Abstract
Background
Helicopter emergency medical services (HEMS) personnel provide on-scene trauma care to patients with high mortality risk. Work in the HEMS setting is characterized by frequent exposure to critical incidents and other stressors. The aim of this study was to further our understanding of the factors underlying HEMS personnel wellbeing to inform organizations regarding workplace interventions that can be implemented to support employees.
Method
We conducted 16 semi-structured interviews with HEMS personnel from a university hospital in The Netherlands. Interview topics included work context, personal characteristics, coping, work engagement, and psychosocial support. To analyze the data, we used a generic qualitative research approach inspired by grounded theory, including open, axial, and selective coding.
Results
The analysis revealed ten categories that provide insight into factors underlying the wellbeing of HEMS personnel and their work context: team and collaboration, coping, procedures, informal peer support, organizational support and follow-up care, drives and motivations, attitudes, other stressors, potentially traumatic events, and emotional impact. Various factors are important to their wellbeing, such as working together with colleagues and social support. Participants reported that HEMS work can have an emotional impact on wellbeing, yet they use multiple strategies to cope with various stressors. The perceived need for organizational support and follow-up care is low among participants.
Conclusion
This study identifies factors and strategies that support the wellbeing of HEMS personnel. It also provides insight into the HEMS work culture and help-seeking behavior in this population. Findings from this study may benefit employers by shedding much-needed light on factors that HEMS personnel feel affect wellbeing.
Introduction
Due to their regular exposure to work-related critical incidents, emergency medical services (EMS) personnel are at increased risk of developing mental health problems (e.g., post-traumatic stress disorder [PTSD], depression, and burn-out) (Citation1–4). The work context of a specific subgroup of regular EMS, helicopter emergency medical services (HEMS), is characterized by exceptionally high exposure to critical incidents when compared to other groups of EMS personnel. Furthermore, HEMS personnel have to deal with challenging working conditions, such as difficult locations and managing flight safety, and have to perform in a demanding psychosocial work context (Citation5–7). Other known occupational stressors are emotionally demanding patient encounters, fatigue, shift work, long working hours, and environmental stressors (Citation5, Citation8–10). While the wellbeing of HEMS personnel is a likely contributor to safe and successful care delivery (Citation10), there is a general lack of research focused on wellbeing and factors that affect the wellbeing of HEMS personnel.
Prior studies show that despite frequent exposure to critical incidents, employees who work in the prehospital setting report high levels of job satisfaction and resilience (Citation1, Citation11, Citation12). Furthermore, previous research provides insight into coping strategies used by prehospital personnel. Examples are keeping an emotional distance and focusing on technical aspects of the job (Citation13, Citation14). Sufficient time to recover, social support, and organizational support are known to be protective factors as well (Citation14–16). Support and recognition from supervisors and colleagues after a potentially traumatic event (PTE) are known to be associated with wellbeing (Citation15, Citation17, Citation18).
As opposed to a large body of literature on wellbeing and coping of ground-based personnel, a limited amount of studies assessing factors that affect the wellbeing of HEMS personnel are available. Canadian HEMS personnel self-reported lower levels of PTSD, depression, anxiety, and stress compared to ground-based personnel (Citation6). A study with HEMS pilots from four European countries indicated low to medium levels of perceived work stressors and high levels of motivation, wellbeing, and energy (Citation8). The studies imply that, despite the challenging work context, HEMS personnel are able to maintain their wellbeing. These results warrant further investigation. Therefore, with this qualitative study, we aimed to further our understanding of the factors underlying HEMS personnel’s wellbeing. This information could inform organizations regarding workplace interventions that can be implemented to support employees.
Methods
Setting
The HEMS team included in this study is based at a university hospital in The Netherlands. A HEMS team can be sent by a dispatcher but can also be requested by an ambulance crew that is already on site. The team is available 24/7 and members work 12.5 hour shifts. Per shift, a team of four roles is operational: a physician, a nurse/helicopter crew member (HCM), a pilot, and a driver/helicopter landing officer (HLO). The only full-time HEMS position is the pilot. It is obligatory for the others to combine it with another position. Physicians work 30% to 40% of their time at the HEMS and 60% to 70% at the university hospital. Nurses/HCMs are 40% to 50% employed at the HEMS and the remaining time at the emergency department of the university hospital or the ambulance service. The ambulance service is a separate organization from the university hospital. Drivers/HLOs work 25% on the HEMS team and 75% operating the ambulance. They receive medical training as part of their job at the ambulance service and are therefore able to provide medical assistance. All team members are trained in crew resource management. See for an overview of activities of the HEMS team included in this study in 2021.
