Abstract
Background
Paediatric occupational therapy (OT) is considered the largest practice area in OT in several regions, including the Eastern Mediterranean (EM) countries.
Aims/objectives
This study aimed to establish a profile of paediatric occupational therapists in EM countries to identify theoretical models, assessments and interventions employed. It also investigated the therapists’ usage of evidence-based practice in their practice.
Material and methods
We conducted a cross-sectional survey using a questionnaire which was distributed electronically to occupational therapists working with children.
Results
The participants included 118 therapists. Majority of the participants were working at rehabilitation centres. The primary client groups were pre- and school-age children with autism spectrum disorder and cerebral palsy. The most frequently used assessments were sensory-related tools. Activities of daily living and play were the most often targeted interventional area. Participants highlighted some of the challenges faced in implementing evidence in their practice.
Conclusion
Paediatric occupational therapists are usually exposed to specific age groups and conditions. However, a lack of knowledge practice in some areas and challenges in others exist.
Significance
Within the EM region, knowledge regarding therapists’ practices is lacking. Actions should be taken to improve current practice and meet the current needs of clients, and utilise evidence-based practices.
Introduction
Paediatric occupational therapy (OT) is considered the largest practice area in OT in several regions, including the Eastern Mediterranean (EM) countries [Citation1,Citation2]. The EM countries comprise 22 countries, including: Afghanistan, Bahrain, Djibouti, Egypt, Islamic Republic of Iran, Iraq, Jordan, Saudi Arabia, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Palestine and Occupied Palestinian territory, Qatar, Somalia, Sudan, Syria, Tunisia, Turkey, United Arab Emirates, and Yemen, as grouped by the World Health Organisation [Citation3]. According to the World Federation of Occupational Therapists (WFOT), ten of the EM countries have educational programs that are also accredited by the WFOT which are Islamic Republic of Iran, Jordan, Saudi Arabia, Kuwait, Lebanon, Morocco, Pakistan, Palestine and Occupied Palestinian territory and Turkey [Citation4]. However, within the EM region, knowledge regarding therapists’ practices is lacking, with no available data concerning the number of therapists; moreover, OT is a relatively new profession, which is in the development stage in EM countries [Citation5].
Paediatric practice in OT includes working with children from birth to the beginning of adulthood [Citation2]. OT is crucial for enabling childhood participation in life occupations that are meaningful and essential for health and development, including self-care, play, and school activities [Citation6]. A therapist assesses, plans, and conducts an intervention while providing OT services [Citation7]. Thus, the therapist should use clinical reasoning, which is the thought process required to plan and implement an intervention [Citation8] while acknowledging practice models for that purpose.
Internationally, several publications have investigated paediatric OT practices that consider the utilisation of theories in practice, assessments, and interventions. These studies in Canada [Citation9], Australia [Citation10], and the United Kingdome (UK) [Citation11], all reported similar findings that are worth mentioning. Concerning the therapist profiles, most therapists were females with a bachelor’s degree. Sensory integration was the most common training program. The most seen client age groups were pre-school and school age children. Therapists usually employ sensory approaches, and some also use neurodevelopmental treatment. In the UK, Australia, and Canada [Citation9–11], the Beery–Buktenica Developmental Test of Visual-Motor Integration [Citation12] and the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2) [Citation13] are the most commonly used standardised assessments. The interventions used for children in these countries focus on the parent/caregiver’s education, activities of daily living, and assistive devices. Although these studies are quite old, they are still important to review, as they provide an invaluable perspective in understanding the profile of paediatric OT in various parts of the world.
More recent studies have focused on populations with specific diagnoses or age groups. Anaby and colleagues [Citation14], examined the OT and physiotherapy services with school-aged children, particularly those with cerebral palsy in Canada. Therapists were focused more on motor skills and task-oriented activities, such as activities of daily living and mobility and less attention was given to leisure and community-based activities. The commonly used outcome measures were Beery–Buktenica Developmental Test of Visual Motor Integration [Citation12], Canadian Occupational Performance Measure [Citation15] and BOT-2 [Citation13] while other evaluation measures that focused on participation and the environment were rarely reported. Another study described the characteristics of current OT practices in the United States with clients with autism [Citation16]. They found that sensory approaches to intervention were frequently utilised and OT practitioners frequently deliver services for clients with autism that adhered to evidence-based practice (EBP). Abu-Dahab [Citation17] also described the current practices of OT for children with autism in Jordan. Non-standardised assessments are more frequently utilised. The focus on school readiness was considered for evaluation and intervention. However, to our knowledge, no studies have explored the profile of paediatric OT in the EM region.
