Abstract
Objectives. This study investigated the influence of higher pressure protection with a small diameter balloon of side branch (SB) on bifurcation lesions. Background. Of the different coronary stent implantation techniques, the modified jailed balloon technique has become a viable option for bifurcation lesions. However, there was no detailed study on the relationship between the balloon inflation pressure of the main vessel (MV) and SB. Methods. In this study, we collected information of patients who underwent percutaneous coronary intervention (PCI) for bifurcated lesions between March 2019 and December 2022. They were divided into two groups according to the operation way: active jailed balloon technique (A-JBT) group and jailed wire technique (JWT) group. Results. A total of 216 patients were enrolled. The A-JBT group had a larger SB stenosis diameter (1.53 ± 0.69 vs. 0.95 ± 0.52, p < .001), the lower degree of stenosis (44.34 ± 18.30 vs. 63.69 ± 17.34, p < .001) compared to the JWT group. However, the JWT group had a higher incidence of SB occlusion (18.0% vs. 1.9%, p < .001) compared to the A-JBT group. Nevertheless, the success rate for both groups was 100%. Conclusions. This novel high inflation pressure and small diameter balloon approach we propose has significant advantages. There is a lower rate of SB occlusion and SB dissection, which is more cost-effective and provides better clinical outcomes for the patient. This method should be considered in the future for treating bifurcation lesions.
1. Introduction
Coronary artery bifurcation lesions constitute approximately 15–20% of all percutaneous coronary intervention (PCI) [Citation1]. PCI success is usually lower in patients with true bifurcation lesions [Citation2]. The double-stent and single-stent methods are the mainstream treatment strategies for bifurcation lesions, but their advantages and disadvantages remain controversial. A study found that the single-stent strategy had higher safety and lower cost long-term follow-up [Citation3]. Currently, the simple single-stent implantation strategy is more popular than the complex double-stent implantation strategy [Citation4]. However, this approach is associated with many complications, among which occlusion of the side branch (SB) can be serious [Citation5]. To overcome this challenge, operators usually use the jailed wire technique (JWT) to assist in restoring blood flow in the SB [Citation6]. Nevertheless, this method is not 100% foul-proof for preventing SB occlusion, because the protection space of the wire is small and cannot prevent the plaque or protrusions from migrating from the main vessel (MV) to the SB [Citation7].
Burzotta et al. proposed the "jailed balloon" technique as the novel SB protection strategy, which can protect the SB during single-stent implantation for bifurcation lesions. The balloon placed under the stent strut without inflation can not only serve as a marker to assist in rewiring but also be inflated to restore blood flow in the SB [Citation7]. Additionally, the CIT-RESOLVE randomized controlled trial found that an active SB protection strategy, specifically the jailed balloon technique, is feasible and significantly reduces the incidence of SB occlusion for high-risk bifurcation lesions [Citation8]. In addition, Depta et al. conducted a case-control study in which the efficacy of jailed balloon in treating non-left main bifurcation lesions was examined, demonstrating that the occlusion rate in the jailed balloon group was significantly lower than that in the non-jailed balloon group [Citation9]. Although the balloon of SB was not inflated during the procedure, the space occupied by the balloon at the SB opening could reduce plaque migration to the SB. Unfortunately, it cannot completely prevent SB occlusion.
Of the different coronary stent implantation techniques, the modified jailed balloon technique has become a viable option. Saito et al. proposed a new jailed balloon technique called the "active" jailed balloon technique, which can effectively prevent SB occlusion, and its biggest characteristic is that the SB balloon is inflation [Citation10]. In addition, a retrospective cohort study from Japan proposed a modified jailed balloon technique, and the inflation pressure of the SB balloon does not affect the SB compromise, but the sample size of the study was small and it was not compared with the wire protection technique [Citation11]. Therefore, this cohort study explored the application of a novel modified jailed balloon technique, comparing it to the JWT. The position and inflation method of the SB and MV balloons will be discussed in detail.
