ABSTRACT
Teamwork quality has been shown to influence patient safety, and simulation-based team-training (SBTT) is an effective means to increase this quality. However, long-term effects are rarely studied. This study aims to investigate the long-term effects of interprofessional SBTT in emergency medicine in terms of global confidence, self-efficacy in interprofessional communication and in emergency medicine situations. Newly graduated doctors, nurses, auxiliary nurses, and medical and nursing students participated. Four emergency medicine scenarios focused on teamwork according to the A-B-C-D-E-strategy. All participants increased their global confidence from 5.3 (CI 4.9–5.8) before to 6.8 (CI 6.4–7.2; p < .0001) after SBTT. Confidence in interprofessional communication increased from 5.3 (CI 4.9–5.8) to 7.0 (CI 6.6–7.4; p < .0001). Students had the greatest gain. The self-efficacy following the A-B-C-D-E strategy increased from 4.9 (CI 4.4–5.3) to 6.6 (CI 6.2–7.0). Again, students had the steepest increase. Newly graduated doctors achieved a superior increase in global confidence as compared to nurses and auxiliary nurses (p < .0001). Their propensity to recommend SBTT to colleagues was 9.9 (CI 9.8–10.0). The positive effects were sustained over a six-month period, indicating that interprofessional SBTT had a positive impact on competence development, and a potential to contribute to increased team quality in emergency medicine care.
Introduction
There is a growing demand to perform effective health care 24 hours a day, 7 days a week and to continuously improve patient safety and quality of care. Research has shown that patients frequently suffer unnecessary harm as a result of medical errors that could have been prevented (Carter et al., Citation2014).
Teamwork quality is recognized as an important and critical factor affecting patient safety (Aldawood et al., Citation2020; Welp et al., Citation2016). Teams are often assembled ad hoc and team membership changes dynamically in standard health care (Manser, Citation2009; Rosenman et al., Citation2015). Deficient team coordination, communication failures and procedural errors have been observed as drawbacks that contribute to reduced patient safety (Leonard et al., Citation2004; Nagpal et al., Citation2010; Rönnerhag et al., Citation2019). To counteract these problems training of healthcare personnel now includes not only training of technical skills, but also training of non-technical skills (Krage et al., Citation2017). Non-technical skills can be defined as “the cognitive and social skills required for efficient and safe operations.” These skills include situation awareness, decision-making, teamwork, leadership, and managing personal resources (Flin et al., Citation2017, edition 2017, p. 1). Systematic and structured approaches to assess patients, e.g., advanced medical life support system (AMLS), have been highlighted as a means to increase patient safety and quality of care. The A-B-C-D-E strategy applied in emergency medicine situations aims to assess and stabilize a patient’s airways, breathing, circulation, disability, and exposure using a structured and systematic protocol (Thim et al., Citation2012).
Despite these endeavors, there are still several reports that show significant rates of healthcare errors caused by human inaccuracies (Nagpal et al., Citation2012; Steyrer et al., Citation2013; Symons et al., Citation2013; Westbrook et al., Citation2015). Apparently, there is still room for great improvements.
Background
Professional skills are not context free, and at a more advanced level these skills could only be achieved through situational experiences in professional practice (Dreyfus, 2004). However, to train skills and working effectively in a team in emergency medicine situations only when “on the job” is unsatisfactory due to patient safety reasons and the random occurrence of suitable patient situations that meet the learners´ intended learning objectives (ILO). Simulation-based team training (SBTT) has therefore been developed as a structured learning activity aimed to obtain the non-technical skills necessary for skillful teamwork without training on real patients (Meurling et al., Citation2013; Robertson et al., Citation2017). There is support for a short-time beneficial effect of SBTT programmes in the improvement of essential team processes, such as communication, coordination and other outcomes, such as knowledge, skills, attitudes and perceptions (Colman et al., Citation2019; Fung et al., Citation2015; Meurling et al., Citation2013). Structured interventions targeting high teamwork quality have been shown to improve teamwork and to develop a safe climate (Hinde et al., Citation2016; Paine et al., Citation2011). Improved self-efficacy has been shown concerning crisis management, medical management, clinical performance and teamwork efficiency after SBTT (Colman et al., Citation2019; Kameg et al., Citation2010; Paige et al., Citation2009). There are studies illustrating that the learning process by itself (McGaghie et al., Citation2016) is effective and transferable to working situations with patients (Ahya et al., Citation2012; Barsuk et al., Citation2012). However, there is a lack of knowledge on the long-term effects of SBTT (McGaghie et al., Citation2016) and patient simulation in the handling of emergency medicine. The interprofessional aspects should be recognized.
It is well known from studies in educational and workplace settings that students in the health professions benefit from learning with, from and about other students, i.e., interprofessional education (IPE). IPE can develop their teamwork skill (Rotz et al., Citation2016) and increase their collaborative and professional competence (Hallin et al., Citation2009). IPE also contributes to improved professional practice and patient perceived quality of care (Hallin et al., Citation2011; Reeves et al., Citation2017). A first ever retrospective cohort study has shown the effects of interprofessional undergraduate training on patient outcome (Hallin et al., Citation2018). IPE is used to prepare both under- and postgraduates for efficient work (Gandhi et al., 20Citation18; Leape et al., Citation2009).
