Abstract
Stigma is an established consequence of the Borderline Personality Disorder (BPD) diagnosis. This diagnosis is subject to revision in the International Classification of Diseases–11th Revision (ICD–11). Using the legal issue of diminished responsibility, this study applied an experimental mock-jury methodology to explore the impact of diagnostic stigma of BPD on jury decision-making. Participants were allocated to one of two versions of a simplified fictitious homicide trial. The group whose defendant was described as having a ‘severe personality disorder, borderline pattern’ rated the defendant as more dangerous, and more in need of segregation and coercive treatment, than controls where the defendant was described as having a ‘complex mental health problem’. Between-group differences in other measures, including the decision to agree a verdict of diminished responsibility, were not found. The ICD-11 ‘severe personality disorder, borderline pattern’ diagnosis may adversely impact the attitudes of jurors considering the question of diminished responsibility.
Introduction
Background
Juror judgements of the moral responsibility of defendants are significantly influenced by psychiatric information (Berryessa et al., Citation2015). Clinicians including psychiatrists and psychologists are frequently commissioned to provide expert witness testimony as to the nature of a defendant’s mental health condition, and how differing diagnostic entities intersect with legal questions of the controllability of criminal behaviour and individual culpability. This is a complex area, as nuanced and shifting clinical descriptors of mental health problems such as ‘borderline personality disorder’ (BPD) meet more rigid, black and white legal conceptualisations of reduced culpability better aligned with models of biologically-based mental illness (Peay, Citation2011). The legal question pertaining to diminished responsibility (DR) in cases of homicide (Homicide Act 1957, as amended by s.52 Coroners and Justice Act 2009) illustrates this complexity.
Why diminished responsibility?
In England and Wales, diminished responsibility (Homicide Act 1957, as amended by s.52 Coroners and Justice Act 2009) is a partial legal defence in cases of homicide by persons with a ‘recognised medical condition’. Should its criteria be met, a defendant is to be convicted of manslaughter rather than murder. This is of practical importance since following the successful application of this defence, options for disposal include potential hospital treatment under s.37 of the Mental Health Act 1983 as part of sentencing, as opposed to a mandatory sentence of life imprisonment.
The diminished responsibility (DR) defence requires the presence of an ‘abnormality in mental functioning’ that:
arose from a recognised medical condition;
substantially impaired the defendant’s ability to do one or more of:
understand the nature of their conduct
form a rational judgement
exercise self-control
provides an explanation for the defendant’s acts and omissions in doing or being a party to the killing. (Homicide Act 1957; as amended by s.52 Coroners and Justice Act 2009)
When the issue of diminished responsibility is considered by a court, the ‘burden of proof’ is on the defendant to prove to the jury on the balance of probabilities that the above criteria are met. The fact that the question is for a jury to determine makes DR a potentially useful locus for research considering the processes of jury decision-making. Similarly, the fact that it is considered on the balance of probabilities – and not to the criminal standard – may also be helpful in experimental research, since a relatively smaller ‘shift’ in certainty may make a more obvious impact on final outcome.
Of course, whilst the question of DR is for a jury to determine, this is done in the face of expert clinical opinion. Clinicians who provide such opinion must consider why a defendant may have been unable to understand their conduct, and whether they were able to form a rational judgement, and/or to exercise self-control in the course of their actions (Mackay, Citation2018). However, the way in which they provide this evidence is, in practice, very much a matter for an individual clinician to determine. Thus, how a clinician describes, presents or categorises a particular defendant could have a significant impact on the decisions made by a jury, with the type of diagnosis applied a specific form of this variance. One can see the power of specific clinical descriptions of defendants by drawing on the literature in regards to the term psychopathy; Kelley et al. (Citation2019) provide a meta-analysis of mock-juror simulation studies and conclude that the description of psychopathy is associated with increased perceptions of dangerousness, being ‘evil’, and an inclination to evoke the death penalty more frequently, as well as give longer sentences overall.
Diminished responsibility and personality disorder diagnoses
In English and Welsh law, whilst there are no formal exclusions for personality disorder being used to make out a case of DR, it seems that personality disorder diagnoses are less likely to be able to be successfully used than other mental health presentations. Mackay (Mackay, Citation2018; Mackay & Mitchell, Citation2017) presents a review of 90 DR pleas made since the amendments of the Coroners and Justice Act 2009, and reports that schizophrenia, personality disorder, psychosis and depression were the four most common diagnoses cited, in that order. Of these 90 cases, 15 cases cited a form of personality disorder (although type not further specified), and 11 of these cases were convicted of murder (receiving mandatory life sentences), while three further cases received discretionary life sentences. No hospital or restriction orders were made. By way of comparison, of 34 cases citing schizophrenia in relation to the DR defence, seven were given mandatory or discretionary life sentences, and 24 were given s.37/41 restriction orders (Mental Health Act 1983/2007). Mackay (Citation2018) notes that in cases concerning diagnoses of personality disorder, expert witnesses often disagreed as to whether the criteria were satisfied, speculating that this led to more contested trials, which evidently failed to persuade juries on the issue of DR.
Beyond England and Wales, Sparr (Citation2009) provides a helpful review of the international perspective of a ‘mental incapacity defence’ and highlights that ‘[m]ental incapacity defences based on personality disorders are more often used in The Netherlands, England, Germany and Belgium, but seldom in Canada and rarely in the United States and Sweden’. Similarly, one may highlight that certain jurisdictions seem to treat personality disorder – or at least antisocial personality disorder, or psychopathy – as an aggravating rather than mitigating factor (for instance, DeMatteo & Edens, Citation2006, provide a detailed review of the way in which assessments of psychopathy have influenced court outcomes).
Professional judgement of personality disorder
Of course, it might be reasonable to consider personality disorder as a barrier to a defence such as diminished responsibility if it were established that personality disorder was a valid and reliable construct that could be consistently meaningfully assessed and determined in clinical practice. Unfortunately, this remains very much a live issue. There has been, for instance, much debate as to whether borderline personality disorder is better conceptualised as a ‘trauma spectrum’ disorder (K. L. Lewis & Grenyer, Citation2009), and models highlighting developmental factors such as attachment have also been proposed (Luyten et al., Citation2019). Furthermore, there is significant ‘blurring’ between BPD presentations and other diagnoses, which might typically be quite differently viewed in a court setting (particularly posttraumatic stress disorder, PTSD, and bipolar disorders; Knefel et al., Citation2016; Smith et al., 2009). This is alongside a parallel literature, outside the scope of this paper, which considers the conceptual issues in relation to antisocial personality disorder and/or psychopathy (Edens et al., Citation2015; Marcus et al., Citation2006; Skeem & Cooke (Citation2010)).
