Abstract
Background
Accurate identification of suicidal crisis presentations to emergency departments (EDs) can lead to timely mental health support, improve patient experience, and support evaluations of suicide prevention initiatives. Poor coding practices within EDs are preventing appropriate patient care. Aims of the study are (1) examine the current suicide-related coding practices, (2) identify the factors that contribute to staff decision-making and patients receiving the incorrect code or no code.
Method
A mixed-methods study was conducted. Quantitative data were collated from six EDs across Merseyside and Cheshire, United Kingdom from 2019 to 2021. Attendances were analyzed if they had a presenting complaint, chief complaint, or primary diagnosis code related to suicidal crisis, suicidal ideation, self-harm or suicide attempt. Semi-structured interviews were conducted with staff holding various ED positions (n = 23).
Results
A total of 15,411 suicidal crisis and self-harm presentations were analyzed. Of these, 21.8% were coded as ‘depressive disorder’ and 3.8% as ‘anxiety disorder’. Absence of an appropriate suicidal crisis code resulted in staff coding presentations as ‘no abnormality detected’ (23.6%) or leaving the code blank (18.4%). The use of other physical injury codes such as ‘wound forearm’, ‘head injury’ were common. Qualitative analyses elucidated potential causes of inappropriate coding, such as resource constraints and problems with the recording process.
Conclusion
People attending EDs in suicidal crisis were not given a code that represented the chief presentation. Improved ED coding practices related to suicidal crisis could result in considerable benefits for patients and more effective targeting of resources and interventions.
INTRODUCTION
Suicidal crisis is a spectrum ranging from thoughts of death with no intent or plan to act upon those thoughts, to specific suicidal thoughts with an intention and plan to die by suicide (Saini et al., Citation2021). It has been shown that the more pervasive the suicidal crisis, the more likely the individual is to engage in self-harm or attempt suicide (Kienhorst, Citation1995). It is estimated that 9% of the population worldwide will experience suicidal thoughts at some point, 30% of whom will go on to make a suicide attempt (Nock et al., Citation2008). It is imperative to intervene and support at the earliest opportunity to reduce individual distress.
The recording of suicidal crisis in emergency departments (EDs) is inconsistent and lacks precision, which can impede appropriate referral and follow-up (McCarthy et al., Citation2021). EDs are often the first point of contact for people experiencing suicide-related distress (Perera et al., Citation2018) and while data are available on attendances for self-harm, no comparable data exist for suicidal crisis in the United Kingdom (UK). Data available from the Northern Ireland Registry of Self-Harm, however, has reported a total of 14,695 presentations to hospital for suicidal ideation from April 2014 to March 2019 (Griffin et al., Citation2020). Poor data capture, in the UK in particular, makes it more difficult to provide adequate care.
High healthcare usage in the period preceding suicide or suicide attempts suggests that healthcare professionals have an opportunity to identify and intervene (Ross et al., Citation2023). In the year prior to suicide, 25% of people have been in contact with mental health services, with 40% having been to the ED (Ahmedani et al., Citation2019). Furthermore, examination of contact with primary and secondary care prior to suicide in Wales from 2000-2017, revealed that in the month prior to suicide 16.6% of cases had an ED contact, compared with 5.5% of controls (John et al., Citation2020). Little research, however, has examined ED coding practices for patients in suicidal crisis. This is surprising given that the National Institute for Health and Care Excellent (NICE) clinical guidelines in England now include best practice for self-harm patients, which covers assessment, management and preventing recurrence (National Institute for Health and Clinical Excellence, Citation2022). Despite the growing recognition that self-harm is a major public health issue (Islam et al., Citation2022; Knipe et al., Citation2022), identification of presentations from ED datasets are difficult. In England, more than 200,000 self-harm presentations are recorded in EDs annually (Hawton et al., Citation2007). However, data underestimates suicide-related attendances by as much as 60% (Clements et al., Citation2016), due to inaccurate coding practices. Clements and colleagues, however, did not investigate the factors that underpin inaccurate coding by staff, which is a gap we aim to address in the present study using a mixed-methods approach.
