Abstract
Purpose
To explore women’s perception of the need for an ultrasound scan before medical abortion provided by telemedicine services.
Methods
We have analysed women’s requests for medical abortion through the website www.womenonweb.org from the 1st of January 2019 to the 5th of October 2020. Before receiving abortion drugs for self-managed medical abortion, women received online counselling and were asked to complete an online survey on pre-abortion ultrasound scan and the reasons for having or not having one. The initial dataset included 62641 entries from 207 countries. Each entry corresponded to a person’s request for medical abortion. Women reported only one or multiple reasons for not having a pre-abortion ultrasound scan.
Results
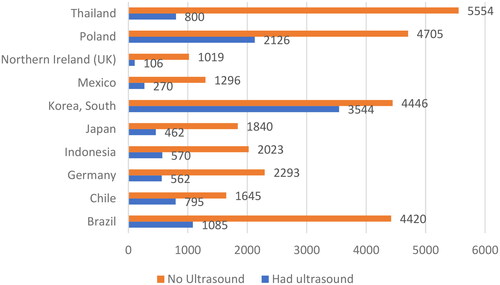
Among 59648 women requesting a medical abortion, 45653 (76,54%) did not have any pre-abortion ultrasound scan and specified a reason for that. The countries with the highest rates of women not having a pre-abortion ultrasound scan were Thailand, Poland, Northern Ireland, Mexico, South Korea, Japan, Chile, Indonesia, Germany, and Brazil. The main reasons for not having a pre-abortion ultrasound scan were being confident regarding pregnancy length; and thus, no need for a scan stated by 10910/34390 women (31.7%), lack of resources stated by 10589/34390 women (30.8%), and privacy issues stated by 6472/34390 women (18.8%).
Conclusion
Most women opting for medical abortion through telemedicine did not undergo a pre-abortion ultrasound scan. The main reason stated was that women did not find it necessary, lack of resources and privacy issues
SHORT CONDENSATION
Women requesting medical abortion through telemedicine were asked about their views and experiences regarding pre-abortion ultrasound scan. Of 59648 women included in the study, 76% did not have a scan. The main reason stated was that women did not find it necessary, lack of resources and privacy issues.
摘要
目的:探讨妇女对远程医疗服务提供的医疗流产前进行超声检查必要性的看法。
方法:我们分析了从2019年1月1日到2020年10月5日在www. womenonweb.org网站上妇女的流产要求。在服用自我管理的流产药物之前, 妇女接受了在线咨询, 并完成一项关于流产前超声检查以及进行或不进行超声检查的原因的在线调查。初始数据集包括来自207个国家的62641个条目。每个条目对应一个人的药物流产请求。妇女报告只有一个或多个原因没有进行流产前超声检查。
结果:在59648名要求药物流产的妇女中, 45653名(76.54%)未进行任何流产前超声检查, 并说明了原因。妇女未进行流产前超声波检查比例最高的国家是泰国、波兰、北爱尔兰、墨西哥、韩国、日本、智利、印度尼西亚、德国和巴西。不做流产前超声检查的主要原因是对妊娠时长有信心;因此, 10910/34390名女性(31.7%)表示不需要超声检查, 10589/34390名女性(30.8%)表示缺乏资源, 6472/34390名女性(18.8%)表示存在隐私问题。
结论:大多数通过远程医疗选择药物流产的妇女没有进行流产前超声检查。主要原因是妇女认为没有必要、缺乏资源和隐私问题。
短评
询问通过远程医疗请求药物流产的妇女对流产前超声扫描的看法和经历。在这项研究中的59648名女性中, 76%没有进行扫描。陈述的主要原因是妇女认为没有必要、缺乏资源和隐私问题。
Background
After the introduction of medical abortion, access to safe abortions has increased [Citation1]. Demedicalization and self-management may improve access to and acceptability of the procedure [Citation2,Citation3]. This includes the development of various models of telemedicine abortion provisions [Citation4]. Following the overturn of Roe vs. Wade, telemedicine has emerged as an option for women to have an abortion in the United States [Citation5].
Telemedicine has become a widely used, safe, and acceptable treatment for medical abortions worldwide [Citation4]. The provision of abortion drugs by mail was started by the non-governmental organisation Women on Web (WoW) to provide safe and effective family planning methods for women living in countries where abortion is restricted [Citation6]. Thousands of women received medications for the termination of pregnancy. Possible barriers to family planning services that can be overcome by telemedicine provision include obligatory counselling or waiting time for the first visit to the abortion clinic, a lack of anonymity, and travel expenses [Citation7]. The global pandemic caused by COVID-19 has limited women’s access to family planning services, even in countries where abortion is legal [Citation8]. As a response, telemedicine provision increased, and new models were developed and adjusted to the context [Citation4,Citation7,Citation9–13].
