Abstract
Aims: This study compared healthcare resource utilization (HRU), healthcare costs, adherence, and persistence among adult patients with schizophrenia using once-monthly (OM) vs twice-monthly (TM) atypical long-acting injectable (LAI) antipsychotic (AP) therapy.
Materials and methods: A longitudinal retrospective cohort study was conducted using Medicaid claims data from six states. Patients initiated on aripiprazole or paliperidone palmitate were assigned to the OM cohort; risperidone-treated patients were assigned to the TM cohort. HRU and healthcare costs were assessed during the first 12 months following stabilization on the medication. Adherence was measured using the proportion of days covered (PDC) during the first year of follow-up. Persistence to the index medication was measured during the first 2 years following the index date. Comparison between the cohorts was achieved using multivariable generalized linear models, adjusting for demographic and clinical characteristics.
Results: Patients in the OM LAI cohort had lower inpatient HRU and medical costs when compared with patients in the TM cohort. Higher medical costs in the TM LAI cohort offset the higher pharmacy costs in the OM LAI cohort. Mean PDC during the first 12 months of follow-up was higher in the OM cohort than in the TM cohort (0.56 vs 0.50, p < .01). Median persistence was longer in the OM cohort than in the TM cohort (7.5 months vs 5.5 months), as was the hazard of discontinuing the index medication (hazard ratio = 0.83, p = .01). Kaplan-Meier rates of persistence at 1 year were higher for OM patients than for TM patients (37.6% vs 29.6%, p < .01).
Limitations: This was a Medicaid sample with few aripiprazole LAI patients (5.4% of OM cohort). Medication use was inferred from pharmacy claims.
Conclusions: Among Medicaid patients in these six states, OM AP treatment was associated with lower HRU, better adherence and persistence, and similar total costs compared to patients on TM treatment.
Introduction
Schizophrenia is a complex psychiatric disorder that is commonly manifested through psychosis and other neuropsychiatric problemsCitation1. Its lifetime prevalence is estimated to be 0.48%, with a higher incidence in urban settings, men, and migrant populationsCitation2–4. In 2010, it was the 16th leading cause of years lived with disability worldwide, and the 9th in high-income North AmericaCitation5. Schizophrenia leads to a considerable decrease in patients’ quality-of-life, but this can be partially alleviated through antipsychotic (AP) pharmacological treatmentCitation6. Although the mechanism of antipsychotic activity is largely unknown, typical APs are believed to work through neurotransmitter antagonism in the brain’s dopamine receptorsCitation7,Citation8.
The prevention of relapses is the primary goal of AP treatmentCitation9,Citation10. However, the definition of what constitutes a “relapse” is not consistent in the literatureCitation11. A recent systematic literature review examined 87 manuscripts with definitions of “relapse” in patients with schizophrenia, and found that 54% of these definitions included the term “hospitalization”, which was also often used as a direct proxy for relapsesCitation12. Furthermore, hospitalizations are the single most important driver of costs in patients with schizophreniaCitation13,Citation14.
Long-term, sustained AP treatment of schizophrenia is critical to treatment successCitation15. Nevertheless, non-adherence to AP treatment is a major issue in the treatment of patients with schizophrenia, and is associated with more relapses (i.e. more hospitalizations) and a poorer quality-of-lifeCitation16–20. One strategy to improve adherence is to opt for an AP long-acting injection rather than an oral formulation, since the injection guarantees the release of the AP over time rather than relying on a patient’s regular oral intake of the medication (i.e. injectable medications provide fewer opportunities to miss a dose)Citation21,Citation22. These long-acting injectable (LAI) APs emerged in the 1960s (i.e. “first-generation” or “typical” LAIs), and their safety and efficacy profiles are widely recognizedCitation23–25.
A new class of LAI APs called “second generation", or “atypical", is hypothesized to lead to better tolerability than typical LAI ApsCitation23,Citation26. Unlike typical APs, atypical APs act as antagonists on serotonin receptors as well as antagonists or partial agonists at dopamine receptorsCitation8. These drugs vary in their frequency of administration. Patients taking injectable risperidone, for instance, receive the drug twice a month, whereas patients taking injectable paliperidone palmitate or injectable aripiprazole receive the drug only once a monthCitation27–29.
