Abstract
Objectives
Implantable cardioverter defibrillator (ICDs) for primary prevention (PP) of sudden cardiac arrest (SCA) is underutilized in developing countries. The Improve SCA study has identified a subset of 1.5 primary prevention (1.5PP) patients with a higher risk of SCA and a significant mortality benefit from ICD therapy. From the perspective of China’s healthcare system, we evaluated the cost-effectiveness of ICD therapy vs. no ICD therapy among 1.5PP patients with a view to informing clinical and policy decisions.
Methods
A published Markov model was adjusted and verified to simulate the course of the disease and describe different health states of 1.5PP patients. The patient characteristics, mortality, utility and complication estimates were obtained from the Improve SCA study and other literature. Cost inputs were sourced from government tender prices, medical service prices and clinical experts’ surveys in 9 Chinese public hospitals. For both ICD and no ICD therapy, the total medical costs and quality-adjusted life-years (QALYs) were modelled over a lifetime horizon and the incremental cost-effectiveness ratio (ICER) was calculated. Deterministic and probabilistic sensitivity analyses were performed to assess the uncertainty of the model parameters. We used the willingness-to-pay (WTP) threshold recommended by China Guidelines for Pharmacoeconomic Evaluations, one to three times China’s GDP per capita (CNY85,698–CNY257,094) in 2022 Chinese Yuan.
Results
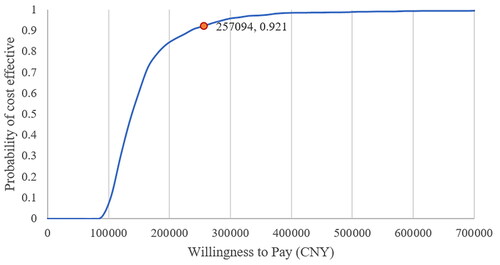
The incremental cost effectiveness ratio (ICER) of ICD therapy compared to no ICD therapy is 139,652 CNY/QALY, which is about 1–2 times China’s GDP per capita. The probability that ICD therapy is cost effective was 92.1%. Results from sensitivity analysis supported the findings of the base case.
Conclusions
ICD therapy compared to no ICD therapy is cost-effective for the 1.5PP patients in China.
Introduction
In China, the disease burden of cardiovascular disease and sudden cardiac death (SCD) has increased rapidly over the past three decades, because of dramatic changes in lifestyle, the growth of living standards, and the aging of the populationCitation1. According to the report of national cardiovascular disease center, an average of 544,000 people died annually due to sudden cardiac arrest (SCA), making it the leading cause of death in ChinaCitation2. Implantable cardioverter defibrillators (ICDs) terminate sudden or unexpected arrhythmias leading to SCA, thus playing a vital role in realizing the goal of SCD prevention. Also, the implantation of ICD has been strongly recommended in clinical guidelines for the management of patients for both primary prevention (PP) and secondary prevention (SP) of SCDCitation3,Citation4. However, despite the strong recommendation of ICD implantation and the extremely high mortality of SCA, ICD therapy adoption remains low in China, partly because of inadequate reimbursement coverage and lack of patient and physician education due to limited health resources and cost considerations.
A prospective, non-randomized, non-blinded, multicenter, global study called Improve SCA has been conducted to identify a subset of the PP population at elevated risk for SCD termed 1.5 primary prevention (1.5PP). The 1.5 PP population consists of patients with at least one of the following additional risk factors: Syncope or pre-syncope (due to suspected ventricular tachycardia (VT)), very low left ventricular ejection fraction (LVEF < 25%), non-sustained ventricular tachycardia (NSVT), and/or frequent premature ventricular contractions (PVCs)Citation5. The study enrolled 3889 patients where ICD utilization in clinically indicated patients is low, including Asia, Latin America, Eastern Europe, the Middle East, and South Africa. It was worth mentioning that over half of those patients were from China. The study results demonstrated that, in 1.5PP population, there is a 49% relative risk reduction in all-cause mortality in patients who received ICD compared to those without ICD implant (HR = 0.51; 95% CI = 0.40–0.66, p < 0.001)Citation6. In addition, the number needed to treat to save 1 life over 3 years in 1.5PP patients and PP patients without 1.5 PP characteristics was 10 and 40, respectively, indicating a higher rate of appropriate therapy in 1.5PP populationCitation6. Considering the explicit clinical advantages of ICD implantation in 1.5PP patients, the cost-effectiveness analysis of ICD therapy in this subset population is highly demanded. In China, the huge population and the limited health care resources have made it difficult for policy makers to allocate the resources and cover the full PP population. In this case, the economic outcomes of ICD therapy in 1.5PP cohort is crucial to the prioritization of health care resources and the necessity of therapy adoption.