The provision of pre-abortion ultrasound scan for the determination of gestational length has become part of many national abortion guidelines for medical abortion. Women seeking help from WoW have also been encouraged to undergo an ultrasound scan to confirm pregnancy length [Citation6]. However, in many settings, ultrasound assessment is not available or implies an extra visit, increased costs, and increased waiting time, thus creating a barrier to abortion treatment. Studies have shown that ultrasound examinations can be omitted in most abortions [Citation13].
The World Health Organisation (WHO) safe abortion guidelines [Citation14] also state that ultrasound scan should not be a necessary part of pre-abortion procedures. Studies also indicate that women are satisfied with omitting the need for pre-abortion ultrasound scan [Citation15,Citation16] Other studies indicate that women may want to see the scan [Citation17–19].
The purpose of this study was to evaluate the use of ultrasound and reasons for non-use ultrasound among from a patient perspective among women who requested abortion through telemedicine from WoW.
Study design
This cross sectional study aimed to analyse women’s views on not using ultrasound evaluation before an abortion. We included women who requested medical abortion through the website www.womenonweb.org (WoW) from the 1st of January 2019 to the 5th of October 2020.
All women were asked to complete an online survey before receiving abortion drugs for self-administration. The online questionnaire included information about the type of pregnancy assessment (clinical diagnosis, ultrasound scan, or self-assessment), last menstrual period, availability of medical help within 60 min from the place of residence, presence of an intrauterine device or pelvic inflammatory disease, contraindications to mifepristone or misoprostol, medical history, history of previous pregnancies, c-section, and age. Data from the WoW database were anonymized and converted into Excel.
The primary outcome was women’s perception of the need for an ultrasound scan before the medical abortion procedure.
The secondary outcome was a comparison of the demographic characteristics of women who did or did not have a pre-abortion ultrasound scan.
In the pre-abortion online consultation women received the following information:” An ultrasound is important because it can determine the exact length of your pregnancy and can diagnose an ectopic pregnancy (a pregnancy outside the womb)”.
Women could choose the reason for not having a pre-abortion ultrasound scan: “I cannot afford one”, “I am unsure where to get one”, “I am afraid my partner or other people will find out”, “I cannot get to a clinic to get one because of distance or lack of transportation”, “I thought I did not need one as I am sure I am pregnant and I know how long I have been pregnant”, “I did not know that I needed one”, “I just did not have time to do it”.
Variables were registered as missing values if no answer was provided by women during the online consultation, or it was impossible to evaluate the answer.
We defined "main reason" for not undergoing a pre-abortion ultrasound scan if it was the sole reason indicated. The category “one of several reasons/multiple” was used when women selected several reasons for not having a pre-abortion ultrasound scan.Descriptive statistics were used to analyse the demographic characteristics of women.
Results
This dataset included 62641 entries from 207 countries. After excluding blank entries and entries that did not correspond to the subject of the answer, 59648 entries were analysed. The ten countries with the highest number of women who had not had a pre-abortion ultrasound scan were Thailand, Poland, Northern Ireland, Mexico, South Korea, Japan, Indonesia, Germany, Chile, Brazil. More women stated their gestational length as >7 weeks (25919) than as <7 weeks (19715).
Among the 59648 women requesting a medical abortion, 45653 (76,54%) did not have any pre-abortion ultrasound scan and specified a reason for that, while 14013 (23,46%) women stated that they had had a pre-abortion ultrasound scan. The demographic characteristics of the women with and without pre-abortion ultrasound scan did not differ significantly ( and ).
Table 1. Demographic characteristics of women who had a pre-abortion ultrasound.
Table 2. Reasons for not having a pre-abortion ultrasound scan.
