Abstract
Objectives
The present study aimed to compare safety and long-term prognosis of patients with chronic total coronary occlusions (CTO) stratified for remaining CTOs after percutaneous coronary intervention (PCI).
Design
The study cohort consisted of patients with coronary artery disease who underwent CTO PCI in a high volume tertiary center from 2009 to 2019 and were registered in Danish high-quality registers. Patients with successful PCI of all CTOs were compared to patients with ≥1 remaining CTO post-procedural. Primary endpoints were analysed using Cox-regression and Kaplan-Meier estimates, and included all-cause mortality, major adverse cardio- and cerebrovascular events (MACCE) and a 30-day safety endpoint.
Results
Procedural success rate was 87.7%, and 76.5% of patients had all CTO(s) opened post-PCI. Safety endpoint occurred in 4.6% of patients, and more frequently in patients with remaining CTO(s) (RD 4.9, 95%CI 0.1, 9.8). All-cause mortality was higher in patients with remaining CTO(s) (Unadjusted HR 1.65, 95% CI 1.03, 2.47, p = .015. Adjusted HR 1.32, 95%CI 0.88–1.99, p = .18) after eight years of follow-up. Risk of MACCE was significantly higher in patients with remaining CTO(s) (Unadjusted HR 1.79, 95% CI 1.34–2.41, p < .001. Adjusted HR 1.51, 95% CI 1.11–2.05, p = .009).
Conclusions
In our centre, CTO PCI was associated with high success rate and low risk of 30-days complications. Presence of remaining CTO(s) after final revascularization attempt was associated with higher but statistically insignificant long-term mortality but was an independent predictor of MACCE.
Introduction
Coronary artery disease (CAD) is a leading cause of mortality and morbidity in the world [Citation1]. Twenty percent of CAD patients have a chronic total occlusion (CTO), which is associated with higher mortality compared to non-CTO CAD [Citation2,Citation3]. Only 15% of CTO patients are treated with percutaneous coronary intervention (PCI), although previous research has shown that PCI improves patients’ quality of life and relieves symptoms [Citation4,Citation5]. Observational studies also suggest a beneficial effect of successful recanalization on mortality and other clinical endpoints [Citation6,Citation7]. However, the prospective randomized trial DECISION-CTO found no such effect. Despite being powered for clinical endpoints, a high crossover rate and a premature stop of inclusion limited the interpretation of the results [Citation8]. CTO PCI is currently considered indicated in patients with significant reversible ischemia and/or refractory symptoms despite optimal medical treatment [Citation9,Citation10].
CTO PCI requires highly skilled operators and entails a risk of complications [Citation11]. Recent developments in procedural techniques and equipment have resulted in decreasing complication rates and increasing success rates [Citation2,Citation9]. However, a significant proportion of CTOs remains occluded despite several attempts at recanalization. In the current study, we aim to evaluate if patients with ≥1 remaining CTO after PCI have a worse prognosis compared to patients with successful recanalization of CTO(s) after adjustment for clinical factors.
Methods
Study design and population
The present study was an observational cohort study based on health registries and medical record audits. Consecutive patients who underwent PCI for ≥1 CTO performed by or under the supervision of a dedicated CTO operator and member of the EuroCTO Club (EHC) at Aarhus University Hospital from 2009 to 2019 were eligible for inclusion [Citation10]. Aarhus University Hospital is the only site performing CTO PCIs in this region comprising 1.3 million inhabitants. All patients were referred to CTO PCI on the indication of symptoms and/or proof of ischemia. Treatment strategy (medical, PCI, or surgical) was decided for each patient at a heart conference considering both symptoms and myocardial viability, coronary anatomy and feasibility of successful PCI, and comorbidities. This heart team consists of interventional cardiologists, cardiothoracic surgeons, and nuclear medicine specialists. The operator performed all complex and redo CTO PCIs at the centre during the period. Procedures were prospectively registered in the European Registry of CTO (ERCTO) and the Western Denmark Heart Registry (WDHR) by the operator. ERCTO is a registry developed by the dedicated EuroCTO Club aiming to evaluate CTO procedures in several European centres and setting standards for the interventional treatment of CTO [Citation10,Citation12]. WDHR is a clinical quality database of procedures from all heart centres in Western Denmark [Citation13]. Demographics, clinical information, and anatomical and procedural characteristics were obtained from these registries. Medical record audits were performed to detect in-hospital complications, events after discharge, causes of death, and additional clinical information of the patients. Data were registered in REDCap and by merging these three data sources; the SKEJ-CTO registry was created.