The increase in the risk of a schizophrenia relapse precipitated by non-adherence to or discontinuation of APs is hypothesized to evolve along a gradient as the effect of the treatment declines with progressive elimination of the AP from the patient’s system, and a corresponding decline in dopamine receptor occupancy (a pharmacodynamic marker of clinical effect). Although evidence on the association between dopamine receptor occupancy with LAI APs and schizophrenia relapses is scantCitation30, the decline in dopamine receptor occupancy occurs more slowly after administration of a LAI AP compared with an oral AP intended for daily use. Similarly, declines in receptor occupancy and clinical effect are expected to occur more slowly after administration of LAIs formulated for OM use (i.e. median half-life of paliperidone palmitate ranges from 25–49 daysCitation28) compared with LAIs formulated for TM use (i.e. half-life of risperidone is 3–6 daysCitation27). This premise informed an earlier simulation study which hypothesized that APs with a lower dosing frequency may result in better adherence, persistence, and health statesCitation31. However, to the best of our knowledge, only one study has examined the relationship between the dosing frequency of atypical LAI APs and outcomes such as hospitalizations in a real-world settingCitation32. However, that study used the first drug dispensing as the index and, therefore, did not restrict the study population to patients who were stabilized on the index medication. Furthermore, the study did not include patients initiated on aripiprazoleCitation32. Therefore, we sought to compare healthcare resource utilization ([HRU] including inpatient utilization as a proxy for relapses), healthcare costs, adherence, and persistence among adult patients with schizophrenia stabilized on the most frequently-prescribed OM (i.e. paliperidone palmitate OM and aripiprazole) vs TM (i.e. risperidone) atypical LAI APs using administrative claims data.
Methods
Data source
A longitudinal retrospective cohort study was conducted. Patients were identified from Medicaid health claims databases from six states (Florida, Iowa, Kansas, Mississippi, Missouri, and New Jersey). Data were available from January 1, 2009 to March 31, 2015, except for Florida (end of data availability: June 30, 2012) and New Jersey (end of data availability: March 31, 2014) and included Medicaid/Medicare crossovers. Variables available included information on patients’ demographic characteristics (age, gender, enrollment start/end dates, and date/year of death, if applicable), medical claims (type of service, dates of service, International Classification of Diseases, 9th revision [ICD-9] diagnoses, and Current Procedural Terminology [CPT] procedure codes), and prescription drug claims (days supplied, date of dispensing, units, and National Drug Codes [NDC]).
All data collected were de-identified in compliance with the patient confidentiality requirements of the Health Insurance Portability and Accountability Act (HIPAA). Therefore, no ethics review was necessary for this study.
Study design and sample selection
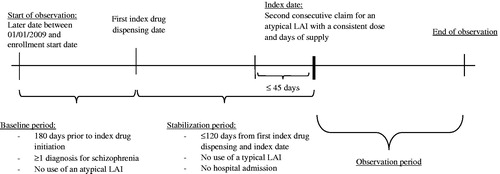
A longitudinal retrospective cohort design was used to conduct this study (). The index date was defined as the second consecutive dispensing of an atypical LAI (i.e. aripiprazole, paliperidone palmitate OM, or risperidone) within 45 days of a previous dispensing with the same dose and number of days of supply. The medication used on the index date was defined as the index medication. Patients were also required to be continuously enrolled in Medicaid for at least 6 months prior to the initiation of the index treatment (baseline period), during which at least one diagnosis of schizophrenia was recorded (ICD-9 code 295.x, not including 295.7). There was no exclusion of patients based on the length of continuous enrollment following the index date. Patients who were younger than 18 years old and those who were admitted to a long-term care facility during the baseline period, but who were discharged after having initiated their index medication, were also excluded.
The period between the first dispensing for an atypical LAI and the index date (the second consecutive dispensing at a consistent dose and days of supply) was included as a stabilization period of a maximum length of 120 days. For the minimization of bias from systematic differences between new and prevalent users of LAI, a new-user design was implemented by excluding patients who had previously used a typical LAI AP during the baseline/stabilization period or an atypical LAI AP during the baseline period. Because new users have a high potential to be changing treatment regimens subsequent to a recent relapse, patients who were admitted to an emergency department, an inpatient stay, a long-term care facility, or a mental health institute during the stabilization period were excluded. The use of a stabilization period was analogous to a flexible-dose transition phase of a clinical trial, where the intention is to restrict the study population to patients initiated on the medication for the purpose of chronic use by removing patients who discontinued or switched LAI AP shortly after being initiated on their index medication. Thereby, outcomes reflected those of a stable patient using the index medication.
