Abstract
Background
Pelvic fractures resulting from high-energy trauma can frequently present with life-threatening hemodynamic instability that is associated with high mortality rates. The role of pelvic exsanguination in causing hemorrhagic shock is unclear, as associated injuries frequently accompany pelvic fractures. This study aims to compare the incidence of hemorrhagic shock and in-hospital outcomes in patients with isolated and non-isolated pelvic fractures.
Methods
Registries-based study of trauma patients hospitalized following pelvic fractures. Data from 1997 to 2021 were cross-referenced between the Israel Defense Forces Trauma Registry (IDF-TR), documenting prehospital care, and Israel National Trauma Registry (INTR) recording hospitalization data. Patients with isolated pelvic fractures were defined as having an Abbreviated Injury Scale (AIS) <3 in other anatomical regions, and compared with patients sustaining pelvic fracture and at least one associated injury (AIS ≥ 3). Signs of profound shock upon emergency department (ED) arrival were defined as either a systolic blood pressure <90 mmHg and/or a heart rate >130 beats per min.
Results
Overall, 244 hospitalized trauma patients with pelvic fractures were included, most of whom were males (84.4%) with a median age of 21 years. The most common injury mechanisms were motor vehicle collisions (64.8%), falls from height (13.1%) and gunshot wounds (11.5%). Of these, 68 (27.9%) patients sustained isolated pelvic fractures. In patients with non-isolated fractures, the most common regions with a severe associated injury were the thorax and abdomen. Signs of shock were recorded for 50 (20.5%) patients upon ED arrival, but only four of these had isolated pelvic fractures. In-hospital mortality occurred among 18 (7.4%) patients, all with non-isolated fractures.
Conclusion
In young patients with pelvic fractures, severe associated injuries were common, but isolated pelvic fractures rarely presented with profound shock upon arrival. Prehospital management protocols for pelvic fractures should prioritize prompt evacuation and resuscitative measures aimed at addressing associated injuries.
Introduction
Pelvic fractures may occur during high-energy trauma and are traditionally considered a cause of potentially life-threatening hemodynamic instability (Citation1–5). Although pelvic fractures account for approximately 3% of all fractures, they are associated with disproportionately high morbidity and mortality, posing a significant burden on both individuals and healthcare systems worldwide (Citation6, Citation7). Patients with pelvic fractures presenting with hemodynamic instability have particularly high mortality rates, previously ranging from approximately 30% (Citation5, Citation8) to upward of 50% (Citation9). Although bleeding due to pelvic fractures may arise from venous, arterial, and bone structures (Citation1, Citation2, Citation10), these injuries are frequently accompanied by other sources of bleeding, such as thoracic or abdominal trauma, resulting from high-energy mechanisms (Citation11, Citation12). Therefore, it remains unclear whether pelvic exsanguination alone can fully account for the high rates of hemodynamic instability and mortality or whether these are largely determined by the extent and severity of associated injuries (Citation8, Citation11–15).
In the prehospital setting, the use of pelvic compression devices remains a widely accepted practice among patients suspected of pelvic fractures (Citation1, Citation2, Citation16–19). Pelvic compression devices are thought to restrict hemorrhage by limiting bleeding from fracture sites, and increasing pelvic stability while promoting clot formation (Citation2, Citation10). Although these devices are widely utilized by prehospital advanced life support (ALS) teams, evidence regarding their benefits remains conflicting (Citation16), and their use by prehospital teams may come at the expense of evacuation time or other resuscitative measures. As such, distinguishing the sources of potentially life-threatening hemorrhage among patients with pelvic fractures could inform the prioritization of prehospital interventions to optimize care while avoiding a delay in evacuation.
In 2022, the Israel Defense Forces Medical Corps (IDF-MC) first implemented the use of pelvic compression devices for use in the prehospital setting when a significant blunt or penetrating pelvic injury is suspected. This study leverages data from two databases capturing the prehospital and in-hospital course of trauma patients cared for by IDF-MC clinicians between 1997–2021, predating the implementation of pelvic binding. The purpose of this study is to compare the incidence of hemorrhagic shock upon arrival at the emergency department (ED) in patients with isolated and non-isolated pelvic fractures, and to assess the in-hospital outcomes for each group.
