Abstract
Background
Small-cell lung cancer (SCLC) is a highly aggressive tumor with a high metastatic potential, particularly affecting current or former heavy smokers. Treatment typically involves chemotherapy, often combined with radiotherapy, and immunotherapy for extensive disease. Prophylactic cranial irradiation is recommended to reduce brain metastases. Elderly SCLC patients face unique challenges due to frailty and comorbidities, leading to increased risks of treatment-related toxicity and malnutrition. The prognostic nutritional index (PNI), a composite marker of nutritional and immune status, has shown promise in predicting outcomes in various malignancies. However, the optimal treatment approach for very elderly SCLC patients remains unclear, as they are often excluded from clinical trials.
Aims
This study aimed to evaluate the survival outcomes of SCLC patients aged 75 years or older and their correlation with PNI.
Study design
Retrospective cohort study.
Methods
The study retrospectively analyzed data from 71 SCLC patients aged ≥75 years, focusing on age, gender, smoking status, chronic diseases, performance status, clinical stage, treatment modality, and pretreatment PNI. Survival estimates were calculated using the Kaplan–Meier method, and multivariate Cox regression analysis was performed to identify independent predictors of overall survival (OS).
Results
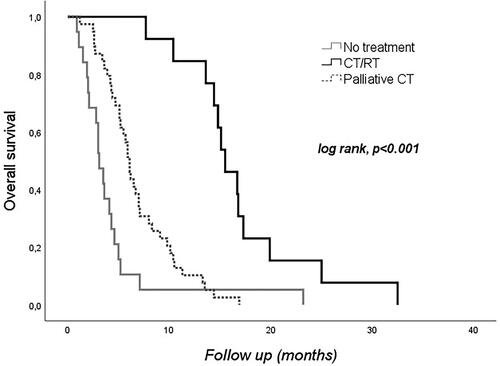
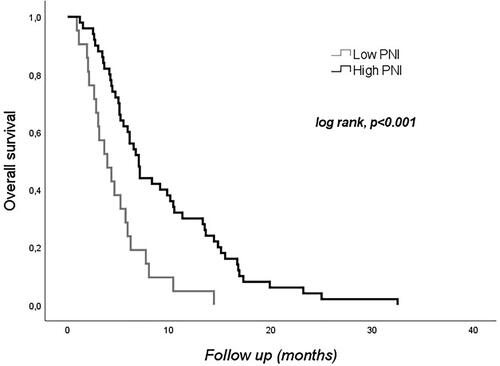
The results demonstrated that 26.8% of very elderly SCLC patients received no active treatment, resulting in a significantly shorter median survival time of 1.3 months. In contrast, patients who underwent aggressive treatment, such as palliative chemotherapy or chemotherapy plus radiotherapy, had significantly longer median survival times. Multivariate analysis revealed that receiving chemotherapy plus radiotherapy was associated with a significant survival benefit compared to no treatment. Furthermore, low PNI (≤40) was independently associated with decreased OS.
Conclusion
This study highlights the importance of active treatment and nutritional support in improving survival outcomes for very elderly SCLC patients. The findings suggest that low PNI and lack of oncological treatment are associated with worse survival outcomes. Therefore, integrating nutritional assessment, interventions, and appropriate treatment strategies are crucial in managing lung cancer patients. Larger, multicenter studies are needed to validate these findings and explore potential interventions to optimize nutritional status and improve outcomes for elderly patients with SCLC.