Eligible patients were separated in two cohorts based on their index medications. Patients whose index medication was aripiprazole or paliperidone palmitate were assigned to the OM cohort (aripiprazole is a 400 mg monthly single intramuscular injection [no sooner than 26 days after the previous injection]Citation29, and paliperidone palmitate [OM] is a monthly intramuscular injection that ranges between 39–234 mgCitation28). Patients whose index medication was risperidone were assigned to the TM cohort (risperidone is a biweekly 25 mg intramuscular injection. Some patients not responding to 25 mg may benefit from a higher dose, not exceeding 50 mg every 2 weeks)Citation27. Patients treated with olanzapine pamoate were not included in this study because of its use through a restricted distribution programCitation33.
All analyses were performed with an intent-to-treat approach, whereby patients were assigned to a cohort based on the medication taken on the index date, and remained in that cohort regardless of subsequent or complementary therapies until the end of their continuous enrollment to Medicaid, death, or the end of data (follow-up).
Study outcomes
Study outcomes included index treatment adherence and persistence, HRU, and Medicaid spending, compared between patients initiated on OM vs TM patients.
Adherence to the index medication was measured using the proportion of days covered (PDC) evaluated during the first year following the index date. The PDC was calculated as the sum of the number of unique days during which the patient had their index medication on hand divided by 365 days, among patients followed for at least 1 year. The proportion of adherent patients was defined as the proportion of patients with a PDC ≥80%. Furthermore, persistence to the index medication was measured during the first 2 years following the index date. Patients were considered persistent if there was no observed gap ≥60 days without coverage by the index medication.
HRU was measured as the frequency of healthcare visits, by type of service (i.e. outpatient visits, emergency room visits, inpatient visits, long-term care visits, mental-health institute visits, 1-day mental-health visits, home care visits, and other services), in addition to the length of stay for inpatient visits, long-term care admissions, and mental health institute admissions (> 1 day). Other services were defined as any service which was not associated with a defined place of service, such as laboratory tests and medical imaging. Medicaid spending was measured using the following components: total healthcare costs (i.e. medical and pharmacy-related costs), pharmacy costs, and medical costs (outpatient costs, emergency room costs, inpatient costs, long-term care costs, mental-health institute costs, one-day mental-health visit costs, home care costs, and other services costs). HRU and Medicaid spending were assessed during the first 12 months following the index date.
Statistical analyses
Adherence comparison between cohorts was conducted using a multivariable linear regression, and the p-value and confidence intervals were generated through bootstrapping techniques with re-sampling (499 iterations). The adjusted odds of achieving a PDC ≥0.80 was computed using a multivariable logistic model. A Kaplan-Meier curve was calculated for both the OM and the TM cohorts to illustrate persistence. Patients were censored at the end of their continuous enrollment or death, whichever occurred first. In order to compare crude persistence rates over time, the difference between the Kaplan-Meier rates was assessed using a Log-rank test at 6, 12, 18, and 24 months. A multivariable Cox proportional hazard model estimated the adjusted hazard ratio with confidence intervals, comparing persistence in the 12 months post-index between the OM and TM cohorts. A sensitivity analysis was conducted where discontinuation was defined as a gap ≥30 days without the index medication on hand.
For HRU, mean, standard deviation, and median of the monthly number of visits or days were reported and compared using a generalized linear model with a negative binomial distribution. Incidence rate ratios (IRR) with 95% CIs and p-values were reported. Inpatient utilization was used as a proxy for relapses and was defined as all-cause inpatient visits/days and all-cause long-term care visits/days. Pharmacy costs were defined as cost information on prescription drug claims. Medical costs comprised outpatient costs, emergency room costs, inpatient costs, long-term care costs, mental-health institute costs, 1-day mental-health visit costs, home care costs, and other services costs. Costs were reported per patient per month. Comparison between the cohorts was achieved using a multivariable linear regression. P-values and 95% CIs were generated through bootstrapping techniques with re-sampling (499 iterations). All costs were inflated to 2015 US dollars.