Every ED attendance is recorded in a database – electronic health records (EHRs) represent a pivotal shift in healthcare documentation by providing a system to store and manage patient health information. Certain data for example demographics, admission information and diagnoses, are routinely collected within these records, in which this data can be extracted, collated and analyzed. Across EDs, International Classification of Diseases (ICD-10) and Systemized Nomenclature of Medicine – Clinical Terms (SNOMED CT) codes have been used to capture presentations, which include diagnostic codes related to ‘suicide attempt (event)’ and ‘suicidal thoughts’. However, in practice, the code for suicidal ideation is inconsistently applied, potentially due to unclear guidelines (Anderson et al., Citation2015). There is conflicting evidence regarding what is used and this makes it difficult to obtain accurate rates of suicidal crisis (Sveticic et al., Citation2020). Furthermore, staff often receive little or no training related to coding presentations and additional contextual factors can hinder their decision-making (McCarthy et al., Citation2023a). To date, no research has collated data from multiple ED sites, nor explored the reasons behind inaccurate and inconsistent coding for suicidal crisis presentations.
Accurate documentation of suicidal crisis is critical to understanding future risk and for improving services. A better understanding of patient presentations could have important implications for patient experiences, which in turn may reduce repeat presentations by ensuring appropriate care is received. More accurate data should also facilitate better decision-making at the level of service provision and policy (e.g., service design, resource allocation). Therefore, the current study aims to investigate:
The current suicide-related coding practices among EDs in Cheshire and Merseyside, UK – identifying the most common codes used and the extent of missing data.
The factors that contribute to staff decision-making and patients receiving the incorrect code or no code.
METHODS
Design
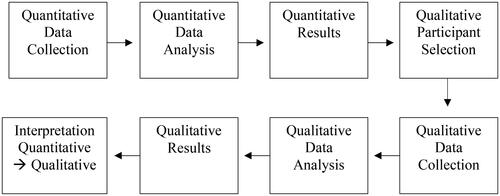
A mixed-methods explanatory sequential study design was adopted (Creswell & Clark, Citation2017). This is a two-phased mixed-methods design which starts with the collection and analysis of quantitative data, followed by the collection and analysis of qualitative data to build upon the initial findings (see ).
Sample
Quantitative data was obtained from a secondary dataset of 15,411 suicidal crisis presentations across six EDs in Merseyside and Cheshire, UK. Qualitative data was gathered through semi-structured interviews (n = 23) with staff currently working in an ED setting. Staff were recruited from a range of roles along the clinical pathway: e.g., ED receptionist, triage nurse, ED doctors, mental health nursing staff and consultant in liaison psychiatry.
Setting
The UK has a universal healthcare system (the National Health Service, NHS), in which EDs represent a key setting for 24/7 urgent and emergency care. Most patients self-present to EDs, although some may have had contact with services beforehand (e.g., ambulance services or medical helpline). Upon arrival, a person will present to reception and ED administrative staff will ask about the presenting problem, choosing an appropriate initial complaint code to best describe the reason for visit. In accordance with the Emergency Care Data Set (ECDS) patients will be assigned a score of 1 to 5 to highlight the severity of a patient’s condition and urgency with which they need to be seen and assessed by a clinician. Triage is part of the pathway used to prioritize patient treatment so that the most acutely unwell patients are seen first depending on the individual needs and clinician assessment, a person can be admitted into hospital to manage and treat physical injuries or referred to liaison psychiatry for a mental health psychosocial assessment.
Measures
Quantitative Data
Quantitative data were extracted from records within six EDs in Merseyside and Cheshire, UK. Quantitative coding data was extracted for all suicidal crisis, suicidal ideation, self-harm and suicide attempt presentations from the 1st January 2019 to 31st December 2021. Data were included if the presentation included a suicide-related code as part of the chief complaint, presenting complaint, primary diagnosis code or secondary diagnosis code. Supplementary Box 1 includes an example search strategy from one ED.
Quantitative data were extracted on attendees’ demographic information (age, sex, ethnicity), attendance information (arrival mode, date and time), coding information and outcome (left before assessment, referral to liaison psychiatry). Different data and variables were available across the participating EDs, for example some EDs did not have outcome data available for analysis (see Table S1 for comparison across sites).
