ABSTRACT
Interprofessional education (IPE) often uses collaborative learning for better teamwork among multiple professions. Its theoretical background is social interdependence theory (SIT), and positive interdependence is key for successful collaborative learning. As there is little theoretical knowledge on how to optimize the social interdependence in IPE, educators often struggle to develop an effective program. Therefore, a more specific explanation of the relationship between social interdependence and interprofessional readiness might make IPE more effective. We aimed to elucidate how students’ social interdependence in collaborative learning relates to interprofessional readiness. Health profession students (n = 259) undertaking a collaborative IPE program were asked to complete two validated questionnaires: Readiness for Interprofessional Learning Scale and Social Interdependence Scale in Collaborative Learning. A structural equation analysis provided a good fit for the data. Awareness of objectives positively predicted interprofessional collaboration and identity, whereas specific roles as health professionals negatively predicted interprofessional roles and identity. As the current healthcare system is highly specialized, there is a dilemma that the more specific a problem is, the clearer it is which profession is responsible for solving it. Hence, strengthening awareness collaboratively may overcome the dilemma. Also, it is necessary to reconstruct a curriculum based on the premise of interprofessional activities.
Introduction
As the complexity of medical care increases, medical practice is quickly evolving into a process that involves many different health professions. All health professionals should be able to work within their own professions, but should also have the ability to interact with other professionals and work as a team. The World Health Organization (WHO) describes interprofessional education (IPE) as when individuals from two or more professions learn about, from, and with each other to enable effective collaboration and improve health outcomes (Gilbert et al., Citation2010). Based on this framework, IPE is beneficial not only with regard to the healthcare outcomes for patients (Hanson et al., Citation2013), but also in promoting patient safety (Institute of Medicine, Citation2013). As IPE enables effective collaboration between multiple health professions for improved health outcomes, it is considered as an essential undergraduate and postgraduate training strategy.
One major purpose of IPE is to teach teamwork. As teamwork in clinical practice is the mutually-beneficial cooperation of various professions, learning strategies involving group activities is often central to IPE (D’Eon, Citation2005; Oandasan & Reeves, Citation2005; Steinert et al., Citation2005). For example, more than half of the IPE programs in Japan incorporate various types of group learning, such as collaborative learning, problem-based learning, or team-based learning (Hean et al., Citation2012; Maeno et al., Citation2013; Rider & Brashers, Citation2006). This is because collaborative learning places students in a practice environment wherein they are able to mutually interact, which allows them to learn interprofessional attitudes in a constructivist manner (Curran et al., Citation2010). Therefore, collaborative learning is aligned with the goals of IPE as it helps foster an attitude of interdependence.
The social interdependence theory (SIT; Johnson & Johnson, Citation2009) is a background theory for collaborative learning which posits that social interdependence exists when the outcomes of individuals are affected not only by their own actions, but by the actions of others as well. There are three components of interdependence: (1) outcome, (2) means, and (3) boundary (Johnson & Johnson, Citation1989). First, outcome interdependence is defined as an orientation toward goals and rewards. Second, means interdependence refers to resources, roles, and task interdependence. Resources are used among group members, some of which are utilized together (i.e., a blackboard); roles are assigned to group participants (e.g., readers, recorders, summarizers, and encouragers); and task interdependence is when group members come to a mutual agreement regarding how to divide and assign the tasks, making each group member responsible for their learning objectives. This consequently leads to the increased productivity of the learning group. Lastly, boundary interdependence refers to the discontinuities used to segregate groups from one another, but function to unify the individuals within these separate groups (e.g., working area, identity, outside competitors; Johnson & Johnson, Citation2009).
There are two types of social interdependence: positive (actions which promote the achievement of joint goals) and negative (actions which obstruct the achievement of each other’s goals). Positive interdependence is key for successful collaborative learning because positive interdependent cooperation results in more frequent use of higher-level reasoning, improved interpersonal relationships, and greater social support (Bate et al., Citation2014; Johnson & Johnson, Citation1989). Furthermore, social interdependence is important for constructing relationships among interprofessional health care providers (Paradis & Whitehead, Citation2018). Therefore, this is why medical schools desire to cultivate positive social interdependent attitudes through IPE among their learners.