Technology-enhanced simulation was used in a meta-analysis associated with a better learning outcome than without training or when it was added to training on the job (Cook et al., Citation2011). An implication of this is that SBTT is an appropriate learning activity and should thus be added to other learning activities aiming to achieve knowledge, skills, and appropriate behaviors in teamwork. Interprofessional SBTT has been shown to result in short-term improvements of students’ team-based attitudes (Sigalet et al., Citation2012; Wang et al., Citation2019), perceptions of collaboration (Dillon et al., Citation2009; Reese et al., Citation2010) and team-based performance (Jankouskas et al., Citation2011). However, there is still a need to clarify whether SBTT have sustained effects on such skills in undergraduates (Tofil et al., Citation2014). Furthermore, there is limited knowledge regarding the effects of SBTT on student teams as compared to teams consisting of educated healthcare professionals and between the professions.
This study aims to investigate the long-term effects of interprofessional simulation-based team training in emergency medicine scenarios in terms of global confidence in acute care situations, self-efficacy in interprofessional communication and in handling of acute emergency situations professionally. A further aim was to assess potential differences in results between the professions and between students and licensed professionals.
Methods
Research design
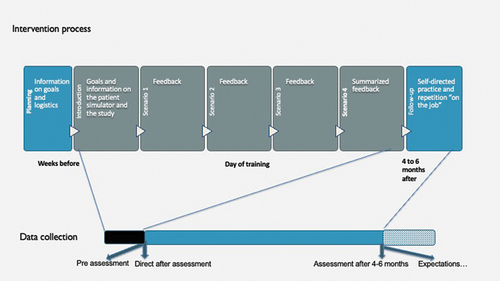
An interventional longitudinal study comparing participants’ self-efficacy before, immediately after, and at six-months after participating in an educational intervention. The rationale for choosing self-efficacy as an outcome measure was based on the Bandura self-efficacy theory that defines self-efficacy as one´s perceived capability to perform actions at designated levels (Bandura, Citation1997). It is well established that self-efficacy has an influence on motivation, self-regulation, and learning, especially in context-specific situations and with support from credible persons (Schunk & Pajares, Citation2009; Schunk & Usher, Citation2012). Acute emergency medicine situations are often contextually well defined with clear evidence-based and well-defined roles. In the SBTT, social persuasion from credible persons is a corner stone in the feedback/debriefing phase. A flow chart of the study is presented in to illustrate the intervention and the data collection procedures.
Educational intervention
The SBTT was performed in a simulation lab with an authentic and fully equipped emergency room where a high-fidelity patient simulator (human patient simulator, METI Inc., Sarasota, Florida, USA) replaced the real patient. The SBTT was facilitated by certified instructors in advanced medical simulation and by well-experienced physicians and nurses. The same group of instructors was present throughout a full educational training and evaluation session. However, the staffing could differ between sessions.
Intended learning outcomes are presented in . The learning activity was based on a selection of predefined standardized scenarios of acute internal medicine scenarios. These scenarios included hypoglycemia, anaphylaxis due to food allergy, acute asthma, myocardial infarction and an acute exacerbation of a chronic obstructive pulmonary disease.
Table 1. Intended learning outcomes for the simulation-based team training in handling of acute emergency medicine situations.
Before SBTT all participants received written information on the learning outcomes and the procedure of SBTT. This included an interactive 30-minute demonstration of the simulator room, the medical equipment, and the patient simulator, and a verbal repeat of the aims. One of the certified instructors demonstrated the correct A-B-C-D-E performance.
Six to eight participants were divided into two teams at each SBTT. The professional teams consisted of one physician as leader, one physician, one nurse and one auxiliary nurse as followers. The student teams consisted of one medical student as leader, one medical student and two student nurses as followers. One team were actors in the scenario, while the other team were observers in an adjacent debriefing room throughout an ongoing video recording. In cases where there were too few participants, the staffing of the acting team was prioritized. The allocation of participants to observers or actors was consecutively altered. The scenario was completed when the medical task was completed, the simulated patient was stabilized or when a plan had been formulated, sometimes organized with the certified instructor acting as consultant. Each team acted in two scenarios and were observed in two. Each scenario lasted approximately 10–15 minutes.
The design of the scenarios and the feedback/debriefing sessions was based on the principles of Crew Resource Management (CRM) that focuses on nontechnical skills including situational awareness, prioritization, role clarity, communication, and debriefing in environments where human errors could have devastating effects (Royal College of Physicians and Surgeons of Canada, Citation2017). Short feedback was provided after each scenario, and a summarized longer feedback and debriefing session was provided directly after the last scenario (see, ). The feedback sessions were structured and started with a self-assessment by the active team followed by feedback concerning both medical and communicative objectives from both the observing team and the certified instructors.
Participants
In total 123 individuals participated. Twenty-one physicians (14 women; 67%), 20 nurses (16 women; 80%), 14 auxiliary nurses (12 women; 86%), 37 medical students (18 women; 49%) and 31 student nurses (27 women; 87%) were scheduled for a half-day of SBTT during the time period May 2012 until March 2015. The physicians were newly graduated doctors, the nurses and auxiliary nurses were staff at the emergency care unit, all employed at a teaching hospital in Sweden. The medical students were all in semester 5 out of 11 of the undergraduate medical programme, and the student nurses were all in semester 4 out of 6 of the nursing programme indicating that all students were at an early stage of clinical training. Only one medical student and 12 nursing students had previous experience of SBTT. Participation in the SBTT was mandatory for the students. However, participation in the study was voluntary, and written informed consent was obtained from all participants. All students agreed to participate and were provided a random number that identified their questionnaire and preserved confidentiality. The Regional Ethical Review Board in Stockholm, Sweden, approved the study: Diary number 2013/1538-31.
