ABSTRACT
Done well, ward rounds (WRs) promote effective, safe care and collaboration; but WR quality varies. An improvement-focused appreciative inquiry (AI) into a large intensive care unit’s WR practices identified a pivotal axis of collaboration between the most senior medical role (the consultant) and the bedside nurse (BSN). This paper examines that axis of interprofessional collaboration (IPC) to deepen understanding of its implications. Data included ethnographic observations, interviews, and co-constructed AI with groups of staff. Four key concepts emerged from cyclical interpretive analysis: “need,” “presence,” “ability” and “willingness.” BSNs and consultants needed the interprofessional WR to enable their work; WR effectiveness was affected by whether they were both present, then able and willing to participate in IPC. BSN presence was necessary for effective and efficient IPC between these key roles. Indirect contributions, based on prior exchanges with colleagues or through written notes, reduced the joint problem-solving through discussion and negotiation that characterizes IPC to less efficient asynchronous interprofessional coordination. Factors affecting “presence,” “ability” and “willingness” are discussed alongside potential mitigations and acknowledgment of asymmetric power. Appreciative examination of interprofessional WRs identified mechanisms supporting and undermining effective WR IPC and the centrality of consultants’ and BSNs’ collaboration.
Introduction
During ward-rounds (WRs) healthcare professionals (HCPs) meet at patients’ bedsides to review and plan care. Done well, the WR discussion and decision-making support timely, safe and effective progression of care and include patients’ perspectives (although in intensive care, many patients will be unable to contribute to the WR conversation). WRs are complex social processes that demand clinical knowledge and acumen, alongside effective prioritization and communication. WRs occupy a substantial proportion of hospital HCPs’ time (Caldwell, Citation2014). This represents a major investment of human and financial resources, yet there are concerns about ineffective WRs and ritualistic WRs with low engagement from some HCPs (Francis, Citation2013; Royal College of Physicians and Royal College of Nursing [RCP & RCN], Citation2012).
We conducted an appreciative inquiry (AI) into WR practices in a large adult critical care unit (ACCU). This highlighted the importance of interprofessional interactions between the most senior HCP and HCPs with considerably less professional status and autonomy, here, the consultant physician leading the WR during its journey around the unit and BSNs who remain with their patients. Critical care BSNs range from junior nurses (who may be recently qualified and/or recently arrived in the UK) to very experienced and senior nurses. Each BSN follows a “management plan” for each patient, which includes priorities for the next 24 hours and attention to longer-term goals. This is reviewed, updated and agreed at the daily consultant-led interprofessional WR. Interprofessional WR discussion produces an updated clinical opinion and shapes the plan, which is recorded, and the consultant’s signature is added (identifying legal responsibility). Consultant-approved urgent updates to the management plan can occur between WRs if clinical information warrants additional consultant intervention.
This paper explores the conditions supporting effective WR interaction between BSNs and consultants using four inductively identified analytical categories: need, presence, willingness and ability. The findings of the collaborative AI with front-line clinicians confirmed that both consultants and BSNs felt strongly that they needed the WR discussion and decision-making. However, the AI also identified several factors which reduce BSNs’ ability to be present for WR discussions, and their willingness and ability to contribute. Whilst some factors are difficult to address (although nonetheless important to describe), other factors are readily addressable through improvement-focused AI. This paper describes a selection of factors which support (or inhibit) BSN-consultant discussion during WRs. The quality improvements developed during this study, and a wider range of findings, are described elsewhere (Merriman, Citation2020).
Background
Many studies have examined the structure and frequency of WRs, often largely quantitatively or through the lens of a single profession. Holistic and collaborative studies, like the one reported here, are much less common. Authors’ concerns include the persistence of ritual centered on medical discourse and hierarchical control, despite extensive changes in healthcare services and professional practice (Paradis et al., Citation2015; Prystajecky et al., Citation2017). Historically, hierarchical control may have been expected and accepted. However, the importance and benefits of interprofessional collaboration (IPC) have been highlighted for many years (Reeves et al., Citation2013) and researchers have advocated interprofessional WRs to enhance the quality of care and increase communication and knowledge diffusion among team members (Paradis et al., Citation2015).
Principles for Best Practice for Conducting Wardrounds, jointly published by medical and nursing professional bodies (RCP & RCN, Citation2012), concluded that to support safe care WRs should be interprofessional and viewed by HCPs as having central importance in the working day. Francis (Citation2013) linked active involvement of BSNs in WRs to high quality patient care, arguing their absence has clear consequences for communication, WR efficiency and patient safety. However, professional, organizational, historical and cultural factors can impede IPC, particularly nurse-consultant collaboration (Reeves et al., Citation2014). Worryingly, studies of nurse-consultant interactions and collaboration during WRs (Liu et al., Citation2013; Manias & Street, Citation2001; Weber et al., Citation2007) suggest that if nurses perceive that their views are not being heard, or they view WRs as ritualistic, they may disengage from this social process whilst remaining physically present, or even absent themselves. Other WR research highlights the dominance of consultants in decision making and argues that consultants should relinquish some control of the WR (Coombs & Ersser, Citation2004) and nurses should develop greater assertiveness and actively participate in discussions and decision making (Busby & Gilchrist, Citation1992; Paradis et al., Citation2015).
Study site
A large, modern, purpose-built ACCU in England, with 44 beds in eight 4-bedded bays and 12 single rooms, 28 intensive care beds for Level 2 and 3 patients,Footnote1 one BSN to one patient as per guidelines (Faculty of Intensive Care Medicine, The and Intensive Care Society [FICM & ICS], Citation2015), and 16 “high-dependency” beds (one BSN between two or three patients, depending on patients’ clinical acuity).