Qualitative Interviews
Qualitative semi-structured interviews (n = 23) were conducted as part of a wider study, where participants were asked about their roles, training, service and staff availability, and factors influencing decision-making (see Table S2 for example questions). Further information on the study method and analysis is available in McCarthy et al. (Citation2023b). For the purpose of this paper, only data relating to coding practices and decision-making were included in the analysis.
Participants permission to audio-record the interview was obtained. Eight interviews were conducted online via Microsoft Teams and 15 were conducted in-person onsite. Onsite recruitment was conducted opportunistically and increased the representation of different staff; for example, ED receptionists have typically been underrepresented in ED research (Van Sleeuwen, Citation2014). Thirteen participants identified as female and 10 as male. Interviews varied in length from 14 to 65 minutes.
Data Analysis
Quantitative
Quantitative data analysis was conducted using Statistical Package for Social Sciences (SPSS) software version 27. Presenting complaint and chief complaint were merged together for the analysis due to inconsistent variable labeling across the participating EDs. We have now named this ‘initial complaint’ for the purpose of this study. Due to the variation of data availability for secondary diagnosis codes across EDs (see Table S1), only primary diagnosis codes have been used in the analysis. Descriptive analyses were conducted to examine the primary diagnosis codes received when the initial complaint was a suicide-related code. Frequencies and percentages were examined. Percentages presented refer to ‘valid cases’, i.e., cases for which the relevant information was available.
Qualitative
Qualitative data were analyzed using thematic analysis (Clarke & Braun, Citation2017). One author (MM) hand-coded the data and discussed codes with the research team. The Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist was used (Booth et al., Citation2014). The purpose of qualitative work was to provide an explanatory role supporting the quantitative findings. A hybrid approach was used in which the initial coding framework was based on the quantitative findings and coded according to them; a deductive approach was also used to allow for unanticipated codes. Relevant qualitative data is thus presented alongside the quantitative data, in line with the explanatory mixed-methods design.
Public and Patient Involvement (PPI)
The team consulted with people with lived experience of attending EDs in suicidal crisis to inform the design of the study on a tri-annual basis. The PPI group advised on the development of information sheets/interview schedule, and wording of questions. The study steering committee, comprising of a range of professionals working within an ED setting, offered invaluable guidance throughout the project. As stated by The National Institute for Health Research (National Institute for Health Research [NIHR], 2019) as good practice at least two members of the PPI group also attended meetings with the steering committee.
Ethical Approval
Ethical approval was granted by NHS Health Research Authority, Integrated Research Application System (IRAS ID: 298407). Research passports were obtained for each individual ED from the general hospital trust. Verbal consent was obtained, witnessed and formally audio-recorded from all participants for the qualitative interviews.
RESULTS
Characteristics of the Quantitative Sample
During the study period from 2019 to 2021, a total of 15,411 suicidal crisis presentations were examined across six EDs in Cheshire and Merseyside, UK. Characteristics of the quantitative sample are presented in . Just over half of the presentations were made by individuals who identify as female (55.1%), just under half as male (44.8%) and 0.1% identified as non-binary; although this perhaps reflects issues of inclusivity in the way gender is discussed and coded in the different EDs. The mean age of people presenting was 32.37 years (SD = 15.09).
TABLE 1. Characteristics of sample presenting to the six EDs examined for suicidal crisis.
The following section presents both quantitative and qualitative findings. The current coding practices for suicidal crisis are presented using quantitative data and are presented in . The factors that contribute to patients receiving the incorrect or no code are then discussed using the qualitative findings.
TABLE 2. Initial complaints by patients and how they were coded at each Emergency department.
Across the participating six EDs, the common primary diagnosis codes include ‘other’ which was used for 40.3% of suicidal crisis attendances, ‘depressive disorder’ (21.8%), ‘suicidal’ (12.4%), and ‘self-harm’ (7.4%). ‘Laceration’ was used less frequently across the sites, accounting for 1.3% of attendances (see for further information).