Methods
Study Design and Setting
We used an observational cohort study design utilizing the Israel Defense Forces Trauma Registry (IDF-TR), focusing on patients hospitalized with pelvic fractures and treated by IDF Advanced Life Support (ALS) teams in the prehospital setting between 1997 and 2021. The IDF ALS teams offer prehospital trauma care to both civilians and military personnel injured in the vicinity of military bases or during operations. Patients requiring further care are then transferred to civilian hospitals within Israel. Prehospital care is documented by IDF clinicians on casualty cards and subsequently recorded in the IDF-TR (Citation20). Additional documentation of injury circumstances, clinical course, and prehospital treatment is conducted by clinicians through a web-based portal, supplementing the information present on the casualty cards. The Israel National Trauma Registry (INTR) maintains a digital database of ED and inpatient care provided to patients with traumatic injuries (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 800–959.9). Patients included in the database are those who are hospitalized or died following ED admission. Patients pronounced dead prior to hospital arrival are not included in the registry (Citation21). Data from the IDF-TR were cross-referenced with matching hospitalization records extracted from the INTR, as previously described (Citation22). Matching of records was performed by comparing Israeli state-issued identification numbers which are individualized and therefore constitute definitive matching of patient records. The IDF Medical Corps Institutional Review Board (#Protocol number: 1948–2018) approved this study. This manuscript adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) recommendations for observational studies (Citation23).
This study included hospitalized patients with traumatic pelvic fractures, identified by querying the INTR for ICD-9-CM codes 808.0–808.9. Fractures were further grouped according to fracture site as has been previously described (Citation7): closed or open fracture of acetabulum (808.0 and 808.1), closed or open fracture of pubis (808.2 and 808.3), closed or open fracture of ilium (808.41 and 808.51), closed or open fracture of ischium (808.42 and 808.52), closed or open fracture of sacrum or coccyx (805.6 and 805.7), multiple closed or open fractures of pelvis (808.43, 808.44, 808.53, and 808.54), or closed or open fracture of other or unspecified part of pelvis (808.49, 808.59, 808.8, and 808.9). Fractures were also stratified to open or closed as per the aforementioned ICD-9-CM codes within this range. Patients with missing documentation of vital signs (blood pressure or heart rate) upon ED arrival were excluded from the study.
Variables and Definitions
Injury severity and regional distribution were assessed utilizing the Abbreviated Injury Scale (AIS) with severe injury defined as AIS ≥ 3 in any body region. Patients with an AIS < 3 in all regions other than the pelvis were defined as having an isolated pelvic fracture. Notably, pelvic fractures are classified under the lower extremity region in the AIS scale. Consequently, and for purposes of this study, we describe severe injuries in the lower extremity region (AIS ≥ 3) are by both taking into account and excluding the contribution of pelvic fractures (i.e., overall lower extremity AIS and lower extremity AIS excluding pelvic fractures).
Profound shock was the primary outcome in this study and ascertained using vital signs recorded upon ED arrival and defined as (Citation1) systolic blood pressure < 90 mmHg and/or (Citation2) heart rate > 130 beats per min. These criteria correspond with those outlined in the IDF-MC Clinical Practice Guidelines for determining profound shock during the study period (Citation22, Citation24). Secondary outcomes included hospital length of stay, intensive care unit (ICU) admission, and in-hospital mortality. Variables extracted from the IDF-TR included injury mechanism, injury setting (military vs. civilian) and prehospital life-saving interventions (tourniquet, hemostatic dressing use, blood products, etc.). The INTR database was utilized to evaluate Injury Severity Score (ISS), blood product administration in the ED and documented surgical interventions during hospitalization. In-hospital fracture related procedures were ascertained using ICD-9-CM codes, range 79.00–79.99, as has been described in previous research (Citation7).
Statistical Analysis
Continuous variables are described as medians and interquartile ranges (IQR) and were compared using the Kruskal-Wallis test due to the lack of normality in the data. Categorial variables are described as n (%). To compare larger contingency tables of categorical variables, the chi-squared test was used, while for 2 × 2 tables, Fisher’s exact test was employed. P-values of less than 0.05 were considered statistically significant for all tests. All statistical analyses were performed using R software version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Population
Overall, 244 hospitalized trauma patients with pelvic fractures and ED vital sign documentation were included. Six patients with pelvic fractures were excluded due to missing hemodynamic vital signs upon arrival to the ED (). The study population included predominantly males (84.4%), with a median age of 21 (IQR 19–25). The most common injury mechanisms were motor vehicle collisions (64.8%), falls from height (13.1%), and gunshot wounds (11.5%) with 16.0% of all patients sustaining a penetrating injury. Injury Severity Score (ISS) was ≥25 for 99 (40.6%) patients. summarizes the demographics and injury characteristics of the study population.
Figure 1. Flow diagram of casualties included in the study. Abbreviations: IDF-TR = Israel Defense Forces Trauma Registry; INTR = Israel National Trauma Registry.
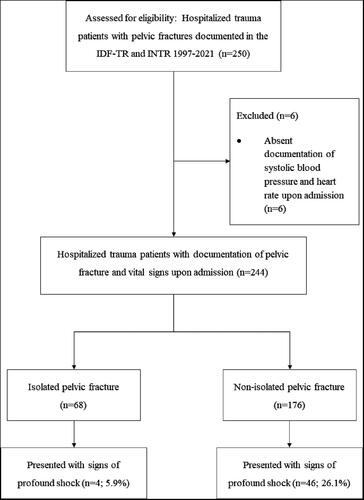
Table 1. Baseline and injury characteristics of study population, stratified by presence of isolated vs. non-isolated pelvic fracture.