The ACCU core team was 48 doctors (16 consultants and 32 doctors known as ‘trainees’Footnote2), the full-time equivalent (FTE) of 166 nurses (including over 150 FTE BSNs), pharmacists (3FTE) and unregistered support staff such as health care assistants and technicians. HCPs from other parts of the hospital had time allocated to ACCU, particularly physiotherapists and occupational therapists. Specialist teams visited patients according to need (e.g., trauma or neurosurgery specialists; dieticians).
The most important forum for clinical review and care planning was the daily interprofessional WRs, starting at 10am. The unit’s size meant a single WR could not review every patient within a reasonable time, so three simultaneous WRs ran, each expected to last 120–150 minutes; two covered half the intensive care beds each, one covered the high-dependency area. The core touring WR team comprised: a consultant (leading the WR), a “nurse-in-charge” (a senior nurse who could co-ordinate and prioritize the allocation of resources, including ward-based staff), trainees and a pharmacist. Other HCPs joined according to need and availability. Patient reviews lasted 10–15 minutes. Information and questions from different sources and perspectives were shared, discussed briefly, and used to inform agreed and documented plans for the next 24 hours. Work was divided between the professions and services needed for each patient’s care.
Before the 10am WR, medical trainees shared responsibility for visiting and provisionally reviewing every patient; performing examinations, checking test results, and interacting with BSNs and other HCPs. BSNs also reviewed their patient(s), completing documentation and noting matters to be raised with the WR team.
Methods
Methodology
We used Appreciative Inquiry (AI) (Cooperrider et al., Citation2008) in partnership with the Unit’s HCPs to draw out factors which supported high quality WRs.
AI seeks to avoid the energy-sapping process of cataloging deficiencies in a social process or organizational system, then finding a solution for each deficiency (Ludema & Fry, Citation2008). Instead, AI generates motivation and change by initiating positive dialogue and analysis among people who are stakeholders in the process or system, often supported by facilitators or researchers. AI has four stages (discovery, dream, design and destiny), focusing first on appreciative questions, such as:
What does it look like when things are going really well?
What is happening that enables things to go really well?
Once provisional understanding of how something functions emerges from dialogue, those engaged in AI become ready to address questions such as:
How can we make more things go well, more of the time?
What do we want things to look like?
How can we move toward that?
The collaborative, improvement-focused AI was supported by regular discussions with an interprofessional steering group of mainly senior clinicians from the study site: five doctors, seven nurses, a pharmacist and physiotherapist. It met five times over 19 months, before, during and after data collection. AI discussions with BSNs occurred in naturally occurring “nursing team days” (NTDs), which supported professional development and team building.
Ethical considerations
Ethical approval for the study was granted after scrutiny by the University hosting CM’s doctoral research (Merriman, Citation2020) and the NHS hospital trust in which the ACCU is located. The main ethical considerations were that the study should not jeopardize patient care or confidentiality, it should enable genuine choice for potential participants and obtain informed consent.
Data collection
Multiple data collection methods were used to develop a rich understanding of WR practices. First, CM conducted 40.2 hours of marginally participant ethnographic observations (Atkinson, Citation2001) of 194 patient reviews during 16 WRs led by 14 different critical care consultants. CM works as a senior critical care nurse in a different city to the study site. This professional experience enabled her to join the WR and make insightful observations without distracting attention from clinical care. This strength was balanced by the need to maintain a researcher’s gaze, rather than a clinician’s gaze. Doctoral supervision and the non-clinical gaze of DF helped ensure this. Observations occurred throughout the week, Monday-Friday. Weekends were omitted on the advice of the Steering Group, since staffing and service delivery were slightly different. The observation template for detailed “field notes” included space to note behaviors that suggested researcher reactivity (Bryman, Citation2008). Some quantifiable matters were noted, e.g., the start time and duration of the WR, how many HCPs participated (noting professions) and if BSNs were present. Brief informal conversations with HCPs helped clarify understanding of what had been seen. Augmenting these, seven HCPs (five consultants, one pharmacist, one nurse) contributed interviews (20–40 minutes, audio recorded, fully transcribed).
After developing preliminary understanding through WR observations, CM led AI whole-group discussions at three NTDs to explore perceptions of current WR practices and develop suggestions for improvement. A brief presentation of selected preliminary findings was used to focus part of the discussion. All 35 participants were BSNs and some also performed the nurse-in-charge role. They ranged in experience from newly qualified to extensive critical care experience). When large groups were subdivided to increase opportunities to contribute, written notes were collected from each subgroup to supplement CM’s field notes. Thus, NTDs included elements of “respondent validation” and generated further data for analysis (Pope & Mays, Citation2006).
Data analysis
Data analysis was inductive, following the interpretivist paradigm (Bryman, Citation2008). First, we analyzed different types of data separately, then each analysis was interrogated from the perspective of the others to create a holistic understanding. For example, preliminary findings from ethnographic observations were placed in the context of the quantitative data and also compared with interview transcripts to guide interpretation. Field notes and interview transcripts were coded using NVivo 10 software. Categories and themes were identified. Rich descriptions of WR processes were developed. SPSS software was used to summarize and explore numerical and categorical data in ways that helped to illuminate and challenge the emerging qualitative analysis. CM and DF worked cyclically, separately and together, using the AI framework to catalyze findings shaped by AI questions (see methodology above). This highlighted the importance of WR IPC between BSNs and consultants, prompting the focus of this paper. The iterative analytic process continued while we developed and checked the findings. This included a deliberate search for disconfirming cases (Miles et al., Citation2014) and respondent validation of emergent findings with the steering group and individuals, at NTDs and a senior managers’ meeting.