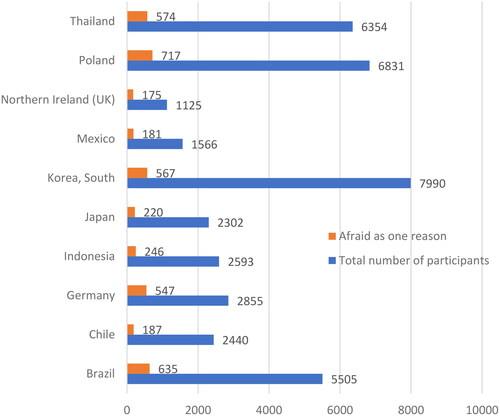
Among women from all countries who accessed the WoW website to have an abortion, the average percent who stated “I cannot afford one” as their main reason for not having a pre-abortion ultrasound scan was 20.9% (6.8%-35%). When this reason was combined with other reasons, the same figure was 20.9% (6.8%-35%). The average percent of women who stated “I am afraid my partner or other people will find out” as their main reason was 11.1% (2.3%-19.9%), and when this was combined with other reasons the figure was 17% (3.8%-30.2%). Lastly, the average percent of women who stated “I thought I did not need one as I am sure I am pregnant and I know how long I have been pregnant” as their only reason was 16.9% (4.4%-29.4%), and when this was combined with other reasons the figure was 27.3% (8.6%-46%) ().
Most women who did not undergo pre-abortion ultrasound scans were from Thailand, Poland, South Korea, and Brazil ( and ).
Figure 2. Distribution of women who state, “I thought I did not need one as I am sure I am pregnant, and I know how long I have been pregnant” by country.
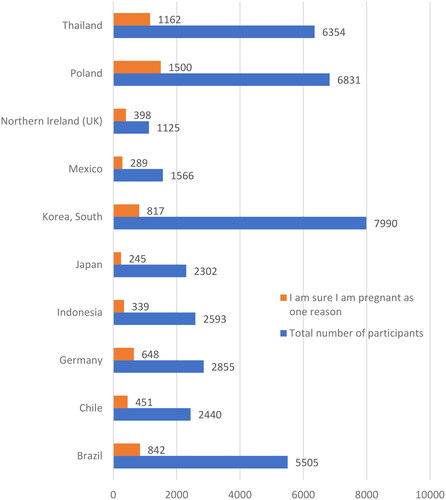
Figure 3. Distribution of women who stated as the main reason for not having ultrasound scan that they could not afford by country (Top 10 countries).
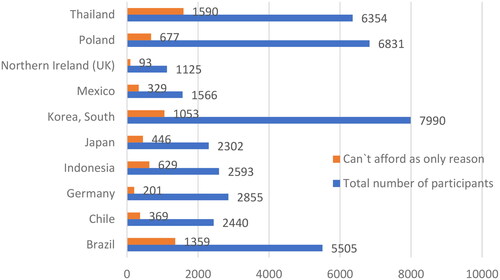
The largest number of women who could not afford to undergo pre-abortion ultrasound scan were from Thailand, Brazil and South Korea ().
Discussion
Our findings show that among women requesting a medical abortion through WoW, a large majority, 76,5%, did not have a pre-abortion ultrasound scan. The main reasons for not having a pre-abortion ultrasound scan were no perceived need, lack of resources, and privacy concerns. No large discrepancies were observed in whether the reason for not having a pre-abortion ultrasound scan was stated as the only reason or in combination with other reasons.
The use of telemedicine service for medical abortion has grown significantly in recent years. This is largely due to the increased access to WoW and similar organisations, web clinics that provide women with safe and legal abortion consultations, and procurement of abortion drugs for self-medication worldwide. This increase in demand can be attributed to several factors. Many countries have restrictions on abortion access, which makes it difficult or impossible to legally obtain an abortion through traditional means. Telemedicine provides access to safe and reliable services that may otherwise not be available. Additionally, as more people become aware of this service and its benefits, more can be expected to take advantage of it and the possibility for self-care [Citation9,Citation10]
A possible barrier to self-care in medical abortion is the common requirement for the pre-abortion ultrasound scan. This may be because of regulatory or perceived or actual medical reasons. However, guidelines on safe abortion issued by the WHO in 2022 included recommendations against pre-abortion ultrasound scan as a routine part of the abortion access. A pre-abortion ultrasound scan can provide dating of the pregnancy and clear visual evidence of the location and number of foetuses [Citation15]. However, in very early gestation, ultrasonography will not be able to locate the pregnancy. No perceived need was a major factor reported for not having an ultrasound scan in the current study. Studies on the self-assessment of pregnancy length, based on LMP and positive pregnancy test, and physical examination are highly effective instruments for evaluating eligibility for the abortion procedure accurate enough to avoid unnecessary ultrasound examination before abortion [Citation20]. Studies have also shown that self-assessment of pregnancy length based on LMP and positive pregnancy test is accurate enough [Citation20]. Indeed, the safety of using LMP or ultrasound scan to determine eligibility for medical abortion has been extensively studied. Research shows that both methods are equally safe for determining gestational age, with no significant difference in outcomes between abortions based on either LMP or ultrasound gestational dating [Citation20]. Another study found that the provision of medical abortion via telemedicine, without a prior pregnancy test and ultrasound (no-test MA), had comparable success rates to test-MA, and self-reported patient satisfaction was excellent for both groups [Citation13]. No-test MA allows patients to access medical abortions sooner and at a lower cost, but it is associated with a higher rate of unplanned in-person clinical encounters and interventions. The results do not show an increased risk of serious outcomes, and the use of no-test MA could facilitate a more equitable expansion of access to MA via telemedicine [Citation13].
