Abstract
Background
Hypertension, hyperlipidemia, and hyperglycemia have emerged as global health concerns of paramount significance. With the burgeoning popularity of mind-body therapy, cardiovascular patients have increasingly exhibited a vested interest in the practice of Tai Chi. The objective of this study seeks to quantitatively assess the impact of Tai Chi interventions on blood pressure, lipid levels, and glucose concentrations among the elderly population, thereby explaining the optimal intervention protocol.
Methods
An extensive search was conducted across multiple databases, including Web of Science, PubMed, CNKI, WANFANG DATA, RISS, KISS, and DBPIA, comprising English, Korean, and Chinese literature. The search strategy employed a retrieval method of subject term 1 + subject term 2, which included both full names and abbreviations of the terms. Specifically, “taijiquan” or “Tai Chi” were set as the Term 1, while Term 2 was set as “blood pressure,” “BP,” “Fasting blood glucose,” “FBG,” “Triglyceride,” and “TG.” Thereafter, the retrieved articles were filtered in accordance with the PICOS method. Risk of bias assessment was performed using RoB 2.0, while data analysis was conducted using Comprehensive Meta-Analysis 3.7.
Results
A total of 57 studies, including 3,856 research subjects, were eligible for inclusion. The findings of the primary effect quantitative synthesis demonstrated that Tai Chi exerted an improvement on systolic blood pressure (SBP) (ES = −0.764, p < .001), diastolic blood pressure (DBP) (ES = −0.426, p = .001), triglyceride (TG) (ES = −0.452, p < .001), and fasting blood glucose concentrations (FBG) (ES = −0.552, p = .002) among middle-aged and elderly individuals. Subgroup analysis further revealed that the intervention effects were significantly influenced by the characteristics of the research subjects and the specific intervention protocol employed.
Conclusion
Tai Chi, as a gentle form of aerobic exercise, exerts a profound impact on reducing blood pressure, fasting blood glucose levels, and triglyceride concentrations among middle-aged and elderly individuals. Notably, the intervention effect is particularly pronounced among male patients afflicted with hypertension, hyperglycemia, and hyperlipidemia. Based on the collective advantages underscored by this research, we strongly recommend engaging in Tai Chi exercises for a minimum duration of 16 weeks, with each session lasting 30–50 min and conducted 6–7 times per week, without any restrictions on the style employed.
1. Introduction
Non-communicable diseases (NCDs) (chronic diseases) present a challenge in terms of early detection and have emerged as a global health concern [Citation1]. The proliferation of unhealthy dietary patterns and sedentary lifestyles in the context of rapid societal advancement has exacerbated the development of NCDs [Citation2]. Notable examples of NCDs include hypertension, hyperlipidemia, and hyperglycemia, which are recognized as pivotal risk factors for cardiovascular ailments and premature mortality [Citation3]. Data from the World Health Organization reveals that NCDs account for approximately 41 million fatalities annually, representing a 74% of all global deaths [Citation3]. Recent statistics indicate that 1.28 billion individuals worldwide suffer from hypertension, while hyperglycemia afflicts 5.37 billion individuals [Citation4]. While specific figures pertaining to the global prevalence of hyperlipidemia remain elusive, a Nature study has determined that hypercholesterolemia alone is responsible for 3.9 million deaths each year [Citation5]. Therefore, hypertension, hyperlipidemia, and hyperglycemia constitute pressing global health predicaments that demand unwavering attention.
Tai Chi, a traditional Chinese martial art with a rich historical legacy spanning centuries, has evolved into different styles, including Chen, Yang, Wu, and Sun, with Chen style being the oldest and Yang style enjoying the widest dissemination [Citation6]. Tai Chi represents a holistic form of exercise that seamlessly integrates gentle physical movements with elements of meditation, bodily awareness, and controlled breathing [Citation7]. The burgeoning popularity of mind-body therapies has contributed to increasing interest in Tai Chi among patients afflicted by cardiovascular diseases [Citation8–10]. Numerous studies have demonstrated the beneficial impact of Tai Chi on hypertension [Citation11–16], hyperglycemia [Citation17–21], and hyperlipidemia [Citation21–23]. However, conflicting findings have also emerged from certain studies [Citation12,Citation24–29]. One meta-analysis concluded that Tai Chi exerted no significant influence on blood pressure [Citation30], while another meta-analysis reported its efficacy in the treatment of hypertension [Citation31]. In summary, the majority of meta-analyses have concurred that Tai Chi yields significant effects on fasting blood glucose levels or triglyceride concentrations, albeit no analyses have been conducted to assess the differential effects of various Tai Chi styles [Citation32–34].
Different Tai Chi styles have been found to yield varying results. For instance, a previous meta-analysis revealed that Yang-style Tai Chi did not exhibit a significant impact on fasting glucose levels, whereas other Tai Chi styles demonstrated a significant reduction in fasting blood glucose after intervention cycles lasting longer than 3 months [Citation35]. Presently, there is ongoing debate regarding whether Tai Chi has a positive effect on ameliorating hypertension, hyperlipidemia, and hyperglycemia. In addition, it remains unknown whether the results of Tai Chi interventions can be influenced by factors such as the style of Tai Chi, the gender of participants, and the duration of the intervention.
In this study, we conducted a quantitative analysis of published research on the effects of Tai Chi intervention on blood pressure (BP), fasting blood glucose (FBG), and triglyceride (TG) through meta-analysis. Our objective was to determine the intervention effects of Tai Chi on BP, FBG, and TG using quantification methods, while also exploring the optimal intervention protocol. The results of this study can serve as a reference for Tai Chi exercise therapy in patients with hypertension, hyperlipidemia, and hyperglycemia.
2. Materials and methods
Meta-analysis was conducted according to the PRISMA 2020 Checklist and have registered in PROSPERO (registration number: CRD42023400731).
2.1. Literature searching
To obtain a more comprehensive collection of articles, we searched not only English databases but also Korean and Chinese databases, including Web of Science, PubMed, CNKI, WANFANG DATA, RISS, KISS, and DBPIA. We employed a searching strategy of subject term 1 + subject term 2 and included both full names and abbreviations of all terms. Subject term 1 was set as “taijiquan” or “Tai Chi,” while subject term 2 encompassed “Blood pressure,” “BP,” “Fasting blood glucose,” “FBG,” “Triglyceride,” and “TG.” We included articles officially published before March 2023. Finally, we obtained a total of 3,160 articles, comprising 1,787 in Chinese, 1,318 in English, and 55 in Korean.
2.2. Inclusion and exclusion of literature
The literature screening process adhered to the PICOS methodology. (1) Research participants: middle-aged adults and the elderly. (2) Interventional group: any style of Tai Chi intervention, such as Chen-style Tai Chi, Yang-style Tai Chi, and Wu-style Tai Chi. Since our focus was solely on the effect of Tai Chi intervention, other treatments like diet and medications were not considered. (3) Control group: Routine physical activity based on daily habits. (4) Evaluation indicators: SBP, DBP, FBG, TG. (5) Study type: randomized controlled trial (RCT). Additionally, unquantified effect values were excluded.
