Abstract
Objectives. Readmission rates following open cardiac surgery are high, affecting patients and the cost of care. This study aimed to investigate the effect of early additional follow-up after open cardiac surgery when 5th-year medical students conducted follow-ups under the supervision of physicians. The primary endpoint was unplanned cardiac-related readmissions within one year. The secondary outcomes were the detection of impending complications and health-related quality of life (HRQOL). Methods. Patients undergoing open cardiac surgery were prospectively included. For intervention, additional follow-up visits, including point-of-care ultrasound, were conducted by supervised 5th-year medical students on postoperative days 3, 14 and 25. Unplanned cardiac-related readmissions, including emergency department visits, were registered within the first year of surgery. Danish National Health Survey 2010 questionnaire was used for HRQOL. In standard follow-up, all patients were seen 4-6 weeks postoperative. Results. For data analysis, 100 of 124 patients in the intervention group and 319 of 335 patients in the control group were included. The 1-year unplanned readmission rates did not differ; 32% and 30% in the intervention and control groups, respectively (p = 0.71). After discharge, 1% of patients underwent pericardiocentesis. The additional follow-up initiated scheduled drainage, contrary to more unscheduled/acute drainages in the control group. Pleurocentesis was more common in the intervention group (17% (n = 17) vs 8% (n = 25), p = 0.01) and performed earlier. There was no difference between groups on HRQOL. Conclusion. Supervised student-led follow-up of newly cardiac-operated patients did not alter readmission rates or HRQOL but may detect complications earlier and initiate non-emergent treatment of complications.
Introduction
Outcomes following open cardiac surgery have improved significantly over the last decades, but still, high readmission rates affect patient recovery, and healthcare costs [Citation1]. Early follow-up has been associated with a lower readmission risk, but prospective studies are sparse and warranted [Citation2–5].
Enhanced recovery programmes with early discharge leave the patient to interpret and act on symptoms, sometimes for several weeks, until scheduled follow-up. Within the first month, 11–32% of patients are readmitted, often due to pericardial/pleural effusions, infections, cardiac arrhythmias, congestive heart failure, or non-specific symptoms like chest pain and dizziness [Citation2–14]. For post-surgical complications, timely detection is vital. Pericardial effusions are, for example, associated with increased morbidity and may lead to life-threatening conditions if untreated [Citation15–17]. Yet, little is known about how different strategies for follow-up affect readmission rates and the detection of imminent complications [Citation2,Citation5]. Further, the improved outcomes after cardiac surgery have entailed our focus towards patients’ impaired health-related quality of life (HRQOL) [Citation18]. Early care and support have been proposed to strengthen HRQOL [Citation19].
Follow-up visits after open-cardiac surgery are traditionally conducted by surgeons, cardiologists, cardiac nurses, or general practitioners. A recent trend in medical education proposes to engage medical students to provide patient care while learning (Value-Added Medical Education) [Citation20]. We have previously shown that medical students can perform Focused-Assessed-Transthoracic Echocardiography (FATE) after little training [Citation21]. Further, we have demonstrated that cardiac-operated patients highly appreciate the feeling of safety related to early post-operative follow-ups conducted by supervised medical students [Citation22]. However, the effect of early follow-up visits after open cardiac surgery performed by supervised medical students on clinical outcomes and HRQOL remains to be investigated.
Thus, this study aimed to investigate the effect of three additional follow-up visits by supervised 5th-year medical students in the first month after open cardiac surgery. The primary outcome was the readmission rate within the first year after surgery, whereas the secondary outcomes were the detection of imminent complications and individual changes in self-reported HRQOL questionnaires.
Materials and methods
Ethical statement
The Regional Committee on Biomedical Research Ethics of the Central Denmark Region approved the project (05-28-19, 1-10-72-92-19), which conforms to the ethical guidelines of the Declaration of Helsinki. Written informed consent from patients was obtained before enrolment.
Study design
This is a prospective study comparing two groups of cardiac-operated patients. One group underwent standard follow-up, and another underwent additional early follow-up conducted by medical students under the supervision of physicians.
