ABSTRACT
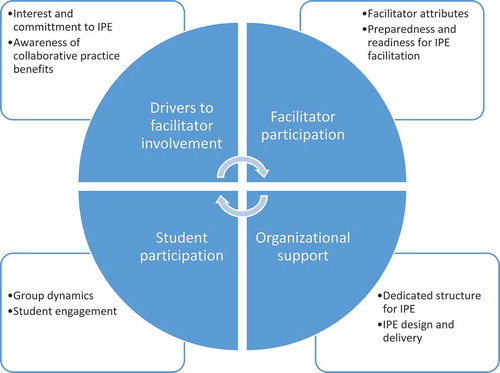
Facilitators are of paramount importance to the success of interprofessional education (IPE) activities; hence, it is crucial to explore their perspectives and experiences in delivering IPE in Qatar. Using an exploratory case study approach, semi-structured interviews were conducted, in 2018, among faculty members, who had facilitated at least one IPE activity in Qatar, from healthcare professional education programs at Qatar University Colleges of Pharmacy, Medicine, and Health Sciences, Weill Cornell Medicine in Qatar, the University of Calgary in Qatar, and the College of North Atlantic. Interviews were recorded and transcribed verbatim. Inductive thematic content analysis was implemented. Twenty-one interviews were conducted with the following professions represented: medicine (n = 6), pharmacy (n = 5), nursing (n = 4), biomedical science (n = 3), respiratory theory (n = 2) and public health (n = 1). Four main themes emerged from the interviews: drivers to facilitator involvement that included interest and commitment to IPE and awareness of collaborative practice benefits; facilitator participation which was based on facilitator attributes and preparedness and readiness for IPE facilitation; the organizational support in terms of dedicated structure for IPE and IPE design and delivery and; student participation in terms of group dynamics and student engagement. Some key recommendations include having a dedicated unit for IPE, scheduling protected time for IPE, and organizing facilitators’ training and debriefing workshops. The facilitators valued and appreciated IPE in preparing students for future collaborative practice. These findings can inform the development of quality and sustainable IPE activities in the future.
Introduction
The World Health Organization (WHO)’s “Global Strategy on Human Resources for Health: Workforce 2030” recognizes the importance of interprofessional education (IPE) and collaborative practice (CP) as part of transformative strategies to scale up health worker education to improve long-term care for older patients, and enhance both the capacity and satisfaction of healthcare workers. This is expected to lead to better team performance and the delivery of cost-effective patient-centred care (World Health Organization, Citation2016). The strategy recommends that educational institutions need to adapt their strategies to align them with transformative educational needs which calls for the promotion of IPE and CP. IPE is defined as a pedagogical strategy of which interaction among a group of healthcare students coming from two or more health professions in order to learn with, from and about each other to promote a culture of collaboration that can be translated into practice settings (Buring, Bhushan, Brazeau et al., Citation2009; CAIPE, Citation2002).
Due to the significant impact of such an educational approach on improving the quality of care, IPE has received increased attention worldwide in the past 20 years and it is well established in some western countries such as Canada, United States, United Kingdom, and Australia. Similarly, the concept of IPE is emerging in the Middle Eastern countries with an increasing number of health professional degree programs aiming to maintain high standards of education through meeting international accreditation standards (Awan et al., Citation2018; El-Awaisi et al., Citation2017; Zeeni et al., Citation2016). Many accrediting bodies of the medical and healthcare programmes require evidence of IPE incorporation into curricula, which is an important element in driving IPE forward and in expediting the healthcare faculty’s positive shift toward this educational transformation (Barker et al., Citation2005; El-Awaisi et al., Citation2016; Olenick & Allen, Citation2013; Thistlethwaite, Citation2015; Wilby et al., Citation2015).
To be most effective, it is recognized that IPE should be embedded in the early stages of undergraduate curricula (Harden, Citation2015). Early immersion enabling these students to prevent negative stereotyping, understand their professional role and valuing the role of other health professionals (Lapkin et al., Citation2012; Lawlis et al., Citation2016). However, from the perspective of program developers, IPE preparation and delivery should not be underestimated. Planning and developing an IPE activity requires an extensive amount of time and resources, reportedly requiring three times the preparation of a traditional course content delivery (Buring, Bhushan, Broeseker et al., Citation2009). In preparation for an IPE event, simply recruiting facilitators may not lead to a worthwhile IPE experience. Even experienced facilitators may not be equipped with the necessary knowledge and skills to facilitate IPE effectively (Egan-Lee, Baker, et al., Citation2011a). This could be due to a lack of exposure to IPE and IPC concepts in their training and/or in their work environment (Anderson et al., Citation2009; Buring, Bhushan, Broeseker et al., Citation2009; Hall & Zierler, Citation2015). A key milestone to the success of IPE endeavours and to ensure students receive a positive experience is the competence and confidence of the IPE facilitator (Anderson et al., Citation2011; Illingworth & Chelvanayagam, Citation2017; LeGros et al., Citation2015). A skilful interprofessional facilitator is neither merely present to observe the team nor is a team member; but should guide the team formation, promote regular reflection, and encourage the development of shared understanding and mutual trust amongst the students (LeGros et al., Citation2015). An IPE facilitator is expected to facilitate team formation, value each profession’s unique contributions, ask questions that stimulate critical thinking, draw conclusions, provide constructive feedback, and manage any potential conflicts among students (Derbyshire et al., Citation2015).
In order to produce a skilled and collaborative workforce to meet the complex needs of healthcare practices and society, IPE facilitators must be well-trained and possess the necessary knowledge, skills, and attitude for effective IPE delivery (Botma, Citation2018; Egan-Lee, Baker, et al., Citation2011a). Inadequate IPE facilitation training was identified as a weakness in a SWOC analysis exploring the four-year experiences of integrating IPE into healthcare curricula in Qatar (El-Awaisi et al., Citation2017). This is also a commonly reported weakness in the IPE landscape globally (Breitbach et al., Citation2013; Evans et al., Citation2014; Reeves et al., Citation2013; Remington et al., Citation2006). Given the importance of an interprofessional facilitator to the success of IPE delivery, it is pivotal to understand the perspectives of facilitators and to explore further their actual experiences in facilitating IPE activities (Anderson et al., Citation2011; Botma, Citation2018).
The literature presents the attributes needed by a facilitator to make IPE facilitation effective: a trained IPE facilitator, readiness for IPE facilitation, positive role modelling, and commitment to IPE concepts and values (Anderson et al., Citation2011; Derbyshire et al., Citation2015; Lindqvist et al., Citation2018). However, there has been no study in Qatar or the Middle East about IPE facilitators’ experiences in facilitation and perceptions in delivering IPE activities. It is likely that the cultural background of a facilitator may influence the interaction between the facilitator and the students, which may ultimately affect the facilitator’s effectiveness in leading an IPE activity. Understanding facilitators’ attitudes and experiences are of great significance to the implementation and sustainability of IPE as they give insights about the facilitators and barriers perceived by IPE facilitators.