Pelvic Fractures and Associated Injuries
Overall, 68 (27.9%) patients sustained isolated pelvic fractures, implying that there were no severe associated injuries (AIS ≥ 3) to other body regions. In the isolated pelvic fracture group 33 (48.5%) had a lower extremity AIS ≥ 3, attributed solely to the pelvic injury. Among patients with non-isolated fractures (n = 176), the most common regions with a severe associated injury were the thorax (55.7%), abdomen (47.7%), lower extremity excluding the presence of pelvic fracture (36.4%), and head (33.5%).
Among the entire study population (n = 244), the overall rate of open pelvic fractures was 17.2%, with no significant differences between patients with isolated versus non-isolated fractures. The most common fracture site was the pubis (n = 120, 49.2%), followed by the acetabulum (n = 93, 38.1%) and sacrum or coccyx (n = 57, 23.4%) with no significant differences in these fracture sites between isolated and non-isolated fractures.
Prehospital Treatment of Pelvic Fractures
describes the prehospital and in-hospital treatment of the study population. In the prehospital setting, 43 (17.6%) patients received crystalloids, 15 (6.1%) received freeze-dried plasma, and 25 (10.2%) were administered tranexamic acid, with no significant differences in proportions between the two groups. Prehospital endotracheal intubation was performed for 38 (15.6%) patients, all with non-isolated fractures. Prehospital pelvic binding was not recorded for any patients, as it was not recommended in the IDF-MC guidelines during the study period. Following hospital arrival 41 (19.3%) patients received blood products, of which only three had isolated fractures (7.3%).
Table 2. Prehospital and in-hospital interventions administered to the study population.
Profound Shock and in-Hospital Outcomes
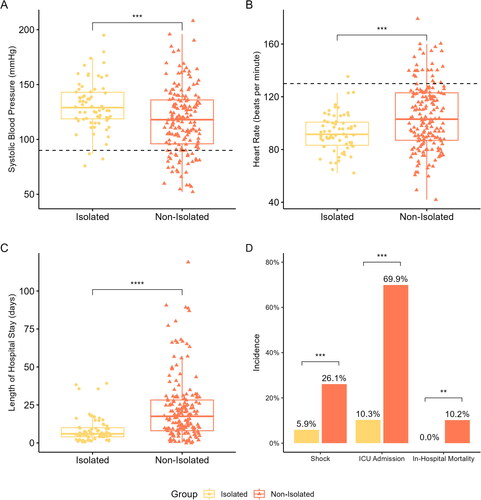
Prehospital vital signs were largely undocumented for the study population (Online Supplemental Table S1). Upon ED arrival, 50 (20.5%) patients presented with signs of shock. Only four (5.9%) of these patients had isolated fractures (), as compared with 46 (26.1% of non-isolated) patients with severe associated injuries (p < 0.001). depicts the vital signs upon hospital presentation and in-hospital outcomes of the study population. Patients with non-isolated fractures were more frequently admitted to the ICU (non-isolated: 69.9% vs. isolated: 10.3%; p < 0.001) and had longer median hospital length of stay (non-isolated: 18 [IQR 8–28] days vs. isolated: 6 [IQR 4–10] days; p < 0.001) as compared with patients with isolated fractures. Patients with non-isolated fractures more frequently underwent fracture related surgery (p < 0.001), including external fixation (p = 0.018), open reduction with external fixation (p = 0.029), and closed reduction with internal fixation (p < 0.001). In-hospital mortality occurred among 18 (7.4%) patients with non-isolated fractures, with no mortality among patients with isolated fractures.
Figure 2. Comparison of the vital signs and in-hospital outcomes of patients with isolated and non-isolated pelvic fractures. Boxplots compare the systolic blood pressure (A) and heart rate (B) upon emergency department arrival as well as hospital length of stay (C) between the groups. Panel D compares the proportions of presentation with signs of profound shock upon arrival, intensive care unit (ICU) admission and in-hospital mortality. **P < 0.01, ***P < 0.001, and ****P < 0.0001.
Discussion
Pelvic fractures are a cause of significant morbidity, and hemorrhagic shock following pelvic fractures is associated with substantial mortality (Citation5, Citation8, Citation13, Citation25). However, due to the high incidence of associated injuries coinciding with pelvic fractures, it is unclear whether hemorrhagic shock can be directly linked to pelvic fractures or rather results from other injuries. In this registry-based cohort study, profound shock upon ED arrival was rare among patients with isolated pelvic fractures, and in-hospital mortality occurred only among patients with non-isolated fractures. Notably, most patients suffering from pelvic fractures had at least one severe associated injury. Presentation with shock, hospital length of stay, ICU admission and in-hospital mortality were all significantly higher in patients with associated injuries, with no significant differences in injury mechanism. Of note, patients with non-isolated pelvic fractures also had significantly higher rates of operative fracture treatment, for either pelvic fractures or fractures in other regions. These findings may suggest that while pelvic fractures are frequently associated with additional severe injuries, when presenting as an isolated injury, they seldom result in hemorrhage significant enough to induce hemorrhagic shock during the prehospital phase of care.
