ABSTRACT
Poor communication within healthcare teams occurs commonly, contributing to inefficiency, medical errors, conflict, and other adverse outcomes. Interprofessional bedside rounds (IBR) are a promising model that brings two or more health professions together with patients and families as part of a consistent, team-based routine to share information and collaboratively arrive at a daily plan of care. The purpose of this systematic scoping review was to investigate the breadth and quality of IBR literature to identify and describe gaps and opportunities for future research. We followed an adapted Arksey and O’Malley Framework and PRISMA scoping review guidelines. PubMed, CINAHL, PsycINFO, and Embase were systematically searched for key IBR words and concepts through June 2020. Seventy-nine articles met inclusion criteria and underwent data abstraction. Study quality was assessed using the Mixed Methods Assessment Tool. Publications in this field have increased since 2014, and the majority of studies reported positive impacts of IBR implementation across an array of team, patient, and care quality/delivery outcomes. Despite the preponderance of positive findings, great heterogeneity, and a reliance on quantitative non-randomized study designs remain in the extant research. A growing number of interventions to improve safety, quality, and care experiences in hospital settings focus on redesigning daily inpatient rounds. Limited information on IBR characteristics and implementation strategies coupled with widespread variation in terminology, study quality, and design create challenges in assessing the effectiveness of models of rounds and optimal implementation strategies. This scoping review highlights the need for additional studies of rounding models, implementation strategies, and outcomes that facilitate comparative research.
Introduction
Poor communication within interprofessional healthcare teams occurs commonly, contributing to inefficiency, medical errors, conflict, and other adverse outcomes (Kohn, Citation2000; Manser, Citation2009). Policymakers have called for interventions and research to improve interprofessional collaboration in practice (Institute of Medicine, Citation2012, Citation2015; Kohn, Citation2000).− Among promising models to improve collaboration is interprofessional bedside rounds (IBR). IBR is a rounding model that brings two or more health professions (i.e. physicians, nurses, pharmacists) together with patients and families as part of a consistent team-based routine to share information and collaboratively arrive at a daily plan of care (Ratelle et al., Citation2018; Reeves et al., Citation2017b). IBR is distinct from models that include multiple professions (i.e. medicine, nursing, pharmacy) but do not engage patients and families. This type of rounding model often occurs in a conference room and is frequently referred to as multidisciplinary rounds. IBR is also distinct from uniprofessional rounding models (often comprised of only physicians or only nurses) that engage patients and families at the bedside but do not include the larger interprofessional team. Both of these rounding models have substantial and growing bodies of research associated with them (Bhamidipati et al., Citation2016; Gurses & Xiao, Citation2006; Holodinsky et al., Citation2015; Mercedes et al., Citation2016; Walton et al., Citation2016; Will et al., Citation2019). IBR incorporates aspects of both of these approaches into one model that is both interprofessional and patient- and family-centered. By creating a framework for regular and better communication, IBR is thought to lead to improvements in team and patient outcomes. Frequently referred to as structured interprofessional bedside rounds (SIBR) or structured interdisciplinary bedside rounds (SIDR) these routines-of-care may improve communication, patient/staff satisfaction and experience, and clinical outcomes (Gonzalo et al., Citation2014; Lane et al., Citation2013; Ratelle et al., Citation2018; Reeves et al., Citation2017b). However, the emerging literature is heterogeneous in terms of how IBR is described and where studies are published. Further, optimal IBR models and best practices for implementation remain unclear.
A systematic scoping review of the literature was conducted to describe study characteristics and outcomes following new implementations of IBR to address this uncertainty. While new implementations of IBR have increased in recent years, little mapping or synthesis of this research has occurred. The purpose of this review was to investigate the breadth and quality of literature to identify and describe gaps and opportunities for future research.
This review builds on existing reviews in three key ways. First, by employing a scoping approach and including qualitative, quantitative, and mixed methods studies, we include a more comprehensive picture of the literature than other recent reviews have captured (Gonzalo et al., Citation2014; Lane et al., Citation2013; Pannick et al., Citation2015; Ratelle et al., Citation2018; Reeves et al., Citation2017b; Will et al., Citation2019). Second, by focusing specifically on IBR, we distinguish our efforts from those with a broader focus on interprofessional collaborative practice models in general (Baik et al., Citation2018; Donovan et al., Citation2018; Reeves et al., Citation2017a, Citation2017b; Weaver et al., Citation2014, Citation2013). Third, by centering our inquiry on rounding models that are both interprofessional and explicitly engage patients and families, this study distinctly complements reviews that focused only on one approach (Bhamidipati et al., Citation2016; Gurses & Xiao, Citation2006; Holodinsky et al., Citation2015; Mercedes et al., Citation2016; Walton et al., Citation2016; Will et al., Citation2019). Our working hypothesis is that combining these two approaches into one rounding model that is both interprofessional and patient- and family-centered holds greater potential to improve communication, care, and outcomes than either model does alone.
Methods
This systematic scoping review was developed and conducted following the adapted five-stage Arksey & O’Malley Framework (Arksey & O’Malley, Citation2005; Daudt et al., Citation2013; Levac et al., Citation2010; Peters et al., Citation2017). Reporting guidelines by PRISMA for Scoping Reviews were used to guide the manuscript’s development (Tricco et al., Citation2018). A review protocol is available upon request. This scoping review was not registered as, at the time of writing, Prospero did not accept registration of scoping reviews.
Formulating the question
Our team included collaborators from five institutions that either have or plan to implement an IBR model in one or more inpatient hospital units. The following three overarching research questions, which align with three of the six purposes that Munn et al. (Citation2018) outline for a scoping review, were addressed
How and where is research on new implementations of IBR being conducted?
What types of evidence (i.e. study designs, outcomes) describing new implementations of IBR are available?
What knowledge gaps exist in the field of IBR research?
Identifying relevant studies: data sources and search strategy
PubMed, CINAHL, PsycINFO, and Embase were searched by a health sciences librarian (FC) in consultation with the first author (EAB) for the concepts of patient care teams, rounds, inpatient hospitals, and at the bedside or in patients’ rooms. Additionally, the term “structured interprofessional bedside rounds” and its possible synonyms were searched as phrases. The search was performed in July 2018 and repeated in January 2019 and July 2020 to complete searching from the inception of the above databases through the end of June 2020. Unique references cited in six systematic reviews were included (Bhamidipati et al., Citation2016; Cypress, Citation2012; Gurses & Xiao, Citation2006; Lane et al., Citation2013; Ratelle et al., Citation2018; Walton et al., Citation2016). Records were de-duplicated with EndNote X9 (EndNote, Citationn.d.) then uploaded into Rayyan (Doha, Qatar; Ouzzani et al., Citation2016). See Appendix I for detailed search strategies.
Study selection
Two reviewers performed blinded title and abstract reviews using Rayyan, a web-based app for reviews (Ouzzani et al., Citation2016). Articles selected for full-text review were organized in REDCap (Nashville, TN) and screened by the lead author and one of 10 other review team members (see Appendix II in Supplementary Materials). At both steps, differences in determination were resolved through discussion and consensus with other reviewers. Studies were included if they were:
(1) published in English,
(2) focused on new IBR implementations,
(3) included patients or family members in rounds,
(4) reported a quantitative, qualitative, or mixed methods study design, and
(5) published in a peer review journal.
Studies were excluded if:
(1) rounds were exclusively educational, or
(2) the described interprofessional intervention was not about rounds.
Data abstraction
Data abstraction took place in two parts using online tools in a REDCap platform. First, the study quality was assessed using the Mixed Methods Assessment Tool (MMAT; Harris et al., Citation2009), a widely used and validated tool for critical appraisal of the methodological quality of studies divided into five categories: qualitative, randomized controlled, non-randomized, quantitative descriptive, and mixed methods (Hong et al., Citation2018). Answers to all MMAT questions are categorical with yes, no, or cannot tell options. The sum of “yes” items provides an overall quality score. Four researchers worked in pairs to independently evaluate the study quality of included articles using the MMAT. Any disagreements within the determination of the review pairs were reviewed and resolved by the lead author.
Nine members of our interprofessional research team abstracted article characteristics using a standardized Data Abstraction Tool (see Appendix III in Supplementary Materials). To mitigate bias and error, the lead author cross-checked a sample of abstractions (more than 25% of included articles; Mathes et al., Citation2017).
Descriptive statistics of abstracted data were performed with STATA SE14 (College Station, TX; StataCorp, Citation2017) and Microsoft Excel 2019 (Redmond, WA; Microsoft Excel Online, n.d.). Short answer fields were analyzed thematically (Attride-Stirling, Citation2001).