The conduction of the study was approved by the regional ethical board of the Central Region of Denmark (ID 1-45-70-72-20). The need for written patient consent was waived according to Danish legislation and due to the observational design. This manuscript follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [Citation14].
Definitions
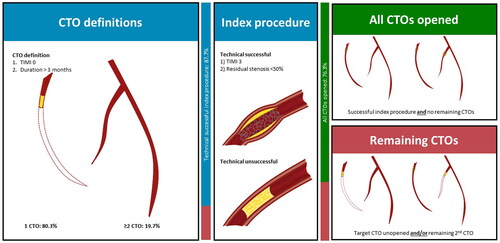
A CTO was defined as a 100% stenosis of the affected lesion with thrombolysis in myocardial infarction (TIMI) flow 0, which was either known (definite CTO) or estimated (probable CTO) to have persisted for at least 3 months [Citation15]. CTOs of a native vessel replaced by well-functioning bypass grafts were not considered CTOs unless a de novo occlusion or significant stenosis of the graft was observed.
Patients with ≥1 remaining CTO after baseline treatment were compared to patients with successful revascularization of all CTO(s). Remaining CTO(s) were defined as either; (1) unopened index CTO due to failed procedure and/or (2) unopened non-index CTO(s), which was left untreated at the operator’s discretion.
Baseline CTO treatment included all staged attempts to revascularize index CTO. The date of enrolment was defined as the date of the final planned revascularization attempt. A technical successful procedure was defined as post-procedural TIMI flow 3 and residual stenosis <50% ().
Figure 1. Study definitions. The cohort consisted of 608 patients presenting with ≥1 CTO (CTO definitions) and underwent CTO PCI at Aarhus University Hospital 2009–2019 (index procedure). It was stratified due to the presence of remaining CTO(s) after index procedure (green and red boxes).
The main endpoint of the current study was threefold; (1) all-cause mortality and (2) a patient-oriented composite of major adverse cardio- and cerebrovascular events (MACCE) consisting of all deaths, any myocardial infarction (MI), target vessel revascularization (TVR), stroke, and hospitalization for cardiac arrest or uncompensated heart failure. Finally, the third endpoint of 30-days safety was addressed as a composite of adverse events including all deaths, any MI, stroke, acute kidney injury (AKI), coronary perforation requiring surgery or pericardiocentesis, stent thrombosis, donor vessel dissection, major bleeding, need for coronary artery bypass grafting (CABG), and vascular complication requiring surgery [Citation15].
Endpoints were defined according to expert consensus recommendations [Citation15]. MI was defined according to the third universal definition of MI and periprocedural MI according to the Society of Cardiovascular Angiography and Intervention [Citation16,Citation17]. Stroke was defined according to the American Stroke Association [Citation18]. TVR was defined as any unplanned revascularization of target vessels. Staged procedures were not included in MACCE. These were defined as planned interventions of non-CTO lesions or index CTO after the index procedure [Citation15]. All cardiovascular hospitalizations lasting >24 h were detected and categorized using ICD-10 codes in medical journals and discharge descriptions. AKI was defined as an increase of serum creatinine of >100% within 48 h [Citation15]. Stent thrombosis was defined according to Academic Research Consortium and major bleeding according to Bleeding Academic Research Consortium (BARC) as ≥ BARC 3 [Citation15,Citation19]. JCTO score was calculated as reported by Morino et al. [Citation20].
In analyses of MACCE and (non-)cardiovascular death, only patients referred from hospitals within the Central Region of Denmark were included, as medical records from other regions were not available for audits. Death status was available for all patients included in the study.