Thus, this research aimed to establish a profile of paediatric occupational therapists in EM countries. The objectives of the study were to:
describe the nature of work for paediatric occupational therapists in EM countries.
identify the theoretical models, assessments, and interventional strategies employed by paediatric occupational therapists in EM countries; and
investigate the factors associated with paediatric occupational therapists’ use of EBP.
Enhancing such knowledge is important for exploring paediatric OT practice in the EM region, which would enable OT educators to determine the existing state and seek measures to improve and amend the gaps in practice. In addition, it will aid in monitoring the current practice, measure the level of efficiency by comparing it with the current EBP and knowledge, and guide the development of this practice further.
Materials and methods
Design and participants
This study employed a cross-sectional survey design. The participants were occupational therapists working in the EM countries. The inclusion criteria were (1) occupational therapists working with children; (2) a minimum of one year experience working with children to ensure sufficient experience in the field; and (3) occupational therapists working in any country within the EM region. Children’s age was based on the participants’ self-evaluation and the country where they were practicing (i.e. within some countries, paediatrics practice is up to the age of 16, while it is up to the age of 18 in others). We excluded students and those working in paediatrics for less than one year.
Measures
The questionnaire’s content was developed based on instruments employed in previous studies [Citation9–11] and updated with more recent literature [Citation18,Citation19] and paediatric OT textbooks [Citation2,Citation20]. Moreover, to validate the questionnaire, expert committee reviewers specialised in the field of OT attended several meetings to review and modify the questions according to the objectives of the study. The expert committee panel consisted of three faculty members specialising in paediatrics and assessment, and two experienced occupational therapists with 10 and 20 years of clinical experience, respectively, in the field of paediatric rehabilitation.
After several meetings and discussions among the expert committee reviewers, a consensus was reached to finalise the approved version of the questionnaire. The approved questionnaire consisted of 25 questions organised into six sections (i.e. demographics, employment characteristics, practice models and frames of reference, assessment, intervention, and evidence-based practice). Closed-ended questions were created, with the majority in the multiple-choice format. In all the sections, owing to the expected diversity in the participants’ backgrounds, additional space was available for non-listed items to be added.
The questionnaire sections were as follows:
Section 1 (Demographics): consisted of nine items. It explored the participants’ demographic data including age, gender, years of working experience with children and in other areas, present country of practice, certifications, conferences/seminar attendance related to paediatrics, whether they worked with an interdisciplinary team (e.g. including physicians, nurses, teachers, social workers or any others from the rehabilitation team), and how often was this conducted (e.g. how old are you? What is your gender? Including this year, how many years have you been practicing in the area of paediatrics occupational therapy?).
Section 2 (Employment characteristics): This section consisted of three items. It targeted the participants’ employment characteristics, including the setting of practice. It also asked about the clients’ age group and the most commonly seen diagnostic groups (e.g. In which of the following areas have you had the majority of your working experience with children?).
Section 3 (Practice models and frames of reference): This section included three items. It focused on the models of practice and frames of reference commonly employed with children and their reason for use. (e.g. What are the practice models that you use in working with children? What are the frames of references that you use in your practice? What are the reasons for using the practice models/frames of references in your practice?).
Section 4 (Assessment): This section consisted of two questions. It included an alphabetically ordered list of 39 assessments used in paediatric areas of practice. These choices were based on an extensive search of OT literature and books that target paediatric OT. In addition, factors related to choice were also included (e.g. What are the most common assessments that you use in working with children? What are the reasons for the selection of assessments used? The participants were encouraged to choose all the applicable options).
Section 5 (Intervention): This section was similar to Section 4, consisting of two questions. It included 40 different interventions used with children receiving OT, which was adopted from a previous systematic review concerning the effectiveness of paediatric OT for children with disabilities [Citation18] (e.g. What are the most common interventions that you use?).