Suicidal Crisis Coded as ‘Anxiety Disorder’ and ‘Depressive Disorder’
Across all the six EDs examined, 581 suicidal crisis attendances were coded as ‘anxiety disorder’ (3.8%) and 3,358 as ‘depressive disorder’ (21.8%). The primary diagnosis code ‘anxiety disorder’ was used less across all EDs, ranging from 1.3% of suicidal crisis attendances in ED2 to 8.6% in ED6. The ‘depressive disorder’ primary diagnosis code was used most frequently from 15.7% of attendances in ED1 to 38.5% in ED6.
Interviews with ED staff elaborated on some of the reasons behind why the primary diagnosis codes of ‘anxiety disorder’ and ‘depressive disorder’ are consistently being used across sites in relation to suicidal presentations.
“We’re limited with the coding that we can have. So, I think there’s this depressive disorder, anxiety disorder, psychotic disorder, and then a couple of others. Now, what you can do is, code formally the depressive disorder, but then in the actual discharge letter, you can then put ‘with suicidal ideation’.” (02: Consultant in Emergency Medicine).
This quotation illustrates the way codes can conceal the complexity of the real nature of the presentation. Further to this, staff discussed how suicidal thoughts may be viewed as a symptom and, due to the medical approach adopted by ED staff, the mental health difficulty is pathologized, resulting in inaccurate coding for suicidal crisis:
“It’s also a thing of we pathologise everything. And I'm just wondering whether we don’t actually pathologise suicidal crisis because it’s more of a behaviour and symptom. So, we pathologise the mental disorder first and code as depression.” (05: Advanced Nurse Practitioner).
‘No Abnormality Detected’
The primary diagnosis code of ‘no abnormality detected’ was used across all EDs, with 23.6% of all suicidal crisis attendances receiving the code (0.2% in ED1 to 13.2% in ED6). It is possible that the use of ‘no abnormality detected’ is related to systematic differences and the sharing of an approach amongst one staffing group within certain EDs. Although uncommon within ED1, medical staff within ED6 discussed using ‘no abnormality detected’ in relation to suicidal crisis attendances frequently.
In interviews, 12/23 staff reported that they use the code ‘no abnormality detected’ in relation to suicidal presentations. Staff discussed the reasons for this in relation to the absence of an appropriate or relevant suicidal crisis code, leaving staff with no other option:
“We would usually just put ‘no abnormality detected’ or just leave the code blank and not put anything. There isn’t another way for us to go about or code suicidal crisis.” (06: Triage Nurse).
“I don’t think you can code self-harm; you can put like ‘laceration’. Most of the time what you end up doing is putting ‘no abnormality detected’, and then just writing what’s happened, which means it’s just gets coded as no abnormality.” (15: ED Doctor).
These quotations where staff use language including ‘just put’ or ‘end up’ encapsulates the problem which seems to indicate that the coding options currently available to staff are unsatisfactory and that much time is spent deliberating over the ‘least worst’ coding option.
Other Physical Injury Codes for Suicidal Behaviors
Across all EDs the use of ‘other physical injury’ primary diagnosis codes was common. Such codes included ‘head injury’ and ‘wound forearm’. The use of other physical injury codes was used from 29.8% in ED1 to 55.2% in EDs 4 and 5.
When asked to elaborate on the use of physical injury codes, staff often discussed this in relation to self-harm. Staff considered the medical treatment aspect of the attendance and often coded according to the physical injury at hand. For example, “we would tend to just put ‘laceration’ for self-harm presentations” (014: ED Receptionist).
Further, staff often considered the implications of using physical injury codes for suicidal crisis presentations. It was noted that the inaccurate coding practices for suicide-related presentation result in the underestimation of such presentations: “…underestimates mental health attendances by about 40-50%…” (02: Consultant in Emergency Medicine).
Issues Related to Missing Data
Across all six EDs, the primary diagnosis code was left blank on 18.4% of occasions. Missing data was highest at ED1 (13.6%) and lowest at ED6 (0.2%).
During the interviews, staff often noted the contextual factors that impede accurate, resulting in a high level of missing data. In the fast-paced environment, ED staff faced pressures that impacted on their ability to accurately code presentations and their decision-making practices. Limited time, competing demands and inadequate training in suicide documentation often resulted in staff leaving the code blank:
“Coding depends upon the time constraint, time to triage, staff often don’t have time to complete the administrative tasks due to the volume of presentations”. (09: Consultant in Emergency Medicine).