Statistical analyses
Continuous variables are expressed as mean ± standard deviation or medians with interquartile ranges. Categorical variables are expressed with numbers and percentages. Main endpoints were followed until the date of an event, loss to follow-up, date of journal audit, or at a maximum of 8 years after enrolment, whichever came first. The maximum of 8 years was set by rounding the 75-percentile of follow-up to the nearest integer in years. Kaplan Meier time-to-event curves were plotted, and crude and adjusted hazard ratios (HR) with confidence intervals (CI) were calculated. Potential confounders were controlled by multivariable Cox regression. Only variables with univariate p-value < .1 were taken into consideration and a backward stepwise selection strategy was used to reach the final model. The assumption of proportional hazards in Cox regression was assessed graphically by a plot of observed versus predicted values and by a log-log plot. Cut-off values of variables were selected based on the assessment of those plots, assessment of martingale residuals, and evaluation of the clinical relevance of each variable. Restricted mean survival/event-free time was calculated for both groups. The risk difference was calculated for the 30-days safety endpoint. A two-sided p < .05 was considered statistically significant. All analyses were performed with STATA, version 16.
Results
Baseline characteristics
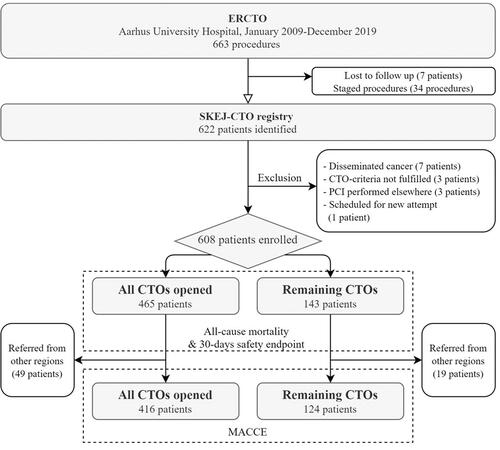
Initially, 663 procedures were identified in the ERCTO during the study period. Thirty-four were staged procedures. Seven patients were lost to follow-up, and fourteen patients did not fulfil the eligibility criteria leaving a complete cohort of 608 patients (). The patient-level success rate of index CTO was 87.7% in this cohort.
In total, 465 patients had all CTO lesions opened (76.5%) and 143 patients were left with remaining CTO(s) (23.5%). Baseline patient characteristics including medical treatment are shown in . The mean age in the full cohort was 65.7 (SD 10.8) years with 80.6% being men. Risk factors were more prevalent among patients with remaining CTO(s), and they had more extensive CAD indicated by a higher prevalence of three-vessel-disease (45.8% versus 24.1%) ( and ). Patients with remaining CTO(s) had a higher Charlson comorbidity index (4.1 SD 1.8 versus 3.4, SD 1.8) ( and A1, Supplementary Material) [Citation21].
Table 1. Patient characteristics.
Table 2. Anatomical and procedural characteristics.
The right coronary artery was the most frequent target vessel of index CTO in both groups (). 120 patients (19.7%) had ≥2 CTOs before treatment, which was more frequent in the “Remaining CTO(s)” group (6.0% versus 64.3%). The success rate of index CTO was 49.0% in patients with remaining CTO(s). The number of failed attempts before the index procedure were 0 (IQR 0, 1) in both groups. JCTO score was 3.1 (SD 1.2) in patients with all CTOs opened and 3.4 (SD 1.0) in patients with remaining CTO(s) ( and A2, Supplementary Material). Wire-crossing strategies of successful index procedures are shown in Figure A1 (Supplementary Material).
30-Days safety
Adverse events within 30 days after the index procedure were observed in 4.6% of patients and were more frequent in patients with remaining CTO(s) (8.4% versus 3.4%) (). Additional complications are described in Table A3 (Supplementary Material).
Table 3. 30-day safety outcome.
All-cause mortality
The median follow-up time was 5.4 years (IQR: 3.1, 8.3). 72 patients (15.5%) with all CTOs opened and 35 patients (24.5%) with remaining CTO(s) died during follow-up (Unadjusted HR 1.65, 95%CI 1.03, 2.47, p = .015) (). No periprocedural deaths were observed. Death within 30 days after enrolment occurred in four patients with remaining CTO(s) and one patient with all CTOs opened.
Figure 3. Main long-term outcome: Kaplan Meier estimates illustrating differences in (A) all-cause mortality and (B) MACCE in patients with all CTOs opened (green) versus with remaining CTOs post index procedure (red). Landmark analyses illustrates difference in (C) all-cause mortality and (D) MACCE between the groups from Day 30 until after 8 years of follow-up. Adjusted HRs are shown on each chart.