Table 1. Overview of HEMS team activities in 2021.
Because most team members work at the HEMS part-time, team members differ per shift. In addition to the helicopter, the team also can use a car to respond to a call. The type of transport is determined based on a protocol that includes weather conditions. When the team is responding by helicopter, the driver/HLO remains at the dispatch station and when the team is being transported by car, this applies to the pilot. No tailor-made support or care structures are organized for the HEMS team specifically. It is protocol to perform a medical and technical debrief after each dispatch, during which the dispatch is discussed chronologically.
Participants and Procedure
In total, 43 members are employed on the HEMS team. Each was asked to register his or her HEMS role, tenure, sex, and age. We then used this information to select a diverse group of 16 participants for interviews. Of the 16 recruited, all agreed to participate. See for an overview of participant characteristics. Participation was voluntary and participants provided written informed consent to use their data for this study. The Medical Ethical Committee of Amsterdam University Medical Center exempted this research study from formal review (W19_495 # 20.013).
Table 2. Overview of interview participants (n = 16).
Data Collection: Interviews
Sixteen semi-structured interviews were conducted between February and April 2021, and each lasted between 60 and 75 minutes. We developed a topic list partially based on literature regarding wellbeing and psychosocial support in prehospital clinicians (Citation13, Citation14, Citation16, Citation19, Citation20), while leaving sufficient room for input from participants during the interviews. The topic list consisted of various topics on the following subjects: work context, the difference between HEMS and other occupations, HEMS roles, work characteristics, personal characteristics, coping, critical incidents, and psychosocial support.
Fifteen interviews were held face-to-face in a private room and one interview was conducted online. Five of the 16 interviews were conducted by two researchers, ensuring researcher triangulation in order to minimize bias in collecting the data. After three interviews, the researchers reviewed the interview topic list and added two new topics that emerged and were also discussed during the first three interviews. After eight interviews, a discussion took place among one author, the second interviewer (mentioned in the acknowledgments), and a second author. During this session, preliminary findings from the interviews were discussed, the topic list was reviewed, and it was concluded it did not need changes.
All interviews were audio-recorded and saved within a protected digital environment to which only three authors had access. All interviews were transcribed verbatim. The transcripts were assigned a code and did not contain immediately identifiable information, such as names or contact information. The interviews were held in Dutch and quotes presented in this study were translated from Dutch to English by one author and reviewed separately by a second author.
Analysis
We used a generic qualitative research approach, inspired by grounded theory (Citation21, Citation22). All interview transcripts were analyzed in MAXQDA2020, a qualitative data analysis software package. The analysis took place in the following steps: open coding, axial coding, and selective coding (Citation21). During open coding we divided the data into fragments while examining the transcript in detail. Next, we compared the fragments and grouped them into categories of the same topic, and assigned a code (Citation21). Open coding was applied to one interview by two authors independently, after which differences were discussed until a consensus was reached. This was repeated for three more interviews, ensuring researcher triangulation to increase the reliability of the analysis and to minimize bias. The remaining 12 interviews were coded by one author and the codes were discussed with a second author. During axial coding, categories were distinguished and it was determined if the codes developed thus far covered the data sufficiently. We also checked if each fragment was coded accordingly or whether a different code was more appropriate. We merged synonym codes and their fragments and assigned subcodes to main codes. This process was also discussed among two authors. Memos were written during the coding process.
During selective coding, codes were merged into categories consisting of different themes. We assessed the connections between the categories based on the coding process and our observations from the data while integrating them within the context of the study. This was discussed among four authors, to strive for intersubjectivity in interpretation. Based on our observations from the data, we created a visual representation to illustrate the relations between the categories. The analysis, interpretation, preliminary findings, and figure were discussed with two authors who are members of the research population, i.e., applying member validation (Citation21, Citation23). This led to a more fine-tuned analysis and visual representation. The final results and figure were also presented to the HEMS team to verify that they were in accordance with their perceptions.
