Abstract
This update to the 2013 joint position statement, Appropriate and Safe Utilization of Helicopter Emergency Medical Services, provides guidance for air medical services utilization based on currently available evidence. Air medical services utilization considerations fall into three major categories: clinical considerations, safety considerations, and system integration and quality assurance.
Clinically, air medical services should accomplish one or more of three primary patient-centered goals: initiation or continuation of locally unavailable advanced or specialty care; expedited delivery to definitive care for time-sensitive interventions; and/or extraction from physically remote or otherwise inaccessible locations that limit timely access to necessary care. Ground-EMS (GEMS) transport is preferred when it is able to provide the necessary level of care and timely transport to definitive care.
Risk identification and safety of both the patient and crew must be uniformly balanced against the anticipated degree of patient medical benefit. While auto-ready and auto-launch practices may increase access to air medical services, they also risk over-use, and so must be rigorously reviewed. Safety is enhanced during multi-agency emergency responses by coordinated interagency communication, ideally through centralized communication centers. Helicopter shopping and reverse helicopter shopping both create significant safety risks and their use is discouraged.
Regional EMS systems must integrate air medical services to facilitate appropriate utilization in alignment with the primary patient goals while being cognizant of local indications, resources, and needs. To maximize consistent, informed air medical services utilization decisions, specific indications for and limitations to air medical services utilization that align with local and regional system and patient needs should be identified, and requests routed through centralized coordinating centers supported by EMS physicians.
To limit risk and promote appropriate utilization of air medical services, GEMS clinicians should be encouraged to cancel an air medical services response if it is not aligned with at least one of the three primary patient-centered goals. Similarly, air medical services clinicians should be empowered to redirect patient transport to GEMS. Air medical services should not routinely be used solely to allow GEMS to remain in their primary service area.
Position Statement
Air medical services involve providing medical care in transit while using either fixed wing (airplane) or rotor wing (helicopter) aircraft to move patients between locations. The modern use and availability of air medical services has expanded access to various health system resources, including specialty care. While this is generally beneficial, such expansion has also contributed to the complexity of health care delivery systems (Citation1, Citation2). Since the publication of the 2013 joint position statement Appropriate and Safe Utilization of Helicopter Emergency Medical Services (Citation3), research has shown that patient benefit is gained from the clinical care capabilities of air medical services independent of potential time saved when transporting patients (Citation4–6). Because the evidence basis for utilization of air medical services continues to evolve, NAEMSP, ACEP, and AMPA believe that an update regarding the appropriate utilization of air medical services is warranted, and that such guidance for utilization can be divided into three major categories: clinical considerations, safety considerations, and system integration and quality assurance considerations.
Clinical Considerations
Air medical services should be used to accomplish one or more of three primary patient-centered goals. All of the statements that follow should be viewed through the lens of these goals:
Initiation or continuation of advanced or specialty care that is not otherwise available locally from hospital or ground EMS resources;
Expedited delivery of the patient to definitive care for time-sensitive interventions; and/or
Extraction, evacuation, and/or rescue from environments that are difficult to access due to geography, weather, remote location, distance, and other factors that limit timely access to a patient or transport by ground EMS.
If a patient’s clinical need for critical care expertise and timely transport to definitive care can be met with ground EMS resources, then ground EMS transport is preferred to air transport transport in most circumstances.
For some non-emergent patients, air medical services resources, usually via fixed wing aircraft with one or more accompanying medical attendants, may be used to repatriate a patient from a distant location to a facility closer to the patient’s home in order to access a higher level of care, provide continuity of care from the patient’s home health care system, and/or access the patient’s local family, social, and medical support community.
Risk Identification and Safety Considerations
For every flight, the level of risk to patient and crew must be carefully weighed against the reasonably anticipated degree of medical benefit to the patient (Citation7, Citation8).
Auto-ready and auto-launch practices intended to increase on-scene access to air medical resources for ill or injured patients can provide medical benefit but can also result in over-use (Citation9–11). Such practices must be subject to rigorous and continuous quality assurance review.
Ground EMS clinicians on scene should be empowered and encouraged to cancel air medical services response if/when it is determined that continuing that response would:
Place the air crew and aircraft at undue risk
Place ground crews at undue risk
Not align with at least one of the three primary patient-centered goals of air medical transport
To enhance safety during multi-agency emergency responses, communication between air medical services and ground EMS and between multiple responding air resources should be routinely coordinated, ideally through centralized communication centers.
For safety reasons, requesting entities should not engage in helicopter shopping. Helicopter shopping is the practice of making calls to multiple air medical services agencies to attempt to secure air transport after an initial service has declined a flight due to safety concerns (Citation12). Similarly, air medical services agencies should not engage in reverse helicopter shopping by seeking out and offering to perform transport missions that have been declined by one or more other services due to safety considerations.
System Integration and Quality Assurance Considerations
Requests for air medical services should first align with the three primary goals of utilization, followed by locally established specific indications, and then considered against locally applicable ground EMS and air medical services resource limitations.
To encourage consistent, informed air medical services utilization decisions, we recommend requests be routed through centralized coordinating centers with access to and oversight by EMS physicians familiar with air medical services care (Citation13).
Ideally, physicians providing oversight of air medical services should meet the requirements set forth in the joint position statement Physician Oversight of Air-based EMS (Citation14).
Physicians providing clinical oversight of air medical services should collaborate with both out-of-hospital and hospital-based stakeholders to establish specific indications for and limitations to utilization that align with local and regional system and patient needs.
These utilization criteria should be widely promulgated to all stakeholders, undergo regular review for adherence, receive periodic updates, and address both scene and interfacility transport.
Air medical services transport destination determination decisions should be based on specific guidelines established by air medical services and hospital stakeholders to ensure medically appropriate distribution of patients to specialty care, including trauma, stroke, cardiac, pediatric, obstetric, and other specialty care hospitals. The effects of insurance-based networks of care must be considered so as to avoid unnecessary increased costs of care to the patient.
Except in situations where patients are in extremely remote locations far from definitive care, air medical services should not be used solely to allow ground EMS to remain in their primary service area.
Air medical services clinicians in the field, supported by concurrent consultation with physician oversight, should be empowered to redirect patient transport to ground EMS when air medical transport does not meet at least one of the three primary goals of air transport, independent of financial consequences to the air medical services agency.
Air medical services are an important resource that can be used in disaster and mass casualty incidents as part of an integrated community approach.
Air medical services agencies should be involved in preparedness planning and exercises as part of a multi-disciplinary emergency and disaster preparedness and response plan.
Air medical services clinicians should be encouraged to collaborate with and/or participate in local, regional, and national disaster response and support teams.
This position statement and resource document highlight the purpose of air medical services and provide guidance regarding its appropriate and safe use for patient care, its integration into the health care system, and the importance of making evidence-guided utilization decisions.
Introduction
Air medical services, encompassing both helicopters (HEMS) and fixed-wing aircraft, must be utilized in a clinically effective, safe, and fiscally responsible manner. Such utilization includes selecting patients who are most likely to benefit while also taking steps to ensure the air medical services mission does not place patients and air crewmembers at undue risk for injury or death. Fiscally responsible utilization helps to ensure the most clinically appropriate and least costly transport resources (ground versus air) are used to meet the patient’s clinical needs.
Patient Benefit from Appropriate Use of Air Medical Services
The decision to use any form of medical transport first requires consideration of the clinical needs of the patient and the ability of available medical resources to meet those needs both before and during transport. Patients may derive benefit from air medical services when one or more of three primary patient-centered needs are identified and met:
initiation or continuation of advanced or specialty care and expertise that is not otherwise available locally from hospital or ground EMS resources;
expedited delivery of the patient to definitive care for time-sensitive interventions; and/or
extraction, evacuation, and/or rescue from environments that are difficult to access due to geography, weather, remote location, distance, and other factors that limit timely access to a patient or transport by ground EMS.
Additionally, for some non-emergent patients, air medical services resources, usually via fixed-wing aircraft with one or more accompanying medical attendants, may be used to repatriate a patient from a distant location to a facility closer to the patient’s home in order to access a higher level of care, provide continuity of care from the patient’s home health care system, and/or to access the patient’s local family, social, and medical support community.
Section 1: Clinical, Temporal, and Geographic Considerations
For any given patient, the clinical experience and expertise of the individual hospital-based or field personnel making an air medical services utilization decision may vary significantly. Objective data should be used whenever possible to guide utilization decisions, including use of diagnostic information such as vital signs or 12-lead EKGs, as well as decision support tools such as validated risk assessment or patient acuity scores calculated from information that is readily available to the requesting personnel (Citation15–17).
Unfortunately, utilization decisions are often encumbered by lack of immediate access to diagnostic tools and information that could otherwise help discriminate between patients who would benefit from and those who would not benefit from either air-delivered care in transit or earlier access to definitive hospital-based interventions. Instead, decisions to use air medical services are often driven by subjective perceptions of potential unknowns rather than by what limited objective data are known. Absent specific objective parameters on which to judge benefit and risk, perceptions of the potential “worst case scenario” can drive decision making. Though at least one scoring system for air medical services utilization has been validated based on straightforward prehospital criteria, there is clearly a need for development and adoption of other objective decision support tools to support utilization decisions (Citation17–20).
Several research limitations have restricted the volume of literature available to guide appropriate utilization decisions made by both hospital and EMS clinicians. Performance of randomized clinical trials comparing air to ground EMS care and transport is limited by the ethical challenges of randomizing patients with known time-sensitive conditions to study arms that could potentially delay delivery to definitive treatment. Secondly, methodology that focuses primarily on the type of transport vehicle used (ground versus air) or the speed of transport fails to recognize the effects of the type and scope of clinical care provided in transit. Furthermore, significant heterogeneity exists across air and ground medical crew staffing models, ranging from single clinicians to multiple medical crewmembers with credentials ranging from the EMT to physician. Crews may also include other specialized clinicians such as perfusionists or respiratory therapists. This varied staffing and the heterogeneity of the resultant clinical care makes it difficult to aggregate or extrapolate study results across specific air medical services agencies or systems of care and may also explain why studies that have compared air to ground EMS transport have provided mixed and even contradictory results (Citation21–34). Despite these limitations, there is evidence in the literature demonstrating the benefits of air-based care for specific patient populations as described below.
Trauma Emergencies
Use of rotor-wing/helicopter air medical services (HEMS) responding directly to the scene for patients with traumatic injuries represents the area with the largest body of supporting evidence in the civilian setting. As far back as 1983, Baxt and Moody showed decreased trauma mortality in patients transported directly from a trauma scene by a single HEMS service staffed with specially trained EMS clinicians when compared to ground transport (Citation35). The authors further validated their findings by applying their study methodology on an even broader scale to seven independent air medical services operating in several regions throughout the United States with a variety of crew configurations. Each of these services were found to achieve reductions in predicted mortality when providing care of trauma patients from the scene (Citation36).
Some of the benefit of air-based care for trauma patients may be dependent on geography and distance from definitive care. Numerous studies have demonstrated that air medical services improves survival in suburban and rural settings when compared to ground transport for various trauma patient populations (Citation19–24, Citation37–40). However, the same benefit has not been consistently conferred in direct-to-scene air response in urban settings (Citation25, Citation26, Citation41). One retrospective study identified a potential survival benefit for urban penetrating trauma patients when HEMS was used in direct-to-scene response. It is unclear whether the benefit is attributable to delivery of a specialized EMS physician to the scene, care provided in transit, or faster delivery to definitive care than ground EMS (Citation27).