Study objectives
The objectives of this exploratory case study were to: (1) explore healthcare professional facilitators’ perceptions about and experiences in delivering IPE activities in Qatar, and; (2) identify the enablers and barriers faced during the planning and implementation of IPE activities.
Methods
Study design and theoretical framework
A qualitative study design using semi-structured face-to-face interviews was deemed appropriate and applied in this study because our goal was to explore, in-depth, the experiences and perceptions of facilitators in facilitating IPE activities. This is commonly used as a method of choice in health services research when a description of experiences of healthcare professionals or patients with a specific phenomenon is required (Sandelowski, Citation2010). The symbolic interactionism theory provides the theoretical framework for this study, suggesting that facilitators’ perceptions and experiences rely on the symbolic meaning that they develop through the process of social interaction between themselves and students while facilitating the IPE activities. This theory is built on three basic tenets. The first of these tenets is that the actions taken are based on meanings generated from either past experiences or a person’s own hypothesized perception. The second tenet is that those meanings are not unified among people. The third of these tenets is that those meanings are not static and can change whether consciously or unconsciously. In other words, we interact with our surroundings based on preexisting symbolic meanings in our minds. Thus, this framework was regarded as suitable for this study as it matches the concept of IPE facilitation by nature (Crotty, Citation1998).
An exploratory single case study approach was employed. This approach is suitable in the context of the present investigation as a case study investigates “contemporary phenomenon in its real-life context, especially when the boundaries between phenomenon and context are not clearly evident” (Yin, Citation2017; Yin, Citation2003). The concept of IPE facilitation was considered as the “phenomenon” of interest, which was researched within the “defined context” of IPE in healthcare professions in Qatar, in the period between 2014 and 2018, the “defined unit”.
Study setting
IPE was formally introduced into healthcare curricula in Qatar in 2014 through the formation of the interprofessional education committee (IPEC) led by Qatar University (QU) College of Pharmacy (CPH) (A. El-Awaisi et al., Citation2017). The committee also included representatives from the other colleges within the university: College of Medicine (CMED) and College of Health Sciences (CHS): biomedical science, public health, and human nutrition. This is in addition to Weill Cornell Medicine in Qatar (WCM-Q); University of Calgary in Qatar (UC-Q) nursing school; and the College of North Atlantic (CNAQ) (dental assistant, emergency medical science, environmental health, medical radiography technology, pharmacy technician and respiratory therapy). These included representations from 14 healthcare programmes. IPEC focuses on providing support in organizing IPE activities at CPH and other health programmes in Qatar, in addition to teaching students and faculty members about IPE and interprofessional collaboration. The model followed by IPEC has been adapted from the University of British Columbia structuring the learning experience of IPE as a continuum starting with exposure, immersion, and then mastery. IPE activities are developed based on the IPE shared competency statement developed for the context of Qatar and include: interprofessional communication, role clarification, shared decision making, and patient-centred care. IPE activities are delivered across the different professional years incorporating 2–6 professions lasting 2–3 hours (El-Awaisi et al., Citation2017). Within each activity, students are divided into different interprofessional teams and are assigned one faculty facilitator.
Participants and sampling
Participants were purposively selected if they have undertaken the role of a facilitator in previous IPE activities organized by IPEC. Purposive sampling was used as it ensures representation of all professions, in addition to the selection of information-rich cases related to participants’ experiences with the IPE activities and to broaden the perspectives on the topic under investigation (Suri, Citation2011). A personalized e-mail was sent to the identified facilitators (i.e. IPEC representatives and faculty members) who fulfilled the study eligibility criteria, inviting them to participate in the study, explaining the study purpose, and providing them with an attachment of the participant’s leaflet. Series of interview schedules and locations were offered, and if they agreed to participate, the participants were asked to choose or provide their availabilities. Those who accepted to take part in the study were sent Microsoft Outlook invitations according to their availabilities.
Topic/Interview guide
The authors developed the topic guide following a thorough review of literature related to studies investigating facilitators’ experiences and perceptions of IPE activities or similar activities and based on the theoretical framework described above. The topic guide contained open-ended and neutral probing questions to avoid socially desirable responses, which is consistent with the principles of conducting qualitative studies (Gill et al., Citation2008). The topic guide was pilot tested among three members in the research team, who have previously facilitated IPE activities but were not included in the results. Piloting topic guide ensures that all interview questions are relevant and appropriate to the context, and gauges the burden of the interview (Gill et al., Citation2008). The developed topic guide comprised four major domains/areas: perceptions and experiences with IPE activities, enablers and barriers to planning IPE activities, delivering and implementing IPE activities, and recommendations to improve IPE delivery.
Data collection
Semi-structured one-to-one interviews were deemed more appropriate than focus groups due to difficulties faced with scheduling, while still providing in-depth information about participants’ perspectives (Gill et al., Citation2008). In addition, a semi-structured approach was used due to its flexibility, as it allows the interviewer to ask key questions that help address the areas to be explored and gives the freedom for the interviewer or interviewee to diverge and offer more detailed responses, in addition to elaborating information that has not been previously thought of by the research team.
A personal e-mail reminder about the interview date, time, and the location was sent to each participant one day prior to the interview. Interviews took place in quiet areas within each facilitator’s respective campus. The interviews were conducted in English. On the day of the interview, each participant was provided with a participant information sheet and an informed consent form to sign. The principal investigator (AE) led the first three interviews in the presence of SS and AA as training for the upcoming interviews. Thereafter, SS and AA independently alternated in leading the interviews. The purpose of this was to decrease the positive response bias participants may have if an IPEC member was present. SS and AA were final year pharmacy students who participated in IPE activities as students, facilitated one IPE activity to understand the process of facilitation prior to this research, and had successfully completed courses which included the design, analysis and interpretation of qualitative studies. Each interview started with a brief introduction about the study and the session, followed by the interview questions administered by the lead interviewer. The interviews were audio-recorded using a digital recorder (SONY digital voice recorder). Each interview session lasted about 45 to 60 minutes. Participants were assured of strict confidentiality and anonymity of the interviews.
As the person conducting the interview is often occupied with having the verbal face-to-face interaction with the interviewee, another team member attended the interviews to take notes. Notes were taken for several purposes, one of which is writing observations that are not evident in an audio record. Another aim for the note-taker is to write down details that the interviewee points out briefly so that the interviewer can ask for more elaboration about those.