Findings
Study participants considered the observed WRs typical of their daily experience. There were very few examples of researcher reactivity and most were slightly exaggerated behavior, showing the participant knew the correct thing to do and ensuring CM noticed this. The reactivity subsided quickly as participants’ attention became focused on the complex business of the WR.
A good WR for this ACCU started close to 10am, was well focused, completed in a timely fashion and had clear evidence of IPC involving all members, but particularly the consultant and BSN. Four key concepts “need,” “presence,” “ability” and “willingness,” emerged from cycles of analysis and interpretation; these support and enable “good” WRs. BSNs and consultants needed the interprofessional WR to review and plan care, and WR effectiveness was affected by whether both were present, then able and willing to participate in WR IPC. The WR in the study setting was defined by the presence of a consultant. Consultants were able and willing to lead WRs. BSN presence was strongly affected by consultants’ (passive or active) decisions. When present, BSNs’ ability and willingness to contribute to the WR was affected by cultural expectations, consultants’ behavior and BSN’s self-efficacyFootnote3.
Need
The interprofessional WR supported consultants’ and BSNs’ joint and profession-specific care and responsibilities. The consultant needed to obtain information about the current situation and progress of each patient, and the progress and outcomes of previously planned care. The WR process expected a trainee to have reviewed the patient before the WR and thus possess the most recent medical overview. However, the BSN possessed the most up-to-date and detailed knowledge of the patient’s (often changing) condition. Almost invariably, consultants wanted BSNs’ current and detailed knowledge to inform an updated clinical opinion and development of the day’s agreed management plan for each patient.
I’m well aware they’re going to be there for twelve hours and I’m going to be there for twenty minutes, ten minutes, half an hour maybe. So I’m going to be there for a snapshot … And ‘Sod’s Law’Footnote4 is that, when I arrive, the patient’s not agitated, the patient’s not moving around, there’s no issue. As soon as I go, the door closes, they’re ripping everything out and there’s a problem, or they’re de-saturating. (Consultant Interview)
BSNs needed the WR to address questions or concerns about their patient’s care, allocate work to be completed by the WR team, update and document the management plan, and check shared understanding of the plan. This supported all HCPs to provide timely and effective care. It enabled BSNs to prioritize, plan and coordinate care. BSNs became anxious if they felt the wait for the updated management plan was too long. They had to decide whether the patient’s condition warranted ringing or bleeping a member of the WR team for guidance or intervention, thus interrupting the WR. They knew that interrupting the WR had negative consequences for its timely progression and completion. This involved weighing risks and inefficiencies, for example, important interventions could be missed or delayed until the next day, particularly interventions requiring hospital teams which do not operate 24/7. Bedside nursing within an ACCU, particularly one with many single rooms, is quite isolating. BSNs did not have a holistic sense of the activity and acuity across the unit. Furthermore, the BSN workforce in this ACCU mainly comprised junior nurses and many were recently qualified or had recently arrived in the UK. This fueled anxiety, a sense of powerlessness and desire for a reasonably predictable WR arrival.
Presence
The presence of the patient’s BSN when the touring WR team reviewed a patient was a necessary antecedent for IPC between the key roles of consultant and BSN. Consultant presence was ensured. If the consultant was at a meeting or called away to an emergency, the WR did not start on time, or if underway, halted until the consultant could resume. In contrast, if the BSN was not present when the WR team arrived to review a patient, the review went ahead, thus excluding the bedside nurse from direct participation in that day’s WR IPC.
If the BSN was not present, the nurse-in-charge within the touring WR team had the opportunity to provide limited nursing input but was unlikely to have been briefed by the BSN. Sometimes the BSN for a neighboring patient contributed a little, but they lacked detailed knowledge of the absent nurse’s patient. Theoretically, the trainee who had reviewed the patient earlier could raise matters highlighted by the BSN during the pre-WR review, this was not observed by CM or mentioned by study participants. Thus, the trainee-BSN axis of IPC did not mitigate BSN absence during the WR updating of management plans. Nevertheless, written notes made by the BSN (e.g., nursing care plans, observation charts) were available for the consultant to review, which consultants often did.
Indirect contributions from bedside nurses, based on prior exchanges with colleagues or through written notes, might be termed asynchronous interprofessional coordination, due to lacking the joint problem-solving through discussion and negotiation that is characteristic of interprofessional collaboration (Reeves et al., Citation2014). Similarly, asynchronous coordination between the consultant and any BSN unable to be present when the WR arrived, relied on BSNs reading and acting upon the written management plan, sometimes augmented by briefing or discussion later, when the nurse-in-charge or trainees left the WR.
