?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objectives
Acute urinary retention (AUR) is one of the most significant complication of benign prostatic hyperplasia (BPH). The gold standard surgical treatment for BPH, transurethral resection of the prostate (TURP), is not without significant side effects and a prolonged hospital stay. The aim of this study is to evaluate the role of Rezūm ™ steam ablation in the treatment of patients with AUR secondary to BPH.
Methods
Patients who developed AUR and failed their trial without a catheter (TWOC) were recruited. They were counselled about the procedure and offered the treatment. Pre-operative, intraoperative and post operate data were collected.
Results
All patients were followed up for a mean period of 7.2 months. 100% of patients passed their TWOC and stopped taking any BPH medications after. There was an average of 43.8% decrease in TRUS volume and a fall of 52.5% in PSA value after intervention. The mean operation time was 8.8 min and mean duration in hospital was 5.8 h. No deterioration in sexual function was reported.
Conclusions
Rezūm ™ steam ablation of the prostate is safe, fast and effective day case procedure in treating patients with AUR secondary to BPH. All patients were satisfied with the functional outcomes.
Introduction
Acute urinary retention (AUR) is defined by the sudden and often painful inability to urinate, which usually requires catheterization [Citation1]. It can be the first presenting symptom for men with benign prostatic hyperplasia (BPH) [Citation2]. More commonly, men with BPH will present with lower urinary tract symptoms (LUTS). Acute urinary retention is one of the most significant progression and complication of BPH [Citation3]. BPH is amongst the conditions that are most often associated with the aging male [Citation4–6]. The incidence of LUTS in men increases with age [Citation7] and a linear association was found between increasing age and worsening LUTS in men [Citation8].
The consequences of BPH can have significant effects to the individual, their family and the healthcare system. BPH is said to affect approximately 3.2 million men in the United Kingdom (UK) and surgery for BPH is one of the 10 most common surgeries performed by the National Health Service (NHS) [Citation9]. It is estimated that £180,797, 430 is spent on treatment for BPH every year, and around 60% of those incurred in secondary care as a consequence of managing its’ complications [Citation9]. On an individual level, the effects of BPH can significantly impact the patient’s quality of life (QoL), especially if they develop AUR [Citation10]. BPH can also cause sexual dysfunction, be it reduced libido or erectile dysfunction. A study found that patients with erectile dysfunction were also likely to have severe LUTS [Citation11].
BPH is managed initially by conservative measures followed by medication. Although medications are very effective in treating symptoms of BPH [Citation12], they can also negatively impact the patient’s QoL, especially with side effects of sexual dysfunction [Citation13]. When medical therapy fails and patients are still symptomatic, surgical treatment is then offered. Currently, transurethral resection of the prostate (TURP) remains to be the gold standard surgical treatment due to its proven long term outcomes [Citation14]. However, this procedure is not without complications, some of which can be significantly devastating to patients [Citation15]. Complications and side effects of TURP that could affect the quality of life of the patient include retrograde ejaculation (65–75%), erectile dysfunction (2–10%) and urinary incontinence (2–10%) [Citation16,Citation17]. Furthermore, the procedure often requires an inpatient hospital admission, with an average of 2–3 nights [Citation18,Citation19]. Newer laser based treatments using thulium or holmium laser enucleation of the prostate [Citation20,Citation21] are being performed but they still require a general or spinal anesthetic, an inpatient stay and have comparable complication rates to TURP [Citation22,Citation23].