More generally, Ayre et al. (Citation2017) argue (from the perspective of clinicians’ involvement in Mental Capacity Act 2005 assessments) that this uncertainty and debate concerning the nosological status of personality disorder cause inconsistency in assessment. This is understandable; in forms of mental disorder thought to occupy more clearly delineated boundaries of biological ‘illness’, such as schizophrenia, clinical judgment of rationality of thought and understanding of consequences is (seemingly) more straightforward (Szmukler, Citation2009). Meanwhile, borderline personality disorder has historically occupied a much more contested, controversial position within the minds of clinicians, who might find it hard to make distinctions between ‘the nature of the pathology’ and ‘the nature of the individual’ (Aviram et al., Citation2006). Furthermore, the literature includes within it more moralistic conceptualisations (e.g., Charland, Citation2006), which speaks to a failure to recognise and integrate the full complexity of BPD, including the core features of severe emotional dysregulation, impulsivity and heightened threat perception (Crowell et al., Citation2009), which are increasingly supported by neurobiological evidence (Leichsenring et al., Citation2011), and which clearly have implications relating to the faculties of understanding and weighing information (Ayre et al., Citation2017).
Contemporary classifications of personality disorder have attempted to address some of these concerns, with the International Classification of Diseases–11th Revision (World Health Organisation, Citation2019) moving to replace the current categorical system with a core personality disorder diagnosis, classification of four levels of severity (subthreshold ‘difficulty’, ‘mild’, ‘moderate’ and ‘severe’), and trait domain specifiers (‘negative affectivity’, ‘detachment’, ‘disinhibition’, ‘dissociality’ and ‘anankastia’) as well as a ‘borderline pattern’ qualifier (Bach & First, Citation2018). Therefore, people with borderline personality disorder might instead be described as having a ‘severe personality disorder, borderline pattern’. The inclusion of the ‘borderline pattern’ qualifier was subject to rigorous debate among the ICD–11 personality disorder working group and has generated a significant degree of controversy (Tyrer et al., Citation2019). Whilst the present study adopts the new ICD–11 terminology, the phrase BPD is used interchangeably to reflect the extant literature.
The stigma of personality disorders
Issues with the conceptualisation and nosology of BPD might not be quite so relevant if it were not for the fact that such a diagnosis is associated with a significant degree of public stigma. People with a personality disorder have historically been identified as ‘the patients psychiatrists dislike’ (G. Lewis & Appleby, Citation1988). A person with a personality disorder may be more likely to be viewed by professionals as morally culpable for their problems, as manipulative and in control of their symptoms and behaviour, and as less likely to recover (Chartonas et al., Citation2017; Lam, Salkovskis, et al., Citation2016; G. Lewis & Appleby, Citation1988; Markham & Trower, Citation2003). Alongside psychopathy and antisocial personality disorder (ASPD), borderline personality disorder may be one of the most stigmatised disorders (Catthoor et al., Citation2015; Sheehan et al., Citation2016). Such stigma is potentially maintained through a challenging interpersonal dynamic between patients and clinicians (Aviram et al., Citation2006) whereby the attachment and mentalising difficulties inherent to the disorder provide challenges to typical clinician–patient power structures and adherence to the ‘sick role’, resulting in labelling of patients as ‘difficult’ (Koekkoek et al., Citation2011; Luyten et al., Citation2019). This perpetuates a cycle of interpersonal rejection, precipitating further emotional distress in patients and the continuance of stigmatising views in clinicians (Aviram et al., Citation2006).
Stigma of BPD may be a particular issue for juries, given that public awareness of the disorder itself is considered to be low (Furnham et al., Citation2015; Sheehan et al., Citation2016). Furthermore, the phenomenology of such stigma superficially appears to overlap with the specific issues that might be subject to consideration by a jury, for instance dangerousness, segregation and punishment (Corrigan et al., Citation2003).
In summary, mental health professionals may conceptualise the difficulties inherent in personality disorder in different ways, due to nosological debate, lack of knowledge or the existence of stigmatising attitudes. This could bear significant implications for the ways in which clinicians present information to a jury. However, of equal importance is the way in which laypeople in juries understand this information and use this to make their own inferences concerning guilt and criminal responsibility. This latter question forms the subject of the present paper.
The current study
It is clear that a juror’s task in considering the question of diminished responsibility is in many ways a multifaceted one. The first limb – that of being persuaded of the presence of a ‘recognised medical condition’ – is presumably significantly influenced by the opinion of the expert clinicians who have assessed the defendant. However, beyond this, the juror will have to make a judgement on the core issues – the ‘substantial impairment’ – based on their understanding of the interaction between the defendant’s actions and their clinical presentation. This understanding will be drawn partly from the clinician (which itself could act as a source of bias or influence) but also significantly from their own beliefs, experiences and knowledge about the person’s mental health problem. This is thus the point at which stigma arising from a mental health condition or personality disorder diagnosis may operate to influence a juror’s judgement. It is noteworthy that nowhere in the DR criteria is any explicit consideration given to diagnosis, and it could be reasonably argued – given the issues with unreliability and stigma outlined previously – that the diagnosis itself should not have a bearing on the outcome for the defendant. Unfortunately, we know through the literature in psychopathy and ASPD cited earlier (Kelley et al., Citation2019), as well as innovative research manipulating the presence of ‘brain scans’ in the court room (Greene & Cahill, Citation2012; Gurley & Marcus, Citation2008), that small changes in the information provided about a defendant can result in significant downstream ‘amplification’ in the later decision-making of jurors. However, the literature in relation to BPD is not so well established.
The present study thus adopts an experimental mock-jury design to assess the impact of a borderline personality disorder diagnosis (presented in line with the revised ICD–11 criteria) on juror attitudes, attributions and decision-making in relation to a defendant seeking the diminished responsibility partial defence. The only manipulation between the two conditions is the diagnostic label given (‘severe personality disorder, borderline pattern’ vs. a deliberately generic ‘complex mental health problem’). Thus, any differences between groups can be reasonably inferred to be causally related to the specific wording of the diagnosis used.
Hypotheses
The hypotheses are bidirectional, reflecting the limited literature in this area. The hypotheses are that the inclusion of a ‘severe personality disorder, borderline pattern’ diagnosis will, compared to a generic ‘complex mental health problem’ diagnosis, be associated with:
differences in causal attributions made by participants regarding the behaviour of the defendant;
differences in the nature of stigmatising attitudes exhibited by participants (mock jurors) toward the defendant;
Differences in individual ratings made relating to whether the partial defence of diminished responsibility should be given.
Method
Design
This study aimed to assess causal attributions, stigma-related beliefs and individual ratings regarding diminished responsibility for homicide by use of a case-simulation methodology. This methodology presents a filmed trial reconstruction (in line with recommendations by Thomas, Citation2010) wherein a fictional defendant with mental health problems is tried for homicide, with study participants forming a mock jury.
The study used a between-subjects design, with quantitative data collected to evaluate potential differences between two differing study conditions: one where the defendant’s mental health problems are described as being part of a ‘severe personality disorder, borderline pattern’ (SPD); and one where they are described as ‘complex mental health problems’ (the control condition). The latter phrase was deliberately chosen to not be a formal mental health diagnosis but to give a clear impression of impairment because of a mental health problem. The manipulation in diagnostic terminology was the only difference between the two vignettes.