Currently, the overall ICD underutilization in China contributed to the lack of health economic evidence of ICD therapy, let al.one health economic evidence in 1.5PP population with the higher risks of SCA. The objective of this study is to critically assess the cost-effectiveness of ICD therapy for the 1.5PP population and drive evidence-based policy decision and health resource allocation.
Methods
A cost-utility analysis was conducted to estimate lifetime costs and quality-adjusted life years (QALYs) from the perspective of China’s healthcare system. In addition, we administrated an expert survey to develop an overview of domestic ICD therapy adoption, collect professional advice about model structure and local parameter inputs. The survey included 15 cardiologists with extensive ICD implant experience from 9 public hospitals in regions with different economic conditions in China, 3 health economic experts, and 2 hospital administrate officers.
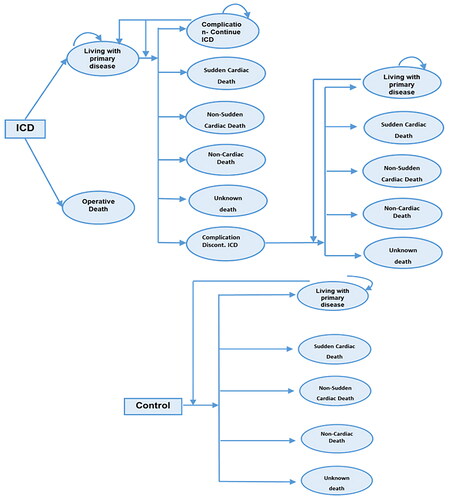
We used a published Markov decision model as a referenceCitation7, adjusted and confirmed it based on literature review, and the consensus of the expert survey (see ). Our model contained several core modifications to the original model: (i) the death categories modelled and the mortality rates were derived from the Improve SCA studyCitation6: sudden cardiac death, non-sudden cardiac death, non-cardiac deaths, unknown death; (ii) the state “well” was renamed as “living with primary disease”, because either ICD therapy or no ICD therapy management cannot completely cure the primary disease; (iii) we used Chinese local cost data and life tables to represent the Chinese context of this study.
Both costs and QALYs were discounted at 5% annually, according to China Guidelines for Pharmacoeconomic Evaluations (2020)Citation8. A lifetime horizon (340 months) was used to capture all relevant costs and impairments of health-related quality of life. The cycle length was 1 month. The model was developed in MicrosoftTM Excel.
Model structure
The 1.5PP patient cohort was simulated and allocated to two different treatment arms: ICD therapy or no ICD therapy, as observed in the Improve SCA studyCitation5. After the assignment of the treatment strategy, patients were run into a consecutive Markov model. Both treatment arms include the following health states: sudden cardiac death, non-sudden cardiac death, non-cardiac deaths, unknown death and living with primary disease. The arm of ICD therapy also includes operative death, ICD-related complications—continued ICD therapy, and ICD-related complications—discontinued ICD therapy. Thus, this model has encompassed all possible outcomes for 1.5PP patients.