Outcome measures
Primary outcomes were assessed self-efficacy four to six months after participation in SBTT; assessed global confidence in acute care situations; assessed interprofessional communication skills; and assessed professional handling of acute emergency medicine.
Secondary outcomes were divergences in self-assessment of effects between professions, and between students and experienced professionals.
Data collection procedure
Two questionnaires (baseline and follow-up versions) were used. They were developed based on a validated questionnaire that, for more than four years, had been used in the ongoing quality assurance process at one of the two SBTT-centers. Based on a literature review, we added questions related to crew resource management (CRM), focusing on interpersonal communication, time-critical decision-making and leadership. The aspects covered in the questionnaires were global confidence in acute care situations; confidence in acute interprofessional communication; self-assessed capability to handle acute emergency medicine in accordance with the A-B-C-D-E strategy. The questionnaires were pilot tested by five professionals and five students. Based on their feedback on clarity and relevance, some of the questions were rephrased. The prefinal questionnaires were discussed in the research group and some further clarifications were included. All answers were graded on a ten-point scale with verbal anchors: 1 denoted “Almost always insecure” and 10 denoted “Almost always secure.” The questionnaires were marked by a number and the participants linked this number to their name in a separate document.
The first questionnaire was collected from participants immediately after the SBTT and the follow-up questionnaire after four to six months.
Statistical analyses
Continuous variables were expressed as means and 95% confidence intervals, and categorical variables were expressed as frequencies, percentages, or both, unless otherwise indicated. A three-factor repeated measurements Analysis of Variance (ANOVA) with two and three-factor interactions was performed on normalized data. The factors were student or professional, profession and time. All analyses were carried out with the statistical software Statistica 12 (StatSoft Inc., Tulsa, OK, USA),
Results
In total, 20 physicians, 18 nurses, 14 auxiliary nurses, 35 medical students and 24 student nurses responded to the two questionnaires yielding a response rate of 90%. The physicians had an average of 31 (CI 23–43) months in the profession, the nurses had 50 (CI 34–67) months, and the auxiliary nurses 129 (CI 62–137) months. Their previous experience of SBTT varied from none to three occasions with a median of one and with no difference between the professions.
The medical students were all in semester 5 out of 11 and the nurse students were all in semester 4 or 5 out of 6. Slightly more than one-third of the nurse students (38%; n = 12) had previous experience of SBTT varying from 1 to 3 occasions with a median of one occasion. Only one of the medical students had previously attended SBTT. The experience of SBTT did thus differ between the student categories (p < .0001; Fisher's exact test).
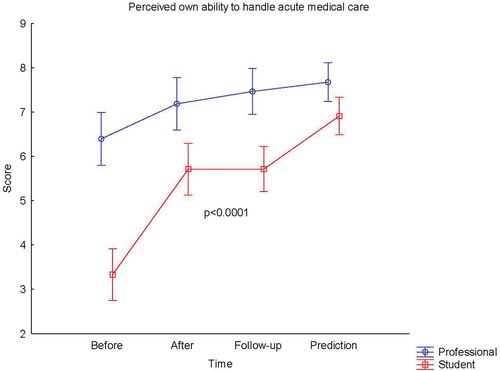
As shown in , the global confidence in acute care situations increased for all participants and was forecasted to be sustained. There was a different time trend among students and professionals (statistical interaction p < .0001) with a steeper increase at follow-up in students. As shown in , the participants’ confidence in acute interprofessional communication increased. The students had the greatest gain at follow-up after 4–6 months (interaction p = .0044). As presented in , the confidence in assessed own capability to handle acute medical care in accordance with the A-B-C-D-E strategy increased from 4.9 (CI 4.4–5.3) to 6.6 (CI 6.2–7.0) at follow-up with a forecast to stay above this level (; p < .0001). There was a different time trend in students compared with professionals (statistical interaction p < .0001) with a steeper increase in students from 3.3 (CI 2.8–3.9) before the SBTT to 5.7 (CI 5.2–6.2) at follow-up.
Figure 2. Self-assessed global confidence in acute care situations before and after simulation-based team training (SBTT). 1. Questionnaire 1: Before refers to their self-assessed knowledge and competence state prior to the SBTT; After refers to their self-assessed knowledge and competence state immediately after the SBTT 2. Questionnaire 2: Follow-up refers to the self-assessed knowledge and competence state 4–6 months after the SBTT and a prediction of own future gain. Student denotes medical and nursing students. Professionals denotes newly graduated doctors, nurses and auxiliary nurses. All answers in the questionnaire were graded on a ten-point scale with verbal anchors: 1 = Almost always insecure and 10 = Almost always secure. Means and 95% confidence intervals are indicated. P-values refers to the change over time in a three factor repeated measurements analysis of variance (ANOVA). .