Case simulation stimuli
This study aimed to provide a realistic approximation of a homicide trial, using a filmed trial reconstruction. The film produced presented a condensed version of such a trial, running to 18 minutes’ viewing time between sections and containing expert witness testimony, prosecution and defence arguments, and instructions to the jury (the participants of the study). The film was produced using a mock-court setting, with the assistance of undergraduate law students as actors. A written case scenario outlining the events of the case supported the film, alongside a diminished responsibility information sheet detailing the criteria of the defence.
Expert witness testimony
The expert witness testimony was also presented as a video, acted by a clinical psychologist with experience in expert witness work, who outlined a mental health history and narrative formulation of the mental health problems of the defendant. This narrative formulation was consistent with clinical descriptions of borderline personality disorder, including features of emotion dysregulation, difficulties with mentalisation and heightened perception of social threat, as well as suicidality and self-harm based risk information. This formulation prominently linked the development of these problems to severe sexual abuse and familial adversity in the defendant’s personal history. This clip contained no references to the events of the crime and was shown before the written case scenario was shared with participants, to enable measurement of stigma-related beliefs based solely upon the defendant’s clinical characteristics, and not their crime.
Case scenario
The written case scenario describes the circumstances of the killing of the victim, prior events of the day and the characters involved. Briefly, the scenario explains that the defendant met the victim at a neighbourhood barbecue event. After the victim behaves in a drunkenly flirtatious way towards the defendant’s younger sister, the defendant is verbally aggressive towards the victim and leaves. The victim seeks to apologise and, upon arriving at the defendant’s house, is attacked and stabbed in the neck by the defendant during an escalating verbal argument. The circumstances of the case are framed in such as a way as to be relevant to the defendant’s history of trauma and their mental health problems: the victim strongly resembles a historical abuser of the defendant; the defendant believes her younger sister was also abused and is strongly protective of her; the defendant has a history of misperceiving threats, and so could conceivably have perceived severe danger and acted in ‘self-defence’; the defendant was highly distressed during and afterward when found by police.
Trial reconstruction
The trial reconstruction consists of prosecution and defence arguments concerning the defence of diminished responsibility, and a judge’s instructions to the jury (the participants of the study) to decide whether this defence was applicable. The defendant is not shown within the film, to avoid conjecture as to appearance or emotional responses interfering with other aspects of judgement of the case. Given the observations of Mackay (Citation2018) relating to common disagreement between expert witnesses in cases involving diminished responsibility, both the prosecution and defence arguments referred to conflicting psychiatric reports commissioned by each respective side. The prosecution argument framed the defendant as manipulative and in control of their actions, and the defence argument portrayed the defendant as a fearful, traumatised individual who thought that she was in severe danger. While their arguments refer to conflicting psychiatric reports, no significant additional clinical information is presented beyond that already presented within the expert witness testimony section.
The judge’s instructions to the jury summed up these arguments and requested that the jury consider the defence of diminished responsibility. These instructions outlined that depending on their verdict, the defendant would be found guilty of either murder or manslaughter on the grounds of diminished responsibility. Simplified implications of each verdict were presented: either a mandatory ‘life sentence’ of 15 years in prison (guilty to murder); or treatment within a secure psychiatric hospital (guilty to manslaughter by diminished responsibility).
(Please see additional materials for the case scenario, script of the film and supporting diminished responsibility criteria sheet.)
Experimental manipulation
The experimental manipulation in this study concerned whether the clinical information presented within the expert testimony and trial reconstruction referred to the ‘severe personality disorder, borderline pattern’ diagnosis, or whether this was removed and replaced with a ‘complex mental health problems’ placeholder term. These are referred to as ‘severe personality disorder’ and ‘complex mental health’ conditions, respectively. This was achieved via the creation of two otherwise identical films.
Measures
Causal Attribution Questionnaire (Dagnan et al., Citation1998; Markham & Trower, Citation2003)
The Causal Attribution Questionnaire (CAQ) was used to assess attributions about the cause of the defendant’s behaviour, and has previously been used in studies assessing attributions of difficult or challenging behaviour with reference to Weiner’s (Citation1986) cognitive–emotional model of attribution (e.g., Dagnan et al., Citation1998). Markham and Trower’s (Citation2003) adapted version of the CAQ (which considered causal attributions made towards people with borderline personality disorder by psychiatric nurses) was adopted. It assesses causal attributions regarding four negative events involving a person, such as ‘X did not attend an appointment at the job centre’, and asks respondents to write a speculative cause (i.e., ‘she was lazy’; ‘she suffers from trauma’). Various parameters of potential attribution are then presented, according to dimensions of locus (how internal or external the cause is to the person), stability (whether this feature is stable or unstable), globality (whether the cause occurs in relation to many events, or very specific ones) and controllability (how controllable the cause was). These are rated on 7-point bipolar scales. In Markham and Trower (Citation2003), participants rated the cause of an incident of challenging behaviour. For this study, the question relating to challenging behaviour was changed to ‘what do you think was a main cause of the crime?’, while the others were unaltered. Each attribution dimension is rated four times, with scores summed to provide a score up to a maximum of 28 points. Russell et al. (Citation1987) provide Cronbach’s alpha scores for the scales of locus (α = .78) stability (α = .85) and controllability (α = .51). From the dataset obtained in this study, the CAQ appeared to have a somewhat less impressive internal consistency, α = .64.
Attribution Questionnaire–27 (AQ–27; Corrigan et al., Citation2003)
The Attribution Questionnaire–27 (AQ–27) asks respondents 27 questions relating to nine domains of stereotypical beliefs towards a person with a mental illness. These domains correspond to blame, anger, pity, dangerousness, help, fear, avoidance, segregation and coercion. There are three questions concerning each domain, with each rated on 9-point bipolar scales, thus a total possible score of 27. Corrigan et al. (Citation2003) reported Cronbach’s alpha coefficients ranging from .70 to .96 across the nine scales. It has been widely used across international samples (Muñoz et al., Citation2015; Pingani et al., Citation2012). From the dataset obtained in this study, the AQ–27 appeared to have a somewhat less impressive internal consistency, α = .67; however, this rose to α = .83 with removal of the pity and help subscales, suggesting some variability in reliability between domains.
The AQ–27 typically presents respondents with a short, written vignette concerning a man named Harry with schizophrenia. For the purposes of this study, this vignette was changed to reflect the defendant and their mental health problems. It does not otherwise refer to the details of the case. It was presented to participants after they had learned about the defendant’s mental health problems, but before they had learned the details of the case.
