging, and storage of medications and medication delivery sundries kept in stock, in both medical bags and on-board EMS vehicles (GRADE Very Low).
Whenever possible and feasible, EMS agencies should consider having a standardized formulary and avoid stocking multiple concentrations of a particular drug in their usual and customary supply.
EMS agencies should consider the use of infusion pumps for the delivery of infused medications. Infusion pumps have been shown to be associated with faster achievement of therapeutic medication blood concentration and faster therapeutic effect than buretrols.
There is insufficient evidence to either support or refute the practice of independent double checking for the administration of medicines by EMS providers
Medical directors should be aware of factors in the EMS setting that increase the likelihood of an error in weight estimation and dose calculation (GRADE Moderate):
There is a higher risk of weight estimation error among patients that are less than 10 years old.
Weight estimation errors are more frequent during encounters where the patient is being resuscitated, receiving an analgesic, or having a seizure.
Drug shortages increase the risk for medication dosing errors, as they force EMS agencies to stock drugs in different concentrations, volumes, labeling, or packaging than their usual and customary supply.
Medication Dosing Safety for Pediatric Patients: Recognizing Gaps, Safety Threats, and Best Practices in the Emergency Medical Services Setting. A Position Statement and Resource Document from NAEMSP Resource Document
Introduction
Approximately 10% of all Emergency Medical Services (EMS) patients are pediatric patients (Citation1,Citation2). However, few pediatric EMS patients receive medications in this setting (Citation3). Pediatric medication dosing is weight-based, potentially requiring complex dosing calculations. Infrequent pediatric encounters, combined with the need to determine the correct dose, and the potential for cognitive and emotional stress during EMS care of severely injured or ill pediatric patients can increase the risk for dosing errors (Citation4–6). Even in the relatively controlled inpatient environment, medication errors are known to be more common in pediatric patients (Citation7). Reports indicate that as many as 37% of pediatric patients administered a medication in the EMS setting have received an inaccurate dose, though it is not clear how many of those inaccurate doses have resulted in harm (Citation8,Citation9).
To address the high risk of medication dosing errors in pediatric patients, it is imperative to understand the evidence and develop guidelines and recommendations to mitigate this problem. To this effort, the authors identified several key concepts which are presented and discussed in this resource document. These concept areas include:
What is known about enhancing dosing safety for patients in the EMS setting?
What are the greatest latent and active safety threats to pediatric medication dosing?
Can dosing safety education and strategies from other settings, (e.g., the emergency department, operating room, inpatient units, and intensive care units) be adapted to the EMS setting?
What is known about the role of standardized formularies in dosing safety? Are standardized formularies and pre-calculation of doses effective methods for decreasing errors? Are drug shortages and concerns for medical director autonomy barriers to standardization of formularies?
Methods
PICO Questions
To address the key concept areas above, the following 17 Population-Intervention-Control-Outcome (Citation10) (PICO) Questions were iteratively developed by the investigators for this scoping review. For the purposes of this study, we defined the term “pediatric patient” to include infants, toddlers, school-age children, and adolescents. The Key concept areas are included here, and the complete PICO questions are available as supplemental material.
Key concept area #1: What is known about enhancing dosing safety for patients in the EMS setting?
Key concept area #2: What are the greatest latent and active safety threats to medication dosing?
Key concept area #3: Can dosing safety education and strategies from other settings, (e.g., the emergency department, operating room, inpatient units, and intensive care units) be adapted to the EMS setting?
Key concept area #4: What is known about the role of standardized formularies in dosing safety? Is a standardized formulary protocol a means for precalculation of doses and decreasing errors? Are drug shortages and concerns for medical director autonomy barriers to standardization of formularies?
Search Strategy
Two reviewers performed a solo literature search for each PICO question. MesH search terms were derived from the Intervention and Control items in the PICO questions outlined above and included articles that were relevant to dosing safety in the EMS setting and/or pediatric dosing safety in other settings. When there were neither relevant pediatric or EMS studies, adult studies from hospital settings were sought. Each primary reviewer identified relevant abstracts in the PubMed database; PubMed was the sole database used to conduct the review. Additional sources were sought via web searches with Google Scholar, and by hand searching from the citations in reviewed articles. Inclusion criteria included clinical trials, observational studies, systematic reviews and case reports written in English. Exclusion criteria included non-peer reviewed literature, and articles written in languages other than English. Each pair of reviewers performed the literature review from July 17 to August 18, 2018. Supplementary literature search and review was performed August 15–22, 2019.
Literature Review Process
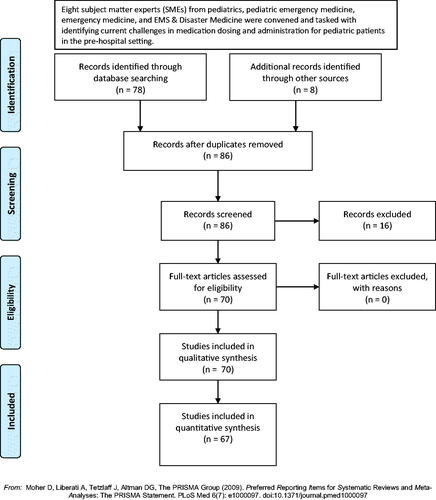
For each PICO question, two investigators independently reviewed the literature to address each question and grade the quality of the evidence. The review process is depicted in , a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement (Citation11). Reviewers then shared the relevant abstracts with their co-reviewer.
In the second phase of the review process, the two reviewers examined the abstracts provided by their co-reviewer and determined whether the abstract fit the PICO question being assessed. When both reviewers agreed that an abstract was relevant, the corresponding manuscript was evaluated in the third phase of the review process. When the reviewers disagreed, there was a discussion about the abstract, and the two reviewers attempted to reach consensus. If consensus could not be reached a predesignated referee was consulted to render a judgment. Abstracts found to be relevant to more than one PICO question were evaluated with the data abstraction for each relevant PICO question.