Section 6 (evidence-based practice EBP): Three questions were included to determine how often the therapist based their practice on EBP in paediatric OT, whether they faced any challenges to implement EBP, and if their answer was yes, a follow up question appeared to investigate these possible challenges (e.g. How often do you base your occupational therapy practice on EBP? Do you face challenges to implement EBP? What are the challenges you are facing to implement EBP?).
Procedure
Following ethics approval from the Kuwait University, the first version of the questionnaire was developed by the expert committee and then piloted. It was piloted with ten actively practicing paediatric occupational therapists. Their average age was 34.4 years and they had an average of 11 years of experience. The piloting stage was performed using paper and pen survey method. Accordingly, two questions were modified. The first question was concerning the participants certification (‘What speciality certification do you have?’). The new question clarified that the question was concerning the certification in paediatrics. Thus, the question was changed to ‘What speciality certification in paediatrics do you have?’. The second modified question was concerning EBP, the previous version was ‘How do you base your occupational therapy service on EBP?’ (in a number between 1 [the least used] to 5 [the mostly used]’. This was modified to ‘How often do you base your OT practice on EBP?’ The choices were: never, less often, sometimes, most of the times, always). This step ensured the psychometric testing of the tool for its validity and reliability since the content validity index was also employed. This index covered two aspects: the clarity of the items (clarity of the questions), and the questions’ relevance to the research topic. Participants in the pilot testing phase were asked to score each of the survey items according to these two components of the content validity index using a 4-point scale response (1-strongly disagree, 2-disagree, 3-agree, and 4-strongly agree). The face validity of the questionnaire was found to be 100%, where all the participants answered yes for the ‘Do you think this questionnaire reflects the purpose of this study targeting the profile of paediatric OT practice?’.
The final version was developed as an online questionnaire to enhance distribution among EM countries. Moreover, the online method is cost-effective and can increase anonymity [Citation21]. It was designed in a way that each therapist was only be able to complete the survey once.
Once the final version was completed, snowball sampling was employed as the recruitment strategy. An invitation message was created and shared with therapists through emails and social media platforms (e.g. Twitter and WhatsApp). Therapists were encouraged as well to share the study’s questionnaire link with their colleagues. In addition, to obtain as wide a sample as possible, the regional associations within these countries were contacted to distribute the invitation message among their members. Another reminder was sent two weeks later.
Data analysis
Statistical analyses were conducted using Statistical Package for Social Sciences (SPSS) (IBM Corp) version 26. The data were cleaned, checked for abnormalities, and coded accordingly. Means and standard deviations were used to describe the continuous variables if they followed a normal distribution. Otherwise, medians and interquartile ranges were reported. Categorical variables are expressed as counts and percentages. The two-sample t-test was conducted to compare the means of normally distributed variables; otherwise, the non-parametric Mann-Whitney U test was conducted. Pearson or Spearman’s correlations were used to estimate the strength of the linear relationship between two continuous variables. To test the association between two categorical variables, the Pearson chi-square test was used if the expected counts were greater than 5 for 80% of the cells; otherwise, Fisher’s exact test was conducted. Stepwise (forward substitution) multiple logistic regression modelling was implemented to model the association between facing challenges to base their practice on EBP as a binary outcome (yes = 1, no = 0) and other covariates and to find the most parsimonious model. Covariates that showed an association with the outcome, with a P value ≤0.30 are allowed in the model. Several values of probability to enter and probability to exit were attempted so that no important covariate could be ignored due to stringent entry or exit criteria. Finally, the model was tested for significance and checked if it fit the data well; the percentage of correct classification was calculated as an indicator of model performance as a classification tool. All the tests were two-tailed and the significance level was set at p < 0.05. A stepwise logistic regression method was implementedto produce the most parsimonious model of association between challenges in implementing EBP and a set of covariates.
Results
A total of 118 occupational therapists who responded to the distributed questionnaire were from different countries within the EM region, including Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Palestine, Qatar, Saudi Arabia, Turkey, and the United Arab Emirates (see ). Descriptive analysis (see ) indicated that participants had a median (IQR) age of 27.5 (9) years and had been practicing OT/paediatric OT for a median (IQR) of 4 (6) years. The participants were mainly female (68.6%) with a bachelor’s degree (72.0%). Approximately 37.3% of the study participants indicated that they did not have a paediatric specialty certification (i.e. gained accredited postgraduate certification). However, the most gained post-graduate certification in paediatrics was in sensory integration (43.2%). A few participants had indicated other certifications such as Brain Gym, DIRFloortime, and The Listening Program.