Results
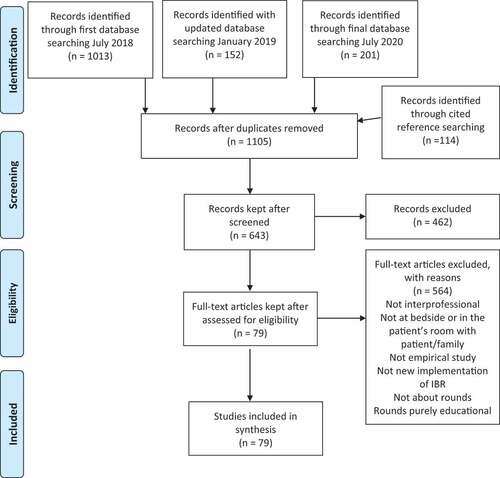
The initial search yielded 1,105 unique articles (). After the title/abstract review, 643 articles were retrieved, and 79 fulfilled inclusion criteria of being both interprofessional (having two or more professions involved) and intentionally engaged with patients and/or family members. Reasons for exclusion are listed in ; for example, rounds were not interprofessional or were purely educational. The professions most frequently described as being involved in IBR were attending physicians (n = 69, 87.3%), bedside nurses (n = 66, 83.5%), and physicians in training (n = 48, 60.8%). Pharmacists (n = 32, 40.5%), advanced practice providers (n = 27, 34.2%), and social workers (n = 22, 27.9%) were also frequent participants in IBR. In the majority of studies (n = 43, 54.4%) the previous rounding model was not sufficiently described to be able to determine where it occurred prior to the shift to IBR. When described, the most common prior locations included conference rooms or team rooms (n = 10, 12.7%), hallways (n = 9, 11.4%), or in-room but uniprofessional (n = 9, 11.4%).
Question 1: When, where, and how is research on new implementations of IBR being conducted?
Publication trends
The number of studies describing new implementations of IBR has increased in recent years (see Appendix IV in Supplementary Materials). While the earliest article meeting inclusion criteria was published in 1988, four or fewer articles were published each year between 1988 and 2013. Starting in 2014, five or more articles were published each year. In 2018, 13 (16.5%) of the 79 articles were published, and as of June 30, 2020, five additional articles had been published. Details of included articles can be found in chronological order in . Appendix V in Supplementary Materials provides a summary table of study characteristics.
Table 1. Abbreviated details of each of the included studies in chronological order (1988-June 30, 2020).
Included articles were published in over 50 journals with a wide array of foci (Appendix VI). The Journal of Hospital Medicine published the largest number of included articles (n = 6, 7.6%), followed by the Joint Commission Journal on Quality and Patient Safety (n = 5, 6.3%), and the Journal of Nursing Care Quality (n = 4, 5.1%).
Study locations
Nearly 75% of included studies took place in the United States (n = 58), followed by the United Kingdom (n = 7, 8.9%), Australia (n = 7, 8.9%), and Canada (n = 3, 3.8%). Brazil, Pakistan, South Korea, Sweden, and Switzerland each originated one study.
The majority of studies were conducted in academic medical centers (n = 64, 81.0%). One-quarter (n = 20, 25.3%) focused on IBR with pediatric patients and their families. The remainder focused on adult (n = 52, 65.8%) or older adult (age 66+) (n = 41, 51.9%) populations.
Acute care (n = 42, 56.0%) or intensive care units (n = 28, 35.4%) were the most common settings for included studies. The most frequent clinical specialties involved were general medical/surgical (n = 37, 46.8%), cardiology (n = 15, 19.0%), and surgery (n = 7, 8.9%). Three or fewer studies reported implementations in oncology, trauma, geriatric, or rehabilitation specialty areas. The remainder either did not describe a specialty area (n = 6, 7.6%) or described implementation across an entire institution (n = 2, 2.5%).
Funding for IBR Research Most publications reported no research funding (n = 52, 65.8%) (). Fourteen publications (17.7%) indicated funding from one or more U.S. federal funding sources – these included: Health Resources and Services Administration (n = 5, 6.3%), National Institutes of Health (n = 4, 5.1%), Veterans Affairs (n = 3, 3.8%), Patient-Centered Outcomes Research Institute (n = 1, 1.3%), or Agency for Healthcare Research and Quality (n = 1, 1.3%). Ten studies (12.7%) credited a foundation grant while 8 (10.1%) cited institutional funding. Three studies (3.8%) reported funding from pharmaceutical companies.
Question 2: What types of evidence describing new implementations of IBR models are available?
Study designs and quality
The majority (n = 69, 87.3%) of included studies asked both clear research questions and collected appropriate data to answer those research questions ().
Table 2. Summary of Mixed Methods Appraisal Tool (MMAT) results by study design (n = 79).
The most frequently published study design was a quantitative non-randomized approach (n = 53, 67.1%). These studies used other non-randomized units or patient groups as controls or utilized a pre-test/posttest approach to measure outcomes associated with IBR implementation. The balance of studies were mixed methods (n = 6, 7.6%), qualitative (n = 5, 6.3%), randomized controlled trials (n = 3, 3.8%), or quantitative descriptive (n = 2, 2.5%). Study quality varied widely across study types (). While small in number (n = 5), qualitative studies were the most highly rated for quality and the majority focused on qualitative explorations of patient and family perspectives of IBR (Berkwitt & Grossman, Citation2015; Cody et al., Citation2018; Hendricks et al., Citation2017; Latta et al., Citation2008; Thorne et al., Citation2017).
Among the non-randomized studies (n = 53), the most common MMAT deficiencies noted were unaddressed confounders (i.e. disease severity of patients) and lack of intervention fidelity. Fidelity is “the degree to which an intervention is delivered as intended” (Proctor et al., Citation2011, p. 69). In nearly 70% of these studies (n = 36) confounders were not accounted for in the design and analysis. In over 50% of these studies (n = 28), reviewers were unable to determine whether the intervention was delivered as intended or concluded that it had not been delivered as intended ().
Guiding theories, frameworks, and policies
Twenty-five articles (31.7%) cited a conceptual framework or theory supporting the study. The most frequently cited originated from the field of Quality Improvement (n = 9, 11.4%), including Plan-Do-Study-Act (Taylor et al., Citation2014), Continuous Quality Improvement (O’Donnell & Gupta, Citation2020), or the Quality Health Outcomes Framework (Mitchell & Lang, Citation2004). The next most common were six studies (7.6%) guided by a patient- and family-centered care (Davidson et al., Citation2017) or a shared decision-making framework (Michalsen et al., Citation2019), followed by five studies (6.3%) that utilized a systems framework – e.g., Toyota production systems (Rotter et al., Citation2019), clinical microsystems, and systems theory (Nelson et al., Citation2007). Finally, three studies (3.8%) referenced an interprofessional framework (Cox et al., Citation2016), and three studies (3.8%) referenced model of change frameworks (Bolton et al., Citation2021; Kotter, Citation2007). Additional frameworks used by individual studies include Meleis’ Transitions Theory (Meleis et al., Citation2000), Social-Material Practice Theory (Schatzki, Citation2002), AIDET format (Braverman et al., Citation2015), and Athletic Training Principles (Southwick et al., Citation2014). We found no articles citing implementation science frameworks or theories.
Nearly half of the reviewed studies (n = 33, 41.7%) referenced one or more specific organizations, policies, or practice guidelines in the framing of their study. The most commonly cited were the National Academy of Sciences’ (formerly the Institute of Medicine) (n = 9, 11.4%) statements on medical error and interprofessional care (Institute of Medicine, Citation2001, Citation2012, Citation2015; Kohn, Citation2000). This was followed by the American Academy of Pediatrics (n = 8, 10.1%) statement on patient- and family-centered rounding models as a standard of practice in inpatient pediatric care (Committee on Hospital Care and Institute for Patient- and Family-Centered Care, Citation2012).
Adoption/adaptation of existing IBR models
References to adoption or adaptation of a rounding model occurred in 40% of articles (n = 32). The most common approach was identifying a rounding model either from a literature review (n = 10, 10.3%) or from the 2015 study of Structured Interdisciplinary Bedside Rounds (SIBR) by Stein et al. (n = 7, 8.9%). Two studies each referenced adopting/adapting models described by Mittal (Citation2014), O’Leary et al. (Citation2011), and O’Leary et al. (Citation2016)), and Gonzalo et al. (Citation2010), Gonzalo et al. (Citation2013, Citation2014a, Citation2014b, Citation2016). Two studies also described adapting models observed in other units within their hospital system (Abu-Rish Blakeney et al., Citation2018; Licata et al., Citation2013). Adoption or adaptation processes were minimally described in most studies beyond referencing these sources.
Team, patient, and care quality/delivery outcomes
Study outcomes were categorized as: (1) team outcomes, (2) patient/client outcomes, or (3) health-care quality and delivery outcomes. Educational outcomes of rounds participation among learners were also considered and are described in the next section. Over half of the included studies evaluated impacts on both team and patient outcomes (n = 41, 51.9%), 25% of studies evaluated only patient outcomes (n = 20, 25.3%), and the remaining 23% of studies evaluated only team outcomes (n = 18, 22.8%) (). Nearly 90% (n = 70, 88.6%) of studies reported one or more health-care quality and delivery outcomes as defined by the Institute of Medicine Standards of Care (Institute of Medicine, Citation2001). A wide range of outcomes ranging from satisfaction to maintenance of confidentiality to incidence of nosocomial infections were evaluated within these broad categories by studies with overall positive results ().