Multivariable adjusted models controlled for demographics (age, sex, race/ethnicity); region of residence (state, urban/rural area); year of the index date; number of unique mental health diagnoses recorded during the baseline period; number of unique antipsychotic agents received during the baseline period; comorbidities at baseline (i.e. diabetes, cardiovascular diseases, substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, depressive disorders, Quan-Charlson Comorbidity IndexCitation34,Citation35); number of outpatients; 1-day mental-health institute, inpatient, and emergency room visits during the baseline period; total costs at baseline; Medicare eligibility; and risperidone dose equivalence on the index date. Risperidone dose equivalence was used as a proxy for the strength of the index medication and was calculated by converting the prescribed dose of the index medication to its oral formulation (in mg), and multiplying this by its oral risperidone equivalenceCitation36.
All analyses were conducted with SAS 9.3 or SAS 9.4 Software (SAS Institute, Cary, NC). A threshold of α = 0.05 was used to define statistical significance.
Results
A total of 785 OM patients and 625 TM patients were retained for analysis. presents the selection process of eligible patients. A majority of patients (94.7%) in the OM cohort were paliperidone palmitate users rather than aripiprazole users (5.3%; ). There was no statistical difference between the cohorts in terms of race, region characteristics (urban, suburban, or rural), insurance eligibility, number of unique mental health diagnoses, number of unique AP agents received, and monthly all-cause pharmacy and medical costs (). Patients in the TM cohort were slightly older (41.5 vs 39.9 years old, p = .02) and more often female (37.1% vs 32.0%, p = .04) than patients in the OM cohort (). Patients in the TM cohort also had a higher Quan-Charlson Comorbidity IndexCitation34,Citation35 (0.6 vs 0.5, p = .03) and more instances of cardiovascular diseases (12.6% vs 7.6%, p < .01; ). There were statistical differences between cohorts in terms of year of index date, oral risperidone daily equivalent dose, and healthcare resource utilization during baseline ().
Figure 2. Patient selection flowchart. ICD-9, International Classification of Diseases, 9th Revision; LAI, long-acting injectable antipsychotic; OM, once monthly; TM, twice monthly.
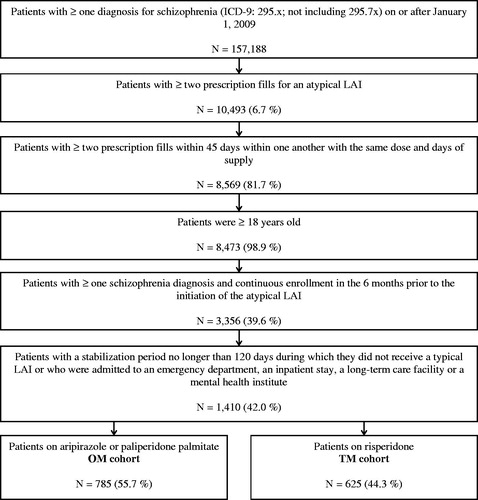
Table 1. Patient characteristics during the baseline period.
The adherence during the first 12 months of follow-up was higher in the OM cohort than in the TM cohort (mean PDC = 0.56 vs 0.50, adjusted mean difference [95% CI] = 0.06 [0.02–0.10], p < .01), although there was no statistically significant difference when looking at the proportion of patients achieving PDC ≥ 0.80 (44% vs 42%, adjusted odds ratio [95% CI] = 1.11 [0.81–1.52], p = .51).
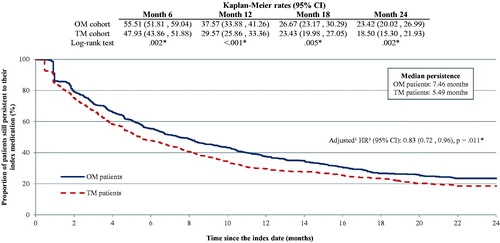
More than 60% of patients in both cohorts had discontinued their index medication after 12 months, and more than 75% of patients in both cohorts had discontinued their index medication after 24 months (). Kaplan-Meier rates of persistent patients were systematically higher for OM patients than for TM patients (12 months = 37.6% vs 29.6%, p < .01; 24 months = 23.4% vs 18.5%, p < .01; ). Similarly, the median persistence was longer in the OM cohort than in the TM cohort (7.5 months vs 5.5 months), and the hazard of discontinuing the index medication was lower in the OM cohort than in the TM cohort (hazard ratio [95% CI] = 0.83 [0.72–0.96], p = .01; ). These results were robust to the sensitivity analysis of using a 30-day gap rather than a 60-day gap.