Rezūm ™ steam ablation of the prostate
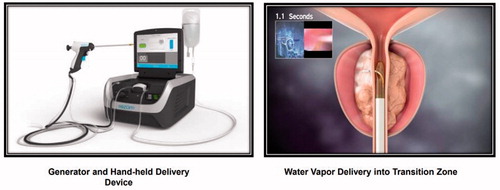
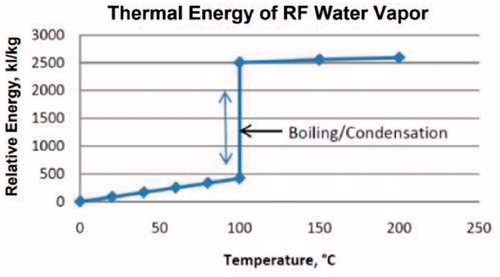
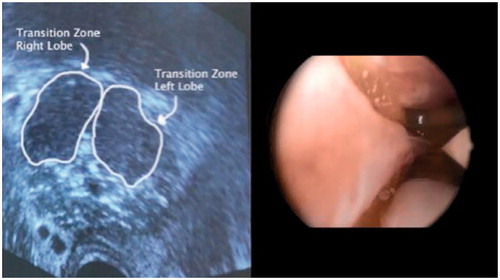
We report on a minimally invasive technique to treat LUTS associated with BPH. Rezūm ™ treats LUTS by using transurethral thermal water vapor therapy [Citation24–27]. Rezūm ™ applies targeted thermal energy to different zones of the prostate [Citation28]. It utilized the radiofrequency heat transfer that exploits the thermodynamic properties of water, resulting in a convectively delivered, precise dose of thermal energy to the prostate [Citation29]. The patient is placed into a standard lithotomy position and the procedure is carried out as a day case procedure either under local or general anesthetic. The system comprises a hand-held transurethral delivery device, which is connected to a radiofrequency generator (). The hand-held delivery device incorporates a standard 30-degree cystoscopy lens [Citation24]. The system is unique in three ways, firstly; there is a heat source where a radiofrequency current is applied to an inductive coil heater, producing thermal energy in the form of water vapor [Citation24,Citation26]. Secondly, there is unique heat transfer via convection [Citation30]. During the treatment, water vapor at 103 °C is delivered via the hand-held device into a 37 °C prostate. There is a phase change where 540 cal/ml of stored thermal energy is released and water vapor turns into liquid [Citation30]. During each course, 9-s bursts of energy is delivered to the transitional zone of the prostate. During this period, there is approximately 70 °C + rise in temperature of the prostate gland (), resulting in instantaneous prostatic cell necrosis [Citation31]. At a temperature of >70 cell death is immediate and irreversible. Lastly, these effects are uniquely confined within their respective pseudocapsules and prostate zones. The water vapor however cannot penetrate the boundaries between different zones of the prostate, and therefore stays within the zone it targets () [Citation32,Citation33].
Aims
The aim of this study is to evaluate the role of Rezūm ™ steam ablation of the prostate in the treatment of patients with acute urinary retention secondary to benign prostatic hyperplasia. More specifically, it can be broken down into several objectives:
Is Rezūm ™ steam ablation of the prostate effective in eliminating acute urinary retention, reducing prostate size and alleviating LUTS?
Is Rezūm ™ steam ablation of the prostate safe and cost effective in treating patients with AUR secondary to BPH?
Can Rezūm ™ steam ablation of the prostate avoid sexual dysfunction and is it a durable and sustainable option in treating BPH?
Methods
A retrospective analysis of patients who developed acute urinary retention (AUR) and subsequently failed their trial without a catheter (TWOC) was performed. A total of 10 patients were identified and deemed suitable for the procedure. Pre-operative data that were collected included patient demographics, BPH medications, prostate specific antigen (PSA) value, residual volume on catheterization, transrectal ultrasound guided (TRUS) volume and International Index of Erectile Function (IIEF) score. Patients were then counselled about the procedure and offered the treatment. Intraoperative data included anesthetic modality, theatre time, operation time, cystoscopic findings and number of treatment cycles. The patients were then followed up after several months [mean= 7.2 months], and post-operative data was collected. These parameters included time to trial without a catheter (TWOC), international prostate symptom score (IPSS), post-void residuals, Qmax, sexual dysfunction, PSA volume, prostate volume, length of stay and any complications.
Inclusion criteria
Age >50 and <90 years, TRUS volume 100 cc, benign digital rectal examination (DRE).
Exclusion criteria
Patients were excluded from the trial if they have a prostate volume of 30 cc or
100 cc. Patients who had urinary implants or penile prosthesis were also excluded.
Results
The results of all 10 patients were included in the study (). All patients were already on some form of pharmacological treatment for LUTS prior to catheterization. 6 patients were taking an alpha-adrenergic antagonists, whilst 4 patients were on combination therapy with an α-blocker and a 5-α-reductase inhibitor. Two patients who were sexually active completed the IIEF score to assess their sexual function.
Table 1. Pre-operative data.
Table 2. Intra-operative data.
Table 3. Post-operative data.
Table 4. Pre and post intervention [Mean follow up period = 7.2 months].
Discussion
Is rezūm ™ steam ablation of the prostate effective in eliminating acute urinary retention, reducing prostate size and alleviating LUTS?
The results indicate that this is an effective approach in treating patients with acute urinary retention. There was a 100% success rate for patients passing their TWOC. All patients that were recruited had initially failed their TWOC, and our follow up revealed that all patients are catheter free after the procedure. 70% of patients passed their first TWOC at 4 weeks and 30% passed the second TWOC at 6 weeks. The mean TRUS volume had also decreased after intervention (73.8 cc and 41.5 cc respectively). This meant that there was an average of 43.8% decrease in TRUS volume after the procedure. Post-operative PSA value also fell by 52.5%. All patients were satisfied with the functional outcomes as their mean QoL score after the treatment was 0.7. On average, the patients had a satisfactory mean Qmax score of 13.7 after the procedure considering the mean age of 75. Finally, the mean PVR volume was significantly reduced to 107.2mls compared to the mean 1100 ml residual volume before treatment.
