Abstract
Objective
To examine the prevalence of infections with high-risk human papillomavirus (HPV) and cervical dysplasia, and the clearance rate of HPV infections, in users of different kinds of intrauterine devices (IUDs) and other contraceptive methods.
Methods
A cross-sectional register-based study including 16,181 women aged 30–49 years participating in the screening programme for cervical cancer in a Swedish County in 2017–2018. Data on contraception from screening records was paired with the HPV test results, cytological and histological follow-up tests and subsequent HPV test.
Results
There was no difference in the risk of being HPV positive, or histological HSIL+, between users of copper-containing IUDs and women with no reported use of contraception. Use of levonorgestrel intrauterine system and hormonal contraception were associated with higher odds for HPV infection in age-adjusted models (aOR 1.21; 95% CI 1.04–1.41, and aOR 1.41; 95% CI 1.22–1.63, respectively) and for HSIL+ (aOR 1.45; 95% CI 1.02–2.06, and aOR 1.56; 95% CI 1.13–2.16, respectively). No significant differences were found in HPV clearance rates.
Conclusions
Reported use of levonorgestrel intrauterine system and hormonal contraception, but not use of copper IUD, was associated with a higher prevalence of HPV infections and histological HSIL + compared to no reported use of contraception.
Short condensation
Women using copper IUD showed no difference in prevalence of HPV or cervical dysplasia compared to women not using contraception in cross-sectional study
Introduction
High-risk human papillomavirus (HPV) infection is considered to be a prerequisite for the development of cervical cancer. It is a common infection among sexually active women and in most cases transient, but when persistent, it can cause dysplasia and cervical cancer [Citation1].
Intrauterine devices (IUDs) are common contraceptive methods for women globally, and both the copper-containing IUD (Cu-IUD) and the levonorgestrel intrauterine system (LNG-IUS), also referred to as hormonal IUD, are highly effective in preventing pregnancy [Citation2–4], but their side effects, positive as well as negative, differ.
A meta-analysis published in 2017 concluded that women who reported ever use of an IUD were less likely to develop cervical cancer (OR 0.64; 95% CI 0.53-0.77), but this meta-analysis was unable to examine the influence of IUD type [Citation5].
Data from a retrospective cohort study suggests that users of Cu-IUD have a lower relative risk of high-grade cervical dysplasia compared with users of LNG-IUS [Citation6]. A study of 302 women indicates that insertion of Cu-IUD results in a higher clearance rate of HPV than insertion of LNG-IUS [Citation7].
Thus, there are indications of a cervical cancer protective effect of IUD use. It has so far in retrospective studies been difficult to distinguish between Cu-IUD users and LNG-IUS users, but there are indications that the possible protective effect is mainly due to use of Cu-IUD. Further examination of the possible effect of LNG-IUS and Cu-IUD on the risk of acquiring an HPV infection and the possibility of clearing the infection or developing cervical dysplasia is required.
In the Region Örebro County, Sweden, the women participating in the screening programme for cervical cancer report the use of contraceptive methods at the time of the screening, with IUD use separated into Cu-IUD and LNG-IUS. These screening records provide a unique opportunity to analyse HPV status and cervical dysplasia in relation to the contraceptive method the women used at the time of screening.
The aim of this research was to separately study the prevalence of HPV and cervical dysplasia among users of Cu-IUD, LNG-IUS and other contraceptive methods, as well as to examine whether the HPV clearance rate is different in women using different types of IUDs.
Material and methods
Study setting
The screening programme for cervical cancer in Sweden invites all women between the ages of 23 and 70 years. Since September 2016 the Region Örebro County has used primary HPV screening with cytology as triage for women 30 years and above, and from 2020 for all women. Before 2020, women younger than 30 years were screened with cytology only.The screening interval has been 3 years for women up to the age of 50, and then 5 years up to the age of 70.
Women included in the primary HPV screening, with a positive HPV test and normal cytology, are invited for a follow-up HPV test in 18–36 months, depending on HPV type, and women with abnormal cytology are referred for colposcopy. Gynaecologists at the local hospitals perform the colposcopies according to national guidelines [Citation8], including cervical biopsy sampling or conisations when required.