Table 3. Team, patient/client, and health-care quality and delivery outcomes reported by included studies following implementation of interprofessional bedside rounds (n = 79).
Outcomes of rounds participation among learners
Thirteen (16.5%) of the 79 included studies considered whether participation in rounds was beneficial to learners (i.e., trainees). IBR participation was described as beneficial (n = 11, 84.6%) in the majority of studies reporting learner outcomes (Cameron et al., Citation2009; Cao et al., Citation2018; Dodek & Raboud, Citation2003; Khan et al., Citation2018; Lewis et al., Citation1988; Lopez et al., Citation2019; Rappaport et al., Citation2010; Saint et al., Citation2013; Seigel et al., Citation2014; Southwick et al., Citation2014; E. Young et al., Citation2018). For example, Lopez et al. (Citation2019) surveyed resident physicians who participated in SIBR implementation and found that, in addition to shortening the length of rounds, that residents felt that “SIBR positively impacted their education, family presence positively impacted learning, and SIBR was more effective than rounds without structure (p. 4).” Two studies reported mixed findings related to participation of learners. Monash et al. (Citation2017) found that despite their model shortening rounds on average by 8 minutes overall, trainees were less satisfied and perceived them to last longer than the previous rounding model. Bekmezian et al. (Citation2019) described adding 5- to 10-minute-long teaching appointments into their rounding structure after concerns surfaced about teaching during their appointment-based family-centered rounds model. In the balance of the 79 included studies, learners were described as being present in 33 studies (41.8%), but learning outcomes were not described. The remaining 33 studies (41.8%) did not report having learners present.
Discussion
Rounds are a complex care routine that occurs daily for most inpatients, although formats vary widely due to overlapping or competing perspectives on the purpose of rounds (Bharwani et al., Citation2012; Holodinsky et al., Citation2015; Monash, Citation2017; Walton et al., Citation2016). Historically, rounds were uni-professional (typically medicine) and provider-centric. Increasingly, rounds have been redesigned to improve outcomes by including other professions (i.e., nursing, pharmacy) and intentional engagement with patients and families (Gonzalo et al., Citation2014). This combination of ubiquity and high variability is what makes rounds an opportune focus for study and improvement efforts.
This systematic scoping review identified studies reporting new IBR implementations beginning in 1988 and with increasing frequency of publications in this field since 2014. The majority of studies report positive impacts of rounding model implementation across an array of the team, patient, and care quality/delivery outcomes. Despite this growth and a preponderance of positive findings, there remains a great deal of heterogeneity and a reliance on quantitative non-randomized study and single-center designs. This makes it challenging to carry out systematic reviews or meta-analyses that would permit moving from IBR as a promising, evidence-informed care model to an evidence-based practice standard of care.
A major weakness of the existing research is a lack of explicit theory to frame why and how IBR might be expected to lead to a broad array of positive changes (Shoemaker et al., Citation2004). Most articles articulated a hypothesis or purpose linking improved communication between interprofessional teams and patients/families during rounds to improved patient outcomes. However, only 30% referenced a specific theory or framework that guided their study. Further, nearly half of the included studies reported on team or patient outcomes, but not both. We considered analyses examining whether patient outcomes (i.e. length of stay or readmissions) improved following IBR implementation without also incorporating assessments of team communication to have the potential for substantial confounding. Future studies should more clearly explicate the theory underlying their research and incorporate assessments of communication into analyses of patient outcomes.
A key impediment to the dissemination of successful IBR systems was a lack of specificity when reporting both pre- and post-intervention rounding models. Many articles referenced previously published IBR models, but few explicitly described the linkage between published models and the implemented model. Although we intended to abstract data about rounding model characteristics, implementation strategies, and implementation outcomes, descriptions were too sparse and varied to map these features to frameworks accurately. Even when studies included robust model details, measures of fidelity were lacking. Assessment of fidelity is essential to understanding whether findings can be attributed to a change in rounding models. However, we found that the majority of quantitative non-randomized studies did not account for confounders, and approximately 50% of these studies did not indicate if the intervention occurred as intended. Incorporating implementation science frameworks and tools in future studies would help develop a clearer picture of whether, how, and why some implementations of IBR lead to improvements in outcomes and others fail to achieve these same goals (Birken et al., Citation2017; Powell et al., Citation2019). Additional specifications would also help to clarify which elements of IBR are essential core components, and which aspects are discretionary or adaptable (Abry et al., Citation2015; Fixsen et al., Citation2009).
Additional funding is needed to close gaps in the IBR literature and to support rigorous multi-site studies with advanced study designs, such as cluster or stepped wedge randomized trials. The majority of studies included in this review did not report funding to support their implementation project, precluding costly investigations with high sample sizes, randomized designs, and rigorous monitoring of implementation fidelity. The recent surge in unfunded studies suggests that front-line care team members are open to innovation in rounding methods and hint at face validity for this type of care model. However, the current science is over-reliant on quantitative non-randomized designs. Research utilizing a variety of designs and methods, particularly qualitative, mixed methods, and RCTs would enrich and strengthen this literature.
Future studies should also address the potential for IBR models to have differential effects for different groups, including the potential to reduce inequities or disparities in inpatient hospital care. Inequities in inpatient care and outcomes are increasingly recognized (Nayfeh & Fowler, Citation2020). Only three studies (Braus et al., Citation2016; Dunn et al., Citation2017; Khan et al., Citation2018) addressed equity in their study designs or results, and those that did found a mix of positive or neutral improvements, although equity or disparities were not the primary foci of these studies. Similarly, while many articles addressed patient satisfaction or patient- and family-centeredness of rounds, the approaches used in these studies ranged widely. Examination of potential mismatches between care team perceptions of patient- and family-centeredness of IBR models and patient- and family perceptions of the same processes to improve these models would be a useful next step. Additionally, patient- and family-centered interventions may need to be developed and tested to determine the best way to orient and support patients and families’ participation in IBR.
Limitations
This review has several limitations. First, while we intentionally used broad search terms and considered a large number of articles for inclusion, the heterogeneity of terms used and the broad array of journals in which this work has been published make it likely that some studies may have been missed. Harmonization of terms for IBR models would have many benefits both in clinical practice areas and for the research literature. Second, we excluded articles that reported implementing interprofessional rounds when we were unable to determine if rounds took place at the bedside and whether patients and families were explicitly engaged. Third, we excluded published conference abstracts, and unpublished and non-peer-reviewed manuscripts. Both may contribute to underestimating the rate at which IBR models are being implemented and overestimating positive outcomes because of well-known publication bias toward positive results (H. Sharma & Verma, Citation2019). Additionally, as described above, we intended to examine implementation strategies and outcomes but could not due to a lack of specificity and heterogeneity in the literature. Finally, all reviewed articles predate the Covid-19 pandemic, and thus application in a pandemic situation represents an unknown and a limitation of the review.
Conclusion
This systematic scoping review investigated the current breadth and quality of literature describing new implementations of IBR that indicate substantial growth and overwhelmingly positive outcomes, albeit with gaps. To close these gaps, we encourage authors to include more detail about the IBR models they are implementing, what implementation strategies they are using, and how the new models are different from usual care prior to IBR implementation. Additionally, situating future studies within theoretical frameworks, using mixed methods approaches, and employing more rigorous study designs has the potential to greatly enhance our understanding of both how and why IBR models work. Carrying out these more complex study designs will require investment from funders to continue to build the evidence base for models of patient- and family-centered interprofessional collaborative practice.
Supplemental Material
Download Zip (119.2 KB)Acknowledgments
The lead author received funding to support her time during the conceptualization, data collection, analysis and manuscript writing for this project from the NIH National Heart, Lung, and Blood Institute K12 (#5K12HL137940) as part of the UW Implementation Science Training Program and her time during manuscript revisions from a National Heart, Lung, and Blood Institute K23 (1K23HL144910-01A1). BK and NS received support from NCATS (UL1 TR002319). RS received support from the Macy Foundation.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the writing and content of this article.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
Notes on contributors
Erin Abu-Rish Blakeney
Erin Abu-Rish Blakeney, PhD, MA, RN is a Research Assistant Professor at the University of Washington (UW) School of Nursing. She is also a co-lead of the Institute of Translational Health Sciences Team Science Core and affiliate faculty with the UW Center for Inteprofessional Education, Research and Practice.
Frances Chu
Frances Chu has a Masters in Library and Information Science and works as an Adjunct Medical Librarian at Gonzaga University. She is also a PhD candidate at the University of Washington School of Nursing.
Andrew A. White
Andrew White, MD is a Professor of Medicine at the University of Washington. He is board certified in Internal Medicine and Clinical Informatics.
G. Randy Smith
Randy Smith is an assistant professor of hospital medicine at Northwestern University Feinberg School of Medicine, and a unit medical director at Northwestern Memorial Hospital.