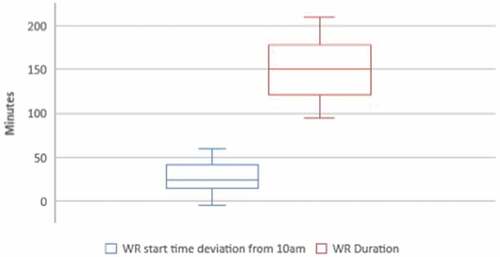
BSNs were present for 145 (75%) of the 194 patient reviews observed. Presence varied between the 16 WRs led by 14 different consultants, range 67%-100%, and was negatively skewed (see and ). Half of WRs achieved BSN presence for over 92% of patient reviews, demonstrating the feasibility of this. Whereas BSN presence varied between 67% and 91% in the other half, with the lowest quarter being most variable (67%-80%). This suggests that a targeted approach to increasing BSN presence at patient reviews would be more efficient than general improvement efforts. We will examine the distribution of WR introductions for BSNs later.
Table 1. Statistics from 16 Ward Rounds (194 patient reviews).
Ability and willingness to be present
Consultants were able and willing to be present during WRs and wanted BSNs to be present, but consultants were not always working in ways that were sufficiently predictable to facilitate BSN presence. and show WR start times from five minutes early to an hour late (mean 25 min late, standard deviation 19 min). Unpredictability was compounded by substantial variation in the pace of the WR (, WR duration range 85–210 min, standard deviation 33 min). Furthermore, 12 of the 16 WRs were halted and resumed, sometimes repeatedly (37 halts, all due to consultant switching attention to another matter, ). Halts were normally just a few minutes, but up to 45 minutes was observed.
Table 2. Summary statistics for timing and pace of 16 WRs.
Table 3. Reasons for WR halts.
Were consultants able and willing to be present to start and complete the WR on schedule, minimizing interruptions? Discussing why WRs started late or overran, consultants identified issues such as: trainees not having reviewed patients, emergencies on the unit, being caught up with other clinical commitments, or their own poor time management (e.g., scheduling activities that clashed with the WR, or prolonged WR teaching). Some said they rarely started at 10am or they made slow progress. It was unusual for a consultant to send a message about a late start to the nurse-in-charge. Some consultants said they could see how late-running WRs may impact on the BSNs’ ability to be present during the WR. Emergencies aside, it was recognized that consultants had substantial autonomy and agency to manage the timing of teaching and most meetings, therefore they were able to avoid disruption to the WR for these reasons. A commitment to this became part of the improvement phase of the appreciative inquiry (see second set of questions in methodology section).
Were BSNs able to be present for WR IPC? They tried but it was tricky. Scheduling personal breaks and work that must be completed away from the bedside around WR participation was largely guesswork, while delaying these could adversely affect care and colleagues. Asking questions or raising concerns after missing the WR review involved similar considerations and anxiety for BSNs as seeking input before the WR arrived (see need section above). No messages were cascaded to BSNs if the WR was starting late, taking longer than usual, or halted. Whilst some consultants mainly led the WR geographically around its section of the unit, others took less predictable routes based on trainees’ (and possibly others’) reports of patient need, and whether trainees had reviewed all patients before the WR. BSNs could usually find out which consultants were leading WRs and those with experience of the consultants’ styles could use this knowledge to refine their estimate of the WR arrival time. Inevitably, BSNs caring for patients later in the WR journey experienced the most uncertainty. shows the BSN was present during most patient reviews. This was partly because in ACCU BSNs are with their patient(s) most of the time, partly because BSNs wanted to be present, if they were able.
Collaborative AI data from NTDs emphasized BSNs’ perceptions that medical colleagues did not realize the impact a delayed or prolonged WR had on nurses’ ability to manage patient care and time effectively. There was a perception of hierarchical “them” (powerful consultants) and “us” (largely powerless BSNs).
We never know if the WR is going to start on time, no one tells us if it is going to be start late or it is taking a long time. It makes it really hard for us to plan our breaks so we can be there for the WR. (NTD)
Consultant interviews and steering group AI discussions supported the BSNs’ perceptions, they acknowledged variation between consultants, unpredictable WR timing and sparse communication about timing. Consultants and BSNs suggested cultural change, developing willingness to start and complete WRs more predictably and communicate delays to BSNs. BSNs felt this would demonstrate that consultants valued BSNs’ presence.
Ability and willingness to participate
When the WR went well the BSN was not only present but willing and able to participate by sharing responsibility for updating the touring WR team with the trainee (verbally and by ensuring records such as fluid balance charts, drug charts and blood results were readily available and up to date), formulating appropriate questions and suggestions for the WR review and actively participating in discussion of management plans. However, BSN participation varied substantially.
A small number of BSNs ignored the touring WR team and continued nursing tasks which could have been paused to participate in the WR, seemingly not willing to participate. A few BSNs were unprepared for the WR, thus not able to participate. Many BSNs would join the WR huddle but barely participate, saying very little (sometimes nothing), mainly speaking only if the consultant asked them for information. Although not exclusively so, the most junior and inexperienced nurses, or nurses whose first language was not English, contributed less to WRs. During AI discussions with nurses CM highlighted that she had observed different levels of contribution from nurses during WRs. These observations resonated with nurses. One group commented:
‘how long the bedside nurse has been working on the unit and language barriers will affect participation in the WR’ (AI NTD)
Recruitment and retention issues meant that many bedside nurses joined the unit less than six months previously and some were very early in their clinical careers. A group of new recruits who were all less than a year post-qualification provided the following feedback:
‘the WR is quite intimidating when you do not have as much knowledge as the medics, this makes is hard to speak up as you do not want to say something that is wrong’ (AI NTD)
International recruitment meant many BSNs had trained outside the UK, the majority in counties where professional cultural norms include less nurse input to interprofessional discussion and decision-making than in the UK. . In addition, AI discussion participants highlighted language barriers several times (steering group, managers, NTD groups). Participants, including BSNs thought some BSNs were not able to participate in the WR because they lacked sufficient experience, confidence or language skills to contribute.
