?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: To estimate the economic burden of needlestick injuries (NSIs) among healthcare workers (HCWs) in China.
Design: A model was built to evaluate the economic burden of NSIs.
Methods: The cost model was developed from a societal perspective, including both direct and indirect costs, with lifetime horizon. The direct costs were categorized into infection prevention and treatment of infections. The indirect cost included productivity loss of both HCWs and his/her family members due to the blood-borne infections. Sub-group analyses were conducted to estimate the cost per NSI when the source patient (SP) was confirmed with hepatitis B virus/hepatitis C virus/human immunodeficiency virus (HBV/HCV/HIV) infection. One-way and probabilistic sensitivity analyses were conducted for all parameters to examine the robustness of the result.
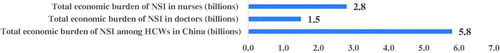
Results: The model projected a total cost of ¥699 for each NSI (direct and indirect cost were ¥553 and ¥146, respectively). The cost per NSI when the SP was confirmed with HBV/HCV/HIV was ¥4,238, ¥18,404, and ¥6,152, respectively. The total economic burden of NSIs among HCWs in China was estimated to be ¥5.8 billion, and about half of the cost was associated with NSIs in nurses, at ¥2.8 billion.
Limitations: This study did not incorporate the costs of litigation/psychological, and the prevalence of the infections was based on the general population, so the actual costs per NSI may be underestimated. More real-world studies of treatment cost about HBV/HCV are needed to further supporting this study.
Conclusions: The economic burden of NSIs among HCWs in China is substantial. Comprehensive NSI prevention programs, including implementation of safety needles and devices, have high potential for healthcare institutions to achieve downstream cost savings and cost offsets.
Introduction
Healthcare workers (HCWs) face high risk of occupational exposure to blood-borne pathogens due to needlestick injuries (NSIs). More than 25 pathogens can be transmitted via needlesCitation1 and cause transient or persistent infections due to NSIs among HCWs. Hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) account for the majority of occupational infections, which are major threats to HCWs in the workplaceCitation1,Citation2. The World Health Organization (WHO) estimated that, of the 37 million HCWs, almost 3 million had one or more NSIs each yearCitation3. It has also been estimated that occupational exposure to percutaneous injuries resulted in about 66,000 HBV, 16,000 HCV, and 1,000 HIV infections worldwide among HCWs each yearCitation4. In the United States (US), the Centers for Disease Control and Prevention (CDC) estimated that hospital-based HCWs experienced 385,000 needle-sticks and other sharps-related injuries each year; an average of ∼1,000 sharps injuries per dayCitation5. In China, the incidence of sharps injuries was estimated to be around 1,032 per 1,000 HCWs per year, and 121.3 per 100 occupied beds per yearCitation6. NSIs negatively impact both the physical and psychological well-being of HCWs, including fear, emotional distress, anxiety, and even depressionCitation7.
In addition, NSIs have been implicated to be a major cause of economic burden. A systematic review of economic analyses related to NSIs documented that the overall costs are increasing over time due to NSIsCitation2 and varied significantly across countries. In the US, it was estimated that the cost per each NSI evaluation was $260Citation8. In Belgium, the direct cost per NSI ranged from €210 to €950 and the indirect cost per NSI ranged from €63 to €844Citation9. However, there is limited data in the literature on the economic burden of NSIs among HCWs in China. The purpose of this study is to estimate the cost for each NSI incidence as well as the economic burden associated with NSIs among HCWs in China.