In order to cultivate interprofessional competence more efficiently, competency-based curricula are being required to include IPE to help develop readiness for interprofessional collaboration (Parsell & Bligh, Citation1999). Based on previous findings and empirical evidence, we developed a hypothetical model in which social interdependence attitude in collaborative learning is one of the constructs of readiness for interprofessional learning. In this model, each factor of social interdependence is interrelated and yet affects all factors of multi-professional collaboration (Johnson & Johnson, Citation2009). Discontinuities between individuals and groups (boundary interdependence) define team and collaboration, and their roles. Problem solving as a team (outcome interdependence) requires collaboration and professional competencies as a team. Sharing resources such as tools and competencies of team members (means interdependence) is the center of interprofessional work. However, we cannot fix the specific relationship between these variables and thus there might be a risk of over-identification regarding the effect of social interdependence, because there is currently insufficient knowledge regarding the roles of social interdependence and IPE in students’ preparedness for interprofessional activities. As there is inadequate knowledge on how to optimize social interdependence through IPE in a theoretical manner, educators often struggle to develop an effective program. Nevertheless, if the relationship between social interdependence and competencies for interprofessional collaboration can be properly explained, then students might be able to collaborate with others more effectively in order to improve health outcomes.
Hence, the aim of this study was to clarify how health profession students perceived social interdependence in relation to interprofessional collaborative learning and their readiness for interprofessional learning.
Methods
Participants
The study sample included fourth-year health professional students from the Shinshu University School of Medicine who completed an interprofessional collaborative learning program in the fall semester of academic year 2018–2019 as part of their 6-year (medicine) or 4-year (nursing, physical therapy, occupational therapy, medical technology) curriculum. In this program, students from multiple professions worked in groups of eight or nine to find solutions to various problems in a patient with amyotrophic lateral sclerosis. The analysis and problem solving of the case was performed in groups and the results of their discussions were submitted as assignments. The groups presented their assignments to the other students, who then peer-reviewed the final output. In effect, the discussions were basically student-led as the tutors from the various health professions only facilitated when needed.
The program was organized from the perspective of SIT. For outcome interdependence, the students shared goals for addressing the problems in the patient case, as well as in the evaluation of the other groups’ assignments. For means interdependence, group members needed to share their tasks and assign specific roles depending on their competence in their respective disciplines. Lastly, for boundary interdependence, students were expected to work in groups and to compete with other groups. With this design, we found that the program contained all three components of social interdependence (Johnson & Johnson, Citation2009).
Data collection and measures
We asked all the students (n = 258; male 119, female 139) from all of the disciplines participating in the program to complete the questionnaires at the end of the program after a written informed consent form was obtained. The questionnaires were administered anonymously. Participants were informed that the survey was not mandatory and would not affect their grade. The students were then given about 15 minutes to answer the questionnaires.
Readiness for interprofessional learning was measured with the Japanese validated version of the Readiness for Interprofessional Learning Scale (RIPLS; Parsell & Bligh, Citation1999; Tamura et al., Citation2012), which was comprised of 19 items. Meanwhile, attitude of social interdependence was measured with the Social Interdependence in Collaborative Learning Scale (SOCS), which was composed of 15 items. The article which reported on SOCS was published in 2020 (Shimizu et al., Citation2020) but the final version was developed in 2018 as a part of our research project. The items were answered on a 5-point Likert scale (5: strongly agree, 4: agree, 3: neutral, 2: disagree, 1: strongly disagree) and the questionnaires were administered online through SurveyMonkey. Higher scores indicated that participants perceived a higher level of social interdependence or readiness for interprofessional collaboration.
The adequacy of the sample size was confirmed by the guidelines of Fayers and Machin (Citation2007), which state that the sample should be more than five times the number of items and greater than 100.