Data Abstraction
During the review process, each PICO question reviewer abstracted each study’s methods, objective findings (if any), subjective findings (if any), biases, and limitations. The reviewer then assigned a strength of the evidence using a standardized rubric (). The strength of the evidence was determined using a rubric provided by the NAEMSP Board of Directors and the Standards and Practice Committee when the Situation-Background-Assessment-Recommendation document proposing this work was accepted. Reviewers abstracted data from articles of all five levels of evidence.
Table 1. Rubric for assigning levels of evidence
After abstracting data from each manuscript for the PICO question at hand, the co-reviewers exchanged the data from their reviews. If discrepancies occurred in the conclusions drawn from the literature review, the primary reviewers worked to reach consensus when possible. In cases where consensus could not be reached, the predesignated referee was consulted to render a judgment. The findings of the two reviewers were then combined, in tabular form, representing a consensus abstraction of each manuscript. The consensus abstractions were assembled into tables for each PICO question. The findings from this third phase of the evaluation are the primary outcome of this scoping review.
Data Summarization
Data abstraction tables were submitted to the lead investigator, who considered the relevance of each abstract to the study questions. Evaluation consisted of the study populations, including types of providers determining medication doses and the population of pediatric patient being treated; the strength of the evidence; biases; methodological strength; and the effect of interventions on dosing safety. The data summarization was used to draft evidence-based recommendations for pediatric EMS medication dosing safety. It should be noted that articles with Level V evidence were not included in determining the evidence-based recommendations. Each position in the position statement was graded High, Medium, Low, or Very Low according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (Citation12).
Results
The working group evaluated 86 articles and identified 70 articles about pediatric dosing safety relevant to EMS practice. Abstracted data from the articles, with summaries of methods and findings, can be found in the Appendix. There were no Evidence Level I Articles, 27 Level II articles, 26 Level III articles, 14 Level IV articles, and 3 Level V articles. An overarching theme in the literature review was a lack of EMS research pertinent to medication safety, and that data from hospital-based studies required extrapolation for use in EMS practice.
Discussion
Key concept area #1: What is known about enhancing dosing safety in the EMS setting?
There is moderately strong evidence to support the use of preprinted dosing cards for the care of pediatric patients in the EMS setting. Expert opinion (Citation13) and peer reviewed research by Bernius et al. (Citation14), Kaji et al. (Citation15), and Hoyle et al. (Citation9) have suggested that preprinted dosing cards decrease the cognitive load on EMS providers when performing pediatric medication dosing. Studies conducted in the hospital setting have shown dosing cards promote cognitive unloading and reduce errors (Citation16). However other studies have shown there is variation in dosing accuracy based on what dosing card system providers use (Citation17,Citation18). Rappaport et al used a simulation-based setting to compare a tape-based preprinted dosing system that provided pre-calculated drug doses given in volumetric units to a tape-based preprinted dosing system that required paramedics to calculate actual doses and found that the pre-calculated tape system performed better with regard to reductions in cognitive errors, improved dosing accuracy, and shortened time to drug administration (Citation18).
With the ubiquity of smart phones and tablet devices, electronic dosing tools are an important aid to the EMS care of pediatric patients. As medical directors consider these programs, ensuring that there was medical oversight of dosing app development is key (Citation19). Single-site randomized controlled trials (RCTs) have demonstrated that dosing apps improve the accuracy of medication dosing during simulated resuscitations in the emergency department (Citation20) and the EMS setting (Citation21). Another RCT, conducted for burn patients, provided a three-way comparison between a novel pediatric dosing app, a paperboard dosing wheel, and a conventional dosing calculations (Citation22). In this study, the app and the wheel both provided quicker, more accurate dosing than conventional calculations. Finally, a digital weight calculation app accounting for patient gender and body habitus yields more accurate weight estimates than length-based tapes (Citation23).
Weight estimates are a barrier to accurate dosing in the EMS setting. Paramedics report their discomfort in estimating pediatric weights and medication doses (Citation4,Citation6) and as many as 20% of pediatric patients have an inaccurate weight estimate in the out-of-hospital setting (Citation6,Citation24). EMS dispatchers demonstrate some degree of accuracy in obtaining information about patient weights in pounds from parents during 911 calls (Citation25). An estimated weight given to EMS providers prior to arrival on scene can assist in pre-arrival planning and may mitigate dosing errors. A simulation-based study showed a hybrid model in which pediatric dosing was done in both pounds and kilograms reduced medication dosing errors when a dosing aid was used (Citation26).
This scoping review examined the utility of stretcher scales for improving dosing safety. A single study by Sinha et al. demonstrated that use of the Broselow-Luten Tape resulted in mean difference of 2.6 kg in the estimation of weight when compared to the weight obtained with a stretcher scale (Citation27). However, this study was limited by a small sample size, and larger pediatric patients (for whom a 2.6 kg difference between estimated and measured weight would be less clinically significant) were over-represented in the sample, making the results of this study difficult to apply to younger and smaller pediatric patients.
There is some evidence to support the use of a standardized dose (e.g. a single dose indicated for a range of weights) to enhance dosing safety in the EMS setting. The aforementioned study by Kaji et al. (Citation15) showed that, along with changing from endotracheal or intravenous epinephrine dosing with two available concentrations of epinephrine to one concentration of epinephrine via the intravenous route only, pre-calculated epinephrine dosing tools decreased dosing errors by roughly one third. In the hospital setting, simplifying gentamicin dosing with a standardized chart decreased errors by 20% (Citation28). In another study evaluating the Broselow-Luten Tape, implementation of a single, fixed medication dose for a range of patient weights was shown to decrease medication errors during simulated pediatric resuscitations by 25% (Citation16).
The standard of dosing in the care of pediatric patients is based on the patient’s weight in kilograms, with both the Emergency Nurses Association and the American Academy of Pediatrics endorsing this practice (Citation29). The National Association of State EMS Officials EMS Compass project explicitly states pediatric weights should be recorded in kilograms only (Citation30). There is a latent safety threat in kilogram-based dosing, however. Shaw et al. showed that in a hospital setting, 12% of wrong dose errors were due to errors in converting weight in pounds to weight in kilograms (Citation31). A study of pediatric patients treated by EMS providers showed a 35% incidence of dosing errors, even when the patient weight was recorded in kilograms (Citation8). Contrary to patient weights in kilograms, weights recorded in pounds are more familiar to paramedics practicing in the United States, and in focus groups paramedics expressed concerns about the potential for error when they convert pounds to kilograms (Citation5).