Data analysis
The interview sessions were transcribed verbatim by two of the researchers (SS and AA) and a professional transcriber. The researchers reviewed each other’s transcripts and listened to all recordings to achieve similarity and validate the transcripts. The data were analyzed manually using thematic content analysis approach. Using inductive thematic step-by-step analysis according to Braun and Clarke (Braun & Clarke, Citation2006), two researchers (SS and AA) independently reviewed each transcript, and coded text that was considered relevant to the research questions to ensure trustworthiness of the data analysis. During this, common phrases that discussed the same idea or meaning were identified. Another team member (AE, AAW, and DR) validated the generated codes. Once all data were coded, the codes were compared and sorted into relevant themes (defined as something that has a certain level of pattern or meaning in relation to the research questions in the data) and subthemes. The identified themes were discussed by the research team (AE, AAW, and DR) and discrepancies were resolved through consensus. Finally, quotes representing the themes were selected based on agreement from all research team members.
Ethical considerations
The study protocol, consent form, and the interview guide were reviewed and approved by the Qatar University Institutional Review Board (approval number: QUST-1-CPH-2018-3). Written informed consent was obtained from each participant after having explained and ensured anonymity and confidentiality.
Results
Twenty-one interviews were conducted with each lasting approximately 45 to 60 minutes. Participant characteristics are highlighted in . Twelve participants (57%) were from Qatar University three colleges: CPH, CMED, and CHS. Just over half of the participants (n = 12, 57%) facilitated 1–3 IPE activity. The thematic analysis yielded four themes: drivers to facilitator involvement; facilitator participation; organizational support and; student participation. The themes were further subdivided into subthemes ().
Table 1. Particpant characteristic (n = 21)
Theme: drivers to facilitator involvement
Interest and commitment to IPE
Facilitators expressed a variety of motives once asked about their drive to engage in IPE activities. Responses varied from curiosity and interest to learn more about IPE, conducting research, to positive previous experiences with IPE activities.
“I didn’t know about IPE at all. And the moment they put the idea forward, that was very interesting area for me.” (Medicine-02)
Other facilitators valued the importance of IPE in preparing students to work collaboratively in healthcare teams, highlighting the negative consequences associated with working in silos.
“I am really quite committed to the concept of professional collaboration. So, I want to make sure that there are opportunities for the students to engage in discussions and share decision making.” (Nursing-02)
“If we didn’t work collaboratively, which is driven by IPE, then you would have a lot of incidents with falls, with deaths, with dementia like delirium, different things like that.” (Nursing-01)
However, some facilitators pointed out some factors that negatively affect their participation in IPE activities, such as previous exposure to negative IPE experiences, and their heavy workload, which was mentioned by all facilitators as a barrier to participate in IPE.
“Workload definitely is the main barrier. Also when you have bad experience with it, maybe you will not feel very comfortable that you want to do that again.” (Pharmacy-04)
Additionally, some facilitators suggested expanding the pool of facilitators, as this would introduce other faculty members to the IPE concept, reduce workload on existing facilitators, and overcome the issue of facilitator shortage.
“IPE activity should not be focused on selected faculty, it should be introduced to all … because some faculty are not aware of these things.” (Biomedical science-1)
“We should involve everybody. We shouldn’t limit it to people that are clinically-oriented or in the clinical section?.” (Pharmacy-03)
Several facilitators stated that they facilitated IPE activities because it was part of their course, while some were assigned by their college to participate without their consultation, indicating that they would like to be notified or consulted before being assigned as facilitators.
“I was selected by the college in order to participate in it, it was really not my interest to do that, but since it was assigned for me, I went for it”. After participating: “I loved it too much, I felt that the students really liked it and it added to their experience and knowledge.” (Biomedical science-03)
“I was asked by the coordinator to turn one of the session I was teaching to an IPE activity.” (Pharmacy-02)
Awareness of collaborative practice benefits
Facilitators expressed positive perceptions about the outcomes of IPE and its benefits. IPE activities helped both students and facilitators learn about and appreciate different professions roles and viewpoints. Facilitators indicated that students were happy to interact with other students, which helps them set basis for future collaboration.
“I know that IPE is quite an essential concept to work on. Especially in this time and age because they’ll work in the same environment eventually, so they need to be educated on basic issues together.” (Medicine-01)
“It was the first time for them to sit with these different specialties and see how they collaborate together to keep the patient safe and to treat the patient, so it was completely new experience and they enjoyed it.” (Biomedical science-02)
“I think the nicest thing about it, is sharing with other professions and learning, sharing their ideas … our students achieve their objectives and then we get to kind of collaborate and they learn from each other which is fun as well … and then in the future maybe you might be working together in the same institution and you will be a familiar face.” (Respiratory Therapy- 02)
Theme: Student participation
Group dynamics
Facilitators described a range of factors that enhance group dynamics in the activities such as group distributions and the number of students per group. Recommendations were to have less students per group, ensure a good mix of professions and designing activities to include two to three professions only as having more can distract the conversation.
“Yeah I think eight. Six to ten (students per group) would be feasible.” (Pharmacy-05)
Also, students’ personalities were viewed as important determinants to group dynamics within the teams, as shy students were not interactive during the sessions, whereas students with outgoing personalities dominated the discussions.
“Depending on their personality, some of the students were very shy, they don’t want to participate at all … Even you feel that you are pulling from them the words.” (Biomedical science-03)
“The dominant people try to continue to be dominant, as I told you before, the stars continue to be stars in the group and in the presentation.” (Medicine-06)
Student engagement
Students’ knowledge and skills were a commonly discussed aspect that enables students to be interactive during IPE activities, as students with solid background knowledge about the topic of the IPE activity were more engaged. Additionally, skills such as teamwork skills, presentation, and communication skills were also attributed to higher level of student engagement.
“So, if they know the subject itself, they will participate more, and the interaction will be more. But sometimes they have a subject where they don’t have a background about this … ” (Medicine-03)
On the contrary, resistance to participation was evident due to several factors, including: language, information barrier, gender barrier, and lack of interest, which was mainly reflected by poor attendance. As for gender barrier, opposing responses were obtained, as some facilitators observed a gender barrier within their groups, and some did not.
“I tried to engage everybody, but they were couple of students who were very quiet … and I tried to make them feel more comfortable, and when she started talking, she was very good. She knew how to express herself, but apparently, when she first saw me, you know very old guy, not an Arab, she probably felt intimidated, I don’t know.” (Medicine-04)
“Some students who come from health sciences particularly female candidate, I felt that they were not really contributing much to the discussion because initially, it was a mixed activity … other candidates were not particularly contributing because the activities were running in English and they felt it’s difficult to communicate in English language.” (Medicine-02)
We had some medical male students and they were very cooperative with the female students … so there’s no barrier in communicating, I didn’t see any difficulty.” (Biomedical Science-01)
Other reasons for student resistance are IPE activities were optional for some professions particularly medical students.