Analysis
The data were initially screened for outliers and missing values (<5%); and missing values were treated using multiple imputation techniques. Descriptive statistics were calculated using IBM SPSS version 26.0. Zero-order correlations between each measure were calculated, and Pearson correlation coefficients were computed.
An exploratory factor analysis (EFA) of both instruments was then performed to explore the underlying structure of the items in our context (Fabrigar et al., Citation1999). We used the maximum likelihood method and promax rotation to confirm that the factor loadings were ≥0.4 and were theoretically consistent. The number of factors were then decided based on the results of Kaiser’s eigenvalues(≥1.0), minimum average partical correlation (MAP; Velicer, Citation1976) and parallel analyses of the eigenvalues and squared multiple correlations (SMC) in the diagonal of the correlation matrix (Horn, Citation1965; Humphreys & Ilgen, Citation1969). Additionally, the alpha-coefficients were computed as an estimate of internal consistency for all factors.
The data of these instruments were analyzed using structural equation modeling (SEM) – a method that can test causal hypotheses among multivariate data. This technique was chosen as it allows for the simultaneous, rather than separate, analysis of all the variables in the model. Since SEM has advanced theories and research in medical education by developing and validating new theoretical models between multiple indicators (Violato & Hecker, Citation2007), we chose the method to clearly explain relations between the two existing conceptual frameworks of social interdependence and readiness for interprofessional learning in collaborative learning, in line with the procedures by Violato and Hecker (Citation2007), which started with our hypothesis as written in the introduction.
SEM was performed using IBM AMOS software version 22.0 (maximum-likelihood method) for the analysis of the relationships among the factors. The following fit indices and criteria were used: chi-square (p ≥.05), chi-square divided by the degrees of freedom (CMIN/df) ≤ 2; goodness-of-fit index (GFI) ≥ 0.90; comparative fit index (CFI) ≥ 0.90; root mean square residual (RMSEA) ≤ 0.1; and PCLOSE value ≥ 0.05 (Violato & Hecker, Citation2007).
Ethics considerations
Students received a written informed consent form, and those who understood the purpose of the research and agreed to participate received the questionnaires.
All the participants were informed that the survey was not mandatory and was not related to their grading. This study was approved by the Institutional Review Board of Shinshu University (#5048).
Results
Complete RIPLS and SOCS items were received from 228 participants (97 males and 131 females; medicine = 94, nursing = 67, occupational therapy = 12, physical therapy = 15, and medical technology = 40). The total response rate was 88.3%.
In the EFA of SOCS (), The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.874, which was satisfactory. The Bartlett’s test of sphericity was significant with p < .001 (χ2 = 1463.197, df = 105). Kaiser method and MAP suggested the three-factor structure, which was consistent with the original literature. However, parallel analysis of eigenvalues suggested the two-factor structure and parallel analysis of SMC suggested the four-factor structure. Therefore, we adopted the three-factor model for SOCS ().
Table 1. Factor analysis of SOCS and RIPLS.
Table 2. Determination of numbers of factors.