Figure 3. Comparison of persistence to index medication during the first 2 years following the index year. CI, confidence interval; HR, hazard ratio; OM, once monthly; TM, twice monthly. *Significant at the 5% level. aAdjusted models controlled for demographics (age, sex, race/ethnicity); region of residence (state, urban/rural area); year of the index date, number of unique mental health diagnoses recorded during the baseline period; number of unique antipsychotic agents received during the baseline period; comorbidities at baseline (diabetes, cardiovascular diseases, substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, depressive disorders, Quan-Charlson Comorbidity Index); number of outpatient, 1-day mental-health institute, inpatient, and emergency room visits during the baseline period; total costs at baseline; Medicare eligibility; and risperidone dose equivalence on the index date. bOM patients vs TM patients: An HR <1 means that TM patients have a higher risk of discontinuing their index drug than OM patients.
shows the monthly rates of the HRU of the cohorts during the first 12 months of follow-up. Patients in the TM cohort had more inpatient utilization than patients in the OM cohort. After adjusting for confounding, patients in the OM cohort had lower rates of utilization for outpatient visits (IRR [95% CI] = 0.89 [0.79–1.00], p = .047), inpatient visits (IRR [95% CI] = 0.73 [0.58–0.92], p = .007), and long-term care visits (IRR [95% CI] = 0.58 [0.35–0.94], p = .026). However, they had more frequent use of other services (IRR [95% CI] = 1.32 [1.04–1.67], p = .022).
Figure 4. Inpatient utilization during the first 12 months following the index date. *Significant at the 5% level. IRR, incidence rate ratio; OM, once monthly; SD, standard deviation; TM, twice monthly. aAdjusted models controlled for demographics (age, sex, race/ethnicity); region of residence (state, urban/rural area); year of the index date; number of unique mental health diagnoses recorded during the baseline period; number of unique antipsychotic agents received during the baseline period; comorbidities at baseline (diabetes, cardiovascular diseases, substance-related and addictive disorders, schizophrenia spectrum and other psychotic disorders, depressive disorders, Quan-Charlson Comorbidity Index); number of outpatient, 1-day mental-health institute, inpatient, and emergency room visits during the baseline period; total costs at baseline; Medicare eligibility; and risperidone dose equivalence on the index date. bIRRs, 95% CIs, and p-values were estimated using a generalized linear model (GLM) with a negative binomial distribution.
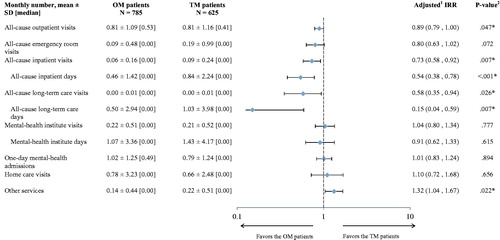
shows the monthly healthcare costs of the cohorts during the first 12 months that followed the index date. After adjusting for confounding, patients in the OM cohort had lower medical costs (monthly) than patients in the TM cohort (adjusted difference [95% CI] = –$460 [–709– –249], p < .001). However, monthly pharmacy costs were higher in the OM cohort (adjusted difference [95% CI] = $313 [204–410], p < .001). When combined, there was no difference in the overall monthly costs observed (adjusted mean difference [95% CI] = –$146 [–420– –84], p = .228).
Table 2. Healthcare costs during the first 12 months following the index date.
Discussion
This longitudinal cohort study sought to compare adherence, persistence, HRU, and Medicaid expenditures among adult patients with schizophrenia using OM vs TM atypical LAI APs using administrative claims data. This study suggests that patients on OM AP treatment (i.e. paliperidone palmitate OM and aripiprazole) had better adherence, better persistence, and lower inpatient utilization than patients on TM treatment (i.e. risperidone). Moreover, while pharmacy costs were higher among OM patients compared to TM patients, the medical cost savings offset the higher pharmacy costs, resulting in a non-significant total cost difference from a Medicaid payer perspective.