Materials and methods
Model overview
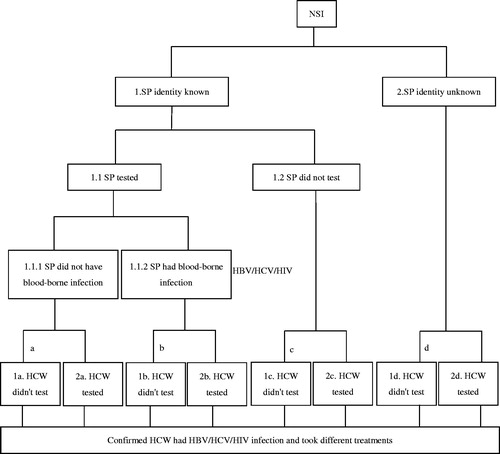
A cost model was developed to estimate the economic burden of NSIs among HCWs in China using Microsoft Excel 2016i (). A societal perspective was adopted in the model. The cost was divided into direct and indirect costs. The direct cost included laboratory (lab) tests, such as tests for HIV antibodies, hepatitis B/C serology, along with treatment costs related to post-exposure prophylaxis (PEP) and cost of infection. The indirect cost included productivity loss of both HCWs and their family members due to blood-borne infections. Direct cost was additionally categorized into two components: cost to prevent infections post-NSI and cost of treatment of infections as needed. A lifetime horizon was adopted and a 3.5% discount rate was applied in calculating the treatment cost of infection with HBV/HCV/HIV. One-way sensitivity analysis was conducted for all parameters by varying ±20% their mean values in the model to examine the robustness of the model. We also conducted a probabilistic sensitivity analysis (PSA) which was based on 5,000 Monte Carlo simulations to examine the uncertainty in the model and the stability of the results when varying the input values. Beta distributions were used for percentage parameters, Gamma distributions for costs, and Triangular distributions for other variable parameters.
Model structure
When NSIs occur, pending on the source patient (SP) situations, different follow-ups may take place as shown in the pathways in the model (): “SP identity known” and “SP identity unknown”. In the “SP identity known” state, SP could either get lab tests or not; HCWs could either get lab tests and ensuing lab tests or not, regardless of the SP’s infection status. The lab tests imply the tests of SP and HCWs immediately after NSIs, and the ensuing lab tests imply the follow-up tests to confirm whether HCWs have been infected or not. In the “SP identity unknown” state, HCWs could also get lab tests and ensuing lab tests or not. The cost per NSI was then estimated following the pathways. The total economic burden of NSI among Chinese HCWs was estimated by taking into consideration the number of HCWs and the cost per NSI. If HCWs were confirmed with blood-borne infection (HBV/HCV/HIV) due to NSIs, we assumed that the initial infection would follow the disease’s natural history and the infected HCWs would receive standard of care treatment. The economic burden of HBV/HCV/HIV was then estimated based on the confirmed infections. The model structure was validated by eight key opinion leaders (KOLs) who were infection specialists with rich experience in hospital infection and control from tertiary care hospitals in Shanghai, Jiangsu, Zhejiang, Sichuan, and Guangxi provinces in China. The background and objectives of the study were introduced to these experts before the model structure was presented to them. The experts confirmed that the model structure appropriately reflected their current local hospital infection and control practices.
Model inputs
Data of the model were mainly obtained from a literature review. In situations in which pertinent information was unavailable, data were estimated based on interviewing the eight KOLs who had rich experience in hospital infection and control. A survey questionnaire was developed for this purpose. The questionnaire included the percentage of SP and HCWs tested after NSIs, the costs of litigation and psychological counseling of NSIs, and the productivity loss of HCWs due to NSIs. These experts were asked to estimate the relevant data needed in the model, and the mean values were calculated as model inputs.
Percentage and transition probability inputs
The percentage of SP identity known was obtained from a multi-center survey study which was conducted in China by Gao et al.Citation6. The percentage of HCWs tested after NSIs in the model was estimated based on interviews of the eight KOLs () as the data was unavailable in the literature. The prevalence of SP infected with HBV/HCV/HIV and the percentage of HCWs who were susceptible to the various infections were extracted from literature in China. The transmission probabilities for at-risk population for HBV/HCV/HIV were obtained from a published study conducted in BelgiumCitation9. Infection risk was calculated based on the prevalence of infection of SP, percentage of HCWs susceptible to the infections, and transmission probability of the infections (HBV/HCV/HIV). The likelihood that the various infections may result in chronic disease status and the associated cost were also derived from the literature.
