Abstract
Objectives. The coronavirus disease 2019 (COVID-19) pandemic, which commenced in 2020, is known to frequently cause respiratory failure requiring intensive care, with occasional fatal outcomes. In this study, we aimed to conduct a retrospective nationwide observational study on the influence of the pandemic on cardiac surgery volumes in Sweden. Results. In 2020, 9.4% (n = 539) fewer patients underwent open-heart operations in Sweden (n = 5169) than during 2019 (n = 5708), followed by a 5.8% (n = 302) increase during 2021 (n = 5471). The reduction was greater than 15% in three of the eight hospitals in Sweden performing open-heart operations. Compared to 2019, in 2020, the waiting times for surgery were longer, and the patients were slightly younger, had better renal function, and a lower European System for Cardiac Operative Risk Evaluation; moreover, few patients had a history of myocardial infarction. However, more patients had insulin-treated diabetes mellitus, hypertension, peripheral vascular disease, reduced left ventricular function, and elevated pulmonary artery pressure. Urgent procedures were more common, but acute surgery was less common in 2020 than in 2019. Early mortality and postoperative complications were low and did not differ during the three years. Conclusion. The 9.4% decrease in the number of heart surgeries performed in Sweden during the 2020 COVID-19 pandemic, compared to 2019, partially recovered during 2021; however, there was no backlog of patients awaiting heart surgery.
Introduction
The coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It is frequently associated with hypoxic respiratory failure, which requires prolonged hospitalisation in vulnerable individuals, occasionally resulting in fatal outcomes [Citation1]. The severity of COVID-19 ranges from a variety of negligible symptoms to cytokine storms, respiratory failure, and circulatory collapse [Citation1,Citation2]. During the 2020 pandemic, hospital resources were allocated to care for critically ill patients with COVID-19, and the number of elective operations was reduced. The capacity to perform cardiac surgery was initially reduced by more than 50% in some centres [Citation3–10]. It was assumed that surgical capacity would need to increase following the pandemic to clear the backlog of deferred cases [Citation4].
This retrospective nationwide observational analysis aimed to assess the effect of the COVID-19 pandemic on open cardiac surgery volumes in Sweden.
Methods
Patients
Information on all cardiac operations performed in adults in Sweden from 2019 to 2021 was obtained from the Swedish Cardiac Surgery Registry in the national Swedish Web-system for Enhancement and Development of Evidence-based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) registry (www.swedeheart.se) [Citation11]. In a retrospective analysis, the number of open-heart operations performed during 2020 and 2021 was compared with those performed in 2019, the year before the pandemic. This study was approved by the Swedish Ethical Review Authority (DNR. 2020-05209, 2022-00736-02). All patients were provided written information before the operation that variables regarding the operation will be exported to the national quality registry the Swedish Cardiac Surgical Register. According to the Communicable Diseases Act, all COVID-19 patients with a positive polymerase chain reaction test for SARS-CoV-2-RNA (ribonucleic acid), regardless of symptoms, were reported via the SmiNet database to the Public Health Agency of Sweden (https://www.folkhalsomyndigheten.se).
Definitions
Information of hypertension, peripheral vascular disease and other diagnoses were based on data reported to the register. Chronic obstructive pulmonary disease was defined as requiring medication with bronchodilators or steroids for lung disease. Diabetes was defined as requiring treatment with either insulin or oral hyperglycaemic drugs or a special diet. Creatinine clearance was estimated using the equation of Cockcroft and Gault [Citation12]. Myocardial infarction was defined based on clinical presentation and elevated biomarkers. Urgent procedures were performed during hospitalisation and acute surgery within 24 h following the decision to operate. The risk of surgery was assessed using the European System for Cardiac Operative Risk Evaluation Score (EuroSCORE) II [Citation13].
Statistical methods
Continuous variables are presented as arithmetic mean and one standard deviation or non-normal distribution with median and interquartile range. Student’s t test was used to compare continuous variable data between the two groups. The Mann–Whitney U test was used for skewed distributions. The chi-square method with Yate’s correction for continuity was applied to analyse the proportions of categorical variables. A p value less than.05 was considered statistically significant. Calculations were performed using STATISTICA 13 (Stat Soft, Dell).