2.3. Data extraction
Data extraction was independently conducted by two researchers (WZ and HJ). Firstly, all articles were imported into Zotero 6.0 software to eliminate duplicates. Subsequently, articles that did not meet the eligibility criteria were excluded after reviewing the title and abstract. In addition, articles that could not be fully accessed or from which effect values could not be extracted were also excluded. Finally, the articles that satisfied the criteria were included in the meta-analysis. Throughout the literature screening process, information such as the title, first author’s name, publication year, sample size, characteristics of the study subjects, and intervention details were extracted to facilitate subsequent data analysis. In cases of disagreement between the two researchers during the data extraction process, a third researcher (KZ) made the final decision.
2.4. Risk of bias and publication bias assessment
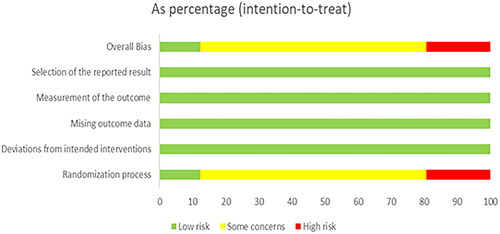
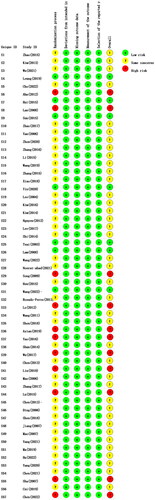
The potential risk of bias in the studies incorporated into this research is appraised using the Cochrane Risk of Bias Tool version 2 (RoB 2.0). The RoB 2.0 instrument comprises five domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Bias risk is delineated into three tiers: low risk, some concerns, and high risk. Moreover, publication bias is evaluated via the funnel plot and Egger’s test found within the Comprehensive Meta-Analysis 3.7 software.
2.5. Data analysis
The assessment of bias risk was conducted using RoB 2.0, while data analysis was performed using Comprehensive Meta-Analysis 3.7 software. In the context of meta-analysis, the standardized mean difference (SMD) is commonly regarded as the primary measure for continuous variables, with Cohen’s d being the most prevalent form of SMD. Previous studies have identified instances of positive deviation and large Cohen’s d values, particularly in small sample sizes. Conversely, Hedges’ g is derived from Cohen’s d after adjusting for factor J (a factor to correct for the positive deviation observed in Cohen’s d) [Citation36]. Therefore, we employed Hedges’ g as the combined effect measure. According to Cohen’s guidelines, an effect size of 0.2 indicates a small effect, 0.5 indicates a moderate effect, and 0.8 indicates a large effect [Citation37]. In addition, the appropriate statistical model was selected based on the magnitude of heterogeneity, as determined by the I2 and P values obtained from the heterogeneity test. Specifically, I2 = 25% indicates low heterogeneity, I2 = 50% indicates moderate heterogeneity and I2 = 75% indicates high heterogeneity [Citation38]. Typically, a random-effects model is employed when I2 ≥ 50% and p < .05, while a fixed-effects model is used when I2 < 50% and p > .05. However, it is important to note that heterogeneity cannot be solely determined by I2 and p values; the potential heterogeneity between different studies must also be taken into consideration [Citation39].
3. Results
3.1. Basic characteristics of included literature
The screening process of the 68 included studies was conducted using Zotero 6.0 software, following the PICOS method. Among these studies, 30 focused on BP [Citation11,Citation12,Citation14–16,Citation25,Citation28,Citation40–62], 18 focused FBG [Citation12,Citation17–21,Citation25,Citation28,Citation44,Citation57,Citation63–70], and 20 focused TG [Citation12,Citation21–24,Citation29,Citation42,Citation44,Citation54,Citation58,Citation61,Citation71–79]. illustrates the screening process. It is worth noting that some studies included multiple intervention groups [Citation14,Citation17,Citation21,Citation73], and one study solely reported SBP without DBP [Citation56]. Therefore, the available datasets for meta-analysis consisted of 31 studies for SBP, 30 studies for DBP, 25 studies for FBG, and 23 studies for TG. Additionally, considering that certain articles provided multiple indicators, such as a study reporting FBG, SBP, and DBP [Citation25], the cumulative number of included articles amounted to 57 (). The included studies encompassed a total of 3856 participants, and their characteristics were organized to facilitate subgroup analysis, including first author, publication year, number of research subjects, gender, abnormal indicators, duration, frequency (times per week), single duration/min, style, and extraction indicators (). The abnormal determination of BP, FBG, and TG was based on the criteria published by the International Diabetes Federation (IDF): BP≧130/85 mmHg, FBG≧100 mg/dl, and TG ≥ 150 mg/dl. Both Chen and Yang styles were included, and if the Tai Chi style was not specified in the article, it was assumed to be conventional Tai Chi, which may comprise multiple Tai Chi styles.
Figure 1. PRISMA 2020 flow chart. This is a PRISMA 2020 flow chart. A total of 3160 articles were initially retrieved, of which 1729 were BP, 624 were FBG and 807 were TG. After screening, a total of 68 articles, including 30 BP, 18 FBG and 20 TG, were finally included in the meta-analysis.
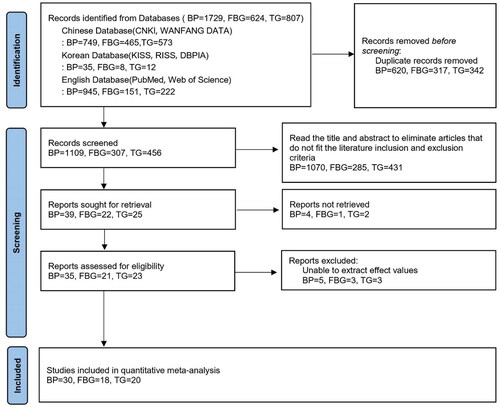
Table 1. Basic characteristics of included articles.
3.2. Risk of bias assessment
The risk of bias in the incorporated studies is illustrated in and . Among these, 11 studies reveal a “High risk” in the Randomization process, 39 studies present “Some concerns” in the Randomization process, and 7 studies denote “Low risk” in the Randomization process. The remaining four risks of bias are shown as Low risk.
3.3. Heterogeneity test and quantitative synthesis of main effects
High heterogeneity (I2 ≥ 75%, p < .001) was observed in all indicators, necessitating the selection of a random effect model to combine the effect values. The findings () demonstrated that Tai Chi exhibited a significant ameliorative effect on BP, FBG, and TG levels in middle-aged and elderly individuals.
Table 2. Quantitative synthesis of main effects.
3.4. Sensitivity analysis
To verify the robustness of the quantitative synthesis of the main effects, a sensitivity analysis was conducted. The results of the sensitivity analysis () indicated that the 95% confidence interval, after individually excluding each study, remained in the 95% confidence interval of the quantitative synthesis of the main effects. In addition, the forest plot of the sensitivity analysis () revealed that the effect values did not significantly differ from the main effects after the removal of any individual study. Therefore, the main effect was considered robust.