Results
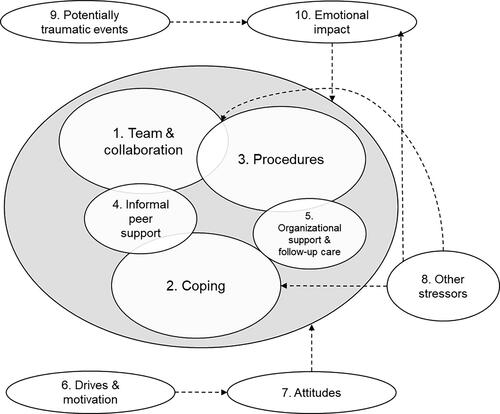
Qualitative analysis of the interviews revealed the various factors underlying HEMS personnel wellbeing and the role of the work context. We grouped our findings into ten categories which, taken together, provide insight into HEMS personnel wellbeing. Five of the ten categories were grouped into ‘core’ categories that represent the underlying elements of wellbeing of HEMS personnel. The remaining five categories were designated as ‘support’ categories, which we believe add context to the five ‘core’ categories. The ‘core’ categories are team and collaboration, coping, procedures, informal peer support and organizational support and follow-up care. The ‘support’ categories are drives and motivation, attitudes, other stressors, potentially traumatic events and emotional wellbeing. The categories and factors within these categories are related, as is presented in . A detailed overview of the categories and corresponding main themes can be found in the Appendix. We will describe each category, and explain how they are inter-related. Quotes from participants are presented to illustrate the findings and the relations between the categories.
Figure 1. Categories underlying the wellbeing of HEMS and their interrelations. Categories 1 – 5 in the grey circle constitute the ‘core’ categories that represent the underlying elements of wellbeing of HEMS personnel. Categories 6 – 10 are ‘support’ categories that add context to the ‘core’ categories.
Team and Collaboration
Participants described how they experienced the various aspects of the team and collaboration. Participants explained that good collaboration occurred when a dispatch was carried out with competent and calm colleagues. Participants commented colleagues needed to rely on each other during the dispatch, work closely together, complement one another, and maintain distinct roles. One participant stated: When the alarm goes off, everyone knows exactly what to do […] each new team member is drilled in that routine because otherwise it won’t work (physician). This quote illustrates how the collaboration is perceived and also how this relates to work procedures (see ).
Participants expressed a strong team mentality. They indicated all team members know each other very well because they work 12.5-hour shifts together and turnover is low. Another element of team mentality expressed by participants is that safety is paramount and the opinion of one team member is decisive. One participant stated: Well, if someone says no, then it’s a definite no. That’s easy. When the pilot says, “I can’t land on that spot safely”, then it’s a no (nurse/HCM).
Most participants indicated they perceive the HEMS team culture as open because they feel safe discussing mistakes in order to learn from those as a team. Participants commented that the team has open conversations and focuses on how they can improve their work procedures instead of holding mistakes against each other. They went on to comment that they feel free to express the emotional impact a dispatch can have. The described culture provides the opportunity for the provision of informal peer support (see ) because colleagues know each other well and are open with each other about various aspects related to work and wellbeing. However, not all team members seem to express such openness, as one participant explained: And I don’t know to what extent other people are affected [by a dispatch] […] it strikes me that not everybody shows their vulnerability by being honest (nurse/HCM).
Participants stated that friction or conflict occurs between team members sometimes, usually concerning choosing the type of transport. Participants expressed that staying behind at the dispatch station can create a sense of feeling excluded from the team. One participant stated: The team returns and you don’t know what they have experienced. […] What is the mood? What happened? Did it impact the team or not? […] It feels like you have to reconnect with the team. (pilot). This quote illustrates how a procedure relates to team and collaboration (see ).
Coping
Coping reflects how participants deal with the potential emotional impact of the HEMS work. The interviews showed that participants use various coping strategies before, during, and after a dispatch. In regard to before a dispatch, participants commented that they feel protected knowing that they are prepared for what they will encounter: Another important thing that makes a difference to me is that we often arrive at the scene second or third. By then the ambulance personnel have already started working, so it’s no longer as raw as when you arrive first (nurse/HCM). In addition, most participants expressed they focus on what they can control and accept that a patient’s fate is often predetermined. Several participants indicated they can be satisfied with their own actions – despite the outcome for the patient. Also, participants indicated that they get used to seeing trauma; this helps to deal with the effects.
During a dispatch, participants explained they keep an emotional distance by focusing on their actions and detaching emotionally from the patient: Because for me, in that moment, a child is an object. I have to perform my job on it. And whether it’s a nice child or not, I don’t look at that. But that’s mainly to protect myself (physician). Based on participants’ descriptions, this is a deliberate strategy that is used often. Participants stated they try to protect themselves in other ways as well, such as walking away or not looking at a deceased patient when this is not necessary.
After a dispatch or shift, different strategies are used by participants to process what they have experienced. Some participants indicated that the medical/technical debrief can help them to get a complete understanding of what happened: Debriefing is also a way of getting it off your chest, so to speak, which works from a medical point of view or if you are having a hard time with it. It helps to go through the entire process and all those questions in a very structured way. So that does help, even if you only talk about medical things, you can get it off your chest. (physician). Moreover, driving home was mentioned by participants as having a calming effect on them, helping to structure their thoughts, leave work behind, and transition to their personal lives.