Results
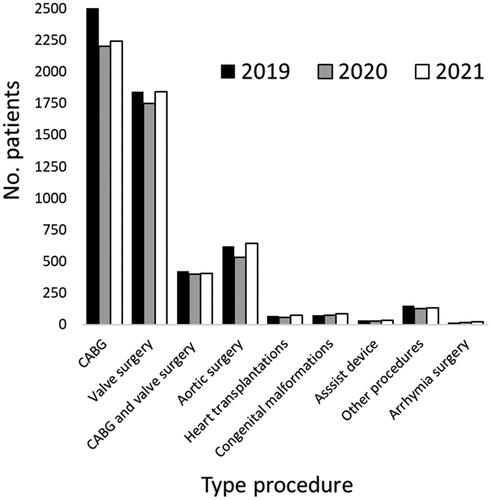
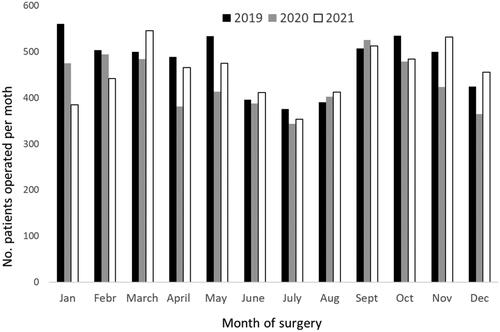
In 2020, during the COVID-19 pandemic (n = 5169), 9.4% (n = 539) fewer patients (p < .001) underwent open-heart surgery in Sweden than in 2019 (n = 5708), followed by a 5.8% (n = 302) increase (p < .001) in 2021 (n = 5471). Coronary artery bypass grafting, valve surgery, and aortic surgery were reduced by 12.1%, 4.8%, and 13.8%, respectively (, Supplementary Table 1). Heart transplantations and the use of ventricular assist devices were fewer and reduced to 16.2% and 20%, respectively. In particular, patients having aortic surgery (20.3%), transplantations (28.3%), and assist devices (29.2%) increased in 2021 compared to 2020. The reduced number of operations during 2020 compared to 2019 was most marked during January, April, May, November, and December ().
Table 1. Characteristics of patients undergoing open cardiac surgery in Sweden during 2019–2021.
In 2020, compared to 2019, the waiting times for heart surgery were longer, the patients were slightly younger, had better renal function, and a lower EuroSCORE II; moreover, few patients had a history of myocardial infarction. However, more patients had insulin-treated diabetes mellitus, hypertension, peripheral vascular disease, reduced left ventricular function, and elevated pulmonary artery pressure (). Urgent procedures were more common, but acute surgery was less common in 2020 than in 2019. Patient characteristics in 2021 were similar to those before the 2019 pandemic. Deaths within 30 days of surgery and postoperative complications were few and did not differ during the three years ().
Table 2. Outcome after open cardiac surgery in Sweden during 2019–2021.
The decrease in the number of surgical patients during the 2020 COVID-19 pandemic, compared to 2019, was greater than 15% in three of the eight hospitals in Sweden performing open-heart surgery. Patient characteristics in these three hospitals were similar to those nationwide, with patients of a younger age, better renal function, and lower EuroSCORE II as well as fewer patients with a history of myocardial infarction presenting in 2020 than in 2019 (Supplementary Tables 2 and 3).
Discussion
In this retrospective nationwide register analysis of cardiac surgery volumes in Sweden during the COVID-19 pandemic, there were 9.4% fewer operations performed in 2020 than in 2019, followed by a 5.8% increase in 2021.
Sweden was hit by several waves of COVID-19, with the Omicron variant emerging late in 2021, which had a benign clinical course. Vaccinated populations have a significantly lower severity of infection from the Omicron variant of COVID-19 than those that are unvaccinated [Citation14]. We initially expected a maximal incidence of COVID-19 cases early in 2020 and that the infection would fade out; however, the second and third waves of virus infection occurred during the winter of 2020–2021.
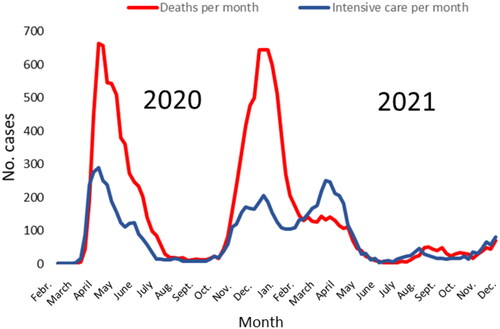
COVID-19 profoundly affected heart surgery activity. Cardiac surgery case volumes decreased 53% in the United States, 51% in Ireland and 57% in France in April 2020 compared to in 2019 [Citation8,Citation9,Citation15]. The reasons involved factors as less patient willingness to attend hospital and risk of COVID-19 exposure, limited capacity for diagnosis of heart disease, curtailed elective operations, shortness of hospital staff and intensive care beds. In contrast to many other countries, Sweden did not implement a lockdown during the pandemic in 2020. This seems to have mitigated the COVID-19 effect with relative moderate reduction of cardiac surgery volumes. We advocated general recommendations to, if possible, work from home, socially distance, and avoid public transportation. Nevertheless, the impact was considerable, with only a few visitors allowed in shops and small audiences in venues. Hospital patients were not allowed visitors, even relatives. Initially, there was a shortage of personal protective equipment, and face masks were rarely used. Sweden experienced numerous mortalities, and there was a high demand for intensive care in early 2020, although extensive spread of the infection did not occur until the autumn of 2020 and early in 2021. As of 31 December 2021, a total of 1,306,286 people in Sweden tested positive for COVID-19, 14,711 of whom died within a month of COVID-19 diagnosis and 8057 patients required intensive care treatment ( and ). Fatalities and cases requiring intensive care were few in relation to the total number COVID-19 cases, particularly among those infected with the Omicron variants in late 2021.