Figure 4. Forest plot of the sensitivity analysis of SBP. This is a Forest plot of the sensitivity analysis of SBP. Forest plots for all indicators show that the effect values were not significantly different from the main effects after the removal of any items.
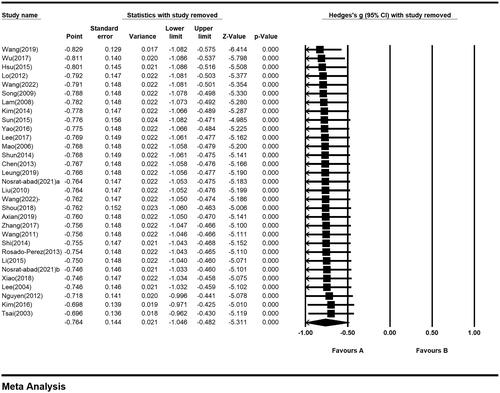
Figure 5. Forest plot of the sensitivity analysis of DBP. This is a Forest plot of the sensitivity analysis of DBP. Forest plots for all indicators show that the effect values were not significantly different from the main effects after the removal of any items.
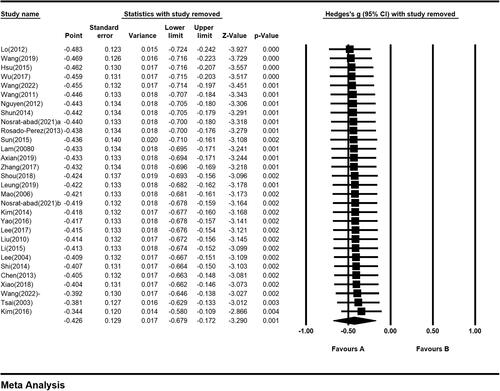
Figure 6. Forest plot of the sensitivity analysis of FBG. This is a Forest plot of the sensitivity analysis of FBG. Forest plots for all indicators show that the effect values were not significantly different from the main effects after the removal of any items.
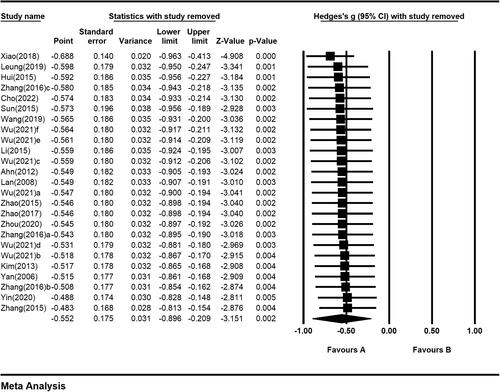
Figure 7. Forest plot of the sensitivity analysis of TG. This is a Forest plot of the sensitivity analysis of TG. Forest plots for all indicators show that the effect values were not significantly different from the main effects after the removal of any items.
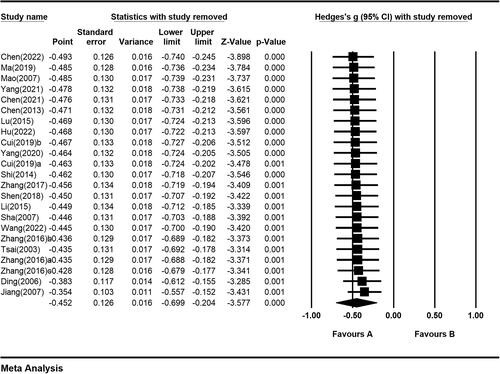
Table 3. Results of the sensitivity analysis.
3.5. Publication bias test
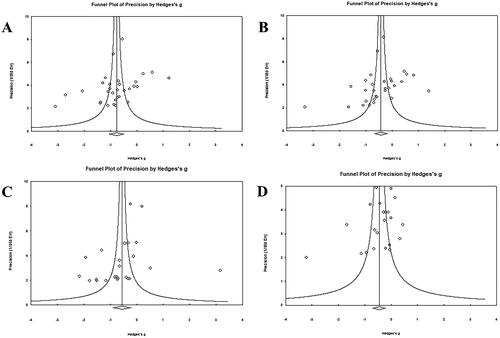
The funnel plot () demonstrated good symmetry for all indicators. Egger’s test revealed no significant publication bias (p > .05) in the data pertaining to SBP (p = .067), DBP (p = .097), FBG (p = .147), and TG (p = .090).
3.6. Subgroup analysis
To explore the optimal intervention protocol, Moderator variables were set including gender, whether the is indicators abnormal, intervention period, frequency, single duration, and Tai Chi style. Since each subgroup should contain at least three studies to ensure the representativeness [Citation80], all indicators of the subgroups were rearranged including intervention cycle, weekly frequency, and single duration. In detail, the intervention cycle was rearranged to three subgroups: 4–8 weeks, 9–16 weeks, and longer than 16 weeks. The weekly frequency was also divided to three subgroups: 2–3 times, 4–5 times, and 6–7 times, while the single duration was grouped to 30–50 min and longer than 60 min. Subgroup analysis couldn’t be performed if there are less than three subgroup studies.
3.6.1. Subgroup analysis of SBP
showed the subgroup analysis of SBP. In prospect of gender, Tai Chi intervention had the best effect on SBP in middle-aged and elderly men (ES = −0.87, p < .001), followed by the studies with no gender distinction (ES = −0.76, p < .001). While the intervention effect of Tai Chi on SBP in women has no statistical significance (p = .07). In the prospect of whether SBP was abnormal, the intervention effect of Tai Chi was more significant in the middle-aged and the elderly with abnormal SBP (ES = −0.84, p < .001) than people with normal SBP (ES = −0.49, p < .001). In the prospect of intervention cycle, the best intervention effect was observed in groups longer than 16 weeks (ES = −0.78, p = .002), followed by 9–16 weeks (ES = −0.76, p < .001), and finally 4-8 weeks (ES = −0.72, p < .001). In the prospect of weekly frequency, the best effect showed in groups of 6–7 times per week (ES = −0.90, p < .001), followed by 2–3 times per week (ES = −0.78, p < .001), and finally 4–5 times per week (ES = −0.68, p = .014). As for the single duration, the intervention effect was better in groups of 30–50 min each time (ES = −1.38, p < .001) than in the groups of 60–120 min each time (ES = −0.49, p = .002). While the intervention effect of conventional Tai Chi (ES = −0.88, p = .018) was better than that Yang-style Tai Chi (ES = −0.73, p < .001).
Table 4. Subgroup analysis of SBP.