Participants, setting and recruitment
Inclusion criteria were adults undergoing elective or subacute open cardiac surgery at Aarhus University Hospital. Exclusion criteria were emergent surgery (patients taken immediately to the operating room upon arrival without appropriate time for the inclusion process), inability to speak and understand the Danish language, residence outside the Central Region of Denmark (due to logistical reasons) or surgery with specialised follow-up programs (e.g. heart transplant).
Patients in the intervention group were enrolled based on available consultation slots in the student clinic. If patients eligible for inclusion exceeded the logistic capacity of the student clinic, patients were randomly divided between the intervention and control groups using computer randomisation.
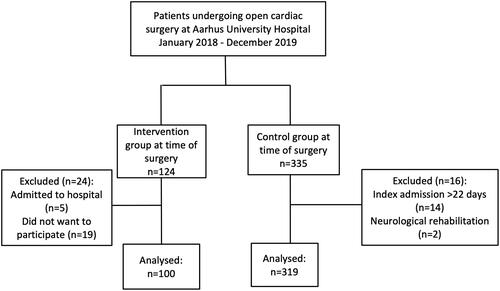
For data analysis, patients in the intervention group were excluded if they did not participate in any study-related outpatient visits after discharge (n = 24). Patients in the control group were excluded if they had an index hospitalisation longer than the intervention group (n = 14) or if transferred directly from the surgical ward to a neurological rehabilitation facility (n = 2), . We chose these arbitrary exclusion criteria from data analysis to seek comparable groups, as length-of-stay is associated with increased postoperative complication rates and risk of readmissions [Citation3,Citation6,Citation7].
Control and intervention group: standard postoperative care and follow-up program
Besides the additional follow-up visits, in the intervention group both groups received standard operative and post-operative care. Patients in both groups were either discharged directly from the surgical unit or transferred and later discharged from their local hospital (typically on days 6–9) [Citation8]. Patients were referred to their general practitioner for suture removal. Follow-up was conducted at the patients’ local hospitals. Some patients had a planned consultation with a physician at their local hospital after two weeks. According to European guidelines, all patients had a planned outpatient visit at their local hospital 4–6 weeks after surgery, where valve-operated patients underwent transthoracic echocardiography [Citation23].
The intervention: additional follow-up performed by supervised medical students
On top of the standard care program, three additional controls were planned for the intervention group. Before discharge (postoperative days 3–5), a FATE was performed to assess pericardial and pleural effusions [Citation24]. After discharge from the hospital, two out-patient consultations were scheduled on days 10 to 15 and 25 to 30 after surgery. This period was previously shown as critical for many readmissions [Citation2–4,Citation6,Citation8]. The outpatient visits comprised a focused interview, a routine clinical examination, and a simple evaluation of the medical treatment. The clinical examination consisted of an electrocardiogram (ECG) to screen for cardiac arrhythmias, a FATE scan to access effusions, and a wound inspection to evaluate signs of infection. When clinically indicated (symptom-driven), patients were sent for pleurocentesis by skilled personnel using chest tubes, followed by mobilisation before drains were discontinued. More than trivial pericardial effusions were consulted with specialist cardiologists for treatment strategy.
Fifth-year medical students led the outpatient consultations supervised by junior doctors, with the possibility of consulting a specialist cardiologist or cardiac surgeon. The supervising junior doctor was present at the FATE scan and the last half of the patient consultation to ensure patient safety.
Data collection and outcome measures
Data were collected from the Western Denmark Heart Registry and electronic medical records [Citation25].
The primary outcome was unplanned cardiac-related readmissions within the first year of surgery. Unplanned cardiac-related readmission was defined as a) admission occurring from 1 day after discharge from the hospital; b) regular admission or emergency department visits; c) unplanned readmission due to cardiac causes or causes related to the surgery. Elective cardiac readmissions for a planned procedure, e.g. pacemaker implantation, were not included. The cause of readmission was based on the International Classification of Disease diagnoses (ICD) given by the physician in charge of discharging the patient. The ICD diagnoses for readmissions were divided into five groups: cardiac, unspecific symptoms (e.g. chest pain, dizziness), causes presumed to be related to the surgery (e.g. effusions, pericarditis), atrial fibrillation/flutter, and infection. Furthermore, treatment of surgical complications was registered. The self-reported HRQOL was assessed using the Danish National Health Survey 2010 questionnaire (14). Questionnaires were sent to patients 1, 6, and 12 months after surgery. Responses were excluded from the analysis if a reply was more than one month late.