A pre-abortion ultrasound could also be the wish of the pregnant person [Citation17]. A previous study found that women had an array of experiences viewing ultrasound images, and many expressed support for giving women the option to view the image even if they ultimately declined [Citation19].
Another major reason for not having a pre-abortion scan in the present study was cost. A previous study suggested that the most important reasons for not having medical abortions in clinics are a lack of resources and privacy concerns [Citation7]. Privacy concern was also among the most common reason for not having an ultrasound in our study. Ultrasound scans can be expensive, especially when a referral and/or extra visit is required, which is also time consuming. However, in line with our findings, previous studies have shown very little difference in the demographic characteristics of those who have undergone ultrasound and those who have not. This suggests that access to ultrasound scan does not appear to be mainly determined by socioeconomic status or other demographic factors, at least in terms of deciding whether or not to get one [Citation21].
While we found that the cost of an ultrasound was a significant factor influencing the decision of women not to undergo the procedure, we also noted that socioeconomic status didn’t appear to be a determining element in this decision-making process. This might seem contradictory at first glance, but it can be reconciled by considering other aspects that influence healthcare choices.
For instance, regardless of their socioeconomic status, women might prioritise their financial resources differently, and some might perceive the cost of ultrasound as a burden, irrespective of their overall wealth. This could be especially relevant in contexts where healthcare expenses are out-of-pocket and immediate, as opposed to being spread over time or covered by insurance.
It’s also plausible that perceptions of cost-effectiveness could be at play here, whereby women of all socioeconomic strata deem the ultrasound as an unwarranted expenditure, particularly if they are confident about their gestational age and perceive no immediate medical benefit from the procedure.
A possible limitation with our study is that there is no information available regarding the outcome of the abortion, however our aim was not to determine the effectiveness of pre-abortion ultrasound but the reasons that women gave for not having a scan prior to their self-managed medical abortion in different contexts. The results rely on self-reported data, which may lead to potential inaccuracies or bias in the results. A strength of the study lies in its large dataset of nearly 60,000 women from low-, middle- and high-income countries with different legal situations, providing a comprehensive view of the use of pre-abortion ultrasound.
The WHO recommends that pregnant women should only receive ultrasound when medically indicated or if they have specific concerns about their pregnancy (WHO 2022). Our study supports that a majority of women chose to have their abortion treatment without the pre-abortion scan. It is likely that this group would have been even larger if the online counselling had not recommended a scan. Updating guidelines in line with the WHO safe abortion guideline would help ensure better access to care for those who need it most by eliminating unnecessary tests or procedures that require additional resources or costs more than necessary without providing any additional benefit. Many countries do not have adequate access to medical care due to financial constraints; therefore, limiting unnecessary testing can help reduce costs while still ensuring that quality healthcare services are available where needed.
We seek to underscore the importance of understanding women’s perspectives on not having a pre-abortion ultrasound. While our research objective may align with existing research, the expansive and diverse sample utilised in this study enables us to make a contribution to the current body of knowledge.Our study encompasses a broad spectrum of participants, selected from varied demographics and geographical locations.
Our findings by reaffirming and expanding upon previous work, enrich the discourse on the importance of women’s preferences in abortion care.
Conclusion
A majority of women who self-managed their abortion supported by WOW did not have a pre-abortion ultrasound scan due to different reasons such as lack of perceived need, but also lack of resources, and privacy concerns. Previous studies show that a routine pre-abortion ultrasound can be omitted, especially if it leads to unnecessary delays and additional costs for the patient. Eliminating this requirement can help reduce barriers to accessing abortion care and ensure that women have access to safe and timely care, and for those who prefer self-care.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Gemzell-Danielsson K, Cleeve A. Estimating abortion safety: advancements and challenges. Lancet. 2017;390(10110):2333–2334. doi: 10.1016/S0140-6736(17)32135-9.
- Afable-Munsuz A, Gould H, Stewart F, et al. Provider practice models for and costs of delivering medication abortion—evidence from 11 US abortion care settings. Contraception. 2007;75(1):45–51. doi: 10.1016/j.contraception.2006.09.009.