Among this study population, more than 20% of patients presented to the ED with signs of shock and over 50% were admitted to the intensive care unit, highlighting the serious nature of traumatic pelvic fractures in a young population. Bleeding resulting from pelvic fractures is believed to predominantly stem from venous fracture sites, but more extensive bleeding from both the intrapelvic vasculature and osseous sources may lead to hemodynamic compromise (Citation25, Citation26). Demetriades et al. (Citation27) reported that 60.6% of patients with severe pelvic fractures required blood transfusion (mean transfusion volume of 3,540 mL). In a sub-group of isolated severe pelvic fractures, 50.6% required blood transfusions (mean volume of 2,718 mL). Therefore, early intervention aimed at achieving hemostasis may benefit patients with bleeding from pelvic fractures.
In the prehospital setting, the primary measures to address severe pelvic hemorrhage include pelvic binding and hemostatic resuscitation aiming to restore circulating volume and potentially correct trauma-induced coagulopathy (Citation28, Citation29). Use of both dedicated products for binding, along with the makeshift application of items such as bed sheets in potentially reducing and stabilizing pelvic fractures has been suggested (Citation28, Citation29). However, in contrast to some previous publications (Citation12, Citation30), the results of this study suggest that hemorrhagic shock instigated solely by pelvic fractures may be rare. One possible explanation for these findings may be the relatively young cohort (median age of 21 years) in this study, which may be characterized by increased physiologic reserves as compared with other patient cohorts.
The high prevalence of signs of profound shock (26.1%) and in-hospital mortality (10.2%) among patients with non-isolated pelvic fractures suggests that the associated injuries significantly affected patient outcomes. The most common regions with a severe associated injury were the thorax (40.2%) and abdomen (34.4%), followed by lower extremity injuries (26.2%). These rates of severe associated injuries are higher than has been previously documented. In a registry-based analysis of 1,545 patients with pelvic fracture, Demetriades and colleagues (Citation12) reported that 16.5% suffered from abdominal injuries. Giannoudis et al. (Citation31) found that concomitant severe injuries (AIS ≥ 3) in the chest (21.2%) and head (16.9%) were the most common among a large cohort of patients with pelvic ring fractures. In this study, patients with associated injuries had significantly longer hospital lengths of stay and rates of ICU admission, and importantly, in-hospital mortality was only recorded among patients with non-isolated pelvic fractures. The substantially higher rates of severe associated injuries may also be attributed to the age distribution of our cohort. While low-energy trauma, such as ground-level falls may cause a pelvic fracture in the elderly population (Citation32), the substantial force required to produce pelvic fractures among young adults may frequently result in other severe injuries. Verbeek et al. (Citation33) demonstrated the latter, showing that older patients with pelvic fractures were significantly less likely to present with severe associated injuries. Therefore, the management of young patients with suspected pelvic fractures should involve a high suspicion for severe concomitant injuries in other regions, which may be the key determinant of patient outcomes (Citation11).
In our study the leading cause of pelvic fractures was motor vehicle accidents, accounting for 64.5% of cases. Falls from height were the second most common cause, while the remaining 22.7% of injuries were attributed to other mechanisms. Although falls comprise a larger proportion of pelvic fracture etiology in elderly populations, road or traffic-related injuries are the leading cause of pelvic fractures in younger populations worldwide (Citation6). As such, depending on the patient population, some studies have reported that motor vehicle accidents accounted for approximately 60% (Citation34–36) to 77% (Citation37) of pelvic fractures. In our cohort, which included injuries occurring in both civilian and military settings, combat-related injury mechanisms served as the primary mechanism in 15% of cases, including blast and gunshot wounds. Parker et al. (Citation38) recently presented the US military experience with managing pelvic fractures in recent conflicts, demonstrating that most were caused by explosive devices and frequently occur with severe lower extremity injuries. Although high-energy blunt injuries are generally a far more frequent cause of pelvic fractures, penetrating pelvic trauma which is more typical in conflict settings, may further complicate the management of such patients. In addition to pelvic fractures, patients with penetrating pelvic trauma are at high risk of sustaining visceral injuries involving the intrapelvic vasculature, gastrointestinal, and genitourinary tracts (Citation39). The complex management of penetrating pelvic injuries remains debated (Citation40, Citation41), and the literature is scarce on the prehospital management of these injuries. Specifically, the efficacy of interventions such as prehospital binding in controlling intrapelvic hemorrhage resulting from penetrating injuries remains unclear. Currently, the IDF-MC guidelines recommend the use of pelvic binders for high-energy penetrating pelvic trauma, even when a fracture is not clearly apparent. However, more research is needed to evaluate the effectiveness of this intervention.