Study population
All women aged 30–49 years who participated in the HPV screening programme 2017–2018 in Region Örebro County were included. Pregnant women were excluded. Information from the screening records was paired with the results from the HPV test. For the HPV-positive women, the results from the subsequent HPV test and the cytological and histological test results were obtained from the local laboratory information management system (Flexlab/Sympathy, Tieto, Sweden). The histopathological examinations included results from cervical biopsies taken at colposcopic examinations, conisations and hysterectomies. Results up to 31 December 2021 were included.
Screening records
At the time of the screening the women filled in a screening record with questions regarding hormonal contraception (including both combined hormonal contraception and progestin-only methods), LNG-IUS, Cu-IUD, current pregnancy, delivery within the previous year, menopausal status and menopausal treatment. The women ticked the boxes of those matters that applied. Midwives confirmed the reported information before performing the screening test.
In the analyses, the cohort was divided into the following groups based on the reported use of contraception at the time of the screening test: hormonal contraception, LNG-IUS, Cu-IUD or no reported contraception. The women who did not tick in any of the boxes for hormonal contraception or IUD were classified to the group ‘no reported contraception’. If the women ticked the boxes for both hormonal contraception and LNG-IUS, they were classified to the LNG-IUS cohort. The cohort of women using hormonal contraception is referred to in this article as women using any hormonal contraception excluding LNG-IUS.
The screening records were excluded from the statistical analysis when the record stated that the woman could not understand Swedish or when the records were not readable. When the boxes were ticked in a way that was not clear to the reader, the participants were excluded from analysis of those questions.
Test analysis
The HPV tests were analysed with the mRNA-based assay Aptima (Hologic, Marlborough, MA, USA) that detects 14 high-risk HPV strains (HPV16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68). The same method was used throughout the study period. The cytology was assessed by IAC-certified cytotechnicians and classified according to the international Bethesda classification system [Citation9]: normal cytology; atypical squamous cells of undetermined significance (ASCUS); atypical squamous cells, cannot exclude high-grade lesion (ASC-H); low-grade squamous intraepithelial lesion (LSIL); high-grade squamous intraepithelial lesion (HSIL); atypical glandular cells; unclear atypia or suspicious cancer.
Pathologists assessed the biopsy specimens according to WHO classification: normal, LSIL, HSIL, adenocarcinoma in situ (AIS) or cancer.
For the included women who had several biopsies or cytology tests taken during the follow-up, the most severe result of the histopathological examinations was noted in the protocol. In the statistical analysis, the test results were divided into normal/LSIL or histological HSIL+ (HSIL, AIS or cancer). For the HPV-positive women, the first follow-up HPV test that came back negative was noted, and for those with persistent HPV infection during the study period, the last positive HPV test was noted. The number of months between the initial test and the follow-up test was noted in the protocol, as well as the information from the follow-up test on contraceptive use, pregnancy, delivery within the previous year, menopausal status and hormonal replacement therapy.
Statistical analysis
The power calculation was based on the following:
Approximately 9000 women in the ages 30-49 years annually take part in the screening programme in Region Örebro County.
Approximately 10% of all women in this age group can be expected to be LNG-IUS users [Citation10].
The group of women using Cu-IUD can be expected to be of the same size, that is, 10% of all women.
In Region Örebro County 6.9% of all women taking part in the screening programme were HPV positive in 2017-2018.
The relative risk for cervical cancer among IUD users has been reported to be 0.64 (95% CI 0.53-0.77) [Citation5]. We make the assumption that the difference in risk of being HPV positive is of the same size.
Based on these assumptions, we hypothesise that the difference in HPV status will be equal to the difference in cervical cancer risk. Assuming 6.9% HPV positivity in the general population, and given a 35% reduced risk of cervical cancer among IUD users seen in the meta-analysis [Citation5], we presumed that 4.5% of Cu-IUD users would be HPV positive. We then needed to include at least 1360 women in each group to show this difference with a power of 80% at a significance level (alpha) of 0.05. Each year approximately 9000 women in the age group 30-49 years take part in the screening programme and 10%, 900 women, were then presumed to be Cu-IUD users. Consequently, we needed to include samples from 1.5 years to reach the adequate sample size. As there were several uncertainties in these estimations, we chose to include data from two years, that is, from 18,000 women.