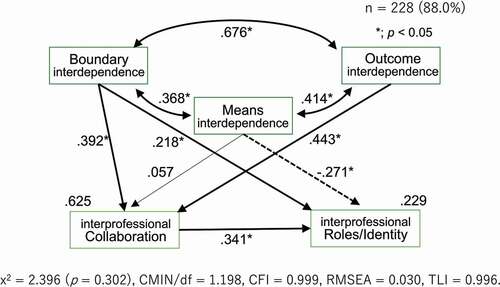
As for the RIPLS (), The Kaiser–Meyer–Olkin measure was 0.930, which was satisfactory. The Bartlett’s test of sphericity was significant with p < .001 (χ2 = 3093.441, df = 171). All of the analyses (Kaiser method, MAP, and parallel analyses of eigenvalues and SMC) suggested a two-factor structure. Although we also analyzed with the three-factor model, the factor loadings of all items for the third factor were <0.4. No item was associated with the third factor and the factor contribution rate of the third factor was very low (10.4%). Therefore, we abandoned the idea of considering the third factor as an independent one and adopted the two-factor model for RIPLS (). Comparing the items and factors of the RIPLS with the original studies (Parsell & Bligh, Citation1999; Tamura et al., Citation2012), we adopted factor 1 (regarding collaboration) and factor 2 (regarding roles) and factor 3 (regarding identity) were regarded as one (). The factor 1 was named “Interprofessional Collaboration” and the second factor was named “Interprofessional Roles and Identity.” The alpha-coefficients indicated satisfactory internal consistency of all the factors (). In estimating the SEM model, we first used a hypothesized model which was mentioned above. We then evaluated the models by reducing the number of paths and optimizing the Goodness-of-Fit and statistical measures. The model shown in showed the best fit with x2 = 2.396 (p = .302), CMIN/df = 1.198, CFI = 0.999, RMSEA = 0.030, TLI = 0.996. In this model, the three components of social interdependence were moderately associated with each other. Boundary and outcome interdependence positively predicted interprofessional collaboration and interprofessional roles/identity. Meanwhile, means interdependence negatively predicted interprofessional roles/identity. Boundary and outcome interdependences were especially useful in predicting interprofessional collaboration, as the model explained 62% of the variance in it. Although we also tested other numbers of factors (two- and four- factor structures) of SOCS, we did not find better models to fit.
Table 3. Results on the instruments.
Discussion
The present study attempted to clarify the causal relationships of the social interdependence components (outcome, means, and boundary) which affect the cultivation of attitudes toward interprofessional collaboration in an IPE program. A sufficient sample size was obtained for an appropriate analysis to be conducted. To the best of our knowledge, the relations between the social interdependence components among health profession students and their readiness for interprofessional work during the collaborative IPE program have not been previously modeled in the specific context of an undergraduate curriculum.
The results of this study demonstrated that boundary interdependence (i.e., interdependence that makes people work as one team) leads to readiness for cooperation, as well as interprofessional roles/identity. In line with this, one of the purposes of IPE is to establish teamwork and build interprofessional collaboration (Thistlethwaite & Moran, Citation2010). Hence, boundary interdependence supports this because it reinforces social identity by uniting groups as a single entity (Johnson & Johnson, Citation2009). This social identity is an important antecedent of cooperative behavior (Tyler & Blader, Citation2001). Therefore, stronger boundary interdependence can be expected to facilitate the achievement of team goals and thus enhance the readiness of IPE.
In addition, outcome interdependence was found to be associated with readiness to collaborate, but there was no significant association with interprofessional roles/ identity. As collaborative practice improves patient outcomes (Zwarenstein et al., Citation2000), students in collaborative IPE are often expected to work in teams to solve patient problems, like those in this study. While interprofessional collaboration delivers effective working relationships, it was not found to be associated with the perceived structure of the team (i.e., identity; Canadian Interprofessional Health Collaborative, Citation2010). Thus, although patient outcomes are influenced by interprofessional collaboration, it does not affect interprofessional identity in our given context.
Furthermore, means interdependence was discovered to be negatively correlated to interprofessional identity. In other words, the more interdependent the means are in IPE, the less interprofessional identity there is. When positive interdependence is established, individual members become aware of their personal responsibilities. In relation to this, as the current healthcare system is highly specialized, it becomes more evident which profession should be responsible for addressing a certain problem, the more specific it is. Therefore, team members may seek to exercise their individual professional competence in order to achieve a specific outcome rather than as a team.
While the other two elements of social interdependence enhanced the readiness of the interprofessional collaboration, the means interdependence appeared to show the opposite: when students tried to demonstrate their disciplinary-specific means, their interprofessional identity would be diminished. Whitehead (Citation2007) claimed a similar difficulty among physicians who found it difficult to balance collaboration and authority for decision-making given the hierarchical nature of the clinical setting. This is supported by the results of this study, which indicate that there is a difficulty in reconciling specialized training with IPE regardless of the discipline.