Table 1. Percentage and transition probability inputs in the model.
Costs inputs
Unit cost of testing and PEP were estimated from unpublished data from China (). These data included frequencies of testing and follow-up procedures for occupational exposure treatment in HCWs from Zhongshan Hospital, a comprehensive teaching hospital affiliated to Fudan University. The corresponding cost of lab tests and PEP were obtained from the compilation of medical service items and their fee schedules in China. The cost associated with infection treatment was estimated from the literature in China. For context, the exchange rate at the time was 1USD = 6.75CNY.
Table 2. Costs inputs in the model.
Other inputs
HCWs’ productivity loss due to NSIs was sourced from the KOL interviews. Based on KOLs’ feedback, the costs of litigation and psychological counseling were not included in the model since they were negligible in China at the present. Other inputs, including survival years of the infections, prevalence of NSIs, and the number of HCWs were derived from the literature in China ().
Table 3. Other inputs in the model.
Results
The economic burden per NSI
The total cost per NSI was estimated to be ¥699, of which ¥553 was associated with direct cost and ¥146 was attributable to indirect cost (productivity loss). For direct cost, ¥319 was spent on testing and PEP, and ¥234 was expensed for treatment of infections ().
Table 4. Economic burden per NSI.
Sub-group analyses of economic burden per NSI
The cost per NSI when SP was confirmed with HBV, HCV, or HIV infections (i.e. HCWs who experienced an NSI were exposed to HBV, HCV, HIV) was estimated to be ¥4,238, ¥18,404, and ¥6,152, respectively. The cost components in these situations are displayed in .
The total economic burden of NSI in China
The total economic burden of NSIs among HCWs in China was estimated to be around ¥5.8 billion and about half of the costs were associated with NSIs in nurses (¥2.8 billion) ().
Table 5. Total economic burden of NSIs among HCWs.
Sensitivity analyses
One-way sensitivity analysis indicated that “probability of SP unknown, HCWs didn’t test” was the most important driver for the cost estimate associated with NSIs (top 10 are presented in ). One-way sensitivity analysis indicated the general robustness of the results.
As the result of the PSA, the distribution of the 5,000 Monte Carlo simulations are shown in . The 95% credible interval of the total cost per NSI is ¥616.3 to ¥782.0. PSA confirmed the stability of the results.
Discussion
Our study was the first analysis to examine the economic burden of NSIs among HCWs in China from a societal perspective. The results indicated that the cost per NSI was about ¥699 (representing 4.16% of per capita GDP in China in 2017Citation27). The direct and indirect costs were ¥553 and ¥146, respectively (representing 3.29% and 0.87% of 2017 per capita GDP in China in 2017). Owing to the large working population of HCWs in China, the total annual economic burden of NSIs amounted to ¥5.8 billion, representing a significant economic burden to the healthcare system and society.
Wang et al.Citation28 conducted a prospective in-hospital study in China. The study collected the cost of prevention and control of occupational exposures of HCWs from the occupational exposure reporting system of a hospital. It was estimated that the cost per case of occupational exposure was ¥349.84, which only included partial direct cost (lab testing and PEP). Our model estimated the direct cost of infection prevention post-NSIs was ¥319, which was similar to the findings reported by Wang et al. Hanmore et al.Citation9 estimated the total direct cost per NSI ranged from €210.01 to €950.34 (∼¥1,841 to ¥8,331 in 2017, representing 3.85% to 17.42% of 2017 per capita GDP in Belgium), while the indirect cost per NSI ranged from €63.22 to €844.22 (∼¥554 to ¥7,401 in 2017, representing 1.16% to 15.47% of 2017 per capita GDP in Belgium). Most of the cost components were similar to the estimates of our study, except the indirect cost components, which included the cost of counseling, compensation, and litigation in addition to productivity loss. In light of local practices for hospital management in China, our study didn’t include the cost of counseling and litigation. A study conducted in SwedenCitation19 estimated that direct cost was about €272 (∼¥2,985, representing 5.94% of 2017 per capita GDP in Sweden) per reported injury, which included PEP, lab tests, and counseling. Compared with studies conducted in other countries, the cost of NSIs estimated in our study was lower, which is likely explained by the differences in the established standard procedures of handling NSIs in hospitals and cost structures in healthcare. More specifically, reasons of the low cost of NSIs probably included the following: First, the ratio of tests and treatment of HCWs after NSIs were low in China. Second, the cost of tests and treatment were low. Finally, our study only included direct costs, except the cost of counseling and other costs.
