Abstract
Objective
To compare the performance of the abdominal handheld point-of-care ultrasonography (POCUS) Butterfly-iQ to gold standard transvaginal ultrasonography (US) in identifying the position of intrauterine devices (IUDs) in the hands of a medical doctor specialised in ultrasonography.
Methods
In this diagnostic accuracy study, a single operator conducted abdominal POCUS followed by conventional transvaginal US. Seventy patients utilising copper or hormonal IUDs were assessed between June 2021 and October 2022. IUDs were categorised as entirely within the uterine cavity or malpositioned. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated for detecting malpositioned IUDs, with conventional US results serving as the reference standard. Concordance rate and Kappa coefficient were computed to assess the agreement between the two ultrasound modalities.
Results
Among the 70 patients, 46 (65.7%) used copper IUDs, and 24 (34.3%) used hormonal IUDs. Conventional transvaginal US showed IUDs entirely within the uterine cavity in 56 (80%) patients and 14 (20%) IUDs were malpositioned. Of the 14 malpositioned IUDs seen by conventional US, POCUS identified 13 demonstrating a sensitivity of 92.9% (66.1–99.8). Of the 56 IUDs entirely within the uterine cavity shown by conventional US, only two cases were considered malpositioned by POCUS demonstrating a specificity of 96.4% (87.7–99.6). The concordance rate was 95.7%, and the Kappa value was 0.87 in differentiating between IUDs entirely within the uterine cavity and those that were malpositioned.
Conclusion
Abdominal POCUS using Butterfly-iQ, when administered by an imaging specialist, exhibited excellent performance in confirming IUDs entirely within the uterine cavity.
SHORT CONDENSATION
Through a smartphone-based handheld point-of-care ultrasonography it was possible to correctly evaluate the position of intrauterine devices (IUDs) in a sample of 70 patients (46 using copper and 24 using hormonal IUDs).
摘要
目的
比较专业超声医师应用经腹手持床旁即时超声(PICUS) Butterfly-iQ与金标准经阴道超声(US)在确定宫内节育器(IUD)位置方面的表现。
方法
在这项诊断准确性研究中, 同一操作者先进行经腹POCUS检查, 然后进行传统的经阴道超声检查。在2021年6月至2022年10月期间, 对70名带含铜或激素的宫内节育器的患者进行了评估。宫内节育器的位置分为完全在宫腔内或移位。计算检测宫内节育器移位的敏感度、特异度、阳性预测值(PPV)、阴性预测值(NPV)和准确度, 以传统US结果作为参考标准。计算一致性指数和Kappa系数以评估两种超声方法之间的一致性。
结果
70例患者中, 46例(65.7%)应用含铜宫内节育器, 24例(34.3%)应用释放激素的宫内节育器。常规经阴道超声显示56例(80%)患者宫内节育器完全位于宫腔内, 14例(20%)宫内节育器移位。在传统经阴道超声发现的14例移位宫内节育器中, POCUS确定了13例, 敏感性为92.9%(66.1-99.8)。传统经阴道超声显示完全位于宫腔内的56个宫内节育器中, 仅2例被POCUS确定为宫腔移位, 其特异度为96.4%(87.7-99.6)。完全位于宫腔内的宫内节育器与移位宫内节育器的一致性指数为95.7%, Kappa值为0.87。
结论
在由影像专家进行经腹超声时, 应用Butterfly-iQ确认完全位于宫腔内的宫内节育器具有很好的效果。
Introduction
In the last 12 years, encouraging results about the performance of point-of-care ultrasound (POCUS) in obstetrics and gynaecology (OB/GYN) have been obtained. Studies showed good to excellent agreement between POCUS and conventional ultrasonography (US) in the following OB/GYN conditions: uterine position, presence of fibroids, presence of endometrial pathology, presence and type of adnexal pathology, viability of early intrauterine pregnancy, fetal presentation, femur length, placenta location, fetal weight and peripartum maternal critical illness such as pleural effusion [Citation1–5]. Moreover, breast and obstetric volume sweep imaging (VSI) acquired with POCUS by operators with no prior ultrasound experience showed satisfactory agreement with the standard US performed by experts [Citation6, Citation7].
