 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Introduction
Patient-specific rehearsal (PsR) is a recent technology within virtual reality (VR) simulation that lets the operators train on patient-specific data in a simulated environment prior to the procedure. Endovascular aneurysm repair (EVAR) is a complex procedure where operative metrics and technical success might improve after PsR.
Material and methods
We compared technical success and operative metrics (endovascular procedure time, contralateral gate cannulation time, fluoroscopy time, total radiation dose, number of angiograms and contrast medium use) between 30 patients, where the operators performed PsR (the PsR group), and 30 patients without PsR (the control group).
Results
The endovascular procedure time was significantly shorter in the PsR group than in the control group (median 44 versus 55 min, p = .017). The other operative metrics were similar. Technical success rates were higher in the PsR group, 96.7% primary and assisted primary outcome versus 90.0% in the control group. The differences were not significant (p = .076).
Conclusions
PsR before EVAR reduced endovascular procedure time, and our results indicate that it might improve technical success, but further studies are needed to confirm those results.
Introduction
Endovascular aneurysm repair (EVAR) is a common treatment for infrarenal aortic aneurysms [Citation1,Citation2]. EVAR represents a complex procedure where the outcome depends on multiple factors, among those the expertise and preparation of the operators performing the procedure [Citation3–8]. A successful EVAR is the result of successful pre-operative planning, technical components, good team workflow, operators’ technical skills, efficient logistics and error prevention [Citation9]. Recent advancements in simulation technology, such as patient-specific rehearsal (PsR) on virtual reality (VR) simulators, open up new possibilities for pre-operative planning and operators’ preparation [Citation10–12]. PsR lets the operators rehearse the procedure on the simulator with patient-specific image data [Citation10,Citation11], and may enhance individual preparedness and team workflow, and ultimately improve operative metrics and outcomes.
With increased focus on patient safety, PsR raises questions related to expectations towards operator preparedness before performing complex procedures [Citation13]. Although common in other high-stake industries or within sports and music performances, practical rehearsal is rare within the surgical and interventional radiology domain [Citation11]. Before PsR, vascular surgeons and interventional radiologists (IR) had limited tools to do practical rehearsal on patient-specific cases, and were in performance mode most of their time [Citation11]. Vascular surgeons and IRs often do a mental rehearsal prior to complex procedures, where the operators either separately or together, go through the CT images, visualize potential challenges, and plan how to overcome them during the actual procedure. PsR on a VR simulator, compared to a mental rehearsal, offers a more complete experience, adding haptic sensations and practical aspects like instrument handling and stent graft deployment.
PsR can also be used to improve the performance of inexperienced operators in an educational perspective. Being a risk-free environment, training on simulators has been proven useful both for acquiring basic and procedural endovascular skills [Citation14–18]. Compared to traditional VR-simulated training, PsR adds relevance to the training and a stronger sensation of high stakes. It is believed that training that is perceived as more relevant, more high-stake, is better retained [Citation19].
We investigated how PsR on a VR simulator influenced operative metrics and outcome by comparing EVAR procedures without PsR (the control group) with a group with PsR prior to the procedure (the PsR group). Patient-specific EVAR rehearsal on the Angio MentorTM (3D Systems Healthcare, Littleton, CO) has been found to aid in the pre-operative planning of component selection and of optimal C-arm angulations, and to reduce errors during EVAR [Citation5,Citation12,Citation20,Citation21]. To our knowledge, this is the first study that investigates PsR on the VIST-LAB simulator (Mentice AB, Gothenburg, Sweden), and the second that investigates actual improvements on operative metrics and outcome in the operating room after PsR [Citation12,Citation21].
Material and methods
Patients undergoing an elective EVAR procedure were allocated to a PsR group or a control group based on availability of operators and simulator. In the PsR group (30 patients), the operators (one vascular surgeon and one IR) performed the PsR 1 day before or the same day as they performed the EVAR. In the control group (30 patients), no prior PsR was performed. The following operative metrics were collected: endovascular procedure time (measured from first angiogram till the last one), contralateral gate cannulation time, fluoroscopy time, total radiation dose ( number of angiograms and contrast medium use (ml), and were compared between the two groups. Operative outcome was evaluated based on procedure-related responses and final angiograms using technical success from Chaikof et al.’s reporting standards for EVAR [Citation22] (), and were judged by two experienced IRs blinded to group status. The study was approved by the Norwegian data inspectorate.