At the beginning of every model cycle, patients can stay in the same state or transition to a different state, except for the complication state. For patients who experience ICD complications or inappropriate shock, they enter the complication state and only remain in the state for one cycle, and then transition either to continued ICD therapy or to discontinued ICD therapy, because of the potential impact on patients’ treatment adherence. Patients from the state of continued or discontinued ICD therapy can progress to the health states of living with primary disease or other death states just as patients who did not have ICD complications. After the expert survey, we assume the overall mortality risk of patients who discontinued ICD being the same as whom in the no ICD therapy arm.
For local clinical practice and most of the trials, patients in either ICD therapy or no ICD therapy were prescribed similar drugs. From the expert surveys, the drug prescription was based on clinical guidelines, including beta-blockers, renin-angiotensin-aldosterone system (RAAS) inhibitors, diuretics, spironolactone, and amiodaroneCitation9.
Clinical data
As mentioned previously, the model represents a subset of PP of SCA population who has at least one additional risk factor called 1.5PP population. PP population refers to patients who are at risk for, but not yet had a documented episode of sustained VT, ventricular fibrillation (VF) or resuscitated cardiac arrestCitation5. The additional risk factors associated with 1.5 PP include syncope or pre-syncope, very low LVEF (LVEF < 25%), NSVT, and/or PVCsCitation5. Based on the baseline characteristics of Chinese subgroup of 1.5PP population in the Improve SCA study, the median starting age of the hypothetical cohort is 61.6 years, and it is 76.1% maleCitation10. The mortality rates of 1.5 PP patients are sourced from the Improve SCA study. Other characteristics for this population are included in the study results previously publishedCitation6. Aligned with clinicians, because of the lack of local clinical evidence, the transition probabilities related to ICD treatment are derived from literature and oversea database, and then confirmed with local interviewed experts rather than only from local experts’ estimates.
The finalized clinical data inputs were shown as below in . The operative death in the ICD treatment arm was based on the US National ICD RegistryCitation11; Lead dislodgement or replacement probabilities after initial implant were derived from previous research, claiming that the annual incidence rates of the initial implant lead failure and lead dislodgement were 0.45% and 1.8% respectivelyCitation12,Citation13. According to the REPLACE registry data, after ICD replacement, the combined rate of lead failure and replacement was 1%Citation14. It is assumed that half of the combined rate is from the causes of lead dislodgement, and the other half is associated with lead failure. The Inappropriate shock rate was the weighted average of results from 4 clinical trials, including MADIT RIT, ADVANCE III, PROVIDE and PainFree SSTCitation15–18. The lead infection rate at first year after initial implant and device replacement were 1.22% and 2.16%, respectively, based on administrative claims from a large insurer in the USCitation19. The following lead infection risk doubled after the first year of initial or replacement implantCitation20. Life table for the Chinese general population was used to obtain age-and sex-specific mortality rates and to adjust the non-cardiac mortality ratesCitation21,Citation22.
Table 1. Transition probabilities.
Economic data
Lifetime direct medical expenses were calculated in this study, including procedure costs of initial ICD implant, post-operative follow-up costs, replacement procedure costs and ICD-related complications costs. ICD initial and replacement procedure costs consist of admission, nursing, medication, examination and diagnostic fees, bed charges, device costs and other expenses. Post-operative follow-up costs only have outpatient charges, such as admission, examination and medication fees. The major components of ICD-related complications costs are the expenses of dislodgement, infection and inappropriate shocks, and long-term inpatient and outpatient costs for primary disease treatment in both groups. The estimated direct medical costs and the frequency of resource use related to 1.5PP are mainly based on the results of expert listed surveys, the public tender prices of ICD devices and consumables. The specific cost parameters are presented in .
Table 2. Cost inputs.
Health-related quality-of-life
There is neither local quality-of-life data nor mapping tools for 1.5PP population in mainland China. Utilities for patients in Taiwan province were used in our study because of similar lifestyle and humanistic educationCitation23. The baseline utility for ICD patients and no ICD patients is assumed to be the same. For patients experiencing ICD-related complications, the disutility of approximately 0.096 is assignedCitation24. Quality-of-life data are listed below in .