2. Methods
2.1. Study design and study population
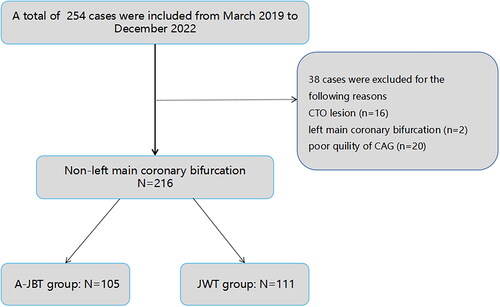
This is a retrospective cohort study, which consecutively enrolled 254 patients with bifurcation lesions at the Second Hospital of Tianjin Medical University, Tianjin, China (between March 2019 and December 2022; ). The study was designed with the principles of the Declaration of Helsinki and was approved by the ethics committee of The Second Hospital of Tianjin Medical University (Ethical Approval Number: KY2023K187). These patients had bifurcation lesions with organic stenosis caused by atherosclerotic coronary artery disease, which resulted in myocardial ischemia or acute coronary syndrome. The bifurcation lesions, with the MV diameter ≥2.5 mm and SB diameter ≥1.5 mm, were evaluated by visual estimation on coronary angiography (CAG). The protected branch was determined by the operator through comprehensive consideration of the surgery with the aim of preserving the SB. The Medina classification was used to stratify the bifurcation lesion according to visual estimation by the operator. The exclusion criteria were left main stem lesion, chronic total occlusion (CTO) and the bifurcation lesions were considered unsuitable for quantitative coronary angiographic (QCA) analysis according to CAG including opening lesions, poor image quality, hindrance of accurate lumen border delineation, severe overlapping or tortuosity of the vessels and presence of a myocardial bridge during vessel measurement. After exclusion, patients with non-left main bifurcation lesions were defined as study subjects and fully evaluated at baseline and during surgery by quantitative CAG analysis. Non-left main bifurcation lesions are defined as lesions that do not involve the left main coronary artery [Citation12]. SB occlusion was defined as SB loss or SB blood flow of thrombolysis in myocardial infarction (TIMI) grade <3.
Figure 1. Our study consecutively enrolled 254 patients with bifurcation lesions at the Second Hospital of Tianjin Medical University, Tianjin, China (between March 2019 and December 2022). Exclusion criteria included left main stem lesion, chronic total occlusion and the bifurcation lesions were considered unsuitable for quantitative coronary angiographic analysis according to CAG. Finally, 216 cases with non-left main bifurcation lesions were defined as the study subjects.
2.2. Active jailed balloon technique (A-JBT) and jailed wire technique
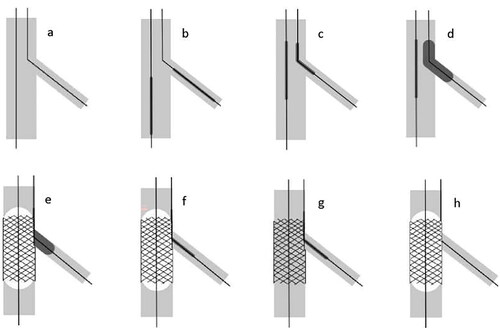
A-JBT: Guidewires were introduced into both the MV and the SB (), and the MV was pre-dilated with a balloon first. The MV stent was placed to the distal of the bifurcation lesion before the jailed balloon was placed in SB (). The MV stent was then withdrawn to an appropriate position that could cover the MV lesion, and the mid-segment of the jailed balloon was adjusted to be located at the ridge of the lesion (). The SB balloon was inflated, and the position of the stent was verified by angiography (). The MV stent was then inflated (), and the pressure of the MV stent balloon should be lower than that of the jailed balloon. Besides, the pressure of the jailed balloon was above 10 atm. The MV stent balloon was deflated first (), followed by the jailed balloon (). The MV stent balloon was kept inside the MV stent, and the blood flow of the SB was observed by angiography. If the SB TIMI grade was ≥3 and there was no dissection, the SB balloon was withdrawn into the guiding catheter and the MV stent balloon was re-inflated to make the stent appose the vessel wall (). According to the expansion of the stent, the diameter of the stent or a slightly larger semi-compliant balloon was selected for further inflation. If there was no significant change in the SB stenosis and the TIMI ≥3, the operation was considered complete. Otherwise, the SB wire was rewired and balloon-stent kissing technique (BKST) or SB stenting was performed if necessary.