‘Nurse confidence can impact on involvement in the WR … … International nurses are less confident due to language barrier, there are 88 ward nurses where English is not their first language. Processing the communication on the WR and also the written documentation is often difficult and time consuming. Do not want to question as may have misunderstood’ (AI-NTD)
This was contrasted with beside-nurses who were willing and able to participate in the WR, joined the touring WR team and contributed when they judged contribution appropriate. That judgment was twofold: first if they felt they had a pertinent contribution to make (ability) and second, if they felt the consultant leading that WR would be willing to consider this contribution from a BSN (willingness). Consequently, some BSNs reported behaving differently (speaking up or remaining passive) depending upon which consultant was leading the WR.
‘Attitudes of the different consultants will have an impact on how the bedside nurse interacts with the WR’ (AI-NTD)
Observations also noted variation in the skillfulness of beside-nurses’ contributions (ability).
Some consultants encouraged BSNs to participate by introducing the WR to the patient and BSN, asking the BSN to join the WR. This suggests these consultants were willing and able to support BSNs’ WR participation, which was valued:
‘it is nice if the WR Drs acknowledge the bedside-nurse and ask for name, giving them a feeling of ‘participation’ and not merely someone who carries out the orders’ (AI NTD)
BSN presence was noticeably more frequent than introductions from the WR team (see and ). Observations suggested that some BSNs needed this introduction as permission or a prompt to pause nursing tasks and join the WR review. During interviews several consultants expressed frustration that they had to ask some BSNs to join the WR, feeling these nurses were unwilling to give the WR review the priority needed to support safe and timely care. To encourage passive or less confident BSNs to participate, some consultants asked the BSN if they had questions for the WR team and used non-verbal communication (e.g., brief pause, eye contact) to signal the desire for a response. This appeared to give some BSNs the opportunity they needed to interact with the WR. Nevertheless, some patient reviews were concluded without the BSN contributing, despite being present.
The AI process, focused on achieving good WRs more often, developed proposals to support BSNs having a more active role in WRs, supported by a clear communication structure setting expectations that both the consultant and nurse-in-charge would support BSNs’ contributions. A WR standard operating procedure was developed, which included a mnemonic to prompt discussion of the range of issues to be covered in each patient review.
Discussion
WRs require substantial staff and information resources, requiring significant expenditure (Caldwell, Citation2014) and pausing other work. Nevertheless WRs, including regular interprofessional WRs, are considered key to safe, effective, efficient in-patient care (Francis, Citation2013). However, there are concerns about ineffective WRs (Prystajecky et al., Citation2017). Prior research provides limited insights into good WR practices. Many studies are one-dimensional, such as observing whether specific tasks are completed (Dolan & Broadbent, Citation2016; Pitcher et al., Citation2016), which HCPs are present (Herring et al., Citation2011), or studying the contributions or perspectives of one profession (Liu et al., Citation2013). In contrast, this appreciative inquiry developed a richly textured understanding of WRs in the study setting. It highlighted the importance of interaction between the consultant leading the WR and the bedside nurse, roles at different ends of spectrums of professional seniority and power. Both roles were key to delivering a good interprofessional WR. Four key concepts, need, presence, willingness and ability, emerged through inductive analysis.
Both consultants and bedside nurses needed up to date clinical reviews and management plans to support profession-specific and interprofessional care and coordination. In this study, and more widely (Henkin et al., Citation2016), an interprofessional WR was central to this. The presence of the patient’s BSN when the touring WR team reviewed a patient was a necessary antecedent for efficient and effective IPC between the key roles of consultant and BSN. Indirect contributions, based on prior exchanges with colleagues or through written notes, reduced the joint problem-solving through discussion and negotiation that characterizes interprofessional collaboration to asynchronous interprofessional coordination (Reeves et al., Citation2014). This limits the extent of cooperation for shared problem-solving, and almost entirely excludes reflective communication, which Engeström (Citation2008) identified as higher-level forms of collaboration than coordination in his seminal exposition of “knotworking.”
The ability of BSN to be present for WR reviews hinged on predictability of the touring WR’s arrival. Principal factors limiting predictability were delays, interruptions, rerouting and lack of communication about the progress of the WR. Other research has described similar difficulties linked to consultants’ working patterns (Singh et al., Citation2012) or a culture of interruptions (Carroll et al., Citation2008). The persistence of such working patterns is often theorized in terms of power or organizational influences (West et al., Citation2015). This study’s AI approach encouraged examination of the extent to which practices were amenable to change to enable BSN presence more often. Consultants recognized that, whilst there were things beyond their control, they had considerable influence over the WR start time, pace and route, and the power to initiate messages via other team members which could make the WR arrival more predictable for BSNs. Consultants committed to starting the WR on time whenever possible and to better communication of delays and changes. Thus, the AI approach of this study encouraged immediate and achievable improvement efforts, enabling the study to go beyond describing and theorizing problems. Similar approaches are likely to work in other contexts.