Figure 1. The number of therapists participated from each country (aBahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates; bJordan, Lebanon and Palestine; cIran and Turkey).
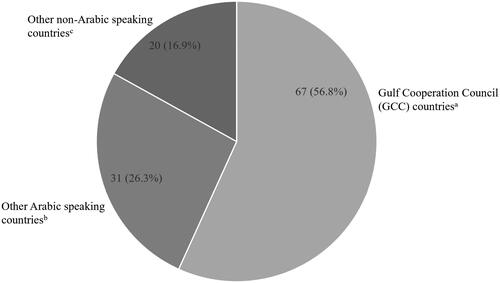
Table 1. Demographic characteristics of the study participants (N = 118).
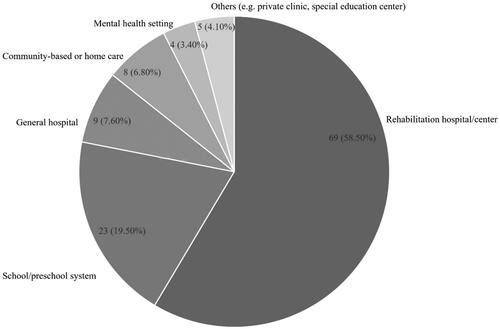
Moreover, approximately 87.3% indicated that they attended conferences/seminars related to paediatric OT and approximaately 38.1% specified that they had always worked with interdisciplinary teams related to paediatric OT. Finally, majority (58.5%) of the participants practiced OT in rehabilitation hospitals/centres, while very few participants (3.4%) practiced in mental health settings ().
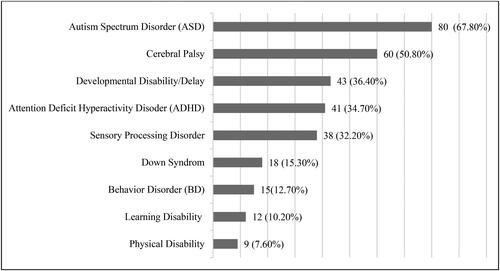
Regarding the client characteristics of the study participants, the most common age groups for practice were pre-school (3–5 years) (94.1%) and school age (6–10 years) (80.5%), while the least practiced age group was adolescents (15–18 years) (20.3%). Furthermore, participants indicated that autism spectrum disorder (ASD; 67.8%) and cerebral palsy (50.8%) were among the most common diagnostic groups they worked with (). Participants reported never or rarely working with clients who had burns, cancer, spina bifida, and obesity.
As for the practice models used and frames of reference implemented in practice among the study participants (see ), the person environment occupation (PEO) (49.2%) and Canadian model of occupation performance and engagement (CMOP-E) (46.6%) were the models most commonly employed in practice. The Ayres Sensory Integration (ASI) (72.0%) and developmental frames of reference (59.3%) were among the most commonly used frames of reference. The data revealed that among the most common reasons for practice models and frames of reference being used were therapists’ clinical reasoning (75.4%) and area of practice (54.2%), while reasons for referrals (16.9%) and organisational rules (9.3%) were among the least common reasons for models of practice and frames of reference use.
Table 2. Models of practice and frames of reference among study participants (N = 118).
As for assessment, reasons, and interventions that were used in work with children, shows the most commonly used ones, in which Sensory Profile-2 [Citation22] (53.4%) and non-standard assessment (39.0%) were among the most frequently used common assessments. Furthermore, availability at the workplace (59.3%) and familiarity with the assessment (46.6%) were among the top reasons for selection of the assessment used. Training at the participant’s workplace (26.3%) and university (31.4%) were among the least common reasons for selection of the assessment used.
Table 3. Common assessments and reasons for their selection with most frequent areas of occupation and interventions used as reported by study participants (Table FootnoteaN = 118).
Data also revealed that activities of daily living (85.6%), play (78.6%), and social participation (70.3%) were among the most frequent areas of OT targeted for treatment. The data also indicated that the most commonly implemented interventions were cognitive orientation to daily occupational performance (CO-OP) (68.1%), play therapy (57.8%), home programs (52.6%), and sensory approaches (50.0%) (see for details).