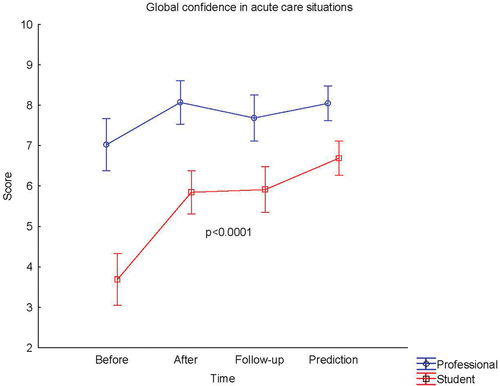
Figure 3. Self-assessed confidence in acute interprofessional communication before and after simulation-based team training (SBTT). 1. Questionnaire 1: Before refers to their self-assessed knowledge and competence state prior to the SBTT; After refers to their self-assessed knowledge and competence state immediately after the SBTT 2. Questionnaire 2: Follow-up refers to the self-assessed knowledge and competence state 4–6 months after the SBTT and a prediction of own future gain. Student denotes medical and nursing students. Professionals denotes newly graduated doctors, nurses and auxiliary nurses. All answers in the questionnaire were graded on a ten-point scale with verbal anchors: 1 = Almost always insecure and 10 = Almost always secure. Means and 95% confidence intervals are indicated. P-values refers to the change over time in a three factor repeated measurements analysis of variance (ANOVA) .
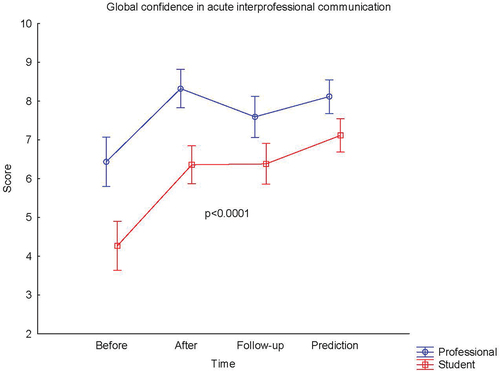
Figure 4. Self-assessed professional handling of acute medical care in accordance with the A-B-C-D-E strategy before and after simulation-based team training (SBTT). 1. Questionnaire 1: Before refers to their self-assessed knowledge and competence state prior to the SBTT; After refers to their self-assessed knowledge and competence state immediately after the SBTT Questionnaire 2: Follow-up refers to the self-assessed knowledge and competence state 4–6 months after the SBTT and a prediction of own future gain. Student denotes medical and nursing students. Professionals denotes newly graduated doctors, nurses and auxiliary nurses. All answers in the questionnaire were graded on a ten-point scale with verbal anchors: 1 = Almost always insecure and 10 = Almost always secure. Means and 95% confidence intervals are indicated. P-values refers to the change over time in a three factor repeated measurements analysis of variance (ANOVA).
At follow-up after participating in SBTT, participants assessed that their confidence in their own professional role was 6.8 (CI 6.4–7.2) in students and 8.6 (CI 8.2–8.9) in professionals (p < .0001). There was no difference in how they deemed that SBTT had contributed to their assessed professional role 7.8 (CI 7.4–8.1) and to their perceptions of patient safety in acute medical situations 7.8 (CI 7.5–8.2).
The global scoring of satisfaction with their simulation sessions did not differ and was 9.3 (CI 9.1–9.5) in students and professionals and their ratings of whether they should recommend SBTT to colleagues were almost similar 9.9 (CI 9.8–10.0), that is, they should all recommend the team-training to their colleagues.
Concerning all three professions, there was a significant statistical interaction of the changes in confidence after SBTT. The reason for this was that physicians had a significant increase in global confidence in acute care situations as compared to both nurses and auxiliary nurses (p < .0001).
Discussion
Regardless of previous level of competence and profession, participation in interprofessional simulation-based team-training was appreciated and resulted in an improved and sustained self-assessed global confidence in acute care situations, confidence in acute interprofessional communication, and in own capability to handle acute internal medical care in accordance with the A-B-C-D-E strategy.
The findings are in the short-time perspective in line with others (Colman et al., Citation2019; Kameg et al., Citation2010; Meurling et al., Citation2013; Paige et al., Citation2009). However, our study had an extended follow-up and included both healthcare professionals and students, and all SBTT was performed in a similar standardized interprofessional setting.
Given the design of the study, we cannot answer why newly graduated doctors had a greater increase in global confidence as compared to nurses and auxiliary nurses. But we know that the newly graduated doctors had fewer years in the profession than the other professional groups. Global professional confidence in acute care situations is a complex construct based on relevant medical knowledge, professional skills, and a professional approach to acute care situations. However, it is crucial for a professional to have a patient safe judging and approach in acute care situations. This necessitates situational understanding and a knowledge of how to behave professionally and in the interaction with others. Dall’Alba and Sandberg have described a two-dimensional framework for professional development (Dall’Alba & Sandberg, Citation2006). The first dimension describes development from a novice to an expert professional. The second dimension describes the development of an embodied understanding of and in practice. Dall’Alba and Sandberg state that the development in both these dimensions is needed to develop expertise in performance. Furthermore, active participation in and structured reflection and questioning in practice are needed to develop such an embodied understanding of and in practice. SBTT is designed to provide both learning in practice and structured feedback from credible persons, which have the possibility to contribute to understanding of practice and to enhance the capability to perform in practice.