An overarching and important coping strategy mentioned by participants is talking to colleagues with the same profession and discussing their actions to validate them. This illustrates how coping is related to informal peer support; talking about a dispatch with colleagues is perceived as helpful (see ). Participants commented that colleagues understand exactly what the HEMS work is about, which makes talking about the job easier. Furthermore, all participants indicated they seek support in their personal lives from their partners, family, or friends and they see a stable home situation as important. Participants stated that doing 'normal’ things at home such as cooking and watching TV helps them to wind down, distract themselves, and clear their heads.
Most participants indicated they would seek organizational support and follow-up care (see ) if they needed it, but also think that does not happen very often in the team. The perceived threshold to request professional support seems high to some participants. One participant stated: It would be a barrier for me to say that I want to have a conversation about it. I would have to have more severe complaints because of it, you know what I mean? (driver/HLO).
Procedures
Participants explained that combining HEMS work with another position at the hospital or ambulance service is important because this part-time structure stimulates maintenance of professional knowledge and skills, and limits exposure to PTEs. One participant commented: And I also think, if you only do this [HEMS] work, you will get a distorted view [of the world] (physician). Procedures provide the context in which participants work together (see team and collaboration, ).
Participants indicated that it is protocol to technically and medically debrief each dispatch. They explained that a debrief does not always happen, for example when a shift is too busy, when the team was canceled right after take-off, or when the dispatch was seen as standard procedure. During a debrief, a dispatch is evaluated chronologically, from start to finish. One participant stated: We always start with alarm and call, followed by planning and navigation. And after that we talk about the flight and then about being on the ground, and lastly we talk about the finalization (nurse/HCM). Some participants commented they perceive debriefing as organizational support and use it as a coping strategy (see ).
Informal Peer Support
In all interviews, participants talked about giving and receiving informal peer support. As stated above (3.1. Team and collaboration), there is strong team cohesion. Participants commented they notice abnormal behavior in team members and act upon this. They appreciate informal peer support, as one participant explains: What I really appreciate is when colleagues already suspect it, they will reach out to you. I don’t feel a barrier, but some people do feel that barrier. In that case, it’s very nice when a colleague notices this (nurse/HCM). This quote illustrates how colleagues can help each other in coping with the potential effects of the HEMS work (see ). Informal peer support seems to be provided automatically, and taking care of each other is perceived as vital to team members’ wellbeing. Most participants stated they see it as part of collaboration and they use it as a coping strategy (see ).
The majority of participants indicated they can talk to colleagues when a dispatch had an emotional impact on them. Some participants commented they perceive it as helpful to discuss their actions with a colleague in the same role, especially physicians. Also, most participants stated they experience humor and chatting with each other as supportive: We regularly have dinner together and drink coffee, things like that. That can be very nice, it differs per team (physician). This quote also illustrates how informal peer support relates to team and collaboration (see ).
Some participants wondered if the current informal peer support should be formalized because not all team members are as active: That also depends on one’s personality. To some people, it comes naturally and others want to do it but need some encouragement (nurse/HCM). Some participants indicated that the informal character could be a risk. One participant explained: If I would experience something distressing and I tell this to a colleague during the handover, I depend on whether or not that colleague thinks about it a week later and asks me how I’m doing (nurse/HCM).
Organizational Support and Follow-Up Care
There is no tailor-made organizational support or follow-up care provided specifically to the HEMS team. The majority of participants indicated they feel they do not need it: We also looked at whether there is a need to discuss our work with an outsider or to find professional psychological support. Looking at myself, I think that up until now I’ve always been able to discuss things within the team (pilot). This quote illustrates how informal peer support is used as a coping strategy (see ). Several participants indicated it was unclear to them where they could find organizational support.
Some participants expressed they think it would be difficult to arrange formal peer support in the HEMS team specifically, because of the unique work context and procedures (see ). The majority of participants stated that organizing formal peer support teams, as is the case within hospitals and ambulance services, would be very difficult. They went on to comment that if this would be formalized as post-dispatch meetings, it would mean a team is not available temporarily. Participants expressed this would be detrimental to the availability of the HEMS team and consequentially to patient care because there are only four HEMS teams in The Netherlands. Ambulance services are available but cannot perform the same advanced procedures as a HEMS team. Furthermore, participants indicated that all dispatches qualify to be discussed with formal peer support, which makes it unsustainable: Also, everything that is qualified for formal peer support to the ambulance services is our regular work. I mean, basically every HEMS dispatch is qualified for formal peer support (pilot). Some participants commented they see debriefing as organizational support, which is part of the HEMS work procedures (see ) and compared it to formal peer support: There is also room to discuss the entire dispatch. And of course that is also a kind of formal peer support meeting, during which you can get everything sorted out for yourself when you don’t have a good feeling about the dispatch (driver/HLO).