“Our student don’t believe it is important for them to attend as IPE is not incorporated in our curriculum, so that’s why most of them they are not attending it as its optional … so that’s why in our curriculum meeting we are trying to put the IPE activity as a major component in our curriculum.” (Medicine-03)
“I was led to believe that their group [medical students] were informed that it was an optional activity and such why no one showed up. Hardly anyone showed up and those that did didn’t do any preparation.” (Pharmacy-02)
Although student awareness of other professions was evident in the activities, some facilitators noticed non-verbalized hierarchy within the teams, where medical students dominated discussions, indicating that physicians are still perceived as leaders in practice. Some facilitators attributed having broader knowledge to more participation.
“I think physicians feel like they have to take charge as well because they are probably trained they are going to be a leader … Whereas maybe my students only could get a couple of things here, right … so I think because the MD and the nurses they have a broader range of everything so they probably take that. Paramedic students are also very vocal again they have that broad range. They can contribute to almost every at least part of the scenario from their perspective mostly.” (Respiratory therapy-02)
“I noticed nursing would step back a bit because there’s someone who’s a doctor in a physician’s medical student might be talking and you could see that … in the back of their mind I think is still instilled and whether it’s part of the hidden curriculum of what they see around and how they feel about it.” (Medicine-05)
Furthermore, facilitators proposed strategies to improve student engagement, such as choosing topics that students are interested in, IPE competitions or simulation-based IPE activities. Many suggested assigning grades for the activity in the form of assessment.
“There has to be some evaluation, and some grades assigned to these activities to motivate students to benefit more from this learning activity.” (Biomedical science-1)
Also, facilitators indicated that the IPE technique and the type of icebreaker used, impacts the level of student engagement, noting that students enjoy more competitive activities.
“I find that the icebreaker activities are key. Last year, we had an intro to IPE, and we did an icebreaker activity that was really active and competitive. It just set the tone for the rest of the activity. Everyone was loud and chatty, and in a good mood, and then I’ve been to other IPEs where the icebreaker was, Oh, introduce yourself, and tell me where you’re from, and your high school. And then that sets the tone. It’s a bit dull and I find that the rest of the activity kind of stays on that tone.” (Respiratory therapy-01)
Theme: facilitator participation
Two subthemes emerged under the theme of active facilitator participation: facilitator’s attributes and their preparedness and readiness for IPE facilitation.
Facilitator attributes
Facilitators proposed a wide range of attributes that they thought were cardinal to being a successful facilitator. They believed that the attributes they identified would contribute to making the IPE event a successful one. Some of these traits were being open-minded, motivated, flexible, neutral, diplomatic, good listener, and multi-tasking.
“S/he should be a good listener, to listen … active listening … not just hearing. I think this is important” (Medicine-06)
“They should be knowledgeable and flexible and to have the passion … should have level of diplomacy and they should be multi-skilled, multi-tasked so they can manage different views, and they should be active.” (Biomedical science-02)
However, some facilitators felt the personality of some of the facilitators could be a barrier:
“There are facilitators that come to facilitate and then when they have the stage . they want to be the stars, they want to talk. even to impose their ideas on the students and to make the students even write their ideas. So they use the student to show-off.” (Medicine-06)
Preparedness and readiness for IPE facilitation
Previous exposure to an IPE event, having clinical experience, attending an orientation session and topic knowledge were all factors that contributed to making facilitators perceive themselves as being prepared to facilitate IPE events and guide event.
“I think I did better with the second one, because I was more prepared. The first time I did it, I was totally worried. It took me a while to understand what we are supposed to do.” (Medicine-4)
“We had an idea as to what is going to be talked about and what we can anticipate the students to do. I think … the preparation in going into that IPE event helped me a lot because it was my first time to do it.” (Nursing-3)
“Sometimes when you have good experience with it [an IPE activity], it is rewarding so you want to do it again” (Pharmacy-04)
In addition, having work-related obstacles and a sense of hierarchy were factors that prevented facilitators from perceiving themselves as being prepared to take part in the IPE activity. Furthermore, some facilitator were not aware of the role of some of the participating students and recommended the need for role clarification even among facilitators.
“I don’t know what they [public health students] are studying.” (Respiratory therapy-2)
Theme: Organizational support
This theme revolved around having commitment from the IPE committee and the design of events’ delivery.
Dedicated structure for IPE
Many participants perceived the dedicated committee for IPE in Qatar (i.e. IPEC) as an enterprise that warrants appreciation. Facilitators applauded the work achieved by the IPEC to ensure successful delivery of the IPE program. Thus, they regarded having such committee as an enabler for IPE implementation.
“If anything surprises me, it is to find people who can actually be committed to something like this out of their own agenda per say, or out of their own portfolio.” (Pharmacy-03)
The IPE program in Qatar is run by committee and not a dedicated unit or centre. Therefore, all needed resources are often coordinated by the host of the IPE event. This can burden the organizers as the transportation, catering, and venue preparation require a budget that is allocated to them.
“It takes resources, money, budget, everything. It is a lot of work.” (Pharmacy-04)
“Our university rents a bus. So that all of our students, unless they decide to drive over, we have a bus that takes us to where we need to go.” (Nursing-03)
IPE design and delivery
Facilitators were able to identify a wide range of aspects regarding the design and delivery of the IPE events. Some of these aspects relate to pre-preparation, logistics, and internal college coordination conflicts. Since different colleges have different academic systems and different calendars, having a convenient time and place, for either preparations or for the activity itself, are two major contributors to facilitators’ participation in IPE events. Therefore, scheduling a common time for all becomes an obstacle. An alternative approach of having remote preparations was brought up by multiple facilitators.
“I don’t know if there is one place where we could have like a common like OneDrive or Google Drive where we put everything up and they can send a notice when there is a change.” (Pharmacy-05)
“My suggestion is to have each month one day dedicated for IPE from all institutions. I mean this would be the ideal way to do it.” (Pharmacy-01)
“Barrier? Besides scheduling? Trying … well it is still scheduling. Trying to find like a time for it that works for everyone.” (Nursing-03)
Logistics associated with the event were identified by facilitators as a factor contributing to the event’s success. When many professions are present in the same event, the large number of students present at the same avenue compromises the quality of IPE delivery. As described by facilitators, at one event, the open area and the background noise made it difficult for the interaction to go smoothly with students. Conversely, in another event, the space was tight, and students could barely move their chairs.
“We were in a very small classroom; we were all put there very tight spaced. That was not so good.” (Nursing-02)
Another highlight that was made by facilitators was the presence of internal conflicts during the planning of the activity. Therefore, some of them made suggestion to eliminate such future conflicts.
“Sometimes there can be like a little bit of miscommunication … Who will do what? [.] Who will inform whom?.” (Biomedical science −1)
One of the suggested recommendations is to have an IPE matrix for tasks:
“In our department, we got what we call a matrix for the tasks. These are the roles and responsibilities for the instructor and these are the roles and responsibilities of the IPE committee members.” (Public Health-01)
Moreover, participants had suggestions that they felt were important to improve their participation and delivery of IPE activities. One suggestion was to design and implement a facilitator development strategy, where facilitators attend training workshops that focus on IPE concepts and effective facilitation before being involved in IPE activities.