Table 3. Utilities.
Analysis
This study first analysed the long-term costs and quality-adjusted life years (QALYs) of ICD therapy and no ICD therapy, respectively, and then calculated the incremental cost-effectiveness ratio (ICER) between two strategies. Both undiscounted and discounted results were calculated to best represent the time value of costs and QALYs. One-way deterministic sensitivity analysis and probabilistic sensitivity analysis were both performed. We used one- and three-times the Gross Domestics Product (GDP) per capita in China for 2022 as the willingness-to-pay (WTP) threshold, as recommended by China Guidelines for Pharmacoeconomic Evaluations (2020)Citation8,Citation25.
Results
Base case results
A summary of the results is presented in . The total discounted costs and QALYs gained by the ICD therapy group amount to CNY471,360 and 7.92 QALYs. In comparison, the total discounted costs and QALYs of no ICD therapy group are CNY215,673 and 6.09 QALYs. The ICER of ICD therapy compared to no ICD therapy was 139,652 CNY/QALY. Considering the 2022 three-folded GDP per capita in China (CNY 257,094), ICD therapy for 1.5 PP of SCD is cost-effective.
Table 4. Base case results.
Sensitivity analyses
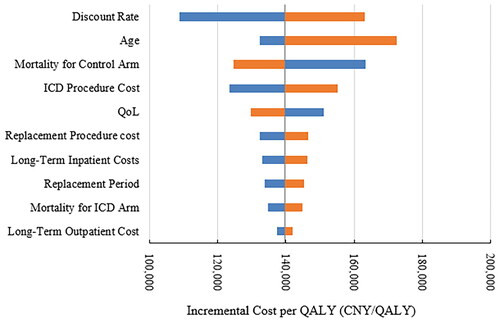
A one-way deterministic sensitivity analysis was conducted to examine the impact of uncertainties in the model parameters. The results presented in the tornado chart below () shows that discount rate, patients’ age at implant, conventional mortality rate, and ICD procedure cost influence the result most significantly. Overall, the ICER stayed under the WTP threshold consistently for all values of the univariate sensitivity analysis.
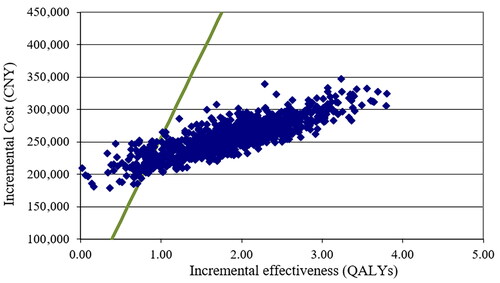
The probabilistic sensitivity analysis (PSA) results were estimated by the Markov model using “Second Order Monte Carlo Simulation”. After 1000 times iterations, and have presented a scatter plot of the cost per QALY results and a cost-effectiveness acceptability curve respectively, showing that 92.1% percent of ICER simulation results fall below the WTP threshold. This PSA result indicates that the cost-effectiveness of ICD therapy as compared with no ICD therapy in 1.5 primary prevention is robust.
Discussion
To our knowledge, this is the first study estimating the economic value of ICD therapy for 1.5PPfrom the perspective of China’s healthcare system. Our study shows that, the ICER of ICD therapy compared to no ICD therapy in 1.5PP is 139,652 CNY/QALY, which is below the willingness to pay threshold, indicating the cost-effectiveness of the ICD therapy. The sensitivity analyses confirmed the robustness of the result.