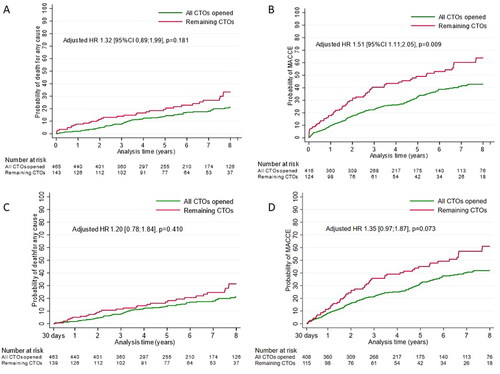
In multivariable regression, left ventricle ejection fraction (LVEF) (categorical <39, 40–49, >50), age >70, and chronic kidney disease (CKD) (s-creatinine >279 µmol/L) were significant predictors for all-cause mortality (Table A4, Supplementary Material). Female sex, three-vessel-disease, diabetes mellitus, previous MI, previous CABG, JCTO score and procedural approach were eliminated after backward selection strategy. Adjusted HR for the presence of remaining CTO(s) was 1.32 (95%CI 0.88, 1.99, p = .18) ().
Table 4. Long-term main outcomes.
Macce
Increased risk of MACCE was observed in patients with remaining CTO(s) (Unadjusted HR of 1.79, 95%CI 1.34, 2.41, p < .001) (). The difference was higher early after enrolment than on long-term (HR 0–30 days 4.44 95%CI 1.65–11.93 versus HR 30 days − 8 years 1.64 95%CI 1.20–2.24) ( and ). The outcomes of MACCE subcategories are shown in Table A5 (Supplementary Material).
In multivariable analysis, significant predictors of MACCE were LVEF, age, CKD, three-vessel-disease, and remaining CTO(s) (Table A4, Supplementary Material). Adjusted HR for remaining CTO(s) was 1.51 (95%CI 1.11, 2.05, p = .009) for 0–8 years ().
Sensitivity analyses
The presence of remaining CTO(s) was strongly associated with cardiovascular death (Table A5, Supplementary Material). Causes of non-cardiovascular death were mainly cancer and death by accidents. Twenty patients were left with > one unopened CTO post-procedural of which seven (35%) died during follow-up, and among patients with a single remaining CTO (123 patients), 28 (22.8%) died. The trend of survival curves was statistically significant (chi2=8.9, p = .003) (Figure A2, Supplementary Material). In a sensitivity analysis with the exclusion of patients with major in-hospital complications we found MACCE estimates similar to the main analysis (Unadjusted HR 1.81 95%CI 1.34–2.45 and adjusted HR 1.50 95%CI 1.09–2.06).
Discussion
We conducted a cohort study of 608 patients undergoing CTO PCI at a tertiary centre. The patient-level technical success rate of index CTO was 87.7% and 76.5% of patients had no remaining CTOs post-procedural. Thirty-day safety endpoint occurred in 4.6%, and more frequently in patients with remaining CTO(s). The presence of remaining CTO(s) post-procedural was an independent predictor of MACCE and associated with higher all-cause mortality, but the latter was statistically insignificant when adjusting for clinical factors.
Safety of CTO PCI
CTO recanalization has been associated with low predictability of success and a high risk of complications [Citation11]. Previously reported success rates vary from <60% up to 85–90% but have increased during the recent decades due to the development of dedicated equipment and techniques [Citation2,Citation5,Citation6,Citation22]. Specialized centres and experienced operators predict improved procedural outcomes, emphasizing a need for operator training and the benefits of concentrating CTO treatment in dedicated centres [Citation2,Citation11]. In our study, all procedures were performed at the only CTO centre in the Central Region of Denmark, which is reflected in a high success rate of 87.7%.
Studies comparing the difference in procedural complications and adverse events between CTO and non-CTO patients are contradicting [Citation11,Citation23]. Due to varying definitions and the risk of underestimating complication rates in retrospective registry-based studies, data cannot be compared without further challenges [Citation24]. This highlights a lack of reporting guidelines in CTO registries. In the current study, we observed low rates of 30-days safety endpoint, which consisted of multiple procedural complications defined after clinical and prognostic relevance following expert consensus recommendations [Citation15].