The evolution of portable ultrasound machines encompasses physical mechanisms of image acquisition, image resolution, data storage, data sharing, and size reduction of ultrasound devices [Citation8]. Some of the pocket probes more recently developed are smartphone-based devices, which in addition to allowing rapid information after physical examination, enable image transmission for remote evaluation by an expert [Citation2, Citation9].
Intrauterine contraceptives include the copper intrauterine device and the levonorgestrel-releasing intrauterine device. These contraceptive modalities belong to the category of long-acting reversible contraceptives (LARCs), distinguished by their heightened contraceptive efficacy [Citation10]. Approximately 17% of female contraceptive users opt for intrauterine devices (IUDs), with the copper IUD being the most commonly utilised reversible contraceptive globally [Citation11]. After the IUD is inserted, a physical examination involving the observation of the string is typically deemed sufficient for evaluating the IUD’s positioning. Nonetheless, certain types of malposition, such as the embedding of the stem in the myometrium, might escape detection, as this particular placement does not affect the length of the strings protruding from the os. The continued presence of symptoms, such as vaginal bleeding six months post-insertion, further underscores the potential utility of ultrasonography in assessing the IUD's status [Citation12–15]. Moreover, in recent decades there has been an expansion of IUD insert procedures related to the greater accessibility, the increased acceptability and use by young nulliparous women, the indication of insertion in the immediate postpartum period, and the role in treating patients presenting with abnormal uterine bleeding. Under some of these referred circumstances, expelled IUD rates may be greater than those previously reported [Citation16–19]. This study aimed to compare the performance of the abdominal handheld point-of-care ultrasonography (POCUS) Butterfly-iQ to gold standard transvaginal ultrasonography in identifying the position of intrauterine devices in the hands of a medical doctor specialised in ultrasonography.
Methods
This study was conducted in Prof. José Aristodemo Pinotti Women’s Hospital, CAISM, Campinas, Brazil, between June 2021 and October 2022. After signing the informed consent form, 165 consecutive patients who had been referred from two outpatient clinics (Cervical Pathology and Family Planning) were selected to undergo abdominal POCUS and conventional transvaginal US. These patients were referred to a specific schedule of one of the researchers (KGA) in the Ultrasound Section. For the statistical evaluation of this study, we enrolled all those who used copper or hormonal IUDs, which totalled 70 patients. The reasons for the US requests were mainly pelvic pain, abnormal uterine bleeding, and IUD position assessment (due to missing IUD string, history of previous IUD expulsion, difficult IUD insertions, or other circumstances in which the gynaecologist thought appropriate). In all the study participants ultrasound examinations were performed at an interval greater than 30 days after IUD insertion. Baseline data and ultrasound features of the study participants were logged in a data collection sheet in Excel (Microsoft Corp., Redmond, WA, USA). Data is available on request from the corresponding author.
Written informed consent was obtained from all included patients. The study was approved by the University’s Research Ethics Committee and by the National Brazilian National Research Ethics Committee (protocol 42981320000005404). For clinical management purposes, the ultrasound report was given based on the findings of the conventional US.
Ultrasonography
Ultrasound machines used were the handheld POCUS Butterfly-iQ (Butterfly Network, Guilford, CT, USA) () and one of the conventional high-definition devices: Logiq P9 (GE HealthCare, Anaheim, CA, USA) or Toshiba Xario SSA-660A (Toshiba Medical Systems Corp., Otawara, Japan). Although studies have shown improvements in the evaluation of the IUD by the three-dimensional ultrasound (3D-US) technique, in this study we chose to consider 2D-US as the gold standard because it is more available and used in a large number of care centres.
Figure 1. Photography of the POCUS Butterfly-iQ device connected to the smartphone used in this study. OB 1/GYN was the chosen preset.
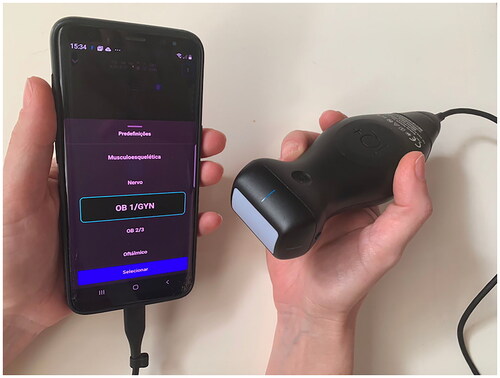
Butterfly-iQ is a device developed with a new technology that replaces traditional piezoelectric crystal material with an ultrasound-on-chip technology, which allows the use of a single transducer to evaluate different regions of the body, reducing costs and increasing portability. This transducer connects to a smartphone or tablet running the Butterfly app so that the image is shown on the screen of the mobile device [Citation9, Citation20]. We used Galaxy S8 (Samsung Electronics Co, ltd, Maetandong, Yeongtong District, Suwon, South Korea) that was compatible with Butterfly-iQ during the period of the study. This smartphone has a screen size of 147.3 mm (diagonal diameter).
