Abstract
Objective
To report an extremely rare case of bladder cancer patient with cervical lymph nodes, abdominal lymph nodes, and bone metastases at the same time.
Methods and results
The case was investigated by follow-up and immunohistochemistry was used in the pathological part.
Result
The patient was diagnosed with bladder cancer (high-grade urothelial metastatic epithelial cell carcinoma) by pathology and immunohistochemistry after transurethral resection of bladder tumor (TURBT) and metastatic bladder cancer by pathology and immunohistochemistry after cervical lymph node aspiration due to neck lymph node enlargement 1 year later, and a CT of the chest and abdomen suggested that the patient also had abdominal lymph node and bone metastases.At the 2.5-year regular chemotherapy follow-up, the patient showed that the abdominal lymph node metastasis disappeared, the cervical lymph node fusion shrank, and the bone metastasis still existed.
Conclusion
1. Regular postoperative review is particularly important; 2.For patients with UCB who undergo TURBT, a effective regular perfusion program should be performed throughout the postoperative period; 3. For patients with postoperative metastatic symptoms of UCB, Complex treatment has a positive effect on patient prognosis; 4.The presence of enlarged head and neck lymph nodes in patients with bladder cancer should also be considered as metastatic of UCB.
Introduction
Urothelial cancer of the bladder (UCB), as the second largest cancer of the genitourinary system, is potentially lethal [Citation1]. There are both internal genetic factors and external environmental factors, the two most obvious risk factors are smoking and long-term exposure to industrial chemical products. UCB has the characteristics of high morbidity, high recurrence rate, high mortality, and the incidence in man is much higher than in woman. However, related studies have shown there was no correlation between any categories that determine tumor aggressiveness of UCB and total testosterone levels in adult man [Citation2]. Ping Wang et al. [Citation3] showed that among 2470 patients with bladder cancer with distant metastasis, the most common site was bone (1183 cases, 47.89%), followed by lung (1140 cases, 46.15%), liver (718 cases, 29.07%), distant lymph nodes (198 cases, 8.01%) and brain (85 cases, 3.44%). The mode of lymphatic metastasis is mainly through lymph node metastasis to pelvic lymph nodes such as obturator foramen and iliac vessels, and rarely to head and neck lymph nodes. Its metastasis basically develops from proximal to distant according to anatomical site [Citation4], here we report an extremely rare case of bladder cancer for cases of cancer metastasis, according to the case reports we have retrieved so far, there is no case of bladder cancer patients with cervical lymph nodes, abdominal lymph nodes, and bone metastases at the same time. At the same time, we conduct a review of relevant literature, which is reported and discussed below.
Case report
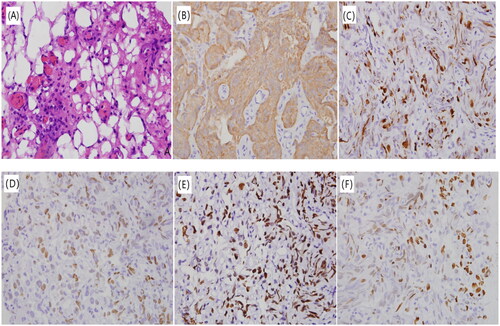
A male patient, 47 years old, was admitted to the outpatient department of our hospital in March 2019 mainly due to painless intermittent gross hematuria. The urine routine showed hematuria, and the color Doppler ultrasound of the urinary system showed that a 1.6*1.1 cm uneven echogenic bulge was seen on the left posterior wall of the bladder, strong echoes were seen inside, considered bladder space-occupying lesions. Then the patient underwent cystoscopy in a local hospital, which showed mild trabecular cell changes in each wall of the bladder, the mucous membrane was not smooth, and the surface seemed to be attached with pseudomembrane-like substances. After biopsy, the pathological consultation in our hospital showed: A small amount of mucosal tissue in the bladder, lymphocyte infiltration in the superficial lamina propria, and proliferative tumor-like urothelial mass in some areas. Combined with IHC examination: GATA-3 (+), P53 (sporadic cells +), P63 (+), Ki-67 (index10%), P16 (+), tend to have a high possibility of early superficial urothelial carcinoma. According to the guidelines of urology, the patient had surgical indications and underwent the transurethral resection of bladder tumors (TURBT). The postoperative pathological diagnosis was consistent with high-grade urothelial carcinoma. Immunohistochemistry shows: AE1/AE3(+), P63(+), P40(+), P53(90%+), Ki67(index80%), Vimentin(-). As shown in .