Statistical analyses
Sample size estimation was performed on the primary endpoint of the 30-day readmission rate based on data from the same hospital [Citation10]. The intervention was estimated to lower the 30-day readmission rate from 32% to 15%. With significance at 5% and power at 80%, we would need 94 patients in each group.
Continuous, normally distributed data are reported as means with standard deviations. Non-normally distributed data are presented as medians with 25th and 75th percentiles (IQR) and compared using Wilcoxon Mann–Whitney rank-sum test. Categorical variables are presented as numbers (%) and compared using Fisher’s exact test. HRQOL answers were analysed by measuring the individual changes in responses from 1 to 6 months and 1 to 12 months. The categorical difference in answers was compared using Fisher’s exact test. REDCap electronic data capture tools hosted at Aarhus University were used for data management [Citation26]. Analyses were performed using Stata/IC 15.1 (StataCorp LP, TX, USA). Statistical significance was defined as a p-value below 0.05.
Results
Flow chart and patient demographics
From January 2018 to December 2019, 459 patients were included in the study (). In the intervention group, 100 of 124 (81%) patients were included in data analyses, and in the control group, 319 of the 335 (95%) patients were included in data analyses. Patient demographics and selected information on surgical and post-surgical parameters are presented in .
Table 1. Patient demographics and clinical characteristics of the total population.
Unplanned cardiac-related readmissions
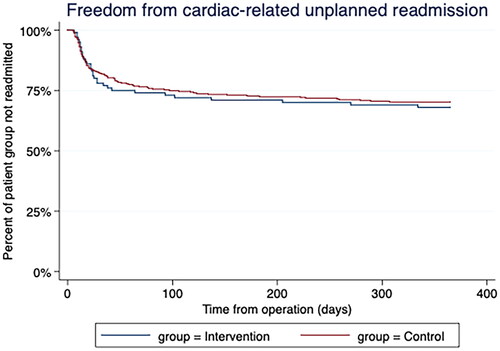
As presented in , there was no difference in unplanned cardiac-related readmission rates within the first year after surgery, 32% (intervention) versus 30% (controls), p = 0.71. At 30 days, the readmission rates were 22% (intervention) versus 18% (controls), p = 0.38.
Table 2. Unplanned readmissions and all-cause mortality within one year.
The time from operation to the first unplanned cardiac-related readmission was 23 (IQR, 13;40) days in the intervention group and 20 (IQR, 12;58) days in the control group (p = 0.84), . Length-of-stay at the first unplanned cardiac-related readmission was less than two days for 20 patients (63% of the readmissions) in the intervention group and 56 patients (59% of the readmissions) in the control group. The most common cause of the first unplanned cardiac-related readmission was non-specific cardiac symptoms in both groups. There was no difference in the distribution of the readmission causes between the groups, p = 0.68. One patient in each group died within the first year after surgery.
Drained pericardial effusions
After discharge from the hospital, one patient in the intervention group was drained for pericardial effusion during a scheduled visit initiated by the student outpatient clinic. In contrast, four patients in the control group underwent pericardiocentesis during unscheduled readmissions due to clinical symptoms (dyspnoea or chest pain). No complications occurred during the pericardiocentesis.
Drained pleural effusions
Pleurocentesis after discharge from the hospital was more common in the intervention group, 17% (n = 17) versus 8% (n = 25) in the control group (p = 0.01). As presented in , patients in the intervention group were drained earlier than patients in the control group, 16 (IQR: 14;28) vs 25 (IQR:18;54) days after surgery, p = 0.04. The drained volume of pleural effusions did not differ between groups, with 900 (IQR: 700;1500) mL in the intervention group and 1275 (IQR: 750;1600) mL in the control group (p = 0.51). In both groups, patients that had undergone a coronary artery bypass graft (CABG) operation were more prone to require thoracentesis than patients undergoing other surgical procedures. The number of patients undergoing pleural drainage at both index admission and after discharge was 3% in the intervention group and 2% in the control group. No complications were reported for the pleural drainages.
