Abstract
Objective: To investigate the relationship between the compliance of bladder cancer patients with cystoscopic follow-up and the treatment protocol, and their health literacy.
Methods: Patients who underwent transurethral resection surgery for bladder tumor were found to have non-muscular invasive bladder carcinoma on pathology examination and then underwent cystoscopic follow-up for 1 year or more were included in the study. Cystoscopic follow-up was recommended to the low- and high-risk groups in terms of progression and recurrence. The patients were evaluated with the Health Literacy Survey-European Union scale.
Results: The mean age of the patients was 67.13 ± 10.77 years. The treatment continuity rate was 80.50% (n = 33) in the adequate health literacy group (n = 41) and significantly higher than the 56.50% (n = 48) rate in the inadequate health literacy group (n = 85) (p = .008). The health literacy results revealed that the health promotion and general index score was higher in the group of patients under the age of 65.
Conclusions: Adequate health literacy in bladder cancer patients is associated with better compliance with the treatment protocol. Young patients show better compliance with the follow-up protocol recommended by the physician. Increasing the follow-up protocol compliance of elderly patients with inadequate health literacy is necessary.
Introduction
Bladder cancer (BC) is a very common genitourinary cancer and is the ninth most common cancer in both genders worldwide [Citation1]. More than 60% of the bladder cancers cases and half of the 165,000 deaths from bladder cancer are seen in developing countries [Citation1]. Bladder cancer is the fourth leading cause of mortality in men and the thirteenth in women among cancers in our country.
The 2009 TNM classification is currently used for the staging and classification of bladder cancers as reported in the guideline prepared by the European Association for Urology (EAU) in 2017 for non-muscular invasive bladder carcinoma (NMIBC). If BC is limited to the mucosa and submucosa, it is classified as NMIBC. Newly diagnosed bladder cancers are limited to the mucosa (stage Ta and CIS) or submucosa (stage T1) in 75–85% of the cases [Citation2,Citation3]. The treatment of NMIBC is transurethral resection of the bladder (TUR-B) and the use of post-TUR-B intravesical mitomycin, intravesical Bacillus Calmette-Guerin (BCG) or intravesical chemotherapy as required. The BC stage is classified as T2 if it involves the detrusor muscle and a different treatment is then necessary. This treatment is more complicated and radical cystectomy is required [Citation2]. Bladder cancers are divided into low-, moderate and high-risk groups to help decide on the treatment [Citation4]. The patients are divided into risk groups according to tumor recurrence and prognostic factors for better determination of post-TUR-B treatment options and follow-up. This classification is also used commonly in follow-up [Citation5]. The follow-up of NMIBC patients is very important. These patients are followed up with imaging methods, cytology and cystoscopy. Methods alternative to cystoscopy have been recommended as cystoscopy is an invasive procedure with potential complications but none of the other methods have been able to replace it so far. The frequency of cystoscopy depends on the risk group [Citation4].
Patient compliance with the treatment protocol is important in terms of survival [Citation6,Citation7]. Cystoscopy compliance has been found to be associated with smoking in bladder cancer cases. Smoking patients show lower compliance with the follow-up protocol [Citation8]. The relationship between patient compliance with medical recommendations and health literacy (HL) has been revealed in previous studies [Citation9–11]. Low HL has also been found to be associated with a poor prognosis in chronic diseases [Citation12–14]. Additionally, the compliance of the patients having poor HL with cancer screening programs is also low [Citation15–18].
Poor HL results in disadvantages for the patients regarding benefiting from treatment services, protection from disease and health promotion issues. We aimed to investigate the relationship between bladder cancer patients' compliance with the cystoscopic follow-up and treatment protocol and HL in this study.
Methods
Patients who underwent TUR-B surgery at the urology department due to a bladder tumor between January 2014 and May 2016 and were found to have NMIBC on pathology evaluation and then underwent cystoscopic follow-up for 1 year or more were included in the study. The treatment of the patients found to have progression and recurrence during follow-up was rearranged. Patients with a cognitive disorder were excluded from the study. The study was conducted with the face to face interview method. Ethics committee approval for the study was obtained from the ethics committee of the hospital. Written informed consent was obtained from all participants before the study.