Earlier studies showed improved survival benefit when air medical services is used for interfacility transfer of trauma patients from hospitals with limited diagnostic, interventional, and critical care resources to designated regional trauma centers (Citation28, Citation29), while more recent studies are equivocal with regard to benefit from air medical services in interfacility transfer (Citation42, Citation43). These patients are at least perceived by the transferring clinicians to potentially benefit from specialized testing or time-sensitive interventions that are not available at the transferring facility, advanced care in transit that is not available from local ground EMS resources, or perceived shorter interfacility transfer times. It is important to distinguish here that the level and quality of care delivered to trauma patients during transfer may be more important than speed. A large multicenter study of isolated severe traumatic brain injury patients transported by helicopter showed improved survival despite longer transport time. This finding suggests that patients in this population primarily receive greater benefit from the earlier initiation of critical care interventions by air medical services clinicians, rather than from the shorter transport times potentially achieved by air (Citation44).
Several studies have attempted to identify objective criteria on which to base use of air medical services for trauma patients. A multidisciplinary panel of experts in trauma, EMS, and evidence-based guideline development created recommendations for the selection of prehospital trauma patients who would most likely benefit from air versus ground transport (Citation45). The panel recommended that triage criteria for all trauma patients include anatomic, physiologic, and situational components to risk-stratify injury severity and guide decisions as to transport modality and destination. More recently, several physiologic criteria have been shown to be predictive of higher odds of mortality and/or need for emergent hospital-based interventions in trauma patients transported by helicopter (Citation17, Citation46, Citation47). The Air Medical Prehospital Triage Criteria (AMPT) Score development and validation studies found that patients with two or more of the following physiologic and anatomic criteria benefit from HEMS transport: GCS <14, respiratory rate <10 or >29, flail chest, hemo/pneumothorax, paralysis, and multisystem trauma (Citation48–50). Interestingly, these patients had increased survival regardless of whether air transport actually shortened time to a trauma center, once again suggesting that the critical care assessment and management provided in transit may play a more important role than the type of vehicle used to transport the patient or the actual duration of the transport interval of patient care (Citation18). Other prehospital scoring systems have been proposed that can guide decision-making (Citation51, Citation52).
Medical Emergencies
Decisions to use air medical services to care for patients with specific medical conditions are supported by varying levels of evidence.
Cardiovascular Emergencies
ST-segment myocardial infarction (STEMI) has a well-established relationship between time to intervention and improved patient outcomes (Citation53). Bypass of non-interventional facilities and/or long distance interfacility transfer of patients for percutaneous coronary intervention (PCI) has shown benefit over locally administered fibrinolytic agents when first medical contact to balloon time is less than 90 minutes (Citation54, Citation55). In addition, in rural areas air medical services may be also able to provide more advanced cardiac monitoring and interventions during transport than local ground EMS can provide. Several studies have shown mixed results when evaluating whether HEMS transport, either from a scene or for interfacility transfer, can help achieve the goal of performing PCI within 90 minutes of first medical contact compared to ground EMS transport (Citation56–60). In general terms, air transport can help achieve shorter first medical contact to device times compared to ground transport for transport distances greater than 30 mi (50 km). However, for transport distance less than 30 mi (50 km), time to intervention is longer for air-transported STEMI patients compared to ground (Citation61). While achieving faster time to definitive intervention appears desirable, it is important to specify that based on current evidence, total ischemic time less than 120 minutes provides maximum patient benefit (Citation62, Citation63), and thus to be clinically meaningful, the decision on use of mode of transport should focus on achieving this target. When either air or ground EMS can achieve a total ischemic time less than 120 minutes, utilization decisions can be guided by evidence that the risk of 1-year mortality from STEMI is increased by 7.5% for each 30-minute delay to device (Citation63, Citation64). This suggests that if air transport can decrease patient time to device by at least 30 minutes, STEMI patients may enjoy an enhanced survival benefit, though no studies have directly evaluated this premise. Currently, no specific literature exists assessing change in STEMI patient outcome when the difference between air and ground first medical contact to device times is less than 30 minutes.
In addition to PCI, other cardiac care interventions such as intra-aortic balloon pumps, ventricular assist devices, extracorporeal cardiopulmonary resuscitation, extracorporeal membrane oxygenation, and post-cardiac arrest care are becoming regionalized. Air medical services may help expand access to these interventions via transport of specialty teams and equipment to the patient, providing interfacility transport care of patients being supported by these devices, or expediting access to these interventions from the field, but whether it confers an outcome benefit is currently unknown.
A specific subset of patients that are sometimes considered candidates for air medical services are those in cardiac arrest. Air scene response for cardiac arrest should typically be rare; however, use of air medical services for transport of cardiac arrest patients with return of spontaneous circulation may improve outcomes and should be considered for primary cardiac events (Citation65). Historically in-flight care of patients in cardiac arrest has proven difficult, and the inability to provide effective high-quality manual chest compressions in flight has been demonstrated by several studies (Citation66–71). Not only do in-flight manual chest compressions generate inadequate perfusion, but unrestrained crew members performing manual chest compressions in flight pose a significant safety risk. However, demonstrated feasibility of mechanical chest compression devices in the air medical services environment, with associated higher rates of return of spontaneous circulation, lower no-flow-fractions, and improved mental performance of crew members when compared to manual chest compressions is shifting the reluctance to transport selected patients in cardiac arrest by air (Citation72, Citation73). Additional study is necessary to determine whether care of cardiac arrest patients with in-flight use of mechanical CPR affects survival and functional outcomes (Citation72, Citation73). Regardless of availability of more effective in-flight CPR strategies, the need for prudent application of guidelines for withholding or terminating resuscitation, such as those developed by NAEMSP and other specialty groups, remains essential (Citation74–76).
Neurologic Emergencies
Acute stroke syndromes are common reasons for transport of patients by both ground and air EMS, and regionalization of stroke care is increasingly prevalent. Similar to STEMI, limiting ischemic time improves outcomes for stroke, yet optimal strategies for both achieving this goal and the timeline to do so continue to evolve.
Unlike STEMI patients who can be differentiated from those with other conditions in the field using objective tools available to EMS clinicians, such as 12-lead EKG, there are significant limitations to the ability of EMS clinicians to differentiate patients with acute neurologic deficits between stroke and non-stroke conditions, to differentiate large vessel occlusion (LVO) strokes from other strokes, and to differentiate ischemic from hemorrhagic strokes (Citation77, Citation78). Prehospital stroke patients differ significantly from those encountered in the interfacility setting, mainly in that interfacility patients have undergone evaluation and diagnostic differentiation at a hospital and are being transferred for specialty care (Citation79). These differences represent significant informational gaps that affect not only rates of air medical services use but also the ability to compare outcome measures across prehospital and interfacility patient groups.
Historically, stroke systems of care promoted the “drip and ship” approach of routing suspected stroke patients from the field to the nearest hospital capable of performing computed tomography imaging and identifying ischemic strokes, followed by initiation of systemic thrombolytic infusions and then transfer to tertiary hospitals for neurologic specialty care. While Chalela et al. were able to show that air medical services could safely transport acute stroke patients receiving thrombolytic agents, a later study by Olson et al. subsequently raised the question of whether air medical services provided any significant benefit to these patients as they stated: “Air transfer of patients with acute ischemic stroke treated with thrombolysis does not seem to impart any benefit to patient outcomes when compared with ground transport.” (Citation80, Citation81) More specifically, considering the time-sensitive intervention, initiation of systemic thrombolysis, had already been started prior to air transport, Olson questioned whether these patients received any benefit of transport by air when being transferred to tertiary care as there was no longer a time-sensitive nature. Further, they noted there was no difference between transport groups with respect to rate of complications, time to procedures, length of ICU stay and hospitalization, modified Rankin Score at discharge, and 24 hour and 30 day mortality. However, the Olson study did not take into consideration that air medical services might still be necessary to either provide a higher level of care than ground EMS during interfacility transport, including continued infusion of thrombolytic medications or management of life-threatening complications of systemic thrombolytics, or that air transport might help limit out of hospital time in these critically ill patients. Further, activation-to-destination times for ground and air transport in this study were on average within 15 minutes of each other, which limits the ability to extrapolate the study findings if the difference between ground and air transport exceeds 15 minutes. It is also important to note that the Olson study was published in 2012, prior to the introduction of today’s advanced endovascular stroke therapies, and thus fails to account for potentially important time-sensitive gains that air medical services might achieve when transporting patients who are candidates for such therapies.
More recently, patients experiencing LVO strokes have been shown to benefit from rapid access to invasive neuro/endovascular interventions (with or without thrombolysis) over use of systemic thrombolysis alone (Citation82–84). Similar to the evolution of STEMI care over time, the care of LVO stroke is transitioning from the current “drip and ship” strategy to an approach in which the ground EMS team providing 9-1-1 response considers bypass of local hospitals that lack interventional therapies in favor of direct transport to primary and comprehensive stroke centers capable of performing endovascular therapies, even if transport time is extended 60 minutes or more (Citation85, Citation86). A recent evaluation of seven different LVO prediction algorithms in use in the EMS setting showed wide variability in sensitivity (38–62%) and specificity (80–93%), high negative predictive values (95–96%), but poor positive predictive values (21–32%), with no specific algorithm outperforming the others across all of the measures of predictive value that the study evaluated (Citation87). Further, the best performing algorithm (RACE, PPV 32%) unfortunately also had the lowest prehospital feasibility score (78%). Additionally, even applying the best-performing EMS LVO prediction algorithm to advise bypass of patients directly to comprehensive stroke centers would have resulted in significant rates of overtriage in this study (Citation88). The lack of existing easy to use prehospital diagnostic tools or screening algorithms with sufficient sensitivity and specificity to effectively differentiate likely LVO from non-LVO ischemic strokes or hemorrhagic strokes remains a weak point in stroke hospital bypass strategies (Citation87, Citation89, Citation90). Until such differentiation can be achieved in the field as reliably and easily as identification of STEMI, and with a similar level of precision and accuracy, the effect of using air over ground EMS to expedite transport of suspected LVO stroke patients directly from the scene to interventional stroke centers will remain unclear. Use of prehospital EEG to provide this level of differentiation is currently being investigated (Citation91–94).
While overall the use of air medical services for stroke has been shown to be cost-effective when examined per quality adjusted life year, more study is needed to better describe the specific subtypes of suspected stroke patients who are most appropriate for aircraft-based care and transport (either from the scene or interfacility) (Citation79, Citation83, Citation95). Currently, unless a stroke patient requires more advanced care in transit than ground EMS can provide, or unless a stroke patient has a definitive time-sensitive intervenable LVO, it is unclear which additional stroke patients might benefit from air medical services. In summary, further research is needed to help inform how air medical services should be incorporated into regional stroke destination protocols.
Obstetric and Neonatal Emergencies
High risk obstetric and neonatal patients often require fetal monitoring and other interventions during transport that exceed the equipment and critical care capabilities of local ground EMS resources, which suggests a potential justification for use of air medical services for these patients. However, there is a paucity of research focused on appropriate patient selection and effects of air medical services utilization on patient outcomes for both the maternal and neonatal populations (Citation96–98).
In general, transfer of a gravid patient with a viable fetus is preferable to transferring the mother and neonate after delivery, as prenatal transfer generally results in better infant outcomes (Citation99–103). In high-risk obstetric patients, however, this preference must be balanced against the significant challenges inherent in potential in-flight delivery of a newborn. For selected cases, it may be appropriate to use air medical services to deliver a specialty care team to the referring facility to stabilize the gravid patient and/or to provide care for the newborn and then continue providing care during ground transport, rather than using air medical services to transport the high-risk gravid patient (Citation104).