“Well, there’s not only multiple systems being used across the country, you know, IT systems, but also different ones within the same hospital. The fact that IT systems still don’t speak to each other, the fact that the sharing of information is so sporadic, the fact that triage will code it on one system, and then the mental health team will use another.” (11: Consultant in Emergency Medicine).
“The new system is just really difficult to use and maybe that’s something to improve is actually make the systems talk to us a bit better about diagnosis and coding. It’s kind of tucked away somewhere., so it would be good to have some sort of prompt to help us.” (05: Advanced Nurse Practitioner).
DISCUSSION
Summary of Main Findings
Inaccurate and inconsistent coding of suicidal crisis attendances was evident both within and between EDs. A large proportion of suicidal crisis presentations were coded as ‘depressive disorder’, ‘anxiety disorder’, ‘no abnormality detected’ or left blank. The factors that contribute to people receiving the incorrect or no code was further explored in interviews. Staff discussed the impact of contextual factors, such as lack of time and competing demands, which resulted codes being left blank. Hospital electronic coding systems were described as “difficult to use” and staff reported how they would benefit from ongoing and up-to-date training on suicidal crisis coding practices and hospital systems.
The current study provides novel insights into suicidal crisis ED coding practices by utilizing a large sample, collating data across multiple UK NHS Foundation Trusts, and using a mixed-methods approach. To date, only one study has previously examined ED suicidal crisis coding in the UK, and this only focused on children and young people. Ashworth et al. (Citation2022) extracted patient data across 240 clinical records at one ED and reported ‘social/social problems’ to be the most commonly used code (38%) for suicidal crisis; similarly noting inaccurate reporting of suicidal crisis. Poor ED coding practices hinder the ability to accurately identify individuals at risk (McCarthy et al., Citation2021); thus, the present results suggest people are not receiving appropriate follow-up care. This can have significant implications for patient treatment and support, such as ensuring people receive a psychosocial assessment. For example, when the Mental Health Triage scale was implemented in Irish EDs, the triage categories assigned for self-harm presentations was significantly safer than when the scale was not used (Tanner et al., Citation2014); highlighting positive implications accurate identification can have on patient safety and care. Due to the novelty of the current study and limited research in this area, future research explicitly examining coding practices across EDs in the UK is needed to get a better picture of coding practice at a national level.
Given the coding issues and variation identified across multiple ED sites in the present study, it is vital that findings are used to inform more consistent practices (i.e., training and clear guidelines) to help ensure individuals are receiving the care they need. Implementing a standardized code for suicidal crisis is urgently needed to ensure accurate and timely data collection. This could be achieved by piloting a new ‘suicidal crisis’ code within a small number of EDs to ensure the code is being implemented appropriately. It would also be beneficial to develop clear and standardized coding guidelines to support staff responsible for coding presentations and ensure regular and up-to-date training is available.
The inaccurate coding practices for suicide-related presentations identified in the current study are consistent with studies conducted in America (Randall et al., Citation2017) and Australia (Howell et al., Citation2013; Sveticic et al., Citation2020). Research on ED coding practices for suicidal crisis presentations is scarce and has not been systemically examined in the UK previously for adult presentations. Furthermore, previous research has failed to investigate decision-making from the perspective of relevant staff across multiple hospitals, providing crucial insights into why coding practices are inconsistent. Providing focused coding training for administrative, medical and mental health staff that is supported by ongoing clinical supervision would ensure consistency and improved accuracy leading to better data quality. EDs would also benefit from a continuous feedback loop that integrates research and practice. Collaborative work with academics, researchers, ED staff, patients and wider stakeholders would help identify issues with coding, address them promptly and facilitate ongoing training and process enhancements.
