Abstract
Aim
Sodium-glucose cotransporter 2 inhibitors have been shown to reduce the risk of cardiovascular disease in type 2 diabetes (T2DM) patients. The purpose of this study was to evaluate cardiovascular disease risk indirectly through Doppler ultrasonography (USG) of carotid artery vascular markers in T2DM patients using dapagliflozin.
Methods
One hundred forty-five patients presenting to our clinic between March 2016 and June 2018 and diagnosed with T2DM were included in the study. These were divided into two groups – a dapagliflozin group of 85 patients and a 60-member non-dapagliflozin control group. Common carotid artery end-diastolic velocity (EDV), peak systolic velocity (PSV), and resistive index (RI) parameters were evaluated using Doppler USG in both groups.
Results
The mean duration of follow-up was 2.2 ± 0.4 years. Mean ages were 45 ± 14 years in the dapagliflozin group and 42 ± 15 in the control group. Mean HbA1c was 7.4 ± 1.6 in the dapagliflozin group and 7.3 ± 2.1 in the control group. Common carotid artery, PSV, and EDV parameters were higher (p = .012/p = .036), while RI was lower (p ˂ .001), in the dapagliflozin group than in the control group.
Conclusion
Vascular resistance was lower in the group using dapagliflozin for diabetes management.
Introduction
Arterial hypertension, cardiovascular diseases, and end-organ damage may be seen with increased peripheral vascular resistance [Citation1]. Doppler ultrasonography (USG) is an effective, non-invasive, and inexpensive scanning method for measuring peripheral vascular resistance [Citation2]. Low values for parameters such as peak systolic (PSV) end-diastolic flow velocity (EDV), and high values for the resistance index (RI), measured using USG from the carotid arteries, have been proved to be associated with cardiovascular disease in numerous studies [Citation3–6]. The atherosclerotic process is accelerated by diabetes, and is correlated with an increased RI detected with carotid Doppler USG [Citation7].
Dapagliflozin is a sodium-glucose co-transporter 2 (SGLT2) inhibitor that reduces renal glucose reabsorption, thus increasing urinary glucose excretion [Citation8]. SGLT2 inhibition in the renal proximal tubule improves urinary glucose excretion and produces mild amelioration in hemoglobin A1C. This, in turn, leads to sustained systolic and diastolic blood pressure reduction, partially through natriuresis and possibly also due to a decrease in sympathetic tone. Randomized clinical trials involving high cardiovascular risk patients with type 2 diabetes (T2DM) suggest that the unique effects of SGLT2 inhibitors on blood pressure and body weight may result in a reduced risk of cardiovascular events and slowed renal disease progression [Citation9]. A benefit in terms of decreased vascular stiffness with dapagliflozin use has been demonstrated in the first days of therapy [Citation10].
The purpose of this study was to indirectly evaluate the effect of at least six months of dapagliflozin therapy on vascular indicators of cardiovascular disease risk, using carotid artery RI measurements at Doppler USG in T2DM patients.
Methods
Patients
One-hundred-forty five patients with T2DM were divided into two groups in this descriptive cross-sectional study, T2DM cases using dapagliflozin for at least six months (n = 85) and T2DM cases not receiving dapagliflozin (n = 60). All patients were diagnosed at the Duzce University Medical Faculty Department of Internal Medicine and Ordu Medical Park Hospital Department of Endocrinology, Turkey. Inclusion criteria were age over 20 years, diagnosis of T2DM, and prescription of dapagliflozin between January 2016 and December 2018. Exclusion criteria were age under 20 years or over 80, pregnancy, and diagnosis of peripheral arterial disease, kidney failure, history of coronary artery disease, heart failure, stroke, vasculopathy or any condition known to affect the RI and other USG parameters. This study was performed in accordance with the principles of the Declaration of Helsinki. Permission for the study was obtained from the institutional ethics committee, and informed consent was obtained from all patients.
Carotid Doppler ultrasonography
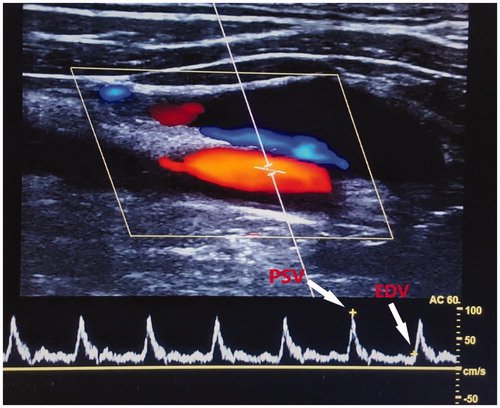
While all patients were screened using thyroid USG, carotid artery Doppler USG was also applied. Carotid Doppler USG was performed with a high-resolution apparatus (Philips Affiniti 70 ultrasound; Philips North America Andover, MA, USA) equipped with a 5–12 MHz wide band linear array probe. All Doppler USG imaging was performed by an experienced specialist. Current velocities were measured as a standard 30–60-degree angle of the lumen. Common carotid artery end-diastolic velocity (EDV), mean peak systolic velocity (PSV), and RI values were determined and recorded (). RI was defined using the formula (PSV-EDV)/PSV.