Diminished Responsibility Questionnaire
To capture judgements relating to the legal question of diminished responsibility, a measure was designed for the purposes of this study, as no measures exist in the literature. This is referred to as the DRQ (Diminished Responsibility Questionnaire). In the DRQ, the circumstances of the crime are broken down into four scenarios, with each part rated against each aspect of the legal DR criteria via 7-point bipolar scales. As an example, one question presented the statement ‘X then took a kitchen knife from the side, opened her front door and stabbed Y in the neck, causing major injuries’. The subsequent scales asked ‘was this related to a recognised medical condition?’ (not related/entirely related), ‘could she understand her conduct, form a rational judgement, or exercise self-control?’ (totally unable/fully able for each) and ‘do any of the factors explain how she acted?’ (these do not/one or more fully explains her actions). In completion of the measure, each factor of the diminished responsibility criteria is rated four times, with scores summed to provide final scores out of a maximum of 28 points for each criterion. The DRQ appeared to have excellent internal consistency, α = .94, possibly reflecting the fact that it is based on a single legal construct with a limited number of questions.
Group-based judgements
All primary analysis was conducted in relation to the individual measures described above. However, to ensure the participants followed a standardised jury procedure, jurors were asked to debate and deliver an overall group-based verdict of whether DR would be granted. To avoid interference with individual judgements, this was conducted after individual measures had been completed.
Participants
The study population consisted of a mixture of undergraduate and postgraduate students from the University of East Anglia, staff members of varying roles employed at the University of East Anglia, and other members of the public from the Norfolk and Suffolk regions of East Anglia, UK. A total of 50 participants took part, composed of 27 undergraduate and postgraduate students, 17 university employees and 6 members of the public. Participant ages ranged from 18 to 60 years. The mean age for the full sample was 29 years (median 24 years), with a mean age of 31 years in the ‘Complex Mental Health Problems’ group, and a mean age of 26.9 years in the ‘Severe Personality Disorder’ group). For other participant characteristics, see .
Table 1. Participant characteristics.
The undergraduate/postgraduate proportion of the sample had a diverse range of fields of study, including biological sciences, medicine, IT, English literature, mathematics and law. Meanwhile, the university employee proportion of the sample consisted of administrative and teaching staff from a varied range of university departments and schools. Potential participants who had fields of study, teaching positions or occupations relating to psychology or psychiatry were excluded from the study at the recruitment stage. This was to ensure a necessary degree of separation from the mental health professions and to limit prior familiarity with elements of the health and diagnostic information presented in the course of the study.
Sample size and power
Power analyses undertaken during the planning stage of the study indicated that the minimum number of participants required for the study was 48. This number was based on planned multivariate analyses of variance (MANOVAs) with a medium effect size of 0.25 and power of 0.8.
Sampling procedure
The study was advertised within the university via newsletters distributed via email, digital screens displayed around the campus and physical advertisements displayed on communal noticeboards. Potential participants registered their interest via email. In addition, on days in which the study was running, mobile noticeboards were placed advertising the study and directing potential participants to specific sessions, allowing for more opportunistic sampling of participants.
Study sessions were conducted in blocks of 8–9 participants, to provide an approximation of a jury experience and to allow for discussion and provision of a ‘jury verdict’ at the end of the study. Participants were not randomised to their respective conditions; this was impractical since many participants of the study were full-time university employees who had to balance time to attend around working hours. However, the participants were naive as to the nature of the differing study conditions until being debriefed at the end of each session.
While this flexibility of recruitment and arrangement of study sessions enabled a larger sample than would otherwise have been achieved, it affected the degree of matching of participants between groups, forming a significant limitation of the study as the final participant groups are demographically different in terms of average age, ethnicity and proportion of undergraduate/postgraduate students to university employees and members of the public.
Recruitment took place between March and October 2019, finishing upon achievement of sufficient participants needed to achieve appropriate statistical power.
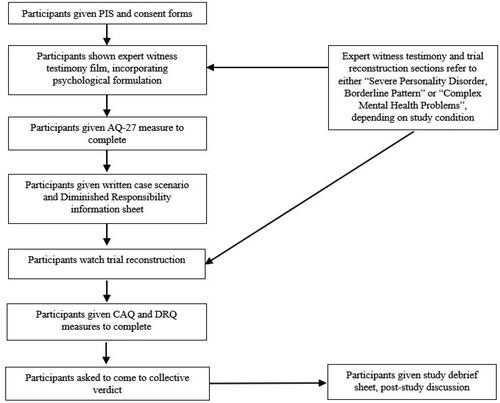
Study procedure
The procedure is described in . The process, in total consisting of watching of the film, reading of the case scenario and diminished responsibility information sheet and provision and completion of study measures, took approximately one hour to complete.
Ethical approval
Ethical approval was gained for this study from the University of East Anglia Faculty of Medicine and Health Sciences ethics panel. Given the nature of the case and graphic descriptions contained within the case scenario, information was provided regarding how participants could seek additional support after the study if they were distressed by the material. No participants felt the need to do so. Participants were paid £5 for their participation in the study.
Data analysis
This study design employed a singular independent variable with two levels: the ‘severe personality disorder’ experimental condition and the ‘complex mental health’ control condition. It assessed potential differences in 18 dependent variables: AQ–27 variables of blame, anger, pity, dangerousness, help, fear, avoidance, segregation and coercion (9); CAQ variables of locus, stability, globality and controllability (4); and DRQ variables of recognised medical condition, understanding, rational judgement, self-control and explaining actions (5).
Analysis using a MANOVA was not possible due to violation of assumptions (failing the homogeneity of variance–covariance matrices assumption); therefore, a series of independent samples t tests were used to compare means for each variable between groups in conjunction with the Holm alpha reduction technique with respect to multiple comparisons (Holm, Citation1979). In the use of this method, p values under .05 are ranked in order of size, smallest first, and critical p values for significance are adjusted relative to this rank. Therefore, these are reported where these are below the traditional .05 level but do not meet the adjusted level for significance, to aid interpretation.
Assessment of the study data using the Shapiro–Wilks test of normality indicated that the data were normally distributed, and so the use of parametric tests was appropriate.
Results
The mean causal attribution, stigma-related belief and diminished responsibility ratings are displayed in , alongside their mean differences and standard error, 95% confidence intervals, t statistics and Cohen’s d effect sizes. Higher numbers for the CAQ causal attribution dimensions indicate greater internal locus of cause, greater stability, greater globality and more control over cause and the event. Higher numbers for the AQ–27 stigma-related beliefs indicate greater endorsement of beliefs in each domain, and greater numbers for the DRQ indicate greater endorsement of each aspect of the diminished responsibility criteria.
Table 2. Between-group Causal Attribution Questionnaire, Attribution Questionnaire–27 and Diminished Responsibility Questionnaire summary statistics, t-statistics and effect sizes.
In regard to the first hypothesis (differences in causal attributions), none of the subscales showed statistically significant differences between groups following Holm alpha reduction. However, the CAQ–Control Cause subscale was associated with a medium between-group effect size (d = 0.65, with participants in the SPD condition tending to report the defendant had a greater control over their actions). It is notable that both CAQ–Stability (likelihood of change) and CAQ–Globality (generalisability across situations) did not show any evidence of between-group differences, though the absolute scores appeared relatively high (indicating that participants in both conditions felt the person’s condition was both stable and global/generalisable). Overall, therefore, there was only limited evidence of a difference in causal attributions between groups.