Similarly, in the case of critically ill newborns who require transfer, initial stabilization of patients at referring institutions is generally preferable to rapid interfacility transfer of an unstable neonate (Citation105). Similar to the obstetric patient, air medical services may be used to bring specialty care resources to the patient for pre-transfer stabilization, followed by specialty neonatal care during transport either by ground or air. Scoring tools such as the Transport Risk Index of Physiological Stability (TRIPS) score or the Risk Score for Transport Patients (RSTP) aid in risk-stratifying neonates and may help support decisions on the best mode of patient transport (Citation106–108).
Other Medical or Surgical Emergencies
The use of air medical services in other high-acuity or time-sensitive conditions has not been well studied. Examples of such patients include those at risk for airway deterioration (angioedema, epiglottitis, inhalation injury), those with emergent need for medical therapies (hemodialysis, hyperbaric oxygen therapy), those needing emergent surgical intervention either in-hospital (aortic dissections/aneurysms, necrotizing fasciitis, limb reimplantation) or in the field (amputation for entrapment), those requiring other nuanced critical care (complex mechanical ventilation, continuous titration of vasoactive medications), or those requiring interventions that cannot be performed at the referring facility. If appropriate ground-based or local critical care transport resources are not available to provide care for these patients, transport by an air medical services agency with such capabilities may be in the patient’s best interest, though there are no organized data on these patient populations.
Transport of Special Resources
In some cases, the primary clinical benefit to the patient occurs when air medical services is not used to transport a patient, but instead is used to transport special medical resources such as personnel, equipment, blood, medications, or organs to the scene or hospital. This might include delivery of supplies in a large mass casualty incident or disaster, delivery of specialized physicians/teams to perform field surgical procedures on entrapped patients, or potentially to help coordinate transport of organ procurement and transplant teams (Citation109, Citation110). There are no organized studies of these services.
Temporal and Geographic Considerations
In the absence of specific air medical services clinical care needs, the decision to use air instead of ground EMS may be driven by the perception that air transport will deliver the patient to definitive care more rapidly. Whether air medical services can actually achieve a clinically significantly shorter time to intervention is multifactorial and may be associated with significant financial costs (Citation111). It is important to recognize that transport by air may require additional time spent on certain time-consuming tasks that may take longer than similar tasks found in the ground transport realm or that are not necessary. These tasks can include differences in the time necessary to prepare to respond, to load and secure patients in the vehicle, to perform preflight safety checks, to depart the scene, to unload the patient, and to transition between the vehicle and the hospital bed. Although air medical services can achieve faster in-transit time than ground EMS for a given distance, these additional air-based time costs can usurp any gains in travel time for air medical services, particularly for shorter transport distances, and especially if ground transport is necessary to move the patient between the scene or referring facility and the aircraft, and/or between the aircraft and the receiving hospital.
It is also important to recognize that distance is an indirect measure of time. Construction, severe ground-traffic congestion, or spontaneous events such as riots or civil unrest may also cause sufficient disruption of ground transport routes to justify use of air medical services to transport patients over the disruption to an appropriate hospital. Similarly, ill or injured hikers, hunters, mountain sports enthusiasts, boaters, or campers in remote or geographically inaccessible areas may benefit from use of air medical services for prompt and safe extraction from areas poorly accessible by ground, even if they do not require critical medical interventions. Use of air medical services can also be critical to the movement of patients in developed areas when significant limitations of normal transport infrastructure arise. Such circumstances may include damage to typical ground transport routes caused by natural disasters like hurricanes or floods.
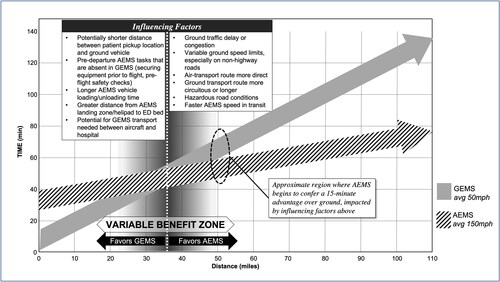
In select cases in Europe, helicopters have been found to reduce transport times by 75% while the costs per transfer, on average, doubled. However, that study did not lead to a consensus on cost versus benefit for HEMS transport (Citation112). A comparison of air and land ambulances in Ontario showed that transport times for land ambulances were significantly shorter over distances <60 mi (<100 km) and equivalent for distances of 60-150 mi (100 km to 250 km), which reflects the additional fixed task time needed for HEMS transport (Citation113). provides further conceptual illustration of the relative differences between ground and air EMS over given distances when taking these fixed and variable times into consideration.
Figure 1. Conceptual Model* of the relationship of GEMS and AEMS time in transit from patient loading (“Time 0/Distance 0”) to emergency department bed arrival. (*based on authors' consensus)
Certain rural and frontier locations with very limited medical resources and capabilities are hundreds or thousands of miles from advanced medical care, and air medical services may be the only practical resource to help transport these patients to a higher level of care (Citation114–116). Though some of these areas are accessible by roads, the transport interval between facilities using ground vehicles may be half a day or more. In these cases, fixed-wing air medical services may be used when transport distances or weather conditions are beyond the capability of HEMS. For this reason, fixed-wing services (either private or commercial) are frequently used for medical repatriation of the sick and injured, providing a range of services from medical escort/attendant to critical care.
Section 2: Risk Identification and Safety Considerations
Risk Identification and Mitigation
The choice to use air medical services should always be driven by the three main patient-centered goals outlined above, and their potential to provide patient-based clinical benefits versus the potential the mission will expose the patient and crew members to certain risks for harm. This risk-benefit assessment must also account for the operational and logistical limitations of available hospital, as well as available air and ground EMS resources. Air medical services may be one potential solution for a given clinical or operational problem, but may not be the best solution. Alternatives, such as local hospital-based care supported by telehealth consultation, provision of care and transfer by non-local ground EMS resources, or ground transport to a nearby non-specialty hospital for interim stabilization, must also be considered (Citation117). Appreciation of local and regional EMS and hospital capabilities and regional transfer patterns and protocols must all be included in the utilization schema for air medical services. Every air and ground EMS utilization decision must include a risk versus benefit analysis for both the patient and the system from both safety and economic perspectives (Citation118).
Safety Factors
The final decision to deploy an air medical resource most importantly demands a favorable safety profile from both an aviation and patient perspective. For a flight to receive a “go” decision, all crew members must agree to the flight without coercion. If at any point the mission has become potentially unsafe, each crewmember should be empowered to request that the mission be aborted.
From an aviation perspective, the safety assessment includes an evaluation of real-time and forecasted weather conditions considered in the context of the capabilities of both the aircraft and the pilot. Inclement weather is one of the main limiting factors for air medical services missions and may include issues with visibility, cloud ceiling, precipitation, wind, and temperature (Citation119–121). Duty hour restrictions for crews and pilots are also important safety measures that affect air medical services availability for missions. Further, pilots must use accurate patient weight, current and predicted fuel levels, and crew weight to determine the safety profile of the mission. In order to shield pilots from inappropriate pressure to accept a mission, pilots should remain insulated from the clinical nature of the flight request until after they have decided conditions are safe for flight (Citation122).
In circumstances where weather or other risks prevent a safe air response or transport by air, air medical services crews might coordinate with ground EMS to perform an “air-by-ground” response. In these cases, the air crew responds to the scene or transferring facility either by air or ground vehicle, initiates patient care, and then continues provision of patient care while using a ground vehicle to transport the patient to definitive care safely. These missions may require special collaboration between local air and ground EMS counterparts and should be pre-planned whenever possible.
Even if conditions are favorable for a flight from an aviation perspective, certain patient-based factors may pose a threat to the crew and the safe operation of the aircraft. These may include girth or weight restrictions which restrict the use of appropriate in-flight restraints, or patient intolerance to barometric pressure changes. In addition, patients who are contaminated with certain chemical, radiological, and/or biological hazards, and those who are exhibiting agitated or violent behavior, may also be deemed to be unsafe to fly (Citation123). In the case of contaminated patients, the personal protective equipment required to protect the air crew may interfere with the safe operation of the aircraft. When a patient exhibits aggressive or agitated behaviors, placing the patient in the confined space of the aircraft in close proximity to the pilot and aircraft controls could result in catastrophe if the behaviors escalate to physical violence in flight. This circumstance creates a potentially conflicting dynamic between the risks and benefits posed to the patient and the flight crew: the added potential medical risk associated with administration of pharmacologic interventions to reduce agitation and/or achieve deep levels of sedation and the potential related need for invasive airway management versus the benefit to the crew and patient of mitigating the risks of injury or death from an aircraft crash that is caused by a physical altercation in flight. In these circumstances, ground transport may be a safer alternative as the patient is more isolated from the vehicle controls and vehicle operator while the vehicle is in motion and because ground vehicles can more rapidly stop compared to executing emergency landing maneuvers of an aircraft. These aspects help lessen the risk of a fatal crash if the patient becomes physically violent in transit. Additionally, while use of sedative medications may still be necessary to effect safe ground transport of potentially or actually violent patients, the ground transport environment may not require use of the deeper levels of sedation needed to effect safe transport in the air environment.
Mission Refusals
It is not uncommon for an air medical services agency to turn down a mission request when any of the aforementioned safety concerns are present, or when the agency does not have the clinical capabilities to care for the patient. Support of such mission “turndown” practices are critical to the safe operation of an air medical services agency and system. However, the entity requesting the mission (a hospital or transferring clinician, for example) likely still needs a transport to occur. An unmet patient transport need may result in two behaviors that can have a significant negative effect on safety by increasing the risk for injury or death of patients and crewmembers if full and transparent communication is not maintained. These behaviors are “helicopter shopping,” and “reverse helicopter shopping.” Each of these behaviors has been noted by the National Transportation Safety Board (NTSB) to be associated with and directly contribute to multiple air medical services crashes that have resulted in fatal or severely life-altering injuries to crewmembers and patients (Citation124). Factors that may contribute to both helicopter shopping and reverse helicopter shopping behaviors include the competitive market among air medical services agencies for patient volume, the development of “preferred provider” agreements between hospitals and local air medical services vendors, an air medical services agency/vendor corporate culture that incentivizes air crews to accept flights in order to achieve arbitrary monthly mission quotas, or workplace culture that pressures air crews to accept missions irrespective of the reasons another air agency turned down the mission request (Citation125).
Helicopter Shopping
“Helicopter shopping” is defined as the practice by a hospital or transferring clinician of making sequential calls to a variety of air medical services agencies while attempting to secure a response that may be limited by weather, distance, or other safety factors, and landing zone availability (Citation12). If safety factors dictate that one company cannot safely complete a mission, the entity requesting the transport needs to recognize that the same safety considerations will often preclude completion of the mission by another company. It is therefore critical that if an air medical services agency declines a flight, the entity requesting transport and/or the air medical services dispatch coordinating center inform all subsequent air agencies of both the prior turndown and the reasons for the refusal (Citation126). In some cases, interagency variation in the clinical and aircraft capabilities of competing programs operating in overlapping service areas can result in one agency being able to perform a patient transport safely despite that mission being refused by a prior agency. For example, one agency may be enhanced vision (EV) equipped and/or instrument flight rules (IFR) capable, and thus be able to safely take a night or low-visibility mission that the first, non-EV/non-IFR agency could not. Further, weather conditions that may prevent one air service based at a certain geographic location from accepting a mission may not prevent a different flight service with a base in a different geographic location from safely accepting the mission. In any of these circumstances, requesting entities must supply subsequent agencies with all prior refusal information in order to allow those subsequent programs to fully determine if the mission fits within their capabilities and safety profiles. Otherwise, a program may unknowingly accept an unsafe flight due to lack of awareness of the previous refusals. For this reason, agencies should always inquire about prior refusals and complete a full safety evaluation of every mission prior to acceptance (Citation118). Multiple position papers on the topic of helicopter shopping have been published by professional organizations within the medical aviation community and generally agree that complete communication of mission safety concerns is vital (Citation12, Citation127).