As expected, if the SP is confirmed with a blood-borne infection, the cost per NSI would be much higher. When the SP is confirmed with HBV/HCV/HIV infections, the corresponding associated cost was estimated to be ¥4,238, ¥18,404, and ¥6,152, respectively (cost for testing and PEP per NSI was ¥397, ¥1,712, and ¥5,354, respectively). Previous research has shown that the risk of getting infected with a blood-borne infection after NSI is higher for HBV than HCVCitation29. In China, however, most HCWs are immune to HBV infection due to implementation of broad HBV vaccination programs. The significantly higher cost for potential HCV vs HBV infections is likely attributable to the greater susceptibility to HCV infection among HCWs and its higher risk of transitioning into a chronic disease state once infected. Our estimate for the cost of NSI with HIV exposure appeared to be low. This was due in no small part to all HIV treatment being currently free in China for patients and government procuring HIV drugs at a large discount. Nevertheless, in light of the continued rise in HIV infection in ChinaCitation30, the cost of NSIs as a result of HIV exposure likely continues to grow in the future.
Considering the high economic burden of NSIs, multi-pronged approaches should be taken to reduce NSIsCitation31. Education and training of safe administration of needles should be a standard curriculum for new HCWs in hospitals. For current HCWs, annual refresher courses should be considered. Standard operating procedures should be established for reporting and follow-ups of NSIs. In addition, NSIs should be leveraged for hospital performance evaluations. Enacting legislation requiring the use of safety injection devices would likely be the most effective measure in reducing NSIs. Numerous studies have demonstrated that adoption of safety devices would lead to a significant decrease in NSIsCitation32–35. While the devices with advanced safety features are more expensive, the financial savings stemming from reduced NSIs were likely more than offset by the acquisition cost, as the US General Accounting Office (GAO) concluded in their evaluation of legislation of universal adoption injection devices with advanced safety featuresCitation36. In light of available evidence, the WHO also recommends the use of safety injection devices and calls on governments to transition to their exclusive use by 2020Citation37.
Our study has several limitations. Several transition probabilities after NSI were derived from the KOLs interviews, since no published data were available. The current study might underestimate the actual costs per NSI because we did not incorporate the costs of litigation and psychological counseling under the current healthcare environment in China. Also, we only included HBV/HCV/HIV infections, without considering other low risk blood-borne infections. Furthermore, we calculated the total costs of the chronic diseases by multiplying the annual cost by the average survival years with the disease, assuming the annual costs of the chronic diseases keep constant over time and any development of the diseases, while the current annual direct cost of treatment for chronic hepatitis B and chronic hepatitis C varied considerably, respectively ¥7,469.27 and ¥69,279.97. More real-world studies of treatment cost about the chronic diseases are needed for further supporting the assumption and the inputs we used in this study. Finally, the prevalence of these three infections were estimated based on epidemiological data from the general population, and the prevalence of blood-borne pathogens is likely to be higher in hospitalized patients.
Conclusions
The economic burden of NSIs among HCWs in China is substantial. Comprehensive NSI prevention programs, including implementation of safety needles and devices, should be conducted in hospitals, which would have high potential for healthcare institutions to achieve a downstream of cost savings and cost offsets.