Consultants were willing and able to be present to lead the WR; generally, they insisted on it. The power to insist reflects senior doctors’ status and autonomy. The practice of insisting may reflect medical dominance (Paradis et al., Citation2015) and traditional expectations among doctors and other HCPs (Prystajecky et al., Citation2017), which could be reinforced by interpretations of legal and professional accountability. Bedside nurses were willing to be present and tried to plan their work and breaks to ensure this. The unpredictable WR arrival time rendered them less able to be present, even though in critical care BSNs are responsible for one patient (occasionally 2–3) and work at the bedside most of the time. Factors which lessened their ability to be present would have greater impact in settings providing less acute care, which have higher patient-nurse ratios. Indeed, in this study other professions (e.g., pharmacists) found it difficult to discern when they could ensure their presence for patient reviews for which they had contributions.
Whilst beside-nurse presence during the WR review was a necessary antecedent to IPC between the consultant and BNS, it was not sufficient. Some BSNs did not join the WR huddle, others joined but did not contribute. Consultants found this frustrating and most tried to encourage BSN contributions. Earlier research emphasizes the consultant’s authoritative position in starting, leading and directing the WR (Busby & Gilchrist, Citation1992; Shaughnessy & Jackson, Citation2015), and the impacts of variation in consultants’ behaviors on the start time of the WR and collaboration with the BSN (Carroll et al., Citation2008; Manias & Street, Citation2001), mostly attributing this to variation in consultants’ hierarchical behavior. Whilst this study had some similar findings in relation to facilitating bedside nurse presence, maintaining the focus of the WR to support its timely completion and supporting interprofessional discussion, this study’s finding of consultants actively seeking collaboration with BSNs challenges traditional explanations of medical dominance and low regard for nurse input. In this study the majority of consultants wanted and valued BSNs’ insights and invited the BSN to contribute to WR discussions. This finding directs attention to some BSNs’ inability or unwillingness to take up this opportunity for reasons such as lack of knowledge, confidence or language. The extent to which junior nurses have a confident grasp of the clinical knowledge relevant to their patients, and effective communication skills in interprofessional interactions, has been questioned previously (Shaughnessy & Jackson, Citation2015). This suggests they may need closer support from more senior nurses. In the WR context this would be the nurse-in-charge role.
International nurses are a welcome and permanent feature of UK healthcare. Some hospital trusts report as much as 50% of their nursing workforce trained outside of the UK, with most originating from countries where English is not their first language (House of Commons, Health Committee, Citation2018). Research suggests that nurses working toward fluency in the language of the workplace (including technical, formal and colloquial language) may work less efficiently (Germack et al., Citation2015), with many nurses reporting embarrassment (Alexis & Vydelingum, Citation2005), frustration (Taylor, Citation2005), reduced feelings of self-worth and impact on their professional image and relationships with colleagues across the multidisciplinary team (Allan & Westwood, Citation2016). Additionally, there are cultural and professional differences for non-UK trained nurses to overcome. These include differences in expectations about nurses’ contributions (Alexis & Vydelingum, Citation2005; Taylor, Citation2005) and interprofessional communication (Magnusdottir, Citation2005; Tregunno et al., Citation2009). Whilst this has been reported as an enduring problem (O’Brien & Ackroyd, Citation2012), support from colleagues or more formal development could mitigate international nurses’ challenges and help inexperienced nurses irrespective of origin. Otherwise, nurses will miss opportunities to contribute well-focused and insightful observations to WR discussions. This may have serious implications for patient care and patient safety (Francis, Citation2013; RCP & RCN, Citation2012).
Strengths and limitations
Whilst findings from one ACCU may not generalize unproblematically to other ACCUs, and differences will increase in non-ACCU hospital settings with different characteristics, the rich descriptions and appreciative approach of this multimethod study yielded multifaceted insights which may have resonance elsewhere and could be used as a basis for reflection and challenge.
The collaborative improvement-focused appreciative inquiry with front-line clinicians helped to surface and clarify issues and suggest practical improvements. AI acknowledges that different social realities co-exist within groups and enables participants to inspire thoughts and actions that help generate individual, group and organizational “flourishing” (Cooperrider & Srivastva, Citation1987). AI methodology has potential weaknesses and risks, such as under-theorization, difficulty maintaining a positive stance or dismissing problems (Ludema & Fry, Citation2008; McIntosh et al., Citation2013). In this study activity theory (Engeström, Citation2015) supported data analysis and theorization.
In the data set used for this paper CM conducted all the ethnographic observations. This single perspective was augmented and challenged through brief conversations with WR participants, semi-structured interviews and through discussion of observations during appreciative inquiry with multiple groups of clinicians over several months. In the wider study (Merriman, Citation2020) ACCU clinical staff conducted the next phase of 50 WR observations, which received the same cycles of analysis by CM and DF alongside AI discussions with clinicians. Finally, CM observed a further 12 WRs. The breadth of data sources and these subsequent two phases helped us to hone the analysis presented here and to mitigate what would otherwise be weaknesses of a single observer.
Conclusion
Earlier research identified a range of problems limiting the effectiveness of WRs but research and responses are mainly deficit-focused and often one-dimensional. This study’s holistic appreciative inquiry into consultant-led interprofessional WR practices in a large ACCU confirmed their importance and focused attention on the axis of IPC between BSNs and consultants. These HCPs need to collaborate to optimize patient care and progress their separate and joint work. An interprofessional WR can meet their needs effectively, providing both are present, otherwise collaboration is reduced to asynchronous coordination and lacks the depth of shared problem-solving and understanding which make IPC more effective. Ensuring the presence of the BSN requires greater predictability of WR arrival. The variable pace of WRs, interruptions, re-routing and, to a lesser extent late starts, all rendered WR arrival at a bed-space difficult to predict, particularly toward the end of the WR. However, the AI generated a range of achievable and relatively small changes that would support the joint presence of consultants and BSNs. These were predominantly within the control of consultants and centered on better communication and more mindful time-keeping. Joint presence was not enough, consultants and BSNs also needed to be willing and able to collaborate. This study found that most consultants wanted and tried to encourage IPC with BSNs (some more effectively than others). Inhibiting factors for BSNs included challenges relating to cultural expectations, clinical knowledge, language and confidence. Beyond BSNs’ individual characteristics, confidence and ability to contribute was influenced by the approach of the consultant.