Kyla Woodward
Kyla Woodward is a PhD candidate at the University of Washington School of Nursing
Danielle C. Lavallee
Danielle Lavallee, PharmD, PhD is the Scientific Director for theBritish Columbia Academic Health Science Network and Affiliate Associate Professor in the Departments Health Services at theUniversity of Washington.
Rachel Marie E. Salas
Rachel Salas, MD, MEd, FAAN, FANA is a board-certified Sleep Neurologist at Johns Hopkins Medicine, Department of Neurology.
Mayumi A. Willgerodt
Mayumi Willgerodt, PhD, MPH, RN, FAAN, FNASN is Associate Professor and Vice-Chair for of Education in the Department of Child, Family, and Population Health Nursing at the University of Washington and affiliate core faculty in the Center for Health Sciences Interprofessional Education Research and Practice (CHSIE) and Leadership and Education in Adolescent Health Training Program (LEAH).
Deborah Dang
Deborah Dang recently retired from the Johns Hopkins Hospital and Health System as Director of Nursing. John Dent, MD, MS is a Professor Emeritus of Medicine at the University of Virginia Health System and a Clinical Professor of Nursing at the University of Virginia School of Nursing.
Elizabeth Ibby Tanner
Elizabeth K. Tanner, Ph.D, R.N., is a registered nurse and Professor Emeritus at Johns Hopkins School of Nursing with a joint appointment in the School of Medicine, Division of Geriatric Medicine and Gerontology. She was core faculty in the Center on Aging and Health; principal faculty in the Center for Innovative Care in Aging and inaugural Director of the Collaborative for Interprofessional Education and Practice.
Nicole Summerside
Nicole Summerside, MHA is an affiliate instructor in the department of Biobehavorial Nursing and Health Informatics at the University of Washington School of Nursing and the Manager of Program Operations for the UW Center for Health Sciences Interprofessional Education, Research and Practice.
Brenda K. Zierler
Brenda Zierler PhD, RN, FAAN is a professor in the Department of Biobehavioral Nursing and Health Informatics at the University of Washington School of Nursing and is adjunct professor in the Department of Health Services at the University of Washington School of Public Health, and in the Departments of Surgery (Vascular Division) and Department of Biomedical Informatics and Medical Education at the University of Washington School of Medicine. She is Co-Lead of the Team Science Core for the UW Institute for Translational Health Sciences and Director of Research and Training for the Center for Health Sciences Interprofessional Education, Research and Practice.
Kevin D. O’Brien
Kevin O’Brien, MD is a Professor of Medicine at the University of Washington and Service Director for Inpatient Cardiology at the University of Washington Medical Center.
Bryan J. Weiner
Bryan Weiner PhD, is Professor, Department of Global Health and Department of Health Systems and Population Health, at the University of Washington.
References
- Abry, T., Hulleman, C. S., & Rimm-Kaufman, S. E. (2015). Using indices of fidelity to intervention core components to identify program active ingredients. American Journal of Evaluation, 36(3), 320–338. https://doi.org/10.1177/1098214014557009
- Abu-Rish Blakeney, E., Lavallee, D. C., Baik, D., Pambianco, S., O’Brien, K. D., & Zierler, B. K, et al. (2018). Purposeful interprofessional team intervention improves relational coordination among advanced heart failure care teams. Journal of Interprofessional Care, 33(5), 481–489. https://doi.org/10.1080/13561820.2018.1560248
- Akuamoah-Boateng, K. A., Wiencek, C., Esquivel, J. H., DeGennaro, G., Torres, B., & Whelan, J. F, et al. (2019). Ramped-up: the development and testing of an interprofessional collaboration model. Journal of Trauma Nursing, 26(6), 281–289. https://doi.org/10.1097/JTN.0000000000000466
- Allen, S. R., Pascual, J., Martin, N., Reilly, P., Luckianow, G., Datner, E., Davis, K., & Kaplan, L. J, et al. (2016). A novel method of optimizing patient- and family-centered care in the ICU. The Journal of Trauma and Acute Care Surgery, 82(3), 582–586. https://doi.org/10.1097/TA.0000000000001332
- Arksey, H., & O’Malley, L. (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616Attride-Stirling, J. (2001). Thematic networks: an analytic tool for qualitative research. Qualitative Research, 1(3), 385–405. https://journals.sagepub.com/doi/10.1177/146879410100100307
- Attride-Stirling, J. (2001). Thematic networks: An analytic tool for qualitative research. Qualitative Research, 1(3), 385–405. https://journals.sagepub.com/doi/10.1177/146879410100100307
- Austin, S., Powers, K., Florea, S., & Gaston, T. (2020). Evaluation of a nurse practitioner-led project to improve communication and collaboration in the acute care setting. Journal of the American Association of Nurse Practitioners. Advance online publication. https://doi.org/10.1097/JXX.0000000000000402
- Baik, D., Abu-Rish Blakeney, E., Willgerodt, M., Woodard, N., Vogel, M., & Zierler, B, et al. (2018). Examining interprofessional team interventions designed to improve nursing and team outcomes in practice: A descriptive and methodological review. Journal of Interprofessional Care, 1–9. https://doi.org/10.1080/13561820.2018.1505714
- Baik, D., & Zierler, B. (2018). RN job satisfaction and retention after an interprofessional team intervention. Western Journal of Nursing Research, 41(4), 615–630. https://doi.org/10.1177/0193945918770815
- Barcellos, R. A., & Chatkin, J. M. (2020). Impact of a multidisciplinary checklist on the duration of invasive mechanical ventilation and length of ICU stay. Jornal Brasileiro De Pneumologia, 46(3), e20180261–3756.
- Basic, D., Huynh, E., Gonzales, R., & Shanley, C. (2018). Structured interdisciplinary bedside rounds, in-hospital deaths, and new nursing home placements among older inpatients. Clinical Interventions in Aging, 13, 2289–2294. https://doi.org/10.2147/CIA.S171508
- Beaird, G. (2019). CE: A historical review of nurse-physician bedside rounding. The American Journal of Nursing, 119(4), 30–38. https://doi.org/10.1097/01.NAJ.0000554525.02127.3b
- Bekmezian, A., Fiore, D. M., Long, M., Monash, B. J., Padrez, R., Rosenbluth, G., & Sun, K. I, et al. (2019). Keeping time: implementing appointment-based family-centered rounds. Pediatric Quality and Safety, 4(4), e182. https://doi.org/10.1097/pq9.0000000000000182
- Berkwitt, A., & Grossman, M. (2015). A qualitative analysis of pediatric patient attitudes regarding family-centered rounds. Hospital Pediatrics, 5(7), 357–362. https://doi.org/10.1542/hpeds.2014-0198
- Bhamidipati, V. S., Elliott, D. J., Justice, E. M., Belleh, E., Sonnad, S. S., & Robinson, E. J, et al. (2016). Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: A systematic review and suggested taxonomy. Journal of Hospital Medicine, 11(7), 513–523. https://doi.org/10.1002/jhm.2575
- Bharwani, A. M., Harris, G. C., & Southwick, F. S. (2012). Perspective: A business school view of medical interprofessional rounds: transforming rounding groups into rounding teams. Academic Medicine: Journal of the Association of American Medical Colleges, 87(12), 1768–1771. https://doi.org/10.1097/ACM.0b013e318271f8da
- Birken, S. A., Powell, B. J., Shea, C. M., Haines, E. R., Alexis Kirk, M., Leeman, J., Rohweder, C., Damschroder, L., & Presseau, J, et al. (2017). Criteria for selecting implementation science theories and frameworks: Results from an international survey. Implementation Science: IS, 12(1), 124. https://doi.org/10.1186/s13012-017-0656-y
- Bolton, R., Logan, C., & Gittell, J. H. (2021). Revisiting relational coordination: A systematic review. The Journal of Applied Behavioral Science. https://doi.org/10.1177/0021886321991597
- Bonello, R. S., Fletcher, C. E., Becker, W. K., Clutter, K. L., Arjes, S. L., Cook, J. J., & Petzel, R. A, et al. (2008). An intensive care unit quality improvement collaborative in nine department of veterans affairs hospitals: reducing ventilator-associated pneumonia and catheter-related bloodstream infection rates. Joint Commission Journal on Quality and Patient Safety, 34(11), 639–645. https://doi.org/10.1016/S1553-7250(08)34081-1
- Braus, N., Campbell, T. C., Kwekkeboom, K. L., Ferguson, S., Harvey, C., Krupp, A. E., Lohmeier, T., Repplinger, M. D., Westergaard, R. P., Jacobs, E. A., Roberts, K. F., & Ehlenbach, W. J, et al. (2016). Prospective study of a proactive palliative care rounding intervention in a medical ICU. Intensive Care Medicine, 42(1), 54–62. https://doi.org/10.1007/s00134-015-4098-1
- Braverman, A. M., Kunkel, E. J., Katz, L., Katona, A., Heavens, T., Miller, A., & Arfaa, J. J, et al. (2015). Do I buy it? how AIDETTM training changes residents’ values about patient care. Journal of Patient Experience, 2(1), 13–20. https://doi.org/10.1177/237437431500200104