A unique component of the current study was the inclusion of qualitative interviews to further explore the reasons for inaccurate suicidal crisis coding among ED staff, an issue which has received limited attention within the current evidence base. The language used by participants (i.e., “just put”) reveals the subjective experience of dealing with a less than fit for purpose system. In combination with this, it is important to recognize the additional time pressures and resource limitation staff face, which impact on coding practices. For example, Downey & Zun (Citation2007) reported that the high number of presentations coupled with the need to meet certain ED targets impacted the provision of timely and high-quality patient care. This information can help to inform the implementation of efficient, clinically relevant and user-friendly electronic health record systems that facilitate accurate and complete documentation of patient encounters.
Strengths and Limitations
To our knowledge, this is the first study to examine adult suicidal crisis coding practices across multiple UK NHS Foundation Trusts, using a mixed-methods approach. A major strength is the inclusion of six EDs, given the majority of past work has been limited to one ED. The inclusion of the qualitative interviews also provides unique insights into the reasoning behind inconsistent coding, which is further strengthened by the recruitment of a wide range of staff, including administrative, medical, and mental health staff, some of whom have been excluded from past studies.
One limitation of this study is the use of hospital-based records as the data source, which, as our study suggests, may be inaccurate. Indeed, despite using a wide range of search terms, it is likely the true number of presentations is underestimated in our dataset. Previous research has highlighted methodological limitations in the use of EHRs, including variations in accuracy resulting in suicide-related presentations being missing and underestimated (McCarthy et al., Citation2021; Stanley et al., Citation2017). Furthermore, although the transcripts and qualitative themes were discussed with all authors, only the primary author was responsible for the coding of transcripts, which may limit the rigor of the findings (Lincoln et al., Citation2011).
Conclusion
The current study provides novel insights into current suicidal crisis coding practices across multiple UK EDs and is the first study to examine why patient coding is inaccurate and variable. Improving recording would enable better use of routinely collected data for research of suicidal crisis whether as dependent or independent variable (McGuckin et al., Citation2022). Currently, there is no evidence-based clinical guidelines for suicidal crisis ED presentations, as there are for self-harm. It is important to prioritize training and education for all healthcare professionals to improve confidence and knowledge of not only suicidal crisis care, but also how to record such presentations on hospital systems. By implementing a standardized code for suicidal crisis within EDs, NHS coding systems and data recording can be improved, leading to better accuracy, decision-making, research, and resource allocation.
AUTHOR NOTES
Molly McCarthy, Pooja Saini, Emma Ashworth and Jason McIntyre, Liverpool John Moores University, Liverpool, United Kingdom of Great Britain and Northern Ireland. Rajan Nathan, Cheshire and Wirral Partnership NHS Foundation Trust, Chester, United Kingdom of Great Britain and Northern Ireland.
Supplemental Material
Download MS Word (25.6 KB)DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
Additional information
Funding
REFERENCES
- Ahmedani, B. K., Westphal, J., Autio, K., Elsiss, F., Peterson, E. L., Beck, A., Waitzfelder, B. E., Rossom, R. C., Owen-Smith, A. A., Lynch, F., Lu, C. Y., Frank, C., Prabhakar, D., Braciszewski, J. M., Miller-Matero, L. R., Yeh, H.-H., Hu, Y., Doshi, R., Waring, S. C., & Simon, G. E. (2019). Variation in patterns of health care before suicide: A population case-control study. Preventive Medicine, 127, 105796. https://doi.org/10.1016/j.ypmed.2019.105796
- Anderson, H. D., Pace, W. D., Brandt, E., Nielsen, R. D., Allen, R. R., Libby, A. M., West, D. R., & Valuck, R. J. (2015). Monitoring suicidal patients in primary care using electronic health records. Journal of the American Board of Family Medicine: JABFM, 28(1), 65–71. https://doi.org/10.3122/jabfm.2015.01.140181
- Ashworth, E., Provazza, S., McCarthy, M., & Saini, P. (2022). Children and young people presenting in a pediatric emergency department in North-West England in suicidal crisis: An exploratory case series study. Frontiers in Psychiatry, 13, 892939. https://doi.org/10.3389/fpsyt.2022.892939
- Booth, A., Hannes, K., Harden, A., Noyes, J., Harris, J., & Tong, A. (2014). COREQ (consolidated criteria for reporting qualitative studies). Guidelines for Reporting Health Research: A User’s Manual. New York, USA: JKohn Wiley & sons, 2014 (eds), 214–226.