Introduction
Small-cell lung cancer (SCLC) is a highly aggressive tumor that often metastasizes by the time of diagnosis. It accounts for approximately 15% of all lung cancers and is strongly linked to smoking [Citation1]. Chemotherapy is a crucial part of SCLC treatment due to its propensity for early metastasis. Standard treatment involves combined chemoradiotherapy for limited disease; and chemotherapy with or without immunotherapy for extensive disease [Citation2]. The majority of SCLC patients (75%) are over 60 years old, with a significant proportion aged 75 years or older [Citation3]. Elderly SCLC patients are more likely to have drug-related adverse effects due to their frailty and other comorbidities. Additionally, decreased intestinal motility and loss of appetite are brought on by alterations to the sensory and digestive systems in aged patients [Citation4]. The nutrition is impaired in approximately 30–40% of cancer patients and elderly people are particularly susceptible to malnutrition, which can have negative clinical effects [Citation5]. There is a strong correlation between nutrition, immune health, and the advancement and prognosis of tumors [Citation6]. By combining serum albumin levels and total circulating lymphocyte count, the prognostic nutritional index (PNI) has been developed, which can effectively assess the nutritional and immunological status of individuals with cancer [Citation7]. Recent studies have highlighted the significance of pretreatment PNI in predicting the outcome of patients with different types of malignancies [Citation8].
The number of extremely elderly SCLC patients is anticipated to increase as the population ages. However, clinical trials often exclude this age group, resulting in a lack of data on the best treatment for these patients. This study aims to address this knowledge gap by describing the survival outcomes of very elderly SCLC patients treated with standard therapy and its relation to PNI.
Materials and methods
The study included ≥ 75-year-old patients followed up in our center with the diagnosis of SCLC between 2010 and 2020. Age, gender, smoking status, chronic disease(s), Eastern Cooperative Oncology Group performance status (ECOG PS), clinical stage at diagnosis, treatment modality, and pretreatment PNI parameters of the patients were analyzed retrospectively. The PNI was calculated according to the following formula: 10 × serum albumin (g/dl) + 0.005 × peripheral lymphocyte count (per mm3). The PNI cutoff was established at 40 based on previous studies [Citation9]. The primary outcome of the study was to investigate the effect of low PNI (≤40) on overall survival (OS) in elderly SCLC patients. Approval for the study was obtained from the local ethics committee.
Statistical analyses
Statistical analyses were performed using IBM® SPSS software version 28 (SPSS Inc., Chicago, IL). Descriptive statistics were presented as frequency (percent), mean ± SD, or median (min–max). The χ2 and Exact tests were used to compare the proportions in different categorical groups. Continuous variables were analyzed with the Student′s t-test. Survival estimates were calculated with the Kaplan–Meier method. OS was defined as the period from diagnosis to death from any cause. The log-rank test was used to identify the independent effects on OS. Prediction of OS was specified using multivariate Cox regression analysis. An overall type-1 error level was used to infer statistical significance.
Results
A total of 71 patients [59 (83.1%) men] with a mean age of 77.8 ± 3.2 years were included in the study. Sixty-six (93%) patients were ex-smokers and 46 (64.8%) patients had at least a chronic disease. At diagnosis, ECOG PS was 0 in 14 (19.7%) patients, 1 in 39 (54.9%) patients, 2 in 14 (19.7%) patients, and 3 in 4 (5.6%) patients. While 13 (18.3%) patients had limited disease at diagnosis, 58 (81.7%) patients had extensive disease. Nineteen (26.8%) patients received no oncological treatment, 13 (18.3%) patients received CT or RT, and 39 (54.9%) patients received palliative CT. The median PNI was 43.8 ± 6.4, with low PNI (≤40) for 21 (29.6%) patients and high PNI (>40) for 50 (70.4%) patients. Age, gender, smoking status, presence of chronic disease, ECOG PS, and stage at diagnosis did not significantly differ between the low and high PNI groups. However, the low PNI group had lower rates of therapy utilization ().
Table 1. Comparison of patient characteristics between groups with low and high PNI.
All patients died during a median follow-up of 5.9 (range, 0.9–32.5) months. The estimated median OS was 5.9 (95%CI: 4.7–7.1) months. No relation was found between gender, smoking status, presence of chronic disease, ECOG PS, or stage at diagnosis with OS (). The median OS was 3.1 (95%CI: 2.3–3.8) months in untreated patients, 6.1 (95%CI: 5.5–6.7) months in patients who received palliative CT, and 15.5 (95%CI: 13.3–17.7) months in patients who received CT and RT (p < 0.001, ). Besides, low (≤40) PNI was associated with decreased OS (p < 0.001, ).