Table 1. Definition of technical success for the intention of this study, based on Chaikof et al.’s [Citation22] reporting standards for EVAR.
Preparation of patient-specific data
A dedicated radiographer used the TeraRecon medical image visualization software (Aquarius Intuition, Version 4.4.12, Foster City, CA) to segment patient-specific CT images of the abdominal aorta, from the renal arteries to the iliac bifurcation, and to export them to STereoLithography (STL) files [Citation23], before importing them into the simulator.
The PsR and the EVAR procedure
The VIST-LAB simulator with VIST-CTM and Bolton Treo® deployment system using the Bolton Case-it EVAR module was used (version 8.3). Haptic feedback was simulated by two haptic feedback devices allowing access from both sides. A table-side user interface allowed for control of table movements and C-arm positioning.
The radiographer who created the STL file was present during the PsR, and occasionally joined the EVAR. The EVAR was performed in a hybrid suite. The PsRs were freely organized and the operators were free to discuss and to redo steps if they wanted. The operators were encouraged to perform the tasks during the PsR as they planned to do them during the real procedure, i.e. the same operator would cannulate the contralateral limb during the PsR and the real case. The patient-specific EVAR rehearsal started after endovascular access and ended with the deployment and verification of the Bolton stent graft system (main body, contra- and ipsilateral legs).
Statistical analysis
Statistical differences in the distribution’s central tendencies (p < .05) between the operative metrics and technical success rates for the PsR group and the control group were investigated using the Mann–Whitney U test using SPSS 25 (IBM Corporation, Armonk, NY). Patient characteristics were tested using Shapiro–Wilk test for normality and appropriate tests for differences in distributions using t-test for equality of means, Mann–Whitney U-test and Fischer’s exact test.
Results
Patient data were similar in both groups () as well as stent grafts used. In the control group, nine stent grafts from Cook Zenith and 21 from Medtronic Endurant II were used, and in the PsR group one Bolton Treo, 8 Cook Zenith and 21 Medtronic Endurant II. Nine vascular surgeons and seven IRs performed the PsRs and the following procedures, where level of operator experience was equally distributed between both groups. Five vascular surgeons had less than 2 years’ experience, the others above 2 years. There was at least one experienced operator present at each procedure.
Table 2. Patient data and operator’s level of experience for all patients.
Operative metrics and outcome were compared between the PsR group (n = 30) and the control group (n = 30). The operative metrics are presented in . illustrates endovascular procedure time measured from first angiogram till the last one. shows contralateral gate cannulation time, where the time was measured from the moment the operator started manipulating the contralateral catheter in the distal part of the aorta with the intention to cannulate the contralateral limb, and was ended when the operator rotated the catheter at the proximal end of the stent graft thereby verifying that the catheter was within the proximal end of the stent graft; shows total fluoroscopy time, the number of angiograms, the total radiation dose/dose area product and illustrates contrast medium use. The endovascular procedure time in the PsR group was significantly shorter, median 44 min versus 55 min for the control group (p = .017) (). The operative metrics: contralateral gate cannulation time, total fluoroscopy time, number of angiograms, total radiation dose and contrast medium use, were similar in both groups and did not show any significant difference (). Operative outcome measured as technical success rates were improved in the PsR group, with 28 primary successes, 1 assisted primary success and 1 technical failure versus 23 primary successes, 4 assisted primary successes and 3 technical failures in the control group (p = .076) (). In both groups none converted, zero 24 h mortality. shows final angiograms of the simulation and the real procedure for two patients: one that ended with primary success and the one that ended with assisted primary success.
Figure 1. Boxplots presenting operative metrics for both groups (median (range)). (a) endovascular procedure time (minutes) measured from first angiogram till the last one, p = .017, (b) contralateral gate cannulation time (minutes), p = .785. The time was measured from the moment the operator started manipulating the contralateral catheter in the distal part of the aorta with the intention to cannulate the contralateral limb, and was ended when the operator rotated the catheter at the proximal end of the stent graft thereby verifying that the catheter was within the proximal end of the stent graft, (c) total fluoroscopy time (minutes), p = .255, (d) number of angiograms, p = .392, (e) total radiation dose/dose area product ( p = .605, (f) contrast medium use (ml), p = .328. The middle band shows the median value, the bottom and the top of the boxes show the 25th and the 75th percentiles, and the ends of the whiskers show the 5th and the 95th percentiles. Outliers are plotted as circles and extreme outliers as stars.