We will discuss IPE from the perspective of SIT based on these results. This study has shown that the components in social interdependence in collaborative learning led to different associations regarding readiness for interprofessional learning.
First, we should analyze the elements for building teamwork and designing an IPE program. Team collaboration has been considered important in IPE. However, it is criticized that “teamwork” is an amorphous word in workplaces (Rydenfält et al., Citation2019), and although team identity is a prerequisite for teamwork, the results of this study can be used to obtain results regarding desirable interprofessional collaboration. For example, there is a dilemma in clinical settings that by simply focusing on the role that each profession should play will lead to reinforcing means interdependence and will not improve the identity of teamwork (Michalec & Hafferty, Citation2015). Instead, the results of this study suggest that one way to overcome this dilemma in IPE is to strengthen boundary interdependence, that is, reinforcing the situations to make professionals aware as a team both internally and externally. As outcome and boundary interdependence are relatively strongly correlated, engaging students in a goal of care is the first step for team building (De Nooijer et al., Citation2021). Also, as a solution to improve the external environment of boundary interdependence, we hypothesize that opportunities (e.g., team competitions) for achieving shared outcomes may enhance boundary interdependence and promote interprofessional readiness. As team competition is uncommon in actual clinical settings, further research is needed to examine the effect of team competition in IPE.
Also, an understanding of the job title must be formed before IPE. Role understanding is considered to be an important competence for collaborative practice (Suter et al., Citation2009). The EFA in this study revealed the items regarding roles and identity were integrated into a single factor. This phenomenon indicates that roles and identities were inseparable, at least in the context of our IPE. However, role understanding needs to be rooted in the interprofessional team, and not in each profession. As pointed out by Paradis and Whitehead (Citation2018), it is necessary to review the curricula of each discipline and construct learning objectives and study plans based on the premise of interprofessional collaboration, rather than activities focused for a single profession.
The present study had a number of limitations. First, this study was based on a specific IPE class at a single institution. This could have affected the findings of the study. In particular, factors regarding roles and identity in the original RIPLS were not divided in the context of this study. A possible cause was that in this context, collaborative learning was conducted in a way that clarified the roles of each profession. Students in this program were assessed by assignments of clinical problems in a case study, as is often the case with many IPE programs (Hean et al., Citation2012). The emphasis on summative assessment in group learning encourages students to seek quick solutions and spoils their diverse inquiring attitude (Harrison et al., Citation2015; Shimizu et al., Citation2021), while professional identity formation requires multiple factors other than patients’ problems (Cruess et al., Citation2015). Students should have had more opportunities to form their professional identity in a broader perspective in addition to the roles expected for the assignments as each profession.
Also, the impact of the health care system in our context cannot be ignored. The competency of healthcare professionals will be inconsistent between undergraduate students and practicing professionals (Primomo, Citation2000; Shinjo & Aramaki, Citation2012; Suzuki et al., Citation2008; Watanabe & Hashimoto, Citation2012). Haruta et al. (Citation2018) summarized the competencies for interprofessional collaboration in Japan, but interprofessional collaboration has yet to be implemented effectively in the country. Explanations provided for this situation include a lack of communication among healthcare staff, strong hierarchical barriers, and a lack of understanding among healthcare workers about their own and their colleagues’ roles and responsibilities (Minamizono et al., Citation2013). Undeniably, interprofessional readiness may have been formed based on this assumption. We hope these relationships will be further studied in replication studies in other parts of the world.