Table 2. Overall survival and demographic and clinical parameters.
Multivariate analysis was used to uncover independent effects on OS for significant factors at the p 0.25 level in the log-rank test. The model showed that receiving CT with RT had a significant survival effect compared to no treatment (HR: 0.153, 95%CI: 0.070–0.335, p < 0.001). It also revealed that low PNI is a treatment-independent predictor of OS (HR: 2.220, 95%CI: 1.282–3.844, p = 0.004) ().
Table 3. Factors affecting overall survival - multivariate Cox regression analysis.
Discussion
Very elderly patients often have multiple comorbidities and poor performance status. Furthermore, pulmonary and cardiovascular conditions worsen their health status, and aging lowers functional reserve. As a result, elderly patients have more difficulty tolerating combined therapy [Citation10]. Most treatment standards for SCLC are based on randomized trials, but these trials often exclude aged patients [Citation11]. Therefore, the conclusions drawn from these studies may not be directly applicable to very elderly patients with SCLC. Our study aimed to fill this knowledge gap by analyzing the SCLC cohort aged 75 and over. We found that more than a quarter (26.8%) of these patients did not receive any active treatment. These patients had a very short median survival time of 3.1 months, reflecting the natural course of untreated SCLC. In contrast, patients who underwent aggressive treatment lived significantly longer.
Chemotherapy plays a key role in the treatment of SCLC since it is a systemic disease. The standard recommendation is 4–6 cycles of a platinum-based chemotherapy doublet. Several studies have demonstrated that receiving less than 4 cycles is associated with a poor prognosis. The Intergroup Trial 0096 showed that elderly patients (age >70 years) had a non-inferior response and survival compared to younger patients if they could receive chemotherapy [Citation12]. Additionally, a randomized trial where elderly patients received four cycles of chemotherapy reported a median survival of 11.5 months [Citation13]. These findings support that elderly patients may benefit from chemotherapy if they can tolerate and complete the treatment [Citation14]. Two previous meta-analyses have reported the survival benefits of adding thoracic radiotherapy (TRT) to chemotherapy in patients with limited SCLC (L-SCLC) [Citation15]. TRT has also been reported to improve the survival of selected extensive-stage SCLC (E-SCLC) patients. In one of these studies, it was reported that patients who received TRT in addition to chemotherapy had significantly improved survival than those who received chemotherapy alone (median survival: 17 vs. 11 months; 5-year survival rate 9.1% vs. 3.7%, respectively (p = 0.04) [Citation16]. In addition, retrospective analyzes of elderly patients with SCLC, reported significantly better survival with the addition of TRT to chemotherapy [Citation17,Citation18]. In our study, patients who received both chemotherapy and local radiotherapy had the longest survival of 15.5 months in line with previous data.
ECOG PS is commonly used to assess the functional status of cancer patients. In this dataset, a substantial proportion of patients had PS 0-1, indicating a relatively good performance status at the time of diagnosis. However, the univariable analysis did not show any association between PS and survival. This suggests that even elderly patients with a poor performance score could still have a chance for systemic chemotherapy, as demonstrated by Deepak Sundriyal in his study [Citation19]. The retrospective studies showed that patients with L-SCLC had a significantly better median survival time compared to those with extensive-stage disease [Citation20]. This highlights the importance of the disease stage in predicting survival outcomes. However, in our data set, the lack of association between stage and survival in the univariable analysis suggests that stage alone may not be a significant predictor of survival.