Pediatric patients of the same age vary in weight and height, causing strategies to standardize medication doses by pediatric patient age to have mixed results. A 2017 meta-analysis used two parameters to determine the accuracy of age-based and weight estimation systems: 70% of weight approximations are within 10% of the actual weight and 90% of weight approximations are within 20% of the actual weight (Citation32). In this study, the Mercy Method, the PAWPER Tape (Citation33), and parental estimate of the pediatric patient’s weight yielded more accurate results than the Broselow-Luten tape. A 2016 meta-analysis of age-based calculations for estimating patient weight showed the Advanced Pediatric Life Support formula yielded the best results when used to calculate doses for lipophilic drugs (e.g. lidocaine, atropine, benzodiazepines), and accounted for the increasing adiposity of pediatric patients (Citation34). In contrast, several studies demonstrate that age-based methods are not as accurate as other weight estimation methods. Another meta-analysis published in 2016 considered a large international cohort of pediatric patients and showed that length-based tapes and parental estimates of weights were more accurate than age-based estimates (Citation35). Similarly, an earlier study by Krieser et al. based in the emergency department showed that the Broselow-Luten tape and parental estimates of pediatric patients’ weights outperformed age-based weight estimates (Citation36). Additionally, a study by O’Leary et al. published in an ethnically diverse Australian emergency department also showed that length-based tools out-performed age-based estimates (Citation37).
Key concept area #2: What are the greatest safety threats to medication dosing (latent or otherwise)?
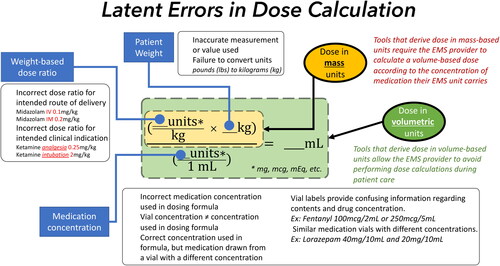
Calculation of a weight-based medication dose requires input of several data points into a formula including the patient’s weight, the concentration of the drug, and the desired weight-based dose. illustrates this formula and highlights the several steps in this formula where input errors can result in incorrect calculations.
Even under non-stressful circumstances, performing dose calculations carries the risk of making calculation errors. A study by Hubble revealed that dosing calculations made by paramedics were correct only 68% of the time in a controlled classroom environment. Errors of commission included conceptual errors (i.e., errors in setting up the problem), mathematical errors, errors in weight conversion, and errors in unit conversion (e.g., grams to milligrams) (Citation38). It was noted that more errors were made among paramedics with more years of experience. Bernius also demonstrated that paramedic accuracy in mathematical calculation performed in a controlled classroom environment was very poor unless a dosing aid was utilized (Citation14) These findings are further reinforced by several papers by Eastwood that showed up to 68% of paramedic students scored 50% or lower on a drug dose calculation examination, with errors including conceptual errors, arithmetical errors, and computational errors (Citation39–41). Even when paramedics are not under on-the-job pressure their ability to perform drug calculations accurately is poor as demonstrated by Eastwood and Boyle who reported finding up to 42% of paramedics with four or more years of experience scoring 50% or less on the drug dose calculation assessment (Citation40,Citation42)
Mathematical computation is an example of working memory, the capacity to store and manipulate information for brief periods of time. Several studies have investigated the effect of stress on working memory of both non-EMS providers and EMS providers and have demonstrated a decremental effect on solving mathematical problems especially under circumstances with a high task load (Citation43–46). Interestingly, Beilock’s study suggests that performance pressure harms individuals most qualified to succeed by consuming the working memory capacity that they rely on for their superior performance. This finding suggests that even the most highly-performing EMS providers are subject to stress-related detriments in mathematical performance. LeBlanc et al. investigated the effect of stress on paramedics’ ability to calculate drug dosages under stress and found that high stress resulted in an increase in medication dosing errors (Citation47). Several other publications by LeBlanc also demonstrate the detrimental effect of acute stress on cognitive performance of EMS providers (Citation48,Citation49).
Qualitative investigations of adverse events and near misses when pediatric patients receive EMS care have demonstrated that the following latent safety threats are associated with poor patient outcomes: a lack of comfort in caring for pediatric patients, medication errors, the absence of properly sized equipment, and errors in skill performance (Citation50,Citation51). More importantly, participants stated errors were sometimes not reported and therefore the true frequency of these events may be underestimated. Paramedics do report being more comfortable providing medications to pediatric patients when there is a good relationship with direct medical oversight and when medication dosing aids are available when providing analgesia to their pediatric patients (Citation51). Though most tools for providing drug dosing information in pediatric emergencies are not specific to EMS care, survey data of EMS providers suggest that an EMS-specific length-based tape and standardized protocols would improve EMS pediatric medication dosing (Citation5).
A specific age-based medication dosing strategy proposed to improve safety is standardizing doses based on the 50th percentile weight for a given age. Commonly used length-based tapes may result in underestimation of patient weights, with attendant errors in medication dosing (Citation52,Citation53). A meta-analysis by Wells et al. showed a commonly used length-based tape is prone to weight overestimates when used for pediatric patients in low- and middle-income countries (Citation52). A 2016 study by Lowe et al. showed that the Handtevy System outperformed the Broselow-Luten tape for weight estimation in taller pediatric patients, while the opposite was true for shorter pediatric patients (Citation54). Of note, the two systems are now nearly identical regarding length-color zones on the length-based tape.
When paramedics use the Broselow-Luten length-based tape in a simulated resuscitation of an infant with hypoglycemia and seizures, there were errors in the use of the tape (e.g. placing the wrong end of the tape at the patient’s head), yet 80% of the time, the tape was used to obtain an accurate weight for the patient (Citation4). A study by the same authors with a simulated pediatric anaphylaxis patient showed better performance of weight estimates (correct 35 of 37 times), and that the Broselow-Luten tape outperformed the pediatric wheel and paramedic guessing for weight estimation (Citation55).