Figure 2. The procedure of the modified active jailed balloon technique. (a) Two guidewires were introduced into both the MV and the SB. (b) The MV was pre-dilated with a balloon first. The MV stent was placed to the distal of the bifurcation lesion before the jailed balloon was placed in SB. (c) The MV stent was withdrawn to an appropriate position that could cover the MV lesion, and the mid-segment of the jailed balloon was adjusted to be located at the ridge of the lesion. (d) The SB balloon was inflated, and the position of the stent was verified by angiography. (e) The MV stent was then inflated. (f) The MV stent balloon was deflated. (g) The jailed balloon was deflated. (h) The MV stent balloon was re-inflated to make the stent appose the vessel wall.
JWT: Guidewires were placed into both the MV and the SB, and the MV was pre-dilated with a balloon. Then, the MV stent was placed and inflated. If the SB TIMI grade was 3 at this time, the SB wire was withdrawn, and according to the inflation of the MV stent, a semi-compliant balloon was selected for further dilation. If there was no significant change in the SB stenosis and the TIMI grade was 3, the treatment was considered complete. Otherwise, the SB wire was rewired and simple dilation or kissing balloon dilation was performed, and the SB stent was implanted if necessary.
2.3. Quantitative coronary angiography analysis
Both MV and SB of target bifurcation lesions were analyzed by QCA. The best projection with the minimum vessel foreshortening and clearest vessel visualization was selected for QCA analysis. The lesion length of the main branch, the reference diameter and the stenotic diameter at the proximal and distal ends of the main branch before and after the procedure, and the lesion length, reference diameter and stenotic diameter of the SB before and after the procedure were measured.
2.4. Statistical analysis
Data analysis was performed using SPSS 25.0 (IBM Corp., Armonk, NY). Mean ± standard deviation was used to express measurement data, Student’s t-test was used to make comparisons between the two groups. Count data were expressed as n (%) and compared between groups using the Chi-square test or Fisher’s exact probability method. The univariable and multivariable were analyzed by the logistic test. p < .05 was considered to be statistically significant.
3. Results
3.1. Baseline data
A total of 216 patients were included in the final analysis with 105 and 111 patients undergoing A-JBT and JWT, respectively. The mean age of the cohort was 65.56 ± 9.87 years. Of these, 163 cases (75.5%) involve the left anterior descending (LAD) artery and 139 cases (64.7%) present with unstable angina pectoris. Moreover, 205 cases (94.91%) were confirmed as true bifurcation lesions (Medina classification 1.1.1, 1.0.1, 0.1.1). At baseline, gender, age, coronary heart disease diagnosis, left ventricular ejection fraction (LVEF) and other baseline dates were not significantly different ().
Table 1. Demographic and clinical characteristics of the study patients.
3.2. Surgical and clinical outcomes
As shown in , both groups had a 100% success rate. After PCI, the A-JBT group had a larger SB stenosis diameter (1.53 ± 0.69 vs. 0.95 ± 0.52, p < .001), lower degree of stenosis (44.34 ± 18.30 vs. 63.69 ± 17.34, p < .001) and smaller change in SB stenosis degree (−16.06 ± 22.48 vs. 8.12 ± 17.15, p < .001) compared to the JWT group. Both groups achieved TIMI grade 3 blood flow in the main treated vessel, but the JWT group had a higher incidence of SB occlusion (18.0% vs. 1.9%, p < .001) compared to the A-JBT group. Both groups had no significant differences in terms of perioperative myocardial infarction, adverse events during hospitalization or anti-angina and anti-thrombotic drug treatments.