Declarations
This study was not supported by grant funding. The authors have not benefited financially from this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Clair Merriman
Dr Clair Merriman is a Principal Lecturer at Oxford Brookes University and Post Doctoral Nursing Researcher at Oxford University Hospital NHS Foundation Trust. Her interests include critical care, workforce development , interprofessional collaboration, workplace learning and learning through simulated professional practice, all of which support patient safety and the quality of working lives.
Della Freeth
Professor Della Freeth is Executive Director of Education at the Royal College of Physicians and honorary Professor of Professional Education in the School of Medicine & Dentistry at Queen Mary University of London. Her academic and development interests centre on workforce development needs, credentialling, interprofessional collaboration, workplace learning and learning through simulated professional practice, all of which support patient safety and the quality of working lives.
Notes
1. Level 3 patients require advanced respiratory support alone or monitoring and support for two or more organ systems. Level 2 patients require detailed observation or intervention, including support for a single failing organ system or post-operative care, and include those “stepping down” from higher levels of care. (Faculty of Intensive Care Medicine, The and Intensive Care Society, Citation2015).
2. ACCU “trainees” are qualified doctors, participating in Internal Medicine Training Specialty Training before becoming eligible to apply for consultant posts.
3. Apart from very minor editing for clarity or readability, participants words are reproduced in quotations in preference to “tidying up” spoken language so that it resembles written language.
4. Colloquial: If something can go wrong it will.
References
- Alexis, O., & Vydelingum, V. (2005). The experiences of overseas black and minority ethnic registered nurses in an English hospital: A phenomenological study. Journal of Research in Nursing, 10(4), 459–472. https://doi.org/10.1177/174498710501000408
- Allan, H., & Westwood, S. (2016). Non-European nurses’ perceived barriers to UK nurse registration. Nursing Standard, 30(37), 45–51. https://doi.org/10.7748/ns.30.37.45.s41
- Atkinson, P. (2001). Handbook of ethnography. SAGE.
- Bryman, A. (2008). Social research methods (3rd ed.). Oxford University Press.
- Busby, A., & Gilchrist, B. (1992). The role of the nurse in the medical ward round. Journal of Advanced Nursing, 17(3), 339–346. https://doi.org/10.1111/j.1365-2648.1992.tb01912.x
- Caldwell, G. (2014). The importance of wardrounds. Retrieved 4 April, 2014, from https://www.dropbox.com/s/tzep6wa8sw4ik0b/The%20Importance%20of%20Ward%20Rounds%20plus%20appendices.pdf
- Carroll, K., Iedema, R., & Kerridge, R. (2008). Reshaping ICU ward round practices using video-reflexive ethnography. Qualitative Health Research, 18(3), 380–390. https://doi.org/10.1177/1049732307313430
- Coombs, M., & Ersser, S. J. (2004). Medical hegamoney in decision-making-a barrier to interdisiplinary working in intensive care? Journal of Advanced Nursing, 46(3), 245–252. https://doi.org/10.1111/j.1365-2648.2004.02984.x
- Cooperrider, D & Srivastva, s. (1987). APPRECIATIVE INQUIRY IN ORGANIZATIONAL LIFE Research in Organizational Change and Development, Vol.1, pages 129-169. https://www.oio.nl/wp-content/uploads/APPRECIATIVE_INQUIRY_IN_Orgnizational_life.pdf
- Cooperrider, D. L., Whitney, D. K., & Stavros, J. M. (2008). Appreciative inquiry handbook: For leaders of change (2nd ed.). Crown Custom Publishing.
- Dolan, R., & Broadbent, P. (2016). A quality improvement project using a problem based post take ward round proforma based on the SOAP acronym to improve documentation in acute surgical receiving. Annals of Medicine and Surgery, 5, 45–48. https://doi.org/10.1016/j.amsu.2015.11.011
- Engeström, Y. (2008). From teams to knots: Activity-theoretical studies of collaboration and learning at work. Cambridge University Press.
- Engeström, Y. (2015). Learning by expanding: An activity-theoretical approach to developmental research (2nd ed.). Cambridge University Press.
- Faculty of Intensive Care Medicine, The and Intensive Care Society. (2015). Guidelines for the provision of intensive care services. Accessed January 2016, from file:///C:/Users/James/Downloads/GPICS.pdf
- Francis, R. (2013) Report of the mid staffordshire NHS foundation trust public inquiry. Retrieved January 2014, from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/279124/0947.pdf
- Germack, H. D., Griffiths, P., Sloane, D. M., Rafferty, A. M., Ball, J. E., & Aiken, L. H. (2015). Patient satisfaction and non-UK educated nurses: A cross-sectional observational study of english national health service hospitals. BMJ Open, 5(12), e009483. https://doi.org/10.1136/bmjopen-2015-009483
- Henkin, S., Chon, T. Y., Christopherson, M. L., Halvorsen, A. J., Worden, L. M., & Rattle, J. T. (2016). Improving nurse-physician teamwork through interprofessional bedside rounding. Journal of Multidisciplinary Healthcare, 9, 201–205. doi: 10.2147/JMDH.S106644
- Herring, R., Desai, T., & Caldwell, G. (2011). Quality and safety at the point of care: How long should a ward round take? Clinical Medicine, 11(1), 20–22. https://doi.org/10.7861/clinmedicine.11-1-20
- House of Commons, Health Committee (2018) The Nursing Workforce. Second Report of Session 2017-19. Retrieved January 4, 2019, from https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/353/353.pdf
- Liu, W., Manias, E., & Gerdtz, M. (2013). Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health (United Kingdom), 17(2), 113–134. DOI: 10.1177/1363459312447257
- Ludema, J., & Fry, R. (2008). The practice of appreciative inquiry. In P. Reason & H. Bradbury (Eds.), The SAGE handbook of action research participative inquiry and practice (pp. 280–318). SAGE.