Figure 1. Pathological results of patient after TURBT. (A) HE staining (×400) showed the pathological type of high-grade uroepithelial carcinoma; (B) IHC (×400) showed positive AE1/AE3 expression; (C) IHC (×400) showed positive Ki67 expression (index 80%); (D) IHC (×400) showed positive P40 expression; (E) IHC (×400) showed positive P53 expression, 90%+; (F) IHC (×400) showed shows positive P63 expression.
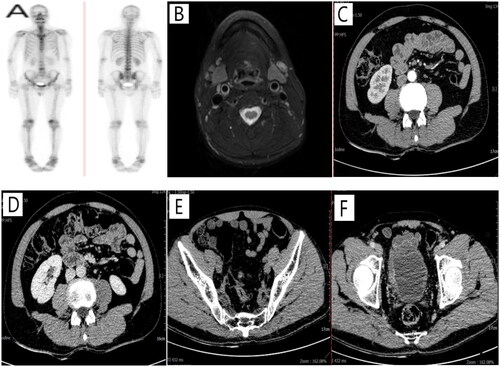
After discharge, the patient was regularly reviewed and underwent intravesical infusion chemotherapy (pirarubicin hydrochloride 8 instillations once a week as induction and thereafter 9 instillations once a month as maintenance). The patient do need the optimal treatment after the first TURBT,which should be intravesical BCG treatment as induction and maintenance when he received the diagnosis of T1HG disease.But it is really difficult to find BCG in our hospital, so we select pirarubicin hydrochloride as intravesical infusion chemotherapy. the case has not received an optimal follow-up (FU) during intravesical infusion chemotherapy. One year later, the patient visited our outpatient department for the first time because of cervical lymphadenopathy. On physical examination, the left side of the neck was palpable, and a subcutaneous mass of about 5.0 cm in diameter was palpable, the texture was tough and fluctuating. The patient underwent chest CT: There were multiple enlarged lymph nodes in the left neck, considering the possibility of metastasis, the whole abdominal CT scan and enhanced CT showed: bladder cancer, posterior wall type, T2N3M1a stage, no liver metastasis, multiple retroperitoneal and pelvic lymph node metastasis. bone scintigraphy scans suggest: 1. Active bone salt metabolism in the lumbar 1–4 vertebrae, and bone metastases are mostly considered; 2. The bone salt metabolism is slightly active after the left 10, except for bone metastases. As shown in . After the patient underwent cervical lymph node biopsy, the pathological findings showed cancer in fibrous tissue. Immunohistochemical results: CK-P(+), P40(+), P63(+), CAm5.2(+), Ki (about 20%), Uroplakin (+), HER2 (3+), combined with the patient’s medical history and pathological and immunohistochemical findings, the lymph nodes biopsied by puncture were consistent with metastases from uroepithelial carcinoma of the bladder. As shown in . After contacting the medical oncology department of our hospital, the patient began to receive "Tislelizumab Injection 200 mg ivd d1" immunotherapy combined with "Gemcitabine injection 1.8 g ivd d1/8 + Cisplatin 130 mg ivd d1" 21 days/cycle regimen chemotherapy for 6 cycles, And zoledronic acid 4 mg ivd for bone metastases to prevent bone destruction. After 6 cycles of maintenance treatment, the patient was assessed to be in fair condition and started chemotherapy with "Disitamab Vedotin For Injection 120 mg" for 9 cycles, during which the patient again developed hematuria. Repeat thyroid color Doppler ultrasound showed that a 1.0*0.6 cm hypoechoic nodule was seen beside the common carotid artery in the left supraclavicular fossa. Neck MRI showed enlarged lymph nodes in the neck IV area and left clavicle. Re-examination of whole-body bone tomography showed that the bone salt metabolism of the lumbar 1–4 vertebrae was lower than before, the density was higher than before, and the scope of osteogenesis was expanded, considering bone metastatic disease, and the salt metabolism of the left 10 posterior ribs was similar to that of the former. Whole abdominal CT showed abnormal abdominal and pelvic lymph nodes disappeared. As shown in . The patient’s re-examination of cystoscopy showed that there were two raised masses on the right side and the left side of the bottom of the bladder, about 0.5–1.0 cm in size. After biopsy was taken and sent for pathological biopsy, it suggested high-grade urothelial carcinoma of the bladder. TURBT was performed again, and the postoperative pathology showed high-grade urothelial carcinoma of the bladder, T2N3M1a stage. The patient continued to receive "Disitamab Vedotin For Injection 120 mg" for intensive treatment after surgery. The patient is currently being followed up.