Statistical analysis
Data analysis was conducted on Statistical Package for the Social Sciences (SPSS) version 21.0 software (SPSS Inc., Chicago, IL, USA). Parametric parameters were expressed as mean plus standard deviation (SD), and non-parametric parameters as median (minimum-maximum) values. The independent t-test and Mann-Whitney U test were applied for comparisons between these groups. Categorical variables were evaluated using Pearson’s chi-square test. A p level of <.05 was regarded as statistically significant.
Results
One hundred forty-five patients were divided into a dapagliflozin group of 85 members (52 male, 33 female) and a non-dapagliflozin control group of 60 members (36 male, 24 female). The mean duration of follow up was 2.2 ± 0.4.years. There was no statistically significant difference between the groups in terms of gender (p=.923). The mean age of the dapagliflozin group was 54.12 ± 13.71 years, and that of the control group was 53.67 ± 14.3 (p=.856). The mean duration of diabetes was 7.6 ± 3.4 years in the dapagliflozin group and 7.5 ± 4.2 years in the control group (p=.762). Mean Hba1c was 7.4 ± 1.6 in the dapagliflozin group and 7.3 ± 2.1 in the control group. The general characteristics of the two groups are shown in . Common carotid artery PSV was 58.12 ± 9.43 cm/s in the dapagliflozin group and 46.72 ± 12.3 cm/s in the control group (p = .036). Common carotid artery EDV was 13.84 ± 1.98 cm/s in the dapagliflozin group and 11.07 ± 4.6 cm/s (p = .012) in the control group. RI values were 0.81 ± 0.54 in the dapagliflozin group and 0.71 ± 0.83 in the control group, and this difference was statistically significant (p = .001). A comparison of Doppler USG parameter values between the groups is shown in .
Table 1. Cases demographic characteristics.
Table 2. A comparison of Doppler USG hemodynamic parameters between the groups.
Discussion
T2DM is a risk factor for cardiovascular disease, limb loss, and mortality [Citation11]. However, there is no convincing evidence to show that improved glucose parameters are by themselves capable of lowering the risk of cardiovascular disease. One randomized controlled trial comparing Empagliflozin, another SGLT2 inhibitor, with placebo in patients with T2DM and high cardiovascular risk reported that the SGLT2 inhibitors seemed to reduce the incidence of cardiovascular events [Citation12]. Empagliflozin has also been observed to reduce arterial stiffness in patients with Type 1 diabetes [Citation13]. However, the mechanisms by which SGLT2 inhibitors lower the risk of cardiovascular events in T2DM is not yet fully understood. The present study examined the effects of dapagliflozin on peripheral arterial resistance and blood flow in T2DM management. A previous study performed to clarify the mechanism involved reported that dapagliflozin improves endothelial functions [Citation10]. That same study also showed that dapagliflozin produces endothelial improvement by reducing oxidative stress. Antioxidants are already known to be capable of preventing endothelial dysfunction associated with hyperglycemia [Citation14]. One striking finding from Solini et al.’s study was that dapagliflozin therapy produced a significant decrease in arterial stiffness measured from the renal arteries, beginning on the second day of treatment, independently of the decrease in blood pressure [Citation10]. That decrease in arterial stiffness is consistent with the results of the present study, which included patients with T2DM, in which treatment with dapagliflozin resulted in higher EDV and PSV values and a lower RI compared to the non-dapagliflozin group at a follow-up time of 2 ± 0.4 years. We think that the reduction of RI is one important reason for the decrease in cardiovascular events associated with SGLT2 inhibitors. Decreased PSV and EDV and increased RI disrupt endothelial function, and this endothelial dysfunction then reduces parenchymal blood flow, thus leading to organ damage [Citation10]. We attributed this finding to dapagliflozin preventing/slowing atherosclerotic plaque development and/or to reducing arterial inflammation.