Conversely, a potential risk mentioned by participants is that they have to ask for support themselves instead of the organization actively providing it. Participants expressed that the perceived barrier to seeking support may be high because of the pressure to be operational at all times; this is related to participants’ attitudes and mindset (see attitudes and ). Participants went on to explain that the work context (see procedures, ) makes it difficult to follow up after incidents, because the team differs each shift.
Drives and Motivation
Participants are highly motivated and get a lot of energy from their work. One participant illustrates this: For me, it really is a world-class job. It makes me so happy. I really haven’t experienced a moment where it stresses me out or I don’t feel like going to work. No, there just isn’t any (pilot). Several participants indicated that joining the HEMS has been their ambition for a long time.
Participants indicated they get energy from the HEMS work because they are able to help people, it is challenging and exciting, and from working with a team. One participant explains: I really enjoy teamwork. Achieving optimal results with limited resources in as short a time as possible, that’s what I really like (physician). This quote also illustrates how motivation is associated with participants’ attitudes toward the HEMS work (see ). Furthermore, participants commented they perceive their work as diverse in terms of patients, locations, and colleagues, and hectic in a positive way. Participants stated they enjoy having to improvise when treating a patient with limited available resources. Participants explained the work gives them a sense of fulfillment; they like to be challenged and help people. This positively influences their attitude toward wanting to be operational at all times (see attitudes, ).
Attitudes
The category “attitudes” concerns how participants think about the other categories collaboration, procedures, coping, informal peer support and organizational support, and follow-up care (see ). Participants commented they expect a professional attitude from themselves and from their colleagues. They went on to explain they expect team members to be able to cope with the HEMS work: You have to be able to deal with it. […] Because if you can’t let it go, you’re going to have a hard time (physician). This quote illustrates this attitude toward coping (see ). The most important personal characteristic mentioned by participants is being a team player. Furthermore, participants expressed it is important that team members have an affinity for trauma care; however, this should not have characteristics of sensation-seeking. Other desirable personal characteristics that are mentioned by participants are being able to make pragmatic choices, showing flexibility, being able to perform under pressure, keeping calm, and the ability to follow through. These desired characteristics illustrate participants’ attitudes toward team and collaboration (see ).
Participants explained that being ready for the next dispatch is the team’s first priority. Participants are extremely motivated to work; they always keep going. Participants stated they want to be available at all times: Basically, no matter how bad it was, we report operational immediately. We debrief the previous dispatch in the time that we have, but when the alarm goes off we have to go again (physician). This quote also illustrates participants’ attitudes toward procedures (see ) and how their high drive and motivation play a role in this attitude (see ). Some participants indicated that they can perceive a barrier when it comes to sharing the need for a break between dispatches: When the alarm goes off, everyone wants to go immediately. Because that’s what we’re here for. So taking a break [and not being operational] is very difficult (driver/HLO). This quote illustrates the inter-relatedness between categories of attitudes and collaboration (see ). Participants commented that it is possible to report not operational, but it practically never happens.
Other Stressors
In addition to PTEs, participants also have to deal with other stressors. Stress at home, especially when having young children, is mentioned by most participants as a factor that can influence their work performance and coping, and vice versa (see ). One participant states: When things are not going well at home […]Then I will withdraw a bit more. When things at work are less pleasant, then you might take that home with you (pilot).
Several participants commented that night shifts and long shifts can be burdensome. Some participants expressed that when shifts are quiet, this can be boring, especially to those staying behind at the station: When the weather is nice, and they [the team] go out all day and I just sit there for 12 hours straight, well, that’s when I return home most spent. (driver/HLO).
Potentially Traumatic Events
HEMS teams are dispatched to critical cases with which they indicate they can cope well. But there are dispatches (PTEs) that are exceptional that can have an emotional impact on participants. All participants stated that dispatches with children have an emotional impact, regardless of their personal situation. One participant explains: For everyone, [dispatches involving] children are more confronting or burdening. People already get nervous when they know it is a child they have to go to. And then everybody is a little more on edge (physician). Participants also expressed that the emotions and despair of a patient’s family can have an emotional impact on them, often more than the suffering of the patient: The whole time you were occupied with the resuscitation of a child […] which is a technical procedure. For me, I can cope with that. The moment you stop [the procedure], there are the parents, who of course will cry vehemently, drop to their knees, who will scream. Those are the things that stick with me (nurse/HCM). This quote also illustrates the emotional impact an incident can have on team members (see ).