In regard to the second hypothesis (differences in stigma-related beliefs), three subscales showed significant between-group differences. These were AQ–Dangerousness (participants rated as more dangerous in the SPD condition), AQ–Segregation (higher need for segregation in the SPD condition) and AQ–Coercion (higher need for coercive treatment in the SPD condition). Furthermore, between-group differences of the AQ–Avoidance scale did not reach statistical significance after Holm adjustment, but were associated with a medium effect size (d = 0.68, with participants in the SPD condition tending to report more need to avoid the defendant). Overall, therefore, there was evidence that in several domains that could be considered highly relevant to juror decision-making, participants in the SPD condition espoused more stigmatic attitudes than those in the control condition.
In regard to the third hypothesis, there was no evidence of between-group differences in the inclination to give a verdict of diminished responsibility, as measured by the domains of the DRQ. However, as illustrates, scores on this measure appeared relatively high across most domains (the minimum, midpoint and maximum scores on this measure are 4, 16 and 28, respectively), suggesting overall that individuals felt that most elements of the DR criteria were met, in both conditions.
This finding is supported by the overall verdicts delivered by the groups, which consistently found in favour of granting diminished responsibility. In most groups this was resolved quickly, and unanimity was reached without substantial debate between participants. Within two of the severe personality disorder groups, unanimity required some debate between participants due to initial differences of opinion. This was, however, resolved quickly, and no group required substantial amounts of time to come to a group verdict. No formal analysis was conducted on the group verdicts.
Discussion
The purpose of this study was to assess whether the manipulation of diagnostic terminology resulted in differences in the way in which a defendant was perceived by mock-jury participants within a homicide trial scenario. The experimental manipulation consisted of calling a defendant’s mental health problems a ‘severe personality disorder (borderline pattern)’ or ‘complex mental health problems’, in the context of otherwise identical trauma-focused clinical information.
Taken together, the results of this study indicate that use of the ‘severe personality disorder (borderline pattern)’ diagnosis resulted in greater endorsement of particular stigmatising beliefs regarding the defendant, although it did not greatly affect attributional inferences made by participants regarding defendant behaviour, or aspects of their overall decision-making concerning the applicability of the diminished responsibility legal defence. Indeed, participants endorsed judgements of manslaughter by diminished responsibility, as opposed to murder, to a universal extent in group verdicts and signalled strong agreement with the criteria in their individual ratings across both groups. The results and their bearing upon the study hypotheses, limitations of the study, potential implications and future directions for research are discussed.
Stigma-related beliefs
The hypothesis that the manipulation of diagnostic terminology would result in differences in stigma-related beliefs, as measured by the AQ–27 (Corrigan et al., Citation2003), was supported by the results. There were significant differences between the SPD and control groups within the domains of dangerousness, coercion and segregation, for which there were large effects. This appears to show that referring to the defendant’s difficulties as a ‘severe personality disorder (borderline pattern)’ resulted in them being perceived as more dangerous, as more in need of coercive psychiatric treatment and more in need of segregation from the public. This measure was taken after exposure to the psychological formulation, but before the events of the case were described, indicating that these results are the effect of the diagnostic terminology itself, and not attitudes developed in response to an account of a homicide.
Taking a broad view of AQ–27 absolute scores across domains, it appears that generally the defendant was viewed in a moderately sympathetic manner. It appears that regardless of diagnostic terminology, participants felt that the defendant was highly pitiable and in need of help, as reflected by consistent high scores in these domains. While the domain of segregation was endorsed to a greater degree in the severe personality disorder condition, scores in both conditions are relatively low, as are those for anger and fear. Therefore, while important differences are shown between the groups within more negative domains, it appears that in this scenario, generally participants felt that the defendant required support, rather than punishment and retribution. It appears, however, that participants also endorsed coercive treatment (described as being forced to take medication, attend treatment or live in a treatment facility) to a moderate extent, and to a greater degree in the severe personality disorder condition. This is a nuanced picture of effects, which requires further study, perhaps with vignettes that might be more ambiguous in terms of the need for support.
The results obtained here from a simple manipulation of diagnostic terminology suggest that there is an intuitive meaning obtained from the diagnostic term used, which is inherently stigmatising. It is noteworthy that such a small manipulation led to the large effects observed. However, this perhaps simply emphasises the power of the terminology used, and is consistent with other findings in relation to ASPD and psychopathy highlighted earlier (e.g., Kelley et al., Citation2019); ‘personality’ has a lay meaning that historically relates to character, constitution and self (Berrios, Citation1993); and the division between ‘personality disorder’ as a clinical entity and ‘personhood’ is not straightforward (Glas, Citation2006). Markham and Trower (Citation2003) suggest that the term implicitly communicates there is ‘something intrinsically “disordered” about the person’. To invoke levels of severity in the new ICD–11 criteria alongside this may provide diagnostic specificity to clinicians (Bach & First, Citation2018), and perhaps add clarity to the legal question of diminished responsibility, which appears muddled by conceptual confusion and discrepancy of clinical opinion (Mackay, Citation2018; Peay, Citation2011). However, it may also carry stigmatising lay meanings relating to dangerousness and a need for coercive treatment. These were present within our results even though mock-jurors appeared to view the defendant in a relatively sympathetic manner, and consistently judged them as having diminished responsibility.
Causal attributions
The hypothesis that the variation in diagnostic terminology between the two groups would result in differences in causal attributions made for the behaviour of the defendant, as measured by the CAQ (Markham & Trower, Citation2003), was not supported by the results. However, high mean scores for locus, stability and globality across both groups indicate that generally participants attributed the defendant’s behaviour to something internal to them as a person, something that was unlikely to change over time and would likely affect how they would behave in a variety of situations.
Diminished responsibility ratings
The hypothesis that the differing diagnostic terminology used between the groups would result in differences to ratings made against the diminished responsibility criteria, as measured using the DRQ developed for this study, was not supported by the results. However, generally high mean scores across these indicate broad agreement that the defendant met the criteria for the diminished responsibility defence.
This finding is of interest as it contrasts with the earlier cited data suggesting that DR verdicts in cases of personality disorder tend to fail (Mackay, Citation2018; Mackay & Mitchell, Citation2017). There are several ways that this might be understood. First, this might be a limitation of the sampling characteristics – that is, that the sample was generally skewed in terms of attitudes associated with less punitive behaviour. Second, this might be understood as a limitation of the vignette used – that is, that the vignette or description of the defendant’s history evoked ‘too much’ sympathy.
Strengths and limitations
The present study is a novel approach to consider a under-researched topic. It uses ecologically valid methods of conveying study stimuli, with efforts undertaken to provide a realistic approximation of a jury trial through its materials and setting through use of a case-simulation method (Thomas, Citation2010). This may be considered a particular strength, since studies concerning jury decision-making often utilise written vignettes and omit a trial procedure and jury discussion (i.e., Berryessa et al., Citation2015; Mossière & Maeder, Citation2016) and have attracted criticism concerning authenticity (Sommers & Elsworth, Citation2003; Thomas, Citation2010).