The patients were divided into low-, moderate and high-risk groups to predict the progression and recurrence risk of the bladder cancer in NMIBC tumors. The patients in the moderate risk group are followed up like the low-risk or high-risk groups according to their clinical situation. Cystoscopic follow-up was performed according to the risk groups of the patients. All the patients with NMIBC underwent an initial cystoscopy at the 3rd month after TUR-B. If this cystoscopy was negative, cystoscopy was performed again 9 months later in the low-risk group and these patients were recommended follow-up with cystoscopy once a year for 5 years. The high-risk group was recommended cystoscopy follow-ups every 3 months for the initial 2 years and every 6 months for 2–5 years afterwards while the high-risk group was recommended lifelong follow-up. The patients with a tumor in the low-risk group were scheduled for cystoscopy two times in the first year and those in the high-risk group were scheduled for the procedure four times in the first year. Patients in the moderate risk group were included in the cystoscopic follow-up program just like the low- or high-risk groups according to their individual and clinical characteristics. Cystoscopy follow-up was performed under local or general anesthesia according to the patient's clinical status. The compliance of the patients with cystoscopic follow-ups was classified as complete and incomplete compliance.
Health literacy was evaluated with the HLS-EU scale. The Health Literacy Survey-European Union (HLS-EU) consists of 47 questions with a score of 1 to 4 (1 = very difficult, 2 = difficult, 3 = easy, 4 = very easy). The Turkish validity and reliability of the scale has been demonstrated by Tanrıover et al. [Citation19]. This scale uses the patient's own perception of the behavior's difficulty for each question. We also used sub-indices (general HL index, health care HL index, disease prevention HL index, health promotion HL index) based on the average values of the HL parameters within the scale. The answers were evaluated using both the general index and sub-indices. We grouped the patients as inadequate HL (0–33 points) and adequate HL (34–50 points) according to the HL sub-group distributions and then investigated the compliance of the NMIBC patients within these groups with cystoscopy follow-up.
Statistical analysis
The compliance of the variables with a normal distribution was investigated using the Shapiro–Wilk test. Constant variables were expressed as mean ± standard deviation. Categorical variables were expressed as n (%). The independent double sample t test was used to compare two groups according to the normality test result and the chi-square test was used for intragroup comparisons of categorical variables. The inner consistency of the HL scale was investigated with the Cronbach alpha coefficient. Reliability coefficients of the HL scale and sub-scales were found to be α = 0.871 for health care, α = 0.892 for disease prevention, α = 0.907 for health promotion, and α = 0.954 for the general scale. A post-hoc analysis was conducted using a large effect size, based upon findings of the present study. The SPSS (IBM Corp., IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp. Released 2012) program was used for the statistical analyses and p < .05 was accepted as statistically significant.
Results
A moderate effect size was obtained by comparing “treatment compliance rates between low risk and high risk”. Using this effect size (r = 0.76) for low risk and n = 69 for high risk, achieved power was estimated as 0.80 at the significance level of α = 0.05.
Socio-demographic characteristics of the participants are given in . The mean age of the patients was 67.13 ± 10.77. There were 111 males and 15 females. In the patient group, 60.3% were primary school graduates, 76.2% had a good income and 73% were not smoking.
Table 1. Socio-demographic characteristics of the participants.
The relationship of socio-demographic data with HL is shown in . The ratio of patients aged <65 years in the adequate HL group was higher than in the inadequate HL group and the ratio of patients aged ≥65 was higher in the inadequate HL group. We found a difference in educational level between the HL groups. Sub-group analyses revealed that the ratio of those with an educational level of primary school or under was higher in the HL group (p < .001). The ratio of those who were secondary school graduates was higher in the adequate HL group (p = .033). The ratio of those who were high school graduates and above was higher in the adequate HL group (p = .012). The ratio of those with good income was higher in the adequate HL group. There was no difference between the HL groups regarding smoking.
Table 2. The relationship of the general characteristics of the participants with the state of health literacy.
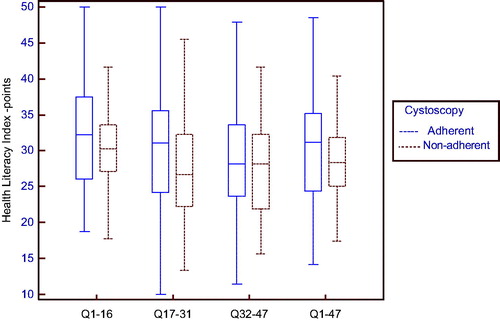
The HL results review showed higher health promotion and general index scores in the group aged <65 (). There was a difference in the sub-dimensions of the HL scale and general scale scores according to the educational level. Health care service scores of those with an educational level of primary school or under were lower than those who were secondary school and high school graduates or above (p < .001 and p < .001, respectively). Disease prevention scores of those whose educational level was primary school or under were also lower than those who were secondary school and high school graduates and above (p = .003 and p = .001, respectively). Health promotion scores of those whose educational level was primary school or under were similarly lower than those who were high school graduates and above (p < .001). Healthcare service scores of those whose educational level was primary school or under were lower than those who were secondary school or high school graduates and above (p = .002 and p < .001, respectively). HL scale sub-dimensions and general scale score of those with low income was lower than those with good income. HL scale sub-dimension and general scale scores showed no difference according to smoking.