Figure 3. Number of reported cases with COVID-19 per month in Sweden in 2020 and 2021. Official statistics from the Public Health Agency of Sweden (https://www.folkhalsomyndigheten.se).
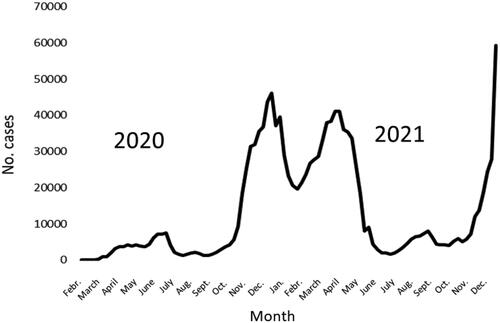
Figure 4. Number of cases that tested positive for COVID‐19 in the month prior to death and number of COVID‐19 cases treated in the intensive care unit per month in Sweden during 2020 and 2021. Official statistics from the Public Health Agency of Sweden (https://www.folkhalsomyndigheten.se).
Multiple factors may have contributed to the reduction in heart operations performed in 2020 compared with 2019. During the pandemic, elderly people and those with cardiovascular risk factors were asked by the Swedish Public Health Agency to stay at home and comply with social distancing restrictions. Media reports of overcrowded hospitals with overloaded intensive care units and patients led to a reluctance to be admitted for elective surgery. Patients scheduled for elective heart surgery were asked stay away from hospitals if they exhibited any airway symptoms. Doctors, nurses, and other hospital staff members were recruited to treat the numerous COVID-19 cases. There was a reduced capacity for preoperative evaluation and significantly reduced beds available in recovery wards and intensive care units, attributable to the number of COVID-19 patients requiring hospitalisation. Acute surgery, such as aortic dissection, could not be deferred. However, the fear of acquiring COVID-19, with its potentially severe outcomes and high mortality rates, resulted in some individuals not seeking early medical treatment for cardiovascular symptoms, leading to serious consequences [Citation16–18].
The average age of surgical patients was slightly lower during the pandemic in 2020 than in 2019. Older patients with cardiovascular disease who were not evaluated by a cardiologist may have contributed to this observation. It is possible that some elderly patients with cardiac disease who could have been treated with cardiac surgery were among those not evaluated due to COVID-19 mortality. These patients may account for, in some part, the reduction in surgical volumes. Moreover, fewer surgical patients had a history of myocardial infarction during the pandemic. This finding is in line with previous reports of a reduced number of patients with myocardial infarction presenting to the hospital during the COVID-19 pandemic [Citation19–21]. Furthermore, surgical outcomes did not differ between patients with and without COVID-19 [Citation22].
The situation changed considerably in 2021 following the advent of effective vaccines, with a marked reduction in severe disease and deaths due to COVID-19. A mass vaccination programme was initiated in early spring 2021. With increased experience, vaccinated staff, isolation of patients, and an increased supply of personal protective equipment to safely perform cardiac surgery, the volume of surgeries recovered [Citation3]. The recovery of cardiac surgery volume in 2021, following the pandemic, was less than anticipated with an increase of approximately 300 cases. The expected backlog of approximately 500 patients with an assumed deferred heart operation did not transpire. The 12.1% reduction in coronary bypass procedures was not explained by patients being administered alternative treatments; for the first time in 30 years, the number of percutaneous catheter interventions declined during 2020 with a small increase in 2021 (www.ucr.uu.se/swedeheart). Although, the incidence of myocardial infarction was reduced during the pandemic, experiences and oral reports from individual centres indicate that, in at least some Swedish centres, the indications for coronary artery bypass grafting and percutaneous catheter intervention were consciously adjusted during the most intense waves of the pandemic due to reduced intensive care unit capacity. The number of heart transplantations increased as organ donation became safer after the introduction of the vaccination programme.
Limitations
The study is retrospective; however, the reliability of data in the Swedish Cardiac Surgery Registry is high, and every heart operation performed in Sweden has been reported [Citation23]. We have not been able to ascertain the exact reasons why 500 fewer patients were operated on in 2020 than in 2019 and why this did not create a backlog of patients requiring surgery during 2021.
Conclusions
COVID-19 had profound effects on cardiac surgery volumes in Sweden, with a reduction of 9.4% in 2020 compared to 2019, but did not influence the safety of the operations. We did not experience an expected backlog of patients requiring surgery after the pandemic.