Previous studies have been mostly performed in the primary prevention population and only three studies are based on 1.5PPCitation23,Citation26,Citation30. The findings of our study are comparable with that of those three studies. Holbrook et al.Citation23 demonstrated that ICD therapy was associated with 10.78 QALYs gained and NT$2,175,478 total costs, whereas no ICD therapy was associated with 7.71 QALYs gained and NT$818,782 total costs; The ICER was 441,153 NT$/QALY. Therefore, ICD therapy should be considered highly cost-effective for 1.5PP population in Taiwan. Higuera et al.Citation26 assessed the cost-effectiveness of ICD therapy versus no ICD therapy in 3 countries in Latin America. The results showed that the incremental costs per QALY saved by ICD therapy are Colombian Pesos COP$46,729,026 in Colombia, Mexican Pesos MXN$246,016 in Mexico, and Uruguayan Pesos UYU$1,213,614 in Uruguay. Another cost-effectiveness study from another Latin American country-Brazil, stated that the ICER of ICD therapy versus no ICD therapy for 1.5PP was R$21,156 per QALYCitation30. Those figures are below the WTP threshold in each country, indicating the ICD therapy being cost-effective. The ICER from our study falls between 1- to 2-folded GDP per capita in China, being similar with those study results from Taiwan and Latin America, and supporting the cost-effectiveness of ICD therapy in China.
SCD is a significant public health issue worldwide and ICD therapy has been recommended as a proven intervention for primary prevention globallyCitation3,Citation4. However, ICD utilization varies among countries. In those developed countries, such as the US, Japan and European countries, the utilization of ICD among eligible candidates could reach 45–52.5%, while the rate falls to 7.7% in Taiwan, and around 12% in AsiaCitation16,Citation27. In China, the number of ICD used is only 4.3 per million, which is extremely low compared to the number from the US (280 per million)Citation28. The reason why ICD therapy is extremely underutilized in China could be comprehensive. A previous study analyzing the reason for the ICD implantation refusal by the patient in developing countries demonstrated that the top three refusal reasons were “patient unable to pay for device”, “patient does not believe in benefit of ICD/CRT-D, and “patient does not want risk associated with implant”, while the Chinese subgroup analysis results kept the same trendCitation29. A study analyzing the ICD utilization in the US also demonstrated that, approximately 95% of the ICD implants occurred in insured patientsCitation28. Those results are similar with what our study gained from expert surveys. Most of our interviewed clinicians mentioned that the major barrier to ICD utilization is patients’ affordability.
In China, the reimbursement for ICD therapy has been raised in some regions recently, such as Shanghai. In the meantime, the patient and clinician education of ICD therapy is also progressing, which is conducive to the use of ICD therapy. However, the reimbursement rate of ICD therapy remains low in most provinces, where only a fraction of the therapy (∼20–50%) can be reimbursed. This makes it burdensome for patients to afford the ICD implant. Therefore, improving the ICD therapy reimbursement rate would largely enhance the therapy utilization.
Given the unbalanced health care resources and fragmented reimbursement financing in different regions, ICD utilization poses a difficult challenge to Chinese health policymakers owing to the limited resources and the large ICD patient population. If clinicians prioritize the use of ICDs for higher-risk patients in whom the efficacy is higher and cost-effectiveness more favorable, the hospital and societal cost will decrease further. As the cost-effectiveness of ICD therapy in 1.5PP population has been well established by our study, it should be a strong reference for the government to make an adjustment to the ICD device reimbursement coverage.
Limitations
There are some limitations in our study. The cost data are mainly from the expert surveys. Although we involved experts from various demographic parts, representing different situations in different parts of China, the estimations from clinicians can still not be precise. However, due to low therapy penetration, the ICD implant cases are scattered, and we cannot collect enough cases in several centers. As this is the best source we can get, we believe our study could be a pilot to further real-world research. In addition, the Improve SCA study we derived the mortality rates from is a non-randomized observational study. We adjusted the mortality for baseline characteristics which may have potential impact in order to reduce the bias.
Conclusions
In China, ICD therapy is cost-effective compared to no ICD therapy in 1.5PP population. The 1.5PP population is a high-value subset of the overall ICD indicated population representing an efficient target for healthcare spending in China.
Transparency
Declaration of financial/other relationships
JF and YS work for Medtronic, the other authors have no potential conflicts of interest.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Previous presentations
The ICD therapy has undergone a provincial alliance volume-based procurement in China and the ICD prices have been adjusted. Given that ICD price is the key factor to procedure cost, we use the latest cost data in this manuscript. Therefore, the results are different from the ISPOR Europe 2023 published abstract.