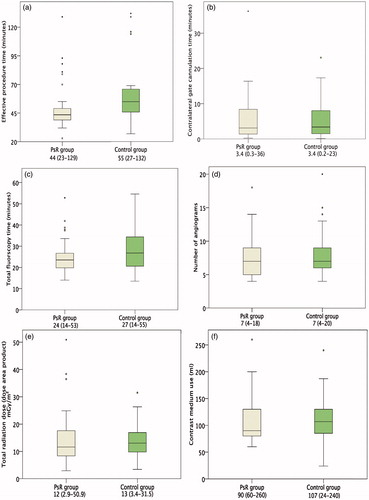
Figure 2. Final angiograms of the PsR and the real procedure (RP) for two patients: one that ended with primary technical success (patient I) and the one that ended with assisted primary technical success (patient II).
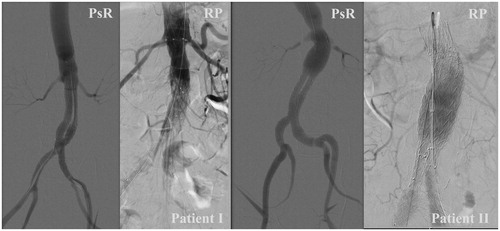
Table 3. Primary and assisted primary technical success, and technical failure rates.
Discussion
PsR using VR simulators is a new tool to train and prepare before treating patients, potentially improving operator preparedness and operative metrics and outcomes. Through comparison of operative metrics and technical success from the two groups of 30 patients, with and without PsR, we found that endovascular procedure time was significantly shorter in the PsR group, and that technical success was improved in the PsR group, but without significant difference. The other operative metrics were similar in both groups.
Regarding radiation dose, in both groups, during the pre-planning, the operators used dedicated visualization software to evaluate patient anatomy and to define optimal C-arm angles to minimize it. Furthermore, the radiation dose largely depends on patient weight (body mass index), which was equally distributed in both groups. All operators would strive to keep the radiation dose and the number of angiograms low, and use clues from the patient anatomy, found when using the visualization software. They would, for example preposition the neck of the stent graft using the relative position of the renal ostium to the patient’s vertebral outlining, visible during plain fluoroscopy, before taking the first angiogram. Further, the amount of contrast used correlates with the number of angiograms. It seems that the PsR did not give added value compared to the traditional planning, concerning radiation dose, number of angiograms, and amount of contrast used. One might argue that the flow between the steps went smoother in the PsR group, reducing the procedure time, but that all steps had to be done in both groups, resulting in similar amount of contrast used, number of angiograms and radiation dose.
PsR is still a recent technology, and to our knowledge, Desender et al. is the only group that have, in addition to this study, investigated actual improvements on operative metrics and outcomes in the operating room after PsR on EVAR [Citation12,Citation21]. Desender et al. investigated technical and nontechnical operative performance [Citation21], and impact on procedural planning and team performance [Citation12] after PsR on a different simulator. They registered errors manually during the EVAR procedures after prior PsR (the PsR group) or no PsR (the control group), and showed a reduction in both minor and major errors in the PsR group [Citation21]. In addition, they found significantly fewer angiograms before deployment of the main body in the PsR group, and no significant difference between endovascular time, fluoroscopy time, contrast medium use, radiation dose, and the total number of angiograms [Citation21]. No significant differences between fluoroscopy time, contrast medium use, radiation dose, and total number of angiograms are in accordance with our findings. However, we did find a significant difference in endovascular procedure time. We measured endovascular procedure time slightly different than Desender et al. [Citation21], but we believe that did not influence the results. Also, in accordance with our findings, Desender et al. did not find significant differences in technical success between the PsR and the control group [Citation12]. In the same study, they found that the interventionalist changed the diameter or length of the main body, the contralateral limb or the iliac extension of the stent graft in 16, 34 or 28% of the cases, respectively [Citation12]. The simulator from Mentice, which we used in our study, however, did not offer the possibility of stent graft measurements, and the length of the different stent graft components was not part of the evaluation. Nevertheless, in one patient, where the contralateral limb occluded the iliac internal artery during the PsR, it was found that the ordered limb was too long. A shorter limb was chosen for the real procedure, which ended with primary technical success. The PsR served as an additional quality check of the planned components.