Table 2. QCA analysis of targeted lesions in the initial and final angiography.
Furthermore, the A-JBT group was more likely to achieve balloon kissing (23.8% vs. 11.7%, p = .02), but there was no significant statistical difference in operative time between the two groups (29.26 ± 13.32 vs. 31.76 ± 15.06, p = .199). In terms of stent and balloon selection, the MV stent diameter (3.00 (2.75, 3.50) vs. 3.00 (2.75, 3.00), p < .001) differed between the two groups, as did the reference balloon diameter (2.00 (2.00, 2.50) vs. 2.00 (2.00, 2.50), p = .028), MV pre-dilation balloon length (20.00 (16.00, 20.00) vs. 16.00 (15.00, 20.00), p < .001) and MV pre-dilation balloon pressure (12.59 ± 3.06 vs. 10.86 ± 2.89, p < .001) in . Additionally, there were no significant differences in terms of serum levels of cardiac troponin T, low-density lipoprotein, creatine kinase (CK), CK-MB, D-dimer, or NT-proBNP between the two groups in and .
Table 3. The characteristics of stent and balloon.
Table 4. Medications and laboratory test results during hospitalization.
Table 5. Procedural outcomes of A-JBT and JWT.
3.3. Univariable and multivariable analyses of SB occlusion
The significant predictors of SB occlusion were identified using logistic regression (). Receiver operating characteristic (ROC) analysis was performed, allowing the cut-off values to be determined: MV proximal stenosis degree of 55.80%; MV distal stenosis degree of 83.86%; SB lesion length of 8.62 mm; SB reference diameter of 2.51 mm and SB stenosis diameter of 0.64 mm, bifurcation angle 45.3°. Univariable analysis was performed on several parameters affecting the results of PCI, and significant associations were found with MV proximal stenosis degree ≥55.80% (p = .011), SB reference vessel diameter ≤2.51 mm (p = .045), SB minimum lumen diameter ≤0.64 mm (p = .001), and bifurcation angle ≥45.3° (p = .02). In the multivariable analysis, the statistical significance of SB reference vessel diameter was offset, but MV proximal stenosis degree ≥55.8% (OR = 3.25 [1.11–9.53], p = .034), SB lesion length ≥8.62 mm (OR = 4.55 [1.37–15.14], p = .013), SB minimum lumen diameter ≤0.64 mm (OR = 4.85[1.68–14.02], p = .004), and bifurcation angle ≥45.3° (OR = 5.62 [1.59–19.84], p = .007) remained significant.
Table 6. Univariable and multivariable analyses for SB occlusion.
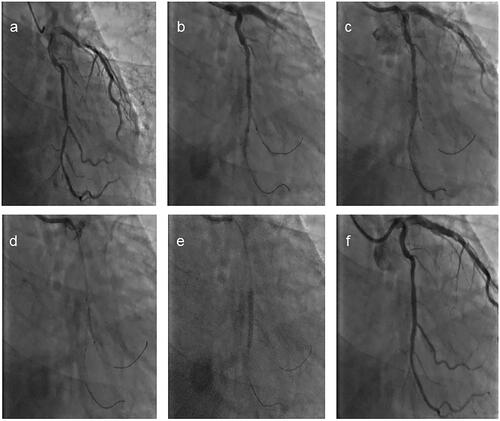
An example case is illustrated here: A PCI procedure was performed on a 67-year-old male patient with a bifurcation lesion in the mid-segment of the left circumflex artery, with the use of an improved active deflection balloon technique for SB protection. The MV was pre-dilated with a 2.5 mm × 16 mm balloon at 16 atm, then a 3.5 mm × 20 mm stent was placed at 8 atm. The SB was protected with a 1.5 mm × 16 mm balloon at 11 atm, and postprocedure assessment revealed no significant increase in the degree of SB stenosis ().