We attempted to better understand the frequency of adopting EBP among study participants in their everyday practice and the challenges faced to do so. The data revealed that approximately 83.3% of the participants faced challenges to adopt the EBP framework. Only 43.9% indicated basing their OT practice on EBP most of the time and very few (2.6%) never based their practice on it. However, participants indicated that among the challenges faced were the lack of organisational support (62.6%), time to incorporate research results in practice (42.1%), dedicated time to find research (40.4%), strong evidence in available research (27.2%), and confidence in analysing and interpreting research studies (21.9%).
presents the associations between the challenges in implementing EBP and a list of covariates. The results indicated that the frequency of commitment to EBP was significantly associated with the challenges faced in implementing it (p-value = 0.035), while the participants’ age (years) (p-value = 0.069) and years of paediatric OT practice (0.081) were marginally significantly associated with the challenges faced in adopting EBP. In particular, participants who were younger and had a few years of paediatric OT practice were more likely to face challenges in implementing EBP. All other covariates considered were not significantly associated with the challenges in implementing EBP. The details of this are presented in .
Table 4. Associations between facing challenges in implementing EBP and some covariates (N = 118).
The results of the most parsimonious model of association between the challenges in implementing EBP and a set of covariates are presented in . The final model revealed that gender, years of OT practice, and frequency of OT practice based on EBP were significantly associated with the challenges in implementing EBP. In particular, the results indicated that females had 5.36 times the odds of facing challenges in EBP compared to males (OR = 5.36, 95%CI:1.088, 26.399). Furthermore, for every one-year increase in OT practice experience, there was a 12.7% decrease in the odds of facing challenges in implementing EBP. Finally, participants who base their OT practice on EBP most of the time or always had higher odds of facing challenges than those who never based their practice on EBP, with estimates of OR = 11.21, 95% CI:1.72, 73.089) and OR = 4.933, 95%CI:1.225, 19.873), respectively.
Table 5. Associations between facing challenges in implementing EBP (yes = 1, no = 0) and some covariates using Table Footnoteastepwise multiple logistic regression model (N = 118).
Finally, to determine confidence in the results produced by the final model of the stepwise procedure, according to the omnibus test of model significance, results indicated that the model was significant (χ2(df = 8)=21.37, p = 0.006). The model also fit the data well according to the Hosmer and Lemeshow test (χ2(df = 8)=5.63, P value = 0.689), and was able to correctly classify 87.7% of the study participants.
Discussion
This study explored the daily practices of paediatric occupational therapists working in the EM region. Similar to other studies in this field, most practicing occupational therapists were found to be females from the young generation [Citation1,Citation9,Citation10]. Majority of the participants had a bachelor’s degree which is the minimum educational requirement to practice within these countries. The limited post-graduates OT programmes in the EM region could have contributed to the lower percentage of the sample with postgraduates degrees, which was also found by Abu Tariah and his colleagues [Citation1]. The overall responses in this sample indicated working within an interdisciplinary team, which could be linked to the practice setting, as more than half of the participants worked in rehabilitation hospitals where more contact was expected with other health care professionals. This interpretation was also reported in a study conducted in Jordan, which indicated that most participants who were other health care professionals, had knowledge about OT from working in rehabilitation settings [Citation23]. However, the participants in this study rarely worked in mental health settings despite it being a crucial area of practice, particularly when considering the situation of COVID-19 and the consequences it has left on children [Citation24]. This could be associated with the stigma towards mental health for patients and their families within the EM countries [Citation25]. As people avoid seeking mental health services in such settings [Citation25], higher demand on OT services is consequently observed in other settings such as the rehabilitation hospitals and centres, thereby resulting in a smaller number of practicing therapists in mental health settings.
In line with their specialty certification, many of the participants were certified in the use of Ayres Sensory Integration, which could be associated with the most commonly seen health conditions (i.e. autism spectrum disorder). This theory of sensory integration has also been highlighted in previous studies as commonly used [Citation9–11]. Despite the increase in the number of patients with other health conditions, such as burns, cancer or obesity, and higher survival rates in these patients, our study reported an absence of OT services for children with these health conditions. In particular, obesity has a high prevalence with a higher prevalence in some countries within the EM region compared to that of North America [Citation26]. Nevertheless, neurodevelopmental treatment is still widely used, as shown by the results, even when the evidence is controversial [Citation27].