IBM SPSS Statistics version 29 was used for statistical calculations. Logistic regression analyses were used to estimate odds ratios and confidence intervals. The participants with missing data on contraception were excluded from the statistical analysis.
Ethical approval
The study was approved by the Swedish Ethical Review Authority (Dnr 2021-01379).
Results
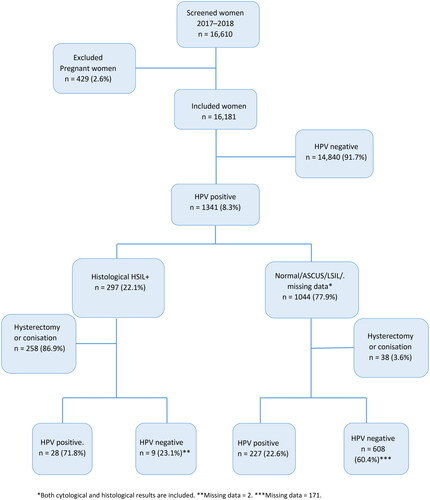
After pregnant women were excluded from the eligible participants, 16,181 women were included in the study. A total of 1341 women (8.3%) were HPV positive, and 297 (1.8%) had a histologically confirmed HSIL+ (). The mean age of all included women was 39.1 years. Of the total participants 373 (2.3%) women were menopausal, 88 women (0.5%) reported menopausal treatment and 1126 women (7%) reported delivery within the previous year before sampling.
Figure 1. Flowchart of participating women in the screening programme, included women and their results in the HPV screening tests, follow-up histological and cytological tests and follow-up HPV tests.
Women using hormonal contraception had higher age-adjusted odds of a positive HPV screening test compared to women not reporting any use of contraception (aOR 1.41; 95% CI 1.22-1.63) (). Use of LNG-IUS was also associated with significantly higher age-adjusted odds of a positive HPV screening test (aOR 1.21; 95% CI 1.04–1.41). For women using Cu-IUD, no significant difference was found compared with women with no reported use of contraception (aOR 1.01; 95% CI 0.81–1.27) (). Neither was there any difference in HPV status between users of Cu-IUD and users of LNG-IUS (aOR 1.19; 95% CI 0.93-1.53) (). Women using hormonal contraception had higher age-adjusted odds of a positive HPV screening test compared to women using Cu-IUD (aOR 1.39; 95% CI 1.09-1.78) (). Menopausal status, menopausal treatment and delivery within a year were not found to be significant confounding factors.
Table 1. Odds of having an HPV infection in the screening tests in relation to reported contraceptive method.
Of the HPV-positive women, 297 (22.1%) had HSIL + in the histological sampling at the clinical examinations (). When adjusting for age, the odds of HSIL + were significantly higher among women using hormonal contraception (aOR 1.56; 95% CI 1.13–2.16) or LNG-IUS (aOR 1.45; 95% CI 1.02–2.06) compared with women who did not report use of contraception. Women using Cu-IUD had no increased odds of HSIL + compared to women with no reported use of contraception (). Neither was there any difference in the odds of HSIL + between users of Cu-IUD and LNG-IUS ().
Table 2. Odds of histologically confirmed HSIL + among HPV-positive cases in relation to reported contraceptive method.
Conisation was performed on 270 (20.1%) of the 1341 HPV-positive women, and 26 (1.9%) underwent a hysterectomy. Out of the 1045 HPV-positive women who did not go through any of these procedures, 617 (59%) had a negative HPV test within the follow-up time (mean follow-up time 28 months/median 35 months). A persistent HPV infection was found in 255 women (24.4%), and 173 (16.6%) had no follow-up test done in the Region Örebro County within the follow-up period of three years. There were no statistically significant differences in HPV clearance between women using different types of contraception ().
Table 3. Odds of HPV clearance in HPV-positive women without treatment in relation to reported contraceptive method.