Figure 3. A PCI procedure was performed on a 67-year-old male patient with a bifurcation lesion in the mid-segment of the left circumflex artery. (a) The CAG displayed that was a true bifurcation of the LCX/OM. (b) The stent (3.5 mm × 20 mm) was withdrawn to an appropriate position that cover the MV lesion, and the mid-segment of the jailed balloon (1.5 mm × 16 mm) was adjusted to be located at the ridge of the lesion. (c) The MV stent was inflated at 8 atm and the jailed balloon was inflated at 11 atm. (d) The MV stent balloon was deflated. (e) The MV stent balloon was re-inflated to make the stent appose the vessel wall. (f) The diameter stenosis of the side branch had a significant improvement.
4. Discussion
Even in the era of drug-eluting stents, stent implantation in bifurcation lesions of the coronary arteries is still challenging and is correlated with higher incidence of procedural complications and adverse cardiovascular events [Citation13], mainly due to the complexity of the anatomy and the potential changes that may occur during PCI of bifurcation lesions. Plaque or protrusion displacement at the bifurcation ridge during PCI, vessel spasm, changes in the bifurcation angle and SB dissection can all lead to adverse clinical outcomes such as SB occlusion. This study explored the optimal surgical approach for bifurcation lesions by comparing the effect of higher pressure A-JBT and JWT on SB occlusion in non-left main bifurcation lesions.
We proposed a new modified jailed balloon technique and compared it with JWT. The results showed that our way had a lower rate of SB occlusion compared with jailed wire technology (1.9% vs. 18.0%, p < .001). In the A-JBT, the diameter, length and pressure of the SB balloon may affect the involvement of the SB [Citation14]. Therefore, the main innovations of our study also lie in these three aspects. First, in terms of balloon diameter selection, to prevent SB dissection caused by the jailed balloon’s excessive compression of the bifurcation opening, we tended to choose a balloon that is smaller than the reference diameter of the SB, with a diameter of 2.5 mm accounting for 55.2% and a diameter of 2.0 mm accounting for 30.4%. As the balloon tends to expand most completely at the middle during vascular release, we placed the distal end of the balloon in the normal vascular segment of the SB and the middle of the balloon at the bifurcation opening to achieve better spatial occupancy. The plaque and protrusion displacement caused by the compression after the MV stent implantation are the main cause of SB occlusion [Citation14], so we chose a higher inflation pressure for the jailed balloon more than the pressure of the MV stent balloon. This higher pressure could better prevent plaques and protrusion from migrating and achieve protective effects on the SB.
For the effectiveness of the patients’ procedure, we did not have a low-pressure balloon group for comparison. And there is a study showing no significant advantage of high inflation pressures for SB balloons but the sample size of the study was small and it was not compared with the wire protection technique [Citation11]. In the cases handled by our modified A-JBT, there was no case of SB dissection, the rate of SB occlusion was significantly lower and the degree of stenosis in the SB was significantly improved, which is more cost-effective for the patient. In addition, compared with the JWT group, the A-JBT group required more kissing balloon inflations, but there was no statistically significant difference between the two groups in terms of operative time. This illustrates that the A-JBT did not prolong the radiation time of the patient and the operator, and it also proved the safety of the surgical procedure.