Further, participants achieved an increased confidence in acute interprofessional communication. To communicate in a distinct and professional manner is crucial, especially when time is restricted as when taking care of critically ill patients. To develop skills to communicate in teams is therefore crucial to increase patient safety (Aldawood et al., Citation2020; Welp et al., Citation2016). Applying the terminology of Dall’Alba and Sandberg (Dall’Alba & Sandberg, Citation2006) professional development builds not only on professional skills development but also on a growing embodied understanding of practice and one´s own professional role in this practice. We argue that a low embodied understanding of and in practice might result in a substandard team coordination and a communication breakdown that might contribute to a patient's injury risk (Helmreich & Davies, Citation1996; Manser, Citation2009). SBTT provides structured training and reflection in a “practice alike” context perceived as authentic. We showed, as might be expected, that the confidence in acute interprofessional communication increased to a greater extent in students as compared to experienced professionals. However, even the professionals in this study did further increase their confidence in acute interprofessional communication. This was achieved in addition to the skills that they had achieved during their previous regular daily work. Given the design of the study, we could only speculate on the reasons. We hypothesize that the structured feedback on their team communication could have contributed to this increase. The contribution of feedback on learning has been shown in repeated studies (Yardley et al., Citation2012).
Confidence in assessing our own capability to handle acute medical care in accordance with the A-B-C-D-E strategy increased both immediately, and at follow-up in all participants regardless of previous experience. However, students had the greatest increase over time. This is expected as students, prior to participation in the SBTT, had almost no practical training in handling of acute care situations.
The A-B-C-D-E strategy is included in the standardized courses in Advanced Medical Life Support (AMLS) offered by the National Association of Emergency Medical Technicians. This course concept has been widely disseminated internationally. However, far from all professionals working in an emergency room, at least in Sweden, have passed these courses. The A-B-C-D-E strategy is only slowly evolving to become a routine strategy in the handling of all critically ill patients for immediate assessment and treatment. We believe that SBTT with its structured introduction, purposive design of scenarios, active participation and constructive feedback on its own and other’s adherence to the strategy was an effective means to learn the strategy, and to start to apply it in routine care.
Strengths and limitations
This study lacks objective outcome measures for training effects. The results are based on the assessments of self-efficacy in context-specified situations rather than objective competence assessments of participants handling of authentic acute care situations. However, evaluation of training effects is a complex task. Back in 1967 Kirkpatrick stated four possible effect levels: Reaction; Knowledge; Behavior; Outcome (Kirkpatrick, Citation1967). Further, he stated that the relevance increases at each level but the difficulty and complexity of evaluation increases in parallel. Given the design of the present study, it was only possible to assess the effects on the lowermost two levels. At the reaction level, we showed a high level of satisfaction with the SBTT and participants would willingly recommend it to others. At the knowledge level, we showed a high degree of self-assessed gain of confidence in medical knowledge, technical, and non-technical skills and of competence to, with confidence, judge and approach critically ill patients. It would have been valuable to add an objective measure on knowledge gain. However, to handle acute care situations is as stated previously a complex team-based task. We argue that to evaluate the causality between an intervention and effect on knowledge gain, especially at an individual level and in a long-term perspective is not doable. We made an initial attempt to evaluate performance in practice and patient outcome, but it turned out to be unfeasible for both practical and ethical reasons. Two studies have shown positive effects of SBTT on an outcome level. However, outcome data was collected during the SBTT sessions and no long-term follow-up was performed (Colman et al., Citation2019; Gilfoyle et al., Citation2017). We argue that, even with a control group, it is hardly possible to conduct a long-term cause effect study on a short-term educational intervention with an objective outcome measure. K Eva and G Regerh concluded based on a theory-oriented literature review that global self-assessment of competence is of limited value (Eva & Regehr, Citation2005). However, situationally bounded and context-specific self-assessments based on a cognitive process can be of higher value and need to be further studied. Therefore, the present study was designed to compare self-efficacy regarding competence, confidence, and performance in authentic context-specific acute emergency medicine situations before, immediately after and at six months after participation in SBTT. The rationale to choose self-efficacy as the main outcome measure was based on the Bandura self-efficacy theory described earlier in this paper (Bandura, Citation1997). In accordance with the findings by (Schunk & Pajares, Citation2009; Schunk & Usher, Citation2012) we argue that the long-term positive effects of SBTT may be associated with given structured feedback and support from credible persons. To perform structured self-efficacy assessments may have additional positive influence on motivation, self-regulation and future learning.
Finally, the resulting improvement was consistent both over time and between participants of different professions and with various preunderstandings and stages of experience. This consistency in improvement strengthens the argument that the positive effects were related to the SBTT and not only to further training. Future studies are needed to confirm our findings and also to attempt to combine objective effect measures during SBTT with long-term contextualized self-assessed effects.
Clinical implications
This study strengthens the evidence that it is feasible to introduce systematic interprofessional simulation-based team training from the early stages of clinical experience, as a complement to practice training in real work situations. We hypothesize that if all acute healthcare professionals and students regularly conducted interprofessional SBTT of emergency medicine, we would achieve significantly improved emergency team coordination and collaboration. This improved and sustained self-assessed confidence in acute medical emergency situations among participants in SBTT would have a positive impact on the future competence development both the structured and that on the job. This, in turn, has the potential to decrease communication failures and procedural errors and should contribute to increased patient safety in accordance with the A-B-C-D-E strategy. Furthermore, it has the potential to improve satisfaction with the working climate. This is especially important for both students and professionals in working situations that alter so frequently as those in emergency medicine, in resuscitation situations, trauma care, operating rooms and in intensive care units.