International teams have conducted investigations in South Africa (Citation17) and Korea (Citation56) of pediatric patient size variation as a latent safety threat. The latter study showed limitations in a formula-based strategy for estimating patient weights and doses by age, especially among older, heavier pediatric patients. A study conducted in an Indian tertiary care hospital showed significant variation between actual weights and weight estimates from a length-based tape (Citation57). A study of paramedics conducted in the United States showed that paramedics could estimate the weights of pediatric patients with moderate accuracy regardless of age, and that a length-based tape improved their weight estimates (Citation24). Appelbaum’s work showed that accounting for pediatric patient size and body habitus improved weight estimates, mitigating the latent safety threat of pediatric patient size variation (Citation23). A study of 179 pediatric patients treated by EMS showed that pediatric patients aged less than ten years old and those with seizures or cardiac arrest were more likely to have incorrect weight estimates by EMS, and were more likely to have medication dosing errors (Citation6).
As previously noted, EMS providers care for pediatric patients less frequently than adults patients, and this may be a latent safety threat to medication dosing (Citation58,Citation59). A 2005 study by Stevens showed 87% of EMS providers in Maine had three or fewer pediatric calls per month, and that being a paramedic and/or having more pediatric continuing education increased comfort with pediatric patients (Citation60). Strategies to mitigate limited field exposure by increasing exposure via training have been suggested. However, the role of frequent training in decreasing medication errors is not clear.
A small RCT by Su et al. that randomized paramedics to have knowledge evaluations and simulated resuscitation training at six months, simulated resuscitation training at six months only, or no additional training showed no difference in pediatric resuscitation knowledge and skills one year after the study began (Citation61). Simulation-based studies of two person paramedic-paramedic or paramedic-emergency medical technician teams showed that medication dosing errors were common in pediatric resuscitations (Citation27,Citation62). Paramedics perceive a need for more frequent pediatric refresher training (Citation51), and there are data to suggest that frequent refresher training does decrease the likelihood of medication dosing errors during EMS patient encounters.
A final potential latent safety threat to pediatric medication dosing in the EMS setting is the use of buretrols, rather than calibrated pumps, for infused medication delivery. A literature search found no pertinent articles in the EMS setting. One study of hospitalized pediatric patients receiving chloramphenicol showed that delivering infusions using pumps and anatomically proximal infusion sites led to higher, faster blood concentration of the drug than when buretrols and more distal sites were used (Citation63,Citation64). Another in vitro study found that use of a buretrol resulted in residual medication in the IV tubing (Citation49) resulting in incomplete medication delivery. In a setting where pediatric patients received propofol for sedation, the use of an infusion pump was associated with faster and more predictable medication effects than the use of a buretrol (Citation65).
Key concept area #3: Can dosing safety education and strategies from other settings (e.g. the emergency department, operating room, inpatient units, and intensive care units) be adapted to the EMS setting?
Given the psychomotor components of medication dosing in pediatrics, such as using a length-based tape to estimate weight, drawing up a specific volume of medication based on patient size, and delivering a specific volume of medication, simulation has a role in providing EMS providers the opportunity to practice and maintain these skills in a realistic setting (Citation66,Citation67). Simulation has been used to improve the accuracy of resuscitation medication dosing by pediatrics residents in the inpatient setting (Citation16) and in the emergency department (Citation68), and a meta-analysis by Sarfati et al. showed simulation improves medication dosing safety for adult patients (Citation69). The latter study cautions educators to consider human factors, such as medication preparation and administration tasks, to avoid introducing new risks to medication dosing safety.
Lammers et al. have shown the utility of simulation for revealing EMS medication dosing errors and their causes in a range of pediatric emergencies (Citation4) including pediatric anaphylaxis (Citation55) and pediatric cardiopulmonary arrest (Citation62). Simulation has also been used to assess the utility of novel dosing safety strategies, such as color-coded, pre-measured volume medication syringes (Citation70). This study by Stevens et al. conducted in a cohort of 10 paramedics in Denver, CO found that the novel syringes decreased time to medication administration and decreased the incidence of critical dosing errors, however this study includes several significant limitations including small sample size and lack of statistical significance and unclear clinical significance of many of the reported findings.
The use of independent medication dosing cross checks has been adopted in other clinical settings for verification of correct dosing and route of administration for various high-risk medications (Citation71,Citation72). However reviews of this practice outside EMS reveal mixed results, with several papers concluding there is insufficient evidence to either support or refute the practice of independent double checking for the administration of medicines (Citation72–75). The Institute of Safe Medication Practices recommends a tempered approach, stating: “When employed judiciously, conducted properly, and bundled with other strategies, manual independent double checks can be part of a valuable defense to prevent potentially harmful errors from reaching patients (Citation76).”
Our review of the literature identified a single EMS-based study that evaluated the effect of a team-based cross-check process for medication verification in the EMS setting (Citation77). This observational study did report a potential decrease in medication administration errors after introduction of a medication cross check procedure, however the study included several limitations including small sample size and lack of statistical significance and unclear clinical significance of many of the reported findings.
The use of two-provider medication cross checking deserves additional attention as a potential risk-mitigation practice especially when medication shortages force EMS agencies to stock medications in packaging, labeling, or concentrations atypical from their usual medication supply. Additionally, the feasibility of performing two-provider crosschecks when partners are spatially isolated (such as when one provider is in the patient compartment of the ambulance and the second provider is driving the ambulance) deserves additional scrutiny.
Key concept area #4: What is known about the role of standardized formularies in dosing safety? Is a standardized formulary protocol a means for pre-calculation of doses and decreasing errors? Are drug shortages and concerns for medical director autonomy barriers to standardization of formularies?
Standardized formularies for medications in the EMS setting could offer improved accuracy and safety for pediatric dosing. In the EMS setting, a mixed-methods study of paramedics by Hoyle et al. revealed that EMS providers were frustrated by frequent drug concentration changes and packaging changes, and that standardization was preferable (Citation78). A 2007 investigation by Kaji et al. showed a color-coded standardized epinephrine dose and route in cardiac arrest yielded an odds ratio of 3.0 for administering an accurate dose (Citation15).