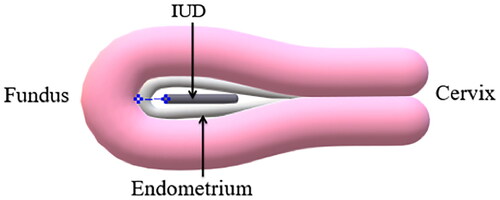
POCUS and the conventional US were performed by one single gynaecologist with a subspecialization in ultrasonography, with full annual ultrasound training at a university hospital after obstetrics and gynaecology residency and more than 15 years of daily practice involving gynaecological ultrasound examinations. Initially, POCUS was performed by a transabdominal approach, with a full or partially filled bladder, then a standard transvaginal scan, with the patient’s bladder empty, was performed during the same visit. Uterine position (anteversion, midline, and retroversion), uterine volume (longitudinal × anteroposterior × transverse diameters × 0.523), and endometrial thickness were evaluated. If the endometrium was not clear it was referred to as not measurable. Other pelvic findings were assessed, but not used in current statistical analysis. Patients used the copper-bearing Tcu-380A intrauterine device (copper IUD) or the 52 mg levonorgestrel-releasing intrauterine device (hormonal IUD). No patients were using the frameless copper IUD. An IUD was identified when both border points of the stem were seen. The position of the IUD was described according to the ultrasound findings by each type of US machine as entirely within the uterine cavity or malpositioned. The IUD was considered entirely within the uterine cavity if the end of the device was above the internal cervical os with no portion in the myometrium. The ones embedded in the myometrium and/or with some degree of expulsion, i.e., with their ends below the internal cervical os were considered malpositioned.
In our study, malpositioned IUDs in expulsion were subclassified into the following situations: <50% within the cervical canal, between 50 and 99% within the cervical canal, and 100% within the cervical canal. We registered the distance between the top of the IUD and the myometrium (the IUD-myometrium distance) () only in cases where the IUD was entirely within the uterine cavity. We did not consider the low-lying IUDs with IUD-myometrium distance greater than 1 cm and the end above the internal cervical os as malpositioned. We found only one IUD with abnormal intrauterine orientation (axial rotation) by the transvaginal US. For statistical evaluation, this case entered the group ‘entirely within the uterine cavity’.
Statistical analysis
All statistical calculations were performed with the R Environment for Statistical Computing (R Core Team, Vienna, Austria) [Citation21]. Statistical calculations were performed using 95% CIs, with p < 0.05 considered significant. Firstly, we compared a few key clinical and demographic features of the patients using either copper IUD or hormonal IUD using Kruskal-Wallis and Chi-squares as indicated. Next, we calculated the performance indicators (sensitivity, specificity, positive and negative predictive values) for POCUS and conventional ultrasound to diagnose the IUD position inside the uterus. We also estimated the agreement between POCUS and conventional ultrasound to determine the IUD position inside the uterus.
Results
According to the gathered data as shown in , among the 70 enrolled patients, 46 (65.7%) used copper IUDs and 24 (34.3%) used hormonal IUDs. Both groups of patients were similar regarding mean age, body mass index (BMI), history of previous infra umbilical laparotomy, and clinical features.
Table 1. Baseline characteristics of subjects.
shows in detail the IUD position found by both types of ultrasound machines. Conventional transvaginal US identified 56 (80%) entirely within the uterine cavity IUDs and 14 (20%) malpositioned IUDs. Of the 14 malpositioned IUDs seen by conventional US, POCUS identified 13 demonstrating a sensitivity of 92.8% (66.1–99.8). Of the 56 IUDs entirely within the uterine cavity shown by conventional US, only two cases were considered malpositioned by POCUS demonstrating a specificity of 96.4% (87.7–99.6) (). We found an agreement rate of 95.7% in differentiating between entirely within the uterine cavity and malpositioned IUDs and a kappa value of 0.87 (). Considering the 46 patients using copper IUDs separately, the agreement rate was 97.8% with an excellent kappa value (0.95). The group of patients with hormonal IUDs contained only 24 subjects, and in this group, we found a lower agreement rate (87.5%) and a kappa value of 0.22. The low prevalence of the condition (only two malpositioned hormonal IUDs) might have affected the kappa statistic for this group.