Reverse Helicopter Shopping
Whereas ‘helicopter shopping’ is a requesting entity practice, ‘reverse helicopter shopping’ is a practice of the air medical services program itself (Citation127). Reverse helicopter shopping occurs when an air agency performs active surveillance for missions turned down by other agencies, and then proactively contacts the requesting entity to offer transport resources as opposed to waiting for the entity to request that program’s response. Reverse helicopter shopping was named as a potential cause in the crash of N191SF in 2019 (Citation125). This practice carries with it many of the same factors as helicopter shopping that increase the risk of the mission: lack of complete knowledge and understanding of the reasons the mission was turned down by another air agency and financial drivers of mission acceptance. In addition, given the requirements of EMTALA to ensure that a transport occurs with “qualified personnel and appropriate equipment”, both reverse helicopter shopping and helicopter shopping may carry liability risks for the referring clinician if a bad outcome results and it is determined that the agency selected was not capable of handling the transport safely (Citation128).
Resultant Policy Changes
The Commission on Accreditation of Medical Transport Services and the National Accreditation Alliance of Medical Transport Applications, the two primary medical transport accrediting organizations in the United States, both require accredited programs to develop policies that discourage helicopter shopping by EMS agencies and hospitals (Citation129, Citation130). These standards call for policy language that specifically addresses how an air medical services program is to interface with other local programs after mission refusals. The Federal Aviation Administration (FAA) has communicated with state EMS directors regarding the problems of both types of shopping and now requires certificate holders to “establish and document and include in their FAA approved preflight risk analysis a procedure for determining whether another helicopter air ambulance operator has refused or rejected a flight request” in order to minimize the communication risks inherent to both helicopter shopping and reverse helicopter shopping (Citation124).
Economic Factors
In addition to the safety risks present for each particular air medical services mission, existing billing and insurance reimbursement models may introduce significant financial burdens to the patient and should be considered when contemplating air versus ground transport.
The financial cost of air medical services care and transport can be significantly higher than similar care provided via ground EMS (Citation112, Citation131). Some of the differences in cost of care delivery can be attributable to higher operating costs for aircraft versus ground vehicles, higher wages for the higher skill level of some clinicians, and lower utilization ratios for air medical services. Another reason for the fee difference in equivalent care between air and ground EMS is that ground EMS billing and reimbursement is restricted by federal programs that limit the amount that can be billed and/or reimbursed for various levels of EMS care and that restrict operational cost recovery to a flat per-loaded-mile rate. In contrast, while clinical portions of billing by air medical services agencies are regulated by the same federal programs, other portions of air billing practices are viewed not as a health care entity but instead as an air-transport entity and as such their operational billing practices enjoy substantial protection from government regulation by the Airline Deregulation Act of 1978. This is one reason there is a substantial variance in the charges/billing practices across independent, hospital-based, and for-profit air medical services agencies.
Several publications have investigated the cost-effectiveness of air medical services for various conditions, including papers by Delgado (trauma), Silbergleit (stroke), Gearhart (trauma), Madiraju (trauma), and Taylor (systematic review) (Citation9, Citation95, Citation111, Citation112, Citation132). Perhaps as best summarized by Taylor, the cost and effectiveness of air medical services “varies considerably between studies,” are affected by “variations inherent in the health systems in which [air medical services] operate,” and ultimately assessments regarding cost-effectiveness must be made at a local level and must be “tailored to account for local system factors.” (Citation112)
In cases where air medical services utilization provides clear clinical benefit to the patient, especially when viewed through the lens of accomplishing any of the three primary goals, the higher cost is usually justifiable. In these situations, air medical services are deemed “medically necessary” and in most cases, will be fairly covered by existing insurance products. It is critical that clinicians across the span of the episode of care, including field or hospital clinicians and the air medical services clinicians, clearly document in the patient’s clinical record not only why the use of air medical services is medically necessary using language focused on how it will achieve any of the three primary goals, but also why the sending facility was unable to manage the patient and what receiving facility resources were anticipated or required.
Situations can occur where ground EMS or hospital clinicians and air medical services clinicians disagree as to whether air resources are necessary for care and transport of the patient. In such situations, referring clinicians should be encouraged to discuss the transport with the flight program’s physician medical director to help better define the risk/benefit profile for the patient. This approach may help avoid settings where justification supporting benefits of air medical services to the patient are weak or absent, which can place the mission at risk of being declared “medically unnecessary” by the insurer, resulting in denial of coverage by insurance products and transfer of the financial burden directly to the patient. Additionally, such conversations may help discourage further helicopter shopping practices by the requesting party.
Provision of consistent availability of ground EMS for a given community can be challenging when resources are scarce, such as the case in many rural and frontier areas. Air medical services may be called to help maintain local ground EMS availability to cover a primary ground response area. In cases where the flight is otherwise medically unnecessary, such practices unfairly shift the cost of ensuring local ground EMS coverage from the community to a single patient and the air medical services agency, often at economic costs to the patient that would be significantly higher than the cost to the local community of more consistently securing adequate ground EMS resources. This practice is strongly discouraged, as it creates significant financial burdens to patients and does not represent appropriate or cost-efficient resource management of air or ground EMS at the local or system level. Ideally these situations can be avoided when appropriate system integration and utilization planning occurs between applicable stakeholders.
Section 3: System Integration and Quality Assurance Considerations
Air medical services integration into local and regional health care systems requires a multifaceted approach with engagement of appropriate stakeholders, oversight and protocol development addressing the air medical services interface with the local EMS system, a robust coordination and communication practice, and vigorous quality assurance and utilization review.
Stakeholders
Appropriate and effective use of air medical services begins with coordinated integration into the broader EMS and health care system. To achieve this level of integration, stakeholders must understand the capabilities of various air medical services resources available to the region, define the role of air medical services within a given geographic area, and develop plans to help coordinate interactions, collaboration, and communication pathways between air and ground EMS, other emergency response services, emergency communications systems, and hospital-based resources.
Physician medical directors and operational directors must be involved in discussions on how to integrate air medical services into the local EMS system, as these leaders best understand the abilities, limitations, and resources available to local air and ground EMS that strongly influence utilization decisions. Medical directors should meet the guidelines for flight physicians and air medical directors as outlined in the NAEMSP position statements Flight Physician Training Program—Core Content and Physician Oversight of Air-based EMS (Citation14, Citation133). Similar guidelines for air medical directors are also outlined by the Air Medical Physician Association (Citation134). Likewise, fire and law enforcement officials must be involved in integration discussions due to their key roles in requesting air medical services response and in coordinating safe landing zone operations. Hospital clinicians and administrators can contribute in-depth knowledge of hospital capabilities to inform appropriate triage and destination choices for specific patient populations. Regional medical advisory boards, state advisory boards, and regulatory agencies ensure that the integration of air medical services is equitable, free from financial bias, and compatible with applicable laws, and functions with other regional networks including STEMI, stroke, trauma, and other specialty care. Finally, aviation officials provide essential input regarding the capability of the local aviation system to support incoming and outgoing air traffic at any time, including use of IFR approaches. This list is not exhaustive; every EMS system should include further participants with system-specific skills and knowledge as necessary.
Oversight of the Air Medical Services – EMS System Interface
Stakeholders should work to identify and adopt objective, evidence-based criteria to drive decisions to request air medical services for both scene response and interfacility transfers based on the clinical, safety, and economic considerations discussed previously. When such objective criteria are not able to be used, education should be provided to personnel who are in positions to request air resources regarding the local air and ground EMS response capabilities and limitations, and air medical services utilization, inclusion, and cancelation criteria (Citation126, Citation135). EMS oversight bodies must establish protocols addressing authorized requestors, dispatching, communication requirements, and quality assurance. State governments will likely provide the majority of the oversight, rules, and regulations for air medical services utilization. Minimal training requirements for health care clinicians on air transport services in that system should also be clearly presented.
Authorized Requestors
Air medical services resources are expensive, both in monetary amounts and in potential risk to life. Careful consideration of who is authorized to request these resources is encouraged to avoid inappropriate requests. In addition, requests that are not indicated may not be financially prudent for the air agency, and repeated inappropriate flights may result in loss of the air agency to the local community. Authorized requestors for air transport resource activation and dispatch include, but are not limited to, on-duty/on-scene first responders (i.e., EMS, law enforcement, and firefighters), local EMS medical directors, an appropriate medical officer within the incident command structure, direct medical oversight physicians, and hospital-based clinicians who determine a patient requires transfer. Authorized requestors should be trained regarding the air medical system’s capabilities, limitations, and appropriate use based on established protocols. Training must include timely cancelation of air resources should on-scene personnel realize that those resources are no longer needed, as misuse of HEMS is thought to primarily occur during scene calls (Citation135). This is especially important in jurisdictions or agencies that may use auto-launch policies, which decrease scene times but likely increase overuse and over-triage. The use of decision support tools may be useful in these circumstances.
In consultation with other involved parties, the most highly trained and experienced authorized requestor present at the time when the realization is made that air services are indicated should be the one to activate air resources. However, only training one person within an EMS system (e.g., only the fire chief, or only the local EMS medical director) to be an authorized requestor can result in significant delays of activation of time-critical air resources and should be avoided. Ground EMS clinicians should be trained adequately so that air resources may be requested as soon as feasible.
Coordination and Communication
Air medical services activation and dispatch should be coordinated with the ground emergency dispatch system by a centralized communication or dispatch center. Coordination and centralization will reduce unnecessary activation and dispatch, particularly if multiple air medical services agencies are operating in the same coverage area. Additionally, a centralized dispatch system can help ensure that the “soonest available” and appropriate air medical services unit is dispatched.
Failure to coordinate communications has led to catastrophic consequences in multiple incidents (Citation136, Citation137). Policies and procedures at the state, regional, or local level should be established to guide the appropriate selection and dispatching of air resources. An even greater need for coordination or centralization of dispatching is necessary when multiple air units are necessary (e.g., large disasters or multiple casualty incidents) (Citation138, Citation139). In these situations, dispatch and communication specialists should have a method available to organize and manage air medical team responses while promoting scene safety and dispatching the appropriate number of units.
Once an air resource is activated and dispatched, the communication system should promote the reliable and accurate flow of information among dispatch centers, air resources, ground EMS, public safety/security, local air traffic control, and the receiving facility. Scene safety is paramount, and communication with scene crews and hospital staff should reinforce this. Maintaining scene safety will require constant, reliable, and redundant communication between ground crews and pilots. On-scene personnel and hospital personnel should be educated about aviation safety and communication requirements during takeoff and landing, especially in hot on/offload situations, and the aviation manager of the air medical services agency should consider offering this training.
Reliable communication is also vital to ensure appropriate medical care and patient handoff. Communication with ground crews, the transferring clinician, and appropriate direct medical oversight should be available to the medical crews during transport (Citation140). Communication with the receiving hospital prior to landing is preferred if the patient’s situation allows, and to facilitate this hospitals should provide reliable and redundant air medical services crew access to the receiving health care team. Follow-up communication from the air medical team to the referring clinicians, whether ground EMS crews or in-hospital clinicians, promotes continuous improvement of the system.