3.6.2. Results of DBP subgroup analysis
showed the subgroup analysis of DBP. In prospect of gender, Tai Chi intervention had the best effect on DBP in middle-aged and elderly men (ES = −0.71, p < .001), followed by the studies with no gender distinction (ES = −0.33, p = .019). While the intervention effect of Tai Chi showed no statistical significance on DBP in women (p = .29). In prospect of whether the indicators is abnormal Tai Chi had a significant intervention effect for the middle-aged and the elderly with abnormal DBP (ES = −0.48, p = .002), while no significant intervention effect showed in the population with normal DBP (p = .308). In the prospect of intervention cycle, the best intervention effect was observed in groups more than 16 weeks (ES = −0.52, p = .021), followed by 9–16 weeks (ES = −0.44, p = .038), while no significant effect showed in groups of 4–8 weeks (p = .311). In prospect of intervention effect of weekly frequency, 4–5 times per week was the best (ES = −0.63, p = .015), followed by 6–7 times per week (ES = −0.51, p < .001), and no statistically significance showed in groups of 2–3 times per week (p = .133). In prospect of single duration, Tai Chi for 30–50 min each time had a significant intervention effect on DBP (ES = 1.01, p < .001), while 60–120 min group have no significance (p = .282). In prospect of style, Yang-style Tai Chi had a significant intervention effect on DBP (ES = −0.50, p = .001), and conventional Tai Chi showed no significant effect (p = .435).
Table 5. DBP subgroup analysis.
3.6.3. Results of FBG subgroup analysis
showed the subgroup analysis of FBG. In prospect of gender, men showed a slightly better intervention effect of Tai Chi on FBG (ES = −0.61, p < .001) than women (ES = −0.60, p = .031), while studies with no gender distinction showed no statically significance (p = .074). In prospect of whether the indicators is abnormal, Tai Chi showed a significant intervention effect on FBG in the middle-aged and the elderly with abnormal FBG (ES = −0.77, p < .001), while in patients with normal FBG, it showed no significant effect (p = .577). In the prospect of the intervention cycle, the groups of more than 16 weeks have a significant effect on FBG (ES = −0.55, p = .008) with no statistically significant effect for 9–16 weeks (p = .051). In the prospect of weekly frequency, the best intervention effect showed in groups of 6–7 times per week (ES = −0.99, p = .019), followed by 2–3 times per week (ES = −0.29, p = .021), and 4–5 times per week was not significant (p = .068). The Tai Chi intervention of 60–120 min each time had a significant effect on reducing FBG (ES = −0.60, p < .001), while 30–50 min each time had no significant effect (p = .309). In prospect of style, The Chen-style intervention effect on FBG (ES = −0.99, p = .013) was better than the effect of conventional Tai Chi (ES = −0.85, p = .019), while Yang-style Tai Chi have no significant effect on reducing FBG (p = .152).
Table 6. FBG subgroup analysis.
3.6.4. Results of TG subgroup analysis
presented the subgroup analysis of TG. The impact of the intervention was found to be statistically significant in studies that did not differentiate by gender (ES = −0.57, p < .001). Notably, among middle-aged and elderly individuals with abnormal TG levels, Tai Chi exhibited a significant intervention effect (ES = −0.57, p < .001), whereas no significant effect was observed in those with normal TG levels (p = .404). Regarding the duration of the intervention, a cycle longer than 16 weeks demonstrated a significant effect in reducing TG (ES = −0.71, p = .002), while the 9–16 weeks cycle did not yield a significant effect (p = .053). As for weekly frequency, the most optimal effect was observed in groups practicing Tai Chi 6–7 times per week (ES = −0.65, p = .027), followed by 4–5 times per week (ES = −0.57, p = .017), whereas the effect of practicing 2–3 times per week was not statistically significant (p = .158). The data pertaining to the duration of each session indicated that Tai Chi interventions lasting 30–50 min significantly reduced TG (ES = −0.88, p < .001), whereas sessions lasting 60–120 min did not yield a significant effect (p = .052). In addition, interventions employing the Yang-style Tai Chi also significantly reduced TG (ES = −0.46, p = .001).
Table 7. TG subgroup analysis.
3.7. Moderator effect
Factors including single duration, style and whether FBG is normal were found to have significant effects (p < .05). Single duration could modulate SBP, DBP, and TG significantly (p < .05) in the middle-aged and the elderly. Also, different Tai Chi style could affect the intervention effect of Tai Chi on DBP (p < .05). The condition of FBG, normal or abnormal, could also affect the intervention effect of Tai Chi on FBG in the middle-aged and the elderly (p < .05). The moderating effects of other variables in each indicators were not significant.
4. Discussion
The primary objective of this meta-analysis is to quantify the effects of Tai Chi interventions on BP, FBG, and TG in middle-aged and elderly individuals and to explore optimal intervention methods through subgroup analyses. The main results indicate that Tai Chi significantly reduces BP, FBG, and TG levels for this demographic. Moreover, this research provides preliminary insights into intervention strategies that maximize benefits, both for individual indicators and when considering all indicators collectively.
4.1. Main effects
The findings of the study exhibit that Tai Chi exerts a significant intervention effect on BP, FBG, and TG in the middle-aged and elderly population, which is consistent with previous meta-analyses [Citation34,Citation35,Citation81–85]. Similar results have also been reported in meta-analyses assessing the effects of fitness qigong on BP, FBG, and TG [Citation86–88]. All of the aforementioned studies, whether directly or indirectly, lend credence to the findings of this research to a certain degree. It is important to highlight that while both Tai Chi and fitness qigong exude the “slow-paced” trait, Tai Chi necessitates diverse stepping maneuvers, in contrast to fitness qigong which predominantly revolves around monotonous cyclic movements devoid of any stepping transitions. A study has demonstrated that both Tai Chi and fitness qigong epitomize the “gentle and slow” paradigm, yet the complexity inherent in Tai Chi surpasses that of fitness qigong [Citation89]. Another study showed that in general, the intensity of Taijiquan is higher than that of Fitness Qigong [Citation90]. Therefore, in future Tai Chi intervention studies, carefully consideration is necessary to appreciate the nuances differentiating Tai Chi and fitness qigong, precluding any potential conflation of the two modalities.
4.2. Subgroup analysis
Firstly, in the prospect of gender, it was observed that the effects of Tai Chi intervention on SBP, DBP, and FBG were more pronounced in males compared to females. However, the effects on TG were not discussed due to the limited number of TG gender subgroups, which fell below the threshold of three. Interestingly, previous investigations have indicated that females exhibit superior long-term performance in general aerobic exercise [Citation91]. This phenomenon may be attributed to the fact that middle-aged and elderly women are in the postmenopausal stage, during which estrogen production decreases, leading to lower exercise efficacy. Notably, a study has demonstrated that males practicing Tai Chi achieve greater reductions in blood lipids compared to their female counterparts [Citation92]. Secondly, this study revealed that individuals with abnormal FBG levels experienced significantly more positive intervention effects in the middle-aged and elderly population, as opposed to those with normal FBG values. These findings align with a taekwondo intervention study [Citation39]. Other studies have also reported enhanced exercise effects in individuals with normal indicators [Citation93]. However, the study conducted by Kodama et al. did not incorporate the exercise cycle, thus accounting for the divergent results. In conclusion, this study suggests that Tai Chi is an optimal intervention for hypertensive, hyperglycemic, and hyperlipidemic males, as it maximizes the intervention benefits.