The high morbidity and mortality associated with pelvic fractures underscore the importance of the initial management of these injuries. Although pelvic binders are widely used in cases of suspected fractures (Citation1, Citation2), and recommended by the Advanced Trauma Life Support (ATLS®) guidelines (Citation42), their role in controlling life-threatening hemorrhage remains uncertain (Citation43). The reduction and stabilization of pelvic binders are believed to decrease fracture site bleeding while protecting any initial blood clot from disruption. The decrease in the pelvic volume may create a tamponade thus reducing venous bleeding (Citation44). However, some have argued that achieving a tamponade effect via external compression in cases of severe hemorrhage is unlikely, as such bleeding is assumed to arise from arterial sources (Citation43). Additionally, it is worth noting that the use of pelvic binders has been associated with high rates of improper placement and rarely, damage to the skin, soft tissue, and peripheral nerves (Citation2, Citation10, Citation45). Despite these concerns, in 2022, the IDF-MC guidelines for the prehospital management of orthopedic trauma recommended early use of pelvic binders during the primary survey for patients with external signs of blunt or penetrating pelvic injury (Citation46). However, this study suggests that associated injuries are the primary cause of profound shock in young patients with pelvic fractures and that their timely treatment should be prioritized to improve outcomes. Therefore, the prehospital application of pelvic binders should not delay evacuation or defer crucial resuscitative measures such as blood product transfusions in hemorrhaging patients. Recent US military experience has also shown that prehospital pelvic binding is underutilized despite being recommended in guidelines (Citation38), highlighting the need for further research to evaluate its impact on patient hemodynamics and identify sub-populations of patients who may benefit from its early use. Finally, additional techniques such as resuscitative endovascular balloon occlusion of the aorta (REBOA) have also been suggested as adjuncts to achieving hemostasis in cases of severe pelvic hemorrhage (Citation47, Citation48), and further data are required to evaluate their potential role in the prehospital armamentarium.
Limitations
There are several limitations to this study. First, this is an observational registry-based study and our ability to infer causation is limited. The use of registry data may be subject to missing or incomplete data, particularly with regards to prehospital care and assessment. Additionally, the use of two cross-referenced registries may lead to the exclusion of patients who cannot be matched due to missing identification numbers in either registry. This study encompasses a 25-year span of registry-based data, and thus, variations in practices or the introduction of interventions, such as prehospital blood product administration (Citation24), could impact the emergence of shock or patient survival, as explored in this manuscript. Nevertheless, when comparing the distinct time frames within the study, we did not observe significant differences in either the characteristics of pelvic fractures or the rates of shock and in-hospital mortality (Online Supplemental Table S3). An additional limitation is that patients with pelvic fractures who died on-scene or prior to hospital admission were not included in the analysis due to their absence from the INTR. As a result, the epidemiology of mortality or early signs of profound shock resulting from pelvic fractures may be underestimated. The determination of profound shock was established through the evaluation of vital signs upon admission to the ED. However, this approach may not capture patients who presented with profound shock in the prehospital setting but underwent stabilizing measures, such as volume resuscitation, prior to ER assessment. Furthermore, it is worth noting that pelvic binders were not routinely used in the IDF during the study period. Therefore, we cannot comment on their potential impact on patients’ vital signs or outcomes. Finally, this study focused solely on outcomes observed during the initial hospitalization and did not examine other important outcomes such as long-term morbidity and mortality.
Conclusions
Our study found that over 25% of patients with pelvic fractures in the prehospital setting presented to the ED with signs of profound shock. However, for isolated pelvic fractures, signs of shock were rare and no in-hospital mortality was recorded, suggesting that when presenting as an isolated injury, hemorrhage caused by pelvic fractures may rarely be sufficient in causing profound shock during prehospital care. These results may have implications for prehospital pelvic management protocols and suggest that external compression should be used without delaying evacuation or resuscitative measures aimed at addressing associated injuries.
Supplemental Material
Download MS Word (204.4 KB)Acknowledgments
We would like to thank the Israel Trauma Group for their continued collaborative efforts, enabling follow-up and insights on the course of trauma patients along the continuum of care.
Disclosure Statement
The authors declare no conflict of interests. This work was conducted as part of the Israel Defense Forces Medical Corps Trauma and Combat Medicine Branch’s efforts for quality control and improvement in trauma care and did not receive any designated funding.
References
- Bonner TJ, Eardley WGP, Newell N, Masouros S, Matthews JJ, Gibb I, Clasper JC. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br. 2011 Nov;93(11):1524–8. Available from http://www.ncbi.nlm.nih.gov/pubmed/22058306 doi:10.1302/0301-620X.93B11.27023.
- Hsu SD, Chen CJ, Chou YC, Wang SH, Chan DC. Effect of early pelvic binder use in the emergency management of suspected pelvic trauma: a retrospective cohort study. Int J Environ Res Public Health. 2017 Oct 12;19(11):1217. doi:10.3390/ijerph19116654.