These findings are consistent with a previous study evaluating similar outcomes in patients with schizophrenia initiated on paliperidone palmitate vs those initiated on risperidone LAICitation32. In a study conducted by Joshi et al.Citation32, lower inpatient utilization among paliperidone palmitate users, but higher likelihood of physician visits, when compared to patients who were initiated on risperidone, were reported. In that study, patients on paliperidone palmitate had a higher mean PDC (0.64 vs 0.36, p < .001) and longer coverage during the 12-month period that followed the initiation of the index medication (234 days vs 132, p < .001) compared to patients treated with risperidoneCitation32. There are notable differences in the selection criteria of the Joshi et al.Citation32 study compared to the present study. Our study selected a population of patients stabilized on their medication, while Joshi et al.Citation32 selected a propensity matched cohort of commercially insured, Medicare supplemental, and Medicaid insured patients initiated on risperidone or paliperidone palmitate. This may explain observed differences in adherence and persistence compared with this study. Even though the original intent of this study was not to conduct a head-to-head comparison of risperidone and paliperidone palmitate, because of the low number of patients who were initiated on aripiprazole, the results of this study are akin to those of Joshi et al.Citation32. The results of the current study add to the robustness of Joshi et al.’sCitation32 conclusions by replicating the results in a sample of Medicaid stabilized patients.
We acknowledge that the present study included only a small proportion of aripriprazole patients, and that it may be interpreted as a head-to-head comparison between risperidone and paliperidone palmitate. However, since paliperidone is the active metabolite of risperidone, and the clinical effectiveness and tolerability of the oral dosage forms for these two atypical APs are comparableCitation37,Citation38, we hypothesized that differences in outcomes between similar chemical entities with different dosing frequencies would be largely mediated through differences in pharmacokinetics rather than pharmacodynamics.
This study reported that patients using less frequently dosed LAI APs had lower rates of relapses, as reflected through lower rates of inpatient utilization. One hypothesis for this effect is that this could be due to the effect of adherence as a mediator. Although this study was not designed to assess the sequential impact of dosing frequency on adherence, and adherence on inpatient utilization, this hypothesis could be substantiated by similar research that looked at the association between adherence and inpatient utilizationCitation39–41. One study examined California Medicaid recipients and found that gaps in AP treatment were a significant predictor of hospital admission (adjusted odds ratio [95% CI] = 1.49 [1.27–1.75])Citation39. Another study used data from the US Schizophrenia Care and Assessment Program, and found that self-reported non-adherence was a significant predictor of relapse, alongside having health insurance, prior relapse, being younger at disease onset, and poorer level of functioningCitation40. This trend seems to be true among elderly patients as well; a third study used Medicare claims to understand the association between non-adherence and found that patients with schizophrenia with high adherence had significantly fewer mean inpatient admissions than those with low adherence (high = 0.44 ± 0.68, low = 0.68 ± 1.00, p = .015) during the 12-month follow-up periodCitation41. Patients in the OM cohort had significantly higher adherence and a better persistence than those in the TM, which may have contributed to the lower inpatient utilization observed in the OM cohort.
Taken together, these findings suggest that atypical APs with less frequent dosing may be associated with fewer relapses. We hypothesize that this could be due to a delay in the loss of therapeutic effect during gaps in therapy, as well as to differences in adherence, although this cannot be directly inferred from the present study. However, a 2013 systematic review that examined the association between AP adherence and economic outcomes, including inpatient HRU, came to the same conclusion as we didCitation42. The similar findings observed in our results and that review corroborate our hypothesis, and may indicate that it applies to APs beyond atypical LAI APs. Further research should investigate the role of adherence as a possible mediator between dosing frequency and health outcomes. In addition, future research could also evaluate the role of dosing frequency and adherence on indirect costs such as absenteeism and loss of productivity.