Destination Decisions
The destination decision for interfacility transports is made by the referring physician. Hospital destination choice for scene calls should be based on alignment of the capabilities and capacity of the hospital with the medical needs of the patient. When patients have medical decision-making capacity, they should be engaged in informed and shared decision-making regarding choice of destination whenever possible and appropriate. Considerations when choosing the destination hospital include preexisting regional destination plans and confirmed availability of specific specialty and time-critical services, equipment, and personnel. This destination may not necessarily be the most proximate facility. Unless all other factors are equal (both facilities offer needed services, have capacity, and are equivalent in time/distance away), destination should not be primarily based on the patient’s (lack of) insurance coverage, ability to pay, or other financial considerations of the receiving hospital (Citation128). For less critical transports, ideally destination facilities that accept the patient’s insurance plan (i.e., are “in-network”) or are preferred by the patient should be considered, though coverage varies by insurance carrier and is modified at intervals, so a consistent approach is challenging. Governing bodies, likely state governments, may establish criteria to guide and regulate the selection of the destination facility. Ground EMS may be needed to facilitate patient transport between helipads or airports and medical facilities.
Utilization Review and Quality Assurance
Though activities centered at defining locally applicable, appropriate air medical services utilization practices are important to establish prior to a request for response, a system designed to review utilization and assure quality of care must also be established in order to ensure utilization procedures and criteria are being appropriately applied.
Whether an air medical services response is initiated at the scene or from a referring hospital for interfacility transfer, the dynamic nature of many illnesses and injuries can make it difficult to accurately identify which patients will definitively realize greater benefit than harm from air medical services care and transport. The complex decision to activate an air response resource should be expected to result in either over- or under-triage of a patient in a certain proportion of cases (Citation141). While under-triage has negative implications for individual patients, over-triage can strain scarce system resources and place an unwarranted financial burden on both the patient and the health care system (Citation111, Citation142). Different local and regional systems have different levels of tolerance for over and under-triage, and discussions regarding acceptable triage of these cases should occur among stakeholders during system integration and planning.
Entities that request air medical services resources, and the programs themselves, should conduct regular review of flight requests, refusals, aborted missions, and completed missions to ensure adherence to the three primary patient-centered goals of air medical services, to the regionally accepted utilization criteria and/or algorithms, and whether ground resources were available and appropriate for patient care. These reviews should be performed regularly to identify opportunities to reduce both under- and over-triage and to accordingly refine local and regional utilization protocols. Such reviews can also inform regional strategies to limit interfacility transport by bringing expertise to the patient rather than transporting the patient to tertiary care facilities (Citation109). Unfortunately the competitive environment of air medical services, whether involving multiple air programs or multiple health care systems, adds competitive pressures that limit the ability to provide meaningful feedback to services that overuse resources. Ideally a neutral body with participants from all programs and health care systems can be established to assist in deriving and disseminating feedback.
The methodology used to evaluate appropriate air medical services utilization must be thoughtfully developed and applied. Retrospective determination of appropriate versus inappropriate utilization using hospital discharge codes or whether the patient received specific hospital-based interventions should be avoided. Such methodology fails to consider the limited information available to the field and transferring clinicians when they are faced with making decisions about using air resources. Rather, utilization review should carefully consider whether the personnel requesting an air response did so appropriately in the context of their training and experience, whether established utilization criteria or algorithms were followed, whether validated scoring systems and decision tools were applied, or if advice was sought from regional coordinating centers or from EMS physician oversight (Citation49, Citation131).
Use of Air Medical Services Resources for Medical Repatriation
Medical repatriation, the process of returning a patient back to his or her home area to receive care from locally based health care entities, can occur in both domestic and international theaters and uses many of the same resources used in the delivery of more familiar air medical services care. These missions may involve singular patients or may involve mass movement of hundreds or thousands of patients such as seen in the repatriation of patients during the global COVID-19 pandemic, or of injured patients following the 2002 terrorist attacks in Kenya (Citation143, Citation144). A few papers have described various patient characteristics, adverse events, and other aspects of air medical services repatriation (Citation144–150). Though this realm of medical care requires similar use of clinicians trained and equipped to provide care in the air medical environment, medical repatriation missions have some unique characteristics that differentiate them from more familiar missions, including geopolitical considerations.
Due to the distances that must be traversed during repatriation missions, these flights usually involve a fixed-wing aircraft operated by a private, corporate, commercial, or military-based entity. In some cases repatriation uses fixed wing aircraft that are not specifically designed for medical transport, which creates some unique challenges to providing care in flight (Citation151). Though the medical care provided during repatriation may be quite complex, patients being repatriated are typically more medically stable than patients receiving care during local interfacility/retrieval or field-response missions. Further, while air medical services missions typically occur “in-country,” repatriation missions often involve international transport of undocumented immigrants, aliens, or foreign nationals back to their countries of origin, creating certain unique ethical and legal issues (Citation152–156). Finally, medical repatriation is variably covered by typical health insurance products and may require purchase of dedicated traveler or repatriation-focused policies, and repatriated patients may be subject to significant out-of-pocket expense.
Despite these differences from more typical missions, repatriation missions must operate under the same physician oversight, utilization review, and quality assurance practices that apply to air medical services as described by this document.
Conclusion
Air medical services are an important part of the health care system. To ensure optimal function of the system, entities that use and provide air medical services resources should work collaboratively to ensure these resources are used in a safe, clinically appropriate, professional, and integrated manner. Every effort should be made to minimize risk to patients and air crews and avoid unnecessary financial burdens to patients. EMS physicians play a critical and central leadership role in assuring such appropriate utilization of air medical services resources.
References
- Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA. Access to emergency care in the United States. Ann Emerg Med. 2009;54(2):261–9. doi:https://doi.org/10.1016/j.annemergmed.2008.11.016.
- Carr BG, Bowman AJ, Wolff CS, Mullen MT, Holena DN, Branas CC, Wiebe DJ. Disparities in access to trauma care in the United States: a population-based analysis. Injury. 2017;48(2):332–8. doi:https://doi.org/10.1016/j.injury.2017.01.008.
- Floccare DJ, Stuhlmiller DFE, Braithwaite SA, Thomas SH, Madden JF, Hankins DG, Dhindsa H, Millin MG. Appropriate and safe utilization of helicopter emergency medical services: a joint position statement with resource document. Prehosp Emerg Care. 2013;17(4):521–5. doi:https://doi.org/10.3109/10903127.2013.804139.
- Hannay RS, Wyrzykowski AD, Ball CG, Laupland K, Feliciano DV. Retrospective review of injury severity, interventions and outcomes among helicopter and nonhelicopter transport patients at a level 1 urban trauma centre. Can J Surg. 2014;57(1):49–54. doi:https://doi.org/10.1503/cjs.000113.
- Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Helicopter transport improves survival following injury in the absence of a time-saving advantage. Surgery. 2016;159(3):947–59. doi:https://doi.org/10.1016/j.surg.2015.09.015.
- Andruszkow H, Lefering R, Frink M, Mommsen P, Zeckey C, Rahe K, Krettek C, Hildebrand F. Survival benefit of helicopter emergency medical services compared to ground emergency medical services in traumatized patients. Crit Care. 2013;17(3):R124. doi:https://doi.org/10.1186/cc12796.
- Bledsoe BE, Wesley AK, Eckstein M, Dunn TM, O'Keefe MF. Helicopter scene transport of trauma patients with nonlife-threatening injuries: a meta-analysis. J Trauma-Injury Infect Crit Care. 2006;60(6):1257–66.
- Ruskin KJ. Helicopter air ambulance services. Curr Opin Anaesthesiol. 2019;32(2):252–6. doi:https://doi.org/10.1097/ACO.0000000000000700.
- Delgado MK, Staudenmayer KL, Wang NE, Spain DA, Weir S, Owens DK, Goldhaber-Fiebert JD. Cost-effectiveness of helicopter versus ground emergency medical services for trauma scene transport in the United States. Ann Emerg Med. 2013;62(4):351–64.e19. doi:https://doi.org/10.1016/j.annemergmed.2013.02.025.
- Berns KS, Caniglia JJ, Hankins DG, Zietlow SP. Use of the autolaunch method of dispatching a helicopter. Air Med J. 2003;22(3):35–41. doi:https://doi.org/10.1016/S1067-991X(03)70006-6.
- Association of Air Medical Services. Position statement: Early activation of an air medical helicopter and auto launch recommendations; 2006. Available from: https://aams.org/publications/early-activation-air-medical-helicopter-auto-launch-recommendations/.
- Position Paper on Helicopter Shopping: International Association of Flight Paramedics; 2006. Accessed February 17, 2021. Available from: http://c.ymcdn.com/sites/www.iafccp.org/resource/resmgr/docs/helicoptershopping.pdf.
- Hirshon JM, Galvagno SM, Comer A, Millin MG, Floccare DJ, Alcorta RL, Lawner BJ, Margolis AM, Nable JV, Bass RR. Maryland's Helicopter Emergency Medical Services experience from 2001 to 2011: system improvements and patients' outcomes. Ann Emerg Med. 2016;67(3):332–40.e3. doi:https://doi.org/10.1016/j.annemergmed.2015.07.503.
- Lyng J, Bleess B, Fairless J, Guyette FX, Martin-Gill C, Steuerwald MT. Physician oversight of air-based emergency medical services: a joint position statement of NAEMSP, ACEP, and AMPA. Prehosp Emerg Care. 2021;25(3):449–50.
- Cudnik MT, Werman HA, White LJ, Opalek JM. Prehospital factors associated with mortality in injured air medical patients. Prehosp Emerg Care. 2012;16(1):121–7. doi:https://doi.org/10.3109/10903127.2011.615011.
- Plevin RE, Evans HL. Helicopter transport: help or hindrance? Curr Opin Crit Care. 2011;17(6):596–600. doi:https://doi.org/10.1097/MCC.0b013e32834c5655.
- Brown JB, Forsythe RM, Stassen NA, Gestring ML. The National Trauma Triage Protocol: can this tool predict which patients with trauma will benefit from helicopter transport? J Trauma Acute Care Surg. 2012;73(2):319–25. doi:https://doi.org/10.1097/TA.0b013e3182572bee.
- Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. External validation of the Air Medical Prehospital Triage score for identifying trauma patients likely to benefit from scene helicopter transport. J Trauma Acute Care Surg. 2017;82(2):270–9. doi:https://doi.org/10.1097/TA.0000000000001326.
- Jacobs LM, Gabram SG, Sztajnkrycer MD, Robinson KJ, Libby MC. Helicopter air medical transport: ten-year outcomes for trauma patients in a New England program. Conn Med. 1999;63(11):677–82.
- Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69(5):1030–4. Discussion 4–6.
- Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care. 2011;15(3):295–302. doi:https://doi.org/10.3109/10903127.2011.569849.
- Galvagno SM, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association Between Helicopter vs Ground Emergency Medical Services and Survival for Adults With Major Trauma. Jama. 2012;307(15):1602–10. doi:https://doi.org/10.1001/jama.2012.467.
- Thomas SH, Harrison TH, Buras WR, Ahmed W, Cheema F, Wedel SK. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma. 2002;52(1):136–45.
- Brathwaite CE, Rosko M, McDowell R, Gallagher J, Proenca J, Spott MA. A critical analysis of on-scene helicopter transport on survival in a statewide trauma system. J Trauma-Injury Infect Crit Care. 1998;45(1):140–6.
- Fischer RP, Flynn TC, Miller PW, Duke JH, Jr. Urban helicopter response to the scene of injury. J Trauma. 1984;24(11):946–51.
- Schiller WR, Knox R, Zinnecker H, Jeevanandam M, Sayre M, Burke J, Young DH. Effect of helicopter transport of trauma victims on survival in an urban trauma center. J Trauma. 1988;28(8):1127–34.
- Shatney CH, Homan SJ, Sherck JP, Ho CC. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma system. J Trauma. 2002;53(5):817–22.
- Cocanour CS, Fischer RP, Ursic CM. Are scene flights for penetrating trauma justified? J Trauma. 1997;43(1):83–6. Discussion 6–8. doi:https://doi.org/10.1097/00005373-199707000-00019.