Today the operators prepare themselves using dedicated visualization software [Citation9] and a mental rehearsal envisaging potential difficulties and how to overcome them. New technologies that might increase operator preparedness is PsR and 3D printing [Citation24,Citation25]. Rigorous use of a visualization software for accurate planning has been found to positively influence EVAR-related outcomes [Citation26]. The PsR compared to the use of a visualization software is a more complete experience with practical training where the operators can train together. Whether PsR improves operator preparedness, and eventually EVAR-related outcomes, might be influenced by the experience of the operators and/or limitations in realism of the PsR. For example, the operators specifically trained on the contralateral gate cannulation, but we did not find any effect of this training in our results, as both groups had similar results on contralateral gate cannulation time. A large proportion of the operators in our study were experienced, which might have influenced the result.
Limitations on physical resemblance are another aspect that might limit the benefit of the PsR. The users pointed out inadequate modelling of biomechanical properties, such as effects of rigidity (calcification), stenosis (atherosclerosis), or the straightening effect of stiff guide wires and introducers on tortuous arteries. These are aspects that led to less realistic simulation of subsequent cannulation, and that might have influenced the results. The remarks on the simulators’ physical resemblance (realism) are in accordance with other simulators offering PsR [Citation5,Citation21]. The Bolton case-it module on the simulator was set up with modified Bolton Treo® deployment devices. The physical exploration of the patient’s anatomy was judged more important than the actual deployment system, but the use of other stent grafts than Bolton Treo® might have influenced the results.
Due to practical aspects, the patients were not actively randomized into either group but were allocated to the simulator group when operators and the simulator were available, creating a potential bias. Potential confounding factors such as patient characteristics and operators’ levels of experience were therefore carefully investigated after the study and were found to be equally distributed between the groups (). Level of experience is usually measured in terms of years of experience or number of (EVAR) procedures. Differences in actual skills do occur between operators with the same years of experience and this was not accounted for. The PsR did not alter the treatment negatively and was performed for patients with varying aortic aneurysm characteristics and the different stent grafts used in this study. Technical and non-technical skills between the vascular surgeon and the IR were rehearsed during the PsR, but not the interaction with the rest of the team. Including the rest of the team might have given different results but would also have added additional costs. Exact power calculations were not possible, as no similar studies were published at the design of the study. Thirty patients in each group were estimated as enough, based on comparable studies. Improved endovascular procedure time for the PsR group was found significantly different; however, a limited number of patients might explain the lack of statistical significance for the other operative metrics and technical success.
As with the introduction of all technology, there are several aspects that need to be accounted for before implementing it into clinical practice, such as time, expertise and cost needed to prepare and perform the PsR, in addition to initial cost of the simulator and the PsR module. Initial cost of the simulator can be distributed, as the simulator can be used to train several endovascular procedures across a range of operator experiences. Regarding the time and expertise needed to prepare the PsR, a considerable learning phase was needed, and a dedicated radiographer would spend between 30 and 180 min to prepare them. The endovascular procedure time was significantly shorter in the PsR group, median 44 versus 55. In a socioeconomic perspective, the time saved in the OR need to be weighed against the time spent on the PsR, in addition to the cost of the VR simulator and the case-it module.
In summary, PsR is a recent technology in EVAR simulation that opens up new possibilities for the operators to prepare themselves before complex procedures. A technology that can be beneficial to operators with different levels of experience. We found that PsR shortened the endovascular procedure time. Improving limited simulator realism on biomechanical properties might improve other operative metrics and outcomes.
Acknowledgements
The authors thank the surgeons and the interventional radiologists, in addition to the operating teams for participating in the study.
Declaration of interest
None of the authors state any conflict of interest or financial ties to disclose.
Additional information
Funding
References
- Behrendt C-A, Sedrakyan A, Rieß HC, et al. Short-term and long-term results of endovascular and open repair of abdominal aortic aneurysms in Germany. J Vasc Surg. 2017;66(6):1704–1717.
- Beck AW, Sedrakyan A, Mao J, et al. Variations in abdominal aortic aneurysm care: a report from the international consortium of vascular registries. Circulation. 2016;134(24):1948–1958.
- Maurel B, Hertault A, Sobocinski J, et al. Techniques to reduce radiation and contrast volume during EVAR. J Thorac Cardiovasc Surg. 2014;55(2 Suppl 1):123–131.