However, there are several limitations to the present study, which should be accounted for. Broadly, these relate to the measures adopted, as well as aspects of the sampling methodology.
In relation the measures used, it is noted that these have been subject to some critical treatment in the literature (e.g., Brown, Citation2008, who outlines a six-factor structure of the AQ–27), and the CAQ (Dagnan et al., Citation1998; Markham & Trower, Citation2003) has not formally been validated in the form used in this study. The CAQ, in particular, showed some evidence of unreliability in the present study. However, alternative, more suitable measures are lacking, and it is not obvious to the authors that better measures might have been used.
In relation to the sampling methodology, there are a number of limitations here that must be acknowledged that together may impinge on ecological validity. Firstly, given the recruitment strategy, it is not possible to consider the sample as population representative. Furthermore, there were some apparent differences between the groups in terms of demographic characteristics. Gender bias may be a particular consideration in terms of the fact that a female defendant was portrayed, since it is known that the respective genders of defendants, victims and jurors appear to impact the way in which jurors appraise defendant–victim power relations, defendant responsibility and believability (Hodell et al., Citation2014; Pozzulo et al., Citation2010). Furthermore, female defendants may be less likely to be convicted of homicide in mock-jury studies (Hodell et al., Citation2014). Secondly, however, there is a broader potential concern here about the make-up of the jury in that with staff and students mixed together, power dynamics may have influenced outcome, at least in the group decision tasks (this should not have impacted the primary individual measures, however). Finally, of course, this was a relatively small sample, and Holm adjustment meant that only relatively large effect sizes were able to be detected.
Future directions for research
Future work to replicate these important but initial findings is necessary. Replication research that seeks to address limitations in the present study should consider ensuring that sampling characteristics are more representative of the general public (and ideally with a larger sample to enable smaller effects to be detected), and further should consider adaptations to the information provided in vignette materials to increase ambiguity of clinical presentation and the extent that this can be linked to the person’s behaviour (with the aim of leading to greater variation in juror decision-making, and thus making a difference in decision-making behaviour more detectable). Additionally, work could focus on revising, improving or adapting the measures used to make them more suitable for application in this context, and potentially look to standardise them against larger and more representative samples.
However, the research also points towards a number of different avenues that could be helpfully explored. Firstly, there is a need to consider the impact of the different elements of personality disorder terminology. The new ICD–11 criteria introduce the potential for generic terms such as ‘severe’ to additionally compound the stigma inferred by descriptors such as ‘borderline’ and, of course, ‘personality disorder’. Are alternative conceptualisations, such as those that focus on the relevance of trauma, any less stigmatising? Can such conceptualisations be considered in other stigmatised personality disorders, such as ASPD and psychopathy?
Secondly, the research points towards a potential avenue that considers the impact of the way in which background information about a case is presented, which might potentially be conveyed within a psychological formulation. This is of pragmatic importance since clinicians providing evidence have significant latitude to determine how to present a clinical assessment, and any structure, format or approach that worked to reduce stigma would be helpful in standardising the experience for defendants. Several initial questions emerge in relation to this topic: the impact of psychological formulation upon juror empathy and decision-making; whether this exists across differing mental health diagnoses; whether different kinds of formulation have differing effects; methods of presentation and accessibility to laypersons; and whether individual juror characteristics affect these concepts.
Thirdly, the research highlights a significant gap in the literature in relation to the impact of stigma of mental health problems in settings other than mental health professionals, which has been the focus of most research (Aviram et al., Citation2006). Other areas, such as interactions with police and emergency services, the criminal justice system, employment support and assessment for disability and social security benefits would be impactful.
Finally, whilst the locus of the present research was situated in the legal question of diminished responsibility, there is the need to consider the relevance of stigma in relation to personality disorders and mental health conditions in a range of different legal judgements. This includes other judgements that might be carried out by juries (notably, findings of guilt), but also decision-making by other actors in the sphere of the criminal court: primarily, lawyers, judges and clinicians.
Conclusion
Overall, these findings seem to have potentially significant implications for the way in which laypeople in juries perceive defendants described as having BPD. Whilst significant between-group differences were not observed across all domains explored (particularly in relation to causal attributions or the actual decision to provide a verdict of diminished responsibility), the significant differences that were identified were in key domains that have the potential to be relevant to the decisions made by juries in relation to people presenting with borderline personality disorder. They provide a prima facie demonstration that stigmatic attitudes that exist in the public in relation to people with borderline personality disorder can also exist in a courtroom context. Whilst the actual implications of such stigmatic attitudes are unknown, and not illustrated clearly by the present research, we know that stigma about BPD in a range of other situations (primarily through research with mental health professionals; Sheehan et al., Citation2016) is associated with therapeutic pessimism (Lam, Poplavskaya, et al., Citation2016, Lam, Salkovskis, et al., Citation2016), greater desired social distance (Aviram et al., Citation2006; Markham, Citation2003), outright dislike and discrimination (G. Lewis & Appleby, Citation1988) and rejection from services (Sulzer, Citation2015). Meanwhile, public awareness of BPD appears to be low, which may suggest that this leads to negative reactions to distress, including seeing those diagnosed with BPD as manipulative (Furnham et al., Citation2015). Furthermore, literature exploring the impact of a diagnosis of ASPD or psychopathy on behaviour in the courtroom environment (e.g., Edens et al., Citation2005, Citation2013) highlights the very real possibility that the observed stigmatic attitudes could indeed ‘bleed’ into courtroom decision-making. The potential for this to occur – particularly bearing in mind the limitations and blurred boundaries between diagnostic entities, should be of significant concern to anybody interested in the just application of criminal law to people with mental health conditions and should stimulate future research opportunities.
Finally, the use of the ICD–11 framework suggests that this framework may be no more effective in reducing stigma than traditional diagnostic descriptions of BPD. These findings broadly echo those of Markham (Citation2003), who identified greater ratings of dangerousness and desired social distance by nurses towards patients with BPD than towards patients with schizophrenia and depression.
As we adopt a new range of personality disorder terminology more than 30 years after G. Lewis and Appleby (Citation1988) called for its abandonment, its utility and unintended consequences must be carefully and critically considered.