Discussion
Findings and interpretation
The women included in this cross-sectional study who reported using hormonal contraception or LNG-IUS had a higher prevalence of HPV infections and histological HSIL + compared with women who did not report use of any contraception. The prevalence of HPV and HSIL + in women who reported use of Cu-IUD did not differ from women who did not report use of any contraception. The findings regarding the increased risk in users of hormonal contraception is in accordance with well-known results from previous studies [Citation11–14].
Results in the context of what is known
Because the meta-analysis by Cortessis et al. found lower risk of cervical cancer for women with intrauterine devices, one could expect a lower prevalence of HPV infections, especially for Cu-IUD, since that was the most-used type of IUD during the time of the data collection in the studies included in the meta-analysis [Citation5]. The findings from the present study suggests that women with Cu-IUD have the same prevalence of HPV infections and HSIL + as women who report no use of contraception but a lower risk than women using hormonal contraception. Women using LNG-IUS showed a higher prevalence of both HPV infections and HSIL+. Castellsagué et al. found no difference in HPV prevalence between users of intrauterine devices and non-users in the meta-analysis, but had no data on type of IUD [Citation15]. In these meta-analyses on the risk of cervical cancer and HPV infections, users of IUDs were compared to non-users with no specified information on contraceptive use in the non-user group [Citation5,Citation15]. When merging results from women who do not use contraception with women using hormonal contraception as a control group, the results can be difficult to interpret. In the present study, women with no reported contraception were primarily chosen for comparison to reduce the impact of hormonal contraception as a confounding factor. On the other hand, using ‘no reported contraception’ with the present definition also implies a serious risk of confounding, as this group also may include users of condoms. We were not able to register condom use, but approximately 15% of women in Sweden have been estimated to rely on condoms as a contraceptive method [Citation16], and consequently, the group of ‘true non-users’ is smaller and may have a different, higher risk.
No significant difference was found in the clearance rate of HPV infections when comparing women using different contraceptives. According to the Swedish national guidelines, women with HSIL + in the age of 30–49 years should be treated with cervical conisation. Therefore, those who underwent treatment were excluded from the analysis regarding clearance, since we wanted to examine the natural course of HPV clearance in women with different types of contraception. The women who were included in the analysis of clearance rate were, as a consequence of the treatment strategy, mostly women with no or low-grade cervical dysplasia; the numbers were small and therefore difficult to draw conclusions from. The persistence of HPV infections is one of the most significant predictors for the risk of recurrence of cervical dysplasia [Citation17], but the number of women with HSIL in this study was too few to analyse HPV persistence in relation to contraceptive use.
Strengths and limitations
The major strength of this study is the collecting of reliable information regarding contraceptive use at the time of screening, which made it possible to distinguish between women using LNG-IUS and women using Cu-IUD. This differentiation between IUD types was not possible to undertake in the meta-analyses on risk of cervical cancer in users of IUDs [Citation5,Citation15]. Even though the present study is not a study on cervical cancer risk, the information regarding the risk of persistent HPV infections is of importance, as this is a prerequisite for the development of cervical cancer.
In this study, the information on contraception is self-reported by the participating women and not collected data from procedure, prescription or data on dispensation from the Swedish Prescribed Drug Register. Moreover, as the alternatives regarding statements of contraceptive use were prespecified in the screening records, we were not able to separate hormonal contraceptive use in users of combined hormonal contraceptives or users of progestin-only methods. Register data can supply information on dispensed hormonal contraception and dispensed LNG-IUS in a huge number of women but do not supply any information on actual use. Moreover, there is no way to find information on actual use of Cu-IUDs, as these are not considered as pharmacological agents, and consequently, are not included in national registers. The information in the screening record is read and confirmed by the midwives who perform the screening tests, and they have great knowledge about contraception; we thereby consider the information on contraceptive use reliable.
The main limitation of the study is the limited available information. Demographic variables, besides age, are not available. There are several factors that might influence the risk of acquiring HPV infections and cervical dysplasia where we lack information. These factors include condom use, number of sexual partners, smoking and previous use of contraception as well as duration of the current IUD use [Citation18,Citation19]. Women who are not sexually active and women who use the condom as a contraception method are included in the group of women who did not report use of contraception. These women have a very low risk of acquiring HPV infections, and we cannot exclude that this may have biased our results.