- Cameron, M. A., Schleien, C. L., & Morris, M. C. (2009). Parental presence on pediatric intensive care unit rounds. Journal of Pediatrics, 155(4), 522–528. https://doi.org/10.1016/j.jpeds.2009.03.035
- Cao, V., Tan, L. D., Horn, F., Bland, D., Giri, P., Maken, K., Cho, N., Scott, L., Dinh, V. A., Hidalgo, D., & Nguyen, H. B, et al. (2018). Patient-centered structured interdisciplinary bedside rounds in the medical ICU. Critical Care Medicine, 46(1), 85–92. https://doi.org/10.1097/CCM.0000000000002807
- Chava, R., Karki, N., Ketlogetswe, K., & Ayala, T. (2020). Multidisciplinary rounds in prevention of 30-day readmissions and decreasing length of stay in heart failure patients: A community hospital based retrospective study. Medicine (Baltimore), 98(27), e16233. https://doi.org/10.1097/MD.0000000000016233
- Chow, M. Y., Nikolic, S., Shetty, A., & Lai, K. (2018). Structured interdisciplinary bedside rounds in an Australian tertiary hospital emergency department: patient satisfaction and staff perspectives. Emergency Medicine Australasia, 31(3), 347–354. https://doi.org/10.1111/1742-6723.13160
- Clarke, D., Nguyen, D., & Overton, K. (2020). Antimicrobial stewardship in spinal cord injury: A multidisciplinary approach. Journal of Spinal Cord Medicine, 1–5. https://doi.org/10.1080/10790268.2020.1731225
- Clay-Williams, R., Plumb, J., Luscombe, G. M., Hawke, C., Dalton, H., Shannon, G., & Johnson, J, et al. (2018). Improving teamwork and patient outcomes with daily structured interdisciplinary bedside rounds: A multimethod evaluation. Journal of Hospital Medicine, 13(5), 311–317. https://doi.org/10.12788/jhm.2850
- Cody, S. E., Sullivan-Bolyai, S., & Reid-Ponte, P. (2018). Making a connection: family experiences with bedside rounds in the intensive care unit. Critical Care Nurse, 38(3), 18–26. https://doi.org/10.4037/ccn2018128
- Committee on Hospital Care and Institute for Patient- and Family-Centered Care. (2012). Patient- and family-centered care and the pediatrician’s role. Pediatrics, 129(2), 394–404. https://doi.org/10.1542/peds.2011-3084
- Cox, M., Cuff, P., Brandt, B., Reeves, S., & Zierler, B. (2016). Measuring the impact of interprofessional education on collaborative practice and patient outcomes. Journal of Interprofessional Care, 30(1), 1–3. https://doi.org/10.3109/13561820.2015.1111052
- Cypress, B. S. (2012). Family presence on rounds: A systematic review of literature. Dimensions of Critical Care Nursing, 31(1), 53–64. https://doi.org/10.1097/DCC.0b013e31824246dd
- Daudt, H. M. L., van Mossel, C., & Scott, S. J. (2013). Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Medical Research Methodology, 13, 48. https://doi.org/10.1186/1471-2288-13-48
- Davidson, J. E., Aslakson, R. A., Long, A. C., Puntillo, K. A., Kross, E. K., Hart, J., Cox, C. E., Wunsch, H., Wickline, M. A., Nunnally, M. E., Netzer, G., Kentish-Barnes, N., Sprung, C. L., Hartog, C. S., Coombs, M., Gerritsen, R. T., Hopkins, R. O., Franck, L. S., Skrobik, Y., & Curtis, J. R, et al. (2017). Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Critical Care Medicine, 45(1), 103–128. https://doi.org/10.1097/CCM.0000000000002169
- Dodek, P. M., & Raboud, J. (2003). Explicit approach to rounds in an ICU improves communication and satisfaction of providers. Intensive Care Medicine, 29(9), 1584–1588. https://doi.org/10.1007/s00134-003-1815-y
- Donovan, A. L., Aldrich, J. M., Gross, A. K., Barchas, D. M., Thornton, K. C., Schell-Chaple, H. M., Gropper, M. A., & Lipshutz, A. K. M., #x0026, University of California, San Francisco Critical Care Innovations Group, et al. (2018). Interprofessional care and teamwork in the ICU. Critical Care Medicine, 46(6), 980–990. https://doi.org/10.1097/CCM.0000000000003067
- Dunn, A. S., Reyna, M., Radbill, B., Parides, M., Colgan, C., Osio, T., Benson, A., Brown, N., Cambe, J., Zwerling, M., Egorova, N., & Kaplan, H, et al. (2017). The impact of bedside interdisciplinary rounds on length of stay and complications. Journal of Hospital Medicine, 12(3), 137–142. https://doi.org/10.12788/jhm.2695
- Dutton, R. P., Cooper, C., Jones, A., Leone, S., Kramer, M. E., & Scalea, T. M, et al. (2003). Daily multidisciplinary rounds shorten length of stay for trauma patients. Journal of Trauma, 55(5), 913–919. https://doi.org/10.1097/01.TA.0000093395.34097.56
- EndNote. (n.d.). Clarivate analytics [computer software]. Retrieved from February 1, 2021. https://endnote.com/
- Fertleman, M., Barnett, N., & Patel, T. (2005). Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Quality & Safety in Health Care, 14(3), 207–211. https://doi.org/10.1136/qshc.2004.011759
- Fixsen, D. L., Blasé, K. A., Naoom, S. F., & Wallace, F. (2009). Core implementation components. Research on Social Work Practice, (5). https://journals.sagepub.com/doi/abs/10.1177/1049731509335549
- Gausvik, C., Lautar, A., Miller, L., Pallerla, H., & Schlaudecker, J. (2015). Structured nursing communication on interdisciplinary acute care teams improves perceptions of safety, efficiency, understanding of care plan and teamwork as well as job satisfaction. Journal of Multidisciplinary Healthcare, 8, 33–37. https://doi.org/10.2147/JMDH.S72623
- Gonzalo, J. D., Chuang, C. H., Huang, G., & Smith, C. (2010). The return of bedside rounds: an educational intervention. Journal of General Internal Medicine, 25(8), 792–798. https://doi.org/10.1007/s11606-010-1344-7
- Gonzalo, J. D., Heist, B. S., Duffy, B. L., Dyrbye, L., Fagan, M. J., Ferenchick, G., Harrell, H., Hemmer, P. A., Kernan, W. N., Kogan, J. R., Rafferty, C., Wong, R., & Elnicki, D. M, et al. (2013). The art of bedside rounds: A multi-center qualitative study of strategies used by experienced bedside teachers. Journal of General Internal Medicine, 28(3), 412–420. https://doi.org/10.1007/s11606-012-2259-2
- Gonzalo, J. D., Himes, J., McGillen, B., Shifflet, V., & Lehman, E. (2016). Interprofessional collaborative care characteristics and the occurrence of bedside interprofessional rounds: A cross-sectional analysis. BMC Health Services Research, 16, 459. https://doi.org/10.1186/s12913-016-1714-x
- Gonzalo, J. D., Kuperman, E., Lehman, E., & Haidet, P. (2014a). Bedside interprofessional rounds: Perceptions of benefits and barriers by internal medicine nursing staff, attending physicians, and housestaff physicians. Journal of Hospital Medicine, 9(10), 646–651. https://doi.org/10.1002/jhm.2245
- Gonzalo, J. D., Wolpaw, D. R., Lehman, E., & Chuang, C. H. (2014). Patient-centered interprofessional collaborative care: Factors associated with bedside interprofessional rounds. Journal of General Internal Medicine, 29(7), 1040–1047. https://doi.org/10.1007/s11606-014-2817-x
- Gonzalo, J. D., Wolpaw, D. R., Lehman, E., & Chuang, C. H. (2014b). Patient-centered interprofessional collaborative care: factors associated with bedside interprofessional rounds. Journal of General Internal Medicine, 29(7), 1040–1047. https://doi.org/10.1008/s11606-014-2817-x
- Gormley, D. K., Costanzo, A. J., Goetz, J., Israel, J., Hill-Clark, J., Pritchard, T., & Staubach, K, et al. (2019). Impact of nurse-led interprofessional rounding on patient experience. The Nursing Clinics of North America, 54(1), 115–126. https://doi.org/10.1016/j.cnur.2018.10.007
- Gurses, A. P., & Xiao, Y. (2006). A systematic review of the literature on multidisciplinary rounds to design information technology. Journal of the American Medical Informatics Association: JAMIA, 13(3), 267–276. https://doi.org/10.1197/jamia.M1992
- Gustafson, K. W., LaBrecque, M. A., Graham, D. A., Tella, N. M., & Curley, M. A. (2016). Effect of parent presence during multidisciplinary rounds on NICU-related parental stress. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 45(5), 661–670. https://doi.org/10.1016/j.jogn.2016.04.012
- Ha, D. R., Forte, M. B., Olans, R. D., Yong, K. O., Olans, R. N., Gluckstein, D. P., Kullar, R., Desai, M., Catipon, N., Ancheta, V., Lira, D., Khattak, Y., Legge, J., Nguyen, K. B., Chan, S., Mourani, J., & McKinnell, J. A, et al. (2019). A multidisciplinary approach to incorporate bedside nurses into antimicrobial stewardship and infection prevention. The Joint Commission Journal on Quality and Patient Safety, 45(9), 600–605. https://doi.org/10.1016/j.jcjq.2019.03.003
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G, et al. (2009). Research electronic data capture (REDCap) A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
- Hendricks, S., LaMothe, V. J., Kara, A., & Miller, J. (2017). Facilitators and barriers for interprofessional rounding: A qualitative study. Clinical Nurse Specialist, 31(4), 219–228. https://doi.org/10.1097/NUR.0000000000000310
- Henkin, S., Chon, T. Y., Christopherson, M. L., Halvorsen, A. J., Worden, L. M., & Ratelle, J. T, et al. (2016). Improving nurse-physician teamwork through interprofessional bedside rounding. Journal of Multidisciplinary Healthcare, 9, 201–205.