Regarding intervention approaches, firstly, concerning the “intervention period,” this study demonstrates that the most significant effects across all indicators are noted when the intervention spans over 16 weeks. Prior research has posited that Tai Chi practices extending beyond 12 weeks might be more beneficial in decreasing BP and TG [Citation31,Citation85]. Moreover, a study into intermittent exercise interventions reveals no significant changes in TG post 6 weeks of intervention; however, following 12 weeks, there is a significant reduction in TG [Citation94]. Such insights suggest that for the mitigation of cardiovascular risk elements, an intervention period exceeding 12 weeks might be apt. Considering the scarcity of available research and data, a more detailed subgroup analysis for intervention durations between 12 and 16 weeks remains elusive. Subsequent studies are necessary to delve deeper into the advantages of intervention spans in this bracket. Drawing from the extant data analysis, this study advocates for an intervention timeframe of 16 weeks or longer, corroborated by earlier research underscoring the necessity for sustained and consistent aerobic exercise interventions to effectively reduce cardiovascular risk determinants [Citation95–97].
Secondly, with respect to “weekly frequency,” the research indicates that, barring DBP, the most favorable effects for other indicators in Tai Chi interventions are achieved with a frequency of 6–7 times weekly. Pertaining to “individual session duration,” the research posits that, excluding FBG, the most efficacious results for other indicators within Tai Chi interventions are realized with a span of 30–50 min per engagement. Therefore, to concurrently enhance SBP, DBP, FBG, and TG indicators, it is advocated to calibrate the frequency to 6–7 instances weekly and the session length to 30–50 min. Such guidelines resonate with the regimen promulgated by the American College of Sports Medicine [Citation98]. In addition, the European Association of Preventive Cardiology promulgated a proclamation, endorsing an aerobic regimen frequency of 6–7 days weekly and a tenure of 45–60 min per engagement to ensure optimal effects on an array of cardiovascular maladies [Citation99]. These recommendations are aligned with the findings of this study. Moreover, a previous study determined that extending the session duration surpassing the benchmarks set by the American College of Sports Medicine is necessary to markedly mitigate cardiovascular peril factors [Citation94]. Such previous findings corroborate the robustness and credibility of the conclusions drawn in this study.
Lastly, pertaining to “style,” this study reveals that conventional Tai Chi exhibits the most pronounced intervention effect on SBP, while Yang-style Tai Chi excels in its intervention effect on DBP, and Chen-style Tai Chi yields the most significant intervention effect on FBG. In the context of TG, both the Chen-style Tai Chi and conventional Tai Chi subgroups are represented by fewer than three studies, rendering them beyond the scope of this discussion. In weighing the cumulative advantages across all indicators, one might infer that any Tai Chi style is a viable choice. Such findings might be attributable to the inherent variations in movement intricacies among the various Tai Chi styles. Specifically, Yang-style Tai Chi and conventional Tai Chi are characterized by their “gentle” and “smooth” motions, whereas Chen-style Tai Chi integrates “rigidity and flexibility,” incorporating a plethora of kicking and leaping actions, thereby positing a marginally higher level of complexity in contrast to the Yang-style and conventional Tai Chi. Nonetheless, it necessitates additional studies to determine whether these variances can influence the intervention effects on SBP, DBP, FBG, and TG.
In light of the aforementioned considerations, for the optimal enhancement of all indicators, this research advocates for a Tai Chi intervention period of no less than 16 weeks, a per-week frequency of 6–7 sessions, each session spanning 30–50 min, with no specific constraints on the Tai Chi style employed.
4.3. Limitations of the study
(1) This study solely focused on the intervention effects of Tai Chi on BP, FBG, and TG in the middle-aged and elderly population, thereby limiting its generalizability to other age groups. (2) The subgroup analysis included certain invalid subgroups due to an insufficient number of studies (less than three). (3) To facilitate the subgroup analysis, the original data were reorganized, such as grouping studies with intervention periods of 4, 6, and 8 weeks into a subgroup of 4-8 weeks, potentially introducing imprecision in the final result. (4) The available data were inadequate to conduct a meta-analysis on “multiple follow-up time points,” thereby reducing the precision of the explored intervention plans.
5. Conclusions
This study suggests that Tai Chi exhibits efficacy in the reduction of SBP, DBP, FBG, and TG among middle-aged and elderly individuals, particularly demonstrating enhanced results in those with abnormal biomarkers. To optimize the efficacy across all indicators, we recommend an intervention duration exceeding 16 weeks, with a weekly frequency of 6–7 sessions and a duration of 30–50 min per session, irrespective of the Tai Chi style employed. In addition, when focusing solely on SBP reduction, the intervention protocol should involve a duration exceeding 16 weeks, a weekly frequency of 6–7 sessions, and a duration of 30–50 min per session, employing the conventional Tai Chi style. For DBP reduction, the intervention protocol should involve a duration exceeding 16 weeks, a weekly frequency of 4–5 sessions, and a duration of 30–50 min per session, utilizing the Yang style of Tai Chi. Similarly, for FBG reduction, the intervention protocol should comprise a duration exceeding 16 weeks, a weekly frequency of 6–7 sessions, and a duration of 30–50 min per session, employing the Yang style of Tai Chi. Finally, for TG reduction, the intervention protocol should involve a duration exceeding 16 weeks, a weekly frequency of 6–7 sessions, and a duration of 30–50 min per session, regardless of the Tai Chi style employed. Considering the limitations in this study, it is necessary that future research devises well-designed RCTs to further enhance the quality of such studies.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
We are happy to provide raw data: https://www.dropbox.com/scl/fi/ud4ieq71bvelf8b987jl3/DATA.xls?dl=0&rlkey=p7vgdnugiv2km1e671t12prjd
Additional information
Funding
References
- Yang H, Fu Y, Hong X, et al. Trend in premature mortality from four major NCDs in Nanjing, China, 2007–2018. BMC Public Health. 2021;21(1):2163. doi: 10.1186/s12889-021-12018-7.
- Owolade A, Mashavakure H, Babatunde AO, et al. Time to relook into non-communicable diseases (NCDs) in Africa: a silent threat overwhelming global health in Africa. Ann Med Surg. 2022;82:104522. doi: 10.1016/j.amsu.2022.104522.
- World Health Organization. Noncommunicable diseases. 2023 [cited 2023 April 5]. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- World Health Organization. Hypertension. 2023 [cited 2023 April 5]. https://www.who.int/news-room/fact-sheets/detail/hypertension
- Taddei C, Zhou B, Bixby H, et al. Repositioning of the global epicentre of non-optimal cholesterol. Nature. 2020;582(7810):73–77. doi: 10.1038/s41586-020-2338-1.