Table 2. Detailed IUD position found by abdominal POCUS and conventional transvaginal US.
Table 3. Diagnostic performance of abdominal POCUS in predicting IUD malposition.
Table 4. Agreement between abdominal POCUS and conventional transvaginal US in detecting IUD position.
In the group of six patients in which conventional US identified a small part of the IUD within the cervical canal (<50% within the cervical canal), POCUS detected four correctly, one embedded in the myometrium and one entirely within the uterine cavity. Yet, POCUS showed <50% of the IUD within the cervical canal in one patient, but it was 100% within the uterine cavity according to conventional US. We did not have cases of inverted IUD (upside-down), evidence of transmural migration through the serosa, or complete expulsion of IUD.
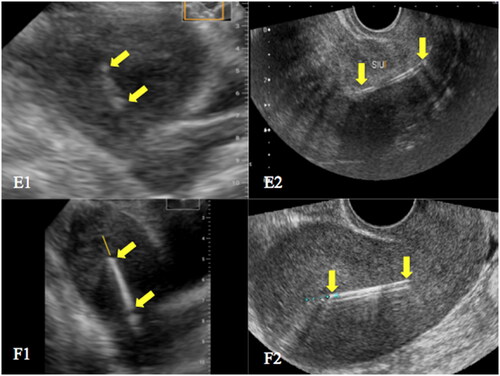
Among the three cases that POCUS revealed IUD embedded in the myometrium, only one was confirmed by conventional US. shows examples of true negative cases with IUDs entirely within the uterine cavity. shows true positive cases: an IUD embedded in the myometrium and an IUD within the cervical canal. Examples of false positive and false negative results are given in .
Figure 3. Ultrasonographic images. A - copper IUD entirely within the uterine cavity in a retroverted uterus by both POCUS (A1) and conventional US (A2); B - hormonal IUD entirely within the uterine cavity in an anteverted uterus by both POCUS (B1) and conventional US (B2). The top and the distal end of the IUDs are indicated by yellow arrows.
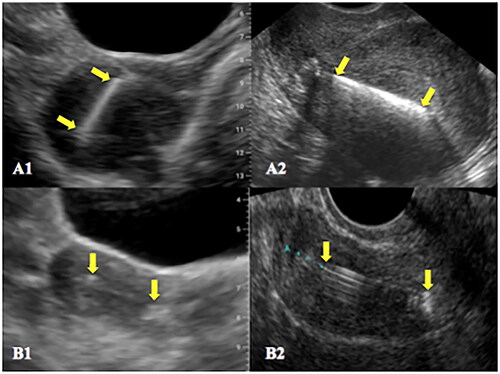
Figure 4. Ultrasonographic images. C - copper IUD entirely within the cervical canal by both POCUS (C1) and conventional US (C2); D - copper IUD embedded in the myometrium by both POCUS (D1) and conventional US (D2). The top and the distal end of the IUDs are indicated by yellow arrows. Asterisks indicate the fundal region of the endometrial cavity.
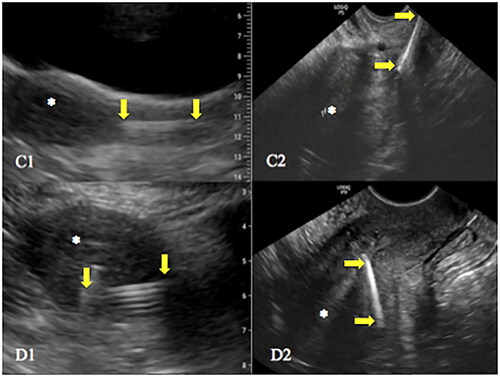
Figure 5. Ultrasonographic images. E - hormonal IUD identified as entirely within the uterine cavity by POCUS (E1) and the same IUD with a small portion within the cervical canal identified by conventional US (E2); F - a small part of a copper IUD apparently within the cervical canal found by POCUS (F1) and the same IUD entirely within the uterine cavity by conventional US (F2). The top and the distal end of the IUDs are indicated by yellow arrows. In the image F1, the proximal portion of the string was probably mistaken for the end of the IUD.