Conclusion
Regardless of previous experience and profession, interprofessional simulation-based team training is an effective means to develop sustainable confidence in emergency internal medicine situations; in acute interprofessional communication; and in self-efficacy to handle emergency medicine situations. The increased self-efficacy in emergency medicine situations was sustained over a six-month period. This indicates that interprofessional SBTT has a positive impact on competence development, and thereby a potential to contribute to increased quality and thereby patient safety in emergency medical care.
Data sharing statement
Additional data can be available by the corresponding author.
Ethics approval
Permission to carry out the study was given by the Regional Ethical Review Board, Stockholm Sweden, diary number 2013/1538-31.
Acknowledgements
The authors would like to acknowledge all participants for giving their time to take part in this study.
Disclosure statement
AK and JK took initiative to the study and designed it together with ML, JA and PH. Then the questionnaires and the SBTT scenarios were developed, and pilot tested. RMS and CW participated in the design of intervention, data collection and acted as instructors during the SBTT. CA and JW participated in student recruitment, development and data collection of the student SBTT. PH performed the validation and the analyses of the data. AK, JK and PH drafted the main parts of the manuscript and all authors provided a critical review of the manuscript.
Additional information
Funding
References
- Ahya, S. N., Barsuk, J. H., Cohen, E. R., Tuazon, J., McGaghie, W. C., & Wayne, D. B. (2012). Clinical performance and skill retention after simulation-based education for nephrology fellows. Seminars in Dialysis, 25(4), 470–473. https://doi.org/10.1111/j.1525-139X.2011.01018.x
- Aldawood, F., Kazzaz, Y., AlShehri, A., Alali, H., & Al-Surimi, K. (2020, February). Enhancing teamwork communication and patient safety responsiveness in a paediatric intensive care unit using the daily safety huddle tool. BMJ Open Quality, 9 (1), e000753. BMJ Open Qual. 2020. PMID: 32098776. https://doi.org/10.1136/bmjoq-2019-000753
- Bandura, A. (1997). Self-efficacy: The exercise of control. Freeman.
- Barsuk, J. H., Cohen, E. R., Vozenilek, J. A., O’Connor, L. M., McGaghie, W. C., & Wayne, D. B. (2012). Simulation-based education with mastery learning improves paracentesis skills. Journal of Graduate Medical Education, 4(1), 23–27. https://doi.org/10.4300/jgme-d-11-00161.1
- Carter, E. J., Pouch, S. M., & Larson, E. L. (2014). The relationship between emergency department crowding and patient outcomes: A systematic review. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau, 46(2), 106–115. https://doi.org/10.1111/jnu.12055
- Colman, N., Figueroa, J., McCracken, C., & Hebbar, K. (2019). Simulation-Based team training improves team performance among pediatric intensive care unit staff. Journal of Pediatric Intensive Care, 8(2), 83–91. https://doi.org/10.1055/s-0038-1676469
- Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., Wang, A. T., Erwin, P. J., & Hamstra, S. J. (2011). Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA, 306(9), 978–988. https://doi.org/10.1001/jama.2011.1234
- Dall’Alba, G., & Sandberg, J. (2006). Unveiling professional development: A critical review of stage models. Review of Educational Research, 76(3), 383–412. https://doi.org/10.3102/00346543076003383
- Dillon, P. M., Noble, K. A., & Kaplan, L. (2009). Simulation as a means to foster collaborative interdisciplinary education. Nursing Education Perspectives, 30(2), 87–90.
- Eva, K. W., & Regehr, G. (2005). Self-assessment in the health professions: A reformulation and research agenda. Academic Medicine: Journal of the Association of American Medical Colleges, 80(10 Suppl), S46–54. https://doi.org/10.1097/00001888-200510001-00015
- Flin, R., O’Connor, P., & Crichton, M. (2017). Safety at the sharp end: A guide to non-technical skills (1st ed.). CRC Press. https://doi.org/10.1201/9781315607467
- Fung, L., Boet, S., Bould, M. D., Qosa, H., Perrier, L., Tricco, A., Tavares, W., & Reeves, S. (2015). Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: A systematic review. Journal of Interprofessional Care, 29(5), 433–444. https://doi.org/10.3109/13561820.2015.1017555
- Gandhi, T. K., Kaplan, G. S., Leape, L., Berwick, D. M., Edgman-Levitan, S., Edmondson, A., Meyer, G., Michaels, D., Morath, J. M., Vincent, C., & Wachter, R. (2018). Transforming concepts in patient safety: A progress report. BMJ Quality & Safety, 27(12), 1019–1026. https://doi.org/10.1136/bmjqs-2017-007756
- Gilfoyle, E., Koot, D. A., Annear, J. C., Bhanji, F., Cheng, A., Duff, J. P., Grant, V. J., St. George-Hyslop, C. E., Delaloye, N. J., Kotsakis, A., McCoy, C. D., Ramsay, C. E., Weiss, M. J., & Gottesman, R. D. (2017). Improved clinical performance and teamwork of pediatric interprofessional resuscitation teams with a simulation-based educational intervention. Pediatric Critical Care Medicine: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 18(2), e62–e69. https://doi.org/10.1097/pcc.0000000000001025
- Hallin, K., Gordon, M., Sköldenberg, O., Henriksson, P., & Kiessling, A. (2018). Readmission and mortality in patients treated by interprofessional student teams at a training ward compared with patients receiving usual care: A retrospective cohort study. BMJ Open, 8(10), e022251. https://doi.org/10.1136/bmjopen-2018-022251
- Hallin, K., Henriksson, P., Dalen, N., & Kiessling, A. (2011). Effects of interprofessional education on patient perceived quality of care. Medical Teacher, 33(1), e22–26. https://doi.org/10.3109/0142159X.2011.530314
- Hallin, K., Kiessling, A., Waldner, A., & Henriksson, P. (2009). Active interprofessional education in a patient based setting increases perceived collaborative and professional competence. Medical Teacher, 31(2), 151–157. https://doi.org/10.1080/01421590802216258
- Helmreich, R. L., & Davies, J. M. (1996). 3 Human factors in the operating room: Interpersonal determinants of safety, efficiency and morale. Baillière’s Clinical Anaesthesiology, 10(2), 277–295. https://doi.org/10.1016/S0950-3501(96)80017-1
- Hinde, T., Gale, T., Anderson, I., Roberts, M., & Sice, P. (2016). A study to assess the influence of interprofessional point of care simulation training on safety culture in the operating theatre environment of a university teaching hospital. Journal of Interprofessional Care, 30(2), 251–253. https://doi.org/10.3109/13561820.2015.1084277. PMID: 26854195.