Similar studies have also confirmed the effectiveness of this method in reducing prostatic volume and treating symptoms of relating to BPH. Dixon et al conducted a pilot study to evaluate the acute ablative capabilities of the prostate [Citation31]. The study found Rezūm ™ to be a success as there was evidence of thermal ablation of the prostate in all the specimens. The thermal ablation using water vapor were confined to the transitional zone of the prostate, which was consistent with the principles of convection. Dixon et al then followed up patients over a 24 month period after the initial pilot study to evaluate the effectiveness of Rezūm ™ [Citation34]. They found a mean change in reduction in IPSS score from 21.7 to 9.6, an improvement of Qmax from 8.3 ml/s to 12 ml/s and a reduction in PVR volume from 78.5 to 62.8 ml [Citation34].
Mynderse et al conducted a study in men who underwent treatment by Rezūm ™ ablation with follow up magnetic resonance imaging (MRI) of their prostate after treatment [Citation35]. The study compared the lesion volume, volume in transitional zone and total prostatic volume before the treatment and at subsequent periods after treatment. Similar to our findings, the study revealed that Rezūm ™ treatment was successful in reducing prostatic volume. Imaging at 6 months indicated that the procedure was successful in reducing lesion volume by a mean of 95.1%, transitional zone volume by 38% and whole prostate volume by 28.9%.
McVary et al also conducted a comprehensive 4 year randomized controlled study, including a crossover trial to evaluate the safety and efficacy of the Rezūm ™ System and to assess its effects on LUTS secondary to BPH [Citation36,Citation37]. Baseline demographics that were collected and then reassessed over a 4 year period include international prostate symptom score (IPSS), Qmax, BPH Impact Index (BPH II) and quality of life (QoL) [Citation37]. At 4 years, there was a −10.1 point reduction in IPSS and 4.2 point improvement in Qmax. BPH II and quality of life was also noted to remain significantly improved after 4 years ( and ) [Citation36–38].
Figure 4. Clinically significant tissue volume reduction. Image taken from Rezum II Pivotal study Patient. Consent from in study. 2013 07-29 ICF Rev 02 Pivotal.
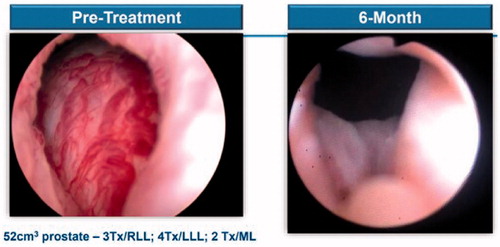
Figure 5. Sustained durability from 4 year data (Rezum II Pivotal Study) [Citation36–38].
![Figure 5. Sustained durability from 4 year data (Rezum II Pivotal Study) [Citation36–38].](/cms/asset/36830054-2bc5-4467-8b56-68d83844faf6/itam_a_1901273_f0005_c.jpg)
Is rezūm ™ steam ablation of the prostate safe and cost effective in treating patients with AUR secondary to BPH?
We collected data on any complications that occurred immediately after the procedure and in the following months. The only adverse effect reported was a blocked catheter that was managed with a simple bladder washout.
None of the patients in our study required an overnight inpatient stay. The mean operation time was short (8.8 min) and the mean time in hospital for all patients was only 5.8 h. This is highly cost effective and would have a significant impact on the NHS as the average length of stay in hospitals for a standard TURP is 2–3 days [Citation19].
Similar findings were also reported by McVary et al during their 4 year crossover study [Citation36]. During their 4 year RCT, no disturbance in sexual function was reported. Amongst the treatment and crossover patients, 57% of them did not report any adverse effects. The adverse effects that were reported by the remaining 43% of patients were mostly mild to moderate in nature. The most common adverse effect that was reported was dysuria (18.1%) and hematuria (11.7%) [Citation36,Citation38]. Other adverse effects included hematospermia, urinary frequency, urinary retention and urgency. However, they all resolved within 3 weeks.
Can rezūm ™ steam ablation of the prostate avoid sexual dysfunction and is it a durable and sustainable option in treating BPH?