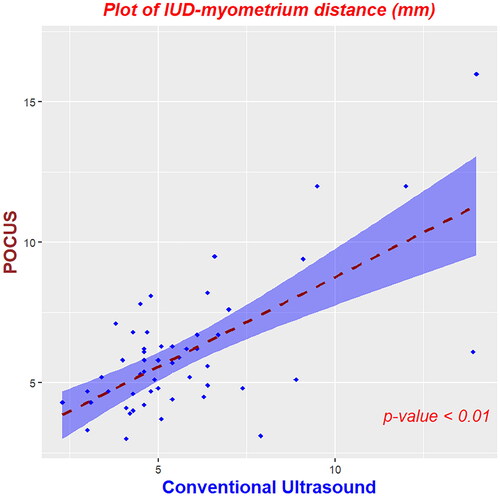
shows a plot with the concordance in IUD-myometrium distance between the two types of US machines. We found six cases of low-lying IUDs detected by one of the types of US, but these cases were not considered malpositioned. They were included in the group entirely within the uterine cavity IUDs. shows case-by-case, IUD-myometrium distances and subjective assessment by POCUS and conventional US in cases of intracavitary low-lying IUDs with a top greater than 10 mm of the myometrium.
Table 5. Case-by-case differences in IUD-myometrium distance and subjective impression for low-lying IUDs found by POCUS and/or conventional US.
Type of IUD, body mass index (BMI), previous infra umbilical laparotomy, endometrial thickness, not measurable endometrium, and uterine position did not affect the agreement between POCUS and conventional US. Nevertheless, uterine volume was marginally significant ().
Table 6. Clinical and ultrasound features that may affect the agreement between abdominal POCUS and conventional transvaginal US.
Discussion
We mainly focused our study on evaluating the feasibility of abdominal POCUS to detect IUDs above and below the internal cervical os, and the ones embedded in the myometrium as they are findings of greater clinical relevance. Although other types of IUD displacement such as abnormal intrauterine orientation and IUD lying lower down in the uterine cavity are frequently mentioned in reports of conventional transvaginal US, scientific societies have suggested the possibility of maintaining the IUD in these situations if in agreement with asymptomatic patients [Citation22]. One reason to consider expectant management in cases of low-lying IUD is that its retention is associated with lower pregnancy rates than removal due to the low rate of initiation of another effective contraception [Citation23].
We have chosen the myometrium-IUD distance instead of the endometrium-IUD distance because we consider it more feasible by the abdominal approach. When there was a sign of IUD expulsion, the measure of this distance was not registered, because the information about the presence of the IUD within the cervical canal became more important for clinical management purposes. In our institution, we have not used the IUD-fundus distance due to variations in myometrial thickness between patients.
We noticed a higher agreement rate between the US machines in the evaluation of copper IUDs (97.8%) compared to hormonal IUDs (87.5%). Although the difference is not statistically significant, it may point to a likely reason for these results. While sonographic identification of a copper IUD is facilitated by its echogenicity, the same is not true for the hormonal IUD. Often, only the proximal and distal ends of the shaft are visible in the sagittal plane [Citation24], as illustrated in .
As far as we know, no previous studies have evaluated the agreement between an abdominal handled POCUS and a transvaginal US in assessing the IUD position. In our study, for all study participants, the IUD was identified by abdominal POCUS, even in obese patients, in those with previous infra umbilical laparotomy, in the retroverted uterus, and when the IUD in question was the hormonal one. We found almost perfect agreement in the distinction between intracavitary and malpositioned IUDs, as well as among different subclassifications of malpositioned IUDs.