Figure 2. Partial imaging examinations after the patient developed metastatic symptoms. (A) whole-body bone tomography showed active bone salt metabolism in lumbar 1–4 vertebrae, mostly considering bone metastases; (B) chest CT showed multiple enlarged lymph nodes in the left side of the neck, considering possible metastases; (C,D) whole-abdomen CT showed multiple retroperitoneal lymph node metastases; (E,F) whole-services CT showed multiple pelvic lymph node metastases.
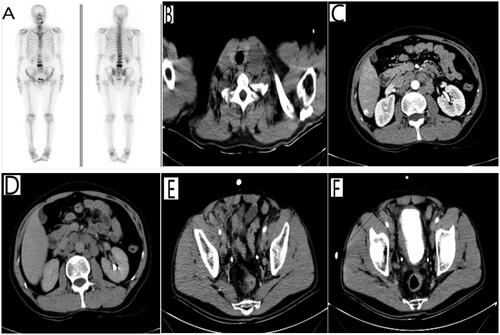
Figure 3. Cervical lymph node biopsy results. (A) HE staining (×400) showed indicates migratory cell carcinoma on cervical lymph node puncture; (B) IHC (×400) showed positive CAm5.2 expression; (C) IHC (×400) showed positive CK-P expression; (D) IHC (×400) showed positive CK8/18 expression; (E) IHC (×400) showed positive HER2 expression (3+); (F) IHC (×400) showed positive Ki67 expression; (G) IHC (×400) showed positive P40 expression; (H) IHC (×400) showed positive P63 expression; (I) IHC (×400) showed positive Uroplakin expression.
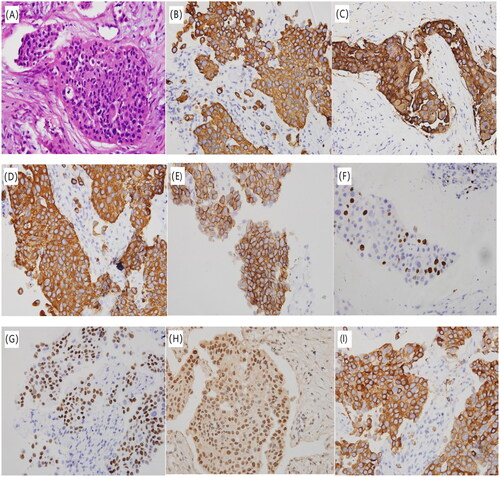
Figure 4. Partial imaging examinations after regular chemotherapy. (A) whole-body bone tomography showed that the bone salt metabolism of the lumbar 1–4 vertebrae was lower than before, the density was higher than before, and the range of osteogenesis was expanded. (B) Magnetic resonance imaging of the neck showed that multiple enlarged lymph nodes were seen in the neck area IV and the left clavicle fossa, both D1WI and T2WI showed high signal, abnormal lymph nodes were considered. (C,D) Whole abdominal CT showed abnormal abdominal lymph nodes disappeared. (E,F) Whole abdominal CT showed abnormal pelvic lymph node disappeared.