While standardized doses offer a means of decreasing medication errors, drug shortages may represent a threat to dose standardization and dosing safety. A review of 1,929 different national drug shortages showed intravenous medications account for 70% of medication shortages, and that the median shortage duration for acute care medications (242 days, IQR 96–624 days) was longer than the median overall medication shortage duration (173 days, IQR 85–531 days) (Citation79). Work conducted at the same site showed that among 1,798 national drug shortages, medications used in the emergency setting represented 610 of the drugs, 52.6% of which were used for life-saving or high-acuity interventions (Citation80). A survey of emergency physicians in China suggested medication shortages are common and compromise patient care (Citation81).
Limitations
The literature analysis presented here reveals a number of gaps in what is known about pediatric dosing safety in the EMS setting. The safest means for determining patient weights (e.g. length-based tapes versus scales built into stretchers) remains unknown. More investigations of length-based tapes and age-based dosing strategies are needed to determine whether an existing or novel dosing system provides the safest and most practical means of administering medications to pediatric patients. Medication crosschecks might help reduce errors, but studies explicitly evaluating this strategy in the EMS setting are lacking and further investigation of their utility in EMS is needed. One specific reservation about crosschecks in EMS is that it may not be practical to conduct a medication cross-check when the ambulance is in motion, or when there is only one paramedic present on-site.
There are several safety risks specific to the United States, including the use of the pound as a unit of weight measure and higher prevalence of obesity in the pediatric population, though the actual effect of obesity and its relationship to clinically meaningful dose adjustments remains unclear (Citation82,Citation83). Our investigation yielded no studies that show whether ideal body weight or actual body weight was a safer means of determining weights for medication dosing. The best strategy for pediatric EMS dosing may consider whether the medication is hydrophilic or hydrophobic (lipophilic). Carasco et al. provide an excellent discussion of this topic (Citation33). Medications used in the EMS setting tend to fall within the hydrophilic category, which is best dosed based on ideal body weight, in which case dosing based on 50th percentile strategies is appropriate. Of the medications commonly used in the EMS setting that are hydrophobic (and as such should ideally be dosed based on actual body weight), including atropine, benzodiazepines, and corticosteroids, the majority of these medications enjoy a broad therapeutic window. While dosing of these hydrophobic drugs based on IBW will tend to underdose patients with higher BMIs, dosing of these medications can typically be easily titrated to effect.
Simulation and other educational modalities have been used to assess errors and safety threats to pediatric medication dosing in the EMS setting however there are few investigations that show correlation between educational interventions for EMS providers and improved dosing safety for pediatric patients.
A final limitation to what is known about pediatric medication dosing safety is the potential impact of statewide or even nationally standardized formularies on the incidence of dosing errors. Investigations of such an intervention could include mixed methods approaches, simulation assessments, and pre- and post- intervention surveillance for dosing errors and harm to patients. However, ongoing and critical inconsistency in the supply of emergency medications and the subsequent need for EMS agencies and systems to make frequent substitutions in their usual and customary medication supply present a major and terminal limitation to the development and implementation of a standardized formulary at any geopolitical level.
Conclusion
EMS medical directors, leaders, and training officers can incorporate the recommendations offered in this document to mitigate the risk of pediatric dosing errors.
| Abbreviations | ||
| EMS | = | Emergency Medical Services |
| NAEMSP | = | National Association of EMS Physicians |
| PICO | = | Population, Intervention, Control, Outcome |
| RCT | = | Randomized Controlled Trial. |
Supplemental Material
Download MS Word (28.8 KB)Supplemental Material
Download MS Word (105.2 KB)References
- Shah MN, Cushman JT, Davis CO, Bazarian JJ, Auinger P, Friedman B. The epidemiology of emergency medical services use by children: an analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12(3):269–76. doi:10.1080/10903120802100167.
- Kannikeswaran N, Mahajan PV, Dunne RB, Compton S, Knazik SR. Epidemiology of pediatric transports and non-transports in an urban Emergency Medical Services system. Prehosp Emerg Care. 2007;11(4):403–7. doi:10.1080/10903120701536677.
- Lerner EB, Dayan PS, Brown K, Fuchs S, Leonard J, Borgialli D, Babcock L, Hoyle JD, Jr, Kwok M, Lillis K, for the Pediatric Emergency Care Applied Research Network (PECARN), et al. Characteristics of the pediatric patients treated by the Pediatric Emergency Care Applied Research Network's affiliated EMS agencies. Prehosp Emerg Care. 2014;18(1):52–9. doi:10.3109/10903127.2013.836262.
- Lammers R, Byrwa M, Fales W. Root causes of errors in a simulated prehospital pediatric emergency. Acad Emerg Med. 2012;19(1):37–47. doi:10.1111/j.1553-2712.2011.01252.x.
- Hoyle JD, Crowe RP, Bentley MA, Beltran G, Fales W. Pediatric prehospital medication dosing errors: a national survey of paramedics. Prehosp Emerg Care. 2017;21(2):185–91. doi:10.1080/10903127.2016.1227001.
- Lim CAE, Kaufman BJ, O’Connor J, Cunningham SJ. Accuracy of weight estimates in pediatric patients by prehospital emergency medical services personnel. Am J Emerg Med. 2013;31(7):1108–12. doi:10.1016/j.ajem.2013.04.018.
- McDowell SE, Ferner HS, Ferner RE. The pathophysiology of medication errors: how and where they arise. Br J Clin Pharmacol. 2009;67(6):605–13. doi:10.1111/j.1365-2125.2009.03416.x.
- Hoyle JD, Davis AT, Putman KK, Trytko JA, Fales WD. Medication dosing errors in pediatric patients treated by emergency medical services. Prehosp Emerg Care. 2012;16(1):59–66. doi:10.3109/10903127.2011.614043.