Conclusions
While boundary interdependence leads to readiness for cooperation as well as interprofessional roles, outcome interdependence was not associated with interprofessional roles. Furthermore, means interdependence faces a dilemma that when students try to demonstrate their disciplinary-specific means, their interprofessional roles would be diminished. For more effective IPE programs, we should engage students in a goal of care for team building, and construct role understanding to be rooted in the interprofessional activities from the beginning, rather than single profession.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We thank the students who participated in the research, and faculty members to coordinate and support the IPE program. We would also like to appreciate Editage (www.editage.com) for English language editing.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Funding
Notes on contributors
Ikuo Shimizu
Ikuo Shimizu, MD, MHPE, is an assistant professor at Safety Management Office, Shinshu University Hospital, Japan, and a PhD candidate at School of Health Professions Education, Maastricht University, The Netherlands. He made substantial contributions to: conception and design, acquisition of data, analysis and interpretation of data as well as drafting the document the manuscript.
Teiji Kimura
Teiji Kimura, PT, PhD, is a professor at Department of Fundamental Physical Therapy, Shinshu University, Japan. He made substantial contributions to design of the work, acquisition of data, as well as critically revising the manuscript.
Robbert Duvivier
Robbert Duvivier, MD, PhD, MBA, combines specialist training in psychiatry at Parnassia Mental Health in the Hague, the Netherlands, with research in education. He currently holds appointments at Maastricht University, the Netherlands, and at the University of Newcastle, Australia where he is a Senior Lecturer in Medical Education. He made substantial contributions to: conception and design, analysis and drafting and critically revising the manuscript.
Cees van der Vleuten
Cees van der Vleuten is a professor and scientific director, School of Health Professions Education, Department of Educational Development and Research, Faculty of Health, Medicine and Life Sciences, Maastricht University, Maastricht, The Netherlands. He made substantial contributions to: conception and design, analysis and drafting and critically revising the manuscript.
References
- Bate, E., Hommes, J., Duvivier, R., & Taylor, D. C. M. (2014). Problem-based learning (PBL): Getting the most out of your students - their roles and responsibilities: AMEE Guide No. 84. Medical Teacher, 36(1), 1–12. https://doi.org/10.3109/0142159X.2014.848269
- Canadian Interprofessional Health Collaborative. (2010). A national interprofessional competency framework. Health San Francisco.
- Cruess, R. L., Cruess, S. R., Boudreau, J. D., Snell, L., & Steinert, Y. (2015). A schematic representation of the professional identity formation and socialization of medical students and residents: A guide for medical educators. Academic Medicine, 90(6), 718–725. https://doi.org/10.1097/ACM.0000000000000700
- Curran, V. R., Sharpe, D., Flynn, K., & Button, P. (2010). A longitudinal study of the effect of an interprofessional education curriculum on student satisfaction and attitudes towards interprofessional teamwork and education. Journal of Interprofessional Care, 24(1), 41–52. https://doi.org/10.3109/13561820903011927
- D’Eon, M. (2005). A blueprint for interprofessional learning. Journal of Interprofessional Care, 19(sup1), 49–59. https://doi.org/10.1080/13561820512331350227
- de Nooijer, J., Dolmans, D. H. J. M., & Stalmeijer, R. E. (2021). Applying landscapes of practice principles to the design of interprofessional education. Teaching and Learning in Medicine, 1–6. https://doi.org/10.1080/10401334.2021.1904937
- Fabrigar, L. R., Wegener, D. T., MacCallum, R. C., & Strahan, E. J. (1999). Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods, 4(3), 272. https://doi.org/10.1037/1082-989X.4.3.272
- Fayers, P. M., & Machin, D. (2007). Scores and measurements: Validity, reliability, sensitivity. In quality of life: The assessment, analysis and interpretation of patient reported outcomes (2nd ed., pp. 77–107). John Wiley & Sons https://doi.org/10.1002/9780470024522.ch4
- Gilbert, J. H. V., Yan, J., & Hoffman, S. J. (2010). A WHO report: Framework for action on interprofessional education and collaborative practice (No. WHO/HRH/HPN/10.3). World Health Organization.