Early detection of vascular changes using Doppler USG may permit immediate measures to be taken aimed at preventing or delaying irreversible tissue damage [Citation6]. Similarly, awareness of the clinical signs of subclinical vascular disease can contribute to the selection of appropriate treatment in patients with T2DM. Inflammation plays a known role in the pathophysiology of atherosclerotic peripheral vascular disease and peripheral vascular resistance [Citation15,Citation16]. Additionally, the presence of high triglyceride, low-density lipoprotein (LDL), insulin, and urea levels, and of diabetes and obesity are associated with an elevated systemic low-grade inflammatory state in men [Citation17]. A relationship has been described between adipose tissue and inflammation, and chronic inflammation contributes to the pathogenesis of diabetes and cardiovascular disease [Citation18]. In addition, negative correlations have been reported between carotid artery velocities and blood pressure, fasting glucose levels, triglyceride levels, BMI, and waist circumference [Citation19,Citation20]. The elevated mean total cholesterol, triglyceride, LDL-cholesterol, and BMI levels in both of our study groups and the improved RI outcomes with dapagliflozin suggest the involvement an anti-inflammatory effect of the drug. Of particular note, no difference was determined in the use of antilipidemics between the groups. Adipose tissue and testosterone levels are inversely correlated, and testosterone levels in men are known to decrease with advanced age. However, the role of testosterone in cardiovascular health and its effect on endothelial functions are still controversial. Its effects also depend on the source (endogenous or exogenous) and dose involved [Citation18,Citation21,Citation22]. Low testosterone levels have been shown to be correlated with carotid intima-media thickness, as well as metabolic syndrome [Citation23]. The prevalence of testosterone deficiency syndrome is as high as 30% in men with diabetes or obesity [Citation24]. Older men with lower testosterone levels are known to exhibit a higher prevalence of morbidities including T2DM [Citation24]. Similarly, a meta-analysis including 56 studies showed lower testosterone and free testosterone levels in men with T2DM [Citation21]. We suggest that a potential subgroup that might benefit from dapagliflozin consists of men with T2DM and low testosterone levels, with correspondingly significantly higher values for biomarkers of subclinical atherosclerosis, such as Apolipoprotein B [Citation25]. Men with T2DM and risk factors for cardiovascular disease, and a more pronounced inflammatory state as observed in patients with high BMI, with augmented adipose tissue, and with hyperlipidemia may benefit from dapagliflozin therapy. Improvement in RI with dapagliflozin therapy suggests that its use may be beneficial in the early stage of vascular disease and endothelial dysfunction. Similarly, erectile dysfunction is considered an early predictor of vascular disease, and is known to be correlated with endothelial progenitor cells, which precede vascular damage [Citation26]. Patients with erectile dysfunction and T2DM can therefore also benefit from this therapy. A similar effect may also be achieved in lower urinary tract dysfunction [Citation27], and patients with obstructive sleep apnea [Citation28] may also benefit.
Due to the cross-sectional nature of this study, no causal relationship could be proved, since this usually requires longitudinal investigation, and this represents one limitation of our research. Another limitation was the small sample size. Patient characteristics, accompanying diseases, various treatments received, etc. may all have affected our findings. Additionally, carotid intima-media thickness, a parameter strongly linked to cardiovascular risk factors, were not measured. Finally, this study provides no data concerning laboratory measurements, lifestyle parameters, or primary healthcare and socioeconomic characteristics.
In conclusion, the findings of this study demonstrate that the SGLT2 inhibitor dapagliflozin caused significant improvement, with an increase in PSV and EDV and a decrease in RI in the common carotid artery. These findings are consistent with the fact that SGLT2 inhibitors reduce cardiovascular events in patients with T2DM. We think that dapagliflozin should be prescribed specifically to patients with risk factors or signs of subclinical vascular disease to prevent accelerated vascular events in T2DM management.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Prejbisz A, Warchoł-Celińska E, Florczak E, et al. Renal resistive index in patients with true resistant hypertension: results from the RESIST-POL study. Kardiologia Polska (Polish Heart J). 2015;74(2):142–150.
- Li J-C, Xu Z-H, Yuan Y, et al. Impact of atherosclerosis and age on Doppler sonographic parameters in the diagnosis of renal artery stenosis. J Ultrasound Med. 2012;31(5):747–755.
- Ulgen MS, Bilici A, Acar M, et al. The relationship of coronary artery disease and carotid Doppler flow velocity and resistance index in patients with no significant carotid stenosis. Angiology. 2001;52(6):433–434.
- Razzaq AA, Khan BA, Jadoon CK, et al. Carotid Doppler ultrasonography in young stroke patients. J Pak Med Assoc. 1999;49(4):97.
- Doi Y, Iwashima Y, Yoshihara F, et al. Renal resistive index and cardiovascular and renal outcomes in essential hypertension. Hypertension. 2012;60(3):770–777.