- Wang C, Collet JP, Lau J. The effect of tai chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501. doi: 10.1001/archinte.164.5.493.
- Yeh G, Wang C, Wayne P, et al. Tai chi exercise for patients with cardiovascular conditions and risk factors a systematic review. J Cardiopulm Rehabil Prev. 2009;29(3):152–160. doi: 10.1097/HCR.0b013e3181a33379.
- Luskin F, Newell K, Griffith M, et al. A review of mind-body therapies in the treatment of cardiovascular disease part 1: implications for the elderly. Altern Ther Health Med. 1998;4:46.
- Taylor-Piliae RE. Tai Chi as an adjunct to cardiac rehabilitation exercise training. J Cardiopulm Rehabil. 2003;23(2):90–96. doi: 10.1097/00008483-200303000-00004.
- Wong SS, Nahin RL. National center for complementary and alternative medicine perspectives for complementary and alternative medicine research in cardiovascular diseases. Cardiol Rev. 2003;11(2):94–98. doi: 10.1097/01.CRD.0000053452.60754.C5.
- Lee E-N. The effects of tai chi exercise program on blood pressure, total cholesterol and cortisol level in patients with essential hypertension. Taehan Kanho Hakhoe Chi. 2004;34(5):829–837. doi: 10.4040/jkan.2004.34.5.829.
- Li H, Qiu Y, Tie Y. Effects of Chen-style Taijiquan on blood biochemical indices and cardiopulmonary function in elderly patients with type 2 diabetes mellitus. Chin J Gerontol. 2015;35:1293–1294. doi: 10.3969/j.issn.1005-9202.2015.05.067.
- Nguyen M, Kruse A. A randomized controlled trial of tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging. 2012;7:185–190. doi: 10.2147/CIA.S32600.
- Nosrat-Abad T, Bayrami M, Namdar H, et al. Effects of tai chi on cardiovascular responses and stress reduction in prehypertensive subjects: a randomized clinical trial. EJHM. 2021;46:85–94. doi: 10.21134/eurjhm.2021.46.3.
- Shun F, Shun C. Effect of tai chi exercise on the intervention of hypertension in the elderly. Chin J Gerontol. 2014;34:6862–6864. doi: 10.3969/j.issn.1005-9202.2014.24.005.
- Wu A. A comparative study of the effects of tai chi and square dance fitness exercises on physical functions of middle-aged and elderly people. Shaanxi: Shaanxi Normal University; 2017.
- Wu J. Effects on body composition, fitness levels and blood composition of type II diabetes patients according to different time of tai chi exercise. Wanju: Woosuk University; 2021.
- Yan W, Zhang J. Effect of tai chi exercise on blood glucose and blood lipids in hyperglycemic patients. Acta Acad Med Jiangxi. 2006;46:194–195. doi: 10.3969/j.issn.1000-2294.2006.04.072.
- Yin N. The effects of health qigong and tai chi on biochemistry and psychology of elderly patients with type 2 diabetes. Zhengzhou: Zhengzhou University; 2020.
- Hui Z. Analysis of the effect of taijiquan practice on blood glucose in type 2 diabetic patients. Contemp Med Forum. 2015;13:4–5.
- Zhang X. Provide shelf taijiquan exercise influence on the effect of adjuvant therapy in patients with type 2 diabetes. Liaoning: Liaoning Normal University, 2016.
- Ding Z, Yang T. Effect of tai chi exercise on lipid and lipoprotein metabolism in patients with hyperlipidemia. Chin J Tissue Eng Res. 2006;10:172–173. doi: 10.3321/j.issn:1673-8225.2006.47.073.
- Jiang R. The influence of taijiquan on the mellitus II patients’ lipid constituents and Insulin-Resistance. Wushu Studies. 2007;10:35–36. doi: 10.3969/j.issn.1004-5643.2007.10.015.
- Chen T. Study on the mechanism of 16 week taijiquan exercise on atherosclerosis in middle-aged and elderly people. Yangzhou: Yangzhou University; 2022.
- Leung L, Chan A, Sit J, et al. Tai chi in Chinese adults with metabolic syndrome: a pilot randomized controlled trial. Complement Ther Med. 2019;46:54–61. doi: 10.1016/j.ctim.2019.07.008.
- Liu C, Wong S, Leung F, et al. Prostanoid TP receptor-mediated impairment of cyclic AMP-dependent vasorelaxation is reversed by phosphodiesterase inhibitors. Eur J Pharmacol. 2010;632(1–3):45–51. doi: 10.1016/j.ejphar.2010.01.008.
- Ma Y, Wu C, Peng C, et al. Complexity-based measures of heart rate dynamics in older adults following long- and short-term Tai Chi training: cross-sectional and randomized trial studies. Sci Rep. 2019;9(1):7500. doi: 10.1038/s41598-019-43602-y.
- Xiao Y. Effects of eight styles of Taijiquan exercise on blood pressure level, vascular endothelial function and quality of life in patients with essential hypertension. Chin J Gerontol. 2018;38:2403–2405. doi: 10.3969/j.issn.1005-9202.2018.10.041.
- Zhang D. A clinical study: effect of 24 movement form of Tai chi on senile patients with essential hypertension. Chengdu: Chengdu University of Traditional Chinese Medicine; 2017.
- Zhu Z, Yan W, Yu Q, et al. Association between exercise and blood pressure in hypertensive residents: a Meta-Analysis. Evid Based Complement Alternat Med. 2022;2022:2453805. doi: 10.1155/2022/2453805.
- Guan Y, Hao Y, Guan Y, et al. Effects of tai chi on essential hypertension and related risk factors: a meta-analysis of randomized controlled trials. J Rehabil Med. 2020;52(5):jrm00057. doi: 10.2340/16501977-2683.
- Chao M, Wang C, Dong X, et al. The effects of tai chi on type 2 diabetes mellitus: a meta-analysis. J Diabetes Res. 2018;2018:7350567–7350569. doi: 10.1155/2018/7350567.
- Song G, Chen C, Zhang J, et al. Association of traditional Chinese exercises with glycemic responses in people with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Sport Health Sci. 2018;7(4):442–452. doi: 10.1016/j.jshs.2018.08.004.
- Wang Y, Yan J, Zhang P, et al. Tai chi program to improve glucose control and quality of life for the elderly with type 2 diabetes: a meta-analysis. Inquiry. 2022;59:469580211067934. doi: 10.1177/00469580211067934.
- Xia T, Yang Y, Li W, et al. Different training durations and styles of tai chi for glucose control in patients with type 2 diabetes: a systematic review and meta-analysis of controlled trials. BMC Complement Altern Med. 2019;19(1):63. doi: 10.1186/s12906-019-2475-y.
- Borenstein M, Cooper H, Hedges L, et al. Effect sizes for continuous data. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta-analysis. 2nd ed. New York: Russell Sage Foundation; 2009; p. 221–235.
- Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1(3):98–101. doi: 10.1111/1467-8721.ep10768783.