Strengths and limitations
This study used a real-world population followed for a longer observation period than what is typical for clinical trials. The data were recent, ethnically diverse, and geographically widespread. Our design simulated a new user of OM or TM LAI, and the implementation of a stabilization period allowed us to create two cohorts of patients initiating the medication for the purpose of chronic use. However, our study is subject to a few limitations. First, these results are derived from a Medicaid-insured population from six states, and may not be generalizable to other populations. Second, given the small proportion of aripiprazole patients, results may be more representative of paliperidone palmitate patients than aripiprazole patients. Third, for the calculation of adherence, intake of the medication is largely inferred from pharmacy claims, which does not guarantee that the patient actually received the injections. However, since the administration of these drugs should be performed by a healthcare professional, this limitation is not as important as similar studies focusing on oral APs. Fourth, since we used an intent-to-treat approach, patient cohort assignment was determined at the index date, in spite of treatments they may have taken subsequently or concomitantly. Finally, administrative claims data are subject to coding errors and omissions. However, this is expected to have affected both cohorts similarly.
Conclusion
In this population of Medicaid-insured patients with schizophrenia, patients stabilized on OM LAI AP had higher adherence and persistence compared to those stabilized on TM LAI AP. Patients stabilized on OM LAI AP had lower rates of inpatient utilization and similar total healthcare costs compared with patients stabilized on TM LAI AP. Higher medical costs in the TM LAI cohort offset the higher pharmacy costs in the OM LAI cohort, resulting in no statistically significant total costs difference between the two cohorts. Further research is warranted to examine the direct and adherence-mediated relationships between LAI AP pharmacology and health and economic outcomes for patients with schizophrenia.
Transparency
Declaration of funding
Supported by Janssen Scientific Affairs, LLC.
Declaration of financial/other relationships
CB is an employee of Janssen Scientific Affairs, LLC, and owns stock/stock options from Johnson & Johnson. MA was a post-doctoral fellow with Janssen Scientific Affairs, LLC during his involvement with the study. DP, YX, PTL, MHL, and PL are employees of Analysis Group, Inc., which has received consultancy fees from Janssen Scientific Affairs, LLC.
Previous presentations
Partial results of this study were presented at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 22nd Annual International Meeting, the Academy of Managed Care Pharmacy (AMCP) Nexus 2016 Conference, and the 33rd International Conference on Pharmacoepidemiology & Therapeutic Risk Management.
Acknowledgments
No assistance in the preparation of this article is to be declared.
References
- Kirkpatrick B, Miller B, Garcia-Rizo C, et al. Schizophrenia: a systemic disorder. Clin Schizophr Relat Psychoses 2014;8:73-9
- Simeone JC, Ward AJ, Rotella P, et al. An evaluation of variation in published estimates of schizophrenia prevalence from 1990–2013: a systematic literature review. BMC Psychiatry 2015;15:193
- Brown AS. The environment and susceptibility to schizophrenia. Prog Neurobiol 2011;93:23-58
- Kirkbride JB, Errazuriz A, Croudace TJ, et al. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-analyses. PLoS One 2012;7:e31660
- Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163-96
- Bobes J, Garcia-Portilla MP, Bascaran MT, et al. Quality of life in schizophrenic patients. Dialogues Clin Neurosci 2007;9:215-26
- Ginovart N, Kapur S. Role of dopamine D(2) receptors for antipsychotic activity. Handb Exp Pharmacol 2012:27-52
- Li P, Snyder GL, Vanover KE. Dopamine targeting drugs for the treatment of schizophrenia: past, present and future. Curr Top Med Chem 2016;16:3385-403
- Wiersma D, Nienhuis FJ, Slooff CJ, et al. Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull 1998;24:75-85
- Citrome L. Schizophrenia relapse, patient considerations, and potential role of lurasidone. Patient Prefer Adherence 2016;10:1529-37
- San L, Serrano M, Canas F, et al. Towards a pragmatic and operational definition of relapse in schizophrenia: A Delphi consensus approach. Int J Psychiatry Clin Pract 2015;19:90-8