Transparency
Declaration of funding
This work was funded by Becton Dickinson (BD) – China.
Declaration of interest
YA and NY are employees of Becton Dickinson, China. VB, SG and EPE are employees of Becton Dickinson, USA.
Disclosure statement
No potential conflict of interest was reported by the author(s).
JME peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
We thank key opinion leaders including Qingfeng Shi from Zhongshan Hospital, Fudan University, Wensen Chen from Jiangsu Province Hospital, Fu Qiao from West China School of Medicine/West China Hospital of Sichuan University, Ziqin Xu from Wenzhou People’s Hospital, Le Yang from Changzhou Second People’s Hospital, Tieer Gan from Zhejiang Provincial Hospital of TCM and Dan Liao from The Maternal and Child Health Hospital of Guangxi Zhuang Autonomous Region, who were infection specialists with rich experience in hospital infection and control for the validation of the model structure. We also thank Xiaohan Hu, MD, PhD from Shanghai Centennial Scientific, China for his editorial assistance in manuscript preparation.
Notes
i Microsoft Corporation, Redmond, WA.
References
- Tarantola A, Abiteboul D, Rachline A. Infection risks following accidental exposure to blood or body fluids in health care workers: a review of pathogens transmitted in. Ajic Am J Infect Control. 2006;34(6):0–375.
- Mannocci A, De Carli G, De Bari V, et al. How much do needlestick injuries cost? A systematic review of the economic evaluations of needlestick and sharps injuries among healthcare personnel. Infect Control Hosp Epidemiol. 2016;37(6):635–646.
- Tarigan LH, Cifuentes M, Quinn M, et al. Prevention of needle-stick injuries in healthcare facilities: a meta-analysis. Infect Control Hosp Epidemiol. 2015;36(7):823–829.
- Prús-Üstün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48:482–490.
- Centers for Disease Control and Prevention. Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program. Atlanta: CDC; 2008.
- Gao X, Hu B, Suo Y, et al. A large-scale survey on sharp injuries among hospital-based healthcare workers in China. Sci Rep. 2017;7(1):7.
- Lee WC, Nicklasson L, Cobden D, et al. Short-term economic impact associated with occupational needlestick injuries among acute care nurses. Curr Med Res Opin. 2005;21(12):1915–1922.
- Orenstein R, Reynolds L, Karabaic M, et al. Do protective devices prevent needlestick injuries among health care workers? Am J Infect Control. 1995;23(6):344–351.
- Hanmore E, Maclaine G, Garin F, et al. Economic benefits of safety-engineered sharp devices in Belgium – a budget impact model. BMC Health Serv Res. 2013;13(1):489.
- Liang X, Bi S, Yang W, et al. Epidemiological serosurvey of Hepatitis B in China — Declining HBV prevalence due to Hepatitis B vaccination. Vaccine. 2009;27(47):6550–6557.
- Chen Y-s, Li L, Cui F-q, et al. Cui Fu-qiang XW. A sero-epidemiological study on hepatitis C in China [article in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32(9):888–891.
- Huang M, Ye L, Liang B, et al. Characterizing the HIV/AIDS Epidemic in the United States and China. Int J Environ Res Public Heal. 2015;13(1):30.
- Yang S. Analysis of the detecting results about the hepatitis B makers of 2265 medical staff and the correlative infection factors [article in Chinese]. Jilin Univ. 2011. [master thesis].
- Yang Z, Ma Y, Zhang P, et al. Analysis on the test result of HBV and HCV in medical workers and its countermeasures [article in Chinese]. Lab Med Clin. 2011;08:2347–2349.
- Hu Xiao Yan Wm Hui, Jian X. Analysis of current status of blood-borne diseases among medical staffs [article in Chinese]. J Mod Med Heal. 2010;26:654–656.
- Leigh JP, Gillen M, Franks P, et al. Costs of needlestick injuries and subsequent hepatitis and HIV infection. Curr Med Res Opin. 2007;23(9):2093–2105.