- Hoyle JD, Ekblad G, Hover T, Woodwyk A, Brandt R, Fales B, Lammers RL. Dosing errors made by paramedics during pediatric patient simulations after implementation of a state-wide pediatric drug dosing reference. Prehosp Emerg Care. 2020;24(2):204–213. doi:10.1080/10903127.2019.1619002.
- Huang X, Lin J, Demner-Fushman D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Annu Symp Proc. 2006;359–63.
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–e130.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ, GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. doi:10.1136/bmj.39489.470347.AD.
- Luten R, Wears RL, Broselow J, Croskerry P, Joseph MM, Frush K. Managing the unique size-related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Acad Emerg Med. 2002;9(8):840–7. doi:10.1197/aemj.9.8.840.
- Bernius M, Thibodeau B, Jones A, Clothier B, Witting M. Prevention of pediatric drug calculation errors by prehospital care providers. Prehosp Emerg Care. 2008;12(4):486–94. doi:10.1080/10903120802290752.
- Kaji AH, Gausche-Hill M, Conrad H, Young KD, Koenig WJ, Dorsey E, Lewis RJ. Emergency medical services system changes reduce pediatric epinephrine dosing errors in the prehospital setting. Pediatrics. 2006;118(4):1493–500. doi:10.1542/peds.2006-0854.
- Shah AN, Frush K, Luo X, Wears RL. Effect of an intervention standardization system on pediatric dosing and equipment size determination: a crossover trial involving simulated resuscitation events. Arch Pediatr Adolesc Med. 2003;157(3):229–36. doi:10.1001/archpedi.157.3.229.
- Wells M, Coovadia A, Kramer E, Goldstein L. The PAWPER tape: a new concept tape-based device that increases the accuracy of weight estimation in children through the inclusion of a modifier based on body habitus. Resuscitation. 2013;84(2):227–32. doi:10.1016/j.resuscitation.2012.05.028.
- Rappaport LD, Brou L, Givens T, Mandt M, Balakas A, Roswell K, Kotas J, Adelgais KM. Comparison of errors using two length-based tape systems for prehospital care in children. Prehosp Emerg Care. 2016;20(4):508–17. doi:10.3109/10903127.2015.1128027.
- Haffey F, Brady RR, Maxwell S. A comparison of the reliability of smartphone apps for opioid conversion. Drug Saf. 2013;36(2):111–7. doi:10.1007/s40264-013-0015-0.
- Siebert JN, Ehrler F, Combescure C, Lacroix L, Haddad K, Sanchez O, Gervaix A, Lovis C, Manzano S. A mobile device app to reduce time to drug delivery and medication errors during simulated pediatric cardiopulmonary resuscitation: a randomized controlled trial. J Med Internet Res. 2017;19(2):e31. doi:10.2196/jmir.7005.
- Low D, Clark N, Soar J, Padkin A, Stoneham A, Perkins GD, Nolan J. A randomised control trial to determine if use of the iResus© application on a smart phone improves the performance of an advanced life support provider in a simulated medical emergency. Anaesthesia. 2011;66(4):255–62. doi:10.1111/j.1365-2044.2011.06649.x.
- Dingley J, Cromey C, Bodger O, Williams D. Evaluation of 2 novel devices for calculation of fluid requirements in pediatric burns. Ann Plast Surg. 2015;74(6):658–64.
- Appelbaum N, Clarke J, Maconochie I, Darzi A. Paediatric weight estimation by age in the digital era: optimising a necessary evil. Resuscitation. 2018;122:29–35. doi:10.1016/j.resuscitation.2017.11.041.
- Vilke GM, Marino A, Fisher R, Chan TC. Estimation of pediatric patient weight by EMT-PS. J Emerg Med. 2001;21(2):125–8. doi:10.1016/S0736-4679(01)00354-7.
- Chassee T, Reischmann D, Mancera M, Hoyle JD. Emergency medical dispatchers can obtain accurate pediatric weights from 9-1-1 callers. Prehosp Emerg Care. 2016;20(6):808–14. doi:10.3109/10903127.2016.1168892.
- Hoyle JD, Jr, Ekblad G, Hover T, Woodwyk A, Brandt R, Fales B, Lammers RL. Analysis of dosing errors made by paramedics during simulated pediatric patient scenarios after implementation of state-wide pediatric drug dosing reference. Prehosp Emerg Care. 2017;1–50.
- Sinha M, Lezine MW, Frechette A, Foster KN. Weighing the pediatric patient during trauma resuscitation and its concordance with estimated weight using Broselow Luten Emergency Tape. Pediatr Emerg Care. 2012;28(6):544–7. doi:10.1097/PEC.0b013e318258ac2e.
- Wong E, Taylor Z, Thompson J, Tuthill D. A simplified gentamicin dosing chart is quicker and more accurate for nurse verification than the BNFc. Arch Dis Child. 2009;94(7):542–5. doi:10.1136/adc.2007.137026.
- Weighing all patients in kilograms. Pediatrics. 2017;140(4). https://pediatrics.aappublications.org/content/pediatrics/140/4/e20172476.full.pdf
- Gerber M. How to measure and improve EMS systems. EMS compass is setting the profession on a path toward performance measurement and improvement. EMS World. 2016;45(1):24–6.
- Shaw KN, Lillis KA, Ruddy RM, Mahajan PV, Lichenstein R, Olsen CS, Chamberlain JM. Reported medication events in a paediatric emergency research network: sharing to improve patient safety. Emerg Med J. 2013;30(10):815–9. doi:10.1136/emermed-2012-201642.
- Wells M, Goldstein LN, Bentley A. The accuracy of emergency weight estimation systems in children-a systematic review and meta-analysis. Int J Emerg Med. 2017;10(1):29. doi:10.1186/s12245-017-0156-5.
- Wells M, Goldstein LN. Optimising emergency weight estimation in underweight and obese children: the accuracy of estimations of total body weight and ideal body weight. Eur J Emerg Med. 2019;26(4):301–307.
- Carasco CF, Fletcher P, Maconochie I. Review of commonly used age-based weight estimates for paediatric drug dosing in relation to the pharmacokinetic properties of resuscitation drugs. Br J Clin Pharmacol. 2016;81(5):849–56. doi:10.1111/bcp.12876.