Table 3. Pleurocenteses after discharge from the surgery.
Questionnaire on health-related quality of life
There was no statistical difference in the patients’ individual differences of self-reported HRQOL between groups, neither from 1 to 6 months nor from 1 to 12 months. As presented in , 1 year after surgery, 6% of respondents in the intervention group and 11% in the control group reported being very limited when walking up more than one floor. Respondents reported being very bothered by sleep problems counted 17% in the intervention group and 10% in the control group one year after surgery.
Table 4. Self-reported health-related quality of life.
Discussion
This is, to the knowledge of the research group, the first study to describe additional follow-up after open cardiac surgery in a supervised student clinic. The additional follow-up did not alter unplanned readmission rates or self-reported HRQOL. Still, post-surgical complications such as the potentially serious condition of pericardial effusions appeared to be detected and treated earlier in the additional follow-up programme than with standard care.
This study stands out from previous patient care and medical education research. First, few studies have compared the readmission rates in various follow-up programs after open cardiac surgery [Citation2,Citation5]. Second, studies remain sparse on patient outcomes from supervised student consultations, and to our knowledge, we present the first study of its kind within open cardiac surgery [Citation27,Citation28].
Unplanned readmission rates
Based on 419 open-cardiac operated patients, we found no significant change between the intervention and the control groups in early nor late readmission rates. The neutral results do not align with previous comparable studies, which report reduced readmission rates from interventions [Citation2,Citation5].
Few intervention studies have been published within open-cardiac surgery follow-up examining readmission rates [Citation2,Citation5]. A Danish study by Borregaard et al. enrolling a total of 1288 heart-valve operated patients, reported an early (30 days) readmission rate of 17% (intervention) and 25% (retrospective cohort), p = 0.002 [Citation2]. The late readmission rate (180 days) was 23% (intervention) vs 37% (retrospective cohort), p < 0.001. Another study, from the United States by Bates et al. on 189 CABG-operated patients, reported a 30-day readmission rate of 12.0% (intervention) vs 25.8% (retrospective cohort), p = 0.02 [Citation5].
A direct comparison between the three studies comprises limitations. Primarily, we conducted a prospective study, contrasting the two studies which compare the intervention to retrospective cohorts. Thus, the difference in those studies regarding readmission rates may reflect the impact of interventions as well as modifications in surgical procedures, standard care etc. Secondly, although some elements of the follow-up programmes were comparable, such as symptom-driven consultations and simple screening for impending complications (e.g. ECG and FATE), others were not. In contrast to our study, Borregaard and Bates focused intervention on patient empowerment before discharge. Borregaard et al. individualised the follow-up based on the estimated risk of complications (assessed by clinical presentation and frailty score), and 90% of patients were assigned additional follow-up. In contrast, Bates et al. continued standard follow-up with a cardiologist 5-10 days after hospital discharge, but intervention ensured the meeting was arranged (the STAAR initiative). Thirdly, the professional competency of the person conducting the consultations differs in our study from the two studies. Where we supervised medical students in performing the patient consultations, Borregaard and Bates focused on consecutive care by a cardiac nurse or a cardiologist.
Although to the knowledge of the research group present the first study on follow-up by supervised medical students after open cardiac surgery employing the endpoints of readmission rates, other studies exist within orthopaedic surgery and internal medicine [Citation27,Citation28]. Like our study, they report neutral results on readmission rates from supervised student follow-ups. In line with these studies, we conclude that patient safety is preserved and argue that supervised student clinics have a role in medical education practice.
The non-change of readmission rates in our study that contrast with the studies by Borregaard and Bates may, among others, be caused by the elements of the professional competency of the person conducting the consultation as well as the timing and the content of the patient consultations. For example, the focus on patient empowerment differed between our study and the literature. Furthermore, as readmission rates in our study were considerably lower than expected, the study may be underpowered to detect any difference between groups.