- Clarke, V., & Braun, V. (2017). Thematic analysis. The Journal of Positive Psychology, 12(3), 297–298. https://doi.org/10.1080/17439760.2016.1262613
- Clements, C., Turnbull, P., Hawton, K., Geulayov, G., Waters, K., Ness, J., Townsend, E., Khundakar, K., & Kapur, N. (2016). Rates of self-harm presenting to general hospitals: A comparison of data from the Multicentre Study of Self-Harm in England and Hospital Episode Statistics. BMJ Open, 6(2), e009749. https://doi.org/10.1136/bmjopen-2015-009749
- Creswell, J. W., & Clark, V. L. P. (2017). Designing and conducting mixed methods research. Sage publications.
- Downey, L. V. A., & Zun, L. S. (2007). Determinates of throughput times in the emergency department. Journal of Health Management, 9(1), 51–58. https://doi.org/10.1177/097206340700900103
- Griffin, E., Kavalidou, K., Bonner, B., O'Hagan, D., & Corcoran, P. (2020). Risk of repetition and subsequent self-harm following presentation to hospital with suicidal ideation: A longitudinal registry study. EClinicalMedicine, 23, 100378. https://doi.org/10.1016/j.eclinm.2020.100378
- Hawton, K., Bergen, H., Casey, D., Simkin, S., Palmer, B., Cooper, J., Kapur, N., Horrocks, J., House, A., Lilley, R., Noble, R., & Owens, D. (2007). Self-harm in England: A tale of three cities: Multicentre study of self-harm. Social Psychiatry and Psychiatric Epidemiology, 42(7), 513–521. https://doi.org/10.1007/s00127-007-0199-7
- Howell, S. C., Wills, R. A., & Johnston, T. C. (2013). Should diagnosis codes from emergency department data be used for case selection for emergency department key performance indicators? Australian Health Review: A Publication of the Australian Hospital Association, 38(1), 38–43. https://doi.org/10.1071/AH13026
- Islam, M. I., Yunus, F. M., Kabir, E., & Khanam, R. (2022). Evaluating risk and protective factors for suicidality and self-harm in Australian adolescents with traditional bullying and cyberbullying victimizations. American Journal of Health Promotion: AJHP, 36(1), 73–83. https://doi.org/10.1177/08901171211034105
- John, A., DelPozo-Banos, M., Gunnell, D., Dennis, M., Scourfield, J., Ford, D. V., Kapur, N., & Lloyd, K. (2020). Contacts with primary and secondary healthcare prior to suicide: Case–control whole-population-based study using person-level linked routine data in Wales, UK, 2000–2017. The British Journal of Psychiatry: The Journal of Mental Science, 217(6), 717–724. https://doi.org/10.1192/bjp.2020.137
- Kienhorst, I. C. (1995). Crisis intervention and a suicidal crisis in adolescents. Crisis, 16(4), 154–156; 183. https://doi.org/10.1027/0227-5910.16.4.154
- Knipe, D., Padmanathan, P., Newton-Howes, G., Chan, L. F., & Kapur, N. (2022). Suicide and self-harm. Lancet (London, England), 399(10338), 1903–1916. https://doi.org/10.1016/S0140-6736(22)00173-8
- Lincoln, Y. S., Lynham, S. A., & Guba, E. G. (2011). Paradigmatic controversies, contradictions, and emerging confluences, revisited. The Sage Handbook of Qualitative Research, 4(2), 97–128.