- Hanson, T. K., Aleman, M., Hart, L., & Yawn, B. (2013). Increasing availability to and ascertaining value of asthma action plans in schools through use of technology and community collaboration. Journal of School Health, 83(12), 915–920. https://doi.org/10.1111/josh.12110
- Harrison, C. J., Könings, K. D., Schuwirth, L., Wass, V., & Van der Vleuten, C. (2015). Barriers to the uptake and use of feedback in the context of summative assessment. Advances in Health Sciences Education, 20(1), 229–245. https://doi.org/10.1007/s10459-014-9524-6
- Haruta, J., Yoshida, K., Goto, M., Yoshimoto, H., Ichikawa, S., Mori, Y., Yoshimi, K., & Otsuka, M. (2018). Development of an interprofessional competency framework for collaborative practice in Japan. Journal of Interprofessional Care, 32(4), 436–443. https://doi.org/10.1080/13561820.2018.1426559
- Hean, S., Craddock, D., Hammick, M., & Hammick, M. (2012). Theoretical insights into interprofessional education: AMEE guide no. 62. Medical Teacher, 34(2), e78–e101. https://doi.org/10.3109/0142159X.2012.650740
- Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika, 30(2), 179–185. https://doi.org/10.1007/BF02289447
- Humphreys, L. G., & Ilgen, D. R. (1969). Note on a criterion for the number of common factors. Educational and Psychological Measurement, 29(3), 571–578. https://doi.org/10.1177/001316446902900303
- Institute of Medicine. (2013). Interprofessional Education for Collaboration. (National Academies Press, Ed.), Biological Conservation (Vol. 181). Washington, D.C.: National Academies Press. h t tps://d oi.o rg/1 0.17226/13486.
- Johnson, D. W., & Johnson, R. T. (1989). Cooperation and competition: Theory and research. Central European (2nd ed.). Interaction Book Company.
- Johnson, D. W., & Johnson, R. T. (2009). An educational psychology success story: Social interdependence theory and cooperative learning. Educational Researcher, 38(5), 365–379. https://doi.org/10.3102/0013189x09339057
- Maeno, T., Takayashiki, A., Anme, T., Tohno, E., Maeno, T., & Hara, A. (2013). Japanese students’ perception of their learning from an interprofessional education program: A qualitative study. International Journal of Medical Education, 4(1), 9–17. https://doi.org/10.5116/ijme.50e5.e29a
- Michalec, B., & Hafferty, F. W. (2015). Role theory and the practice of interprofessional education: A critical appraisal and a call to sociologists. Social Theory & Health, 13(2), 180–201. https://doi.org/10.1057/sth.2015.2
- Minamizono, S., Hasegawa, H., Hasunuma, N., Kaneko, Y., Motohashi, Y., & Inoue, Y. (2013). Physician’s perceptions of interprofessional collaboration in clinical training hospitals in Northeastern Japan. Journal of Clinical Medicine Research, 5(5), 350–355. https://doi.org/10.4021/jocmr1474w
- Oandasan, I., & Reeves, S. (2005). Key elements for interprofessional education. Part 1: The learner, the educator and the learning context. Journal of Interprofessional Care, 19(SUPPL. 1), 21–38. https://doi.org/10.1080/13561820500083550
- Paradis, E., & Whitehead, C. R. (2018). Beyond the lamppost: A proposal for a fourth wave of education for collaboration. Academic Medicine, 93(10), 1457–1463. https://doi.org/10.1097/ACM.0000000000002233
- Parsell, G., & Bligh, J. (1999). The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Medical Education, 33(2), 95–100. https://doi.org/10.1046/j.1365-2923.1999.00298.x
- Primomo, J. (2000). Nursing around the world: Japan - preparing for the century of the elderly. Online Journal of Issues in Nursing, 5(2), MS1. www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume52000/No2May00/JapanElderlyCentury.aspx
- Rider, E. A., & Brashers, V. (2006). Team-based learning: A strategy for interprofessional collaboration. Medical Education, 40(5), 486–487. https://doi.org/10.1111/j.1365-2929.2006.02434.x