- Moylan JA, Fitzpatrick KT, Beyer AJ, 3rd, Georgiade GS. Factors improving survival in multisystem trauma patients. Ann Surg. 1988;207(6):679–85. doi:https://doi.org/10.1097/00000658-198806000-00006.
- Nicholl JP, Brazier JE, Snooks HA. Effects of London helicopter emergency medical service on survival after trauma. BMJ. 1995;311(6999):217–22. doi:https://doi.org/10.1136/bmj.311.6999.217.
- Beaumont O, Lecky F, Bouamra O, Surendra Kumar D, Coats T, Lockey D, Willett K. Helicopter and ground emergency medical services transportation to hospital after major trauma in England: a comparative cohort study. Trauma Surg Acute Care Open. 2020;5(1):e000508. doi:https://doi.org/10.1136/tsaco-2020-000508.
- Cunningham P, Rutledge R, Baker CC, Clancy TV. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma. 1997;43(6):940–6.
- Tsuchiya A, Tsutsumi Y, Yasunaga H. Outcomes after helicopter versus ground emergency medical services for major trauma-propensity score and instrumental variable analyses: a retrospective nationwide cohort study. Scand J Trauma Resusc Emerg Med. 2016;24(1):140. doi:https://doi.org/10.1186/s13049-016-0335-z.
- Buchanan IM, Coates A, Sne N. Does mode of transport confer a mortality benefit in trauma patients? Characteristics and outcomes at an Ontario Lead Trauma Hospital. CJEM Can J Emerg Med Care. 2016;18(5):363–9. doi:https://doi.org/10.1017/cem.2016.15.
- Baxt WG, Moody P. The impact of a rotorcraft aeromedical emergency care service on trauma mortality. JAMA. 1983;249(22):3047–51.
- Baxt WG, Moody P, Cleveland HC, Fischer RP, Kyes FN, Leicht MJ, Rouch F, Wiest P. Hospital-based rotorcraft aeromedical emergency care services and trauma mortality: a multicenter study. Ann Emerg Med. 1985;14(9):859–64. doi:https://doi.org/10.1016/S0196-0644(85)80634-X.
- Schwartz RJ, Jacobs LM, Juda RJ. A comparison of ground paramedics and aeromedical treatment of severe blunt trauma patients. Conn Med. 1990;54(12):660–2.
- Hamman BL, Cué JI, Miller FB, O'Brien DA, House T, Polk HC, Richardson JD, Jr. Helicopter transport of trauma victims: does a physician make a difference? J Trauma. 1991;31(4):490–4. doi:https://doi.org/10.1097/00005373-199104000-00007.
- Schmidt U, Frame SB, Nerlich ML, Rowe DW, Enderson BL, Maull KI, Tscherne H. On-scene helicopter transport of patients with multiple injuries–comparison of a German and an American system. J Trauma. 1992;33(4):548–53. Discussion 53–5.
- Younge PA, Coats TJ, Gurney D, Kirk CJ. Interpretation of the Ws statistic: application to an integrated trauma system. J Trauma. 1997;43(3):511–5. doi:https://doi.org/10.1097/00005373-199709000-00021.
- Rhinehart ZJ, Guyette FX, Sperry JL, Forsythe RM, Murdock A, Alarcon LH, Peitzman AB, Rosengart MR. The association between air ambulance distribution and trauma mortality. Ann Surg. 2013;257(6):1147–53. doi:https://doi.org/10.1097/SLA.0b013e31827ee6b0.
- Borst GM, Davies SW, Waibel BH, Leonard KL, Rinehart SM, Newell MA, Goettler CE, Bard MR, Poulin NR, Toschlog EA, et al. When birds can't fly: an analysis of interfacility ground transport using advanced life support when helicopter emergency medical service is unavailable. J Trauma Acute Care Surg. 2014;77(2):331–6. Discussion 6–7. doi:https://doi.org/10.1097/TA.0000000000000295.
- Fan E, MacDonald RD, Adhikari NK, Scales DC, Wax RS, Stewart TE, Ferguson ND. Outcomes of interfacility critical care adult patient transport: a systematic review. Crit Care. 2006;10(1):R6. doi:https://doi.org/10.1186/cc3924.
- Aiolfi A, Benjamin E, Recinos G, De Leon Castro A, Inaba K, Demetriades D. Air versus ground transportation in isolated severe head trauma: a national trauma data bank study. J Emerg Med. 2018;54(3):328–34. doi:https://doi.org/10.1016/j.jemermed.2017.11.019.
- Boyd CR, Corse KM, Campbell RC. Emergency interhospital transport of the major trauma patient: air versus ground. J Trauma. 1989;29(6):789–93. Discussion 93–4. doi:https://doi.org/10.1097/00005373-198906000-00015.
- Wuerz R, Taylor J, Smith JS. Accuracy of trauma triage in patients transported by helicopter. Air Med J. 1996;15(4):168–70. doi:https://doi.org/10.1016/S1067-991X(96)90025-5.
- Holcomb JB, Niles SE, Miller CC, Hinds D, Duke JH, Moore FA. Prehospital physiologic data and lifesaving interventions in trauma patients. Mil Med. 2005;170(1):7–13. doi:https://doi.org/10.7205/MILMED.170.1.7.
- Thomas SH, Brown KM, Oliver ZJ, Spaite DW, Lawner BJ, Sahni R, Weik TS, Falck-Ytter Y, Wright JL, Lang ES, et al. An evidence-based guideline for the air medical transportation of prehospital trauma patients. Prehosp Emerg Care. 2014;18(sup1):35–44. doi:https://doi.org/10.3109/10903127.2013.844872.
- Brown JB, Gestring ML, Guyette FX, Rosengart MR, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Development and Validation of the Air Medical Prehospital Triage Score for Helicopter Transport of Trauma Patients. Annals of Surgery. 2016;264(2):378–85. doi:https://doi.org/10.1097/SLA.0000000000001496.
- Chen X, Gestring ML, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL, Brown JB. Speed is not everything: identifying patients who may benefit from helicopter transport despite faster ground transport. J Trauma Acute Care Surg. 2018;84(4):549–57. doi:https://doi.org/10.1097/TA.0000000000001769.
- Udekwu P, Schiro S, Toschlog E, Farrell M, McIntyre S, Winslow J, 3rd. Trauma system resource preservation: a simple scene triage tool can reduce helicopter emergency medical services overutilization in a state trauma system. J Trauma Acute Care Surg. 2019;87(2):315–21. doi:https://doi.org/10.1097/TA.0000000000002309.
- Nolan B, Tien H, Haas B, Saskin R, Nathens A. The rapid emergency medicine score: a critical appraisal of its measurement properties and applicability to the air retrieval environment. Air Med J. 2019;38(3):154–60. doi:https://doi.org/10.1016/j.amj.2019.02.001.
- Moyer P, Ornato JP, Brady WJ, Davis LL, Ghaemmaghami CA, Gibler WB, Mears G, Mosesso VN, Zane RD. Development of systems of care for ST-elevation myocardial infarction patients: the emergency medical services and emergency department perspective. Circulation. 2007;116(2):e43–e48. doi:https://doi.org/10.1161/CIRCULATIONAHA.107.184047.
- Widimský P, Budesínský T, Vorác D, Groch L, Zelízko M, Aschermann M, Branny M, St'ásek J, Formánek P. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial–PRAGUE-2. Eur Heart J. 2003;24(1):94–104. doi:https://doi.org/10.1016/S0195-668X(02)00468-2.
- Dalby M, Bouzamondo A, Lechat P, Montalescot G. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation. 2003;108(15):1809–14. doi:https://doi.org/10.1161/01.CIR.0000091088.63921.8C.
- Stone CK, Hunt RC, Sousa JA, Whitley TW, Thomas SH. Interhospital transfer of cardiac patients: does air transport make a difference? Air Med J. 1994;13(5):159–62. doi:https://doi.org/10.1016/S1067-991X(05)80106-3.
- Berns KS, Hankins DG, Zietlow SP. Comparison of air and ground transport of cardiac patients. Air Med J. 2001;20(6):33–6. doi:https://doi.org/10.1016/S1067-991X(01)70008-9.
- Grines CL, Westerhausen DR, Grines LL, Hanlon JT, Logemann TL, Niemela M, Weaver WD, Graham M, Boura J, O’Neill WW, et al. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction: the Air Primary Angioplasty in Myocardial Infarction study. J Am Coll Cardiol. 2002;39(11):1713–9. doi:https://doi.org/10.1016/S0735-1097(02)01870-3.
- Blankenship JC, Haldis TA, Wood GC, Skelding KA, Scott T, Menapace FJ. Rapid triage and transport of patients with ST-elevation myocardial infarction for percutaneous coronary intervention in a rural health system. Am J Cardiol. 2007;100(6):944–8. doi:https://doi.org/10.1016/j.amjcard.2007.04.031.
- Aguirre FV, Varghese JJ, Kelley MP, Lam W, Lucore CL, Gill JB, Page L, Turner L, Davis C, Mikell FL, et al. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation. 2008;117(9):1145–52. doi:https://doi.org/10.1161/CIRCULATIONAHA.107.728519.
- Hakim R, Revue E, Saint Etienne C, Marcollet P, Chassaing S, Decomis MP, Yafi W, Laure C, Gautier S, Godillon L, et al. Does helicopter transport delay prehospital transfer for STEMI patients in rural areas? Findings from the CRAC France PCI registry. Eur Heart J Acute Cardiovasc Care. 2020;9(8):958–65. doi:https://doi.org/10.1177/2048872619848976.
- Denktas AE, Anderson HV, McCarthy J, Smalling RW. Total ischemic time: the correct focus of attention for optimal ST-segment elevation myocardial infarction care. JACC Cardiovasc Interv. 2011;4(6):599–604. doi:https://doi.org/10.1016/j.jcin.2011.02.012.
- De Luca G, Suryapranata H, Zijlstra F, van't Hof AWJ, Hoorntje JCA, Gosselink ATM, Dambrink J-H, de Boer M-J. Symptom-onset-to-balloon time and mortality in patients with acute myocardial infarction treated by primary angioplasty. J Am Coll Cardiol. 2003;42(6):991–7. doi:https://doi.org/10.1016/S0735-1097(03)00919-7.
- Alrawashdeh A, Nehme Z, Williams B, Smith K, Brennan A, Dinh DT, Liew D, Lefkovits J, Stub D. Impact of emergency medical service delays on time to reperfusion and mortality in STEMI. Open Heart. 2021;8(1):e001654. doi:https://doi.org/10.1136/openhrt-2021-001654.
- Werman HA, Falcone Ra Fau-Shaner S, Shaner S, Fau-Herron H, Herron H, Fau-Johnson R, Johnson R, Fau-Lacey P, Lacey P, Fau-Childress S, et al. Helicopter transport of patients to tertiary care centers after cardiac arrest. Am J Emerg Med. 1999;17(2):130–4. doi:https://doi.org/10.1016/S0735-6757(99)90043-8.
- Putzer G, Braun P, Zimmermann A, Pedross F, Strapazzon G, Brugger H, Paal P. LUCAS compared to manual cardiopulmonary resuscitation is more effective during helicopter rescue-a prospective, randomized, cross-over manikin study. Am J Emerg Med. 2013;31(2):384–9. doi:https://doi.org/10.1016/j.ajem.2012.07.018.
- Rehatschek G, Muench M, Schenk I, Dittrich W, Schewe JC, Dirk C, Hering R. Mechanical LUCAS resuscitation is effective, reduces physical workload and improves mental performance of helicopter teams. Minerva Anestesiol. 2016;82(4):429–37.
- Gässler H, Kümmerle S, Ventzke MM, Lampl L, Helm M. Mechanical chest compression: an alternative in helicopter emergency medical services? Intern Emerg Med. 2015;10(6):715–20. doi:https://doi.org/10.1007/s11739-015-1238-0.