Unlike the EM countries, many paediatric occupational therapists work in school systems in Western countries [Citation28]. This is despite the fact that the most common age group for occupational therapists in the EM countries is between 3-10 years. Therefore, many children’s problems may not be addressed within this region as very few therapists work there.
The survey results described a variety of assessment tools with sensory-related assessments being very common (e.g. Sensory Profile-2 [Citation22], Sensory Processing Measure-2 [Citation29], Sensory Integration and Praxis Test [Citation30], and clinical observation of motor and postural skills). Similar to previous studies [Citation9–11], the BOT-2 [Citation13] and Peabody Developmental Motor Scales [Citation31] were widely used. However, the use of the Beery–Buktenica Developmental Test of Visual-Motor Integration [Citation12], which is prevalent in other counties [Citation9–11], was not observed in this study. Brown et al. [Citation7] demonstrated that despite the popularity of visual-motor integration among the participants in their study, it was not a tool of choice for children who required rehabilitation. This point should be taken into consideration since the majority of the participants in this study worked in rehabilitation centres (58.5%).
A lack of consistency was observed between the assessment tools used by the participants and interventions applied. The data indicated Cognitive Orientation to Daily Occupational Performance (CO-OP), cognitive interventions, visual motor interventions, handwriting interventions, play therapy, and social skills training as the most common interventions used when none of the common assessments targeted these areas. Therapists’ selection for the assessment tools is influenced by their availability as indicated in the results, which could have contributed to this discrepancy. This is in line with a previous study on the use of cognitive assessments by occupational therapists [Citation32].
This lack of consistency might also suggest considering EBP. This could be linked to the participants having fewer years of experience, as the results demonstrated that those with less experience faced more challenges and had fewer specialty certifications. However, these participants are encouraged to attend continuous education programmes and work with an interdisciplinary team that can assist them in improving and overcoming these issues over time. In addition, the majority of the participants indicated that they often based their treatment on evidence, which is in contrast to many studies in wherein although health care professionals recognise the importance of EBP, they do not employ it efficiently [Citation33].
The most cited challenges related to the implementation of EBP were the lack of organisational support (62.6%) and lack of time (42.1%; 40.4%), which should be considered when interpreting the results. Aspects related to research, analysis, and interpretation are another concern. These issues have been identified across different regions and professions [Citation34–36]. Nevertheless, the reasons contributing to these factors should be investigated as they have been associated with the quality of services provided, health care outcomes, and benefits received by the children [Citation37].
Implications
Educational curricula: In order to support best practice, major points should be considered within the educational curricula of entry-level OT programs, including emphasising on EBP and how these could be utilised in everyday practice. Nevertheless, it is crucial to focus on teaching trending and common health issues seen in real-life practice with the education system. This will empower practitioners to work in a variety of areas and have confidence in dealing with patients of different health conditions (e.g. cancer, burns) and age groups, including adolescents who despite their struggles, were reported as clients by only a minority of participants in this study.
Practicing therapists: The findings can support practicing occupational therapists in evolving their identification, interpretation and translation of new knowledge and evidence into practice. In addition, communities of practicing occupational therapists or interest groups can utilise this information to support professional development around competencies with assessments, tests and measures.
Management level: When considering the practice area, the availability and familiarity of assessment tools is a major concern; accordingly, managers should encourage practitioners to hold seminars and workshops to update the knowledge of attending occupational therapists.
Future practice: International occupational therapy associations should be encouraged to form an international committee that targets relevant issues addressing the desired assessments and treatment interventions used in paediatric OT. This will, in turn, support up-to-date practices and optimise OT service delivery for children with various levels of disability.
Methodological considerations/limitations
This is the first study designed to explore the daily practices of paediatric occupational therapists in EM countries. However, it could not cover equal number of participants from different countries. No information regarding non-respondents was provided; thus, some of the EM countries were not covered. Another limitation concerning recruited participants through professional organisations is that these memberships are optional and can only contact their paid members. It is also important to acknowledge that the construction of the survey’s questions can influence the collected data. Moreover, we did not study each health condition in depth concerning the models used for assessment and intervention, warranting further investigation. In addition, an online method was used, which might have contributed to the bias in obtaining responses by those who were interested in the subject area. Furthermore, the sampling of participants may have contributed to missing out certain therapists. Therefore, our study findings should be interpreted with caution within the limitations of the study.