This study found the effects of the procedure was still evident in all patients after a 7.2 month follow up period. All patients stopped any BPH medications. The study conducted by McVary et al also supports the durability of Is Rezūm ™ in the treatment of BPH. Over a 4 year period, the surgical retreatment rates were 4.4% and only two patients (5.2%) returned to BPH medications [Citation36,Citation38].
Gupta et al also evaluated the three year treatment outcome of Rezūm ™ water vapor therapy compared to BPH medications with data from the MTOPS trial [Citation39]. The study looked at symptom improvement via IPSS reduction, impact on sexual function and rates of clinical progression. They concluded that a single Rezūm ™ procedure provided effective and sustainable improvements in IPSS with lower observed clinical progression rates compared to long-term use of BPH medications.
For patients who were sexually active, no deterioration was reported in this study. In fact, there was a slight increase (9.3%) in their sexual function after the procedure. McVary et al also looked at sexual function by comparing data from the Rezūm ™ study and the MTOPS trial [Citation40]. They found that a single Rezūm ™ treatment had no damaging effects on sexual function compared to the negative effects on sexual function with the use of BPH medications.
Conclusion
The results concluded that Rezūm ™ steam ablation of the prostate is safe, fast and effective in treating patients with AUR secondary to BPH. The sample size was small, and hence further research should be conducted in a multicenter setting, with a larger cohort and a longer follow up period. However, all patients in this study were catheter free and satisfied with the functional outcomes as shown by IPSS, QoL, Qmax and PVR volume. Anatomy such as middle lobes did not affect the patient outcomes and in men who were sexually active no deterioration was reported. All patients stopped any BPH medication. This cohort of patients opted for general anesthesia; however, it can be performed under sedation, spinal and local anesthesia. The only adverse effect reported was a blocked catheter that was managed with a simple bladder washout. In summary, Rezūm ™ is a safe, effective day case procedure for men with AUR secondary to BPH and further studies with a larger sample size is being conducted.
Disclosure statement
This is to acknowledge that there are no financial interest or benefit that has arisen from the direct applications of our research.
References
- Dawson C, Whitfield H. ABC of urology. Urological emergencies in general practice. BMJ. 1996;312(7034):838–840.
- Verhamme KMC, Dieleman JP, van Wijk MAM, et al. Low incidence of acute urinary retention in the general male population: the triumph project. Eur Urol. 2005;47(4):494–498.
- Roehrborn CG. The epidemiology of acute urinary retention in benign prostatic hyperplasia. Rev Urol. 2001;3(4):187–192.
- Bardoli AD, Taylor WSJ, Mahmalji W. Can the UroLift prostatic implant device treat the symptoms of benign prostatic hypertrophy, avoid sexual dysfunction and reduce hospital TURP waiting times? A single centre, single surgeon experience and review of the literature. Aging Male. 2017;20(3):192–197.
- Singam P, Hong GE, Ho C, et al. Nocturia in patients with benign prostatic hyperplasia: evaluating the significance of ageing, co-morbid illnesses, lifestyle and medical therapy in treatment outcome in real life practice. Aging Male. 2015;18(2):112–117.
- Calogero AE, Burgio G, Condorelli RA, et al. Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male. 2019;22(1):12–19.
- Logie J, Clifford GM, Farmer RDT. Incidence, prevalence and management of lower urinary tract symptoms in men in the UK. BJU Int. 2005;95(4):557–562.
- Verhamme KMC, Dieleman JP, Bleumink GS, et al. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care—the triumph project. Eur Urol. 2002;42(4):323–328.
- Kirby RS, Kirby M, Fitzpatrick JM. Benign prostatic hyperplasia: counting the cost of its management. BJU Int. 2010;105(7):901–902.
- Thomas K, Oades G, Taylor-Hay C, et al. Acute urinary retention: what is the impact on patients' quality of life? BJU Int. 2005;95(1):72–76.
- Demir O, Akgul K, Akar Z, et al. Association between severity of lower urinary tract symptoms, erectile dysfunction and metabolic syndrome. Aging Male. 2009;12(1):29–34.
- Yassin A, Saad F, Hoesl CE, et al. Alpha-adrenoceptors are a common denominator in the pathophysiology of erectile function and BPH/LUTS-implications for clinical practice. Andrologia. 2006;38(1):1–12.
- Favilla V, Russo GI, Privitera S, et al. Impact of combination therapy 5-alpha reductase inhibitors (5-ARI) plus alpha-blockers (AB) on erectile dysfunction and decrease of libido in patients with LUTS/BPH: a systematic review with meta-analysis. Aging Male. 2016;19(3):175–181.
- Mishriki SF, Grimsley SJS, Nabi G, et al. Improved quality of life and enhanced satisfaction after TURP: prospective 12-year follow-up study. Urology. 2008;72(2):322–326.