Ethics approval and consent to participate
The Ethical Committee of the Shanghai Health Development and Research Center approved the study protocol. The writer and research team confirm that this research caused no harm (physical or mental) to any participants. The research process complies with the Declaration of Helsinki. The investigation was conducted after written informed consent was obtained from all participants.
Acknowledgements
Hui Sun and Xin Liu are first co-authors. We would like to thank all the staff involved in the field survey for their excellent research assistance, all authors agreed on the final version of the manuscript to be published.
Additional information
Funding
References
- Shen C, Ge J. Epidemic of cardiovascular disease in China: current perspective and prospects for the future. Circulation. 2018;138(4):342–344. doi: 10.1161/CIRCULATIONAHA.118.033484.
- Shengshou HU, Runlin GAO, Lisheng LIU, et al. Summary of the 2018 report on cardiovascular diseases in China. Chinese Circ J. 2019;34(03):209–220.
- Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36(41):2793–2867. doi: 10.1093/eurheartj/ehv316.
- Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American college of cardiology/American heart association task force on practice guidelines (writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. [published correction appears in Circulation. 2009 Aug 4; 120(5):e34-5]. Circulation. 2008;117(21):e350–e408.
- Zhang S, Singh B, Rodriguez DA, et al. Improve the prevention of sudden cardiac arrest in emerging countries: the improve SCA clinical study design. Europace. 2015;17(11):1720–1726. doi: 10.1093/europace/euv103.
- Zhang S, Ching CK, Huang D, et al. Utilization of implantable cardioverter-defibrillators for the prevention of sudden cardiac death in emerging countries: improve SCA clinical trial. Heart Rhythm. 2020;17(3):468–475. doi: 10.1016/j.hrthm.2019.09.023.
- Cowie MR, Marshall D, Drummond M, et al. Lifetime cost-effectiveness of prophylactic implantation of a cardioverter defibrillator in patients with reduced left ventricular systolic function: results of Markov modelling in a European population. Europace. 2009;11(6):716–726. doi: 10.1093/europace/eup068.
- Wang LT, Peng LB, Peng Y, et al. Comparative analysis between 2020 version and 2011 version on China guidelines for pharmacoeconomic evaluation. China J Pharm Econ. 2021;16(03):5–8 + 15.
- Guidelines for rational use of heart failure medications. 2nd ed. Chinese J Front Med Sci. 2019;11(07):1–78.
- Liang Y, Zhang S, Zhang Z, et al. Implantable cardioverter defibrillators for sudden cardiac death prevention in China: a regional analysis from the improve SCA clinical trial. Int J Heart Rhythm. 2020;5(1):1. doi: 10.4103/IJHR.IJHR_7_20.
- Hammill SC, Kremers MS, Stevenson LW, et al. Review of the registry’s fourth year, incorporating lead data and pediatric ICD procedures, and use as a national performance measure. Heart Rhythm. 2010;7(9):1340–1345. doi: 10.1016/j.hrthm.2010.07.015.
- Ghani A, Delnoy PP, Ramdat Misier AR, et al. Incidence of lead dislodgement, malfunction and perforation during the first year following device implantation. Neth Heart J. 2014;22(6):286–291. doi: 10.1007/s12471-014-0556-6.
- Providência R, Kramer DB, Pimenta D, et al. Transvenous implantable cardioverter-defibrillator (ICD) lead performance: a meta-analysis of observational studies. J Am Heart Assoc. 2015;4(11):e002418.
- Poole JE, Gleva MJ, Mela T, et al. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation. 2010;122(16):1553–1561. doi: 10.1161/CIRCULATIONAHA.110.976076.