Conclusion
Current paediatric OT practices in EM countries have many similarities to those in other regions. In this study, we identified the daily practices of occupational therapists in terms of the most commonly seen health conditions and age groups, in addition to their use of theories, assessments, and interventions. Several issues were identified and should be addressed within the OT educational curricula and professional development initiatives. Therapists lack experience in working with certain health conditions, and the theoretical models, assessments and interventions most commonly used are not congruent with each other, in addition to the challenges faced in implementing EBP within this field. Most importantly, these findings should be considered to improve the educational curricula and current practice and future studies should be conducted to fill the gap in real-life practice.
Acknowledgements
The author sincerely thanks the therapists who participated in this study.
Disclosure statement
The author reports there are no competing interests to declare.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Abu Tariah HS, Abu‐Dahab SM, Hamed RT, et al. Working conditions of occupational therapists in Jordan. Occup Ther Int. 2011;18(4):1–12. doi: 10.1002/oti.319.
- Kuhaneck H, Case-Smith J. The occupational therapy process in pediatrics: overview of essential concepts. In: O ‘Brien. J, Kuhaneck H, editors. Case-Smith’s occupational therapy for children and adolescent. 8th ed. Missouri: Elsevier; 2020. p. 1–17.
- World Health Organization. WHO Eastern Mediterranean Region. 2023 [cited 2023 Sep 4]. Available from: https://www.emro.who.int/countries.html
- World Federation of Occupational Therapists. WFOT Approved Education Programmes. 2023 [cited 2023 Sep 4]. Available from: https://wfot.org/programmes/education/wfot-approved-education-programmes
- Alotaibi N, Shayea A, Nadar M, et al. Investigation into health science students’ awareness of occupational therapy: implications for interprofessional education. J. Allied Health. 2015;44(1):3–9.
- American Occupational Therapy Association. Occupational Therapy’s Distinct Value in Children & Youth. 2021. Available from: https://www.aota.org/Practice/Children-Youth/distinct-value.aspx
- American Occupational Therapy Association. Occupational therapy practice framework: domain and process. (4th ed). Am. J. Occupat. Therapy. 2020; 74(Suppl. 2): 7412410010. doi: 10.5014/ajot.2020.74S2001
- O’Brien J. Introduction to occupational therapy. 5th ed. Missouri: Elsevier; 2018.
- Brown GT, Rodger S, Brown A, et al. A profile of Canadian pediatric occupational therapy practice. Occup Ther Health Care. 2007;21(4):39–69. doi: 10.1080/J003v21n04_03.
- Rodger S, Brown GT, Brown A. Profile of paediatric occupational therapy practice in Australia. Aus Occup Therapy J. 2005;52(4):311–325. doi: 10.1111/j.1440-1630.2005.00487.x.
- Howard L. A survey of paediatric occupational therapists in the United Kingdom. Occup Ther Int. 2002;9(4):326–343. doi: 10.1002/oti.172.
- Beery KE, Beery NA. The Beery-Buktenica developmental test of Visual-Motor integration: administration, scoring, and teaching manual. 5th ed. Minneapolis, MN: NCS Pearson; 2004.
- Bruininks R, Bruininks B. Bruininks-Oseretsky test of motor proficiency. 2nd ed. Minneapolis: NCS Pearson; 2005.
- Anaby D, Korner-Bitensky N, Steven E, et al. Current rehabilitation practices for children with cerebral palsy: focus and gaps. Phys Occup Ther Pediatr. 2017;37(1):1–15. doi: 10.3109/01942638.2015.1126880.
- Law M, Baptiste S, Carswell A, et al. Canadian occupational performance measure. 5th ed. Ottawa, ON: CAOT Publications ACE; 2014.
- Watling R, Daughton N. Current practices in OT for autistic clients: alignment with evidence-based practice & practice guidelines. Am. J. Occupat. Therapy. 2023;77(Supplement_2):7711510337p1–7711510337p1. doi: 10.5014/ajot.2023.77S2-PO337.
- Abu-Dahab S. Current practices of OT for children with autism spectrum disorder in Jordan. Am. J. Occupat. Therapy. 2020;74(4_Supplement_1):7411505246p1–7411505246p1. doi: 10.5014/ajot.2020.74S1-PO9321.