“I think probably leadership, leading a team. Also, communication skills, how to effectively communicate without … and empowering the students to speak. What other things they need? What is IPE, a lot of facilitators don’t know what IPE is? Most facilitators are so quick at only trying to promote their own role. When really that is not your role as a facilitator. So that is one of the things that needs to be learned.” (Nursing-02)
“The skills! How to facilitate, how to get people to talk, why is it important. For some facilitators, they don’t know why is this important. This needs to be highlighted in training sessions” (Pharmacy-01)
Additionally, it was suggested to provide incentives for facilitators participation by providing continuing professional development (CPD) points through Qatar Council for Healthcare Practitioners. Furthermore, debriefing and feedback, following the IPE activities, with facilitators were recommended. Different participants pointed out that a debriefing session is a chance to reflect on what went well during the event and what didn’t. That way, continuous improvement to both facilitators and organizers is expected where facilitators improve the things that didn’t go very well in future events. Regarding the mode of delivery of debriefing, preferences varied among facilitators. While some of them preferred to have a face-to-face debriefing session by the end of the event, others thought that an e-mail sent later during the day would be sufficient. Those who believe that an e-mail is a better way to debrief find it difficult to stay after long three hours as they have other commitments.
“I hope we could have better more meetings afterwards, more communication to see how to improve things to put them better. I don’t recall we had such thing, but I think it will come up with time that you always you have to follow up and try to make things become happening better.” (Medicine-01).
Discussion
This study is the first study in Qatar which provides qualitative focused insights into the experiences and perceptions of healthcare facilitators in delivering IPE activities in Qatar. Facilitators are paramount to the success of an IPE event regardless of the learning theories, active learning techniques, the complexity of the simulation, or the timing in the students’ training. With the intention of promoting collaborative practice, this study identified key perceptions of facilitators based on their experiences in the IPE program including both enablers and barriers to positive IPE experiences: facilitator involvement, student and facilitator participation during the event and organization support, along with recommendations to improve the delivery and sustainability of IPE.
Developing and refining the design and delivery of individual IPE sessions as part of an IPE program requires significant time and effort. Previous studies have noted that a lack of leadership and the need for prioritization of IPE in the curriculum were important barriers to delivering positive IPE experiences (Bennett et al., Citation2011; Lindqvist et al., Citation2018). Facilitators deemed important that organizational support for an IPE program allows a focused team to manage logistics, provide dedicated leadership, and focused change management. Facilitators acknowledged that unclear faculty expectations in the development or delivery of IPE events, and lack of facilitator recognition were barriers to positive IPE experiences and hindered their enthusiasm to engage in future IPE activities. They also noted their lack of experience, understanding of core IPE principles, and unsureness as factors to adequately facilitate the learning needs of all included professions stating that facilitator development sessions would be able to meet their needs. These findings are consistent with what has been reported in the published literature (Botma, Citation2018; Egan-Lee, Baker, et al., Citation2011b; Milot et al., Citation2017). The IPE program offered in the context of this study has a dedicated committee to assist in these tasks. However, the facilitators have identified key opportunities for their own professional development with a necessity for conceptual interprofessional clarity (Egan-Lee, Baker, et al., Citation2011b; Evans et al., Citation2016; Ruiz et al., Citation2013; West et al., Citation2016). The development of core facilitation skills are considered as fundamental in facilitator development initiatives (Sullivan et al., Citation2009).
Before an IPE event takes place, an adequate number of facilitators must volunteer or be volunteered. This was reported in other studies as an important challenge to implement and sustain IPE (Brashers et al., Citation2012; Lapkin et al., Citation2012; Lee et al., Citation2012). Facilitators identified that their own interest and commitments to promoting professional collaboration were the main drivers to getting involved. However, the reasons for facilitators not being as motivated to participate included a heavy workload and negative previous IPE experiences. Having numerous professions involved in an IPE program were identified as both an enabler for a positive experience, but also a barrier to positive experiences. Developing IPE activities and cases including 5–8 professions who have a direct, meaningful impact on a scenario is difficult to achieve. A study of Norwegian and English IPE educators stated that a successful event depends on clinically relevant scenarios supported by trained facilitators (Lindqvist et al., Citation2018). The issue of realism is pivotal to successfully deliver IPE activities (Freeth et al., Citation2008; Reeves et al., Citation2002), and it constitutes an essential component of Knowles’ adult learning principles (Knowles, Citation1980). Additionally, other exploratory case studies of healthcare students’ experiences with IPE activities revealed that students were not satisfied with the artificial nature of the activities, which curtail their value, and perceive IPE more positively when academic knowledge and professional practice connect (Oandasan & Reeves, Citation2005; Osman, Citation2017; Rosenfield et al., Citation2011), further supporting the participants views regarding this matter. This could be attributed to previous IPE sessions, where participants highlighted that unrealistic scenarios were used for the sake of incorporating all professions in one case. Thus, efforts should be made to create meaningful and relevant interprofessional experiences for students through designing realistic cases and having a good mix of professions.
As the IPE event is underway, facilitators acknowledged two major factors which contributed to positive experiences – the facilitators’ participation and the students’ participation. From the facilitator perspective, it has been previously identified that facilitators need to be prepared for the day by having a commitment to be fully engaged and to have an awareness of learning context and IPE principles (Derbyshire et al., Citation2015). Our results were similar to this notion, but also noted that facilitators should be open-minded, flexible, diplomatic and engage all professions equally. The strategy of facilitator involvement was not explicitly mentioned by participants in this study, whereas another study found that facilitator-driven and facilitator-controlled were the most frequent strategies employed compared to student-driven scenario management (Ruiz et al., Citation2013). This also reflects a key opportunity to train facilitators to optimize student participation and reduce small group didactic IPE experiences.
From the student perspective, facilitators noted that too large of groups with imbalanced professional representation caused disruption of group dynamics. Similarly, engaging the students in the activity was trouble-free if the students had adequate knowledge of the topic but presented difficulties as healthcare profession hierarchy was evident. All IPE events in our program were delivered in English and facilitators found that those students with limited English were not as actively engaged as those confident in their English language skills. Additionally, facilitators noted that some students may leave early from the activity. This could be the fact that outside of an attendance mark, there may be no assignments or post-activity assessment that requires the students to be physically present and mentally engaged. Finally, facilitators did not find that having mixed gender groups had a major impact on the participation of students who come from gender-segregated programs (e.g., the pharmacy and health sciences programs in Qatar). Within the cultural context in the Middle East, gender segregation exists in some of the universities in the Gulf region, including Qatar University, and hence may impact student engagement in the activity. Acknowledging these cultural differences must be taken into considerations when facilitating IPE activities (Badry & Willoughby, Citation2015; El-Awaisi et al., Citation2018). This has been previously described in a student perspective’s study which noted that only a minority of students enrolled in unisex program found having male students in their groups as culturally challenging (El-Awaisi et al., Citation2018). Students upon graduation are expected to interact with all healthcare professionals and patients, regardless of their gender.