Table 3. The change of health literacy according to the patient characteristics.
The treatment continuity rate was 80.50% (n = 33) in the adequate HL group (n = 41) and 56.50% (n = 48) in the inadequate HL group (n = 85) with a statistically significant difference (p = .008). The relationship between treatment continuity and mean HL scores is given in .
Table 4. The relationship of health literacy and sub-groups with treatment continuity.
There was no difference between the groups who were observed or not observed to be compliant with the treatment according to the sub-dimensions of the HL scale and general scale score (). There was no difference by stage between the age groups (). The rate of compliance of the group aged under 65 with treatment was higher than the ≥65 age group.
Table 5. The relationship between age and risk group and treatment compliance.
Discussion
The study revealed better health literacy in patients fully complying with the follow-up protocol. Treatment compliance of younger patients was also better than the elderly patients. Health literacy was found to be associated with the age, educational state and economic state of the patients. We did find any relationship between smoking and treatment compliance, unlike previous studies.
Progression and recurrence are important in bladder cancer. The recurrence rate within 5 years is 30–80% and the progression rate 1–45% [Citation20]. The main purpose in the follow-up and treatment of these tumors is to decrease recurrence, prevent progression, and protect the bladder functions. Follow-up programs for this purpose take the risk groups into account by considering the clinical and pathological features of the tumor [Citation21]. The follow-up of NMIBC patients should avoid unnecessary frequent follow-up of the low-risk group and inadequate follow-up of the high-risk group. Cystoscopy and urine cytology are the accepted follow-up methods. Low-risk factors are primary, solitary, TaG1 (low grade, low malignant potential papillary urothelial neoplasm (PUNLMP)), <3 cm tumors without CIS. Tumors between the low- and high-risk categories are moderate risk tumors. High-risk factors are T1, high grade (G3), multiple, recurring and >3 cm Ta(G1-G2) tumors with CIS. Cystoscopic follow-up is recommended according to the risk group. Cystoscopy results direct the follow-up and treatment. Many factors affect the compliance of cancer patients with the follow-up protocol. These factors may be related to the physician, the patient or a combination of these. Inadequate patient–physician communication, the workload of the clinic performing the follow-up, and the education of the patient are among the leading causes.
Cancer patients with low health literacy have been reported to have lower rates of attending screening visits [Citation15–18]. Health literacy is a concept related to competence of patients being treated for their disorder and the protection and improvement of their health. We found 100% compliance with the follow-up protocol in patients with excellent HL compared to much lower rates in those with limited and inadequate health literacy. Informing patients may be expected to be a cost-effective approach in patients with bladder cancer due to the expectation that the prognosis will be better in patients who fully comply with the follow-up protocol.
The correlation between the treatment compliance and age can be explained with better cognitive functions of the younger patients and higher expectations from life. The cognitive impairment rate in individuals over the age of 65 is known to be 10–20% and is higher in males [Citation22]. The loss in cognitive function and degradation in health literacy can be considered as an obstacle for older individuals to benefit adequately from health services [Citation23–27]. Bladder cancer is generally a disease of older men. Patients with bladder cancer can therefore be considered to have a partial decrease of their cognitive functions. The compliance of these patients with follow-up should be closely followed and the patient should be contacted for appointment reminders as necessary. Similarly, the life expectancy of elderly patients may be low. It may, therefore, be necessary to take initiatives to increase the motivation of elderly patients with bladder cancer. Any relationship between health literacy and the prognosis of the disease can be revealed with prospective studies.
Limitations
A limitation was that the study was single centered. Multi-center studies evaluating the prognosis with a higher number of patients will enable better determination of the importance of HL for patients with bladder cancer.
Conclusions
Adequate health literacy in patients with bladder cancer is associated with better compliance with the treatment protocol. Young patients follow the follow-up protocol recommended by the physician better. Studies aimed at increasing the compliance of elderly patients with inadequate health literacy with the follow-up protocol should be performed.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
- Anastasiadis A, de Reijke TM. Best practice in the treatment of nonmuscle invasive bladder cancer. Ther Adv Urol. 2012;4:13–32.