- Foster HE, Barry MJ, Dahm P, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J Urol. 2018;200(3):612–619.
- British Association of Urological Surgeons (BAUS). Transurethral Prostatectomy (TURP) for benign disease [Internet]; 2017. Available from: https://www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/TURP%20for%20benign.pdf.
- Rassweiler J, Teber D, Kuntz R, et al. Complications of Transurethral Resection of the Prostate (TURP)—incidence, management, and prevention. Eur Urol. 2006;50(5):969–980.
- Kirollos MM. Length of postoperative hospital stay after transurethral resection of the prostate. Ann R Coll Surg Engl. 1997;79:284–288.
- Gravas S, Bach T, Bachmann A. EAU Guidelines on the management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO) [Internet]; 2020. Available from: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Management-of-non-neurogenic-male-LUTS-2016.pdf.
- Sarma D, Singh Y, Baruah SJ, et al. Thulium laser vaporization versus vapoenucleation (without morcellation) technique for BPH: do we have a winner? JELEU. 2019;2(1):e24–e36.
- Vazirian-Zadeh M, Anderson J, Gill R, et al. Thulium Laser Enucleation of the Prostate (ThuLEP) as a technique for treatment of BPH: evaluation of a six-year experience at a single institution. JELEU. 2018;1(2):e10–e14.
- Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004;172(5):1926–1929.
- Cornu J-N, Ahyai S, Bachmann A, et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol. 2015;67(6):1066–1096.
- Hoey M. Water vapor for tissue ablation. NxThera Inc; 2009.
- Green Z, Westwood J, Somani BK. What's new in Rezum: a transurethral water vapour therapy for BPH. Curr Urol Rep. 2019;20(7):39.
- Westwood J, Geraghty R, Jones P, et al. Rezum: a new transurethral water vapour therapy for benign prostatic hyperplasia. Ther Adv Urol. 2018;10(11):327–333.
- Dhliwayo B, Mukhtar S. Novel surgical treatments for benign prostatic hyperplasia. JELEU. 2019;2(1):e17–e23.
- Elterman D. New less invasive management of BPH. Toronto, Ontario, Canada; 2020 [cited 2020 Oct 24]. Available from: https://content.tts.org/content/videos/cua/MH2020/Dean_Elterman.pdf.
- Magistro G, Chapple CR, Elhilali M, et al. Emerging minimally invasive treatment options for male lower urinary tract symptoms. Eur Urol. 2017;72(6):986–997.
- Dixon C, Cedano ER, Pacik D, et al. Efficacy and safety of Rezūm system water vapor treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology. 2015;86(5):1042–1047.
- Dixon C, Cedano ER, Mynderse L, et al. Transurethral convective water vapor as a treatment for lower urinary tract symptomatology due to benign prostatic hyperplasia using the Rezūm® system: evaluation of acute ablative capabilities in the human prostate. RRU. 2015;7:13–18.
- Burr JM, Hay DJ, Ludgate S, et al. Hot and cold technologies for tissue ablation in urology. BJU Int. 2006;98(6):1149–1153.
- McNeal JE. The zonal anatomy of the prostate. Prostate. 1981;2(1):35–49.
- Dixon C, Cedano ER, Pacik D, et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol. 2016;8:207–216.
- Mynderse LA, Hanson D, Robb RA, et al. Rezūm system water vapor treatment for lower urinary tract symptoms/benign prostatic hyperplasia: validation of convective thermal energy transfer and characterization with magnetic resonance imaging and 3-dimensional renderings. Urology. 2015;86(1):122–127.
- McVary KT, Rogers T, Roehrborn CG. Rezūm water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-year results from randomized controlled study. Urology. 2019;126:171–179.
- McVary KT, Gange SN, Gittelman MC, et al. Minimally invasive prostate convective water vapor energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2016;195(5):1529–1538.
- McVary KT, Roehrborn CG. Three-year outcomes of the prospective, randomized controlled rezūm system study: convective radiofrequency thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Urology. 2018;111:1–9.
- Gupta N, Rogers T, Holland B, et al. Three-year treatment outcomes of water vapor thermal therapy compared to doxazosin, finasteride and combination drug therapy in men with benign prostatic hyperplasia: cohort data from the MTOPS trial. J Urol. 2018;200(2):405–413.
- McVary KT, Rogers T, Mahon J, et al. Is sexual function better preserved after water vapor thermal therapy or medical therapy for lower urinary tract symptoms due to benign prostatic hyperplasia? J Sex Med. 2018;15(12):1728–1738.