Early detection of imminent complications
Previous studies have stated that readmissions often occur before the first planned follow-up, and timely detection of complications has been proposed to lower readmission rates [Citation4]. Borregaard et al. concluded that the lower readmission rate in their intervention group was primarily driven by fewer unplanned readmissions caused by pericardial effusions or unspecific cardiac symptoms [Citation2]. Due to small patient groups and the well-described limitations in chart-level details, we chose robust outcome parameters such as pericardial and pleural drainages to compare groups. We identified a tendency for earlier detection of the potentially serious condition of pericardial effusion. In the intervention group, pericardial drainage was scheduled (initiated by the student clinic). In the control group, patients were readmitted acutely to the hospital (symptom-driven). Our study does not have the statistical power to support solid conclusions. Still, our findings correspond with previous studies where routine FATE after cardiac surgery has changed patient management [Citation2,Citation29]. The timely detection of imminent complications may support clinical decision-making and treatment strategy and improve procedure safety. Still, as the Choosing Wisely concept advocates, unnecessary tests are aimed to be reduced [Citation30]. Therefore, we need better evidence regarding balancing the detection and treatment of impending post-operative complications, including effusions.
In our study, more patients were drained for pleural effusions in the intervention group, 17% vs 8% (p = 0.01). This is the first study to provide consecutive data for pleural drainage until one year after cardiac surgery. Our findings correspond with a previous study where scheduled point-of-care ultrasound scans changed patient management for 7 of 80 patients within 30 days of surgery [Citation29]. We have previously demonstrated that drainage of pleural effusions improves walking distance and may improve morbidity after cardiac surgery [Citation10]. Few studies have described the consequences of persistent pleural effusions [Citation31]. Long-time follow-up studies on pleural effusions after cardiac surgery are needed to guide best practices.
HRQOL
We did not identify any difference in the HRQOL questionnaire answers between groups in our study. No studies have previously compared HRQOL from two follow-up programmes within one year of cardiac surgery. However, a previous study reported that nurse-practitioner-managed follow-up programs initiated better outcomes regarding physical functioning status two weeks after surgery [Citation19]. The effect of student-led consultation on self-reported quality of life has previously been compared between an interprofessional training unit and standard care, in an orthopaedic team, without difference between groups [Citation32]. We need more extensive comparative studies for solid conclusions on advancing HRQOL after open cardiac surgery.
Implication for clinical and medical education practice
Many papers in clinical medicine address the high unplanned readmission rates after open cardiac surgery [Citation1,Citation2, Citation4–9,Citation11,Citation12,Citation33]. Moreover, in medical education, integrating value-added medical student roles into patient care has been proposed to better patient care and medical education [Citation20]. Thus, establishing a student clinic to conduct follow-ups for newly cardiac-operated patients under supervision seemed plausible.
For patient care, the neutral study outcome where intervention neither improved patient care nor jeopardised patient safety does not argue for implementing the demonstrated set-up. Although patients described a feeling of safety connected to the additional follow-up programme, more time, resources and money were likely spent on the intervention compared to the control group [Citation22]. In contrast, Borregaard et al. decreased unplanned readmission rates and costs [Citation34]. Thus, the potential for better patient care and lower costs exists, but our setup was unfitting.
For medical education practice, we have provided a concrete example of aligning patient care and medical education in a cardiac surgery department [Citation20]. Earlier studies have shown pre-graduate clerkship learning suffers from active student engagement, particularly in surgical departments [Citation35]. Thus, we assume the scheduled student activity enabled students to apply medical knowledge and skills into clinical practice and also to learn the behaviour of a competent physician [Citation36,Citation37].
This study provides a concrete example of integrating a value-added medical student role into a patient care system. Although clinical education demands resources, our results showed unbalance of service versus learning in the presented setup within the measured outcomes. Combined with previous studies, there likely exist a potential to lower readmission rates when optimising patient follow-up after open cardiac surgery. Here medical students may have a more defined role, e.g. to perform FATE, which may better balance service and learning.
Limitations
Limitations of our study include the study design, where patient randomisation was not achieved.
Patients were relocated to their local hospital, where follow-up was conducted. Thus, the two groups may differ in operative and post-operative care, including patient education. Further, 24 of 124 included patients in the intervention group excluded from the data analysis. The excluded patient group can represent patients with the most complications. Although the statistical power calculation for this study was based on data from the same hospital, the readmission rate in our study was lower, thus impairing the study power. Patients who responded to the surveys may represent a biased sample. Future follow-up and research must strive to overcome the current methodological limitations to identify strategies for improvement in follow-up after open cardiac surgery.