- Sexton WJ, Wiegand LR, Correa JJ, et al. Bladder cancer: a review of non-muscle invasive disease. Cancer Control. 2010;17:256–268.
- Sylvester RJ, van der Meijden AP, Oosterlinck W, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49:466–475.
- Busato Júnior WF, Almeida GL, Ribas CA, et al. EORTC risk model to predict progression in patients with non-muscle-invasive bladder cancer: is it safe to use in clinical practice? Clin Genitourin Cancer. 2016;14:176–182.
- Khare SR, Aprikian A, Black P, et al. Quality indicators in the management of bladder cancer: a modified Delphi study. Urol Oncol. 2017;35:328–334.
- Karl A, Adejoro O, Saigal C, et al. AND Urologic Diseases in America Project. General adherence to guideline recommendations on initial diagnosis of bladder cancer in the United States and influencing factors. Clin Genitourinary Cancer. 2014;12:270–277.
- Kowalkowski MA, Goltz HH, Petersen NJ, et al. Educational opportunities in bladder cancer: increasing cystoscopic adherence and the availability of smoking-cessation programs. J Canc Educ. 2014;29:739–745.
- Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns. 2016;99:1079–1086.
- (a) Komenaka IK, Nodora JN, Hsu CH, et al. Association of health literacy with adherence to screening mammography guidelines. Obstet Gynecol. 2015;125:852–859. (b) Speros C. Health literacy: concept analysis. J Adv Nurs. 2005;50: 633–640.
- Martin LR, Williams SL, Haskard KB, et al. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–199.
- Volk RJ, Jibaja-Weiss ML, Hawley ST, et al. Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns. 2008;73:482–489.
- DeWalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239.
- Sheridan SL, Halpern DJ, Viera AJ, et al. Interventions for individuals with low health literacy: a systematic review. J Health Commun. 2011;16(sup3):30–54.
- Sentell TL, Tsoh JY, Davis T, et al. Low health literacy and cancer screening among Chinese Americans in California: a cross-sectional analysis. BMJ Open. 2015;5:e006104.
- Kobayashi LC, Wardle J, von Wagner C. Limited health literacy is a barrier to colorectal cancer screening in England: evidence from the English Longitudinal Study of Ageing. Prev Med. 2014;61:100–105.
- Sentell T, Braun KL, Davis J, et al. Health literacy and meeting breast and cervical cancer screening guidelines among Asians and whites in California. Springer Plus. 2015;4:432.
- van der Heide I, Uiters E, Jantine Schuit A, et al. Health literacy and informed decision making regarding colorectal cancer screening: a systematic review. Eur J Public Health. 2015;25:575–582.
- Durusu-Tanrıöver M, Yıldırım HH, Demiray-Ready FN, et al. Türkiye Sağlık Okuryazarlığı Araştırması. Birinci Baskı. Ankara: Sağlık-Sen Yayınları; 2014.
- Babjuk M, Burger M, Zigeuner R, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. EurUrol. 2013;64:639–653.
- van Rhijn BW, Zuiverloon TC, Vis AN, et al. Molecular grade (FGFR3/MIB-1) and EORTC risk scores are predictive in primary nonmuscle-invasive bladder cancer. Eur Urol. 2010;58:433–441.
- Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312:2551–2561.
- Goh VH, Hart WG. Association of general and abdominal obesity with age, endocrine and metabolic factors in Asian men. Aging Male. 2016;19:27–33.
- Kosilov K, Kuzina I, Kuznetsov V, et al. Cognitive functions and health-related quality of life in men with benign prostatic hyperplasia and symptoms of overactive bladder when treated with a combination of tamsulosin and solifenacin in a higher dosage. Aging Male. 2017 [Nov 7]; [9 p.]. DOI:10.1080/13685538.2017.1398723
- Kocoglu H, Alan C, Soydan H, et al. Association between the androgen levels and erectile function, cognitive functions and hypogonadism symptoms in aging males. Aging Male. 2011;14:207–212.
- Martin DM, Wittert G, Burns NR. Gonadal steroids and visuo-spatial abilities in adult males: implications for generalized age-related cognitive decline. Aging Male. 2007;10:17–29.
- Bozkurt H, Demirci H. Health literacy among older persons in Turkey. Aging Male. 2018 [Feb 10]; [6 p.]. DOI:10.1080/13685538.2018.1437901