- Havel C, Schreiber W, Riedmuller E, Haugk M, Richling N, Trimmel H, Malzer R, Sterz F, Herkner H. Quality of closed chest compression in ambulance vehicles, flying helicopters and at the scene. Resuscitation. 2007;73(2):264–70. doi:https://doi.org/10.1016/j.resuscitation.2006.09.007.
- Braunfels S, Meinhard K, Zieher B, Koetter KP, Maleck WH, Petroianu GA. A randomized, controlled trial of the efficacy of closed chest compressions in ambulances. Prehosp Emerg Care. 1997;1(3):128–31. doi:https://doi.org/10.1080/10903129708958804.
- Thomas SH, Stone CK, Bryan-Berge D. The ability to perform closed chest compressions in helicopters. Am J Emerg Med. 1994;12(3):296–8. doi:https://doi.org/10.1016/0735-6757(94)90142-2.
- Gassler H, Ventzke MM, Lampl L, Helm M. Transport with ongoing resuscitation: a comparison between manual and mechanical compression. Emerg Med J. 2013;30(7):589–92. doi:https://doi.org/10.1136/emermed-2012-201142.
- Winther K, Bleeg RC. LUCAS(™)2 in Danish search and rescue helicopters. Air Med J. 2016;35(2):79–83. doi:https://doi.org/10.1016/j.amj.2015.10.010.
- Millin MG, Khandker SR, Malki A. Termination of resuscitation of nontraumatic cardiopulmonary arrest: resource document for the National Association of EMS Physicians position statement. Prehosp Emerg Care. 2011;15(4):547–54. doi:https://doi.org/10.3109/10903127.2011.608872.
- Millin MG, Galvagno SM, Khandker SR, Malki A, Bulger EM, Subcommittee on Emergency Services–Prehospital of the American College of Surgeons’ Committee on Trauma (ACSCOT). Withholding and termination of resuscitation of adult cardiopulmonary arrest secondary to trauma: resource document to the joint NAEMSP-ACSCOT position statements. J Trauma Acute Care Surg. 2013;75(3):459–67. doi:https://doi.org/10.1097/TA.0b013e31829cfaea.
- American College of Surgeons Committee on Trauma, American College of Emergency Physicians Pediatric Emergency Medicine C, National Association of EMS Physicians, American Academy of Pediatrics Committee on Pediatric Emergency Medicine, Fallat ME. Withholding or termination of resuscitation in pediatric out-of-hospital traumatic cardiopulmonary arrest. Ann Emerg Med. 2014;63(4):504–15. doi:https://doi.org/10.1016/j.annemergmed.2014.01.013.
- English SW, Rabinstein AA, Mandrekar J, Klaas JP. Rethinking prehospital stroke notification: assessing utility of emergency medical services impression and Cincinnati Prehospital Stroke Scale. J Stroke Cerebrovasc Dis. 2018;27(4):919–25. doi:https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.10.036.
- Rudd M, Buck D, Ford GA, Price CI. A systematic review of stroke recognition instruments in hospital and prehospital settings. Emerg Med J. 2016;33(11):818–22. doi:https://doi.org/10.1136/emermed-2015-205197.
- Leira EC, Stilley JD, Schnell T, Audebert HJ, Adams HP, Jr. Helicopter transportation in the era of thrombectomy: the next frontier for acute stroke treatment and research. Eur Stroke J. 2016;1(3):171–9. doi:https://doi.org/10.1177/2396987316658994.
- Chalela JA, Kasner SE, Jauch EC, Pancioli AM. Safety of air medical transportation after tissue plasminogen activator administration in acute ischemic stroke. Stroke. 1999;30(11):2366–8. doi:https://doi.org/10.1161/01.str.30.11.2366.
- Olson MD, Rabinstein AA. Does helicopter emergency medical service transfer offer benefit to patients with stroke? Stroke. 2012;43(3):878–80. doi:https://doi.org/10.1161/STROKEAHA.111.640987.
- Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJH, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. doi:https://doi.org/10.1056/NEJMoa1411587.
- Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–30. doi:https://doi.org/10.1056/NEJMoa1414905.
- Todo K, Sakai N, Kono T, Hoshi T, Imamura H, Adachi H, Kohara N. National Institutes of Health Stroke Scale-Time Score Predicts Outcome after Endovascular Therapy in Acute Ischemic Stroke: a retrospective single-center study. J Stroke Cerebrovasc Dis. 2016;25(5):1187–91. doi:https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.01.027.
- Venema E, Burke JF, Roozenbeek B, Nelson J, Lingsma HF, Dippel DWJ, Kent DM. prehospital triage strategies for the transportation of suspected stroke patients in the United States. Stroke. 2020;51(11):3310–9. doi:https://doi.org/10.1161/STROKEAHA.120.031144.
- Rynor H, Levine J, Souchak J, Shashoua N, Ramirez M, Gonzalez IC, Ramos V, Saxena A, Veledar E, Starosciak AK, et al. The effect of a county prehospital FAST-ED initiative on endovascular treatment times. J Stroke Cerebrovasc Dis. 2020;29(11):105220. doi:https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105220.
- Nguyen TTM, van den Wijngaard IR, Bosch J, van Belle E, van Zwet EW, Dofferhoff-Vermeulen T, Duijndam D, Koster GT, de Schryver ELLM, Kloos LMH, et al. Comparison of prehospital scales for predicting large anterior vessel occlusion in the ambulance setting. JAMA Neurol. 2021;78(2):157–64. doi:https://doi.org/10.1001/jamaneurol.2020.4418.
- Zachrison KS, Khatri P. Self-driven prehospital triage decisions for suspected stroke-another step closer. JAMA Neurol. 2021;78(2):146–8. doi:https://doi.org/10.1001/jamaneurol.2020.4425.
- Krebs W, Sharkey-Toppen TP, Cheek F, Cortez E, Larrimore A, Keseg D, Panchal AR. Prehospital stroke assessment for large vessel occlusions: a systematic review. Prehosp Emerg Care. 2018;22(2):180–8. doi:https://doi.org/10.1080/10903127.2017.1371263.
- Sugimura Y, Ikeda T, Shindo S, Namitome S, Miura M, Wada K, Nagao Y, Yamanouchi Y, Terasaki T, Nakajima M, et al. Pre-hospital Diagnosis of Large Vessel Occlusion in Patients Being Transported by Helicopter. J Stroke Cerebrovasc Dis. 2021;30(1):105416. doi:https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105416.
- Gottlibe M, Rosen O, Weller B, Mahagney A, Omar N, Khuri A, Srugo I, Genizi J. Stroke identification using a portable EEG device - a pilot study. Neurophysiol Clin. 2020;50(1):21–5. doi:https://doi.org/10.1016/j.neucli.2019.12.004.
- Van Stigt MN. Identification of large vessel occlusions in patients with suspected stroke using ambulant electroencephalography. 2020. [cited March 11, 2021]. Available from: http://essay.utwente.nl/83377/
- Loudon W, Wong A, Finnigan S, Tippett V. Stroke Prehospital Informed Decision-Making Using EEG Recordings (SPIDER). Prehosp Disaster Med. 2019;34(s1):S87–S8. doi:https://doi.org/10.1017/S1049023X19001821.
- Lumley HA, Flynn D, Shaw L, McClelland G, Ford GA, White PM, Price CI. A scoping review of pre-hospital technology to assist ambulance personnel with patient diagnosis or stratification during the emergency assessment of suspected stroke. BMC Emerg Med. 2020;20(1):30. doi:https://doi.org/10.1186/s12873-020-00323-0.
- Silbergleit R, Scott PA, Lowell MJ, Silbergleit R. Cost-effectiveness of helicopter transport of stroke patients for thrombolysis. Acad Emerg Med. 2003;10(9):966–72. doi:https://doi.org/10.1197/s1069-6563(03)00316-6.
- Elliott JP, O'Keeffe DF, Freeman RK. Helicopter transportation of patients with obstetric emergencies in an urban area. Am J Obstet Gynecol. 1982;143(2):157–62. doi:https://doi.org/10.1016/0002-9378(82)90646-9.
- Jony L, Baskett TF. Emergency air transport of obstetric patients. J Obstet Gynaecol Can. 2007;29(5):406–8. doi:https://doi.org/10.1016/S1701-2163(16)35491-3.
- O'Hara R, O'Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J. 2012;29(4):327–32. doi:https://doi.org/10.1136/emj.2010.104190.
- Hohlagschwandtner M, Husslein P, Klebermass K, Weninger M, Nardi A, Langer M. Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet. 2001;265(3):113–8. doi:https://doi.org/10.1007/s004040100197.
- Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK, Canadian Neonatal Network. Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol. 2001;98(2):247–52. doi:https://doi.org/10.1016/s0029-7844(01)01438-7.
- Shlossman PA, Manley JS, Sciscione AC, Colmorgen GH. An analysis of neonatal morbidity and mortality in maternal (in utero) and neonatal transports at 24-34 weeks' gestation. Amer J Perinatol. 1997;14(08):449–56. doi:https://doi.org/10.1055/s-2007-994178.
- Kollée LA, Brand R, Schreuder AM, Ens-Dokkum MH, Veen S, Verloove-Vanhorick SP. Five-year outcome of preterm and very low birth weight infants: a comparison between maternal and neonatal transport. Obstet Gynecol. 1992;80(4):635–8.
- Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA. Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics. 2002;109(5):745–51. doi:https://doi.org/10.1542/peds.109.5.745.
- Scott J. Obstetric transport. Obstet Gynecol Clin North Am. 2016;43(4):821–40. doi:https://doi.org/10.1016/j.ogc.2016.07.013.
- Whyte HE, Jefferies AL, Canadian Paediatric Society, Fetus and Newborn Committee. The interfacility transport of critically ill newborns. Paediatr Child Health. 2015;20(5):265–75. doi:https://doi.org/10.1093/pch/20.5.265.
- Lee SK, Zupancic JA, Pendray M, Thiessen P, Schmidt B, Whyte R, Shorten D, Stewart S, Canadian Neonatal Network. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr. 2001;139(2):220–6. doi:https://doi.org/10.1067/mpd.2001.115576.
- Lucas da Silva PS, Euzébio de Aguiar V, Reis ME. Assessing outcome in interhospital infant transport: the transport risk index of physiologic stability score at admission. Am J Perinatol. 2012;29(7):509–14. doi:https://doi.org/10.1055/s-0032-1310521.
- Markakis C, Dalezios M, Chatzicostas C, Chalkiadaki A, Politi K, Agouridakis PJ. Evaluation of a risk score for interhospital transport of critically ill patients. Emerg Med J: EMJ. 2006;23(4):313–7. doi:https://doi.org/10.1136/emj.2005.026435.
- Mantecchini L, Paganelli F, Morabito V, Ricci A, Peritore D, Trapani S, Montemurro A, Rizzo A, Del Sordo E, Gaeta A, et al. Transportation of organs by air: safety, quality, and sustainability criteria. Transplant Proc. 2016;48(2):304–8. doi:https://doi.org/10.1016/j.transproceed.2015.12.050.
- Englesbe MJ, Shah S, Cutler JA, Africano R, Lynch R, Seely M, Hasz R, Sweeney ML, Roberts J, Merion RM, et al. Improving organ procurement travel practices in the United States: proceedings from the Michigan Donor Travel Forum. Am J Transplant. 2010;10(3):458–63. doi:https://doi.org/10.1111/j.1600-6143.2009.02964.x.
- Madiraju SK, Catino J, Kokaram C, Genuit T, Bukur M. In by helicopter out by cab: the financial cost of aeromedical overtriage of trauma patients. J Surg Res. 2017;218:261–70. doi:https://doi.org/10.1016/j.jss.2017.05.102.
- Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury. 2010;41(1):10–20. doi:https://doi.org/10.1016/j.injury.2009.09.030.
- Rolnitsky A, Ng E, Asztalos E, Shama Y, Karol D, Findlater C, Garsch M, Dunn M. a quality improvement intervention to reduce necrotizing enterocolitis in premature infants with probiotic supplementation. Pediatr Qual Saf. 2019;4(5):e201. doi:https://doi.org/10.1097/pq9.0000000000000201.
- Rzońca P, Świeżewski SP, Jalali R, Gotlib J, Gałązkowski R. Helicopter Emergency Medical Service (HEMS) response in rural areas in Poland: retrospective study. Int J Environ Res Public Health. 2019;16(9):1532.
- Hotvedt R, Thoner J, Almdahl SM, Bjørsvik G, Berge L, Sparr T, Ytre-Arne K, Kristiansen IS, Førde OH, Magnus AC, et al. Which groups of patients benefit from helicopter evacuation? Lancet (London, England). 1996;347(9012):1362–6. doi:https://doi.org/10.1016/S0140-6736(96)91010-7.
- Gerard D, Raffin H, Lebreton G. Aeromedical evacuation using extra corporeal life support after resuscitated cardiac arrest. Aerosp Med Hum Perform. 2017;88(4):431–3. doi:https://doi.org/10.3357/AMHP.4470.2017.
- Aucar J, Granchi T, Liscum K, Wall M, Mattox K. Is regionalization of trauma care using telemedicine feasible and desirable? Am J Surg. 2000;180(6):535–9. doi:https://doi.org/10.1016/s0002-9610(00)00516-x.
- National Transportation Safety Board. Special Investigation Report on Emergency Medical Services Operations. Washington, DC 2006. NTSB/SIR-06/01. Available from: https://www.google.com/books/edition/_/HXRq_BBfFb8C?hl=en&gbpv=1&bsq=shopping
- Østerås Ø, Brattebø G, Heltne JK. Helicopter-based emergency medical services for a sparsely populated region: a study of 42,500 dispatches. Acta Anaesthesiol Scand. 2016;60(5):659–67. doi:https://doi.org/10.1111/aas.12673.
- Lawless J, Tallon JM, Petrie D. Aborted air medical missions: a 4-year quality review of a Canadian province-wide air medical program. Air Med J. 2005;24(2):79–82. doi:https://doi.org/10.1016/j.amj.2004.12.006.
- Aherne BB, Zhang C, Chen WS, Newman DG. Preflight risk assessment for improved safety in helicopter emergency medical service operations. Aerosp Med Hum Perform. 2019;90(9):792–9. doi:https://doi.org/10.3357/AMHP.5330.2019.
- Nix S, Buckner S, Cercone R. A review of risk analysis and helicopter air ambulance accidents. Air Med J. 2014;33(5):218–21. doi:https://doi.org/10.1016/j.amj.2014.06.011.
- Le Cong M, Finn E, Parsch C. Management of the acutely agitated patient in a remote location: a consensus statement from Australian aeromedical retrieval services. Med J Aust. 2015;202(4):182–3. doi:https://doi.org/10.5694/mja14.01162.
- Department of Transportation Federal Aviation Administration. Helicopter Air Ambulance, Commercial Helicopter, and Part 91 Helicopter Operations. 2014. RIN 2120 -AJ53. Available from: http://federalregister.gov/a/2014-03689
- National Transportation Safety Board. Helicopter Air Ambulance Collision with Terrain, Survival Flight Inc., Bell 407 Helicopter, N191SF, near Zaleski, Ohio, January 29, 2019. 2020. Air Accident Report NTSB/AAR-20/01. Available from: https://www.ntsb.gov/investigations/AccidentReports/Reports/AAR2001.pdf
- McGinnis KK, Judge T, Nemitz B, O'connor R, Bass R, Bishop B, Kim D, Kupas D, Rupert E, Eroe ER, et al. Air medical services: future development as an integrated component of the Emergency Medical Services (EMS) System: a guidance document by the Air Medical Task Force of the National Association of State EMS Officials, National Association of EMS Physicians, Association of Air Medical Services. Prehosp Emerg Care. 2007;11(4):353–68. doi:https://doi.org/10.1080/10903120701536578.
- Good NR, Air & Surface Transport Nurses Association, Emergency Nurses Association and International Association of Flight and Critical Care Paramedics. Responsible "helicopter shopping" through selective resource management. Air Med J. 2019;38(3):143–6. doi:https://doi.org/10.1016/j.amj.2019.02.007.
- American College of Emergency Physicians. EMTALA fact sheet. Available from: https://www.acep.org/life-as-a-physician/ethics–legal/emtala/emtala-fact-sheet/.
- Commission on Accreditation of Medical Transport Systems. Special Operations Accreditation Standards. 2018. Report No.: First Edition. Available from: https://www.camts.org/wp-content/uploads/2017/05/2018-Special-Ops-standards.pdf
- National Accreditation Alliance of Medical Transport Applications. Medical Transport Accreditation Standards, Revision 1.6.3. 2018. Available from: https://intranet.naamta.com/includes/secure_file.cfm?ID=2&menuID=5061
- Chhabra KR, McGuire K, Sheetz KH, Scott JW, Nuliyalu U, Ryan AM. Most patients undergoing ground and air ambulance transportation receive sizable out-of-network bills. Health Aff (Millwood). 2020;39(5):777–82. doi:https://doi.org/10.1377/hlthaff.2019.01484.
- Gearhart PA, Wuerz R, Localio AR. Cost-effectiveness analysis of helicopter EMS for trauma patients. Ann Emerg Med. 1997;30(4):500–6. doi:https://doi.org/10.1016/S0196-0644(97)70010-6.
- Krohmer JR, Hunt RC, Benson N, Bieniek RB. Flight physician training program—core content. Prehosp Disaster Med. 1993;8(2):183–4. doi:https://doi.org/10.1017/S1049023X00040309.
- Medical direction and medical control of air medical services: position statement of the Air Medical Physician Association approved by the AMPA Board of Trustees October 1998, revised April 2002. Air Med J. 2003;22(1):14–5.
- Hafner JW, Downs M, Cox K, Johncox JE, Schaefer TJ. Inappropriate helicopter emergency medical services transports: results of a national cohort utilization review. Prehosp Emerg Care. 2012;16(4):434–42. doi:https://doi.org/10.3109/10903127.2012.689928.
- Werfelman L. Procedural disregard. Aerosafety World. 2009;4(7):32–6.
- Cline PE. Human Error Analysis of Helicopter Emergency Medical Services (HEMS) accidents using the human factors analysis and classification system (HFACS). J Aviation/Aerospace Educ Res. 2018;28(1):43–62.
- Harmsen AM, Giannakopoulos G, Franschman G, Christiaans H, Bloemers F. Limitations in prehospital communication between trauma helicopter, ambulance services, and dispatch centers. J Emerg Med. 2017;52(4):504–12. doi:https://doi.org/10.1016/j.jemermed.2016.11.010.
- Harmsen AMK, Geeraedts LMG, Giannakopoulos GF, Terra M, Christiaans HMT, Mokkink LB, Bloemers FW. National consensus on communication in prehospital trauma care, the DENIM study. Scand J Trauma Resusc Emerg Med. 2017;25(1):67. doi:https://doi.org/10.1186/s13049-017-0414-9.
- Dalto JD, Weir C, Thomas F. Analyzing communication errors in an air medical transport service. Air Med J. 2013;32(3):129–37. doi:https://doi.org/10.1016/j.amj.2012.10.019.
- Grabowski RL, McNett M, Ackerman MH, Schubert C, Mion LC. Critical care helicopter overtriage: a failure mode and effects analysis. Air Med J. 2019;38(6):408–20. doi:https://doi.org/10.1016/j.amj.2019.07.012.
- Taylor CB, Curtis K, Jan S, Newcombe M. Helicopter emergency medical services (HEMS) over-triage and the financial implications for major trauma centres in NSW, Australia. BMC Emerg Med. 2013;13:11. doi:https://doi.org/10.1186/1471-227X-13-11.
- Cornelius B, Cornelius A, Crisafi L, Collins C, McCarthy S, Foster C, Shannon H, Bennett R, Brown S, Rodriguez K, et al. Mass air medical repatriation of coronavirus disease 2019 patients. Air Med J. 2020;39(4):251–6. doi:https://doi.org/10.1016/j.amj.2020.04.005.
- Marmor M, Goldstein L, Levi Y, Onn E, Blumenfeld A, Kosashvili Y, Levy G, Hirschorn G, Heldenberg E, Or J, et al. Mass medical repatriation of injured civilians after terrorist attack in Mombassa, Kenya: medical needs, resources used, and lessons learned. Prehosp Disaster Med. 2005;20(2):98–102. doi:https://doi.org/10.1017/s1049023x00002260.
- Dewhurst AT, Farrar D, Walker C, Mason P, Beven P, Goldstone JC. Medical repatriation via fixed-wing air ambulance: a review of patient characteristics and adverse events. Anaesthesia. 2001;56(9):882–7. doi:https://doi.org/10.1046/j.1365-2044.2001.02059-2.x.
- Greuters S, Christiaans HMT, Veenings B, Loer SA, Boer C. Evaluation of repatriation parameters: does medical history matter? J Travel Med. 2009;16(1):1–6. doi:https://doi.org/10.1111/j.1708-8305.2008.00253.x.
- Felkai PP, Marcolongo T, Van Aswegen M. Stranded abroad: a travel medicine approach to psychiatric repatriation. J Travel Med. 2020;27(2):taaa013. doi:https://doi.org/10.1093/jtm/taaa013.
- Thomas MD, Hinds R, Walker C, Morgan F, Mason P, Hildick-Smith D. Safety of aeromedical repatriation after myocardial infarction: a retrospective study. Heart. 2006;92(12):1864–5. doi:https://doi.org/10.1136/hrt.2006.094607.
- Duchateau F-X, Legrand J-M, Verner L, Brady WJ. Commercial aircraft repatriation of patients with pneumothorax. Air Med J. 2013;32(4):200–2. doi:https://doi.org/10.1016/j.amj.2012.10.022.
- Leggat PA, Fischer PR. Accidents and repatriation. Travel Med Infect Dis. 2006;4(3–4):135–46. doi:https://doi.org/10.1016/j.tmaid.2005.06.008.
- Veldman A, Diefenbach M, Fischer D, Benton A, Bloch R. Long-distance transport of ventilated patients: advantages and limitations of air medical repatriation on commercial airlines. Air Med J. 2004;23(2):24–8. doi:https://doi.org/10.1016/j.amj.2003.12.009.
- Zoellner ER. Medical repatriation: examining the legal and ethical implications of an emerging practice. Washington Univ J Law Policy. 2010;32(1):515–38.
- Donelson K. Medical repatriation: the dangerous intersection of health care law and immigration. J Health Care Law Policy. 2015;18(2):347–70.
- Hennebry JL, Williams G. Making vulnerability visible: medical repatriation and Canada's migrant agricultural workers. CMAJ. 2015;187(6):391–2. doi:https://doi.org/10.1503/cmaj.141189.
- Young M. Medical repatriation in the United States: an ethical appraisal. In: School HM, editor [Doctoral Dissertation]. 2016. [cited March 17, 2021]. Available from: http://nrs.harvard.edu/urn-3:HUL.InstRepos:40620246.
- McLaughlin RH. Criteria for medical repatriation and the context of inadequate access to care. Am J Bioeth. 2012;12(9):14–6. doi:https://doi.org/10.1080/15265161.2012.692451.