Furthermore, participants explained that when they can identify with the patient or situation this can affect them, especially when the situation has similarities with their personal (home) environments. Participants further indicated that (social) media can exacerbate the effects, as more information on the background and life of the patient makes them more relatable. Participants commented this makes it difficult to keep an emotional distance from the patient, and it involuntarily confronts them with the dispatch. Also, extreme situations, such as feeling unsafe after a shooting, were stated by participants as making them more aware of the harm people can inflict on each other. One participant illustrated: Extreme, really extreme things. That it’s just out of the ordinary. You will think, how can someone do something like that to a child? (Driver/HLO).
Furthermore, participants commented that doubts about their actions and feeling like they are losing control during a dispatch can have negative effects on them. A participant explained: I think mainly for all of us it’s about a loss of control. I think we all feel super secure because we know exactly what we’re doing and how we’re going to do it […] the situations where things take an unexpected turn, when we feel like there’s no control anymore, that is especially difficult for us (nurse/HCM).
Emotional Impact
HEMS teams are exposed to PTEs on a frequent basis. Some participants expressed that they keep thinking about a dispatch sometimes. Most participants stated this lasts a few days at most. Several participants indicated that they can recall any particular dispatch from a while ago when they want to, to even the smallest details. This illustrates how PTEs can have an emotional impact (see ).
Most participants report there are moments when they feel “out of balance”, meaning they feel something is off with their mood or wellbeing. Tell-tale signs mentioned by participants are feeling less energized, irritable, forgetful, or cranky: When I am out of balance, I often notice that when I am not able to think very clearly anymore, am not as focused anymore. (driver/HLO).
Some participants indicated that the HEMS work made them more careful: But it [HEMS work] has made me calmer and more careful, I think, in my own life (driver/HLO). They went on to indicate that the HEMS work also can influence their parenting style, e.g., being more protective or strict with their children and not allowing them to take up certain hobbies.
Most participants expressed they do not experience any sleeping problems, although occasionally a few do. Some participants noted experiencing negative emotions such as feeling tense, on guard, or feeling terrible when a patient dies. During the interviews, several participants wondered about how they cope with and process what they experience. They asked how it is possible that they are feeling fine and are mostly unbothered: But I do notice sometimes that I think ‘but everything you see, where does it all go? (nurse/HCM). Some participants wondered if it will hit them later, during retirement.
The emotional effects can have an influence on the other categories (see ); for example, how well a participant is able to cope with PTEs, work together to provide informal peer support, and their overall work performance.
Discussion
With this qualitative study, we aimed to further our understanding of the factors underlying The wellbeing of HEMS personnel to inform organizations in regard to workplace interventions that can be implemented to support employees. Various factors are of importance to HEMS personnel wellbeing, such as social support and team collaboration. Furthermore, different coping strategies are used to deal with the frequent exposure to PTEs. The perceived need for organizational support and follow-up care is low.
We found three consistent aspects of the HEMS work that can have an emotional impact. These were incidents involving children, identifying with the patient or the situation, and the emotions of a patient’s family. These results are consistent with prior research with ground-based personnel (Citation24, Citation25). Coping strategies found in this study, such as keeping an emotional distance from the patient by focusing on technical activities, have also been found in ambulance workers, paramedics, physicians, and nurses (Citation13, Citation14, Citation26). Furthermore, the importance of informal peer support found in this study is in accordance with prior research (Citation1, Citation17, Citation19, Citation24, Citation27), and has been associated with lower levels of distress in paramedics (Citation15). In addition to informal peer support, the reported benefits of medical and technical debriefing found in this study are in line with findings resulting from research with paramedics (Citation8, Citation14, Citation24). All of these factors can contribute to a supportive work environment. Prior research has found that a time-out period between dispatches can be beneficial (Citation16, Citation20, Citation27). Findings from this study, however, suggest that being operational at all times is of high importance to HEMS personnel and, as a result, a time-out period is rarely used by participants in this study, which could be a potential risk to their wellbeing.
The perceived need for organizational support or follow-up care is low among the participants in this study. This may be due to work culture, attitudes toward help-seeking, or not realizing the need for help, although it has been found that paramedics tend to have a high mental health literacy (Citation28). Another possible explanation based on previous research is a perceived barrier and/or help-seeking being stigmatized, e.g., afraid of being seen as weak or thinking it would have a negative effect on career progression (Citation27, Citation28).