- Higgins J, Thompson S, Deeks J, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557.
- Han Z, Ju H. Meta-analysis of the intervention effects of taekwondo on metabolic syndrome indicators. Front Physiol. 2023;14:1069424. doi: 10.3389/fphys.2023.1069424.
- Axian W, Zhang L, Li Y, et al. Effect of taijiquan exercise on blood pressure and heart rate of hemodialysis patients. 2019;20:776–780. doi: 10.3969/j.issn.1009-587X.2019.09.008.
- Hsu W, Hsu R, Lin Z, et al. Effects of circuit exercise and tai chi on body composition in middle-aged and older women. Geriatr Gerontol Int. 2015;15(3):282–288. doi: 10.1111/ggi.12270.
- Hu J. Study on the curative effect of taijiquan on hypertension and TCM mechanism. Sichuan Sports Science. 2022;5:49–52 + 78. doi: 10.13932/j.cnki.sctykx.2022.05.11.
- Hu Q, Qian Y, Liu X, et al. Effects of 12-week tai chi exercise on the microvascular reactivity of the Middle-aged and elderly patients with mild hypertension and its mechanism. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2021;37(6):683–687. doi: 10.12047/j.cjap.6164.2021.080.
- Hui S, Xie Y, Woo J, et al. Effects of tai chi and walking exercises on weight loss, metabolic syndrome parameters, and bone mineral density: a cluster randomized controlled trial. Evid Based Complement Alternat Med. 2015;2015:976123–976110. doi: 10.1155/2015/976123.
- Kim J-H. The effect of tai chi chuan training on the automatic cardiac nerve activity and blood pressure in elderly women with hypertension. Off J Koeran Soc Dance Sci. 2014;31:157–168. doi: 10.21539/ksds.2014.31.1.157.
- Kim S, Kim W, Kim H. Cheol the long-term effect of tai chi exercise on blood pressure, heart rate, and lipid profile in older women with hypertension. Korean J Adapt Phys Act. 2016;24:35–46. doi: 10.17006/kjapa.2016.24.4.35.
- Lam P, Dennis S, Diamond T, et al. Improving glycaemic and BP control in type 2 diabetes the effectiveness of tai chi. Aust Fam Physician. 2008;37(10):884–887.
- Lee YM. The effects of tai chi on waist circumference and blood pressure in the elderly. J Phys Ther Sci. 2017;29(1):172–175. doi: 10.1589/jpts.29.172.
- Liu X, Jin H. Observation on effect of tai chi chuan on cardiopulmonary function of older people. China Practical Medical. 2010;5:34–35. doi: 10.3969/j.issn.1673-7555.2010.02.016.
- Lo H, Yeh C, Chang S, et al. A tai chi exercise programme improved exercise behaviour and reduced blood pressure in outpatients with hypertension. Int J Nurs Pract. 2012;18(6):545–551. doi: 10.1111/ijn.12006.
- Mao H, Sha P. Effect of tai chi exercise on blood pressure, plasma nitrogen monoxidum and endothelin in hypertensive patients. Chin J Tissue Eng Res. 2006;10:65–67. doi: 10.3321/j.issn:1673-8225.2006.48.025.
- Nguyen MH, Kruse A. The effects of tai chi training on physical fitness, perceived health, and blood pressure in elderly Vietnamese. Open Access J Sports Med. 2012;3:7–16. doi: 10.2147/OAJSM.S27329.
- Rosado-Perez J, Ortiz R, Santiago-Osorio E, et al. Effect of tai chi versus walking on oxidative stress in Mexican older adults. Oxid Med Cell Longev. 2013;2013:298590–298598. doi: 10.1155/2013/298590.
- Shi Z, Wen H, Liu F, et al. The effects of tai chi on the renal and cardiac functions of patients with chronic kidney and cardiovascular diseases. J Phys Ther Sci. 2014;26(11):1733–1736. doi: 10.1589/jpts.26.1733.
- Shou X, Wang L, Zhu L, et al. Effect of Tai Chi chuan on emotion and heart rate variability of in-service hypertension patients. China Modern Doctor. 2018;56:95–99.
- Song R, Ahn S, So H, et al. Effects of Tai Chi exercise on cardiovascular risk factors and quality of life in post-menopausal women. J Korean Acad Nurs. 2009;39(1):136–144. doi: 10.4040/jkan.2009.39.1.136.
- Sun J, Buys N. Community-based mind-body meditative tai chi program and its effects on improvement of blood pressure, weight, renal function, serum lipoprotein, and quality of life in Chinese adults with hypertension. Am J Cardiol. 2015;116(7):1076–1081. doi: 10.1016/j.amjcard.2015.07.012.
- Tsai J, Wang W, Chan P, et al. The beneficial effects of Tai Chi chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9(5):747–754. doi: 10.1089/107555303322524599.
- Wang S, Tian L, Ma T, et al. Effectiveness of tai chi on blood pressure, stress, fatigue, and sleep quality among Chinese women with episodic migraine: a randomised controlled trial. Evid Based Complement Alternat Med. 2022;2022:2089139–2089110. doi: 10.1155/2022/2089139.
- Wang X, Li Y, Liu N. Empirical study of taijiquan interventions on the prevention and cure of hypertension. J Beijing Sport Univ. 2011;34:75–77. doi: 10.19582/j.cnki.11-3785/g8.2011.09.020.
- Wang Y, Guo X, Liu L, et al. Effects of Tai-Chi and running exercises on cardiorespiratory fitness and biomarkers in sedentary middle-aged males: a 24-week supervised training study. Biology. 2022;11(3):375 doi: 10.3390/biology11030375.
- Yao X, Luo L, Hong B, et al. Effect of taijiquan exercise on exercise mood and bone mineral density and physiological indexes of elderly male patients with osteoporosis. J Guizhou Normal Univ. 2016;34:32–36. doi: 10.3969/j.issn.1004-5570.2016.03.006.
- Ahn S, Song R. Effects of Tai Chi exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. J Altern Complement Med. 2012;18(12):1172–1178. doi: 10.1089/acm.2011.0690.
- Cho B-J, Kim S-R. Effects of Tai Chi on cardiovascular disease risk factors among the korean elderly. J Korea Soc Comput Inf. 2022;27:195–202.
- Kim Y-J. The effects of tai chi training on metabolic syndr ome risk factors in middle aged obese women. Ulsan: UlsanUniversity; 2013.
- Lan C, Su T-C, Chen S-Y, et al. Effect of Tai Chi chuan training on cardiovascular risk factors in dyslipidemic patients. J Altern Complement Med. 2008;14(7):813–819. doi: 10.1089/acm.2008.0143.
- Wang X, Ye L. The effect of 24 simplified taijiquan on primary hypertension with mild anxiety state in the elderly. Fujian J TCM. 2019;50:73–75.
- Zhao G. Effects of taijiquan on the physique, blood lipid, insulin resistance and HbA1c of patients with type 2 diabetes. Changwon: Changwon National University; 2015.