- Novak I, Honan I. Effectiveness of paediatric occupational therapy for children with disabilities: a systematic review. Aust Occup Ther J. 2019;66(3):258–273. doi: 10.1111/1440-1630.12573.
- Lynch H, Prellwitz M, Schulze C, et al. The state of play in children’s occupational therapy: a comparison between Ireland, Sweden and Switzerland. Br. J. Occupat. Therapy. 2018;81(1):42–50. doi: 10.1177/0308022617733256.
- Kramer P, Hinojosa J, Howe T. Frames of reference for pediatric occupational therapy. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2018.
- Helou S, Abou-Khalil V, El Helou E, et al. Factors related to personal health data sharing: data usefulness, sensitivity and anonymity. Public Health Inform. 2021;281:1051–1055.
- Dunn W. Sensory profile-2. San Antonio, TX: Pearson Publishing; 2014.
- AlHeresh R, Nikopoulos CK. The role of the occupational therapist in Jordan: a survey of the members of the healthcare team exploring their knowledge about occupational therapy in rehabilitation hospitals. Disabil Rehabil. 2011;33(9):778–786. doi: 10.3109/09638288.2010.509460.
- Imran N, Zeshan M, Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 pandemic. Pak J Med Sci. 2020;36(COVID19-S4):S67–S72. doi: 10.12669/pjms.36.COVID19-S4.2759.
- Zolezzi M, Alamri M, Shaar S, et al. Stigma associated with mental illness and its treatment in the arab culture: a systematic review. Int J Soc Psychiatry. 2018;64(6):597–609. doi: 10.1177/0020764018789200.
- Elkum N, Al‐Arouj M, Sharifi M, et al. Prevalence of childhood obesity in the state of Kuwait. Pediatr Obes. 2016;11(6):e30–e34. doi: 10.1111/ijpo.12090.
- Reidy T, Bolt P, Naber E. Neurromotor conditions: cerebral palsy. In: O ‘Brien J, Kuhaneck H, editors. Case-Smith’s occupational therapy for children and adolescent. 8th ed. Missouri: Elsevier; 2020. p. 764–785.
- O’Donoghue C, O’Leary J, Lynch H. Occupational therapy services in school-based practice: a pediatric occupational therapy perspective from Ireland. Occup Ther Int. 2021;2021:6636478–6636411. doi: 10.1155/2021/6636478.
- Parham LD, Ecker CL, Kuhaneck H. Sensory processing measure, second edition (SPM-2). Western Psychological Services; 2021.
- Ayres AJ. Sensory integration and praxis test. SIPT manual. Torrance, CA: Western Psychological Services; 1989.
- Fewell R, Folio R. Peabody developmental motor scales second edition: guide to item administration. Texas: shoal Creek Boulevard; 2000.
- Manee FS, Nadar MS, Alotaibi NM, et al. Cognitive assessments used in occupational therapy practice: a global perspective. Occup Ther Int. 2020;2020:8914372–8914378. doi: 10.1155/2020/8914372.
- Kristensen HK, Ytterberg C, Jones DL, et al. Based evidence in stroke rehabilitation: an investigation of its implementation by physiotherapists and occupational therapists. Disabil Rehabil. 2016;38(26):2564–2574. doi: 10.3109/09638288.2016.1138550.
- Trembath D, Sulek R, Paynter J, et al. Staff views on supporting evidence based practice for children with ASD. Disabil Rehabil. 2019;41(4):436–444. doi: 10.1080/09638288.2017.1396367.
- Lindström A-C, Bernhardsson S. Evidence-based practice in primary care occupational therapy: a cross-sectional survey in Sweden. Occup Ther Int. 2018;2018:5376764–5376769. doi: 10.1155/2018/5376764.
- Alrowayeh HN, Buabbas AJ, Alshatti TA, et al. Evidence-based physical therapy practice in the state of Kuwait: a survey of attitudes, beliefs, knowledge, skills, and barriers. JMIR Med Educ. 2019;5(1):e12795. doi: 10.2196/12795.
- Krueger RB, Sweetman MM, Martin M, et al. Occupational therapists’ implementation of evidence-based practice: a cross sectional survey. Occup Ther Health Care. 2020;34(3):253–276. doi: 10.1080/07380577.2020.1756554.