The studies suggest that a low PNI is associated with worse outcomes in SCLC [Citation21,Citation22]. The retrospective studies showed that PNI could be used as an independent prognostic factor for elderly patients with oncology disease [Citation23]. In addition to its prognostic value, PNI has also been investigated as a predictive marker for treatment response and toxicity in SCLC. Several studies have reported that patients with a low PNI are more likely to experience severe treatment-related side effects, such as hematological complications and infections [Citation24]. The results of our study indicated that patients with low PNI (≤40) had significantly decreased OS compared to those with high PNI (>40). Multivariate analysis revealed that low PNI was an important predictor of OS, regardless of treatment received. Identification of PNI as an independent prognostic factor is essential for clinical evaluation. The PNI could serve as a useful prognostic tool in clinical practice, helping to identify patients who may require additional support or interventions to optimize their nutritional status.
It is important to note that this study has several limitations. First, this is a retrospective and single-center study. Second, the sample size is small and therefore does not represent accurately the elderly patient group diagnosed with SCLC. On the other hand, PNI was calculated only once before treatment variability was not recorded, and other biomarkers were not included in the assessment. However, the data found in the study are valuable as they show that the lives of elderly patients with SCLC can be extended with treatment and the right nutritional support. Therefore, there is a need to confirm the data in larger, multicenter studies.
Conclusion
Our study suggests that older patients who received active treatment, such as palliative chemotherapy or chemotherapy plus radiotherapy, had a longer median survival compared to those who did not receive therapy. This finding aligns with the general understanding that active treatment can improve survival outcomes in elderly SCLC patients. The findings suggest that low PNI and lack of oncological treatment are associated with worse survival outcomes. These results emphasize the importance of considering nutritional status and appropriate treatment strategies in the management of lung cancer patients. Further research with larger cohorts is warranted to validate these findings and explore potential interventions to improve the nutritional status and outcomes of lung cancer patients.
Ethical approval
The study was approved by the Health Sciences Ethics Committee of Manisa Celal Bayar University (Decision no: 20.478.486/1569, Date: 02.11.2022).
Authors’ contributions
Concept – E.A.; Design – E.A., S.M.; Data Collection or Processing – S.M.; Analysis or Interpretation – E.A.; Literature Search – E.A.; Writing – E.A., S.M.; Critical Review – S.M.; Fundings – E.A., S.M.
Acknowledgment
None.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Govindan R, Page N, Morgensztern D, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006;24(28):4539–4544. doi: 10.1200/JCO.2005.04.4859.
- Horn L, Mansfield AS, Szczęsna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med. 2018;379(23):2220–2229. doi: 10.1056/NEJMoa1809064.
- Rudin CM, Brambilla E, Faivre-Finn C, et al. Small-cell lung cancer. Nat Rev Dis Primers. 2021;7(1):3. doi: 10.1038/s41572-020-00235-0.
- Mastronuzzi T, Grattagliano I. Nutrition as a health determinant in elderly patients. Curr Med Chem. 2019;26(19):3652–3661. doi: 10.2174/0929867324666170523125806.
- Arends J, Baracos V, Bertz H, et al. ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr. 2017;36(5):1187–1196. doi: 10.1016/j.clnu.2017.06.017.
- Barreira JV. The role of nutrition in cancer patients. Nutr Cancer. 2021;73(11–12):2849–2850. doi: 10.1080/01635581.2020.1839519.
- Wang D, Hu X, Xiao L, et al. Prognostic nutritional index and systemic immune-inflammation index predict the prognosis of patients with HCC. J Gastrointest Surg. 2021;25(2):421–427. doi: 10.1007/s11605-019-04492-7.
- Ding P, Guo H, Sun C, et al. Combined systemic immune-inflammatory index (SII) and prognostic nutritional index (PNI) predicts chemotherapy response and prognosis in locally advanced gastric cancer patients receiving neoadjuvant chemotherapy with PD-1 antibody sintilimab and XELOX: a prospective study. BMC Gastroenterol. 2022;22(1):121. doi: 10.1186/s12876-022-02199-9.