The HEMS personnel reported various work aspects gave them energy, such as collaboration with colleagues, helping people, and positive challenges. Aspects of work that give employees energy are known in the literature as job resources (Citation29). According to the Job Demands-Resources model, job resources predict work (dis)engagement and help employees cope with aspects of the job that require sustained physical and/or psychological effort, i.e., job demands (Citation29–31). This could indicate that the high level of job resources and work engagement in HEMS personnel in this study helps them to maintain their wellbeing. It underlines the importance of supporting employees in maintaining their job resources.
The high motivation and work engagement found in this study may be contributing factors to HEMS personnel wellbeing. High motivation has been associated with higher job satisfaction and higher psychological wellbeing in nurses (Citation32). Our findings suggest that, in general, participants are able to maintain their wellbeing, congruent with studies with HEMS personnel reporting low levels of psychological complaints, high levels of wellbeing, and high work engagement (Citation5, Citation6, Citation9, Citation10).
Our study has some limitations to consider. The majority of the interviews and analysis were conducted by one researcher. However, as recommended in the literature (Citation21), multiple researchers were involved in conducting part of the interviews and analyzing the data and the analysis and interpretations were discussed in a team of researchers. This use of researcher triangulation strengthened the rigor of the data collection and data analysis. Although we aimed to include a diverse group of participants, differences in culture, and operational and organizational procedures should be taken into account when applying the results to inform policy making decisions in other high-risk occupational settings. As prescribed in the literature, we used member validation to strengthen the quality and applicability of the results (Citation21, Citation23). While we carefully selected participants based on several characteristics, selection bias cannot be ruled out completely.
Conclusion
With this qualitative study, we identified factors and strategies that support the wellbeing of HEMS personnel. We showed that several factors are important, such as working together with colleagues, being challenged, helping people, and social support. In addition, HEMS personnel use various coping strategies to deal with the frequent exposure to PTEs, such as seeking support from colleagues and keeping an emotional distance. The perceived need for organizational support and follow-up care is low and seen as complicated given the unique work context. We believe these results can inform organizations regarding workplace interventions that can be implemented to support employees.
Acknowledgments
We would like to thank Charlie Steen for her help in designing the figure and Ine Spee for her help with conducting part of the interviews.
Disclosure Statement
Author MdL is a member of the Gerbrand de Jong Fonds. This study has been conducted by the independent research center ARQ Center of Expertise for the Impact of Disasters and Crises. The funders had no influence on the outcomes of this study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author MvH. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Additional information
Funding
References
- Alexander DA, Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br J Psychiatry. 2001;178(1):76–81. doi:10.1192/bjp.178.1.76.
- Stevelink SAM, Pernet D, Dregan A, Davis K, Walker-Bone K, Fear NT, Hotopf M. The mental health of emergency services personnel in the UK Biobank: a comparison with the working population. Eur J Psychotraumatol. 2020;11(1):1799477. doi:10.1080/20008198.2020.1799477.
- Berger W, Coutinho ESF, Figueira I, Marques-Portella C, Luz MP, Neylan TC, Marmar CR, Mendlowicz MV. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):1001–11. doi:10.1007/s00127-011-0408-2.
- Petrie K, Milligan-Saville J, Gayed A, Deady M, Phelps A, Dell L, Forbes D, Bryant RA, Calvo RA, Glozier N, et al. Prevalence of PTSD and common mental disorders amongst ambulance personnel: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):897–909. doi:10.1007/s00127-018-1539-5.
- Radstaak M, Geurts SA, Beckers DG, Brosschot JF, Kompier MA. Recovery and well-being among Helicopter Emergency Medical Service (HEMS) pilots. Appl Ergon. 2014;45(4):986–93. doi:10.1016/j.apergo.2013.12.002.
- Harenberg S, McCarron MCE, Carleton N, O'Malley T, Ross T. Experiences of trauma expression anxiety and stress in Canadian HEMS. J Community Saf Well-Being. 2018;3(2):18–21. doi:10.35502/jcswb.62.
- Cowley A, Durge N. The impact of parental accompaniment in paediatric trauma: a helicopter emergency medical service (HEMS) perspective. Scand J Trauma Resusc Emerg Med. 2014;22(1):1–5. doi:10.1186/1757-7241-22-32.
- Bauer H, Herbig B. Occupational stress in helicopter emergency service pilots from 4 European countries. Air Med J. 2019;38(2):82–94. doi:10.1016/j.amj.2018.11.011.
- Reid BO, Haugland H, Abrahamsen HB, Bjornsen LP, Uleberg O, Kruger AJ. Prehospital stressors: a cross-sectional study of Norwegian helicopter emergency medical physicians. Air Med J. 2020;39(5):383–8. doi:10.1016/j.amj.2020.05.016.