Hierarchy within the students was perceived to hinder their participation, with medical students leading or dominating the discussions (Steinert, Citation2005). Not only this, but the study directed the spotlight on having hierarchy even within facilitator-to-facilitator interaction. This finding could be attributed to the inherent professional tribalism (Smith et al., Citation2009) where faculty members tend to boost the students’ ego. Interestingly, several studies outlined that attitudes and stereotypes held by faculty members are barriers to IPE (Aston et al., Citation2012; Lee et al., Citation2012; Steinert, Citation2005). Also, favouring students of their profession can undermine the learning process for other professions (Ho et al., Citation2008). These imbalances of power between different healthcare students could be transferred into practice if not met with constructive interventions. A few interventions to overcome these attitudes were explored. For example, identification of attitudes and stereotypes by facilitators themselves (Aston et al., Citation2012), and faculty development strategies before implementing IPE was successful in emphasizing the importance of IPE in teamwork and collaboration (Steinert, Citation2005). Thus, such interventions should be executed among healthcare facilitators in Qatar.
The implications of this study suggest that facilitators have positive experiences with IPE events if they have an internal motivation and commitment to IPE, are prepared for IPE events through orientations and their workload of IPE events being valued and accounted for. These can be achieved with the support of a dedicated organizational structure for IPE, having a local IPE champion, and having clear expectations of an event (Gilbert, Citation2005; Oandasan & Reeves, Citation2005). A proposed approach would be to have a dedicated IPE specialist to assist in the implementation and execution of IPE initiatives. This position is ideally situated to assist in facilitator development to ensure they have the required skills needed to facilitate IPE activities through continuous faculty development workshops.
Limitations
This study is not without limitations. A few facilitators from other disciplines including nutrition, medial radiographers, and paramedics were not able to be interviewed. Member checking of transcripts to ensure the correct understanding of the participants which may impact the credibility of the results were not performed. However, the credibility is maximized as saturation was reached. Participants were assumed to be fluent in English, although English was not the first language of many interviewees, which could have impeded them from expressing their thoughts and opinions. To minimize this, questions were asked more than once in different ways to ensure data consistency. Despite these limitations, this study was the first in Qatar to explore facilitators’ perceptions about delivering IPE activities, and it provided some insights into the enablers and challenges faced with regards to several aspects of IPE implementation from the context of developing countries and multi-cultural pluralistic environment.
Future research should focus on direct observations (e.g., video recordings) of both students and facilitators in an IPE activity as this would generate deeper insight into the actual facilitation process and key issues observed such as gender disparity, dominant personalities, and dynamic between disciplines. Mixed method approaches of questionnaires and focus groups could be employed to elicit students’ perceptions and experiences of IPE activities. This could also be used to assess facilitator competencies in Qatar and explore their insights into how the delivery of IPE could be improved. Besides, it is recommended that the upcoming studies should explore the effectiveness and compare the different strategies of IPE delivery with respect to the quality of outcomes achieved at the end of IPE activities. Finally, though symbolic interactionism theory was going to be initially used as the theoretical framework for the study, it becomes apparent during the analysis that many facilitators were new to the facilitation process. As these facilitators are still in the process of acquiring knowledge, or symbols, this precluded the thorough application of this theory. However, symbolic interactionism theory could be used in the future to identify facilitators experiences further as facilitators become more acquainted with IPE concepts.
Conclusion
In conclusion, the study explored the perceptions and experiences of healthcare facilitators in the delivery of IPE activities in terms of enablers, challenges faced, and how these could be improved during the development, planning, and implementation of IPE events. The main findings that emerged were that facilitators value IPE activities in preparing students for collaborative practice, and that facilitators should display a wide range of attributes to deliver IPE effectively. Participants regarded previous exposure to IPE, students’ and facilitators’ knowledge and skills, structural organization, planning, and preparation as enablers to the implementation of IPE. Whereas, hierarchy within students and facilitators, logistics, and limited resources were identified as implementation challenges. Some key recommendations include having a dedicated unit for IPE, scheduling protected time for IPE amongst all academic healthcare institutions, and organizing facilitators’ training and debriefing workshops along with the provision of accredited CPD points as an incentive for participating. These findings can inform the development of quality IPE and help in providing the best quality education experience.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Funding
Notes on contributors
Alla El-Awaisi
Dr Alla El-Awaisi is currently the Assistant Dean for Student Affairs at College of Pharmacy in Qatar University and is the Chair of the Interprofessional Education program at QU Health. Dr El-Awaisi received her Master of Pharmacy degree from Strathclyde University in Glasgow (UK), MSc in Prescribing Science and PhD in Interprofessional Education and Collaborative Practice from the Robert Gordon University (UK). Her research expertise lies in the area of interprofessional education and collaborative practice, patient safety, medical and pharmacy education.
Saba Sheikh Ali
Dr. Saba Sheikh Ali is an internal medicine Clinical Pharmacist at Hamad Medical Corporation. She received her Bachelor of Pharmacy from Qatar University (QU) in 2018. She then completed her Doctor of pharmacy (PharmD) degree in 2019 from QU. Saba’s Research interests include internal medicine and pharmacy practice.
Aya Abu Nada
Ms. Aya Abu Nada is an inpatient pharmacist at Sidra medicine for obstetrics and pediatrics. Aya is a member of the code blue champion multidisciplinary team at the hospital responding to emergencies. She is a certified provider of pediatric advanced life support by the American Heart Association and the American Academy for Pediatrics.
Daniel Rainkie
Dr. Daniel Rainkie is a clinical lecturer in the College of Pharmacy at Qatar University and is a clinical pharmacy specialist with the Advanced Heart Failure clinic at Heart Hospital, Hamad Medical Corporation. His interprofessional work stems from a passion to bring together teams to provide safe and effective patient centered care. Dr Rainkie is the chair of the assessment committee, evidence-base medicine committee and coordinator for the undergraduate evidence-based medicine series.
Ahmed Awaisu
Dr Ahmed Awaisu is the Head of Department of Clinical Pharmacy and Practice in the College of Pharmacy at Qatar University. His research centers around optimization of medicines use, outcome-based research, pharmacoepidemiology, and pharmacy education including interprofessional education and performance-based assessment.