- McCarthy, M., McIntyre, J., Nathan, R., & Saini, P. (2023a). Factors influencing emergency department staff decision-making for people attending in suicidal crisis: A systematic review. Archives of Suicide Research: Official Journal of the International Academy for Suicide Research, 28(1), 35–49. https://doi.org/10.1080/13811118.2023.2173113
- McCarthy, M., McIntyre, J., Nathan, R., Ashworth, E., & Saini, P. (2023b). Staff perspectives of emergency department pathways for people attending in suicidal crisis: A qualitative study. Journal of Psychiatric and Mental Health Nursing, 0: 1–12. https://doi.org/10.1111/jpm.12991
- McCarthy, M., Saini, P., Nathan, R., & McIntyre, J. (2021). Improve coding practices for patients in suicidal crisis. BMJ (Clinical Research ed.), 375, n2480. https://doi.org/10.1136/bmj.n2480
- McGuckin, T., Crick, K., Myroniuk, T. W., Setchell, B., Yeung, R. O., & Campbell-Scherer, D. (2022). Understanding challenges of using routinely collected health data to address clinical care gaps: A case study in Alberta, Canada. BMJ Open Quality, 11(1), e001491. https://doi.org/10.1136/bmjoq-2021-001491
- National Institute for Health and Clinical Excellence. (2022). Self-harm: Assessment, management and preventing recurrence. https://www.nice.%20org.uk/guidance/ng225/resources/selfharm-assessment-management-and-%20preventing-recurrence-pdf-66143837346757
- National Institute for Health Research [NIHR]. (2019). National standards for public involvement. https://doi.org/10.1111/hex.13000
- Nock, M. K., Borges, G., Bromet, E. J., Alonso, J., Angermeyer, M., Beautrais, A., Bruffaerts, R., Chiu, W. T., de Girolamo, G., Gluzman, S., de Graaf, R., Gureje, O., Haro, J. M., Huang, Y., Karam, E., Kessler, R. C., Lepine, J. P., Levinson, D., Medina-Mora, M. E., … Williams, D. (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry: The Journal of Mental Science, 192(2), 98–105. https://doi.org/10.1192/bjp.bp.107.040113
- Perera, J., Wand, T., Bein, K. J., Chalkley, D., Ivers, R., Steinbeck, K. S., Shields, R., & Dinh, M. M. (2018). Presentations to NSW emergency departments with self‐harm, suicidal ideation, or intentional poisoning, 2010–2014. The Medical Journal of Australia, 208(8), 348–353. https://doi.org/10.5694/mja17.00589
- Randall, J. R., Roos, L. L., Lix, L. M., Katz, L. Y., & Bolton, J. M. (2017). Emergency department and inpatient coding for self‐harm and suicide attempts: Validation using clinician assessment data. International Journal of Methods in Psychiatric Research, 26(3), e1559. https://doi.org/10.1002/mpr.1559
- Ross, E., Murphy, S., O'Hagan, D., Maguire, A., & O'Reilly, D. (2023). Emergency department presentations with suicide and self-harm ideation: A missed opportunity for intervention? Epidemiology and Psychiatric Sciences, 32, e24. https://doi.org/10.1017/S2045796023000203
- Saini, P., Hunt, A., Taylor, P., Mills, C., Clements, C., Mulholland, H., Kullu, C., Hann, M., Duarte, R., Mattocks, F., Guthrie, E., & Gabbay, M. (2021). Community Outpatient Psychotherapy Engagement Service for Self-harm (COPESS): a feasibility trial protocol. Pilot and Feasibility Studies, 7(1), 165. https://doi.org/10.1186/s40814-021-00902-3
- Stanley, B., Currier, G. W., Chesin, M., Chaudhury, S., Jager-Hyman, S., Gafalvy, H., & Brown, G. K. (2017). Suicidal behavior and non-suicidal self-injury in emergency departments underestimated by administrative claims data. Crisis, 39(5), 318–325. https://doi.org/10.1027/0227-5910/a000499
- Sveticic, J., Stapelberg, N. C., & Turner, K. (2020). Suicidal and self-harm presentations to Emergency Departments: The challenges of identification through diagnostic codes and presenting complaints. Health Information Management: Journal of the Health Information Management Association of Australia, 49(1), 38–46. https://doi.org/10.1177/1833358319857188
- Tanner, R., Cassidy, E., & O’Sullivan, I. (2014). The Need for Mental Health Triage in the ED Following Self-Harm. Advances in Emergency Medicine, 2014(4), 1–9. https://doi.org/10.1155/2014/492102
- Van Sleeuwen, R. (2014). The reception perception: An evaluation of medical receptionists’ viewpoints in the healthcare community (Doctoral dissertation). Southern Utah University. Department of Communication. https://www.suu.edu/hss/comm/masters/capstone/thesis/r-vansleeuwen.pdf