A limitation of our study is the low number of malpositioned IUDs, which might preclude a reliable generalisation about the assessment of these cases. Furthermore, POCUS and conventional US were both performed by a single experienced imaging specialist. The question remains whether non-imaging specialists will also properly locate the IUDs by the abdominal POCUS. Based on our results, it is difficult to predict whether gynaecologists, even after little training in ultrasonography, will be able to adequately identify the uterus and the sonographic signs related to the presence of the IUD within the uterine cavity, especially in the evaluation of hormonal IUDs that often appear subtly through abdominal assessment. As the Butterfly-iQ is a new device not yet approved in Brazil and has not been used before by the investigators and in our institution, we think it was important for a specialist to get used to the particularities of the machine and to know its potential in advance before starting training other professionals with this or other handheld US, which has been the second stage of our research.
In recent years, indications for the use of IUDs for contraception purposes, and some types of gynaecological treatment have increased and consequently the absolute number of IUD complications [Citation19, Citation25–27]. Although routine ultrasonographic evaluation of IUD position is not indicated, it is necessary to evaluate those patients who present with symptoms concerning expulsion, missing or longer IUD strings, or those with risk factors that increase the likelihood of expulsion or malposition [Citation22]. The availability of a POCUS may allow immediate assessment during or after difficult IUD insertions and at follow-up outpatient visits. It can be useful, especially in low-resource countries, where part of the population has little access to health care and ultrasound examinations [Citation28]. Another point to be considered is that the abdominal assessment of this type of POCUS is less invasive. A diagnostic tool that avoids the transvaginal route after gynecological physical examinations and often painful IUD insertion procedures could bring benefits to patient care.
Conclusion
POCUS Butterfly-iQ in the hands of an imaging specialist has an excellent performance in confirming IUDs that are entirely within the uterine cavity. Further studies are necessary with more cases of malpositioned IUDs as well as with less experienced examiners.
Acknowledgments
KGA was supported by Coordination of Improvement of Higher Education Personnel - Brazil (Capes) - 88887.372719/2019-00. National Council for Scientific and Technological Development (CNPq) supported SD and LOS, grants numbers 304544/2022-1 and 308871/2021-9, respectively. We would like to thank Prof. Dr. Rodrigo Menezes Jales, director of medical imaging at Prof. José Aristodemo Pinotti Women’s Hospital, CAISM, University of Campinas, Unicamp, for his kind support in carrying out this study.
Disclosure statement
The authors declare that they have no competing interests. The institution and the authors did not receive any payment or benefit from the ultrasound machines or smartphone companies cited in this study.
References
- Sayasneh A, Preisler J, Smith A, et al. Do pocket-sized ultrasound machines have the potential to be used as a tool to triage patients in obstetrics and gynecology? Ultrasound Obstet Gynecol. 2012;40(2):145–150. doi: 10.1002/uog.11184.
- Toscano M, Szlachetka K, Whaley N, et al. Evaluating sensitivity and specificity of handheld point-of-care ultrasound testing for gynecologic pathology: a pilot study for use in low resource settings. BMC Med Imaging. 2020;20(1):121. (published online ahead of print October 27, 2020)doi: 10.1186/s12880-020-00518-8.
- Pedersen JK, Sira C, Trovik J. Handheld transabdominal ultrasound, after limited training, may confirm first trimester viable intrauterine pregnancy: a prospective cohort study. Scand J Prim Health Care. 2021;39(2):123–130. doi: 10.1080/02813432.2021.1910643.
- Bajwa SJS, Kurdi MS, Sutagatti JG, et al. Point-of-care ultrasound (POCUS) for the assessment of volume status and fluid management in patients with severe pre-eclampsia: a systematic review and meta-analysis. Indian J Anaesth. 2021;65(10):716–730. doi: 10.4103/ija.ija_820_21.
- Leggett CB, Naqvi M, Esakoff TF, et al. Incorporating personal-device-based point-of-care ultrasound into obstetric care: a validation study. Am J Obstet Gynecol. 2022;226(4):552.e1-552–e6. doi: 10.1016/j.ajog.2021.11.031.
- Marini TJ, Castaneda B, Iyer R, et al. Breast ultrasound volume sweep imaging: a new horizon in expanding imaging access for breast cancer detection. J Ultrasound Med. 2023;42(4):817–832. doi: 10.1002/jum.16047.
- Toscano M, Marini TJ, Drennan K, et al. Testing telediagnostic obstetric ultrasound in Peru: a new horizon in expanding access to prenatal ultrasound. BMC Pregnancy Childbirth. 2021;21(1):328. doi: 10.1186/s12884-021-03720-w.