- Gasparini M, Proclemer A, Klersy C, et al. Effect of long-detection interval vs standard-detection interval for implantable cardioverter-defibrillators on antitachycardia pacing and shock delivery: the ADVANCE III randomized clinical trial. JAMA. 2013;309(18):1903–1911. [published correction appears in JAMA. 2013 Jun 26;309(24):2552]. doi: 10.1001/jama.2013.4598.
- Auricchio A, Schloss EJ, Kurita T, et al. Low inappropriate shock rates in patients with single- and dual/triple-chamber implantable cardioverter-defibrillators using a novel suite of detection algorithms: pain Free SST trial primary results. Heart Rhythm. 2015;12(5):926–936. doi: 10.1016/j.hrthm.2015.01.017.
- Saeed M, Hanna I, Robotis D, et al. Programming implantable cardioverter-defibrillators in patients with primary prevention indication to prolong time to first shock: results from the PROVIDE study. J Cardiovasc Electrophysiol. 2014;25(1):52–59. doi: 10.1111/jce.12273.
- Moss AJ, Schuger C, Beck CA, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012;367(24):2275–2283. doi: 10.1056/NEJMoa1211107.
- Eby EL, Bengtson LGS, Johnson MP, et al. Economic impact of cardiac implantable electronic device infections: cost analysis at one year in a large U.S. health insurer. J Med Econ. 2020;23(7):698–705. doi: 10.1080/13696998.2020.1751649.
- Hussein AA, Baghdy Y, Wazni OM, et al. Microbiology of cardiac implantable electronic device infections. JACC Clin Electrophysiol. 2016;2(4):498–505. doi: 10.1016/j.jacep.2016.01.019.
- China Statistical Yearbook. 2021. http://www.stats.gov.cn/sj/ndsj/2021/indexch.htm.
- Li H, Natale A, Zhu W, et al. Causes and consequences of discontinuation of the implantable cardioverter-defibrillator therapy in non-terminally ill patients. Am J Cardiol. 1998;81(10):1203–1205. doi: 10.1016/s0002-9149(98)00090-3.
- Holbrook R, Higuera L, Wherry K, et al. Implantable cardioverter defibrillator therapy is cost effective for primary prevention patients in Taiwan: an analysis from the improve SCA trial. PLoS One. 2020;15(11):e0241697. doi: 10.1371/journal.pone.0241697.
- Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter-defibrillators. N Engl J Med. 2005;353(14):1471–1480. doi: 10.1056/NEJMsa051989.
- National Bureau of Statistics of China. Statistical communiqué of the People's Republic of China on the 2022 National Economic and Social Development. 2022. http://www.stats.gov.cn/sj/zxfb/202302/t20230228_1919011.html.
- Higuera L, Holbrook R, Wherry K, et al. Comparison of cost-effectiveness of implantable cardioverter defibrillator therapy in patients for primary prevention in Latin America: an analysis using the improve SCA study. J Med Econ. 2021;24(1):173–180. doi: 10.1080/13696998.2021.1877451.
- Younis A, Wilkoff BL. Implantable cardioverter-defibrillator for primary prevention in Asia. JACC Asia. 2023;3(3):321–334. doi: 10.1016/j.jacasi.2022.11.014.
- Patel NJ, Edla S, Deshmukh A, et al. Gender, racial, and health insurance differences in the trend of implantable cardioverter-defibrillator (ICD) utilization: a United States experience over the last decade. Clin Cardiol. 2016;39(2):63–71. doi: 10.1002/clc.22496.
- Singh B, Zhang S, Ching CK, et al. Improving the utilization of implantable cardioverter defibrillators for sudden cardiac arrest prevention (improve SCA) in developing countries: clinical characteristics and reasons for implantation refusal. Pacing Clin Electrophysiol. 2018;41(12):1619–1626. doi: 10.1111/pace.13526.
- Wherry K, Holbrook R, Higuera L, et al. Cost-effectiveness analysis of implantable cardioverter defibrillator therapy for primary prevention patients with additional risk factors in Brazil. Int J Cardiovasc Sci. 2021;34(6):692–701.