- Chuang S-Y, Bai C-H, Cheng H-M, et al. Common carotid artery end-diastolic velocity is independently associated with future cardiovascular events. Eur J Prev Cardiolog. 2016;23(2):116–124.
- Kinouchi M, Aihara K, Fujinaka Y, et al. Diabetic conditions differentially affect the endothelial function, arterial stiffness and carotid atherosclerosis. JAT. 2014;21(5):486–500.
- Gonzalez DE, Foresto RD, Ribeiro AB. SGLT-2 inhibitors in diabetes: a focus on renoprotection. Rev Assoc Med Bras. 2020;66(suppl 1):s17–s24.
- Yandrapalli S, Aronow WS. Cardiovascular benefits of the newer medications for treating type 2 diabetes mellitus. J Thorac Dis. 2017;9(7):2124–2134.
- Solini A, Giannini L, Seghieri M, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16(1):138.
- Hu W-S, Lin C-L. A nationwide cohort study of the role of CHADS2 score in predicting lower extremity amputation and death among patients with peripheral arterial occlusive disease. Aging Male. 2019;22(1):39–44.
- Birkeland KI, Jørgensen ME, Carstensen B, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. The Lancet Diabetes & Endocrinology. 2017;5(9):709–717.
- Cherney DZ, Perkins BA, Soleymanlou N, et al. The effect of empagliflozin on arterial stiffness and heart rate variability in subjects with uncomplicated type 1 diabetes mellitus. Cardiovasc Diabetol. 2014;13(1):28.
- Title LM, Cummings PM, Giddens K, et al. Oral glucose loading acutely attenuates endothelium-dependent vasodilation in healthy adults without diabetes: an effect prevented by vitamins C and E. J Am Coll Cardiol. 2000;36(7):2185–2191.
- Savoia C, Sada L, Zezza L, et al. Vascular inflammation and endothelial dysfunction in experimental hypertension. Int J Hypertens. 2011;2011:1–8.
- Velioglu Y, Yuksel A. Complete blood count parameters in peripheral arterial disease. Aging Male. 2019;22(3):187–191.
- Kawada T, Otsuka T, Endo T, et al. Aging, components of metabolic syndrome and serum C-reactive protein showed significant relationship with carotid atherosclerosis. Aging Male. 2012;15(1):42–47.
- Mohamad N-V, Wong SK, Wan Hasan WN, et al. The relationship between circulating testosterone and inflammatory cytokines in men. The Aging Male. 2019;22(2):129–140.
- Chytilova E, Malik J, Kasalova Z, et al. Lower wall shear rate of the common carotid artery in treated type 2 diabetes mellitus with metabolic syndrome. Physiol Res. 2009;58(2):185 ̶ 191.
- Irace C, Carallo C, Crescenzo A, et al. NIDDM is associated with lower wall shear stress of the common carotid artery. Diabetes. 1999;48(1):193–197.
- Zhang J, Li X, Cai Z, et al. Association between testosterone with type 2 diabetes in adult males, a meta-analysis and trial sequential analysis. The Aging Male. [cited 2019 Jan 16]:[12 p.].DOI:10.1080/13685538.2018.1557139
- Mäkinen JI, Perheentupa A, Irjala K, et al. Endogenous testosterone and brachial artery endothelial function in middle-aged men with symptoms of late-onset hypogonadism. Aging Male. 2011;14(4):237–242.
- Kwon H, Lee D-G, Kang HC, et al. The relationship between testosterone, metabolic syndrome, and mean carotid intima-media thickness in aging men. Aging Male. 2014;17(4):211–215.
- Erenpreiss J, Fodina V, Pozarska R, et al. Prevalence of testosterone deficiency among aging men with and without morbidities. Aging Male. [cited 2019 Jun 1]:[5 p.]. DOI: 10.1080/13685538.2019.1621832
- Rezanezhad B, Borgquist R, Willenheimer R, et al. Association between serum levels of testosterone and biomarkers of subclinical atherosclerosis. Aging Male. 2018;21(3):182–186.
- Condorelli RA, Calogero AE, Vicari E, et al. Endothelial progenitor cells and erectile dysfunction: a brief review on diagnostic significance and summary of our experience. Aging Male. 2013;16(2):29–32.
- Azab S. The impact of atherosclerosis on lower urinary tract function. Aging Male. 2013;16(3):108–111.
- Bahar Y, Annakkaya AN, Sen C, et al. Assessment of the frequency of deep venous thromboembolism in obstructive sleep apnea syndrome. Aging Male. [cited 2019 Aug 22]:[6 p.]. DOI:10.1080/13685538.2019.1654451