- Young KD, Korotzer NC. Weight estimation methods in children: a systematic review. Ann Emerg Med. 2016;68(4):441–51.e410. doi:10.1016/j.annemergmed.2016.02.043.
- Krieser D, Nguyen K, Kerr D, Jolley D, Clooney M, Kelly AM. Parental weight estimation of their child's weight is more accurate than other weight estimation methods for determining children's weight in an emergency department? Emerg Med J. 2007;24(11):756–9. doi:10.1136/emj.2007.047993.
- O'Leary F, John-Denny B, McGarvey K, Hann A, Pegiazoglou I, Peat J. Estimating the weight of ethnically diverse children attending an Australian emergency department: a prospective, blinded, comparison of age-based and length-based tools including Mercy, PAWPER and Broselow. Arch Dis Child. 2017;102(1):46–52. doi:10.1136/archdischild-2016-310917.
- Hubble MW, Paschal KR, Sanders TA. Medication calculation skills of practicing paramedics. Prehosp Emerg Care. 2000;4(3):253–60. doi:10.1080/10903120090941290.
- Eastwood K, Boyle MJ, Williams B. Mathematical and drug calculation abilities of paramedic students. Emerg Med J. 2013;30(3):241–2. doi:10.1136/emermed-2011-200929.
- Eastwood K, Boyle MJ, Williams B. Undergraduate paramedic students cannot do drug calculations. World J Emerg Med. 2012;3(3):221–6. doi:10.5847/wjem.j.issn.1920-8642.2012.03.011.
- Eastwood KJ, Boyle MJ, Williams B. Paramedics' ability to perform drug calculations. West J Emerg Med. 2009;10(4):240–3.
- Boyle MJ, Eastwood K. Drug calculation ability of qualified paramedics: a pilot study. World J Emerg Med. 2018;9(1):41–5. doi:10.5847/wjem.j.1920-8642.2018.01.006.
- Beilock SL, Carr TH. When high-powered people fail: working memory and “choking under pressure” in math. Psychol Sci. 2005;16(2):101–5. doi:10.1111/j.0956-7976.2005.00789.x.
- Wolf OT. The influence of stress hormones on emotional memory: relevance for psychopathology. Acta Psychol (Amst). 2008;127(3):513–31. doi:10.1016/j.actpsy.2007.08.002.
- Lupien SJ, Gillin CJ, Hauger RL. Working memory is more sensitive than declarative memory to the acute effects of corticosteroids: a dose-response study in humans. Behav Neurosci. 1999;113(3):420–30. doi:10.1037//0735-7044.113.3.420.
- MA S. Stress, cognition, and human performance: a literature review and conceptual framework. https://ntrs.nasa.gov/citations/20060017835. Published 2004. Accessed November 25, 2019.
- LeBlanc VR, MacDonald RD, McArthur B, King K, Lepine T. Paramedic performance in calculating drug dosages following stressful scenarios in a human patient simulator. Prehosp Emerg Care. 2005;9(4):439–44. doi:10.1080/10903120500255255.
- Leblanc VR, Regehr C, Tavares W, Scott AK, Macdonald R, King K. The impact of stress on paramedic performance during simulated critical events. Prehosp Disaster Med. 2012;27(4):369–74. doi:10.1017/S1049023X12001021.
- LeBlanc VR. The effects of acute stress on performance: implications for health professions education. Acad Med. 2009;84(10 Suppl):S25–S33. doi:10.1097/ACM.0b013e3181b37b8f.
- Cushman JT, Fairbanks RJ, O'Gara KG, Crittenden CN, Pennington EC, Wilson MA, Chin NP, Shah MN. Ambulance personnel perceptions of near misses and adverse events in pediatric patients. Prehosp Emerg Care. 2010;14(4):477–84. doi:10.3109/10903127.2010.497901.
- Cottrell EK, O'Brien K, Curry M, Meckler GD, Engle PP, Jui J, Summers C, Lambert W, Guise JM. Understanding safety in prehospital emergency medical services for children. Prehosp Emerg Care. 2014;18(3):350–8. doi:10.3109/10903127.2013.869640.
- Wells M, Goldstein LN, Bentley A, Basnett S, Monteith I. The accuracy of the Broselow tape as a weight estimation tool and a drug-dosing guide - A systematic review and meta-analysis. Resuscitation. 2017;121:9–33. doi:10.1016/j.resuscitation.2017.09.026.
- Nieman CT, Manacci CF, Super DM, Mancuso C, Fallon WF. Use of the Broselow tape may result in the underresuscitation of children. Acad Emerg Med. 2006;13(10):1011–9. doi:10.1197/j.aem.2006.06.042.
- Lowe CG, Campwala RT, Ziv N, Wang VJ. The Broselow and Handtevy resuscitation tapes: a comparison of the performance of pediatric weight prediction. Prehosp Disaster Med. 2016;31(4):364–75. doi:10.1017/S1049023X16000455.
- Lammers R, Willoughby-Byrwa M, Fales W. Medication errors in prehospital management of simulated pediatric anaphylaxis. Prehosp Emerg Care. 2014;18(2):295–304. doi:10.3109/10903127.2013.856501.
- Park J, Kwak YH, Kim DK, Jung JY, Lee JH, Jang HY, Kim HB, Hong KJ. A new age-based formula for estimating weight of Korean children. Resuscitation. 2012;83(9):1129–34. doi:10.1016/j.resuscitation.2012.01.023.
- Shah V, Bavdekar SB. Validity of Broselow tape for estimating weight of Indian children. Indian J Med Res. 2017;145(3):339–46.
- Laraque D, Boscarino J, Battista A, Fleischman A, Casalino M, Hu Y, Ramos S, Adams RE, Schmidt J, Chemtob C. Reactions and needs of tristate-area pediatricians after the events of September 11th: implications for children's mental health services. Pediatrics. 2004;113(5):1357–66. doi:10.1542/peds.113.5.1357.