- Sozel H, Beypinar I, Sezgin Goksu S. Prognostic impact of prognostic nutritional index and neutrophil/lymphocyte ratio in patients with small-cell lung cancer. EJMI. 2021;5(2):207–212. doi: 10.14744/ejmi.2021.54277.
- Lichtman SM. Therapy insight: therapeutic challenges in the treatment of elderly cancer patients. Nat Clin Pract Oncol. 2006;3(2):86–93. doi: 10.1038/ncponc0420.
- Okamoto H, Watanabe K, Kunikane H, et al. Randomised phase III trial of carboplatin plus etoposide vs split doses of cisplatin plus etoposide in elderly or poor-risk patients with extensive disease small-cell lung cancer: JCOG 9702. Br J Cancer. 2007;97(2):162–169. doi: 10.1038/sj.bjc.6603810.
- Yuen AR, Zou G, Turrisi AT, et al. Similar outcome of elderly patients in intergroup trial 0096: cisplatin, etoposide, and thoracic radiotherapy administered once or twice daily in limited stage small cell lung carcinoma. Cancer. 2000;89(9):1953–1960. doi: 10.1002/1097-0142(20001101)89:9<1953::AID-CNCR11>3.0.CO;2-6.
- Liu S, Guo H, Kong L, et al. The prognostic factors in the elderly patients with small cell lung cancer: a retrospective analysis from a single cancer institute. Int J Clin Exp Pathol. 2015;8(9):11033–11041.
- Jett JR, Schild SE, Kesler KA, et al. Treatment of small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5):e400S–e419S. doi: 10.1378/chest.12-2363.
- Pignon JP, Arriagada R, Ihde DC, et al. A meta-analysis of thoracic radiotherapy for small-cell lung cancer. N Engl J Med. 1992;327(23):1618–1624. doi: 10.1056/NEJM199212033272302.
- Slotman BJ, van Tinteren H, Praag JO, et al. Radiotherapy for extensive stage small-cell lung cancer - Authors’ reply. Lancet. 2015;385(9975):1292–1293. doi: 10.1016/S0140-6736(15)60679-1.
- An CC, Jing W, Zhang Y, et al. Thoracic radiation therapy could give survival benefit to elderly patients with extensive-stage small-cell lung cancer. Future Oncol. 2017;13(13):1149–1158. doi: 10.2217/fon-2016-0467.
- Corso CD, Rutter CE, Park HS, et al. Role of chemoradiotherapy in elderly patients with limited-stage small-cell lung cancer. J Clin Oncol. 2015;33(36):4240–4246. doi: 10.1200/JCO.2015.62.4270.
- Sundriyal D, Kumar P, Kumar U, et al. Chemotherapy in geriatric patients with poor performance status small cell lung cancer: series from a tertiary care center. Aging Med. 2022;5(2):138–141. doi: 10.1002/agm2.12205.
- Sagman U, Maki E, Evans WK, et al. Small-cell carcinoma of the lung: derivation of a prognostic staging system. J Clin Oncol. 1991;9(9):1639–1649. doi: 10.1200/JCO.1991.9.9.1639.
- He X, Zhou T, Yang Y, et al. Advanced lung cancer inflammation index, a new prognostic score, predicts outcome in patients with small-cell lung cancer. Clin Lung Cancer. 2015;16(6):e165–71–e171. doi: 10.1016/j.cllc.2015.03.005.
- Hong S, Zhou T, Fang W, et al. The prognostic nutritional index (PNI) predicts overall survival of small-cell lung cancer patients. Tumour Biol. 2015;36(5):3389–3397. doi: 10.1007/s13277-014-2973-y.
- Zhou T, Zhan J, Hong S, et al. Ratio of C reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep. 2015;5(1):10481. doi: 10.1038/srep10481.
- Yang Y, Gao P, Song Y, et al. The prognostic nutritional index is a predictive indicator of prognosis and postoperative complications in gastric cancer: a metaanalysis. Eur J Surg Oncol. 2016;42(8):1176–1182. doi: 10.1016/j.ejso.2016.05.029.