- Olivares JM, Sermon J, Hemels M, et al. Definitions and drivers of relapse in patients with schizophrenia: a systematic literature review. Ann Gen Psychiatry 2013;12:32
- Nicholl D, Akhras KS, Diels J, et al. Burden of schizophrenia in recently diagnosed patients: healthcare utilisation and cost perspective. Curr Med Res Opin 2010;26:943-55
- Lafeuille MH, Laliberte-Auger F, Lefebvre P, et al. Impact of atypical long-acting injectable versus oral antipsychotics on rehospitalization rates and emergency room visits among relapsed schizophrenia patients: a retrospective database analysis. BMC Psychiatry 2013;13:221
- Llorca PM. Partial compliance in schizophrenia and the impact on patient outcomes. Psychiatry Res 2008;161:235-47
- Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas 2014;5:43-62
- Coldham EL, Addington J, Addington D. Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand 2002;106:286-90
- Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 2008;8:32
- Sendt KV, Tracy DK, Bhattacharyya S. A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res 2015;225:14-30
- Kaplan G, Casoy J, Zummo J. Impact of long-acting injectable antipsychotics on medication adherence and clinical, functional, and economic outcomes of schizophrenia. Patient Prefer Adherence 2013;7:1171-80
- Brissos S, Veguilla MR, Taylor D, et al. The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal. Ther Adv Psychopharmacol 2014;4:198-219
- Samalin L, Garnier M, Auclair C, et al. Clinical decision-making in the treatment of schizophrenia: focus on long-acting injectable antipsychotics. Int J Mol Sci 2016;17:1935
- Rossi G, Frediani S, Rossi R, et al. Long-acting antipsychotic drugs for the treatment of schizophrenia: use in daily practice from naturalistic observations. BMC Psychiatry 2012;12:122
- De Berardis D, Marini S, Carano A, et al. Efficacy and safety of long acting injectable atypical antipsychotics: a review. Curr Clin Pharmacol 2013;8:256-64
- Markowitz M, Fu DJ, Levitan B, et al. Long-acting injectable paliperidone palmitate versus oral paliperidone extended release: a comparative analysis from two placebo-controlled relapse prevention studies. Ann Gen Psychiatry 2013;12:22
- Llorca PM, Abbar M, Courtet P, et al. Guidelines for the use and management of long-acting injectable antipsychotics in serious mental illness. BMC Psychiatry 2013;13:340
- Risperidal Consta(C) [package insert]. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2007
- Invega Sustenna(R) [package insert]. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2009
- Abilify Maintena(R) [package insert]. Tokyo, Japan: Otsuka Pharmaceutical Co. Ltd.; 2016
- Uchida H, Suzuki T. Dose and dosing frequency of long-acting injectable antipsychotics: a systematic review of PET and SPECT data and clinical implications. J Clin Psychopharmacol 2014;34:728-35
- Furiak NM, Gahn JC, Klein RW, et al. Estimated economic benefits from low-frequency administration of atypical antipsychotics in treatment of schizophrenia: a decision model. Ann Gen Psychiatry 2012;11:29
- Joshi K, Pan X, Wang R, et al. Healthcare resource utilization of second-generation long-acting injectable antipsychotics in schizophrenia: risperidone versus paliperidone palmitate. Curr Med Res Opin 2016;32:1873-81
- Zyprexa Relprevv(C) [package insert]. Indianapolis, IN: Eli Lilly and Company; 2012
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130-9
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83
- Leucht S, Samara M, Heres S, et al. Dose equivalents for second-generation antipsychotics: the minimum effective dose method. Schizophr Bull 2014;40:314-26
- Nussbaum A, Stroup TS. Paliperidone for schizophrenia. Cochrane Database Syst Rev 2008:CD006369
- Melnik T, Soares BG, Puga ME, et al. Efficacy and safety of atypical antipsychotic drugs (quetiapine, risperidone, aripiprazole and paliperidone) compared with placebo or typical antipsychotic drugs for treating refractory schizophrenia: overview of systematic reviews. Sao Paulo Med J 2010;128:141-66
- Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull 2008;34:173-80
- Ascher-Svanum H, Zhu B, Faries DE, et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry 2010;10:2
- Offord S, Lin J, Wong B, et al. Impact of oral antipsychotic medication adherence on healthcare resource utilization among schizophrenia patients with Medicare coverage. Community Ment Health J 2013;49:625-9
- Dilla T, Ciudad A, Alvarez M. Systematic review of the economic aspects of nonadherence to antipsychotic medication in patients with schizophrenia. Patient Prefer Adherence 2013;7:275-84