- Zhao G, Chen M, Zhuang L, et al. Effects of tijiquan on the physique, blood lipid, insulin resistance of patients with type 2 diabetes. J Nanjing Sport Institute. 2017;16:1–7.
- Zhou L. Effect of Tai Chi on the treatment effect and physical fitness of overweight type 2 diabetic patients index. New World Diabetes. 2020;23(2):1–2. doi: 10.16658/j.cnki.1672-4062.2020.02.001.
- Chen J. Effect of tai chi exercise on blood lipids in elderly patients with coronary heart disease. Guide Chin Med. 2013;11:583–584. doi: 10.15912/j.cnki.gocm.2013.02.271.
- Chen Y. Effects of tai chi exercise on cancer-related fatigue, body composition and blood lipid of breast cancer patients after chemotherapy. Wuhan: Wuhan Sports University; 2021.
- Cui Y, Niu A. Effect of 24-week tai chi exercise on AIP, ABI and PWV in the Middle-aged and elderly. J Huzhou Teachers College. 2019;41:94–99. doi: 10.3969/j.issn.1009-1734.2019.08.018.
- Ma C, Hong Y, Shi C, et al. Effects of practicing tai chi on cardiac function and 6-minute walk distance in community patients with coronary heart disease. Chin J Sports Med. 2020;39:26–32. doi: 10.3969/j.issn.1000-6710.2020.01.004.
- Mao Y, Ma L, Lv Y, et al. The influences of taijiquan and comprehensive exercises on blood lipid metabolism of senile women. Chin J Woman Child Health Res. 2007;18:374–376. doi: 10.3969/j.issn.1673-5293.2007.05.008.
- Sha P. Effect of taijiquan exercise on the nitrogen monoxidum and blood lipid of elder patients with atherosclerosis. Chin J Tissue Eng Res. 2007;11:6832–6834. doi: 10.3321/j.issn:1673-8225.2007.34.051.
- Shen S. Study on the intervention effect and mechanism of tai chi exercise on patients with abnormal arterial stiffness. Yangzhou: Yangzhou University; 2018.
- Yang H, Yu D, Zhou S, et al. Influence of tai chi rehabilitation exercise on cardiac function and blood lipid levels in aged CHF patients. Chin J Cardiovasc Rehabil Med. 2021;30:382–387. doi: 10.3969/j.issn.1008-0074.2021.04.03.
- Yang L. Effects of tai chi exercise on cardiovascular function of serving police. J Harbin Inst Phys Educ. 2020;38:92–96. doi: 10.3969/j.issn.1008-2808.2020.02.014.
- Song H, Zmyslinski-Seelig A, Kim J, et al. Does facebook make you lonely?: A meta analysis. Comput Hum Behav. 2014;36:446–452. doi: 10.1016/j.chb.2014.04.011.
- Liu Y, Wang L, Fan X, et al. A meta-analysis of the effects of tai chi on glucose and lipid metabolism in middle-aged and elderly diabetic patients: evidence from randomized controlled trials. evidence. Evid Based Complement Alternat Med. 2021;2021:6699935. doi: 10.1155/2021/6699935.
- Pan X, Mahemuti A, Zhang X, et al. Effect of tai chi exercise on blood lipid profiles: a meta-analysis of randomized controlled trials. J Zhejiang Univ Sci B. 2016;17(8):640–648. doi: 10.1631/jzus.B1600052.
- Wu Y, Johnson B, Chen S, et al. Tai Ji Quan as antihypertensive lifestyle therapy: a systematic review and Meta-Analysis. J Sport Health Sci. 2021;10(2):211–221. doi: 10.1016/j.jshs.2020.03.007.
- Xia T, Yang Y, Li W, et al. Meditative movements for patients with type 2 diabetes: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2020;2020:5745013–5745012. doi: 10.1155/2020/5745013.
- Yin Y, Yu Z, Wang J, et al. Effects of the different tai chi exercise cycles on patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. 2023;10:1016629. doi: 10.3389/fcvm.2023.1016629.
- Lin H, Wan M, Ye Y, et al. Effects of Baduanjin exercise on the physical function of middle-aged and elderly people: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Med Ther. 2023;23(1):38. doi: 10.1186/s12906-023-03866-4.
- Lin J, Gao Y, Guo Y, et al. Effects of qigong exercise on the physical and mental health of college students: a systematic review and meta-analysis. BMC Complement Med Ther. 2022;22(1):287. doi: 10.1186/s12906-022-03760-5.
- Zou L, Zhang Y, Sasaki JE, et al. Wuqinxi qigong as an alternative exercise for improving risk factors associated with metabolic syndrome: a Meta-Analysis of randomized controlled trials. Int J Environ Res Public Health. 2019;16(8):1396. doi: 10.3390/ijerph16081396.
- Yang T. A comparative study of the effects of 24-step taijiquan and fitness qigong-Mawangdui guiding technique on the intervention of type 2 diabetes mellitus patients’ conditions. Liaoning: Liaoning Normal University; 2023.
- Wang M. A comparative study of the intensity and energy consumption of four typical taijiquan and fitness qigong routines. Hebei: Hebei Normal University; 2019.
- Al Kubaisy W, Mohamad M, Ismail Z, et al. Gender differences: motivations for performing physical exercise among adults in Shah Alam. Procedia Soc Behav Sci. 2015;202:522–530. doi: 10.1016/j.sbspro.2015.08.181.
- Zhang J, Lv S, Wang J, et al. Modulation by tai chi boxing of the therapeutic effect in patients with type 2 diabetes mellitus Sout-gender difference. J Beijing Normal Univ. 2019;55:545–550. doi: 10.16360/j.cnki.jbnuns.2019.04.017.
- Kodama S, Tanaka S, Saito K, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol – a meta-analysis. Arch Intern Med. 2007;167(10):999–1008. doi: 10.1001/archinte.167.10.999.
- Alkahtani S. Comparing fat oxidation in an exercise test with moderate-intensity interval training. J Sports Sci Med. 2014;13:51–58. doi: 10.1177/1754337113493083.
- Dustman R, Ruhling R, Russell E, et al. Aerobic exercise training and improved neuropsychological function of older individuals. Neurobiol Aging. 1984;5(1):35–42. doi: 10.1016/0197-4580(84)90083-6.
- Hagberg JM, Graves JE, Limacher M, et al. Cardiovascular responses of 70- to 79-yr-old men and women to exercise training. J Appl Physiol (1985). 1989;66(6):2589–2594. doi: 10.1152/jappl.1989.66.6.2589.
- Ma J. Effects of aerobic exercise on body morphology in obese university students. Revista Brasileira de Medicina Do Esporte. 2022;29 doi: 10.1590/1517-8692202329012022_0221.
- Pate R, Pratt M, Blair S, et al. Physical activity and public health: a recommendation from the centers for disease control and prevention and the American college of sports medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402.
- Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2021;28(5):460–495.