- Sallinen M, Laukkanen-Nevala P, Puttonen S, Virkkunen I, Vanttola P, Olkinuora A. Well-being at work among helicopter emergency medical service personnel in Finland. 2019. http://www.julkari.fi/handle/10024/138164.
- Gayton SD, Lovell GP. Resilience in ambulance service paramedics and its relationships with well-being and general health. Traumatology. 2012;18(1):58–64. doi:10.1177/1534765610396727.
- Streb M, Haller P, Michael T. PTSD in paramedics: resilience and sense of coherence. Behav Cogn Psychother. 2014;42(4):452–63. doi:10.1017/S1352465813000337.
- Regehr C, Goldberg G, Hughes J. Exposure to human tragedy, empathy, and trauma in ambulance paramedics. Am J Orthopsychiatry. 2002;72(4):505–13. doi:10.1037/0002-9432.72.4.505.
- Avraham N, Goldblatt H, Yafe E. Paramedics’ experiences and coping strategies when encountering critical incidents. Qual Health Res. 2014;24(2):194–208. doi:10.1177/1049732313519867.
- Gouweloos-Trines J, Tyler MP, Giummarra MJ, Kassam-Adams N, Landolt MA, Kleber RJ, Alisic E. Perceived support at work after critical incidents and its relation to psychological distress: a survey among prehospital providers. Emerg Med J. 2017;34(12):816–22. doi:10.1136/emermed-2017-206584.
- Halpern J, Gurevich M, Schwartz B, Brazeau P. Interventions for critical incident stress in emergency medical services: a qualitative study. Stress Health. 2009b;25(2):139–49. doi:10.1002/smi.1230.
- Olff M. Bonding after trauma: on the role of social support and the oxytocin system in traumatic stress. Eur J Psychotraumatol. 2012;3(1):18597. doi:10.3402/ejpt.v3i0.18597.
- Van Herpen MM, Te Brake H, Olff M. Stress at work: self‐monitoring of stressors and resources to support employees. Stress Health. 2021;38(2):402–9.
- Regehr C, Millar D. Situation critical: high demand, low control, and low support in paramedic organizations. Traumatology. 2007;13(1):49–58. doi:10.1177/1534765607299912.
- Halpern J, Gurevich M, Schwartz B, Brazeau P. What makes an incident critical for ambulance workers? Emotional outcomes and implications for intervention. Work Stress. 2009;23(2):173–89. doi:10.1080/02678370903057317.
- Boeije H. Analysis in qualitative research. London: Sage publications; 2010.
- Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3–21. doi:10.1007/BF00988593.
- Cutcliffe JR, McKenna HP. When do we know that we know? Considering the truth of research findings and the craft of qualitative research. Int J Nurs Stud. 2002;39(6):611–8. doi:10.1016/S0020-7489(01)00063-3.
- Clompus SR, Albarran JW. Exploring the nature of resilience in paramedic practice: a psycho-social study. Int Emerg Nurs. 2016;28:1–7. doi:10.1016/j.ienj.2015.11.006.
- Compton S, Madgy A, Goldstein M, Sandhu J, Dunne R, Swor R. Emergency medical service providers’ experience with family presence during cardiopulmonary resuscitation. Resuscitation. 2006;70(2):223–8.
- Sorensen R, Iedema R. Emotional labour: clinicians’ attitudes to death and dying. J Health Organ Manage. 2009;23(1):5–22. doi:10.1108/14777260910942524.
- Auth NM, Booker MJ, Wild J, Riley R. Mental health and help seeking among trauma-exposed emergency service staff: a qualitative evidence synthesis. BMJ Open. 2022;12(2):e047814. doi:10.1136/bmjopen-2020-047814.
- Krakauer RL, Stelnicki AM, Carleton RN. Examining mental health knowledge, stigma, and service use intentions among public safety personnel. Front Psychol. 2020;11:1–7. doi:10.3389/fpsyg.2020.00949.
- Bakker AB, Demerouti E. Job demands–resources theory: taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–85. doi:10.1037/ocp0000056.
- Xanthopoulou D, Bakker AB, Demerouti E, Schaufeli WB. The role of personal resources in the job demands-resources model. Int J Stress Manage. 2007;14(2):121–41. doi:10.1037/1072-5245.14.2.121.
- Bakker AB, Van Veldhoven M, Xanthopoulou D. Beyond the demand-control model. J Personnel Psychol. 2010;9(1):3–16. doi:10.1027/1866-5888/a000006.
- Elhosany WA-E, Helal OM. The relationship between psychological wellbeing and work motivation among staff nurses in governmental hospitals in Port Said. Port Said Sci J Nurs. 2020;7(4):21–39.