Discussion
Urological tumors metastasize to lymph nodes above the diaphragm in fewer cases, with renal cancer being the most common, while metastatic cell carcinoma of the bladder metastasizes mainly to pelvic lymph nodes via lymph nodes such as the obturator fossa and iliac vessels, and rarely to head and neck lymph nodes. Hessan et al. [Citation5] retrospectively studied a study of 845 patients with head and neck metastases from genitourinary tract including kidney, prostate, bladder, testis, penis, urethra and ureteral tumors, only 31 (3.7%) of these tumors developed metastases to the cervical and supraclavicular lymph nodes and only 3 of 207 metastases originated from UBC. According to a large retrospective autopsy data reported by Wallmeroth et al. [Citation6]. Metastases in cervical lymph nodes were rare (4%) and always associated with other nodal metastases. They think there was no significant difference in frequency and distribution of nodal metastases between patients with and without cystectomy. But the mechanism of metastasis is not fully understood, with hematologic and lymphatic vascular spread via vertebral veins [Citation7] to the head and neck as its possible route, mainly because its metastasis basically develops from proximal to distant according to anatomical site. Lymph node metastasis of bladder cancer has also been reported to be associated with postoperative hypercalcemia [Citation8], but its recurrence and metastasis are not dependent on the characteristics of the primary tumor [Citation9], and microscopic or macroscopic metastasis of bladder cancer at the time of diagnosis is the reason why invasive urothelial carcinoma cannot be cured [Citation10]. There are some cases of bladder cancer presenting with supradiastinal lymph nodes metastasis after surgery.As shown in .
Table 1. cases of bladder cancer presenting with supradiastinal lymph nodes metastasis after surgery.
For patients with cervical lymph node metastasis in bladder cancer, which has suggested end-stage bladder cancer status, it is difficult to evaluate the standard treatment in such cases due to the rare reports of such cases, short survival and loss of access to surgical radical treatment. Related studies have shown androgen suppression therapy (comprising a 5-a reductase inhibitor (5-ARi) and androgen deprivation therapy (ADT)) can effectively reduce the incidence, recurrence and mortality of UCB, among which 5-Ari can effectively reduce cancer-specific mortality, and ADT can effectively reduce the recurrence rate of UCB [Citation14], and in some patients with high recurrence rate, palliative radiotherapy, chemotherapy and immunotherapy measures are mentioned [Citation9,Citation15]. As suggested by 2019 urology guidelines: radiotherapy, palliative cystectomy, and symptomatic supportive treatment (including management of urinary tract obstruction, hematuria and lower urinary tract symptoms, and management of symptoms associated with metastases) are feasible for patients with non-radically resectable tumors (1、T4a; 2、lymph nodes cannot be removed; 3、M+;). Another study noted that even concomitant prostate cancer as a second malignancy did not represent a risk factor for survival even in patients with organ-restricted UCB [Citation16]. The patient we reported here received TURBT after being diagnosed with UCB, one year later, he was diagnosed with bladder cancer metastasis by lymph node biopsy and was treated with regular chemotherapy and regular outpatient review. For bone metastases to prevent bone destruction, he was treatedwith chemotherapy and zoledronic acid . The review showed that the cervical lymph nodes had decreased in extent and the abdominal lymph nodes did not show but the bone metastases remained. At present, Chemotherapy regimens for metastatic bladder cancer are mostly GC regimens (gemcitabine + cisplatin) and MVAC (methotrexate + doxorubicin + cisplatin) regimens, although both are very important for bladder cancer patients after surgery, there was no significant difference in the pathological remission rate, but the adverse reactions of the GC regimen were mild, which may be related to the lower toxicity of the GC regimen. According to the relevant literature, the average efficiency of cisplatin-based systemic chemotherapy was reported to be about 50–60% [Citation17], and advanced bladder metastatic cell carcinoma achieved 0–35% complete remission with an overall remission rate of 12–73% for patients with metastatic disease in cisplatin-based combination chemotherapy [Citation18]. Combined with the case we reported this time, When he was diagnosed with bladder cancer with cervical lymph node metastasis, the cisplatin-based GC chemotherapy regimen was given, which showed a positive effect in the progression of the disease. This also shows the importance of regular chemotherapy for patients with metastatic bladder cancer, which has a positive effect on patient prognosis. This patient is still under follow-up.
Conclusion
It is the first case report that the lymph nodes in the neck were pathologically diagnosed as metastatic UCB. Due to the lack of large-scale reports of such cases, the diagnosis and treatment of bladder cancer metastasis is still routinely treated, and the precise diagnosis and treatment needs to be further discussed. Therefore, at present, for patients diagnosed like this case, we draw the following conclusions: 1. Regular postoperative review is particularly important; 2. For patients with UCB who undergo TURBT, a effective regular perfusion program should be performed throughout the postoperative period; 3. For patients with postoperative metastatic symptoms of UCB, Complex treatment has a positive effect on patient prognosis; 4. The presence of enlarged head and neck lymph nodes in patients with bladder cancer should also be considered as metastatic of UCB.