Ethical standards
Declaration of conflicts of interest
James Baker has declared no conflicts of interest
Ian Edwards has declared no conflicts of interest
Peter Beazley has declared no conflicts of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of East Anglia Faculty of Medicine and Health Sciences and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
Expert Testimony and Mock Trial Script
Download MS Word (20.1 KB)Case Scenario
Download MS Word (13.7 KB)Jury Decision Making - Diminished Responsibility - Additional Materials
Download MS Word (23.2 KB)References
- Aviram, R. B., Brodsky, B. S., & Stanley, B. (2006). Borderline personality disorder, stigma, and treatment implications. Harvard Review of Psychiatry, 14(5), 249–256. https://doi.org/https://doi.org/10.1080/10673220600975121
- Ayre, K., Owen, G. S., & Moran, P. (2017). Mental capacity and borderline personality disorder. BJPsych Bulletin, 41(1), 33–36. https://doi.org/https://doi.org/10.1192/pb.bp.115.052753
- Bach, B., & First, M. B. (2018). Application of the ICD-11 classification of personality disorders. BMC Psychiatry, 18(1), 1–14. https://doi.org/https://doi.org/10.1186/s12888-018-1908-3
- Berrios, G. E. (1993). European views on personality disorders: A conceptual history. Comprehensive Psychiatry, 34(1), 14–30. https://doi.org/https://doi.org/10.1016/0010-440X(93)90031-X
- Berryessa, C. M., Milner, L. C., Garrison, N. A., & Cho, M. K. (2015). Impact of psychiatric information on potential jurors in evaluating high-functioning autism spectrum disorder (hfASD). Journal of Mental Health Research in Intellectual Disabilities, 8(3–4), 140–167. https://doi.org/https://doi.org/10.1080/19315864.2015.1040176
- Brown, S. A. (2008). Factors and measurement of mental illness stigma: A psychometric examination of the Attribution Questionnaire. Psychiatric Rehabilitation Journal, 32(2), 89–94. https://doi.org/https://doi.org/10.2975/32.2.2008.89.94
- Catthoor, K., Feenstra, D. J., Hutsebaut, J., Schrijvers, D., & Sabbe, B. (2015). Adolescents with personality disorders suffer from severe psychiatric stigma: Evidence from a sample of 131 patients. Adolescent Health, Medicine and Therapeutics, 6, 81–89. https://doi.org/https://doi.org/10.2147/AHMT.S76916
- Charland, L. (2006). Moral nature of the DSM-IV Cluster B personality disorders. Journal of Personality Disorders, 20(2), 116–125. https://doi.org/https://doi.org/10.1521/pedi.2006.20.2.116
- Chartonas, D., Kyratsous, M., Dracass, S., Lee, T., & Bhui, K. (2017). Personality disorder: Still the patients psychiatrists dislike? BJPsych Bulletin, 41(1), 12–17. https://doi.org/https://doi.org/10.1192/pb.bp.115.052456
- Corrigan, P., Markowitz, F. E., Watson, A., Rowan, D., & Kubiak, M. A. (2003). An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior, 44(2), 162–179. https://doi.org/https://doi.org/10.2307/1519806
- Crowell, S. E., Beauchaine, T. P., & Linehan, M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510. https://doi.org/https://doi.org/10.1037/a0015616
- Dagnan, D., Trower, P., & Smith, R. (1998). Care staff responses to people with learning disabilities and challenging behaviour: A cognitive-emotional analysis. The British Journal of Clinical Psychology, 37(1), 59–68. https://doi.org/https://doi.org/10.1111/j.2044-8260.1998.tb01279.x
- DeMatteo, D., & Edens, J. F. (2006). The role and relevance of the Psychopathy Checklist-Revised in court: A case law survey of U.S. courts (1991–2004). Psychology, Public Policy, and Law, 12(2), 214–241. https://doi.org/https://doi.org/10.1037/1076-8971.12.2.214
- Edens, J. F., Colwell, L. H., Desforges, D. M., & Fernandez, K. (2005). The impact of mental health evidence on support for capital punishment: Are defendants labeled psychopathic considered more deserving of death? Behavioral Sciences & the Law, 23(5), 603–625. https://doi.org/https://doi.org/10.1002/bsl.660
- Edens, J. F., Cox, J., Smith, S. T., DeMatteo, D., & Sörman, K. (2015). How reliable are Psychopathy Checklist-Revised scores in Canadian criminal trials? A case law review. Psychological Assessment, 27(2), 447–456. https://doi.org/https://doi.org/10.1037/pas0000048
- Edens, J. F., Davis, K. M., Fernandez Smith, K., & Guy, L. S. (2013). No sympathy for the devil: Attributing psychopathic traits to capital murderers also predicts support for executing them. Personality Disorders, 4(2), 175–181. https://doi.org/https://doi.org/10.1037/a0026442
- Furnham, A., Lee, V., & Kolzeev, V. (2015). Mental health literacy and borderline personality disorder (BPD): What do the public “make” of those with BPD? Social Psychiatry and Psychiatric Epidemiology, 50(2), 317–324. https://doi.org/https://doi.org/10.1007/s00127-014-0936-7
- Glas, G. (2006). Person, personality, self, and identity: A philosophically informed conceptual analysis. Journal of Personality Disorders, 20(2), 126–138. https://doi.org/https://doi.org/10.1521/pedi.2006.20.2.126
- Greene, E., & Cahill, B. S. (2012). Effects of neuroimaging evidence on Mock Juror decision making. Behavioral Sciences & the Law, 30(3), 280–296. https://doi.org/https://doi.org/10.1002/bsl.1993
- Gurley, J. R., & Marcus, D. K. (2008). The effects of neuroimaging and brain injury on insanity defences. Behavioral Sciences & the Law, 26(1), 85–97. https://doi.org/https://doi.org/10.1002/bsl.797
- Hodell, E. C., Wasarhaley, N. E., Lynch, K. R., & Golding, J. M. (2014). Mock Juror gender biases and perception of self-defense claims in intimate partner homicide. Journal of Family Violence, 29(5), 495–506. https://doi.org/https://doi.org/10.1007/s10896-014-9609-2
- Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 6(2), 65–70. https://www.jstor.org/stable/4615733
- Kelley, S. E., Edens, J. F., Mowle, E. N., Penson, B. N., & Rulseh, A. (2019). Dangerous, depraved, and death-worthy: A meta-analysis of the correlates of perceived psychopathy in jury simulation studies. Journal of Clinical Psychology, 75(4), 627–643. https://doi.org/https://doi.org/10.1002/jclp.22726
- Knefel, M., Tran, U. S., & Lueger-Schuster, B. (2016). The association of posttraumatic stress disorder, complex posttraumatic stress disorder, and borderline personality disorder from a network analytical perspective. Journal of Anxiety Disorders, 43, 70–78. https://doi.org/https://doi.org/10.1016/j.janxdis.2016.09.002
- Koekkoek, B., Hutschemaekers, G., van Meijel, B. & Schene, A. (2011). How do patients come to be seen as ‘difficult’?: A mixed-methods study in community mental health care. Social Science & Medicine, 72(4), 504–512. https://doi.org/https://doi.org/10.1016/j.socscimed.2010.11.036
- Lam, D. C. K., Poplavskaya, E. V., Salkovskis, P. M., Hogg, L. I., & Panting, H. (2016). An experimental investigation of the impact of personality disorder diagnosis on clinicians: Can we see past the borderline? Behavioural and Cognitive Psychotherapy, 44(3), 361–373. https://doi.org/https://doi.org/10.1017/S1352465815000351
- Lam, D. C. K., Salkovskis, P. M., & Hogg, L. I. (2016). ‘Judging a book by its cover’: An experimental study of the negative impact of a diagnosis of borderline personality disorder on clinicians' judgements of uncomplicated panic disorder. The British Journal of Clinical Psychology, 55(3), 253–268. https://doi.org/https://doi.org/10.1111/bjc.12093
- Leichsenring, F., Leibing, E., Kruse, J., New, A. S., & Leweke, F. (2011). Borderline personality disorder. The Lancet, 377(9759), 74–84. https://doi.org/https://doi.org/10.1016/S0140-6736(10)61422-5
- Lewis, G., & Appleby, L. (1988). Personality disorder: The patients psychiatrists dislike. The British Journal of Psychiatry: The Journal of Mental Science, 153, 44–49. https://doi.org/https://doi.org/10.1192/bjp.153.1.44
- Lewis, K. L., & Grenyer, B. F. S. (2009). Borderline personality or complex posttraumatic stress disorder? An update on the controversy. Harvard Review of Psychiatry, 17(5), 322–328. https://doi.org/https://doi.org/10.3109/10673220903271848
- Luyten, P., Campbell, C., & Fonagy, P. (2019). Borderline personality disorder, complex trauma, and problems with self and identity: A social-communicative approach. Journal of Personality, 88(1), 88–105. https://doi.org/https://doi.org/10.1111/jopy.12483
- Mackay, R. (2018). The impairment factors in the new diminished responsibility plea. Criminal Law Review, 6, 462–471.