Ethics approval
This study was approved by the Swedish Ethical Review Authority (DNR. 2020-05209).
Consent form
Informed consent was obtained from the surgical patients to analyse and publish anonymised data.
Author contributions
TI, MD, and ÖF contributed equally to this work and participated in the design, acquisition of data, analyses, and drafting and revision of the manuscript. All the authors have read and approved the final manuscript.
Supplemental Material
Download MS Word (19.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the study’s ethical consent, data are not available for sharing.
Additional information
Funding
References
- Dhakal BP, Sweitzer NK, Indik JH, et al. SARS-CoV-2 infection and cardiovascular disease: COVID-19 heart. Heart Lung Circ. 2020;29(7):973–987.
- Ferroni E, Rossi PG, Alegiani SS, et al. Survival of hospitalized COVID-19 patients in Northern Italy: a population-based cohort study by the ITA-COVID-19 network. Clin Epidemiol. 2020;12:1337–1346.
- Gunaydin S, Stammers AH. Perioperative management of COVID-19 patients undergoing cardiac surgery with cardiopulmonary bypass. Perfusion. 2020;35(6):465–473.
- Salenger R, Etchill EW, Ad N, et al. The surge after the surge: cardiac surgery post-COVID-19. Ann Thorac Surg. 2020;110(6):2020–2025.
- George I, Salna M, Kobsa S, et al. The rapid transformation of cardiac surgery practice in the coronavirus disease 2019 (COVID-19) pandemic: insights and clinical strategies from a centre at the epicentre. Eur J Cardiothorac Surg. 2020;58(4):667–675.
- Yates MT, Balmforth D, Kirmani BH, et al. A multi-centre prospective cohort study of patients on the elective waiting list for cardiac surgery during the COVID-19 pandemic. J R Soc Med. 2022;115(9):348–353.
- Harky A, Poole G, Axiaq A, et al. COVID-19 and cardiac surgery: do outcomes differ? J Card Surg. 2020;35(12):3391–3394.
- Nguyen TC, Thourani VH, Nissen AP, et al. The effect of COVID-19 on adult cardiac surgery in the United States in 717 103 patients. Ann Thorac Surg. 2022;113(3):738–746.
- Casey L, Khan N, Healy DG. The impact of the COVID-19 pandemic on cardiac surgery and transplant services in Ireland’s national centre. Ir J Med Sci. 2021;190(1):13–17.
- Sethuraman N, Jeremiah SS, Ryo A. Interpreting diagnostic tests for SARS-CoV-2. JAMA. 2020;323(22):2249–2251.
- Jernberg T, Attebring MF, Hambraeus K, et al. The swedish web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). Heart. 2010;96(20):1617–1621.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41.
- Nashef SA, Sharples LD, Roques F, et al. EuroSCORE II and the art and science of risk modelling. Eur J Cardiothorac Surg. 2013;43(4):695–696.
- Lauring AS, Tenforde MW, Chappell JD, et al. Clinical severity of, and effectiveness of mRNA vaccines against, covid-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: prospective observational study. BMJ. 2022;376:e069761.
- Nader J, Anselmi A, Tomasi J, et al. Adult cardiac surgery during COVID-19 lockdown: impact on activity and outcomes in a high-volume centre. Arch Cardiovasc Dis. 2021;114(5):364–370.
- Masroor S. Collateral damage of COVID-19 pandemic: delayed medical care. J Card Surg. 2020;35(6):1345–1347.
- Lidin M, Lynga P, Kinch-Westerdahl A, et al. Patient delay prior to care-seeking in acute myocardial infarction during the outbreak of the coronavirus SARS-CoV2 pandemic. Eur J Cardiovasc Nurs. 2021;20(8):752–759.
- Ivert T, Dalen M. Dismal outcome if delayed cardiac surgery because of coronavirus disease 2019. Interact Cardiovasc Thorac Surg. 2022;35(2):1–6.
- Mohammad MA, Koul S, Olivecrona GK, et al. Incidence and outcome of myocardial infarction treated with percutaneous coronary intervention during COVID-19 pandemic. Heart. 2020;106(23):1812–1818.
- Solomon MD, McNulty EJ, Rana JS, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693.
- Boukhris M, Azzalini L, Baystrukov V, et al. Impact of the COVID-19 pandemic on acute coronary syndrome and stroke volumes in non-Western countries. Cardiovasc Revasc Med. 2021;27:95–97.
- Ivert T, Dalen M. Testing for coronarvirus disease 2019 before cardiac surgery-safe outcome of infected patients. J Cardiothorac Surg. 2022;17(1):201.
- Vikholm P, Ivert T, Nilsson J, et al. Validity of the Swedish cardiac surgery registry. Interact Cardiov Thorac Surg. 2018;27(1):67–74.