- Holodinsky, J. K., Hebert, M. A., Zygun, D. A., Rigal, R., Berthelot, S., Cook, D. J., & Stelfox, H. T, et al. (2015). A survey of rounding practices in Canadian adult intensive care units. PloS One, 10(12), e0145408. https://doi.org/10.1371/journal.pone.0145408
- Hong, Q. N., Gonzalez‐Reyes, A., & Pluye, P. (2018). Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the mixed methods appraisal tool (MMAT). Journal of Evaluation in Clinical Practice, 24(3), 459–467. https://doi.org/10.1111/jep.12884
- Huang, K. T., Minahan, J., Brita-Rossi, P., Aylward, P., Katz, J. T., Roy, C., Schnipper, J., & Boxer, R, et al. (2017). All together now: impact of a regionalization and bedside rounding initiative on the efficiency and inclusiveness of clinical rounds. Journal of Hospital Medicine, 12(3), 150–156. https://doi.org/10.12788/jhm.2696
- Huynh, E., Basic, D., Gonzales, R., & Shanley, C. (2017). Structured interdisciplinary bedside rounds do not reduce length of hospital stay and 28-day re-admission rate among older people hospitalised with acute illness: an Australian study. Australian Health Review, 41(6), 599–605. https://doi.org/10.1071/AH16019
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academy Press. 2001.
- Institute of Medicine. (2012). Best care at lower cost: the path to continuously learning health care in America. https://www.nap.edu/catalog/13444/best-care-at-lower-cost-the-path-to-continuously-learning
- Institute of Medicine. (2015). Measuring the impact of interprofessional education on collaborative practice and patient outcomes. The National Academies Press. https://doi.org/10.17226/21726.
- Jacobowski, N. L., Girard, T. D., Mulder, J. A., & Ely, E. W. (2010). Communication in critical care: family rounds in the intensive care unit. American Journal of Critical Care, 19(5), 421–430. https://doi.org/10.4037/ajcc2010656
- Justice, L. B., Cooper, D. S., Henderson, C., Brown, J., Simon, K., Clark, L., Fleckenstein, E., Benscoter, A., & Nelson, D. P, et al. (2016). Improving communication during cardiac ICU multidisciplinary rounds through visual display of patient daily goals. Pediatric Critical Care Medicine, 17(7), 677–683. https://doi.org/10.1097/PCC.0000000000000790
- Kang, J., Cho, Y. J., & Choi, S. (2020). State anxiety, uncertainty in illness, and needs of family members of critically ill patients and their experiences with family-centered multidisciplinary rounds: A mixed model study. PLoS One, 15(6), e0234296. https://doi.org/10.1371/journal.pone.0234296
- Khan, A., Spector, N. D., Baird, J. D., Ashland, M., Starmer, A. J., Rosenbluth, G., & Landrigan, C. P, et al. (2018). Patient safety after implementation of a coproduced family centered communication programme: multicenter before and after intervention study. BMJ, 363, k4764. https://doi.org/10.1136/bmj.k4764
- Kohn, L. T. (Ed.). (2000). To err is human: Building a safer health system. Institute of Medicine, Committee on Quality of Health Care in America. National Academies Press (US). 2000. http://www.ncbi.nlm.nih.gov/books/NBK225182/.
- Kotter, J. P. (2007). Leading change: Why transformation efforts fail. Harvard Business Rev.
- Kucukarslan, S. N., Peters, M., Mlynarek, M., & Nafziger, D. A. (2003). Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Archives of Internal Medicine, 163(17), 2014–2018. https://doi.org/10.1001/archinte.163.17.2014
- Ladak, L. A., Premji, S. S., Amanullah, M. M., Haque, A., Ajani, K., & Siddiqui, F. J, et al. (2012). Family-centered rounds in Pakistani pediatric intensive care settings: Non-randomized pre- and post-study design. International Journal of Nursing Studies, 50(6), 717–726. https://doi.org/10.1016/j.ijnurstu.2012.05.009
- Lane, D., Ferri, M., Lemaire, J., McLaughlin, K., & Stelfox, H. T. (2013). A systematic review of evidence-informed practices for patient care rounds in the ICU. Critical Care Medicine, 41(8), 2015–2029. https://doi.org/10.1097/CCM.0b013e31828a435f
- Latta, L. C., Dick, R., Parry, C., & Tamura, G. S. (2008). Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: A qualitative study. Academic Medicine, 83(3), 292–297. https://doi.org/10.1097/ACM.0b013e3181637e21
- Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: advancing the methodology. Implementation Science, 5, 69. https://doi.org/10.1186/1748-5908-5-69
- Lewis, C., Knopf, D., Chastain-Lorber, K., Ablin, A., Zoger, S., Matthay, K., Glasser, M., & Pantell, R, et al. (1988). Patient, parent, and physician perspectives on pediatric oncology rounds. Journal of Pediatrics, 112(3), 378–384. https://doi.org/10.1016/S0022-3476(88)80316-0
- Li, J., Talari, P., Kelly, A., Latham, B., Dotson, S., Manning, K., Thornsberry, L., Swartz, C., & Williams, M. V, et al. (2018). Interprofessional teamwork innovation model (ITIM) to promote communication and patient-centred, coordinated care. BMJ Quality & Safety, 27(9), 700–709. https://doi.org/10.1136/bmjqs-2017-007369
- Licata, J., Aneja, R. K., Kyper, C., Spencer, T., Tharp, M., Scott, M., & Pasek, T. A, et al. (2013). A foundation for patient safety: phase I implementation of interdisciplinary bedside rounds in the pediatric intensive care unit. Critical Care Nurse, 33(3), 89–91. https://doi.org/10.4037/ccn2013280
- Lopez, M., Vaks, Y., Wilson, M., Mitchell, K., Lee, C., Ejike, J., Oei, G., Kaufman, D., Hambly, J., Tinsley, C., Bahk, T., Samayoa, C., Pappas, J., & Abd-Allah, S, et al. (2019). Impacting satisfaction, learning, and efficiency through structured interdisciplinary rounding in a pediatric intensive care unit: A quality improvement project. Pediatric Quality and Safety, 4(3), e176. https://doi.org/10.1097/pq9.0000000000000176
- Luthy, C., Francis Gerstel, P., Pugliesi, A., Piguet, V., Allaz, A. F., & Cedraschi, C, et al. (2017). Bedside or not bedside: evaluation of patient satisfaction in intensive medical rehabilitation wards. PloS One, 12(2), e0170474. https://doi.org/10.1371/journal.pone.0170474
- Makowsky, M. J., Koshman, S. L., Midodzi, W. K., & Tsuyuki, R. T. (2009). Capturing outcomes of clinical activities performed by a rounding pharmacist practicing in a team environment: the COLLABORATE study [NCT00351676]. Medical Care, 47(6), 642–650. https://doi.org/10.1097/MLR.0b013e3181926032
- Malec, A., Mork, A., Hoffman, R., & Carlson, E. (2018). The care team visit: approaching interdisciplinary rounds with renewed focus. Journal of Nursing Care Quality, 33(2), 135–142. https://doi.org/10.1097/NCQ.0000000000000279
- Manser, T. (2009). Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143–151. https://doi.org/10.1111/j.1399-6576.2008.01717.x
- Mathes, T., Klaßen, P., & Pieper, D. (2017). Frequency of data extraction errors and methods to increase data extraction quality: A methodological review. BMC Medical Research Methodology, 17. https://doi.org/10.1186/s12874-017-0431-4
- McGrath, B. A., Lynch, J., Bonvento, B., Wallace, S., Poole, V., Farrell, A., Diaz, C., Khwaja, S., & Roberson, D. W, et al. (2017). Evaluating the quality improvement impact of the global tracheostomy collaborative in four diverse NHS hospitals. BMJ Quality Improvement Reports, 6(1). https://doi.org/10.1136/bmjquality.u220636.w7996
- Meleis, A. I., Sawyer, L. M., Im, E. O., Hilfinger Messias, D. K., & Schumacher, K. (2000). Experiencing transitions: An emerging middle-range theory. ANS. Advances in Nursing Science, 23(1), 12–28. https://doi.org/10.1097/00012272-200009000-00006
- Mercedes, A., Fairman, P., Hogan, L., Thomas, R., & Slyer, J. T. (2016). Effectiveness of structured multidisciplinary rounding in acute care units on length of stay and satisfaction of patients and staff: A quantitative systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(7), 131–168. https://doi.org/10.11124/JBISRIR-2016-003014
- Michalsen, A., Long, A. C., DeKeyser Ganz, F., White, D. B., Jensen, H. I., Metaxa, V., Hartog, C. S., Latour, J. M., Truog, R. D., Kesecioglu, J., Mahn, A. R., & Curtis, J. R, et al. (2019). Interprofessional shared decision-making in the ICU: A systematic review and recommendations from an expert panel. Critical Care Medicine, 47(9), 1258–1266. https://doi.org/10.1097/CCM.0000000000003870