- Holt PJ, Poloniecki JD, Khalid U, et al. Effect of endovascular aneurysm repair on the volume-outcome relationship in aneurysm repair. Circ Cardiovasc Qual Outcomes. 2009;2(6):624–632.
- Davis GR, Illig KA, Yang G, et al. An approach to EVAR simulation using patient specific modeling. Ann Vasc Surg. 2014;28(7):1769–1774.
- Moll FL, Powell JT, Fraedrich G, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European society for vascular surgery. Eur J Vasc Endovasc Surg. 2011;41:S1–S58.
- Nayahangan LJ, Konge L, Schroeder TV, et al. A national needs assessment to identify technical procedures in vascular surgery for simulation based training. Eur J Vasc Endovasc Surg. 2017;53(4):591–599.
- Doyen B, Bicknell CD, Riga CV, et al. Evidence based training strategies to improve clinical practice in endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2018;56(5):751–758.
- Rolls AE, Riga CV, Rudarakanchana N, et al. Planning for EVAR: the role of modern software. J Cardiovasc Surg (Torino). 2014;55(1):1–7.
- Willaert WI, Aggarwal R, Van Herzeele I, et al. Recent advancements in medical simulation: patient-specific virtual reality simulation. World J Surg. 2012;36(7):1703–1712.
- Willaert WI, Aggarwal R, Nestel DF, European Virtual Reality Endovascular Research Team, EVEResT, et al. Patient-specific simulation for endovascular procedures: qualitative evaluation of the development process. Int J Med Robot. 2010;6(2):202–210.
- Desender L, Van Herzeele I, Lachat M, et al. A multicentre trial of patient specific rehearsal prior to EVAR: impact on procedural planning and team performance. Eur J Vasc Endovasc Surg. 2017;53(3):354–361.
- Willaert WI, Aggarwal R, Van Herzeele I, et al. Patient-specific endovascular simulation influences interventionalists performing carotid artery stenting procedures. Eur J Vasc Endovasc Surg. 2011;41(4):492–500.
- Våpenstad C, Buzink SN. Procedural virtual reality simulation in minimally invasive surgery. Surg Endosc. 2013;27(2):364–377.
- See KW, Chui KH, Chan WH, et al. Evidence for endovascular simulation training: a systematic review. Eur J Vasc Endovasc Surg. 2016;51(3):441–451.
- Nesbitt CI, Birdi N, Mafeld S, et al. The role of simulation in the development of endovascular surgical skills. Perspect Med Educ. 2016;5(1):8–14.
- Saratzis A, Calderbank T, Sidloff D, et al. Role of simulation in endovascular aneurysm repair (EVAR) training: a preliminary study. Eur J Vasc Endovasc Surg. 2017;53(2):193–198.
- Vento V, Cercenelli L, Mascoli C, et al. The role of simulation in boosting the learning curve in EVAR procedures. J Surg Educ. 2018;75(2):534–540.
- Prentice R. Bodies in formation: an ethnography of anatomy and surgery education. Durham, US: Duke University Press. 2012.
- Desender L, Rancic Z, Aggarwal R, et al. Patient-specific rehearsal prior to EVAR: a pilot study. Eur J Vasc Endovasc Surg. 2013;45(6):639–647.
- Desender LM, Van Herzeele I, Lachat ML, et al. Patient-specific rehearsal before EVAR: influence on technical and nontechnical operative performance. A randomized controlled trial. Ann Surg. 2016;264(5):703–709.
- Chaikof EL, Blankensteijn JD, Harris PL, et al. Reporting standards for endovascular aortic aneurysm repair. J Vasc Surg. 2002;35(5):1048–1060.
- Webb PA. A review of rapid prototyping (RP) techniques in the medical and biomedical sector. J Med Eng Technol. 2000;24(4):149–153.
- Mitsouras D, Liacouras P, Imanzadeh A, et al. Medical 3D printing for the radiologist. Radiographics. 2015;35(7):1965–1988.
- Tam MD, Latham TR, Lewis M, et al. A pilot study assessing the impact of 3-D printed models of aortic aneurysms on management decisions in EVAR planning. Vasc Endovasc Surg. 2016;50(1):4–9.
- Sobocinski J, Chenorhokian H, Maurel B, et al. The benefits of EVAR planning using a 3D workstation. Eur J Vasc Endovasc Surg. 2013;46(4):418–423.