- World Health Organization. Health worker role in providing safe abortion care and post abortion contraception. Geneva: World Health Organization; 2015.
- Endler M, Lavelanet A, Cleeve A, et al. Telemedicine for medical abortion: a systematic review. BJOG. 2019;126(9):1094–1102. doi: 10.1111/1471-0528.15684.
- DeNicola N, Grossman D, Marko K, et al. Telehealth interventions to improve obstetric and gynecologic health outcomes. Obstet Gynecol. 2020;135(2):371–382. doi: 10.1097/AOG.0000000000003646.
- Gomperts R, Jelinska K, Davies S, et al. Using telemedicine for termination of pregnancy with mifepristone and misoprostol in settings where there is no access to safe services. BJOG. 2008;115(9):1171–1178. doi: 10.1111/j.1471-0528.2008.01787.x.
- Aiken ARA, Guthrie KA, Schellekens M, et al. Barriers to accessing abortion services and perspectives on using mifepristone and misoprostol at home in Great Britain. Contraception. 2018;97(2):177–183. doi: 10.1016/j.contraception.2017.09.003.
- Aiken ARA, Starling JE, Gomperts R, et al. Demand for self-managed online telemedicine abortion in eight european countries during the COVID-19 pandemic: a regression discontinuity analysis. BMJ Sex Reprod Health. 2021;47(4):238–245. doi: 10.1136/bmjsrh-2020-200880.
- Killinger K, Günther S, Gomperts R, et al. Why women choose abortion through telemedicine outside the formal health sector in Germany: a mixed-methods study. BMJ Sex Reprod Health. 2022;48(e1):e6–12–e12. doi: 10.1136/bmjsrh-2020-200789.
- Atay H, Perivier H, Gemzell-Danielsson K, et al. Why women choose at-home abortion via teleconsultation in France: drivers of telemedicine abortion during and beyond the COVID-19 pandemic. BMJ Sex Reprod Health. 2021;47(4):285–292. doi: 10.1136/bmjsrh-2021-201176.
- van Ooijen LT, Gemzell-Danielsson K, Waltz M, et al. A trans-national examination of the impact of the COVID-19 pandemic on abortion requests through a telemedicine service. BMJ Sex Reprod Health. 2022;48(3):179–184. doi: 10.1136/bmjsrh-2021-201159.
- Brandell K, Vanbenschoten H, Parachini M, et al. Telemedicine as an alternative way to access abortion in Italy and characteristics of requests during the COVID-19 pandemic. BMJ Sex Reprod Health. 2022;48(4):252–258. doi: 10.1136/bmjsrh-2021-201281.
- Aiken A, Lohr P, Lord J, et al. Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021;128(9):1464–1474. doi: 10.1111/1471-0528.16668.
- World Health Organization. WHO consolidated guideline on self-care interventions for health: sexual and reproductive health and rights. Geneva: WHO; 2019.
- Schmidt‐Hansen M, Cameron S, Lord J, et al. Initiation of abortion before there is definitive ultrasound evidence of intrauterine pregnancy: a systematic review with meta‐analyses. Acta Obstet Gynecol Scand. 2020;99(4):451–458. doi: 10.1111/aogs.13797.
- Heller R, Cameron S. Termination of pregnancy at very early gestation without visible yolk sac on ultrasound. J Fam Plann Reprod Health Care. 2015;41(2):90–95. doi: 10.1136/jfprhc-2014-100924.
- Andersson IM, Christensson K, Gemzell-Danielsson K. Experiences, feelings and thoughts of women undergoing second trimester medical termination of pregnancy. PLoS One. 2014;9(12):e115957. doi: 10.1371/journal.pone.0115957.
- Wiebe ER, Adams L. Women’s perceptions about seeing the ultrasound picture before an abortion. Eur J Contracept Reprod Health Care. 2009;14(2):97–102. doi: 10.1080/13625180902745130.
- Kimport K, Upadhyay UD, Foster DG, et al. Patient viewing of the ultrasound image prior to abortion. Contraception. 2013;88(5):666–670. doi: 10.1016/j.contraception.2013.07.006.
- Ralph LJ, Ehrenreich K, Barar R, et al. Accuracy of self-assessment of gestational duration among people seeking abortion. Am J Obstet Gynecol. 2022;226(5):710.e1-710–e21. doi: 10.1016/j.ajog.2021.11.1373.
- Bizjak I, Fiala C, Berggren L, et al. Efficacy and safety of very early medical termination of pregnancy: a cohort study. BJOG. 2017;124(13):1993–1999. doi: 10.1111/1471-0528.14904.