Long-term prognosis in CTO patients
Previous studies have found a higher risk of death after unsuccessful CTO PCI compared to successful CTO PCI [Citation6,Citation7]. In the present study, patients with remaining CTO(s) included both; (1) patients with unsuccessful procedures for index CTO and/or (2) patients left with an untreated non-index CTO(s). We hypothesized that the presence of an unopened CTO leads to a larger area of myocardium at risk and thereby higher mortality, as previous research has shown higher mortality in STEMI-patients by the presence of a non-culprit CTO, and improvements in coronary blood reserve and hyperemic myocardial blood flow after recanalization of CTO [Citation25–27]. Moreover, we aimed to strengthen the external validity of the study population by including patients with ≥2 CTOs pre-procedural. In this cohort, one of five had ≥2 CTOs pre-procedural, which is comparable to other cohorts of CTO patients [Citation5]. The study cohort is representative of CTO PCI patients, and the high quality of data due to Danish registers and meticulous medical record audits with long follow-ups are major strengths of this study [Citation13].
We demonstrated that the presence of remaining CTO(s) was an independent predictor of the composite endpoint of MACCE eight years after enrollment. Particularly, incidents of cardiovascular death and hospitalization for cardiovascular reasons are higher in patients with remaining CTO(s). The results support that presence of an unopened CTO does lead to a higher risk of future cardiovascular events but based on these observational data we are not able to explain the mechanisms. Higher all-cause mortality was also observed in patients with remaining CTO(s) compared to patients in the successful arm, but this difference was not statistically significant when adjusting for multiple clinical factors. This may be explained by insufficient power due to the size of the cohort, and deaths of non-cardiovascular reasons might have diluted the effects in our main analysis, as no less than 50 deaths were known to be non-cardiovascular. However, patients with remaining CTOs were more comorbid and had more severe CAD at baseline compared to patients with all CTOs opened.
This study was observational and included only patients referred to CTO PCI on the indication of refractive symptoms and/or significant reversible ischemia i.e. in accordance with current national and international guidelines [Citation9]. The randomised EUROCTO trial demonstrated an effect of CTO PCI regarding symptom control and quality of life improvement [Citation4]. The DECISION CTO trial investigated prognosis and was neutral and the results were limited by a high crossover rate and premature stop of inclusion [Citation8]. Future randomized trials still need to address if CTO PCI is superior to medical treatment alone in improving the prognosis of CTO patients, and our findings indicate the importance of successful and safe treatment in patients with an indication of CTO PCI. Results show that patients with remaining unopened CTO(s) despite attempts of revascularization are a high-risk group, who might benefit from closer follow-up and further optimization of medical therapy.
Limitations
The study had several limitations. First, data were observational, and there was no control group of CTO patients receiving medical therapy alone. This leaves a risk of bias, and randomized multicentre trials will be needed to decide if PCI is the most beneficial treatment for CTO patients. Second, there can be different reasons for leaving a CTO unopened in the group with remaining CTO(s) post-procedural, which results in a heterogeneity of this group of patients. Unfortunately, data for these reasons are not available in our data sources. Moreover, the study was subject to selection bias, as the two groups differed regarding comorbidity and severity of CAD. Imaging assessing ischemia was not available in our data, but we presented an overall symptomatic cohort, which is in accordance with current guidelines () [Citation9]. Third, events and in-hospital complications could only be detected in medical records from the Central Region of Denmark, post-procedural biomarkers were not available in all patients, and only complications from index procedures were registered to prevent immortal time bias. In that, there was a risk of missing events and complications. Fourth, a high number of non-cardiovascular deaths might have affected the results of the main analyses of all-cause mortality. Finally, the study was a single-centre study, which impairs the external validity. However, baseline and procedural characteristics, success rates, and complication rates are comparable to OPEN CTO and PROGRESS CTO registries (Table A5, Supplementary Material) [Citation28,Citation29].
Conclusions
In a single centre cohort study, investigating outcomes after CTO PCI, we demonstrated high safety 30 days after treatment, particularly in patients with all CTOs opened compared to patients with remaining CTO(s). Patients with all CTOs opened had a lower risk of MACCE, and a favourable long-term survival was also observed in this group, but the latter was not statistically significant in multivariable analysis. Further studies with sufficient power are needed to confirm the findings and randomized trials are needed to evaluate if CTO PCI is superior to medical therapy alone in improving prognosis of CTO patients.