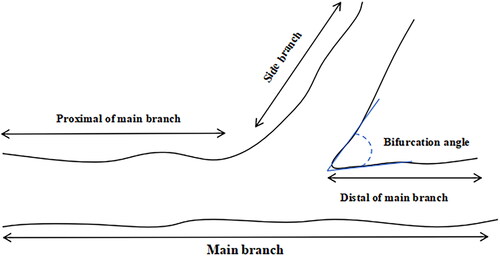
In the multivariable analysis for SB occlusion, the MV proximal stenosis degree ≥55.80% could increase the risk of SB occlusion, which was consistent with some research results [Citation5]. The degree of narrowing at the proximal end of the main lesion has a greater impact on the SB than that at the distal end. Plaque shift was significantly associated with plaque volume reduced in the proximal segment of MV but not in the distal segment of MV by intravascular ultrasound (IVUS) analysis [Citation14]. In addition, the length of the SB lesion ≥8.62 mm is also significantly associated with SB occlusion, which suggests that preventive measures should be taken when treating bifurcation lesions with longer SB lengths. Direct SB post-dilatation or BKST after MV stent inflation can reduce the time of myocardial ischemia caused by SB occlusion. The impact of the bifurcation angle on the occlusion rate of SB during PCI of bifurcation lesions remains a topic of debate. The bifurcation angle is defined in . Some researches have reported a higher SB involvement, restenosis and major adverse cardiovascular events rate with smaller bifurcation angles [Citation15]. Nonetheless, Yoshitaka Goto et al. mentioned that the bifurcation angle was not correlated with SB involvement after main branch stent implantation [Citation16]. In our study, we find the connection between the larger bifurcation angle and SB occlusion. This is partly due to the fact that as the bifurcation angle increases, wall shear stress decreases and the oscillatory shear index near the protrusion significantly increases, promoting plaque formation and intimal hyperplasia at the bifurcation lesion [Citation17,Citation18]. When squeezed by the MB stent, the SB is more susceptible to occlusion due to protrusion and plaque displacement [Citation14,Citation19]. Another reason may be related to the increased pressure drop and flow resistance [Citation20]. Furthermore, bifurcation angle ≥50° was also found to be an independent predictor of major adverse cardiovascular events following stenting of bifurcation lesions during long-term follow-up [Citation21].
This study has several limitations, primarily being a retrospective study from a single center. Thus, selection bias for the A-JBT or JWT is unavoidable. Additionally, only non-left main bifurcation lesions were included, so the limited applicability concerning SB occlusion and target lesion remained. Third, due to the retrospective study, no 12-month follow-up CAG was performed to assess the progression of bifurcation lesions in patients after the procedure.
5. Conclusions
Our study innovatively proposes the concept that the higher inflation pressure of the SB’s balloon compared to the MV stent balloon and has improved the PCI process. The JWT group had a higher incidence of SB occlusion compared to the A-JBT group and this was no case of SB dissection in the A-JBT group. This method should be considered in the future for treating bifurcation lesions.
Author contributions
Jiuchun Qiu (MD) participated in the conception and design of the experiments. Longyan Li (MM) contributed to data collection and data analysis. Weiding Wang (MD) is the JBT technique operator. Xinjian Li (MD) contributed to statistical analysis of data. Zizhao Zhang (MM) is also the technique operator. Shuai Shao (MD) provided the financial support and participated in data analysis. Guangping Li (MD, Dr) improved the case screening method. Gary Tse (Dr) and Tong Tiu (MD, Dr) contributed to article writing. All authors contributed to and approved the submission of the article.
Supplementary_Material
Download Zip (1.4 MB)Acknowledgements
The authors would like to acknowledge their colleagues in the department and other study participants for their valuable contributions and all of them agreed to submit the article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Louvard Y, Thomas M, Dzavik V, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008;71(2):175–183. doi: 10.1002/ccd.21314.
- Park TK, Park YH, Song YB, et al. Long-term clinical outcomes of true and non-true bifurcation lesions according to medina classification-results from the COBIS (Coronary Bifurcation Stent) II Registry. Circ J. 2015;79(9):1954–1962. doi: 10.1253/circj.CJ-15-0264.
- Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions. Circulation. 2010;121(10):1235–1243. [Database] doi: 10.1161/CIRCULATIONAHA.109.888297.