Conclusion
This study showed that supervised student-led follow-up of newly cardiac-operated patients did not alter unplanned cardiac-related readmission rates or self-reported health-related quality of life. Detection and treatment of complications such as the potentially serious condition of pericardial effusions appeared safe and allowed more timely detection and treatment than standard follow-up.
Our results conclude that supervised student follow-up after cardiac surgery can be performed with satisfactory patient safety. Still, a different setup may be applicable to balance adding value to patient care and medical education wisely.
Acknowledgments
We owe a great thanks to all participating patients and the medical students for contributing to patient care. We thank Vibeke Laursen and Betina Aalling for their invaluable help during the project. Further, we thank nurses, secretaries, physicians, and other staff in the Central Region of Denmark for contributing to the project.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Adelborg K, Horvath-Puho E, Schmidt M, et al. Thirty-year mortality after coronary artery bypass graft surgery: a Danish nationwide population-based cohort study. Circ Cardiovasc Qual Outcomes. 2017; 10(5):e002708.
- Borregaard B, Dahl JS, Riber LPS, et al. Effect of early, individualised and intensified follow-up after open heart valve surgery on unplanned cardiac hospital readmissions and all-cause mortality. Int J Cardiol. 2019;289:30–36.
- Maniar HS, Bell JM, Moon MR, et al. Prospective evaluation of patients readmitted after cardiac surgery: analysis of outcomes and identification of risk factors. J Thorac Cardiovasc Surg. 2014;147(3):1013–1018.
- Trooboff SW, Magnus PC, Ross CS, et al. A multi-center analysis of readmission after cardiac surgery: experience of the northern New England cardiovascular disease study group. J Card Surg. 2019;34(8):655–662.
- Bates OL, O'Connor N, Dunn D, et al. Applying STAAR interventions in incremental bundles: improving post-CABG surgical patient care. Worldviews Evid Based Nurs. 2014;11(2):89–97.
- Feng TR, White RS, Gaber-Baylis LK, et al. Coronary artery bypass graft readmission rates and risk factors – a retrospective cohort study. Int J Surg. 2018;54(Pt A):7–17. Jun
- Hannan EL, Zhong Y, Lahey SJ, et al. 30-day readmissions after coronary artery bypass graft surgery in New York state. JACC Cardiovasc Interv. 2011; 4(5):569–576.
- Hansen LS, Hjortdal VE, Jakobsen CJ. Relocation of patients after cardiac surgery: is it worth the effort? Acta Anaesthesiol Scand. 2016; 60(4):441–449.
- Hirji SA, Percy ED, Zogg CK, et al. Thirty-day nonindex readmissions and clinical outcomes after cardiac surgery. Ann Thorac Surg. 2020;110(2):484–491.
- Hansen LS, Hjortdal VE, Jakobsen CJ, et al. Early, dedicated follow-up and treatment of pleural effusions enhance the recovery rate after open cardiac surgery: results from a randomized, clinical trial. Eur J Cardiothorac Surg. 2017;51(1):58–66.
- Weiss MG, Moller JE, Dahl JS, et al. Causes and characteristics associated with early and late readmission after open-heart valve surgery. J Card Surg. 2020;35(4):747–754.
- Shahian DM, He X, O'Brien SM, et al. Development of a clinical registry-based 30-day readmission measure for coronary artery bypass grafting surgery. Circulation. 2014;130(5):399–409.
- Shawon MSR, Odutola M, Falster MO, et al. Patient and hospital factors associated with 30-day readmissions after coronary artery bypass graft (CABG) surgery: a systematic review and meta-analysis. J Cardiothorac Surg. 2021;16(1):172.
- Hansen LS, Hjortdal VE, Andreasen JJ, et al. 30-day mortality after coronary artery bypass grafting and valve surgery has greatly improved over the last decade, but the 1-year mortality remains constant. Ann Card Anaesth. 2015;18(2):138–142.