- Mackay, R., & Mitchell, B. (2017). The new diminished responsibility plea in operation- some initial findings. Criminal Law Review, 1, 18–35.
- Marcus, D. K., Lilienfeld, S. O., Edens, J. F., & Poythress, N. G. (2006). Is antisocial personality disorder continuous or categorical? A taxometric analysis. Psychological Medicine, 36(11), 1571–1581. https://doi.org/https://doi.org/10.1017/S0033291706008245
- Markham, D. (2003). Attitudes towards patients with a diagnosis of ‘borderline personality disorder’: Social rejection and dangerousness. Journal of Mental Health, 12(6), 595–612. https://doi.org/https://doi.org/10.1080/09638230310001627955
- Markham, D., & Trower, P. (2003). The effects of the psychiatric label ‘borderline personality disorder’ on nursing staff’s perceptions and causal attributions for challenging behaviours. The British Journal of Clinical Psychology, 42(Pt 3), 243–256. https://doi.org/https://doi.org/10.1348/01446650360703366
- Mossière, A., & Maeder, E. M. (2016). Juror decision making in not criminally responsible on account of mental disorder trials: Effects of defendant gender and mental illness type. International Journal of Law and Psychiatry, 49(Pt A), 47–54. https://doi.org/https://doi.org/10.1016/j.ijlp.2016.05.008
- Muñoz, M., Guillén, A. I., Pérez-Santos, E., & Corrigan, P. W. (2015). A structural equation modeling study of the Spanish Mental Illness Stigma Attribution Questionnaire (AQ-27-E)). The American Journal of Orthopsychiatry, 85(3), 243–249. https://doi.org/https://doi.org/10.1037/ort0000059
- Peay, J. (2011). Personality disorder and the law: Some awkward questions. Philosophy, Psychiatry and Psychology, 18(3), 231–244. https://doi.org/https://doi.org/10.1353/ppp.2011.0035
- Pingani, L., Forghieri, M., Ferrari, S., Ben-Zeev, D., Artoni, P., Mazzi, F., Palmieri, G., Rigatelli, M., & Corrigan, P. W. (2012). Stigma and discrimination toward mental illness: Translation and validation of the Italian version of the attribution questionnaire-27 (AQ-27-I). Social Psychiatry and Psychiatric Epidemiology, 47(6), 993–999. https://doi.org/https://doi.org/10.1007/s00127-011-0407-3
- Pozzulo, J. D., Dempsey, J., Maeder, E., & Allen, L. (2010). The effects of victim gender, defendant gender, and defendant age on juror decision making. Criminal Justice and Behavior, 37(1), 47–63. https://doi.org/https://doi.org/10.1177/0093854809344173
- Russell, D. W., McAuley, E., & Tarico, V. (1987). Measuring causal attributions for success and failure: A comparison of methodologies for assessing causal dimensions. Journal of Personality and Social Psychology, 52(6), 1248–1257. https://doi.org/https://doi.org/10.1037/0022-3514.52.6.1248
- Sheehan, L., Nieweglowski, K., & Corrigan, P. (2016). The stigma of personality disorders. Current Psychiatry Reports, 18(1), 1–7. https://doi.org/https://doi.org/10.1007/s11920-015-0654-1
- Skeem, J. L., & Cooke, D. J. (2010). Is criminal behavior a central component of psychopathy? Conceptual directions for resolving the debate. Psychological Assessment, 22(2), 433–445. https://doi.org/https://doi.org/10.1037/a0008512
- Smith, D. J., Muir, W. J., & Blackwood, D. H. (2006). Neurocognitive impairment in euthymic young adults with bipolar spectrum disorder and recurrent major depressive disorder. Bipolar Disorders, 8(1), 40–46. https://doi.org/https://doi.org/10.1111/j.1399-5618.2006.00275.x
- Sommers, P. C., & Elsworth, S. R. (2003). How much do we really know about race and juries? A review of social science theory and research. University of Chicago Law Review, 78(3), 997–1031.
- Sparr, L. F. (2009). Personality disorders and criminal law: An international perspective. The Journal of the American Academy of Psychiatry and the Law, 37(2), 168–181.
- Sulzer, S. H. (2015). Does “difficult patient” status contribute to de facto demedicalization? The case of borderline personality disorder. Social Science & Medicine (1982), 142, 82–89. https://doi.org/https://doi.org/10.1016/j.socscimed.2015.08.008
- Szmukler, G. (2009). “Personality disorder” and capacity to make treatment decisions. Journal of Medical Ethics, 35(10), 647–650. https://doi.org/https://doi.org/10.1136/jme.2009.030395
- Thomas, C. (2010). Are juries fair? (Ministry of Justice Research Series 1/10). Ministry of Justice. https://www.justice.gov.uk/downloads/publications/research-and-analysis/moj-research/are-juries-fair-research.pdf
- Tyrer, P., Mulder, R., Kim, Y.-R., & Crawford, M. (2019). The development of the ICD-11 classification of personality disorders: An amalgam of science, pragmatism, and politics. Annual Review of Clinical Psychology, 15, 481–502. https://doi.org/https://doi.org/10.1146/annurev-clinpsy-050718-095736
- Weiner, B. (1986). An attributional theory of motivation and emotion. Springer.
- World Health Organisation (2019). International statistical classification of diseases and related health problems (11th ed.). World Health Organisation. https://icd.who.int/