- Hildick-Smith D, Lassen J, Albiero R, et al. Consensus from the 5th European Bifurcation Club Meeting. EuroIntervention. 2010;6(1):34–38. doi: 10.4244/EIJV6I1A6.
- Hahn J-Y, Chun WJ, Kim J-H, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions. J Am Coll Cardiol. 2013;62(18):1654–1659. doi: 10.1016/j.jacc.2013.07.041.
- Lassen J, Burzotta F, Banning A, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th Consensus Document from the European Bifurcation Club. EuroIntervention. 2018;13(13):1540–1553. doi: 10.4244/EIJ-D-17-00622.
- Burzotta F, De Vita M, Sgueglia G, et al. How to solve difficult side branch access? EuroIntervention. 2010;6(Suppl. J):J72–J80.
- Dou K, Zhang D, Pan H, et al. Active SB-P versus conventional approach to the protection of high-risk side branches: the CIT-RESOLVE trial. JACC Cardiovasc Interv. 2020;13(9):1112–1122.
- Depta JP, Patel Y, Patel JS, et al. Long-term clinical outcomes with the use of a modified provisional jailed-balloon stenting technique for the treatment of nonleft main coronary bifurcation lesions. Catheter Cardiovasc Interv. 2013;82(5):E637–E646. doi: 10.1002/ccd.24778.
- Saito S, Shishido K, Moriyama N, et al. Modified jailed balloon technique for bifurcation lesions. Catheter Cardiovasc Interv. 2018;92(3):E218–E226. doi: 10.1002/ccd.2733429205789
- Nomura T, Wada N, Ota I, et al. Inflation pressure in side branch during modified jailed balloon technique does not affect side branch outcomes. J Interv Cardiol. 2021;2021:8839897.
- Louvard Y, Medina A. Definitions and classifications of bifurcation lesions and treatment. EuroIntervention. 2015;11(Suppl. V):V23–V26.
- Al Suwaidi J, Yeh W, Cohen HA, et al. Immediate and one-year outcome in patients with coronary bifurcation lesions in the modern era (NHLBI dynamic registry). Am J Cardiol. 2001;87(10):1139–1144.
- Koo B-K, Waseda K, Kang H-J, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010;3(2):113–119. doi: 10.1161/CIRCINTERVENTIONS.109.887406.
- Gil RJ, Vassilev D, Formuszewicz R, et al. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol. 2009;22(6):E1–E10.
- Yoshitaka Goto Y, Kawasaki T, Koga N, et al. Plaque distribution patterns in left main trunk bifurcations: prediction of branch vessel compromise by multidetector row computed topography after percutaneous coronary intervention. EuroIntervention. 2012;8(6):708–716. doi: 10.4244/EIJV8I6A110.
- Huo Y, Finet G, Lefevre T, et al. Which diameter and angle rule provides optimal flow patterns in a coronary bifurcation? J Biomech. 2012;45(7):1273–1279. doi: 10.1016/j.jbiomech.2012.01.033.
- Sayed Razavi M, Shirani E. Development of a general method for designing microvascular networks using distribution of wall shear stress. J Biomech. 2013;46(13):2303–2309. doi: 10.1016/j.jbiomech.2013.06.005.
- Rodriguez-Granillo GA. Coronary artery remodelling is related to plaque composition. Heart. 2005;92(3):388–391. doi: 10.1136/hrt.2004.057810.
- Dou K, Zhang D, Xu B, et al. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE Score System. JACC Cardiovasc Interv. 2015;8(1):39–46. doi: 10.1016/j.jcin.2014.08.011.
- Dzavik V, Kharbanda R, Ivanov J, et al. Predictors of long-term outcome after crush stenting of coronary bifurcation lesions: importance of the bifurcation angle. Am Heart J. 2006;152(4):762–769. doi: 10.1016/j.ahj.2006.04.033.