- Fleischman RJ, Yarris LM, Curry MT, Yuen SC, Breon AR, Meckler GD. Pediatric educational needs assessment for urban and rural emergency medical technicians. Pediatr Emerg Care. 2011;27(12):1130–5.
- Stevens SL, Alexander JL. The impact of training and experience on EMS providers' feelings toward pediatric emergencies in a rural state. Pediatr Emerg Care. 2005;21(1):12–7.
- Su E, Schmidt T, Mann N, Zechnich A. A randomized controlled trial to assess decay in acquired knowledge among paramedics completing a pediatric resuscitation course. Acad Emerg Med. 2000;7(7):779–86. doi:10.1111/j.1553-2712.2000.tb02270.x.
- Lammers RL, Willoughby-Byrwa M, Fales WD. Errors and error-producing conditions during a simulated, prehospital, pediatric cardiopulmonary arrest. Simul Healthc. 2014;9(3):174–83. doi:10.1097/SIH.0000000000000013.
- Nahata MC, Powell DA, Glazer JP, Hilty MD. Effect of intravenous flow rate and injection site on in vitro delivery of chloramphenicol succinate and in vivo kinetics. J Pediatr. 1981;99(3):463–6. doi:10.1016/S0022-3476(81)80351-4.
- Nahata MC, Powell DA, Durrell D, Glazer JP. Delivery of tobramycin by three infusion systems. Chemotherapy. 1984;30(2):84–7. doi:10.1159/000238251.
- Abdallah C, Hannallah R, Patel K. MR-compatible pumps versus manual titration of propofol for pediatric sedation. J Med Eng Technol. 2010;34(7-8):443–7. doi:10.3109/03091902.2010.515286.
- Weinberg E, Auerbach M, Shah N. The use of simulation for pediatric training and assessment. Curr Opin Pediatr. 2009;21(3):282–7. doi:10.1097/MOP.0b013e32832b32dc.
- Bokhari R, Bollman-Mcgregor J, Kahol K, Smith M, Feinstein A, Ferrara J. Design, development, and validation of a take-home simulator for fundamental laparoscopic skills: using Nintendo Wii for surgical training. Am Surg. 2010;76(6):583–6. doi:10.1177/000313481007600620.
- Frush K, Hohenhaus S, Luo X, Gerardi M, Wiebe RA. Evaluation of a web-based education program on reducing medication dosing error: a multicenter, randomized controlled trial. Pediatr Emerg Care. 2006;22(1):62–70. doi:10.1097/01.pec.0000195760.97199.7e.
- Sarfati L, Ranchon F, Vantard N, Schwiertz V, Larbre V, Parat S, Faudel A, Rioufol C. Human-simulation-based learning to prevent medication error: A systematic review. J Eval Clin Pract. 2019;25(1):11–20. doi:10.1111/jep.12883.
- Stevens AD, Hernandez C, Jones S, Moreira ME, Blumen JR, Hopkins E, Sande M, Bakes K, Haukoos JS. Color-coded prefilled medication syringes decrease time to delivery and dosing errors in simulated prehospital pediatric resuscitations: a randomized crossover trial. Resuscitation. 2015;96:85–91. doi:10.1016/j.resuscitation.2015.07.035.
- Alsulami Z, Choonara I, Conroy S. Nurses' knowledge about the double-checking process for medicines administration. Nurs Child Young People. 2014;26(9):21–6. doi:10.7748/ncyp.26.9.21.e378.
- Schwappach DL, Pfeiffer Y, Taxis K. Medication double-checking procedures in clinical practice: a cross-sectional survey of oncology nurses' experiences. BMJ Open. 2016;6(6):e011394. doi:10.1136/bmjopen-2016-011394.
- Alsulami Z, Conroy S, Choonara I. Double checking the administration of medicines: what is the evidence? A systematic review. Arch Dis Child. 2012;97(9):833–7. doi:10.1136/archdischild-2011-301093.
- Hewitt T, Chreim S, Forster A. Double checking: a second look. J Eval Clin Pract. 2016;22(2):267–74. doi:10.1111/jep.12468.
- Ekmekjian T, Castiglione S. What evidence exists that describes whether manual double checks should be performed independently or synchronously to decrease the risk of medication administration error? August ed. Montreal, Quebec, Canada: McGill University Health Centre; 2017.
- Institute for Safe Medication Practices. Independent double checks worth the effort if used judiciously and properly. https://www.ismp.org/resources/independent-double-checks-worth-effort-if-used-judiciously-and-properly [accessed 2019 Jun 06].
- Misasi P, Keebler JR. Medication safety in emergency medical services: approaching an evidence-based method of verification to reduce errors. Ther Adv Drug Saf. 2019;10:2042098618821916. doi:10.1177/2042098618821916.
- Hoyle JD, Sleight D, Henry R, Chassee T, Fales B, Mavis B. Pediatric prehospital medication dosing errors: a mixed-methods study. Prehosp Emerg Care. 2016;20(1):117–24. doi:10.3109/10903127.2015.1061625.
- Chen SI, Fox ER, Hall MK, Ross JS, Bucholz EM, Krumholz HM, Venkatesh AK. Despite federal legislation, shortages of drugs used in acute care settings remain persistent and prolonged. Health Aff (Millwood). 2016;35(5):798–804. doi:10.1377/hlthaff.2015.1157.
- Hawley KL, Mazer-Amirshahi M, Zocchi MS, Fox ER, Pines JM. Longitudinal trends in U.S. drug shortages for medications used in emergency departments (2001-2014). Acad Emerg Med. 2016;23(1):63–9. doi:10.1111/acem.12838.
- Yang C, Cai W, Li Z, Page AT, Fang Y. The current status and effects of emergency drug shortages in China: perceptions of emergency department physicians. PLoS One. 2018;13(10):e0205238. doi:10.1371/journal.pone.0205238.
- Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561–6. doi:10.1001/jamapediatrics.2014.21.
- Callaghan LC, Walker JD. An aid to drug dosing safety in obese children: development of a new nomogram and comparison with existing methods for estimation of ideal body weight and lean body mass. Anaesthesia. 2015;70(2):176–82. doi:10.1111/anae.12860.