Ethical approval
The report of this study was approved by the ethics commit-tee of our institution, and written informed consent was obtained from the patient.
Acknowledgments
The authors sincerely thank the patient for his contribution to the publication of this case report.
Disclosure statement
No potential conflicts of interest were disclosed.
Additional information
Funding
References
- Soave A, Kluwe L, Yu H, et al. Copy number variations in primary tumor, serum and lymph node metastasis of bladder cancer patients treated with radical cystectomy. Sci Rep. 2020;10(1):21562–21562.
- Kafkasli A, Yazici O, Can U, et al. Testosterone status is not associated with bladder cancer parameters in adult male patients: results of a prospective controlled study. Aging Male. 2021;24(1):101–105.
- Wang P, Zang S, Li G, et al. The role of surgery on the primary tumor site in bladder cancer with distant metastasis: significance of histology type and metastatic pattern. Cancer Med. 2020;9(24):9293–9302. [
- Roth B, Wissmeyer MP, Zehnder P, et al. A new multimodality technique accurately maps the primary lymphatic landing sites of the bladder. Eur Urol. 2010;57(2):205–211.
- Hessan H, Strauss M, Sharkey FE. Urogenital tract carcinoma metastatic to the head and neck. Laryngoscope. 1986;96:1352–1356.
- Wallmeroth A, Wagner U, Moch H, et al. Patterns of metastasis in muscle invasive bladder cancer (pT2-4): an autopsy study on 367 patients. Urol Int. 1999;62(2):69–75.
- Tunio M, Rafi M, Hashmi A, et al. Choroidal metastasis from primary transitional cell carcinoma of urinary bladder: a case report and review of literature. Rawal Med J. 2011;36:69–70.
- Ando T, Katagiri A, Nakayama R, et al. Hypercalcemia associated with lymph node metastasis following radical cystectomy for bladder cancer. IJU Case Rep. 2018;1(1):25–28.
- Sengelov L, Kamby C, von der MH. Pattern of metastases in relation to characteristics of primary tumor and treatment in patients with disseminated urothelial carcinoma. J Urol. 1996;155(1):111–114.
- Stein JP, Cai J, Groshen S, et al. Risk factors for patients with pelvic lymph node metastases following radical cystectomy with en bloc pelvic lymphadenectomy: concept of lymph node density. J Urol. 2003;170(1):35–41.
- Kancharla VP, Gulmi FA, Agheli A, et al. Transitional cell carcinoma of the bladder manifestating as malignant lymphoma with generalized lymphadenopathy. Case Rep Oncol. 2010;3(2):125–130.
- Tunio MA, Asiri M, Bayoumi Y, et al. Cervical lymph node metastasis from transitional cell carcinoma of urinary bladder: case report and review of literature. JST. 2012;2(3):59.
- Xie H, Xu Y-M. A case of postoperative axillary lymph node metastasis from bladder cancer. J Clin Urol. 2002;17(12):645.
- Kim A, Kim MS, Ahn JH, et al. Clinical significance of 5-α reductase inhibitor and androgen deprivation therapy in bladder cancer incidence, recurrence, and survival: a meta-analysis and systemic review. Aging Male. 2020;23(5):971–978.
- Zhou L, Liang X, Zhang K. Assessment of the clinical efficacy of simultaneous transurethral resection of both bladder cancer and the prostate: a systematic review and meta-analysis. Aging Male. 2020;23(5):1182–1193.
- Kachanov M, Vetterlein MW, Soave A, et al. Oncologic impact of concomitant prostate cancer characteristics at the time of radical cystoprostatectomy for bladder cancer: a population-based analysis. Aging Male. 2022;25(1):54–61.
- Matsui Y, Nishiyama H, Watanabe J, et al. The current status of perioperative chemotherapy for invasive bladder: a multiinstitutional retrospective study in Japan. Int J Clin Oncol. 2005;10(2):133–138.
- Chester JD, Hall GD, Forster M, et al. Systemic chemotherapy for patients with bladder cancer-current controversies and future directions. Cancer Treat Rev. 2004;30(4):343–358.