- Jankouskas, T. S., Haidet, K. K., Hupcey, J. E., Kolanowski, A., & Murray, W. B. (2011). Targeted crisis resource management training improves performance among randomized nursing and medical students. Simulation in Healthcare: Journal of the Society for Simulation in Healthcare, 6(6), 316–326. https://doi.org/10.1097/SIH.0b013e31822bc676
- Kameg, K., Howard, V. M., Clochesy, J., Mitchell, A. M., & Suresky, J. M. (2010). The impact of high fidelity human simulation on self-efficacy of communication skills. Issues in Mental Health Nursing, 31(5), 315–323. https://doi.org/10.3109/01612840903420331
- Kirkpatrick, D. L. (1967). Evaluation of training. In R. Craig & I. Bittel (Eds.), Training and development handbook. McGraw-Hill.
- Krage, R., Zwaan, L., Tjon Soei Len, L., Kolenbrander, M. W., van Groeningen, D., Loer, S. A., & Schober, P. (2017). Relationship between non-technical skills and technical performance during cardiopulmonary resuscitation: Does stress have an influence? Emergency Medicine Journal: EMJ, 34(11), 728–733. https://doi.org/10.1136/emermed-2016-205754
- Leape, L., Berwick, D., Clancy, C., Conway, J., Gluck, P., Guest, J., Lawrence, D., Morath, J., O’Leary, D., O’Neill, P., Pinakiewicz, D., & Isaac, T. (2009). Transforming healthcare: A safety imperative. Quality & Safety in Health Care, 18(6), 424–428. https://doi.org/10.1136/qshc.2009.036954
- Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: The critical importance of effective teamwork and communication in providing safe care. Quality & Safety in Health Care, 13 Suppl 1(Suppl 1), i85–90. https://doi.org/10.1136/qhc.13.suppl_1.i85
- Manser, T. (2009). Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143–151. https://doi.org/10.1111/j.1399-6576.2008.01717.x
- McGaghie, W. C., Issenberg, S. B., Petrusa, E. R., & Scalese, R. J. (2016, October). Revisiting ‘A critical review of simulation-based medical education research: 2003-2009.’ Medical Education, 50(10), 986–991. PMID: 27628715 Review. https://doi.org/10.1111/medu.12795
- Meurling, L., Hedman, L., Sandahl, C., Felländer-Tsai, L., & Wallin, C. J. (2013). Systematic simulation-based team training in a Swedish intensive care unit: A diverse response among critical care professions. BMJ Quality & Safety, 22(6), 485–494. https://doi.org/10.1136/bmjqs-2012-000994
- Nagpal, K., Arora, S., Vats, A., Wong, H. W., Sevdalis, N., Vincent, C., & Moorthy, K. (2012). Failures in communication and information transfer across the surgical care pathway: Interview study. BMJ Quality & Safety, 21(10), 843–849. https://doi.org/10.1136/bmjqs-2012-000886
- Nagpal, K., Vats, A., Lamb, B., Ashrafian, H., Sevdalis, N., Vincent, C., & Moorthy, K. (2010). Information transfer and communication in surgery: A systematic review. Annals of Surgery, 252(2), 225–239. https://doi.org/10.1097/SLA.0b013e3181e495c2
- Paige, J. T., Kozmenko, V., Yang, T., Paragi Gururaja, R., Hilton, C. W., Cohn, I., Jr., & Chauvin, S. W. (2009). High-fidelity, simulation-based, interdisciplinary operating room team training at the point of care. Surgery, 145(2), 138–146. https://doi.org/10.1016/j.surg.2008.09.010
- Paine, L. A., Rosenstein, B. J., Sexton, J. B., Kent, P., Holzmueller, C. G., & Pronovost, P. J. (2011). Republished paper: Assessing and improving safety culture throughout an academic medical centre: A prospective cohort study. Postgraduate Medical Journal, 87(1028), 428–435. https://doi.org/10.1136/pgmj.2009.039347rep
- Rönnerhag, M., Severinsson, E., Haruna, M., Berggren, I., and et al. (2019, March). A qualitative evaluation of healthcare professionals’ perceptions of adverse events focusing on communication and teamwork in maternity care. Journal of Advanced Nursing, 75(3), 585–593. Epub 2018 Nov 8.J Adv Nurs. 2019. PMID: 30264487. https://doi.org/10.1111/jan.13864
- Reese, C. E., Jeffries, P. R., & Engum, S. A. (2010). Learning together: Using simulations to develop nursing and medical student collaboration. Nursing Education Perspectives, 31(1), 33–37.
- Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017). Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Systematic Review, 6(6), Cd000072. https://doi.org/10.1002/14651858.CD000072.pub3
- Robertson, J. M., Dias, R. D., Yule, S., & Smink, D. S. (2017, May). Operating room team training with simulation: A systematic review. Laparoendoscopic and Advanced Surgical Techniques, 27 (5), 475–480. PMID: 28294695. https://doi.org/10.1089/lap.2017.0043
- Rosenman, E. D., Ilgen, J. S., Shandro, J. R., Harper, A. L., & Fernandez, R. (2015). A systematic review of tools used to assess team leadership in health care action teams. Academic Medicine: Journal of the Association of American Medical Colleges, 90(10), 1408–1422. https://doi.org/10.1097/ACM.0000000000000848
- Rotz, M. E., Dueñas, G. G., Zanoni, A., & Grover, A. B. (2016). Designing and evaluating an interprofessional experiential course series involving medical and pharmacy students. American Journal of Pharmaceutical Education, 80(5), 85. https://doi.org/10.5688/ajpe80585
- Royal College of Physicians and Surgeons of Canada, Optimizing crisis resource management to improve patient safety and team performance: A handbook for all acute care health professionals. 2017. http://www.royalcollege.ca/rcsite/ppi/educational-resources-e. Accessed 20 April 2020
- Salik, I., & Ashurst, J. V. (2019). Closed loop communication training in medical simulation.
- Schunk, D. H., & Pajares, F. (2009). Self-efficacy theory. In K. R. Wentzel & A. Wigfield (Eds.), Handbook of motivation at school (pp. 35–53). Routledge.
- Schunk, D. H., & Usher, E. L. (2012). Social cognitive theory and motivation. In R. M. Ryan (Ed.), The Oxford handbook of human motivation (pp. 13–27). Oxford University Press.
- Sigalet, E., Donnon, T., & Grant, V. (2012). Undergraduate students’ perceptions of and attitudes toward a simulation-based interprofessional curriculum: The kidsim attitudes questionnaire. Simulation in Healthcare: Journal of the Society for Simulation in Healthcare, 7(6), 353–358. https://doi.org/10.1097/SIH.0b013e318264499e
- Steyrer, J., Schiffinger, M., Huber, C., Valentin, A., & Strunk, G. (2013, Oct-December). Attitude is everything? The impact of workload, safety climate, and safety tools on medical errors: A study of intensive care units. Health Care Management Review, 38(4), 306–316. Health Care Manage Rev. 2013. PMID: 23085639. https://doi.org/10.1097/HMR.0b013e318272935a
- Symons, N. R., Almoudaris, A. M., Nagpal, K., Vincent, C. A., & Moorthy, K. (2013). An observational study of the frequency, severity, and etiology of failures in postoperative care after major elective general surgery. Annals of Surgery, 257(1), 1–5. https://doi.org/10.1097/SLA.0b013e31826d859b
- Thim, T., Krarup, N. H. V., Grove, E. L., Rohde, C. V., & Løfgren, B. (2012). Initial assessment and treatment with the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach. International Journal of General Medicine, 5, 117–121. https://doi.org/10.2147/IJGM.S28478
- Tofil, N. M., Morris, J. L., Peterson, D. T., Watts, P., Epps, C., Harrington, K. F., Leon, K., Pierce, C., & White, M. L. (2014). Interprofessional simulation training improves knowledge and teamwork in nursing and medical students during internal medicine clerkship. Journal of Hospital Medicine: An Official Publication of the Society of Hospital Medicine, 9(3), 189–192. https://doi.org/10.1002/jhm.2126
- Wang, Z., Feng, F., Gao, S., & Yang, J. (2019, December). A systematic meta-analysis of the effect of interprofessional education on health professions students’ attitudes. Journal of Dental Education, 83(12), 1361–1369. J Dent Educ. 2019. PMID: 31548305 Review. Epub 2019 Sep 23. https://doi.org/10.21815/JDE.019.147
- Welp, A., Meier, L. L., & Manser, T. (2016 Apr 19). The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: A longitudinal study. Critical Care / the Society of Critical Care Medicine, 20(1), 110. https://doi.org/10.1186/s13054-016-1282-9. Crit Care. 2016. PMID: 27095501.
- Westbrook, J. I., Li, L., Lehnbom, E. C., Baysari, M. T., Braithwaite, J., Burke, R., Conn, C., & Day, R. O. (2015). What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care / ISQua, 27(1), 1–9. https://doi.org/10.1093/intqhc/mzu098
- Yardley, S., Teunissen, P. W., & Dornan, T. (2012). Experiential learning: AMEE guide no. 63. Medical Teacher, 34(2), e102–115. https://doi.org/10.3109/0142159x.2012.650741