- Rydenfält, C., Borell, J., & Erlingsdottir, G. (2019). What do doctors mean when they talk about teamwork? Possible implications for interprofessional care. Journal of Interprofessional Care, 33(6), 714–723. https://doi.org/10.1080/13561820.2018.1538943
- Shimizu, I., Kikukawa, M., Tada, T., Kimura, T., Duvivier, R., & van der Vleuten, C. (2020). Measuring social interdependence in collaborative learning: Instrument development and validation. BMC Medical Education, 20(1), 177. https://doi.org/10.1186/s12909-020-02088-3
- Shimizu, I., Matsuyama, Y., Duvivier, R., & van der Vleuten, C. (2021). Contextual attributes to promote positive social interdependence in problem-based learning: A focus group study. BMC Medical Education, 21(1), 222. https://doi.org/10.1186/s12909-021-02667-y
- Shinjo, D., & Aramaki, T. (2012). Geographic distribution of healthcare resources, healthcare service provision, and patient flow in Japan: A cross sectional study. Social Science & Medicine, 75(11), 1954–1963. https://doi.org/10.1016/j.socscimed.2012.07.032
- Steinert, Y., Cruess, S., Cruess, R., & Snell, L. (2005). Faculty development for teaching and evaluating professionalism: From programme design to curriculum change. Medical Education, 39(2), 127–136. https://doi.org/10.1111/j.1365-2929.2004.02069.x
- Suter, E., Arndt, J., Arthur, N., Parboosingh, J., Taylor, E., & Deutschlander, S. (2009). Role understanding and effective communication as core competencies for collaborative practice. Journal of Interprofessional Care, 23(1), 41–51. https://doi.org/10.1080/13561820802338579
- Suzuki, Y., Gibbs, T., & Fujisaki, K. (2008). Medical education in Japan: A challenge to the healthcare system. Medical Teacher, 30(9–10), 846–850. https://doi.org/10.1080/01421590802298207
- Tamura, Y., Seki, K., Usami, M., Taku, S., Bontje, P., Ando, H., Taru, C., & Ishikawa, Y. (2012). Cultural adaptation and validating a Japanese version of the readiness for interprofessional learning scale (RIPLS). Journal of Interprofessional Care, 26(1), 56–63. https://doi.org/10.3109/13561820.2011.595848
- Thistlethwaite, J., & Moran, M. (2010). Learning outcomes for interprofessional education (IPE): Literature review and synthesis. Journal of Interprofessional Care, 24(5), 503–513. https://doi.org/10.3109/13561820.2010.483366
- Tyler, T. R., & Blader, S. L. (2001). Identity and cooperative behavior in groups. Group Processes & Intergroup Relations, 4(3), 207–226. https://doi.org/10.1177/1368430201004003003
- Velicer, W. F. (1976). Determining the number of components from the matrix of partial correlations. Psychometrika, 41(3), 321–327. https://doi.org/10.1007/BF02293557
- Violato, C., & Hecker, K. G. (2007). How to use structural equation modeling in medical education research: A brief guide. Teaching and Learning in Medicine, 19(4), 362–371. https://doi.org/10.1080/10401330701542685
- warenstein, M., Reeves, S., Barr, H., Hammick, M., Koppel, I., & Atkins, J. (2000). Interprofessional education: effects on professional practice and health care outcomes. In Merrick Zwarenstein (Ed.), Cochrane Database of Systematic Reviews (CD002213). Chichester, UK: John Wiley & Sons, Ltd. h t tps://d oi.o rg/1 0.1002/14651858.CD002213
- Watanabe, R., & Hashimoto, H. (2012). Horizontal inequity in healthcare access under the universal coverage in Japan; 1986-2007. Social Science and Medicine, 75(8), 1372–1378. https://doi.org/10.1016/j.socscimed.2012.06.006
- Whitehead, C. (2007). The doctor dilemma in interprofessional education and care: How and why will physicians collaborate? Medical Education, 41(10), 1010–1016. https://doi.org/10.1111/j.1365-2923.2007.02893.x