LNG-IUS has indications other than contraception, for example, heavy menstrual bleeding, dysmenorrhoea or endometrial protection with hormone replacement treatment. This might explain why LNG-IUS was associated with a higher prevalence of HPV infections and HSIL + only after adjustments for age, since older women have a lower prevalence of HPV infections [Citation20]. Cu-IUDs, on the other hand, have no indication other than contraception, and one can therefore assume that women who use a Cu-IUD are sexually active. Still there is no information on number of sexual partners and whether that is different between women using hormonal contraception, LNG-IUS or Cu-IUD in this study.
Data on vaccination is not available in the current screening records. HPV vaccination has been offered to girls aged 10–12 years in Sweden from the year 2010. The age cohort in this study has thus not been offered HPV vaccination in the regular vaccination programme, but opportunistic vaccination and vaccination in research projects could have occurred.
Clinical implications
Cervical cancer is the fourth most common cause of cancer death in women worldwide, and in some countries it is the leading cause of cancer death in women [Citation21]. HPV vaccination has been introduced in many national immunisation schedules, mostly in high-income countries, but the vaccination rate is still low in older women and in low- and middle-income countries [Citation22]. Therefore, the need to understand the risk factors is still great.
Research implications
Use of combined oral contraceptives is known to be a risk factor for cervical cancer [Citation23], but less is known about different types of IUDs and their effect on the risk of cervical cancer. The results from this study suggest that women with Cu-IUD do not have a prevalence of HPV infections different from that of women with no contraception, and future studies are needed to evaluate whether the copper component in the intrauterine devices affects the cervical tissue. Does the copper affect the HPV infection persistence or other stages in the cervical dysplastic process?
Conclusion
Women who report use of hormonal contraception and LNG-IUS have a higher prevalence of HPV infections and HSIL + than women who report no use of contraception in the screening programme for cervical cancer. The prevalence of HPV and HSIL + among women who use Cu-IUD does not differ from women who report no use of contraception.
Contribution to authorship
LJ collected and analysed data and wrote the manuscript. EC and LT have collected and analysed data and revised the article. JB designed the study and contributed to data analysis and to the writing of the manuscript. LB designed the study and contributed to data analysis and to the writing of the manuscript.
Supplemental Material
Download MS Word (14.4 KB)Disclosure statement
JB has received honorariums for giving lectures in hormonal contraception for Organon, Campuspharma, Exceltis and Gedeon Richter. LJ, EC, LT and LB have no interests to disclose.
Data availability statement
The data that support the findings of this study are available from the corresponding author, LJ, upon reasonable request.
Additional information
Funding
References
- Walboomers JMM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F.
- Mansour D, Inki P, Gemzell-Danielsson K. Efficacy of contraceptive methods: a review of the literature. Eur J Contracept Reprod Health Care. 2010;15 (sup2):S19–S31. doi: 10.3109/13625187.2010.532999.
- Buhling KJ, Zite NB, Lotke P, et al. Worldwide use of intrauterine contraception: a review. Contraception. 2014;89(3):162–173. doi: 10.1016/j.contraception.2013.11.011.
- United Nations DoEaSA, Population Division. Contraceptive Use by Method 2019: data Booklet (ST/ESA/SER.A/435); 2019.
- Cortessis VK, Barrett M, Brown Wade N, et al. Intrauterine device use and cervical cancer risk: a systematic review and meta-analysis. Obstet Gynecol. 2017;130(6):1226–1236. doi: 10.1097/AOG.0000000000002307.
- Spotnitz ME, Natarajan K, Ryan PB, et al. Relative risk of cervical neoplasms among copper and levonorgestrel-releasing intrauterine system users. Obstet Gynecol. 2020;135(2):319–327. doi: 10.1097/AOG.0000000000003656.
- Lekovich JP, Amrane S, Pangasa M, et al. Comparison of human papillomavirus infection and cervical cytology in women using copper-containing and levonorgestrel-containing intrauterine devices. Obstet Gynecol. 2015;125(5):1101–1105. doi: 10.1097/AOG.0000000000000760.