- Mitchell, P. H., & Lang, N. M. (2004). Framing the problem of measuring and improving healthcare quality: has the quality health outcomes model been useful?. Medical Care, 42(2), II4–11. https://doi.org/10.1097/01.mlr.0000109122.92479.fe
- Mittal, V. (2014). Family-centered rounds. Pediatric Clinics of North America, 61(4), 663–670. https://doi.org/10.1016/j.pcl.2014.04.003
- Monaghan, J., Channell, K., McDowell, D., & Sharma, A. K. (2005). Improving patient and career communication, multidisciplinary team working and goal-setting in stroke rehabilitation. Clinical Rehabilitation, 19(2), 194–199. https://doi.org/10.1191/0269215505cr837oa
- Monash, B. (2017). What’s the purpose of rounds? A qualitative study examining the perceptions of faculty and students. Journal of Hospital Medicine, 12(11). https://doi.org/10.12788/jhm.2835
- Monash, B., Najafi, N., Mourad, M., Rajkomar, A., Ranji, S. R., Fang, M. C., Glass, M., Milev, D., Ding, Y., Shen, A., Sharpe, B. A., & Harrison, J. D, et al. (2017). Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. Journal of Hospital Medicine, 12(3), 143–149. https://doi.org/10.12788/jhm.2694
- Mork, A., Krupp, A., Hankwitz, J., & Malec, A. (2018). Using kotter’s change framework to implement and sustain multiple complementary ICU initiatives. Journal of Nursing Care Quality, 33(1), 38–45. https://doi.org/10.1097/ncq.0000000000000263
- Moroney, N., & Knowles, C. (2006). Innovation and teamwork: introducing multidisciplinary team ward rounds. Nursing Management (Harrow, London, England: 1994), 13(1), 28–31. https://doi.org/10.7748/nm2006.04.13.1.28.c2047
- Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E, et al. (2018). Systematic review or scoping review? guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. https://doi.org/10.1186/s12874-018-0611-x
- Nayfeh, A., & Fowler, R. A. (2020). Understanding patient- and hospital-level factors leading to differences, and disparities, in critical care. American Journal of Respiratory and Critical Care Medicine, 201(6), 642–644. https://doi.org/10.1164/rccm.202001-0116ED
- Nelson, E. C., Batalden, P. B., & Godfrey, M. M. (Eds.). (2007). Quality by design: A clinical microsystems approach (1st ed.). Jossey-Bass.
- O’Donnell, B., & Gupta, V. (2020). Continuous quality improvement. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK559239/.
- O’Leary, K. J., Haviley, C., Slade, M. E., Shah, H. M., Lee, J., & Williams, M. V, et al. (2011). Improving teamwork: Impact of structured interdisciplinary rounds on a hospitalist unit. Journal of Hospital Medicine, 6(2), 88–93. https://doi.org/10.1002/jhm.714
- O’Leary, K. J., Killarney, A., Hansen, L. O., Jones, S., Malladi, M., Marks, K., & Shah, M., & H, et al. (2016). Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Quality & Safety, 25(12), 921–928. https://doi.org/10.1136/bmjqs-2015-004561
- Okere, A. N., Renier, C. M., & Willemstein, M. (2016). Comparison of a pharmacist-hospitalist collaborative model of inpatient care with multidisciplinary rounds in achieving quality measures. American Journal of Health-System Pharmacy, 73(4), 216–224. https://doi.org/10.2146/ajhp150225
- Opper, K., Beiler, J., Yakusheva, O., & Weiss, M. (2019). Effects of implementing a health team communication redesign on hospital readmissions within 30 days. Worldviews on Evidence-Based Nursing, 16(2), 121–130. https://doi.org/10.1111/wvn.12350
- Oshimura, J. M., Downs, S. M., & Saysana, M. (2014). Family-centered rounding: Can it impact the time of discharge and time of completion of studies at an academic children’s hospital?. Hospital Pediatrics, 4(4), 228–232. https://doi.org/10.1542/hpeds.2013-0085
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Palokas, J. M., Northington, L., Wilkerson, R. R., & Boss, B. J. (2014). An interactive evaluation of patient/family centered rounds on pediatric inpatient units. Journal of Pediatric Nursing, 30(4), e9–e15. https://doi.org/10.1016/j.pedn.2014.11.005
- Pannick, S., Davis, R., Ashrafian, H., Byrne, B. E., Beveridge, I., Athanasiou, T., Wachter, R. M., & Sevdalis, N, et al. (2015). Effects of interdisciplinary team care interventions on general medical wards: A systematic review. JAMA Internal Medicine, 175(8), 1288–1298. https://doi.org/10.1001/jamainternmed.2015.2421
- Peters, M. D., Godfrey, C. M., McInerney, P., Baldini Soares, C., Khali, H., & Parker, D, et al. (2017). Chapter 11: Scoping reviews. In E. Aromataris & Z. Munn (Eds.), Joanna Briggs Institute reviewer’s manual. https://reviewersmanual.joannabriggs.org/
- Powell, B. J., Fernandez, M. E., Williams, N. J., Aarons, G. A., Beidas, R. S., Lewis, C. C., McHugh, S. M., & Weiner, B. J, et al. (2019). Enhancing the impact of implementation strategies in healthcare: A research agenda. Frontiers in Public Health, 7, 3. https://doi.org/10.3389/fpubh.2019.00003
- Proctor, E., Silmere, H., Raghavan, R., Hovmand, P., Aarons, G., Bunger, A., Griffey, R., & Hensley, M, et al. (2011). Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health, 38(2), 65–76. https://doi.org/10.1007/s10488-010-0319-7
- Rappaport, D. I., Cellucci, M. F., & Leffler, M. G. (2010). Implementing family-centered rounds: pediatric residents’ perceptions. Clinical Pediatrics, 49(3), 228–234. https://doi.org/10.1177/0009922809346568
- Ratelle, J. T., Sawatsky, A. P., Kashiwagi, D. T., Schouten, W. M., Erwin, P. J., Gonzalo, J. D., Beckman, T. J., & West, C. P, et al. (2018). Implementing bedside rounds to improve patient-centred outcomes: A systematic review. BMJ Quality & Safety, 28(4). https://doi.org/10.1136/bmjqs-2017-007778
- Redley, B., Campbell, D., Stockman, K., & Barnes, S. (2020). Mixed methods quality evaluation of structured interprofessional medical ward rounds. Internal Medicine Journal, 50(2), 222–231. https://doi.org/10.1111/imj.14330
- Reeves, S., Clark, E., Lawton, S., Ream, M., & Ross, F. (2017a). Examining the nature of interprofessional interventions designed to promote patient safety: A narrative review. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 29(2), 144–150. https://doi.org/10.1093/intqhc/mzx008
- Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017b). Interprofessional collaboration to improve professional practice and healthcare outcomes. The Cochrane Database of Systematic Reviews, 6, CD000072. https://doi.org/10.1002/14651858.CD000072.pub3
- Rosen, P., Stenger, E., Bochkoris, M., Hannon, M. J., & Kwoh, C. K. (2009). Family-centered multidisciplinary rounds enhance the team approach in pediatrics. Pediatrics, 123(4), e603–8. https://doi.org/10.1542/peds.2008-2238
- Rotter, T., Plishka, C., Lawal, A., Harrison, L., Sari, N., Goodridge, D., Flynn, R., Chan, J., Fiander, M., Poksinska, B., Willoughby, K., & Kinsman, L, et al. (2019). What is lean management in health care? development of an operational definition for a cochrane systematic review. Evaluation & the Health Professions, 42(3), 366–390. https://doi.org/10.1177/0163278718756992
- Roussel, M. G., Gorham, N., Wilson, L., & Mangi, A. A. (2013). Improving recovery time following heart transplantation: The role of the multidisciplinary health care team. Journal of Multidisciplinary Healthcare, 6, 293–302. https://doi.org/10.2147/jmdh.S31457
- Saint, S., Fowler, K. E., Krein, S. L., Flanders, S. A., Bodnar, T. W., Young, E., & Moseley, R. H, et al. (2013). An academic hospitalist model to improve healthcare worker communication and learner education: Results from a quasi-experimental study at a veterans affairs medical center. Journal of Hospital Medicine, 8(12), 702–710. https://doi.org/10.1002/jhm.2105
- Scarsi, K. K., Fotis, M. A., & Noskin, G. A. (2002). Pharmacist participation in medical rounds reduces medication errors. American Journal of Health-System Pharmacy, 59(21), 2089–2092. https://doi.org/10.1093/ajhp/59.21.2089
- Schatzki, T. R. (2002). The site of the social: A philosophical account of the constitution of social life and change. Penn State University Press.