References
- Anderson, E. S., Cox, D., & Thorpe, L. N. (2009). Preparation of educators involved in interprofessional education. Journal of Interprofessional Care 23(4), 81–94. England. https://doi.org/10.1080/13561820802565106
- Anderson, E. S., Thorpe, L. N., & Hammick, M. (2011). Interprofessional staff development: Changing attitudes and winning hearts and minds. Journal of Interprofessional Care, 25(1), 11–17. https://doi.org/10.3109/13561821003721311
- Aston, S. J., Rheault, W., Arenson, C., Tappert, S. K., Stoecker, J., Orzoff, J., … Mackintosh, S. (2012). Interprofessional education: A review and analysis of programs from three academic health centers. Academic Medicine : Journal of the Association of American Medical Colleges, 87(7), 949–955. https://doi.org/10.1097/ACM.0b013e3182583374
- Awan, A. A., Awan, Z. A., Alshawwa, L., Tekian, A., Park, Y. S., & Altyar, A. (2018). Integrating an interprofessional education initiative: Evidence from King Abdulaziz University. Medical Teacher, 40(sup1), S15–s21. https://doi.org/10.1080/0142159x.2018.1464651
- Badry, F., & Willoughby, J. (2015). Higher education revolutions in the Gulf: Globalization and institutional viability (Vol. 24). Routledge.
- Barker, K. K., Bosco, C., & Oandasan, I. F. (2005). Factors in implementing interprofessional education and collaborative practice initiatives: Findings from key informant interviews. Journal of Interprofessional Care, 19 (Suppl 1), 166–176. England. https://doi.org/10.1080/13561820500082974
- Bennett, P. N., Gum, L., Lindeman, I., Lawn, S., McAllister, S., Richards, J., … Ward, H. (2011). Faculty perceptions of interprofessional education. Nurse Education Today, 31(6), 571–576. https://doi.org/10.1016/j.nedt.2010.09.008
- Botma, Y. (2018). Consensus on interprofessional facilitator capabilities. Journal of Interprofessional Care, 33(3), 277–279. https://doi.org/10.1080/13561820.2018.1544546
- Brashers, V., Peterson, C., Tullmann, D., & Schmitt, M. (2012). The University of Virginia interprofessional education initiative: An approach to integrating competencies into medical and nursing education. Journal of Interprofessional Care, 26(1), 73–75. https://doi.org/10.3109/13561820.2011.636846
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Breitbach, A. P., Sargeant, D. M., Gettemeier, P. R., Ruebling, I., Carlson, J., Eliot, K., … Gockel-Blessing, E. A. (2013). From buy-in to integration: Melding an interprofessional initiative into academic programs in the health professions. Journal of Allied Health, 42(3), e67–73. https://pubmed.ncbi.nlm.nih.gov/24013253/
- Buring, S. M., Bhushan, A., Brazeau, G., Conway, S., Hansen, L., & Westberg, S. (2009). Keys to successful implementation of interprofessional education: Learning location, faculty development, and curricular themes. American Journal of Pharmaceutical Education, 73(4), 60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2720356/
- Buring, S. M., Bhushan, A., Broeseker, A., Conway, S., Duncan-Hewitt, W., & Hansen, L. (2009). Interprofessional education: Definitions, student competencies, and guidelines for implementation. American Journal of Pharmaceutical Education, 73(4), 59. https://doi.org/10.5688/aj730459
- CAIPE. (2002). Interprofessional education – A definition. Centre for the Advancement of Interprofessional Education. Retrieved from http://www.caipe.org.uk/resources/
- Crotty, A. (1998). The foundations of social research: Meaning and perspective in the research: Meaning and perspective in the research process. Sage.
- Derbyshire, J. A., Machin, A. I., & Crozier, S. (2015). Facilitating classroom based interprofessional learning: A grounded theory study of university educators’ perceptions of their role adequacy as facilitators. Nurse Education Today, 35(1), 50–56. https://doi.org/10.1016/j.nedt.2014.05.001
- Egan-Lee, E., Baker, L., Tobin, S., Hollenberg, E., Dematteo, D., & Reeves, S. (2011a). Neophyte facilitator experiences of interprofessional education: Implications for faculty development. Journal of Interprofessional Care, 25(5), 333–338. https://doi.org/10.3109/13561820.2011.562331
- Egan-Lee, E., Baker, L., Tobin, S., Hollenberg, E., Dematteo, D., & Reeves, S. (2011b). Neophyte facilitator experiences of interprofessional education: Implications for faculty development. Journal of Interprofessional Care, 25(5), 333–338. https://doi.org/10.3109/13561820.2011.562331
- El-Awaisi, A., Hajj, S. E., Joseph, M., & Diack, L. (2016). Interprofessional education in the Arabic-speaking Middle East: Perspectives of pharmacy academics. Journal of Interprofessional Care, 30(6), 769–776.. https://doi.org/10.1080/13561820.2016.1218830
- El-Awaisi, A., Hajj, S. E., Joseph, M., & Diack, L. (2018). Perspectives of pharmacy students in Qatar toward interprofessional education and collaborative practice: A mixed methods study. Journal of Interprofessional Care, 32(6), 674–688. https://doi.org/10.1080/13561820.2018.1498466
- El-Awaisi, A., Wilby, K. J., Wilbur, K., El Hajj, M. S., Awaisu, A., & Paravattil, B. (2017). A Middle Eastern journey of integrating Interprofessional Education into the healthcare curriculum: A SWOC analysis. BMC Medical Education, 17(1), 15. https://doi.org/10.1186/s12909-016-0852-5
- Evans, S., Knight, T., Sonderlund, A., & Tooley, G. (2014). Facilitators’ experience of delivering asynchronous and synchronous online interprofessional education. Medical Teacher, 36(12), 1051–1056. https://doi.org/10.3109/0142159x.2014.918254
- Evans, S., Shaw, N., Ward, C., & Hayley, A. (2016). “Refreshed … reinforced … reflective”: A qualitative exploration of interprofessional education facilitators’ own interprofessional learning and collaborative practice. Journal of Interprofessional Care, 30(6), 702–709. https://doi.org/10.1080/13561820.2016.1223025
- Freeth, D. H. M., Reeves, S., Koppel, I., & Barr, H. (2008). Effective interprofessional education: development, delivery, and evaluation. John Wiley & Sons.
- Gilbert, J. H. V. (2005). Interprofessional learning and higher education structural barriers. Journal of Interprofessional Care, 19(sup1), 87–106. https://doi.org/10.1080/13561820500067132
- Gill, P., Stewart, K., Treasure, E., & Chadwick, B. (2008). Methods of data collection in qualitative research: Interviews and focus groups. British Dental Journal, 204, 291–295. https://doi.org/10.1038/bdj.2008.192
- Hall, L. W., & Zierler, B. K. (2015). Interprofessional Education and Practice Guide No. 1: Developing faculty to effectively facilitate interprofessional education. Journal of Interprofessional Care, 29(1), 3–7. https://doi.org/10.3109/13561820.2014.937483
- Harden, R. M. (2015). Interprofessional education: The magical mystery tour now less of a mystery. Anatomical Sciences Education, 8(4), 291–295. https://doi.org/10.1002/ase.1552
- Ho, K., Jarvis-Selinger, S., Borduas, F., Frank, B., Hall, P., Handfield-Jones, R., … Rouleau, M. (2008). Making interprofessional education work: The strategic roles of the academy. Academic Medicine : Journal of the Association of American Medical Colleges, 83(10), 934–940. https://doi.org/10.1097/ACM.0b013e3181850a75
- Illingworth, P., & Chelvanayagam, S. (2017). The benefits of interprofessional education 10 years on. The British Journal of Nursing, 26(14), 813–818. https://doi.org/10.12968/bjon.2017.26.14.813
- Knowles, M. (1980). The modern practice of adult education – From pedagogy to androgogy. Follet Publishing.