- Mi M, Kanakaris NK, Wu X, Giannoudis PV. Management and outcomes of open pelvic fractures: an update. Injury. 2021 Oct 1;52(10):2738–45. doi:10.1016/j.injury.2020.02.096.
- Hermans E, Edwards MJR, Goslings JC, Biert J. Open pelvic fracture: the killing fracture? J Orthop Surg Res. 2018 Apr 13;13(1):83. doi:10.1186/s13018-018-0793-2.
- Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano R, Blackburn A, et al. Current management of hemorrhage from severe pelvic fractures: results of an American Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg. 2016;80(5):717–25. doi:10.1097/TA.0000000000001034.
- Hu S, Guo J, Zhu B, Dong Y, Li F. Epidemiology and burden of pelvic fractures: results from the Global Burden of Disease Study 2019. Injury. 2023 Feb 1;54(2):589–97. doi:10.1016/j.injury.2022.12.007.
- Buller LT, Best MJ, Quinnan SM. A nationwide analysis of pelvic ring fractures: incidence and trends in treatment, length of stay, and mortality. Geriatr Orthop Surg Rehabil. 2016 Mar 1;7(1):9–17. Available from: doi:10.1177/2151458515616250.
- Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano RD, Blackburn A, Scalea TM, Stein DM, Williams L, Conflitti J, et al. Pelvic fracture pattern predicts the need for hemorrhage control intervention-Results of an AAST multi-institutional study. J Trauma Acute Care Surg. 2017;82(6):1030–8. Available from https://journals.lww.com/jtrauma/Fulltext/2017/06000/Pelvic_fracture_pattern_predicts_the_need_for.8.aspx
- Eastridge BJ, Starr A, Minei JP, O’keefe GE. The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. 2002.
- DuBose JJ, Burlew CC, Joseph B, Keville M, Harfouche M, Morrison J, Fox CJ, Mooney J, O'Toole R, Slobogean G, et al. Pelvic fracture-related hypotension: a review of contemporary adjuncts for hemorrhage control. J Trauma Acute Care Surg. 2021 Oct 1;91(4):e93–103–e103. Available from http://www.ncbi.nlm.nih.gov/pubmed/34238857 doi:10.1097/TA.0000000000003331.
- Poole GV, Ward EF, Muakkassa FF, Hsu HSH, Griswold JA, Rhodes RS. Pelvic fracture from major blunt trauma. Outcome is determined by associated injuries. Ann Surg. 1991;213(6):532–9. Available from https://pubmed.ncbi.nlm.nih.gov/2039283/ doi:10.1097/00000658-199106000-00002.
- Demetriades D, Karaiskakis M, Toutouzas K, Alo K, Velmahos G, Chan L. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195(1):1–10. doi:10.1016/s1072-7515(02)01197-3.
- Wu YT, Cheng CT, Tee YS, Fu CY, Liao CH, Hsieh CH. Pelvic injury prognosis is more closely related to vascular injury severity than anatomical fracture complexity: the WSES classification for pelvic trauma makes sense. World J Emerg Surg. 2020 Aug 17;15(1):48. Available from doi:10.1186/s13017-020-00328-x.
- Skitch S, Engels PT. Acute management of the traumatically injured pelvis. Emerg Med Clin North Am. 2018 Feb 1;36(1):161–79. doi:10.1016/j.emc.2017.08.011.
- Lunsjo K, Tadros A, Hauggaard A, Blomgren R, Kopke J, Abu-Zidan FM. Associated injuries and not fracture instability predict mortality in pelvic fractures: a prospective study of 100 patients. J Trauma Inj Infect Crit Care. 2007;62(3):687–91. Available from https://journals.lww.com/jtrauma/Fulltext/2007/03000/Associated_Injuries_and_Not_Fracture_Instability.22.aspx doi:10.1097/01.ta.0000203591.96003.ee.
- Pap R, McKeown R, Lockwood C, Stephenson M, Simpson P. Pelvic circumferential compression devices for prehospital management of suspected pelvic fractures: a rapid review and evidence summary for quality indicator evaluation. Scand J Trauma Resusc Emerg Med. 2020 Jul 13;28(1):65. Available from doi:10.1186/s13049-020-00762-5.
- Magnone S, Coccolini F, Manfredi R, Piazzalunga D, Agazzi R, Arici C, Barozzi M, Bellanova G, Belluati A, Berlot G, et al. Management of hemodynamically unstable pelvic trauma: results of the first Italian consensus conference (cooperative guidelines of the Italian Society of Surgery, the Italian Association of Hospital Surgeons, the Multi-specialist Italian Society of Young Surgeons, the Italian Society of Emergency Surgery and Trauma, the Italian Society of Anesthesia, Analgesia, Resuscitation and Intensive Care, the Italian Society of Orthopaedics and Traumatology, the Italian Society of Emergency Medicine, the I. World J Emerg Surg. 2014 Mar 7;9(1):18. [cited 2023 Jan 27Available from https://pubmed.ncbi.nlm.nih.gov/24606950/ doi:10.1186/1749-7922-9-18.
- Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017 Jan 18;12(1):5. [cited 2023 Jan 27 Available from https://pubmed.ncbi.nlm.nih.gov/28115984/
- Zingg T, Piaget-Rossel R, Steppacher J, Carron P-N, Dami F, Borens O, Albrecht R, Darioli V, Taffé P, Maudet L, et al. Prehospital use of pelvic circumferential compression devices in a physician-based emergency medical service: a 6-year retrospective cohort study. Sci Rep. 2020 Dec 1;10(1):5106. doi:10.1038/s41598-020-62027-6.
- Tsur AM, Nadler R, Lipsky AM, Levi D, Bader T, Benov A, Glassberg E, Chen J. The Israel Defense Forces Trauma Registry: 22 years of point-of-injury data. J Trauma Acute Care Surg. 2020;89(2S Suppl 2):S32–S38. doi:10.1097/TA.0000000000002776.
- Tordjman K, Rouach V, Jaffe A, Givon A, Bodas M, Greenman Y. Lower incidence of hip fractures among elderly Ethiopian immigrants to Israel: first assessment from the Israel National Trauma Registry (INTR) 2011–2020. Osteoporos Int. 2023 Feb 13;34(5):993–7. Available from doi:10.1007/s00198-023-06698-7.
- Mitchnik IY, Talmy T, Radomislensky I, Chechik Y, Shlaifer A, Almog O, Gendler S. Femur fractures and hemorrhagic shock: implications for point of injury treatment. Injury. 2022 Aug 24;53(10):3416–22. doi:10.1016/j.injury.2022.08.053.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. doi:10.1016/j.ijsu.2014.07.013.
- Talmy T, Mitchnik IY, Malkin M, Avital G, Benov A, Glassberg E, Almog O, Gendler S. Adopting a culture of remote damage control resuscitation in the military: insights from the Israel defense forces decade of experience. Transfusion (Paris) [Internet]. 2023;63(S3):S83–S95. https://pubmed.ncbi.nlm.nih.gov/37042676/ doi:10.1111/trf.17357.
- Kim MJ, Lee JG, Lee SH. Factors predicting the need for hemorrhage control intervention in patients with blunt pelvic trauma: a retrospective study. BMC Surg. 2018 Nov 16;18(1):101. Available from doi:10.1186/s12893-018-0438-8.
- Mirza A, Ellis T. Initial management of pelvic and femoral fractures in the multiply injured patient. Crit Care Clin. 2004 Jan;20(1):159–70. Available from https://linkinghub.elsevier.com/retrieve/pii/S0749070403000964 doi:10.1016/s0749-0704(03)00096-4.
- Demetriades D, Karaiskakis M, Toutouzas K, Alo K, Velmahos G, Chan L. Pelvic Fractures: epidemiology and Predictors of Associated Abdominal Injuries and Outcomes2002.
- Biffl WL. Control of pelvic fracture–related hemorrhage. Surg Open Sci. 2022 Apr 1;8:23–6. Available from:/pmc/articles/PMC8892196/
- Lee C, Porter K. The prehospital management of pelvic fractures. Emerg Med J. 2007 Feb;24(2):130–3. [Available from:/pmc/articles/PMC2658194/ doi:10.1136/emj.2006.041384.
- Papakostidis C, Giannoudis P v Pelvic ring injuries with haemodynamic instability: efficacy of pelvic packing, a systematic review. Injury [Internet]. 2009 Nov 1;40(SUPPL. 4):S53–S61. Available from http://www.injuryjournal.com/article/S0020138309005579/fulltext
- Giannoudis PV, Grotz MRW, Tzioupis C, Dinopoulos H, Wells GE, Bouamra O, Lecky F. Prevalence of pelvic fractures, associated injuries, and mortality: the United Kingdom perspective. J Trauma Inj Infect Crit Care. 2007 Oct;63(4):875–83. Available from https://journals.lww.com/jtrauma/Fulltext/2007/10000/Prevalence_of_Pelvic_Fractures,_Associated.24.aspx doi:10.1097/01.ta.0000242259.67486.15.
- Ghassibi M, Boyalakuntla DS, Gentile J. Low-energy pelvic ring fractures in the elderly population: expected outcomes and associated mortality rates. J Clin Med Res. 2019;11(11):725–8. Available from:/pmc/articles/PMC6879025/ doi:10.14740/jocmr3891.
- Verbeek DO, Ponsen KJ, Fiocco M, Amodio S, Leenen LPH, Goslings JC. Pelvic fractures in the Netherlands: epidemiology, characteristics and risk factors for in-hospital mortality in the older and younger population. Eur J Orthop Surg Traumatol. 2018 Feb 1;28(2):197–205. Available from https://pubmed.ncbi.nlm.nih.gov/28993913/ doi:10.1007/s00590-017-2044-3.
- Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H. Epidemiology of pelvic ring injuries. Injury [Internet]. 1996;27:13–20. Available from https://www.sciencedirect.com/science/article/pii/S0020138396901060 doi:10.1016/S0020-1383(96)90106-0.
- Schmal H, Markmiller M, Mehlhorn AT, Sudkamp NP. Epidemiology and outcome of complex pelvic injury. Acta Orthop Belg. 2005 Feb;71(1):41–7.
- Yang NP, Chan CL, Chu D, Lin YZ, Lin KB, Yu CS, et al. Epidemiology of hospitalized traumatic pelvic fractures and their combined injuries in Taiwan: 2000-2011 National Health Insurance data surveillance. Biomed Res Int. 2014;2014:878601.
- Ghosh S, Aggarwal S, Kumar V, Patel S, Kumar P. Epidemiology of pelvic fractures in adults: our experience at a tertiary hospital. Chin J Traumatol. 2019 Jun;22(3):138–41. doi:10.1016/j.cjtee.2019.03.003.
- Parker W, Despain RW, Bailey J, Elster E, Rodriguez CJ, Bradley M. Military experience in the management of pelvic fractures from OIF/OEF. BMJ Mil Health. 2023 Apr 1;169(2):108–11. Available from https://pubmed.ncbi.nlm.nih.gov/32938710/ doi:10.1136/bmjmilitary-2020-001469.
- Hornez E, Monchal T, Boddaert G, Chiron P, Danis J, Baudoin Y, Daban J-L, Balandraud P, Bonnet S. Penetrating pelvic trauma: initial assessment and surgical management in emergency. J Visc Surg. 2016 Aug 1;153(4 Suppl):79–90. doi:10.1016/j.jviscsurg.2016.04.006.
- Erdman MK, Munger AM, Brown M, Schellenberg M, Tucker D, Inaba K, Fleming ME, Marecek GS. Injury and treatment patterns of ballistic pelvic fractures by anatomic location. Eur J Orthop Surg Traumatol. 2021 Jan 1;31(1):111–9. Available from doi:10.1007/s00590-020-02744-w.
- Tisnovsky I, Katz SD, Pincay JI, Garcia Reinoso L, Redfern JAI, Pascal SC, Wham BC, Naziri Q, Suneja N. Management of gunshot wound-related hip injuries: a systematic review of the current literature. J Orthop. 2021 Jan 1;23:100–6. Available from:/pmc/articles/PMC7804341/ doi:10.1016/j.jor.2020.12.029.
- Henry S, Brasel K, Stewart RM. ATLS Advanced Trauma Life Support. American College of Surgeons; 2018.
- Schweigkofler U, Wohlrath B, Trentzsch H, Horas K, Hoffmann R, Wincheringer D. Is there any benefit in the pre-hospital application of pelvic binders in patients with suspected pelvic injuries? Eur J Trauma Emerg Surg. 2021 Apr 1;47(2):493–8. Available from https://pubmed.ncbi.nlm.nih.gov/31612271/ doi:10.1007/s00068-019-01239-6.
- Chesser TJS, Cross AM, Ward AJ. The use of pelvic binders in the emergent management of potential pelvic trauma. Injury. 2012 Jun;43(6):667–9. doi:10.1016/j.injury.2012.04.003.
- Naseem H, Nesbitt PD, Sprott DC, Clayson A. An assessment of pelvic binder placement at a UK major trauma centre. Ann R Coll Surg Engl. 2018 Feb 1;100(2):101–5. Available from:/pmc/articles/PMC5838689/ doi:10.1308/rcsann.2017.0159.
- Mitchnik I, Gendler S, Talmy T, Shlaifer A, Chechik Y, Almog O. Treatment of Orthopedic Trauma. In: military Trauma and Combat Medicine, Israeli Comprehensive Combat Casualty Care, Israel Defense Forces Medical Corps2022.
- Pieper A, Thony F, Brun J, Rodière M, Boussat B, Arvieux C, Tonetti J, Payen J-F, Bouzat P. Resuscitative endovascular balloon occlusion of the aorta for pelvic blunt trauma and life-threatening hemorrhage: a 20-year experience in a Level I trauma center. J Trauma Acute Care Surg. 2018 Mar 1;84(3):449–53. Available from https://pubmed.ncbi.nlm.nih.gov/29298239/ doi:10.1097/TA.0000000000001794.
- Harfouche M, Inaba K, Cannon J, Seamon M, Moore E, Scalea T, DuBose J. Patterns and outcomes of zone 3 REBOA use in the management of severe pelvic fractures: results from the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery database. J Trauma Acute Care Surg. 2021 Apr 1;90(4):659–65. Available from https://pubmed.ncbi.nlm.nih.gov/33405470/ doi:10.1097/TA.0000000000003053.