- Corte G, Bayat S, Tascilar K, et al. Performance of a handheld ultrasound device to assess articular and periarticular pathologies in patients with inflammatory arthritis. Diagnostics (Basel). 2021;11(7):1139. doi: 10.3390/diagnostics11071139.
- Baribeau Y, Sharkey A, Chaudhary O, et al. Handheld. Point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth. 2020;34(11):3139–3145. doi: 10.1053/j.jvca.2020.07.004.
- Buhling KJ, Zite NB, Lotke P, et al. Worldwide use of intrauterine contraception: a review. Contraception. 2014;89(3):162–173. doi: 10.1016/j.contraception.2013.11.011.
- United Nations, Department of Economic and Social Affairs, Population Division. 2019). Contraceptive Use by Method 2019: data Booklet (ST/ESA/SER.A/435) https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_contraceptiveusebymethod_databooklet.pdf. (Accessed December 2023).
- de Kroon CD, van Houwelingen JC, Trimbos JB, et al. The value of transvaginal ultrasound to monitor the position of an intrauterine device after insertion. A Technology Assessment Study. Hum Reprod. 2003;18:2323–2327.
- Baker CC, Creinin MD. Long-Acting reversible contraception. Obstet Gynecol. 2022;140(5):883–897. doi: 10.1097/AOG.0000000000004967.
- Maged AM, Nada AM, Abdelwahab H, et al. The value of ultrasound guidance during IUD insertion in women with RVF uterus: a randomized controlled trial. J Gynecol Obstet Hum Reprod. 2021;50(4):101875. doi: 10.1016/j.jogoh.2020.101875.
- World Health Organization. Medical eligibility criteria for contraceptive use. Reproductive health and research., 5th edn. Geneva: world Health Organization; 2015. https://www.who.int/publications/i/item/9789241549158 (Accessed June 2023).
- Averbach SH, Ermias Y, Jeng G, et al. Expulsion of intrauterine devices after postpartum placement by timing of placement, delivery type, and intrauterine device type: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020;223(2):177–188. doi: 10.1016/j.ajog.2020.02.045.
- Laporte M, Marangoni M, Jr, Surita F, et al. Postplacental placement of intrauterine devices: a randomized clinical trial. Contraception. 2020;101(3):153–158. doi: 10.1016/j.contraception.2019.12.006.
- Marangoni M, Jr, Laporte M, Surita F, et al. One-year follow up on post-placental IUD insertion: a randomized clinical trial. Acta Obstet Gynecol Scand. 2021;100(4):596–603. doi: 10.1111/aogs.14081.
- Jatlaoui TC, Riley HEM, Curtis KM. The safety of intrauterine devices among young women: a systematic review. Contraception. 2017;95(1):17–39. doi: 10.1016/j.contraception.2016.10.006.
- Butterfly iQ. (product information). Butterfly Network, Inc., Burlington, MA USA, 2023
- R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing: vienna, Austria, 2014. http://www.R-project.org/ (Accessed February 2023).
- American College of Obstetricians and Gynecologists. Clinical challenges of long-acting reversible contraceptive methods. Committee opinion no. 672. Obstet Gynecol. 2016;128:e69-77.
- Golightly E, Gebbie AE. Low-lying or malpositioned intrauterine devices and systems. J Fam Plann Reprod Health Care. 2014;40(2):108–112. doi: 10.1136/jfprhc-2013-100684.
- Moschos E, Twickler DM. Does the type of intrauterine device affect conspicuity on 2D and 3D ultrasound? AJR Am J Roentgenol. 2011;196(6):1439–1443. doi: 10.2214/AJR.10.5483.
- Daniels K, Daugherty J, Jones J. Current contraceptive status among women aged 15-44: united States, 2011-2013. NCHS Data Brief. 2014;173(173):1–8.
- Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009-2012. Obstet Gynecol. 2015;126(5):917–927. doi: 10.1097/AOG.0000000000001094.
- American college of obstetricians and gynecologists. Long-Acting Reversible Contraception: implants and Intrauterine Devices. Practice Bulletin No. 186. Obstet Gynecol. 2017;130:e251-69.
- Recker F, Weber E, Strizek B, et al. Point-of-care ultrasound in obstetrics and gynecology. Arch Gynecol Obstet. 2021;303(4):871–876. doi: 10.1007/s00404-021-05972-5.