- Schiller, W. R., & Anderson, B. F. (2003). Family as a member of the trauma rounds: A strategy for maximized communication. Journal of Trauma Nursing, 10(4), 93–101. https://doi.org/10.1097/00043860-200310040-00001
- Seigel, J., Whalen, L., Burgess, E., Joyner, B. L., Purdy, A., Saunders, R., & Willis, T. S, et al. (2014). Successful implementation of standardized multidisciplinary bedside rounds, including daily goals, in a pediatric ICU. Joint Commission Journal on Quality and Patient Safety, 40(2), 83–90. https://doi.org/10.1016/S1553-7250(14)40010-2
- Sharma, H., & Verma, S. (2019). Is positive publication bias really a bias, or an intentionally created discrimination toward negative results?. Saudi Journal of Anaesthesia, 13(4), 352–355. https://doi.org/10.4103/sja.SJA_124_19
- Sharma, U., & Klocke, D. (2014). Attitudes of nursing staff toward interprofessional in-patient-centered rounding. Journal of Interprofessional Care, 28(5), 475–477. https://doi.org/10.3109/13561820.2014.907558
- Shaughnessy, L., & Jackson, J. (2015). Introduction of a new ward round approach in a cardiothoracic critical care unit. Nursing in Critical Care, 20(4), 210–218. https://doi.org/10.1111/nicc.12149
- Shoemaker, P., Tankard, J. W., Jr., & Lasorsa, D. (2004). How to build social science theories. SAGE Books. https://sk.sagepub.com/books/how-to-build-social-science-theories.
- Southwick, F., Lewis, M., Treloar, D., Cherabuddi, K., Radhakrishnan, N., Leverence, R., Xiaoxia, H., & Cottler, L, et al. (2014). Applying athletic principles to medical rounds to improve teaching and patient care. Academic Medicine, 89(7), 1018–1023. https://doi.org/10.1097/ACM.0000000000000278
- StataCorp. (2017). Stata Statistical Software: Release 15. [Computer software]. College Station, TX: StataCorp LLC.Microsoft Excel Online. (n.d.). Spreadsheet Software. [Computer software]. https://www.microsoft.com/en-us/microsoft-365/excel
- Stein, J., Payne, C., Methvin, A., Bonsall, J. M., Chadwick, L., Clark, D., Castle, B. W., Tong, D., & Dressler, D. D, et al. (2015). Reorganizing a hospital ward as an accountable care unit. Journal of Hospital Medicine, 10(1), 36–40. https://doi.org/10.1002/jhm.2284
- Sunkara, P. R., Islam, T., Bose, A., Rosenthal, G. E., Chevli, P., Jogu, H., Tk, L. A., Huang, -C.-C., Chaudhary, D., Beekman, D., Dutta, A., Menon, S., & Speiser, J. L, et al. (2020). Impact of structured interdisciplinary bedside rounding on patient outcomes at a large academic health centre. BMJ Quality & Safety, 29(7), 569–575. https://doi.org/10.1136/bmjqs-2019-009936
- Taylor, M. J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D., & Reed, J. E, et al. (2014). Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Quality & Safety, 23(4), 290–298. https://doi.org/10.1136/bmjqs-2013-001862
- Thorne, K., Andersson-Gare, B., Hult, H., & Abrandt-Dahlgren, M. (2017). Co-producing interprofessional round work: designing spaces for patient partnership. Quality Management in Health Care, 26(2), 70–82. https://doi.org/10.1097/QMH.0000000000000133
- Timmel, J., Kent, P. S., Holzmueller, C. G., Paine, L., Schulick, R. D., & Pronovost, P. J, et al. (2010). Impact of the comprehensive unit-based safety program (CUSP) on safety culture in a surgical inpatient unit. Joint Commission Journal on Quality and Patient Safety, 36(6), 252–260. https://doi.org/10.1016/S1553-7250(10)36040-5
- Treacy, P. J., Snelling, P., Ragg, J., Carson, P., & O’Rourke, I. (2002). Impact of a multidisciplinary team approach upon patency rates of arteriovenous fistulae. Nephrology, 7(2), 66–71. https://doi.org/10.1046/j.1440-1797.2002.00089.x
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., & Straus, S. E, et al. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Tripathi, S., Arteaga, G., Rohlik, G., Boynton, B., Graner, K., & Ouellette, Y, et al. (2015). Implementation of patient-centered bedside rounds in the pediatric intensive care unit. Journal of Nursing Care Quality, 30(2), 160–166. https://doi.org/10.1097/NCQ.0000000000000107
- Uhlig, P. N., Brown, J., Nason, A. K., Camelio, A., & Kendall, E. (2002). John M. Eisenberg patient safety awards. System innovation: concord hospital. Joint Commission Journal on Quality Improvement, 28(12), 666–672. DOI: 10.1016/s1070-3241(02)28072-4
- Vega, M. W., Juarez, M., Lee, J. Y., Srivaths, P., Williams, E., & Akcan Arikan, A, et al. (2018). Quality improvement bedside rounding audits enhance protein provision for pediatric patients receiving continuous renal replacement therapy. Pediatric Critical Care Medicine?: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 19(11), 1054–1058. https://doi.org/10.1097/PCC.0000000000001698
- Voos, K. C., Ross, G., Ward, M. J., Yohay, A. L., Osorio, S. N., & Perlman, J. M, et al. (2011). Effects of implementing family-centered rounds (FCRs) in a neonatal intensive care unit (NICU). Journal of Maternal-Fetal & Neonatal Medicine, 24(11), 1403–1406. https://doi.org/10.3109/14767058.2011.596960
- Walton, V., Hogden, A., Johnson, J., & Greenfield, D. (2016). Ward rounds, participants, roles and perceptions: literature review. International Journal of Health Care Quality Assurance, 29(4), 364–379. https://doi.org/10.1108/IJHCQA-04-2015-0053
- Weaver, S. J., Dy, S. M., & Rosen, M. A. (2014). Team-training in healthcare: A narrative synthesis of the literature. BMJ Quality & Safety, 23(5), 359–372. https://doi.org/10.1136/bmjqs-2013-001848
- Weaver, S. J., Lubomksi, L. H., Wilson, R. F., Pfoh, E. R., Martinez, K. A., & Dy, S. M, et al. (2013). Promoting a culture of safety as a patient safety strategy: A systematic review. Annals of Internal Medicine, 158(5 Pt. 2), 369–374. https://doi.org/10.7326/0003-4819-158-5-201303051-00002
- Wickersham, A., Johnson, K., Kamath, A., & Kaboli, P. J. (2018). Novel use of communication technology to improve nurse-physician communication, teamwork, and care coordination during bedside rounds. Journal of Communication in Healthcare, 11(1), 56–61. https://doi.org/10.1080/17538068.2018.1431425
- Will, K. K., Johnson, M. L., & Lamb, G. (2019). Team-based care and patient satisfaction in the hospital setting: A systematic review. Journal of Patient-Centered Research and Reviews, 6(2), 158–171. https://doi.org/10.17294/2330-0698.1695
- Wright, S., Bowkett, J., & Bray, K. (1996). The communication gap in the ICU A possible solution. Nursing in Critical Care, 1(5), 241–244. https://pubmed.ncbi.nlm.nih.gov/9594125/
- Wrobleski, D. M., Joswiak, M. E., Dunn, D. F., Maxson, P. M., & Holland, D. E. (2014). Discharge planning rounds to the bedside: A patient- and family-centered approach. MEDSURG Nursing, 23(2), 111–116. https://pubmed-ncbi-nlm-nih-gov.offcampus.lib.washington.edu/24933789/
- Young, E., Paulk, J., Beck, J., Anderson, M., Burck, M., Jobman, L., & Stickrath, C, et al. (2018). Impact of altered medication administration time on interdisciplinary bedside rounds on academic medical ward. Journal of Nursing Care Quality, 32(3), 218–225. https://doi.org/10.1097/NCQ.0000000000000233
- Young, M. P., Gooder, V. J., Oltermann, M. H., Bohman, C. B., French, T. K., & James, B. C, et al. (1998). The impact of a multidisciplinary approach on caring for ventilator-dependent patients. International Journal for Quality in Health Care, 10(1), 15–26. https://doi.org/10.1093/intqhc/10.1.15