- Magnusdottir, H. (2005). Overcoming strangeness and communication barriers: A phenomenological study of becoming a foreign nurse. International Nursing Review, 52(4), 263–269. https://doi.org/10.1111/j.1466-7657.2005.00421.x
- Manias, E., & Street, A. (2001). Nurse-doctor interactions during critical care ward rounds. Journal of Clinical Nursing, 10(4), 442–450. https://doi.org/10.1046/j.1365-2702.2001.00504.x
- McIntosh, P., Freeth, D., & Berridge, E. J. (2013). Supporting accomplished facilitation: Examining the use of appreciative inquiry to inform the development of learning resources for medical educators. Educational Action Research, 21(3), 376–391. https://doi.org/10.1080/09650792.2013.815044
- Merriman, C. (2020). ‘What are the components of a ‘good’ ward round in a large critical care unit and how can we make them happen more often? An Appreciative Inquiry Study [Unpublished PhD Thesis]. Queen Mary University.
- Miles, M. B., Saldaña, J., & Huberman, A. M. (2014). Qualitative data analysis: A methods sourcebook, Edition 3. SAGE.
- O’Brien, T., & Ackroyd, S. (2012). Understanding the recruitment and retention of overseas nurses: Realist case study research in national health service hospitals in the UK. Nursing Inquiry, 19(1), 39–50. https://doi.org/10.1111/j.1440-1800.2011.00572.x
- Paradis, E., Leslie, M., & Gropper, M. (2015). Interprofessional rhetoric and operational realities: An ethnographic study of rounds in four intensive care units. Advances in Health Sciences Education, 21(4), 735–748. https://doi.org/10.1007/s10459-015-9662-5
- Pitcher, M., Lin, J. T., Thompson, G., Tayaran, A., & Chan, S. (2016). Implementation and evaluation of a checklist to improve patient care on surgical ward rounds. ANZ Journal of Surgery, 86(5), 356–360. https://doi.org/10.1111/ans.13151
- Pope, C., & Mays, N. (2006). Qualitative research in health care (3rd ed.). Blackwell; London: BMJ Books.
- Prystajecky, M., Lee, T., Abonyi, S., Perry, R., & Ward, H. (2017). A case study of healthcare providers’ goals during interprofessional rounds. Journal of Interprofessional Care, 31(4), 463–469. https://doi.org/10.1080/13561820.2017.1306497
- Reeves, S., McMillan, S. E., Kachan, N., Paradis, E., Leslie, M., & Kitto, S. (2014). Interprofessional collaboration and family member involvement in intensive care units: Emerging themes from a multi-sited ethnography. Journal of Interprofessional Care, 29(3), 230–237. https://doi.org/10.3109/13561820.2014.955914
- Reeves, S., Perrier, L., Goldman, J., Freeth, D., & Zwarenstein, M. (2013). Interprofessional education: Effects on professional practice and healthcare outcomes (update) (Vol. Issue 3. Art. No.: CD002213). Cochrane Database of Systematic Reviews.
- Royal College of Physicians and Royal College of Nursing. (2012). Ward rounds in medicine-best practice guidelines. RCP.
- Shaughnessy, L., & Jackson, J. (2015). Introduction of a new ward round approach in a cardiothoracic critical care unit. Nursing in Critical Care, 20(4), 210–218. https://doi.org/10.1111/nicc.12149
- Singh, S., Lipscomb, G., Padmakumar, K., Ramamoorthy, R., Ryan, S., Bates, V., Crompton, S., Dermody, E., & Moriarty, K. (2012). Republished: Daily consultant gastroenterologist ward rounds: Reduced length of stay and improved inpatient mortality. Postgrad Med J, 88(1044), 583–587.
- Taylor, B. (2005). The experiences of overseas nurses working in the NHS: Results of a qualitative study. Diversity in Health and Social Care, 2, 17–27.
- Tregunno, D., Peters, S., Campbell, H., & Gordon, S. (2009). International nurse migration: U-turn for safe workplace transition. Nursing Inquiry, 16(3), 182–190. https://doi.org/10.1111/j.1440-1800.2009.00448.x
- Weber, H., Stockli, M., Nubling, M., & Langewitz, W. A. (2007). Communication during ward rounds in internal medicine. An analysis of patient-nurse-physician interactions using RIAS. Patient Education and Counseling, 67(3), 343–348. https://doi.org/10.1016/j.pec.2007.04.011
- West, M. A., Armit, K., Loewenthal, L., Eckert, R., West, T., & Lee, A. (2015). Leadership and leadership development in health care: The evidence base. FMLM/The King’s Fund/CCL.