- Tzu-Yin C. Estimation of the Direct Cost Caused by Percutanesous Injuries in Taiwan Healthcare Workers. TaiwanDepartment Nurs Coll Med Natl Taiwan Univ Master Thesis 2011. 1–38.
- Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61(1):S58–S68.
- Glenngård AH, Persson U. Costs associated with sharps injuries in the Swedish health care setting and potential cost savings from needle-stick prevention devices with needle and syringe. Scand J Infect Dis. 2009;41(4):296–302.
- Li Yan W, Huai Z, Wei WY. Investigation on the cost of patients with different outcomes related to hepatitis B virus infection in Beijing. Basic Clin Med. 2014;34:1235–1240.
- Hu M, Chen W. Assessment of total economic burden of Chronic Hepatitis B (CHB) – related diseases in Beijing and Guangzhou, China. Value in Health. 2009;12:S89–S92.
- Liu Y, Chen W. HS. Comparison of medical expenditure after the implementation of health insurance reimbursement for hepatitis C outpatient treatment. Chinese Heal Econ. 2011;30:60–61.
- Zhang X, Li M, Feng Y, et al. Study on economic burden caused by antiretroviral treatment for people living with HIV/AIDS and influencing factors in Nanjing. Zhonghua Liu Xing Bing Xue Za Zhi. 2015;36(5):440–444.
- National data. [cited 2020 Mar 04]. Available from: http://data.stats.gov.cn/easyquery.htm?cn=C01.
- Yuan S-e, Li Ying-Lan TD. Monitoring of occupational exposure among health care workers [article in Chinese]. Chinese J Nosocomiology. 2015;21(3):150–154.
- National data. [cited 2020 Mar 04]. Available from: http://data.stats.gov.cn/easyquery.htm?cn=C01&zb=A0O02&sj=2015.
- Data of GDP. [cited 2020 Mar 04]. Available from: https://www.kuaiyilicai.com/stats/global/yearly/g_gdp_per_capita_ppp/2017.html
- Wang B, Li Lin L, Juan ZY. Characteristics as well as prevention and control costs of occupational exposure to blood-borne pathogens. Chinese J Infect Control. 2018;17:979–982.
- Shiao J, Guo L, McLaws ML. Estimation of the risk of bloodborne pathogens to health care workers after a needlestick injury in Taiwan. Am J Infect Control. 2002;30(1):15–20.
- Phipps W, Honghong W, Min Y, et al. Risk of medical sharps injuries. Am J Infect Control. 2002;30(5):277–282.
- Motaarefi H, Mahmoudi H, Mohammadi E. Factors associated with needlestick injuries in health care occupations: a systematic review. J Clin Diagnostic Res. 2016;10:1–4.
- Fukuda H, Yamanaka N. Reducing needlestick injuries through safety- engineered devices: results of a Japanese multi-centre study. J Hosp Infect. 2016;92(2):147–153.
- Sossai D, Guardo MDI, Foscoli R, et al. Efficacy of safety catheter devices in the prevention of occupational needlestick injuries: applied research in the Liguria Region (Italy). J Prev Med Hyg. 2016;57(2):110–114.
- Harb AC, Tarabay R, Diab B, et al. Safety engineered injection devices for intramuscular, subcutaneous and intradermal injections in healthcare delivery settings: a systematic review and meta-analysis. BMC Nurs. 2015;14:71.
- Ballout RA, Diab B, Harb AC, et al. Use of safety-engineered devices by healthcare workers for intravenous and/or phlebotomy procedures in healthcare settings: a systematic review and meta-analysis. BMC Health Serv Res. 2016;16:458.
- GAO. The cost-effectiveness impact on selected devices of hospital needle-stick injury prophylaxis. Washington, DC: GAO; 2000.
- World Health Organization. WHO guideline on the use of safety-engineered syringes for intramuscular, intradermal and subcutaneous injections in health-care settings. Geneva: WHO; 2015.