- Lapkin, S., Levett-Jones, T., & Gilligan, C. (2012). A cross-sectional survey examining the extent to which interprofessional education is used to teach nursing, pharmacy and medical students in Australian and New Zealand universities. Journal of Interprofessional Care, 26(5), 390–396. https://doi.org/10.3109/13561820.2012.690009
- Lawlis, T., Wicks, A., Jamieson, M., Haughey, A., & Grealish, L. (2016). Interprofessional education in practice: Evaluation of a work integrated aged care program. Nurse Education in Practice, 17, 161–166. https://doi.org/10.1016/j.nepr.2015.11.010
- Lee, B., Celletti, F., Makino, T., Matsui, H., & Watanabe, H. (2012). Attitudes of medical school deans toward interprofessional education in Western Pacific Region countries. Journal of Interprofessional Care, 26(6), 479–483. https://doi.org/10.3109/13561820.2012.706336
- LeGros, T. A., Amerongen, H. M., Cooley, J. H., & Schloss, E. P. (2015). Using learning theory, interprofessional facilitation competencies, and behavioral indicators to evaluate facilitator training. Journal of Interprofessional Care, 29(6), 596–602. https://doi.org/10.3109/13561820.2015.1040874
- Lindqvist, S., Vasset, F., Iversen, H. P., Hofseth Almås, S., Willumsen, E., & Ødegård, A. (2018). University teachers’ views of interprofessional learning and their role in achieving outcomes - a qualitative study. Journal of Interprofessional Care, 33(2), 190–199. https://doi.org/10.1080/13561820.2018.1534809
- Milot, E., Museux, A. C., & Careau, E. (2017). Facilitator training program: The Universite Laval Interprofessional Initiative. Social Work in Health Care, 56(3), 202–214. https://doi.org/10.1080/00981389.2016.1265630
- Oandasan, I., & Reeves, S. (2005). Key elements for interprofessional education. Part 1: The learner, the educator and the learning context. Journal of Interprofessional Care, 19(sup1), 21–38. https://doi.org/10.1080/13561820500083550
- Olenick, M., & Allen, L. R. (2013). Faculty intent to engage in interprofessional education. Journal of Multidisciplinary Healthcare, 6, 149–161. https://doi.org/10.2147/JMDH.S38499
- Osman, A. (2017). What makes medical students receptive to interprofessional education? Findings from an exploratory case study. Journal of Interprofessional Care, 31(5), 673–676. https://doi.org/10.1080/13561820.2017.1340876
- Reeves, S., Freeth, D., McCrorie, P., & Perry, D. (2002). ‘It teaches you what to expect in future … ‘: Interprofessional learning on a training ward for medical, nursing, occupational therapy and physiotherapy students. Medical Education, 36(4), 337–344. DOI: 10.1046/j.1365-2923.2002.01169.x
- Reeves, S., Perrier, L., Goldman, J., Freeth, D., & Zwarenstein, M. (2013). Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Systematic Reviews, 3, Cd002213. https://doi.org/10.1002/14651858.CD002213.pub3
- Remington, T. L., Foulk, M. A., & Williams, B. C. (2006). Evaluation of evidence for interprofessional education. American Journal of Pharmaceutical Education, 70(3), 66. https://pubmed.ncbi.nlm.nih.gov/17136186/
- Rosenfield, D., Oandasan, I., & Reeves, S. (2011). Perceptions versus reality: A qualitative study of students’ expectations and experiences of interprofessional education. Search Results, 45(5), 471–477. https://doi.org/10.1111/j.1365-2923.2010.03883.x
- Ruiz, M. G., Ezer, H., & Purden, M. (2013). Exploring the nature of facilitating interprofessional learning: Findings from an exploratory study. Journal of Interprofessional Care, 27(6), 489–495. https://doi.org/10.3109/13561820.2013.811640
- Sandelowski, M. (2010). What’s in a name? Qualitative description revisited. Research in Nursing & Health, 33(1), 77–84. https://doi.org/10.1002/nur.20362
- Smith, K. M., Scott, D. R., Barner, J. C., Dehart, R. M., Scott, J. D., & Martin, S. J. (2009). Interprofessional education in six US colleges of pharmacy. American Journal of Pharmaceutical Education, 73(4), 61. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2720357/
- Steinert, Y. (2005). Learning together to teach together: Interprofessional education and faculty development. Journal of Interprofessional Care, 19(Suppl 1), 60–75. https://doi.org/10.1080/13561820500081778
- Sullivan, C. A. L. C. R. L., Cruess, S. R., & Steinert, Y. (2009). Teaching medical professionalism. Cambridge Univ Press.
- Suri, H. (2011). Purposeful sampling in qualitative research synthesis (Vol. 11).
- Thistlethwaite, J. E. (2015). Interprofessional education: Implications and development for medical education. Educación Médica, 16(1), 68–73. https://doi.org/10.1016/j.edumed.2015.04.007
- West, C., Graham, L., Palmer, R. T., Miller, M. F., Thayer, E. K., Stuber, M. L., … Carney, P. A. (2016). Implementation of interprofessional education (IPE) in 16 U.S. medical schools: Common practices, barriers and facilitators. Journal of Interprofessional Education & Practice (Online), 4, 41–49. https://doi.org/10.1016/j.xjep.2016.05.002
- Wilby, K. J., Al-Abdi, T., Hassan, A., Brown, M. A., Paravattil, B., & Khalifa, S. I. (2015). Attitudes of pharmacy and nutrition students towards team-based care after first exposure to interprofessional education in Qatar. Journal of Interprofessional Care, 29(1), 82–84. https://doi.org/10.3109/13561820.2014.933949
- World Health Organization. (2016). Global strategy on human resources for health: Workforce 2030.
- Yin, R. (2003). Case study research: Design and methods (2 ed.). SAGE.
- Yin, R. K. (2017). Case study research and applications:. Design and methods: Sage publications.
- Zeeni, N., Zeenny, R., Hasbini-Danawi, T., Asmar, N., Bassil, M., Nasser, S., … Hoffart, N. (2016). Student perceptions towards interprofessional education: Findings from a longitudinal study based in a Middle Eastern university. Journal of Interprofessional Care, 30(2), 165–174. https://doi.org/10.3109/13561820.2015.1117060