- Cancercentrum. Nationellt vårdprogram livmoderhalscancerprevention: Regionala cancercentrum. i samverkan; 2022 [updated 2022-11-15; cited 2023 2023-06-14]; Version 4.0:[Available from: https://kunskapsbanken.cancercentrum.se/diagnoser/livmoderhalscancerprevention/vardprogram/.
- Pangarkar MA. The bethesda system for reporting cervical cytology. Cytojournal. 2022;19:28. doi: 10.25259/CMAS_03_07_2021.
- Lindh I, Skjeldestad FE, Gemzell-Danielsson K, et al. Contraceptive use in the nordic countries. Acta Obstet Gynecol Scand. 2017;96(1):19–28. doi: 10.1111/aogs.13055.
- Winer RL, Lee SK, Hughes JP, et al. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am J Epidemiol. 2003;157(3):218–226. doi: 10.1093/aje/kwf180.
- Nielsen A, Iftner T, Munk C, et al. Acquisition of high-risk human papillomavirus infection in a population-based cohort of Danish women. Sex Transm Dis. 2009;36(10):609–615. doi: 10.1097/OLQ.0b013e3181a96d0e.
- Shew ML, Ermel AC, Tong Y, et al. Episodic detection of human papillomavirus within a longitudinal cohort of young women. J Med Virol. 2015;87(12):2122–2129. doi: 10.1002/jmv.24284.
- Skorstengaard M, Lynge E, Napolitano G, et al. Risk of precancerous cervical lesions in women using a hormone-containing intrauterine device and other contraceptives: a register-based cohort study from Denmark. Hum Reprod. 2021;36(7):1796–1807. doi: 10.1093/humrep/deab066.
- Castellsagué X, Díaz M, Vaccarella S, et al. Intrauterine device use, cervical infection with human papillomavirus, and risk of cervical cancer: a pooled analysis of 26 epidemiological studies. Lancet Oncol. 2011;12(11):1023–1031. doi: 10.1016/S1470-2045(11)70223-6.
- Wulff M, Lalos A. The condom in relation to prevention of sexually transmitted infections and as a contraceptive method in Sweden. Eur J Contracept Reprod Health Care. 20049(2):69–77. doi: 10.1080/13625180410001715636.
- Bogani G, Sopracordevole F, Ciavattini A, et al. Duration of human papillomavirus persistence and its relationship with recurrent cervical dysplasia. Eur J Cancer Prev. 2023;32(6):525–532. doi: 10.1097/CEJ.0000000000000822.
- Lam JU, Rebolj M, Dugué PA, et al. Condom use in prevention of human papillomavirus infections and cervical neoplasia: systematic review of longitudinal studies. J Med Screen. 2014;21(1):38–50. doi: 10.1177/0969141314522454.
- Jensen JT, Lukkari-Lax E, Schulze A, et al. Contraceptive efficacy and safety of the 52-mg levonorgestrel intrauterine system for up to 8 years: findings from the mirena extension trial. Am J Obstet Gynecol. 2022;227(6):873.e1–873.e12. doi: 10.1016/j.ajog.2022.09.007.
- Monsonego J, Cox JT, Behrens C, et al. Prevalence of high-risk human papilloma virus genotypes and associated risk of cervical precancerous lesions in a large U.S. screening population: data from the ATHENA trial. Gynecol Oncol. 2015;137(1):47–54. doi: 10.1016/j.ygyno.2015.01.551.
- WHO International Agency for Research on Cancer. Estimated number of new cases in 2020, worldwide, females, all ages. 2020. Access date 2021-05-17.
- Bruni L, Saura-Lázaro A, Montoliu A, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev Med. 2021;144:106399. doi: 10.1016/j.ypmed.2020.106399.
- Iversen L, Sivasubramaniam S, Lee AJ, et al. Lifetime cancer risk and combined oral contraceptives: the royal college of general practitioners’ oral contraception study. Am J Obstet Gynecol. 2017;216(6):580.e1-580–e9. doi: 10.1016/j.ajog.2017.02.002.