- Ashikhmina EA, Schaff HV, Sinak LJ, et al. Pericardial effusion after cardiac surgery: risk factors, patient profiles, and contemporary management. Ann Thorac Surg. 2010;89(1):112–118.
- Light RW. Pleural effusions after coronary artery bypass graft surgery. Curr Opin Pulm Med. 2002; 8(4):308–311.
- Pepi M, Muratori M, Barbier P, et al. Pericardial effusion after cardiac surgery: incidence, site, size, and haemodynamic consequences. Br Heart J. 1994;72(4):327–331.
- Baig K, Harling L, Papanikitas J, et al. Does coronary artery bypass grafting improve quality of life in elderly patients? Interact Cardiovasc Thorac Surg. 2013;17(3):542–553.
- Sawatzky JA, Christie S, Singal RK. Exploring outcomes of a nurse practitioner-managed cardiac surgery follow-up intervention: a randomized trial. J Adv Nurs. 2013; 69(9):2076–2087.
- Gonzalo JD, Dekhtyar M, Hawkins RE, et al. How can medical students add value? Identifying roles, barriers, and strategies to advance the value of undergraduate medical education to patient care and the health system. Acad Med. 2017;92(9):1294–1301.
- Heiberg J, Hansen LS, Wemmelund K, et al. Point-of-care clinical ultrasound for medical students. Ultrasound Int Open. 2015;1(2):E58–66.
- Kjaer LB, Ilkjaer C, Hoffmann T, et al. Exploring patient experiences in the student outpatient clinic – a contribution to learning. Patient Educ Couns. 2021;104(11):2756–2762.
- Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. EuroIntervention. 2022;17(14):e1126–e1196.
- Jensen MB, Sloth E, Larsen KM, et al. Transthoracic echocardiography for cardiopulmonary monitoring in intensive care. Eur J Anaesthesiol. 2004;21(9):700–707.
- Schmidt M, Maeng M, Jakobsen CJ, et al. Existing data sources for clinical epidemiology: the western Denmark heart registry. Clin Epidemiol. 2010;2:137–144.
- Harris PA, Taylor R, Minor BL, et al. The RED Cap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- Hallin K, Gordon M, Skoldenberg O, et al. Readmission and mortality in patients treated by interprofessional student teams at a training ward compared with patients receiving usual care: a retrospective cohort study. BMJ Open. 2018;8(10):e022251.
- Au AG, Padwal RS, Majumdar SR, et al. Patient outcomes in teaching versus nonteaching general internal medicine services: a systematic review and meta-analysis. Acad Med. 2014;89(3):517–523.
- Christiansen LK, Frederiksen CA, Juhl-Olsen P, et al. Point-of-care ultrasonography changes patient management following open heart surgery. Scand Cardiovasc J. 2013;47(6):335–343.
- Choosing Wisely. Available from: https://www.choosingwisely.org/societies/the-society-of-thoracic-surgeons/.
- Kollef MH. Chronic pleural effusion following coronary artery revascularization with the internal mammary artery. Chest. 1990; 97(3):750–751.
- Hansen TB, Jacobsen F, Larsen K. Cost effective interprofessional training: an evaluation of a training unit in Denmark. J Interprof Care. 2009;23(3):234–241.
- Maniar H. Hospital readmissions after cardiac surgery: is it a game worth playing? J Thorac Cardiovasc Surg. 2015; 149(3):858.
- Borregaard B, Moller JE, Dahl JS, et al. Early follow-up after open heart valve surgery reduces healthcare costs: a propensity matched study. Open Heart. 2019;6(2):e001122.
- Brennan N, Corrigan O, Allard J, et al. The transition from medical student to junior doctor: today’s experiences of tomorrow’s doctors. Med Educ. 2010; 44(5):449–458.
- Ginsburg S, Regehr G, Hatala R, et al. Context, conflict, and resolution: a new conceptual framework for evaluating professionalism. Acad Med. 2000;75(10 Suppl):S6–S11.
- Dornan T, Conn R, Monaghan H, et al. AMEE guide 129 experience based learning (ExBL): clinical teaching for the twenty-first century. Lilley P, editor. Dundee, UK: Association for Medical Education in Europe (AMEE); 2018.