Supplemental Material
Download Zip (80.4 KB)Acknowledgments
We thank Jakob Hjort for assistance in data management.
Disclosure statement
EHC and ENH have received institutional grants from ASAHI, Philips and Orbus Neich. The other authors declare no conflicts of interest.
Data availability statement
Data of the current study cannot be shared due to restrictions.
Additional information
Funding
References
- DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390(10100):1260–1344.
- Hoebers LP, Claessen BE, Dangas GD, et al. Contemporary overview and clinical perspectives of chronic total occlusions. Nat Rev Cardiol. 2014;11(8):458–469.
- Ramunddal T, Hoebers LP, Henriques JP, et al. Prognostic impact of chronic total occlusions: a report from SCAAR (Swedish coronary angiography and angioplasty registry). JACC Cardiovasc Interv. 2016;9(15):1535–1544.
- Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39(26):2484–2493.
- Ramunddal T, Hoebers LP, Henriques JP, et al. Chronic total occlusions in Sweden–a report from the Swedish coronary angiography and angioplasty registry (SCAAR). PLoS One. 2014;9(8):e103850.
- Christakopoulos GE, Christopoulos G, Carlino M, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 2015;115(10):1367–1375.
- Khan MF, Wendel CS, Thai HM, et al. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv. 2013;82(1):95–107.
- Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019;139(14):1674–1683.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
- Galassi AR, Werner GS, Boukhris M, et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention. 2019;15(2):198–208.
- Brilakis ES, Banerjee S, Karmpaliotis D, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (national cardiovascular data registry). JACC Cardiovasc Interv. 2015;8(2):245–253.
- Konstantinidis NV, Werner GS, Deftereos S, et al. Temporal trends in chronic total occlusion interventions in Europe. Circ Cardiovasc Interv. 2018;11(10):e006229.
- Schmidt M, Maeng M, Madsen M, et al. The Western Denmark heart registry: its influence on cardiovascular patient care. J Am Coll Cardiol. 2018;71(11):1259–1272.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
- Ybarra LF, Rinfret S, Brilakis ES, et al. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC consensus recommendations. Circulation. 2021;143(5):479–500.
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020–2035.
- Moussa ID, Klein LW, Shah B, et al. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: an expert consensus document from the society for cardiovascular angiography and interventions (SCAI). Catheter Cardiovasc Interv. 2014;83(1):27–36.
- Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2013;44(7):2064–2089.
- Lemesle G, Delhaye C, Bonello L, et al. Stent thrombosis in 2008: definition, predictors, prognosis and treatment. Arch Cardiovasc Dis. 2008;101(11–12):769–777.
- Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (multicenter CTO registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–221.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6(2):128–136.
- Werner GS, Hochadel M, Zeymer U, et al. Contemporary success and complication rates of percutaneous coronary intervention for chronic total coronary occlusions: results from the ALKK quality control registry of 2006. EuroIntervention. 2010;6(3):361–366.
- Rigger J, Hanratty CG, Walsh SJ. Common and uncommon CTO complications. Interv Cardiol. 2018;13(3):121–125.
- Claessen BE, Dangas GD, Weisz G, et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur Heart J. 2012;33(6):768–775.
- Schumacher SP, Kockx M, Stuijfzand WJ, et al. Ischaemic burden and changes in absolute myocardial perfusion after chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2020;16(6):e462–e471.
- Ybarra LF, Rinfret S. Why and how should we treat chronic total occlusion? Evolution of state-of-the-art methods and future directions. Can J Cardiol. 2020;2022:38(10S1):S42-S53.
- Tajti P, Karmpaliotis D, Alaswad K, et al. The hybrid approach to chronic total occlusion percutaneous coronary intervention: update from the PROGRESS CTO registry. JACC Cardiovasc Interv. 2018;11(14):1325–1335.
- Sapontis J, Hirai T, Patterson C, et al. Intermediate procedural and health status outcomes and the clinical care pathways after chronic total occlusion angioplasty: a report from the OPEN-CTO (outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures) study. Catheter Cardiovasc Interv. 2020;10(15):1523–1534.